Effect of Two Different Dietary Weight Loss Strategies on Risk Factors for Urinary Stone Formation and Cardiometabolic Risk Profile in Overweight Women
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Study Design
2.3. Anthropometric and Clinical Measurements
2.4. Laboratory Methods
2.5. Statistical Methods
3. Results
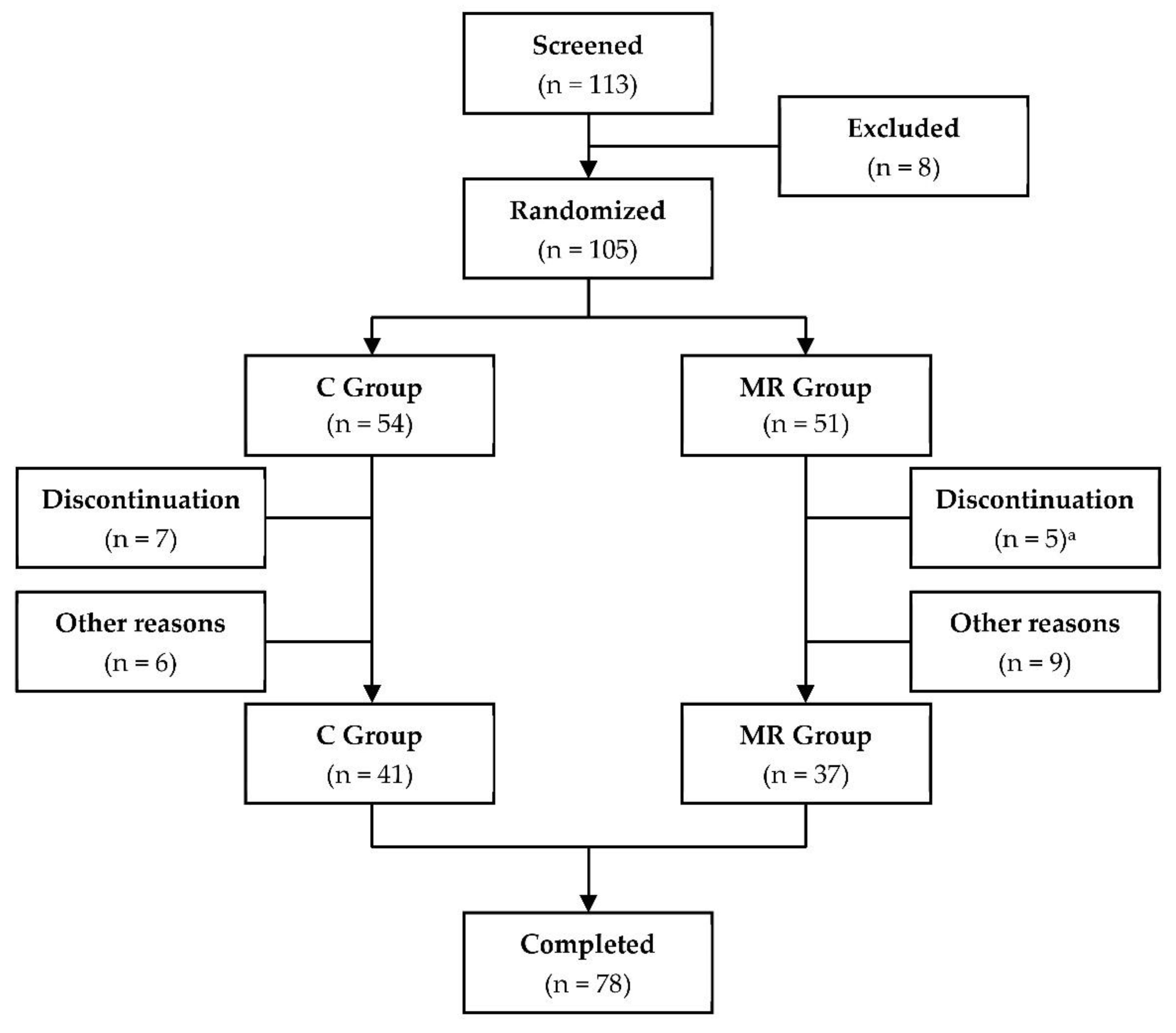
3.1. Participants
3.2. Anthropometric and Clinical Characteristics
3.3. Cardiometabolic Risk Profile
3.4. Clinical Chemistry and Biochemical Characteristics
3.5. Urine Composition
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization (WHO). Obesity and Overweight. 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 17 September 2022).
