The Effects of n-3 PUFA Supplementation on Bone Metabolism Markers and Body Bone Mineral Density in Adults: A Systematic Review and Meta-Analysis of RCTs
Abstract
:1. Introduction
2. Methods
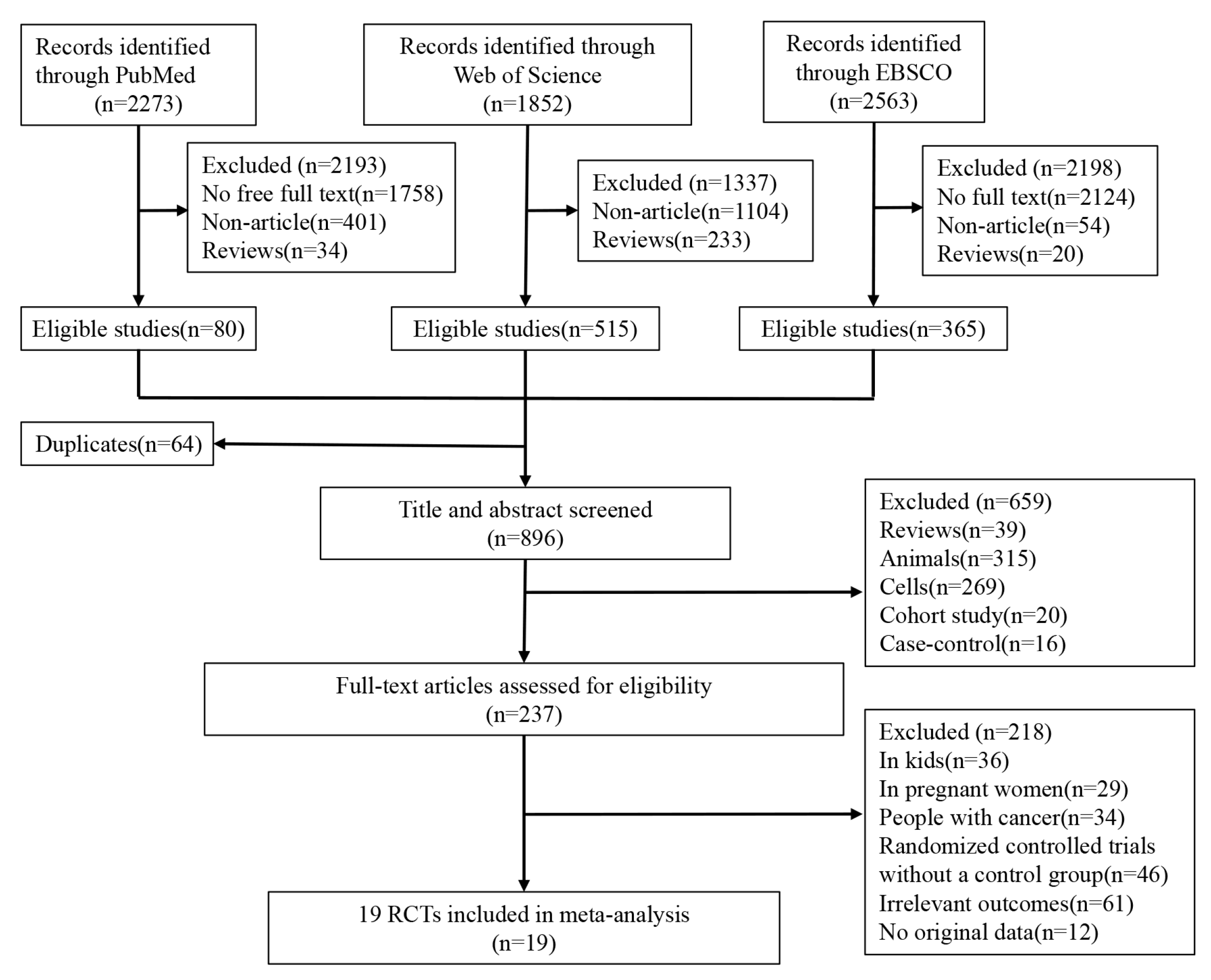
2.1. Search Strategy and Selection Criteria
2.2. Assessment of Study Quality
2.3. Statistical Analysis
3. Results
3.1. Overview of Included Articles
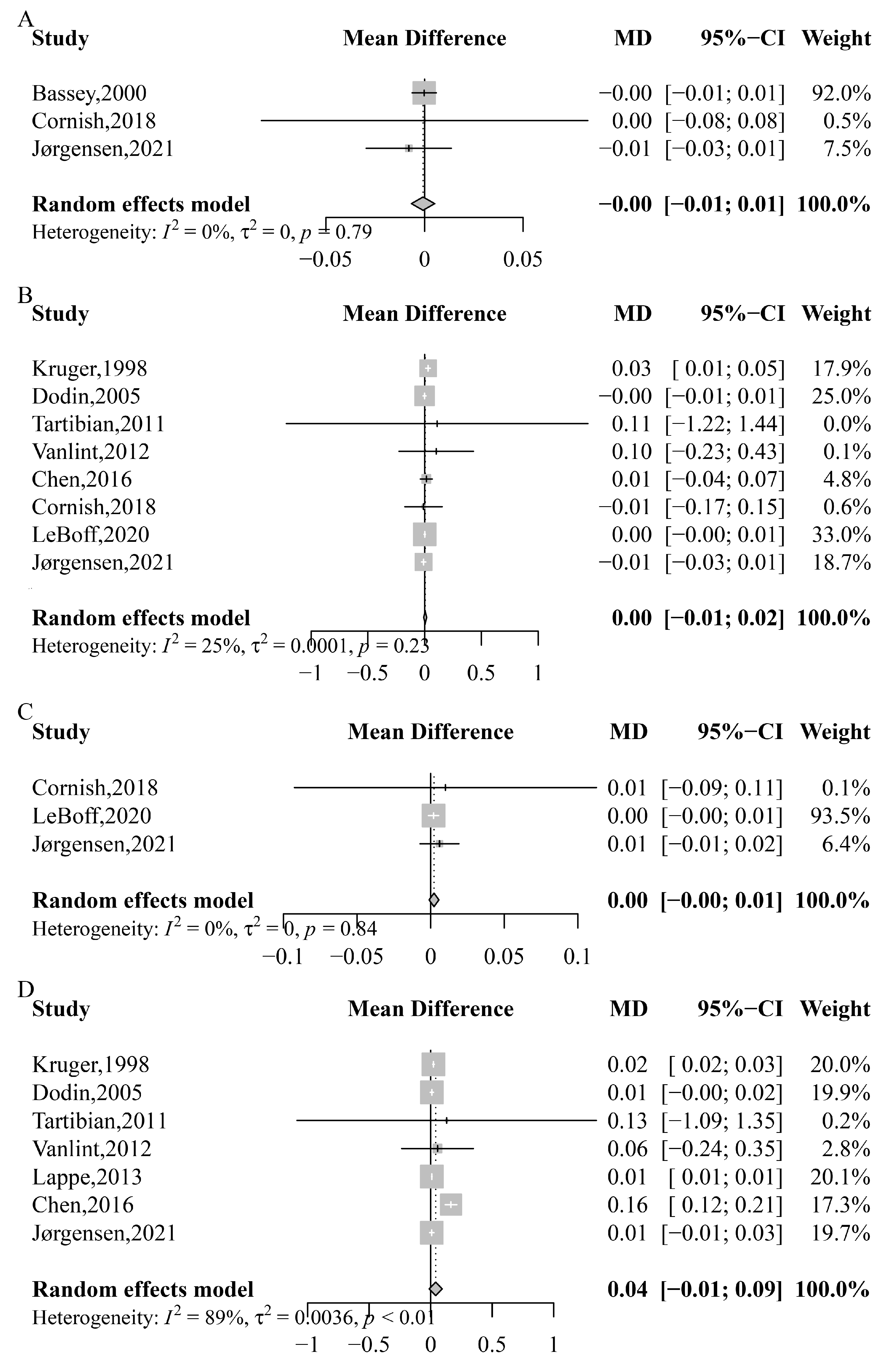
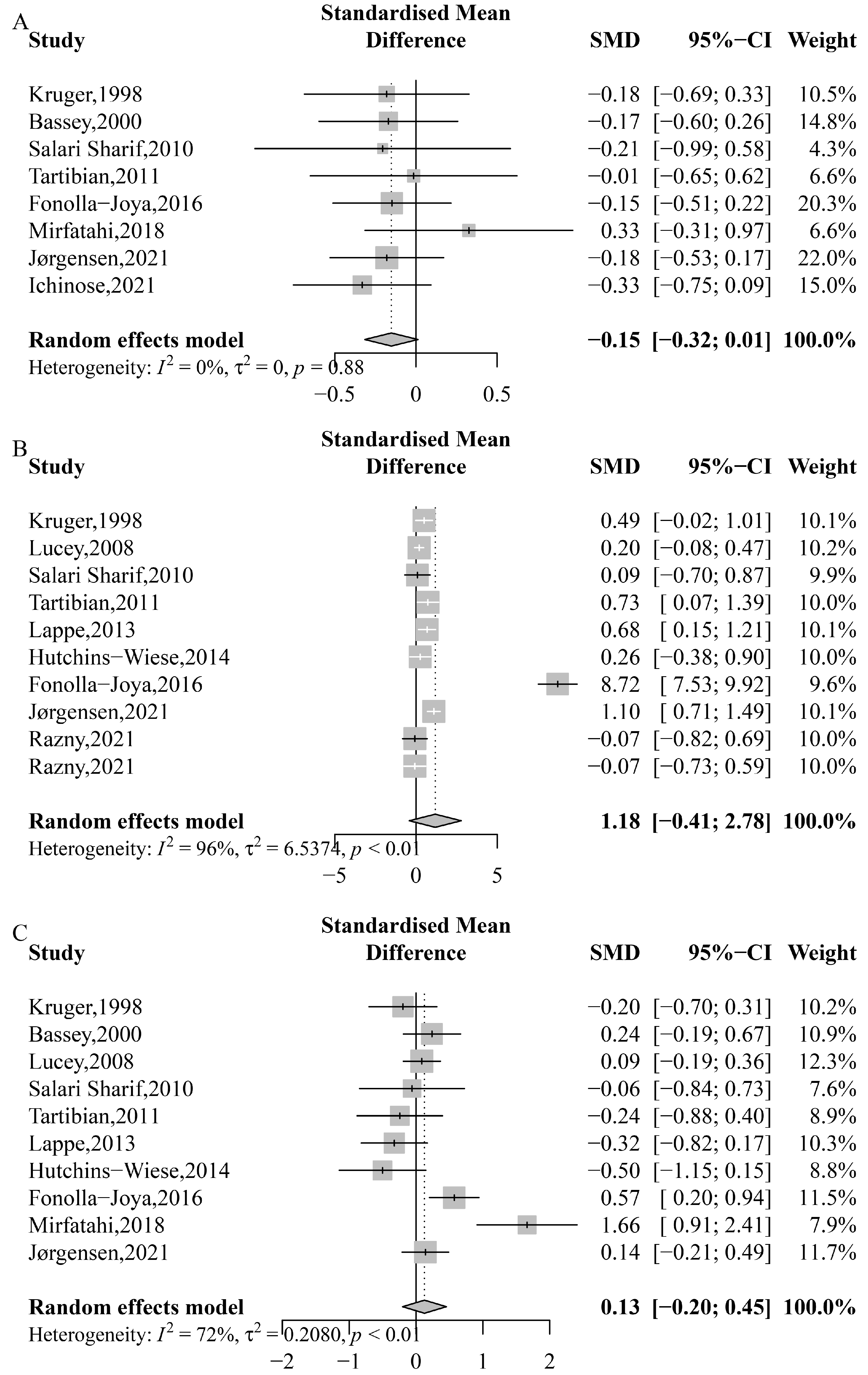
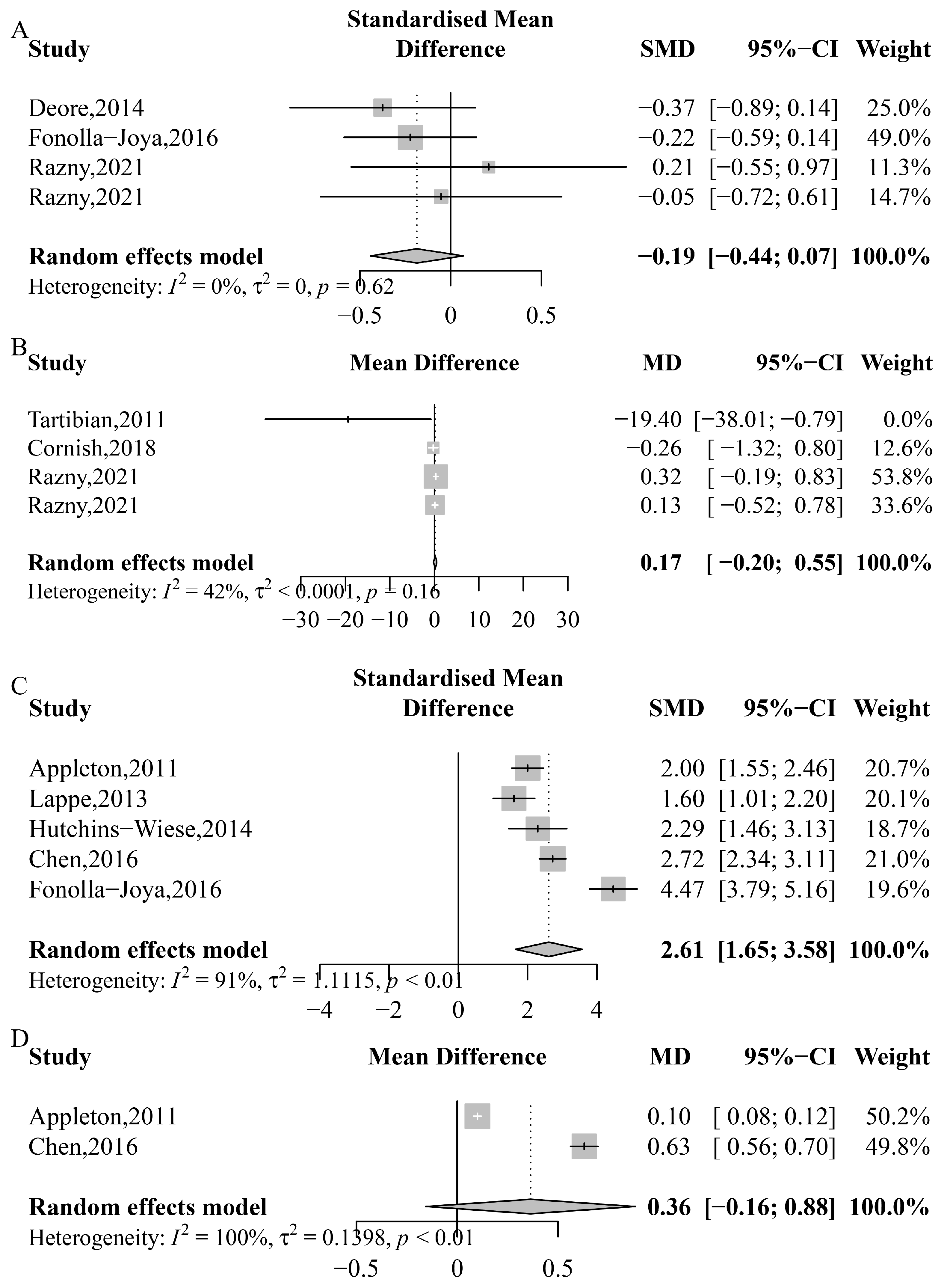
3.2. Bone Mineral Density
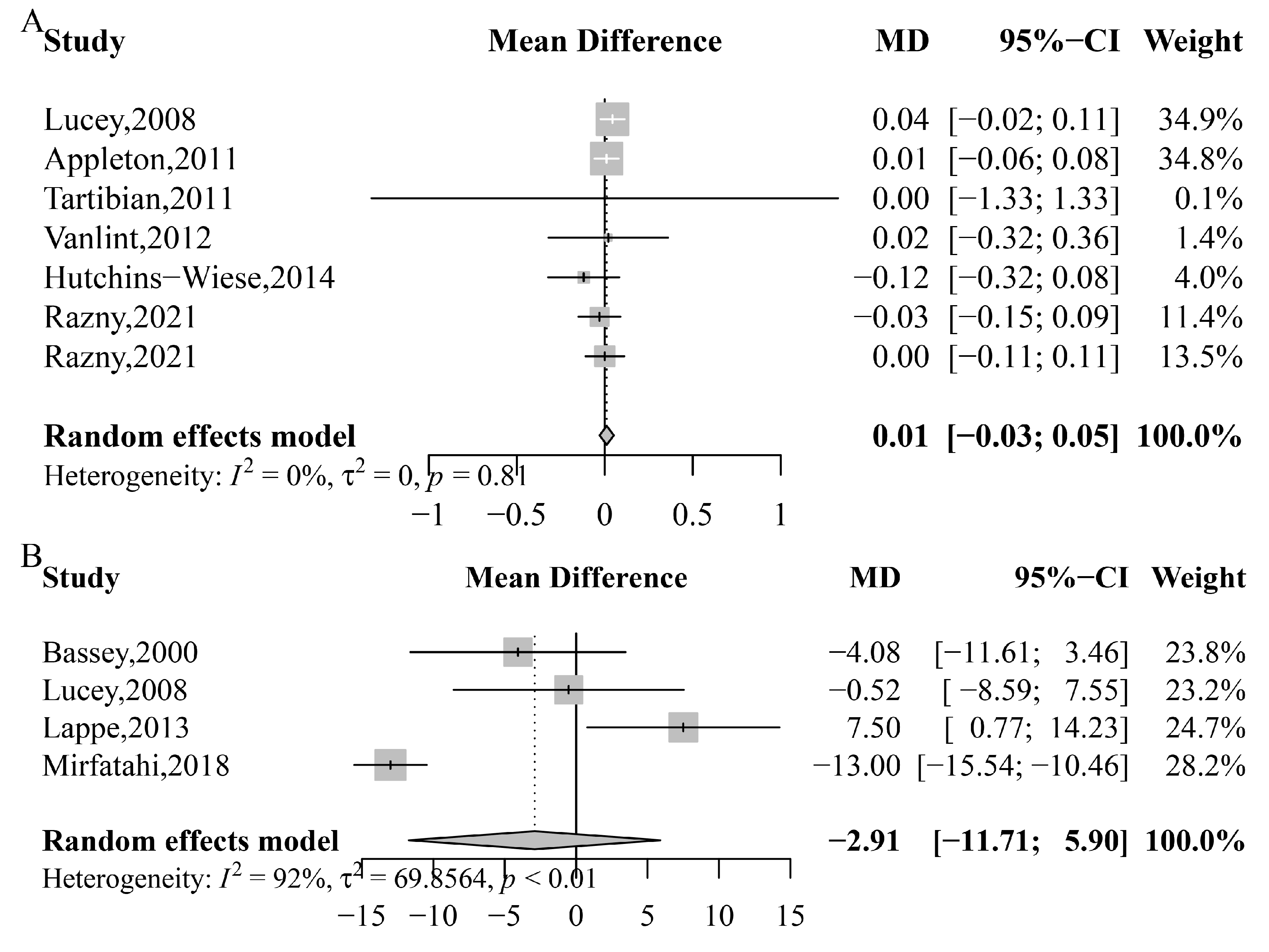
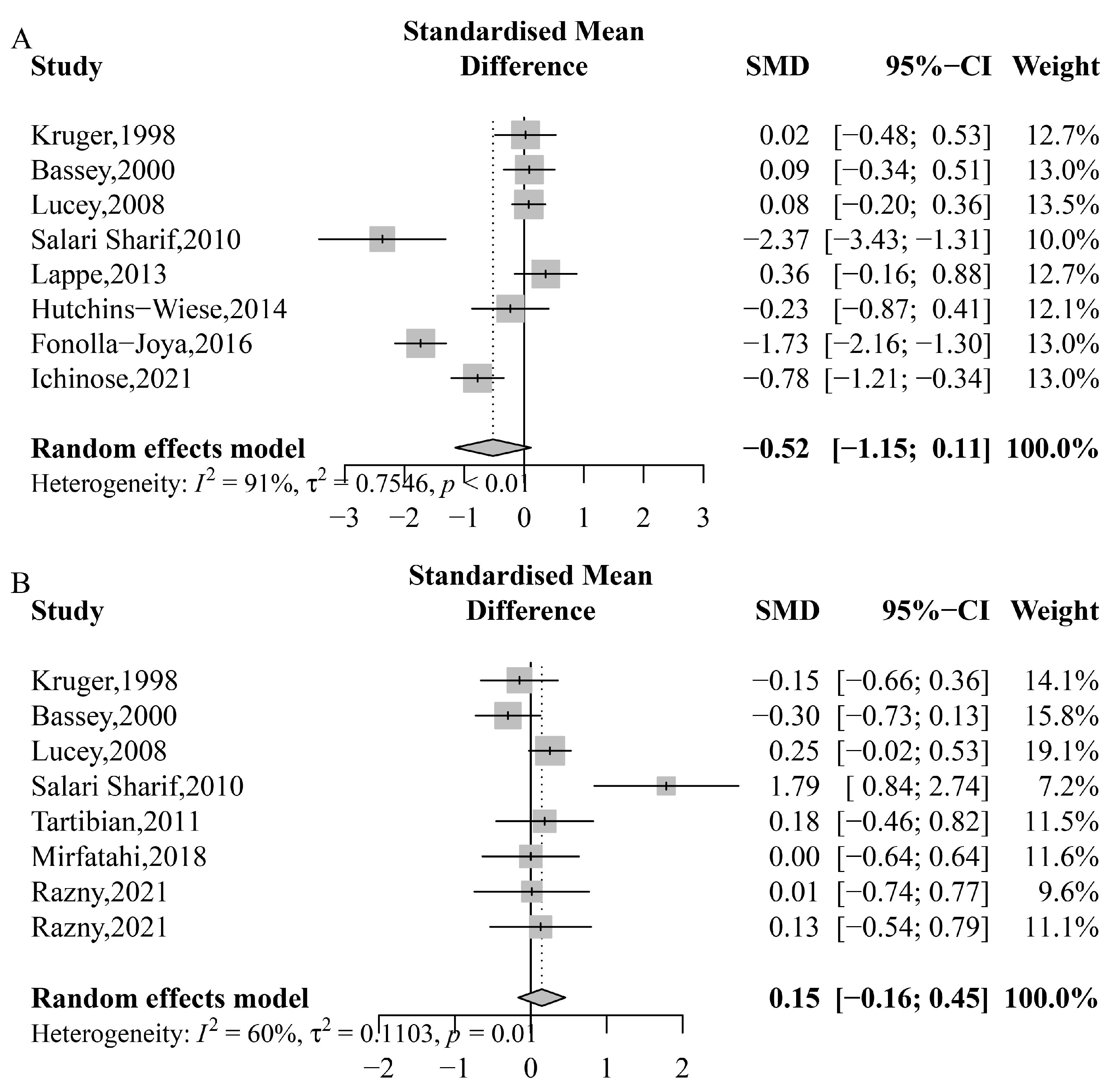
3.3. Bone Biomarkers
3.4. Serum Calcium, 25(OH)D and PTH
3.5. CRP, IL-6, Blood n-3 PUFA and Blood n-3 PUFA:n-6 PUFA Ratio
3.6. Sensitivity Analyses and Cumulative Meta-Analysis
3.7. Publication Bias Assessment
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Peck, W.A. Consensus development conference: Diagnosis, prophylaxis, and treatment of osteoporosis. Am. J. Med. 1993, 94, 646–650. [Google Scholar] [CrossRef]
- Kim, J.M.; Lin, C.; Stavre, Z.; Greenblatt, M.B.; Shim, J.H. Osteoblast-Osteoclast Communication and Bone Homeostasis. Cells 2020, 9, 2073. [Google Scholar] [CrossRef]
- Cheng, X.; Zhao, K.; Zha, X.; Du, X.; Li, Y.; Chen, S.; Wu, Y.; Li, S.; Lu, Y.; Zhang, Y.; et al. Opportunistic Screening Using Low-Dose CT and the Prevalence of Osteoporosis in China: A Nationwide, Multicenter Study. J. Bone Miner. Res. 2021, 36, 427–435. [Google Scholar] [CrossRef] [PubMed]
- Xiao, P.L.; Lu, H.D. Response to: Estimation of osteoporosis prevalence among a population is reasonable only after the concerned reference bone mineral density database and cutpoint T-score have been validated. Osteoporos. Int. 2023, 34, 419–420. [Google Scholar] [CrossRef]
- Juan, A.; Frontera, G.; Cacheda, A.P.; Ros, I.; Narváez, J.; Marí, B.; Nolla, J.M. Epidemiology of osteoporosis and its determinants in physically active Majorcan elderly. Mediterr. J. Rheumatol. 2020, 31, 42–49. [Google Scholar] [CrossRef]
- Cheraghi, P.; Cheraghi, Z.; Bozorgmehr, S. The Prevalence and risk factors of osteoporosis among the elderly in Hamadan province: A cross sectional study. Med. J. Islam. Repub. Iran. 2018, 32, 111. [Google Scholar] [CrossRef] [Green Version]
- Chaudhary, N.K.; Timilsena, M.N.; Sunuwar, D.R.; Pradhan, P.M.S.; Sangroula, R.K. Association of Lifestyle and Food Consumption with Bone Mineral Density among People Aged 50 Years and Above Attending the Hospitals of Kathmandu, Nepal. J. Osteoporos. 2019, 2019, 1536394. [Google Scholar] [CrossRef] [Green Version]
- Ko, C.H.; Yu, S.F.; Su, F.M.; Chen, J.F.; Chen, Y.C.; Su, Y.J.; Lai, H.M.; Chiu, W.C.; Hsu, C.Y.; Cheng, T.T.; et al. High prevalence and correlates of osteoporosis in men aged 50 years and over: A nationwide osteoporosis survey in Taiwan. Int. J. Rheum. Dis. 2018, 21, 2112–2118. [Google Scholar] [CrossRef] [PubMed]
- Cooper, C.; Cole, Z.A.; Holroyd, C.R.; Earl, S.C.; Harvey, N.C.; Dennison, E.M.; Melton, L.J.; Cummings, S.R.; Kanis, J.A. Secular trends in the incidence of hip and other osteoporotic fractures. Osteoporos. Int. 2011, 22, 1277–1288. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xu, Y.; Wu, Q. Decreasing trend of bone mineral density in US multiethnic population: Analysis of continuous NHANES 2005-2014. Osteoporos. Int. 2018, 29, 2437–2446. [Google Scholar] [CrossRef] [PubMed]