- Zatońska, K.; Psikus, P.; Basiak-Rasała, A.; Stępnicka, Z.; Gaweł-Dąbrowska, D.; Wołyniec, M.; Gibka, J.; Szuba, A.; Połtyn-Zaradna, K. Obesity and Chosen Non-Communicable Diseases in PURE Poland Cohort Study. Int. J. Environ. Res. Public Health 2021, 18, 2701. [Google Scholar] [CrossRef] [PubMed]
- Aune, D.; Mahamat-Saleh, Y.; Norat, T.; Riboli, E. Body Fatness, Diabetes, Physical Activity and Risk of Kidney Stones: A Systematic Review and Meta-Analysis of Cohort Studies. Eur. J. Epidemiol. 2018, 33, 1033–1047. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Al-Hayek, S.; Schwen, Z.R.; Jackman, S.V.; Averch, T.D. The Impact of Obesity on Urine Composition and Nephrolithiasis Management. J. Endourol. 2013, 27, 379–383. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.-C.; Kim, Y.-J.; Kim, T.-H.; Yun, S.-J.; Lee, N.K.; Kim, W.-J. Impact of Obesity in Patients with Urolithiasis and Its Prognostic Usefulness in Stone Recurrence. J. Urol. 2008, 179, 570–574. [Google Scholar] [CrossRef]
- Taylor, E.N.; Curhan, G.C. Body Size and 24-Hour Urine Composition. Am. J. Kidney Dis. 2006, 48, 905–915. [Google Scholar] [CrossRef]
- Siener, R.; Glatz, S.; Nicolay, C.; Hesse, A. The Role of Overweight and Obesity in Calcium Oxalate Stone Formation. Obes. Res. 2004, 12, 106–113. [Google Scholar] [CrossRef]
- Reddy, S.T.; Wang, C.-Y.; Sakhaee, K.; Brinkley, L.; Pak, C.Y.C. Effect of Low-Carbohydrate High-Protein Diets on Acid-Base Balance, Stone-Forming Propensity, and Calcium Metabolism. Am. J. Kidney Dis. 2002, 40, 265–274. [Google Scholar] [CrossRef]
- Ferraz, R.R.N.; Tiselius, H.-G.; Heilberg, I.P. Fat Malabsorption Induced by Gastrointestinal Lipase Inhibitor Leads to an Increase in Urinary Oxalate Excretion. Kidney Int. 2004, 66, 676–682. [Google Scholar] [CrossRef] [Green Version]
- Matlaga, B.R.; Shore, A.D.; Magnuson, T.; Clark, J.M.; Johns, R.; Makary, M.A. Effect of Gastric Bypass Surgery on Kidney Stone Disease. J. Urol. 2009, 181, 2573–2577. [Google Scholar] [CrossRef]
- Lieske, J.C.; Mehta, R.A.; Milliner, D.S.; Rule, A.D.; Bergstralh, E.J.; Sarr, M.G. Kidney Stones Are Common after Bariatric Surgery. Kidney Int. 2015, 87, 839–845. [Google Scholar] [CrossRef]
- Espino-Grosso, P.M.; Canales, B.K. Kidney Stones After Bariatric Surgery: Risk Assessment and Mitigation. Bariatr. Surg. Pract. Patient Care 2017, 12, 3–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bassiony, A.I.; Sabry, A.; Shiha, O.; ElGeidie, A.; Nassar, M.K. The Short-Term Renal Effects of Bariatric Surgery: A Comparative Study Between Sleeve Gastrectomy and One Anastomosis Gastric Bypass Operations Among Egyptian Patients with Severe Obesity. Obes. Surg. 2020, 30, 4494–4504. [Google Scholar] [CrossRef] [PubMed]
- Neuschwander-Tetri, B.A. Non-Alcoholic Fatty Liver Disease. BMC Med. 2017, 15, 45. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Younossi, Z.M. The Epidemiology of Nonalcoholic Steatohepatitis. Clin. Liver Dis. 2018, 11, 92–94. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chalasani, N.; Younossi, Z.; Lavine, J.E.; Charlton, M.; Cusi, K.; Rinella, M.; Harrison, S.A.; Brunt, E.M.; Sanyal, A.J. The Diagnosis and Management of Nonalcoholic Fatty Liver Disease: Practice Guidance from the American Association for the Study of Liver Diseases. Hepatology 2018, 67, 328–357. [Google Scholar] [CrossRef] [Green Version]
- Targher, G.; Day, C.P.; Bonora, E. Risk of Cardiovascular Disease in Patients with Nonalcoholic Fatty Liver Disease. N. Engl. J. Med. 2010, 363, 1341–1350. [Google Scholar] [CrossRef] [Green Version]
- Targher, G.; Byrne, C.D. Non-Alcoholic Fatty Liver Disease: An Emerging Driving Force in Chronic Kidney Disease. Nat. Rev. Nephrol. 2017, 13, 297–310. [Google Scholar] [CrossRef] [Green Version]
- Qin, S.; Wang, S.; Wang, X.; Wang, J. Non-Alcoholic Fatty Liver Disease and the Risk of Urolithiasis: A Systematic Review and Meta-Analysis. Medicine 2018, 97, e12092. [Google Scholar] [CrossRef]
- Wijarnpreecha, K.; Lou, S.; Panjawatanan, P.; Sanguankeo, A.; Pungpapong, S.; Lukens, F.J.; Ungprasert, P. Nonalcoholic Fatty Liver Disease and Urolithiasis. A Systematic Review and Meta-Analysis. J. Gastrointest. Liver Dis. 2018, 27, 427–432. [Google Scholar] [CrossRef]
- Danilovic, A.; Marchini, G.S.; Pucci, N.D.; Coimbra, B.; Torricelli, F.C.M.; Batagello, C.; Vicentini, F.C.; Srougi, M.; Nahas, W.C.; Mazzucchi, E. Effect of a Low-Calorie Diet on 24-Hour Urinary Parameters of Obese Adults with Idiopathic Calcium Oxalate Kidney Stones. Int. Braz. J. Urol. 2021, 47, 1136–1147. [Google Scholar] [CrossRef]
- Metzner, C.E.; Folberth-Vögele, A.; Bitterlich, N.; Lemperle, M.; Schäfer, S.; Alteheld, B.; Stehle, P.; Siener, R. Effect of a Conventional Energy-Restricted Modified Diet with or without Meal Replacement on Weight Loss and Cardiometabolic Risk Profile in Overweight Women. Nutr. Metab. 2011, 8, 64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Werness, P.G.; Brown, C.M.; Smith, L.H.; Finlayson, B. EQUIL2: A BASIC Computer Program for the Calculation of Urinary Saturation. J. Urol. 1985, 134, 1242–1244. [Google Scholar] [CrossRef] [PubMed]
- Amato, M.C.; Giordano, C.; Pitrone, M.; Galluzzo, A. Cut-off Points of the Visceral Adiposity Index (VAI) Identifying a Visceral Adipose Dysfunction Associated with Cardiometabolic Risk in a Caucasian Sicilian Population. Lipids Health Dis. 2011, 10, 183. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bedogni, G.; Bellentani, S.; Miglioli, L.; Masutti, F.; Passalacqua, M.; Castiglione, A.; Tiribelli, C. The Fatty Liver Index: A Simple and Accurate Predictor of Hepatic Steatosis in the General Population. BMC Gastroenterol. 2006, 6, 33. [Google Scholar] [CrossRef] [Green Version]
- LaMonte, M.J.; Ainsworth, B.E.; DuBose, K.D.; Grandjean, P.W.; Davis, P.G.; Yanowitz, F.G.; Durstine, J.L. The Hypertriglyceridemic Waist Phenotype among Women. Atherosclerosis 2003, 171, 123–130. [Google Scholar] [CrossRef]
- National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Final Report. Circulation 2002, 106, 3143–3421. [Google Scholar] [CrossRef]