- Looker, A.C.; Sarafrazi Isfahani, N.; Fan, B.; Shepherd, J.A. Trends in osteoporosis and low bone mass in older US adults, 2005-2006 through 2013-2014. Osteoporos. Int. 2017, 28, 1979–1988. [Google Scholar] [CrossRef]
- Cheung, C.L.; Ang, S.B.; Chadha, M.; Chow, E.S.; Chung, Y.S.; Hew, F.L.; Jaisamrarn, U.; Ng, H.; Takeuchi, Y.; Wu, C.H.; et al. An updated hip fracture projection in Asia: The Asian Federation of Osteoporosis Societies study. Osteoporos. Sarcopenia 2018, 4, 16–21. [Google Scholar] [CrossRef]
- Wang, L.; Yu, W.; Yin, X.; Cui, L.; Tang, S.; Jiang, N.; Cui, L.; Zhao, N.; Lin, Q.; Chen, L.; et al. Prevalence of Osteoporosis and Fracture in China: The China Osteoporosis Prevalence Study. JAMA Netw. Open. 2021, 4, e2121106. [Google Scholar] [CrossRef] [PubMed]
- Groenendijk, I.; den Boeft, L.; van Loon, L.J.C.; de Groot, L. High Versus low Dietary Protein Intake and Bone Health in Older Adults: A Systematic Review and Meta-Analysis. Comput. Struct. Biotechnol. J. 2019, 17, 1101–1112. [Google Scholar] [CrossRef] [PubMed]
- Wu, D.; Cline-Smith, A.; Shashkova, E.; Perla, A.; Katyal, A.; Aurora, R. T-Cell Mediated Inflammation in Postmenopausal Osteoporosis. Front. Immunol. 2021, 12, 687551. [Google Scholar] [CrossRef]
- Wang, Y.; Ding, H.; Wang, X.; Wei, Z.; Feng, S. Associated Factors for Osteoporosis and Fracture in Chinese Elderly. Med. Sci. Monit. 2019, 25, 5580–5588. [Google Scholar] [CrossRef] [PubMed]
- Hopman, W.M.; Berger, C.; Joseph, L.; Morin, S.N.; Towheed, T.; Anastassiades, T.; Adachi, J.D.; Hanley, D.A.; Prior, J.C.; Goltzman, D. Longitudinal assessment of health-related quality of life in osteoporosis: Data from the population-based Canadian Multicentre Osteoporosis Study. Osteoporos. Int. 2019, 30, 1635–1644. [Google Scholar] [CrossRef]
- Leslie, W.D.; Yan, L.; Lix, L.M.; Morin, S.N. Time dependency in early major osteoporotic and hip re-fractures in women and men aged 50 years and older: A population-based observational study. Osteoporos. Int. 2022, 33, 39–46. [Google Scholar] [CrossRef]
- Dou, Y.; Wang, Y.; Chen, Z.; Yu, X.; Ma, D. Effect of n-3 polyunsaturated fatty acid on bone health: A systematic review and meta-analysis of randomized controlled trials. Food Sci. Nutr. 2022, 10, 145–154. [Google Scholar] [CrossRef]
- Salari, P.; Rezaie, A.; Larijani, B.; Abdollahi, M. A systematic review of the impact of n-3 fatty acids in bone health and osteoporosis. Med. Sci. Monit. 2008, 14, Ra37–Ra44. [Google Scholar]
- Orchard, T.S.; Pan, X.; Cheek, F.; Ing, S.W.; Jackson, R.D. A systematic review of omega-3 fatty acids and osteoporosis. Br. J. Nutr. 2012, 107 (Suppl. S2), S253–S260. [Google Scholar] [CrossRef] [Green Version]
- Mozaffari, H.; Djafarian, K.; Mofrad, M.D.; Shab-Bidar, S. Dietary fat, saturated fatty acid, and monounsaturated fatty acid intakes and risk of bone fracture: A systematic review and meta-analysis of observational studies. Osteoporos. Int. 2018, 29, 1949–1961. [Google Scholar] [CrossRef]
- Sadeghi, O.; Djafarian, K.; Ghorabi, S.; Khodadost, M.; Nasiri, M.; Shab-Bidar, S. Dietary intake of fish, n-3 polyunsaturated fatty acids and risk of hip fracture: A systematic review and meta-analysis on observational studies. Crit. Rev. Food Sci. Nutr. 2019, 59, 1320–1333. [Google Scholar] [CrossRef]