- Grundy, S.M.; Cleeman, J.I.; Daniels, S.R.; Donato, K.A.; Eckel, R.H.; Franklin, B.A.; Gordon, D.J.; Krauss, R.M.; Savage, P.J.; Smith, S.C., Jr.; et al. Diagnosis and Management of the Metabolic Syndrome: An American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 2005, 112, 2735–2752. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alberti, K.G.M.M.; Zimmet, P.; Shaw, J.; IDF Epidemiology Task Force Consensus Group. The Metabolic Syndrome—A New Worldwide Definition. Lancet 2005, 366, 1059–1062. [Google Scholar] [CrossRef]
- Levey, A.S.; Stevens, L.A.; Schmid, C.H.; Zhang, Y.L.; Castro, A.F.; Feldman, H.I.; Kusek, J.W.; Eggers, P.; Van Lente, F.; Greene, T.; et al. A New Equation to Estimate Glomerular Filtration Rate. Ann. Intern. Med. 2009, 150, 604–612. [Google Scholar] [CrossRef]
- Choi, H.K.; Liu, S.; Curhan, G. Intake of Purine-Rich Foods, Protein, and Dairy Products and Relationship to Serum Levels of Uric Acid: The Third National Health and Nutrition Examination Survey. Arthritis Rheum. 2005, 52, 283–289. [Google Scholar] [CrossRef]
- Aihemaitijiang, S.; Zhang, Y.; Zhang, L.; Yang, J.; Ye, C.; Halimulati, M.; Zhang, W.; Zhang, Z. The Association between Purine-Rich Food Intake and Hyperuricemia: A Cross-Sectional Study in Chinese Adult Residents. Nutrients 2020, 12, 3835. [Google Scholar] [CrossRef] [PubMed]
- Faller, J.; Fox, I.H. Ethanol-Induced Hyperuricemia: Evidence for Increased Urate Production by Activation of Adenine Nucleotide Turnover. N. Engl. J. Med. 1982, 307, 1598–1602. [Google Scholar] [CrossRef] [PubMed]
- King, C.; Lanaspa, M.A.; Jensen, T.; Tolan, D.R.; Sánchez-Lozada, L.G.; Johnson, R.J. Uric Acid as a Cause of the Metabolic Syndrome. Contrib. Nephrol. 2018, 192, 88–102. [Google Scholar] [CrossRef] [PubMed]
- Ni, W.; Wang, R.; Liu, Z.; Yuan, X.; Chi, H.; Lv, D.; Sun, Y.; Liu, P.; Xu, J. Association of Serum Uric Acid with Metabolic Syndrome and Its Components: A Cross-Sectional Study in Chinese Coastal Population. Metab. Syndr. Relat. Disord. 2020, 18, 103–109. [Google Scholar] [CrossRef] [Green Version]
- Lee, J.W.; Cho, Y.K.; Ryan, M.; Kim, H.; Lee, S.W.; Chang, E.; Joo, K.J.; Kim, J.T.; Kim, B.S.; Sung, K.C. Serum Uric Acid as a Predictor for the Development of Nonalcoholic Fatty Liver Disease in Apparently Healthy Subjects: A 5-Year Retrospective Cohort Study. Gut Liver 2010, 4, 378–383. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Wei, F.; Fan, Y. High Serum Uric Acid and Risk of Nonalcoholic Fatty Liver Disease: A Systematic Review and Meta-Analysis. Clin. Biochem. 2016, 49, 636–642. [Google Scholar] [CrossRef] [PubMed]
- Jensen, T.; Niwa, K.; Hisatome, I.; Kanbay, M.; Andres-Hernando, A.; Roncal-Jimenez, C.A.; Sato, Y.; Garcia, G.; Ohno, M.; Lanaspa, M.A.; et al. Increased Serum Uric Acid over Five Years Is a Risk Factor for Developing Fatty Liver. Sci. Rep. 2018, 8, 11735. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chao, G.; Chen, L. Study on the Independent Effect of Thyroid Hormone Based on Uric Acid Level on NAFLD. J. Health Popul. Nutr. 2021, 40, 21. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Z.; Song, K.; Qiu, J.; Wang, Y.; Liu, C.; Zhou, H.; Xu, Y.; Guo, Z.; Zhang, B.; Dong, C. Associations between Serum Uric Acid and the Remission of Non-Alcoholic Fatty Liver Disease in Chinese Males. PLoS ONE 2016, 11, e0166072. [Google Scholar] [CrossRef] [Green Version]
- Sedhom, S.S.; Badary, O.A.; Salama, S.H.; Mokhles, M.A. Assessment of the Therapeutic Effect of Allopurinol on Patients with Non-Alcoholic Fatty Liver Disease Associated with Hyperuricemia by Cytokeratin 18. In Proceedings of the 9th Euro Global Gastroenterology Conference, Valencia, Spain, 24–25 October 2016. [Google Scholar]
- West, B.; Luke, A.; Durazo-Arvizu, R.A.; Cao, G.; Shoham, D.; Kramer, H. Metabolic Syndrome and Self-Reported History of Kidney Stones: The National Health and Nutrition Examination Survey (NHANES III) 1988–1994. Am. J. Kidney Dis. 2008, 51, 741–747. [Google Scholar] [CrossRef]
- Wong, Y.; Cook, P.; Roderick, P.; Somani, B.K. Metabolic Syndrome and Kidney Stone Disease: A Systematic Review of Literature. J. Endourol. 2016, 30, 246–253. [Google Scholar] [CrossRef] [PubMed]
- Boyd, C.; Wood, K.; Whitaker, D.; Assimos, D.G. The Influence of Metabolic Syndrome and Its Components on the Development of Nephrolithiasis. Asian J. Urol. 2018, 5, 215–222. [Google Scholar] [CrossRef] [PubMed]
- Ping, H.; Lu, N.; Wang, M.; Lu, J.; Liu, Y.; Qiao, L.; Wang, Y.; Jiang, L.; Zhang, X. New-Onset Metabolic Risk Factors and the Incidence of Kidney Stones: A Prospective Cohort Study. BJU Int. 2019, 124, 1028–1033. [Google Scholar] [CrossRef] [PubMed]
- Maalouf, N.M.; Cameron, M.A.; Moe, O.W.; Adams-Huet, B.; Sakhaee, K. Low Urine pH: A Novel Feature of the Metabolic Syndrome. Clin. J. Am. Soc. Nephrol. 2007, 2, 883–888. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bamberger, J.N.; Rosen, D.C.; Khusid, J.A.; Kaplan-Marans, E.; Gallante, B.; Kapoor, A.; Paranjpe, I.; Atashsokhan, D.J.; Atallah, W.M.; Gupta, M. The Impact of Metabolic Syndrome Components on Urinary Parameters and Risk of Stone Formation. World J. Urol. 2021, 39, 4483–4490. [Google Scholar] [CrossRef]
- Domingos, F.; Serra, A. Nephrolithiasis is associated with an increased prevalence of cardiovascular disease. Nephrol. Dial. Transplant. 2011, 26, 864–868. [Google Scholar] [CrossRef] [Green Version]
- Ferraro, P.M.; Taylor, E.N.; Eisner, B.H.; Gambaro, G.; Rimm, E.B.; Mukamal, K.J.; Curhan, G.C. History of Kidney Stones and the Risk of Coronary Heart Disease. JAMA 2013, 310, 408–415. [Google Scholar] [CrossRef] [Green Version]
- Friedman, A.N. High-Protein Diets: Potential Effects on the Kidney in Renal Health and Disease. Am. J. Kidney Dis. 2004, 44, 950–962. [Google Scholar] [CrossRef]
- Ko, G.-J.; Rhee, C.M.; Kalantar-Zadeh, K.; Joshi, S. The Effects of High-Protein Diets on Kidney Health and Longevity. J. Am. Soc. Nephrol. 2020, 31, 1667–1679. [Google Scholar] [CrossRef] [PubMed]
- Ogna, A.; Forni Ogna, V.; Bochud, M.; Guessous, I.; Paccaud, F.; Burnier, M.; Wuerzner, G. Association between Obesity and Glomerular Hyperfiltration: The Confounding Effect of Smoking and Sodium and Protein Intakes. Eur. J. Nutr. 2016, 55, 1089–1097. [Google Scholar] [CrossRef] [PubMed]
| C Group n = 41 Mean ± SD/n (%) | MR Group n = 37 Mean ± SD/n (%) | C vs. MR p Value | |
|---|---|---|---|
| Age (years) | 50.2 ± 11.0 | 49.0 ± 12.8 | 0.821 a |