- Shen, D.; Zhang, X.; Li, Z.; Bai, H.; Chen, L. Effects of omega-3 fatty acids on bone turnover markers in postmenopausal women: Systematic review and meta-analysis. Climacteric 2017, 20, 522–527. [Google Scholar] [CrossRef]
- Abdelhamid, A.; Hooper, L.; Sivakaran, R.; Hayhoe, R.P.G.; Welch, A. The Relationship Between Omega-3, Omega-6 and Total Polyunsaturated Fat and Musculoskeletal Health and Functional Status in Adults: A Systematic Review and Meta-analysis of RCTs. Calcif. Tissue Int. 2019, 105, 353–372. [Google Scholar] [CrossRef] [Green Version]
- Iolascon, G.; Gimigliano, R.; Bianco, M.; De Sire, A.; Moretti, A.; Giusti, A.; Malavolta, N.; Migliaccio, S.; Migliore, A.; Napoli, N.; et al. Are Dietary Supplements and Nutraceuticals Effective for Musculoskeletal Health and Cognitive Function? A Scoping Review. J. Nutr. Health Aging 2017, 21, 527–538. [Google Scholar] [CrossRef] [PubMed]
- Ruxton, C.H.; Derbyshire, E.; Toribio-Mateas, M. Role of fatty acids and micronutrients in healthy ageing: A systematic review of randomised controlled trials set in the context of European dietary surveys of older adults. J. Hum. Nutr. Diet. 2016, 29, 308–324. [Google Scholar] [CrossRef] [PubMed]
- Griel, A.E.; Kris-Etherton, P.M.; Hilpert, K.F.; Zhao, G.; West, S.G.; Corwin, R.L. An increase in dietary n-3 fatty acids decreases a marker of bone resorption in humans. Nutr. J. 2007, 6, 1–8. [Google Scholar] [CrossRef] [Green Version]
- LeBoff, M.S.; Chou, S.H.; Murata, E.M.; Donlon, C.M.; Cook, N.R.; Mora, S.; Lee, I.M.; Kotler, G.; Bubes, V.; Buring, J.E. Effects of supplemental vitamin D on bone health outcomes in women and men in the VITamin D and OmegA-3 TriaL (VITAL). J. Bone Miner. Res. 2020, 35, 883–893. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mirfatahi, M.; Imani, H.; Tabibi, H.; Nasrollahi, A.; Hedayati, M. Effects of Flaxseed Oil on Serum Bone Turnover Markers in Hemodialysis Patients: A Randomized Controlled Trial. Iran. J. Kidney Dis. 2018, 12, 215–222. [Google Scholar] [PubMed]
- Kavyani, Z.; Musazadeh, V.; Fathi, S.; Hossein Faghfouri, A.; Dehghan, P.; Sarmadi, B. Efficacy of the omega-3 fatty acids supplementation on inflammatory biomarkers: An umbrella meta-analysis. Int. Immunopharmacol. 2022, 111, 109104. [Google Scholar] [CrossRef]
- Konukoglu, D. Bone markers. Int. J. Med. Biochem. 2019, 2, 65–78. [Google Scholar] [CrossRef]
- Greenblatt, M.B.; Tsai, J.N.; Wein, M.N. Bone Turnover Markers in the Diagnosis and Monitoring of Metabolic Bone Disease. Clin. Chem. 2017, 63, 464–474. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Proudfoot, D. Calcium Signaling and Tissue Calcification. Cold Spring Harb. Perspect. Biol. 2019, 11, 35303. [Google Scholar] [CrossRef] [PubMed]
- Hart, N.H.; Newton, R.U.; Tan, J.; Rantalainen, T.; Chivers, P.; Siafarikas, A.; Nimphius, S. Biological basis of bone strength: Anatomy, physiology and measurement. J. Musculoskelet. Neuronal Interact. 2020, 20, 347–371. [Google Scholar] [PubMed]
- Bouillon, R.; Marcocci, C.; Carmeliet, G.; Bikle, D.; White, J.H.; Dawson-Hughes, B.; Lips, P.; Munns, C.F.; Lazaretti-Castro, M.; Giustina, A.; et al. Skeletal and Extraskeletal Actions of Vitamin D: Current Evidence and Outstanding Questions. Endocr. Rev. 2019, 40, 1109–1151. [Google Scholar] [CrossRef] [Green Version]
- Hajishengallis, G.; Chavakis, T. Local and systemic mechanisms linking periodontal disease and inflammatory comorbidities. Nat. Rev. Immunol. 2021, 21, 426–440. [Google Scholar] [CrossRef]
- Place, D.E.; Malireddi, R.K.S.; Kim, J.; Vogel, P.; Yamamoto, M.; Kanneganti, T.D. Osteoclast fusion and bone loss are restricted by interferon inducible guanylate binding proteins. Nat. Commun. 2021, 12, 496. [Google Scholar] [CrossRef]
- Cornish, S.M.; Myrie, S.B.; Bugera, E.M.; Chase, J.E.; Turczyn, D.; Pinder, M. Omega-3 supplementation with resistance training does not improve body composition or lower biomarkers of inflammation more so than resistance training alone in older men. Nutr. Res. 2018, 60, 87–95. [Google Scholar] [CrossRef]
- Jørgensen, H.S.; Eide, I.A.; Jenssen, T.; Åsberg, A.; Bollerslev, J.; Godang, K.; Hartmann, A.; Schmidt, E.B.; Svensson, M. Marine n-3 Polyunsaturated Fatty Acids and Bone Mineral Density in Kidney Transplant Recipients: A Randomized, Placebo-Controlled Trial. Nutrients 2021, 13, 2361. [Google Scholar] [CrossRef] [PubMed]
- Razny, U.; Goralska, J.; Calder, P.C.; Gruca, A.; Childs, C.E.; Kapusta, M.; Slowinska-Solnica, K.; Dembinska-Kiec, A.; Solnica, B.; Malczewska-Malec, M. The Effect of Caloric Restriction with and without n-3 PUFA Supplementation on Bone Turnover Markers in Blood of Subjects with Abdominal Obesity: A Randomized Placebo-Controlled Trial. Nutrients 2021, 13, 3096. [Google Scholar] [CrossRef]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Page, M.J.; Moher, D.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E. PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. BMJ 2021, 372, n160. [Google Scholar] [CrossRef]
- Oremus, M.; Wolfson, C.; Perrault, A.; Demers, L.; Momoli, F.; Moride, Y. Interrater reliability of the modified Jadad quality scale for systematic reviews of Alzheimer’s disease drug trials. Dement. Geriatr. Cogn. Disord. 2001, 12, 232–236. [Google Scholar] [CrossRef]
- Schwarzer, G. meta: An R package for meta-analysis. R News 2007, 7, 40–45. [Google Scholar]
- Balduzzi, S.; Rücker, G.; Schwarzer, G. How to perform a meta-analysis with R: A practical tutorial. Evid.-Based Ment. Health 2019, 22, 153–160. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Higgins, J.P.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions; John Wiley & Sons: Chichester, UK, 2008. [Google Scholar]
- Higgins, J.P.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef]
- Bischoff-Ferrari, H.A.; Vellas, B.; Rizzoli, R.; Kressig, R.W.; Da Silva, J.A.; Blauth, M.; Felson, D.T.; McCloskey, E.V.; Watzl, B.; Hofbauer, L.C. Effect of vitamin D supplementation, omega-3 fatty acid supplementation, or a strength-training exercise program on clinical outcomes in older adults: The DO-HEALTH randomized clinical trial. JAMA 2020, 324, 1855–1868. [Google Scholar] [CrossRef]
- Appleton, K.M.; Fraser, W.D.; Rogers, P.J.; Ness, A.R.; Tobias, J.H. Supplementation with a low-moderate dose of n-3 long-chain PUFA has no short-term effect on bone resorption in human adults. Br. J. Nutr. 2011, 105, 1145–1149. [Google Scholar] [CrossRef] [Green Version]
- Bassey, E.J.; Littlewood, J.J.; Rothwell, M.C.; Pye, D.W. Lack of effect of supplementation with essential fatty acids on bone mineral density in healthy pre- and postmenopausal women: Two randomized controlled trials of Efacal v. calcium alone. Br. J. Nutr. 2000, 83, 629–635. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, J.S.; Hill, C.L.; Lester, S.; Ruediger, C.D.; Battersby, R.; Jones, G.; Cleland, L.G.; March, L.M. Supplementation with omega-3 fish oil has no effect on bone mineral density in adults with knee osteoarthritis: A 2-year randomized controlled trial. Osteoporos. Int. 2016, 27, 1897–1905. [Google Scholar] [CrossRef] [PubMed]