| Weight (kg) | 86.2 ± 9.6 | 85.8 ± 8.9 | 0.790 a |
| Height (cm) | 164.4 ± 6.2 | 164.3 ± 6.0 | 0.982 a |
| BMI (kg/m2) | 31.8 ± 2.2 | 31.7 ± 2.2 | 0.811 a |
| BMI 27.0–29.9 kg/m2 (n) | 9 (22.0%) | 9 (24.3%) | 0.867 b |
| BMI 30.0–34.9 kg/m2 (n) | 28 (68.3%) | 26 (70.3%) | 0.867 b |
| BMI 35.0–39.9 kg/m2 (n) | 4 (9.8%) | 2 (5.4%) | 0.867 b |
| WC (cm) | 96.4 ± 6.9 | 95.5 ± 7.4 | 0.681 a |
| WC 80–88 cm (n) | 6 (14.6%) | 7 (18.9%) c | 0.762 d |
| WC > 88 cm (n) | 35 (85.4%) | 29 (78.4%) c | 0.762 d |
| BP systolic (mmHg) | 130.0 ± 19.4 | 132.3 ± 18.2 | 0.262 a |
| BP diastolic (mmHg) | 80.6 ± 9.2 | 80.4 ± 10.2 | 0.714 a |
| Glucose (mg/dL) e | 87.9 ± 11.1 | 90.9 ± 14.2 | 0.494 a |
| TC (mg/dL) e | 238.1 ± 35.2 | 235.9 ± 51.1 | 0.893 a |
| HDL-C (mg/dL) e | 58.7 ± 11.9 | 56.9 ± 15.6 | 0.401 a |
| TG (mg/dL) f | 155.0 ± 86.5 | 207.6 ± 158.2 | 0.425 a |
| Serum uric acid (mg/dL) e | 4.92 ± 0.99 | 5.17 ± 1.28 | 0.451 a |
| Smokers (n) | 7 (17.1%) | 6 (16.2%) | 1.000 d |
| C Group n = 41 Mean ± SD n (%) | MR Group n = 37 Mean ± SD n (%) | C vs. MR | |||||
|---|---|---|---|---|---|---|---|
| Baseline | Week 12 | p Value a | Baseline | Week 12 | p Value a | p Value b | |
| Weight (kg) | 86.2 ± 9.6 | 81.2 ± 8.9 | <0.001 | 85.8 ± 8.9 | 79.4 ± 8.9 | <0.001 | 0.072 |
| Relative weight (%) | 100 ± 0 | 94.2 ± 4.1 | <0.001 | 100 ± 0 | 92.5 ± 3.1 | <0.001 | 0.048 |
| Weight loss > 5% (n/%) | – | 22 (53.7%) | – | – | 29 (78.4%) | – | 0.032 c |
| BMI (kg/m2) | 31.8 ± 2.2 | 30.0 ± 2.2 | <0.001 | 31.7 ± 2.2 | 29.4 ± 2.4 | <0.001 | 0.068 |
| Waist circumference (cm) | 96.4 ± 6.9 | 91.0 ± 7.0 | <0.001 | 95.5 ± 7.4 | 88.5 ± 7.7 | <0.001 | 0.086 |
| Hip circumference (cm) d | 115.0 ± 6.4 | 110.1 ± 6.8 | <0.001 | 114.3 ± 6.3 | 108.7 ± 5.9 | <0.001 | 0.623 |
| Thigh circumference (cm) | 64.6 ± 4.8 | 62.0 ± 5.1 | <0.001 | 64.3 ± 5.0 | 61.0 ± 5.0 | <0.001 | 0.124 |
| WHtR | 0.587 ± 0.043 | 0.554 ± 0.047 | <0.001 | 0.581 ± 0.044 | 0.539 ± 0.048 | <0.001 | 0.082 |
| WHR d | 0.84 ± 0.05 | 0.84 ± 0.06 | 0.428 | 0.83 ± 0.05 | 0.82 ± 0.06 | 0.044 | 0.344 |
| VAI e,f | 2.28 ± 1.44 | 2.22 ± 1.16 | 0.798 | 3.49 ± 3.26 | 2.96 ± 2.48 | 0.316 | 0.596 |
| FLI e,g | 65.6 ± 15.9 | 53.1 ± 18.8 | <0.001 | 69.2 ± 21.8 | 52.4 ± 24.4 | <0.001 | 0.212 |
| BFM (kg) | 38.2 ± 6.7 | 34.0 ± 6.3 | <0.001 | 37.7 ± 6.4 | 32.7 ± 6.5 | <0.001 | 0.110 |
| BFM (%) | 44.0 ± 3.7 | 41.7 ± 4.1 | <0.001 | 43.7 ± 3.6 | 40.9 ± 4.3 | <0.001 | 0.209 |
| BCM (kg) | 25.8 ± 2.6 | 25.0 ± 2.5 | <0.001 | 25.7 ± 2.5 | 24.7 ± 2.4 | <0.001 | 0.681 |
| BCM (%) | 30.1 ± 3.0 | 30.9 ± 3.0 | <0.001 | 30.1 ± 2.7 | 31.3 ± 3.3 | <0.001 | 0.216 |
| LBM (kg) | 48.3 ± 4.5 | 47.5 ± 3.9 | <0.001 | 48.4 ± 3.6 | 47.0 ± 3.5 | <0.001 | 0.131 |
| LBM (%) | 56.3 ± 3.8 | 58.7 ± 4.2 | <0.001 | 56.6 ± 3.5 | 59.5 ± 4.3 | <0.001 | 0.324 |
| ECM (kg) | 22.6 ± 2.7 | 22.5 ± 2.3 | 0.942 | 22.7 ± 2.2 | 22.3 ± 2.3 | 0.085 | 0.222 |
| ECM (%) | 26.2 ± 1.9 | 27.8 ± 2.2 | <0.001 | 26.5 ± 2.3 | 28.2 ± 2.6 | <0.001 | 0.811 |
| BP systolic (mmHg) | 130.0 ± 19.4 | 120.1 ± 13.9 | 0.014 | 132.3 ± 18.2 | 119.6 ± 13.8 | 0.001 | 0.183 |