- Deore, G.D.; Gurav, A.N.; Patil, R.; Shete, A.R.; Naiktari, R.S.; Inamdar, S.P. Omega 3 fatty acids as a host modulator in chronic periodontitis patients: A randomised, double-blind, palcebo-controlled, clinical trial. J. Periodontal. Implant. Sci. 2014, 44, 25–32. [Google Scholar] [CrossRef] [Green Version]
- Dodin, S.; Lemay, A.; Jacques, H.; Légaré, F.; Forest, J.C.; Mâsse, B. The effects of flaxseed dietary supplement on lipid profile, bone mineral density, and symptoms in menopausal women: A randomized, double-blind, wheat germ placebo-controlled clinical trial. J. Clin. Endocrinol. Metab. 2005, 90, 1390–1397. [Google Scholar] [CrossRef] [PubMed]
- Fonolla-Joya, J.; Reyes-García, R.; García-Martín, A.; López-Huertas, E.; Muñoz-Torres, M. Daily Intake of Milk Enriched with n-3 Fatty Acids, Oleic Acid, and Calcium Improves Metabolic and Bone Biomarkers in Postmenopausal Women. J. Am. Coll. Nutr. 2016, 35, 529–536. [Google Scholar] [CrossRef] [PubMed]
- Hutchins-Wiese, H.L.; Picho, K.; Watkins, B.A.; Li, Y.; Tannenbaum, S.; Claffey, K.; Kenny, A.M. High-dose eicosapentaenoic acid and docosahexaenoic acid supplementation reduces bone resorption in postmenopausal breast cancer survivors on aromatase inhibitors: A pilot study. Nutr. Cancer 2014, 66, 68–76. [Google Scholar] [CrossRef] [PubMed]
- Ichinose, T.; Matsuzaki, K.; Kato, M.; Tanabe, Y.; Tachibana, N.; Morikawa, M.; Kato, S.; Ohata, S.; Ohno, M.; Wakatsuki, H.; et al. Intake of Docosahexaenoic Acid-Enriched Milk Beverage Prevents Age-Related Cognitive Decline and Decreases Serum Bone Resorption Marker Levels. J. Oleo Sci. 2021, 70, 1829–1838. [Google Scholar] [CrossRef]
- Kruger, M.C.; Coetzer, H.; de Winter, R.; Gericke, G.; Van Papendorp, D.H. Calcium, gamma-linolenic acid and eicosapentaenoic acid supplementation in senile osteoporosis. Aging 1998, 10, 385–394. [Google Scholar] [CrossRef]
- Lappe, J.; Kunz, I.; Bendik, I.; Prudence, K.; Weber, P.; Recker, R.; Heaney, R.P. Effect of a combination of genistein, polyunsaturated fatty acids and vitamins D3 and K1 on bone mineral density in postmenopausal women: A randomized, placebo-controlled, double-blind pilot study. Eur. J. Nutr. 2013, 52, 203–215. [Google Scholar] [CrossRef] [Green Version]
- Lucey, A.J.; Paschos, G.K.; Cashman, K.D.; Martínéz, J.A.; Thorsdottir, I.; Kiely, M. Influence of moderate energy restriction and seafood consumption on bone turnover in overweight young adults. Am. J. Clin. Nutr. 2008, 87, 1045–1052. [Google Scholar] [CrossRef] [Green Version]
- Salari Sharif, P.; Asalforoush, M.; Ameri, F.; Larijani, B.; Abdollahi, M. The effect of n-3 fatty acids on bone biomarkers in Iranian postmenopausal osteoporotic women: A randomized clinical trial. Age 2010, 32, 179–186. [Google Scholar] [CrossRef] [Green Version]
- Tartibian, B.; Hajizadeh Maleki, B.; Kanaley, J.; Sadeghi, K. Long-term aerobic exercise and omega-3 supplementation modulate osteoporosis through inflammatory mechanisms in post-menopausal women: A randomized, repeated measures study. Nutr. Metab. 2011, 8, 71. [Google Scholar] [CrossRef] [Green Version]