| BP diastolic (mmHg) | 80.6 ± 9.2 | 75.5 ± 8.3 | 0.009 | 80.4 ± 10.2 | 76.0 ± 8.6 | 0.036 | 0.752 |
| Heart rate (1/min) h | 78.1 ± 11.6 | 76.0 ± 12.6 | 0.145 | 79.1 ± 12.8 | 76.9 ± 10.5 | 0.292 | 0.986 |
| C Group n = 41 n (%) | MR Group n = 37 n (%) | C vs. MR | |||||
|---|---|---|---|---|---|---|---|
| Baseline | Week 12 | p Value a | Baseline | Week 12 | p Value a | p Value b | |
| Weight reduction > 5% | – | 22 (53.7%) | – | – | 29 (78.4%) | – | 0.032 |
| WC > 88 cm | 35 (85.4%) | 26 (63.4%) | 0.041 | 29 (78.4%) | 19 (51.4%) | 0.027 | 0.622 |
| BP systolic ≥ 130 mmHg | 23 (56.1%) | 16 (39.0%) | 0.184 | 25 (67.6%) | 12 (32.4%) | 0.005 | 0.699 |
| BP diastolic ≥ 85 mmHg | 12 (29.3%) | 7 (17.1%) | 0.295 | 14 (37.8%) | 5 (13.5%) | 0.032 | 0.858 |
| BP ≥ 130/85 mmHg | 11 (26.8%) | 7 (17.1%) | 0.424 | 13 (35.1%) | 4 (10.8%) | 0.025 | 0.748 |
| TG ≥ 150 mg/dL c | 11 (37.9%) | 13 (44.8%) | 0.790 | 14 (50.0%) | 15 (53.6%) | 1.000 | 0.747 |
| HDL-C < 50 mg/dL d | 9 (30.0%) | 10 (33.3%) | 1.000 | 10 (35.7%) | 11 (39.3%) | 1.000 | 0.921 |
| Fasting glucose ≥ 110 mg/dL d | 2 (6.7%) | 0 (0%) | 0.492 | 2 (7.1%) | 1 (3.6%) | 1.000 | 0.942 |
| FLI ≥ 60 c,e | 20 (69.0%) | 10 (34.5%) | 0.017 | 20 (71.4%) | 11 (39.3%) | 0.031 | 0.980 |
| Hypertriglyceridemic waist c,f | 10 (34.5%) | 8 (27.6%) | 0.777 | 12 (42.9%) | 8 (28.6%) | 0.403 | 0.947 |
| Atherogenic dyslipidemia c,g | 0 (0%) | 0 (0%) | – | 2 (7.1%) | 3 (10.7%) | 1.000 | 0.159 |
| Metabolic syndrome c,h | 13 (44.8%) | 9 (31.0%) | 0.417 | 17 (60.7%) | 10 (35.7%) | 0.108 | 0.669 |
| Metabolic syndrome c,i | 5 (17.2%) | 3 (10.3%) | 0.706 | 8 (28.6%) | 6 (21.4%) | 0.758 | 0.536 |
| Metabolic syndrome c,j | 14 (48.3%) | 13 (44.8%) | 1.000 | 17 (60.7%) | 14 (50.0%) | 0.591 | 0.800 |
| C Group n = 30 a Mean ± SD | MR Group n = 28 a Mean ± SD | C vs. MR | |||||
|---|---|---|---|---|---|---|---|
| Baseline | Week 12 | p Value b | Baseline | Week 12 | p Value b | p Value c | |
| Total protein (g/dL) | 7.45 ± 0.35 | 7.48 ± 0.47 | 0.843 | 7.37 ± 0.35 | 7.54 ± 0.54 | 0.238 | 0.549 |
| Glucose (mg/dL) | 87.9 ± 11.1 | 86.3 ± 10.4 | 0.506 | 90.9 ± 14.2 | 90.4 ± 10.8 | 0.625 | 0.760 |
| HbA1c (%) | 5.59 ± 0.48 | 5.55 ± 0.40 | 0.657 | 5.59 ± 0.43 | 5.59 ± 0.46 | 0.986 | 0.777 |
| TC (mg/dL) | 238.1 ± 35.2 | 226.3 ± 42.6 | 0.015 | 235.9 ± 51.1 | 221.1 ± 53.0 | 0.028 | 0.960 |
| HDL-C (mg/dL) | 58.7 ± 11.9 | 55.5 ± 11.5 | 0.005 | 56.9 ± 15.6 | 54.6 ± 14.2 | 0.005 | 0.856 |
| LDL-C (mg/dL) d | 159.2 ± 24.9 | 148.4 ± 31.8 | 0.009 | 154.0 ± 38.6 | 140.9 ± 38.5 | 0.001 | 0.940 |
| TG (mg/dL) d | 155.0 ± 86.5 | 150.0 ± 65.1 | 0.643 | 207.6 ± 158.2 | 178.6 ± 121.7 | 0.287 | 0.773 |
| TG/HDL-C d | 2.79 ± 1.72 | 2.78 ± 1.37 | 0.949 | 4.23 ± 4.03 | 3.69 ± 3.03 | 0.508 | 0.596 |
| LDL-C/HDL-C d | 2.80 ± 0.63 | 2.73 ± 0.67 | 0.442 | 2.85 ± 0.85 | 2.69 ± 0.80 | 0.026 | 0.345 |
| TC/HDL-C | 4.2 ± 0.8 | 4.2 ± 0.8 | 0.839 | 4.4 ± 1.2 | 4.2 ± 1.1 | 0.327 | 0.382 |
| GOT (U/L) | 24.7 ± 6.5 | 23.1 ± 5.7 | 0.132 | 24.4 ± 6.4 | 24.4 ± 6.4 | 0.557 | 0.596 |
| GPT (U/L) | 29.1 ± 15.6 | 25.3 ± 13.9 | 0.045 | 29.4 ± 13.5 | 26.7 ± 11.7 | 0.302 | 0.719 |
| GGT (U/L) | 28.4 ± 13.6 | 24.8 ± 11.4 | <0.001 | 34.9 ± 29.2 | 29.0 ± 20.5 | 0.002 | 0.455 |