- Vanlint, S.J.; Ried, K. Efficacy and tolerability of calcium, vitamin D and a plant-based omega-3 oil for osteopenia: A pilot RCT. Maturitas 2012, 71, 44–48. [Google Scholar] [CrossRef]
- Murshed, M. Mechanism of Bone Mineralization. Cold Spring Harb. Perspect. Med. 2018, 8, 31229. [Google Scholar] [CrossRef]
- Lewis, J.D.; Abreu, M.T. Diet as a Trigger or Therapy for Inflammatory Bowel Diseases. Gastroenterology 2017, 152, 398–414.e396. [Google Scholar] [CrossRef]
- Tortosa-Caparrós, E.; Navas-Carrillo, D.; Marín, F.; Orenes-Piñero, E. Anti-inflammatory effects of omega 3 and omega 6 polyunsaturated fatty acids in cardiovascular disease and metabolic syndrome. Crit. Rev. Food Sci. Nutr. 2017, 57, 3421–3429. [Google Scholar] [CrossRef]
- Saini, R.K.; Keum, Y.S. Omega-3 and omega-6 polyunsaturated fatty acids: Dietary sources, metabolism, and significance-A review. Life Sci. 2018, 203, 255–267. [Google Scholar] [CrossRef]
- Shahidi, F.; Ambigaipalan, P. Omega-3 Polyunsaturated Fatty Acids and Their Health Benefits. Annu. Rev. Food Sci. Technol. 2018, 9, 345–381. [Google Scholar] [CrossRef]
- Anez-Bustillos, L.; Cowan, E.; Cubria, M.B.; Villa-Camacho, J.C.; Mohamadi, A.; Dao, D.T.; Pan, A.; Fell, G.L.; Baker, M.A.; Nandivada, P. Effects of dietary omega-3 fatty acids on bones of healthy mice. Clin. Nutr. 2019, 38, 2145–2154. [Google Scholar] [CrossRef] [PubMed]
- Da Boit, M.; Sibson, R.; Sivasubramaniam, S.; Meakin, J.R.; Greig, C.A.; Aspden, R.M.; Thies, F.; Jeromson, S.; Hamilton, D.L.; Speakman, J.R.; et al. Sex differences in the effect of fish-oil supplementation on the adaptive response to resistance exercise training in older people: A randomized controlled trial. Am. J. Clin. Nutr. 2017, 105, 151–158. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gartlehner, G.; Patel, S.V.; Reddy, S.; Rains, C.; Schwimmer, M.; Kahwati, L. Hormone Therapy for the Primary Prevention of Chronic Conditions in Postmenopausal Persons: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA 2022, 328, 1747–1765. [Google Scholar] [CrossRef] [PubMed]
- Schlesinger, P.H.; Braddock, D.T.; Larrouture, Q.C.; Ray, E.C.; Riazanski, V.; Nelson, D.J.; Tourkova, I.L.; Blair, H.C. Phylogeny and chemistry of biological mineral transport. Bone 2020, 141, 115621. [Google Scholar] [CrossRef]
- Deluca, H.F. History of the discovery of vitamin D and its active metabolites. Bonekey Rep. 2014, 3, 479. [Google Scholar] [CrossRef] [Green Version]
- Isanejad, M.; Tajik, B.; McArdle, A.; Tuppurainen, M.; Sirola, J.; Kröger, H.; Rikkonen, T.; Erkkilä, A. Dietary omega-3 polyunsaturated fatty acid and alpha-linolenic acid are associated with physical capacity measure but not muscle mass in older women 65-72 years. Eur. J. Nutr. 2022, 61, 1813–1821. [Google Scholar] [CrossRef] [PubMed]
- Poulsen, R.C.; Kruger, M.C. Detrimental effect of eicosapentaenoic acid supplementation on bone following ovariectomy in rats. Prostaglandins Leukot. Essent. Fat. Acids 2006, 75, 419–427. [Google Scholar] [CrossRef] [PubMed]
- Hansen, K.E.; Johnson, R.E.; Chambers, K.R.; Johnson, M.G.; Lemon, C.C.; Vo, T.N.; Marvdashti, S. Treatment of Vitamin D Insufficiency in Postmenopausal Women: A Randomized Clinical Trial. JAMA Intern. Med. 2015, 175, 1612–1621. [Google Scholar] [CrossRef] [PubMed]
- Laird, E.; O’Halloran, A.M.; Carey, D.; Healy, M.; O’Connor, D.; Moore, P.; Shannon, T.; Molloy, A.M.; Kenny, R.A. The Prevalence of Vitamin D Deficiency and the Determinants of 25(OH)D Concentration in Older Irish Adults: Data From The Irish Longitudinal Study on Ageing (TILDA). J. Gerontol. A Biol. Sci. Med. Sci. 2018, 73, 519–525. [Google Scholar] [CrossRef] [Green Version]
- Granic, A.; Hill, T.R.; Davies, K.; Jagger, C.; Adamson, A.; Siervo, M.; Kirkwood, T.B.; Mathers, J.C.; Sayer, A.A. Vitamin D Status, Muscle Strength and Physical Performance Decline in Very Old Adults: A Prospective Study. Nutrients 2017, 9, 379. [Google Scholar] [CrossRef] [Green Version]
| First Author (Year) | Nation | G | Age (Years) | Population | N (I/C) | I/C | D | Outcomes | Modified Jadad Scale Score |
|---|---|---|---|---|---|---|---|---|---|
| Kruger (1998) [58] | South Africa | F | 79.5 ± 5.56 | osteopenic women | 60 (29/31) | 0.42 g n-3/placebo (SFA) | 18 mo | sCa; 25(OH)D; BAP; OC; PTH; lumbar spine BMD; femoral neck BMD | 3 |
| Bassey (2000) [51] | UK | F | 45.7 ± 11.1 | pre- and post-menopausal women | 88 (40/48) | Efacal/Ca | 12 mo | sCa; NTx-1; BAP; OC; PTH; TBMD | 5 |
| Dodin (2005) [54] | Canada | F | 54.7 ± 4.3 | women aged 45–65 | 179 (85/94) | flaxseed oil (9.12 g n-3)/placebo (wheat germ) | 12 mo | lumbar spine BMD; femoral neck BMD | 7 |
| Lucey (2008) [60] | US | M&F | 32.5 ± 5.3 | young overweight adults | 276 (210/66) | lean fish (0.3 g n-3), salmon (3.0 g n-3), fish-oil (1.5 g n-3)/control (no seafood) | 2 mo | 25(OH)D; NTx-1; CTx-1; BAP; OC; PTH | 4 |
| Salari Sharif (2010) [61] | Iran | F | 61.4 ± 7.4 | postmenopausal osteoporotic women | 25 (13/12) | n-3 capsules (0.9 g n-3)/placebo | 6 mo | sCa; 25(OH)D; BAP; OC; PTH | 4 |
| Appleton (2011) [50] | UK | M&F | NA | mild–moderately depressed individuals | 113 (53/60) | 1.48 g n-3 (0.63 g EPA + 0.85 g DHA)/placebo (olive oil) | 3 mo | CTx-1; n-3 PUFA: n-6 PUFA; serum n-3 PUFA | 5 |
| Tartibian (2011) [62] | Iran | F | 61.1 ± 8.0 | healthy postmenopausal women aged 58–78 | 38 (20/18) | n-3 capsules (0.6 g EPA + 0.4 g DHA)/ control | 6 mo | sCa; 25(OH)D; CTx-1; OC; PTH; lumbar spine BMD; femoral neck BMD; IL-6 | 3 |
| Vanlint (2012) [63] | Australia | M&F | 59.2 | individuals with osteopenia | 40 (20/20) | 0.4 g DHA + Ca/placebo (Ca) | 12 mo | CTx-1; lumbar spine BMD; femoral neck BMD | 6 |
| Lappe (2013) [59] | US | F | 54.7 ± 2.4 | postmenopausal women | 70 (35/35) | GBB/control (Ca) | 6 mo | 25(OH)D; NTx-1; BAP; PTH; femoral neck BMD; serum n-3 PUFA | 6 |
| Hutchins (2014) [56] | US | F | 61.8 ± 9.5 | postmenopausal women | 38 (20/18) | 4.0 g n3 (EPA + DHA)/placebo (sunflower oil) | 3 mo | 25(OH)D; CTx-1; BAP; PTH; serum n-3 PUFA | 6 |
| Deore (2014) [53] | India | NA | 44.9 ± 28.9 | patients with chronic periodontitis aged 30–60 | 60 (30/30) | 0.18 g EPA + 0.12 g DHA/placebo (liquid paraffin) | 3 mo | CRP | 6 |
| Chen (2016) [52] | Australia | M&F | 61.0 ± 10.0 | aged over 40 years with clinical knee OA | 202 (101/101) | high dose (4.5 g EPA + 4.5 g DHA); low dose (0.45 g EPA + 0.45 g DHA) | 24 mo | lumbar spine BMD; femoral neck BMD; n-3 PUFA: n-6 PUFA; serum n-3 PUFA | 7 |
| Fonolla-Joya (2016) [55] | Spain | F | 59.7 ± 5.8 | postmenopausal women | 117 (63/54) | 0.2 g n3 (EPA + DHA) + vitamins/control(vitamins) | 12 mo | sCa; 25(OH)D; BAP; PTH; serum n-3 PUFA; CRP | 5 |
| Mirfatahi (2018) [30] | Iran | M&F | 63.5 ± 5.7 | stable hemodialysis patients | 38 (19/19) | flaxseed oil (3.45 g ALA)/control (triglycerides oil) | 2 mo | sCa; NTx-1; OC; PTH | 7 |
| Cornish (2018) [39] | Canada | M | 71.1 ± 5.5 | men ≥65 | 24 (12/12) | 3.0 g n3 (EPA + DHA)/control (omega 3-6-9) | 3 mo | TBMD; lumbar spine BMD; total hip BMD; IL-6 | 4 |
| LeBoff (2020) [29] | US | M&F | 63.8 ± 6.1 | men ≥50, women ≥55 | 771 (388/383) | VtD + 1.0 g n3/placebo | 24 mo | lumbar spine BMD; total hip BMD | 4 |
| Jørgensen (2021) [40] | Norway | M&F | 53 ± 14 | recipients with stable kidney function | 132 (66/66) | 2.6 g n3 (0.46 g EPA + 0.38 g DHA)/placebo (olive oil) | 11 mo | sCa; 25(OH)D; PTH; TBMD; lumbar spine BMD; total hip BMD; femoral neck BMD | 5 |
| Razny (2021) [41] | Poland | M&F | 41.0 ± 9.9 | subjects aged 25–65 with overweight or abdominal obesity | 189 (95/94) | IS + 1.8 g n3; CR + 1.8 g n3/IS + placebo; CR + placebo | 3 mo | 25(OH)D; CTx-1; OC; CRP; IL-6 | 6 |
| Ichinose (2021) [57] | Japan | M&F | 69.1 ± 5.1 | healthy elderly Japanese | 87 (46/41) | acid-enriched milk (0.434 g n3)/placebo milk | 12 mo | sCa; BAP | 6 |
| Subgroup Analysis | Lumbar Spine BMD | Femoral Neck BMD | NTx-1 | Serum Calcium | 25(OH)D | Blood n-3 PUFA |
|---|---|---|---|---|---|---|
| Country | ||||||
| Eastern country | 0.03 [0.01, 0.05] | 0.02 [0.02, 0.03] | ||||
| Western country | 0.00 [−0.00, 0.01] | 0.05 [−0.02, 0.11] | ||||
| Gender | ||||||
| male | 0.01 [0.01, 0.02] | 1.10 [−5.73, 7.94] | 2.79 [1.08, 4.49] | |||
| female and male | 0.08 [−0.04, 0.20] | −9.66 [−15.60, −3.71] | 2.38 [1.67,3.08] | |||
| Average age class | ||||||
| ≥60 | 0.09 [−0.04, 0.23] | 0.43 [0.11, 0.74] | 2.65 [2.30, 3.00] | |||
| <60 | 0.01 [0.01, 0.01] | 1.52 [−0.79, 3.84] | 3.03 [0.22, 5.84] | |||
| Control type | ||||||
| placebo | 0.02 [0.01, 0.03] | 2.07 [1.67, 2.47] | ||||
| other control | 0.09 [−0.06, 0.23] | 2.92 [1.31, 4.54] | ||||
| Duration class | ||||||
| >6 months | 0.05 [−0.02, 0.12] | −0.19 [−0.37, −0.01] | 3.41 [−1.75, 8,57] | 3.57 [1.86, 5.29] | ||
| ≤6 months | 0.01 [0.01, 0.01] | 0.07 [−0.33, 0.46] | 0.29 [0.11, 0.47] | 1.93 [1.59, 2.26] | ||
| Intervention type | ||||||
| n-3 only | 0.36 [0.06, 0.66] | 2.36 [1.87, 2.85] | ||||
| n-3 + others | 3.28 [−2.02, 8.57] | 3.03 [0.22, 5.84] | ||||
| Dose class | ||||||
| >1 g/d | 2.36 [1.87, 2.85] | |||||
| ≤1 g/d | 3.03 [0.22, 5.84] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gao, J.; Xie, C.; Yang, J.; Tian, C.; Zhang, M.; Lu, Z.; Meng, X.; Cai, J.; Guo, X.; Gao, T. The Effects of n-3 PUFA Supplementation on Bone Metabolism Markers and Body Bone Mineral Density in Adults: A Systematic Review and Meta-Analysis of RCTs. Nutrients 2023, 15, 2806. https://doi.org/10.3390/nu15122806
Gao J, Xie C, Yang J, Tian C, Zhang M, Lu Z, Meng X, Cai J, Guo X, Gao T. The Effects of n-3 PUFA Supplementation on Bone Metabolism Markers and Body Bone Mineral Density in Adults: A Systematic Review and Meta-Analysis of RCTs. Nutrients. 2023; 15(12):2806. https://doi.org/10.3390/nu15122806
Chicago/Turabian StyleGao, Jie, Chenqi Xie, Jie Yang, Chunyan Tian, Mai Zhang, Zhenquan Lu, Xiangyuan Meng, Jing Cai, Xiaofei Guo, and Tianlin Gao. 2023. "The Effects of n-3 PUFA Supplementation on Bone Metabolism Markers and Body Bone Mineral Density in Adults: A Systematic Review and Meta-Analysis of RCTs" Nutrients 15, no. 12: 2806. https://doi.org/10.3390/nu15122806