| Uric acid (mg/dL) | 4.92 ± 0.99 | 4.78 ± 0.98 | 0.407 | 5.17 ± 1.28 | 4.87 ± 1.21 | 0.013 | 0.312 |
| Homocysteine (µmol/L) | 10.5 ± 2.0 | 11.7 ± 2.7 | 0.035 | 12.6 ± 4.9 | 11.8 ± 3.6 | 0.155 | 0.010 |
| Folic acid (µg/L) | 11.4 ± 4.5 | 12.3 ± 7.7 | 0.931 | 10.0 ± 4.5 | 14.6 ± 6.1 | <0.001 | 0.005 |
| Creatinine (mg/dL) | 0.87 ± 0.08 | 0.91 ± 0.07 | 0.001 | 0.89 ± 0.12 | 0.90 ± 0.11 | 0.486 | 0.071 |
| GFR (mL/min/1.73 m2) e | 78.6 ± 11.6 | 74.6 ± 10.3 | 0.001 | 79.6 ± 15.0 | 79.0 ± 14.9 | 0.452 | 0.067 |
| CRP (mg/L) f | 4.4 ± 3.5 | 5.0 ± 5.6 | 0.726 | 5.2 ± 3.8 | 5.3 ± 4.4 | 0.883 | 0.883 |
| TSH (mU/L) g | 1.39 ± 0.91 | 1.40 ± 0.76 | 0.871 | 1.52 ± 0.91 | 1.63 ± 0.96 | 0.146 | 0.368 |
| TAC (µmol/L) | 282.8 ± 42.3 | 294.2 ± 38.0 | 0.455 | 270.0 ± 26.5 | 284.0 ± 33.7 | 0.085 | 0.570 |
| Cortisol (nmol/L) | 366.9 ± 143.3 | 480.9 ± 144.2 | <0.001 | 431.4 ± 150.9 | 562.9 ± 171.1 | <0.001 | 0.685 |
| TAC/Cortisol (103) | 0.91 ± 0.45 | 0.68 ± 0.26 | 0.006 | 0.72 ± 0.29 | 0.56 ± 0.20 | 0.001 | 0.740 |
| C Group n = 41 Mean ± SD | MR Group n = 37 Mean ± SD | C vs. MR | |||||
|---|---|---|---|---|---|---|---|
| Baseline | Week 12 | p Value a | Baseline | Week 12 | p Value a | p Value b | |
| Volume (L/24 h) | 2.113 ± 0.753 | 2.404 ± 0.801 | 0.018 | 2.114 ± 0.669 | 2.764 ± 1.143 | < 0.001 | 0.211 |
| pH | 6.38 ± 0.62 | 6.31 ± 0.63 | 0.890 | 6.19 ± 0.52 | 6.41 ± 0.57 | 0.062 | 0.232 |
| Density (g/cm3) | 1.007 ± 0.004 | 1.006 ± 0.004 | 0.269 | 1.008 ± 0.004 | 1.006 ± 0.003 | 0.001 | 0.184 |
| Sodium (mmol/24 h) | 163 ± 82 | 153 ± 67 | 0.756 | 165 ± 71 | 146 ± 85 | 0.083 | 0.299 |
| Potassium (mmol/24 h) | 57 ± 27 | 62 ± 31 | 0.387 | 62 ± 22 | 67 ± 35 | 0.907 | 0.617 |
| Calcium (mmol/24 h) | 3.53 ± 1.84 | 3.74 ± 2.31 | 0.555 | 4.17 ± 2.30 | 4.64 ± 2.84 | 0.941 | 0.850 |
| Magnesium (mmol/24 h) | 3.25 ± 1.80 | 3.10 ± 1.73 | 0.553 | 3.56 ± 1.64 | 3.67 ± 2.12 | 0.665 | 0.931 |
| Ammonium (mmol/24 h) | 20.1 ± 9.8 | 21.1 ± 10.1 | 0.368 | 21.0 ± 11.0 | 20.9 ± 11.5 | 0.743 | 0.324 |
| Chloride (mmol/24 h) | 178 ± 90 | 177 ± 71 | 0.729 | 185 ± 77 | 172 ± 96 | 0.172 | 0.198 |
| Phosphate (mmol/24 h) | 24.0 ± 10.2 | 23.9 ± 11.2 | 0.848 | 24.9 ± 9.8 | 24.1 ± 14.7 | 0.094 | 0.269 |
| Sulfate (mmol/24 h) | 18.0 ± 7.7 | 18.1 ± 8.2 | 0.837 | 20.5 ± 8.5 | 22.6 ± 9.6 | 0.464 | 0.577 |
| Creatinine (mmol/24 h) | 9.04 ± 4.12 | 8.70 ± 3.95 | 0.980 | 9.69 ± 3.50 | 8.83 ± 5.59 | 0.070 | 0.212 |
| Uric acid (mmol/24 h) | 2.78 ± 1.21 | 2.97 ± 1.10 | 0.322 | 3.02 ± 1.27 | 2.85 ± 1.01 | 0.261 | 0.148 |
| Oxalate (mmol/24 h) | 0.349 ± 0.180 | 0.289 ± 0.126 | 0.226 | 0.333 ± 0.106 | 0.297 ± 0.155 | 0.068 | 0.584 |
| Citrate (mmol/24 h) | 3.100 ± 1.792 | 3.050 ± 1.757 | 0.848 | 2.891 ± 1.672 | 3.014 ± 1.983 | 0.988 | 1.000 |
| RS Brushite | 0.575 ± 0.353 | 0.550 ± 0.630 | 0.148 | 0.630 ± 0.506 | 0.626 ± 0.461 | 0.929 | 0.319 |
| RS Struvite | 0.066 ± 0.130 | 0.064 ± 0.119 | 0.788 | 0.035 ± 0.051 | 0.040 ± 0.049 | 0.602 | 0.605 |
| RS Uric acid | 0.714 ± 0.672 | 0.851 ± 1.289 | 0.599 | 1.021 ± 0.983 | 0.547 ± 0.596 | 0.002 | 0.085 |
| RS Calcium oxalate | 3.183 ± 1.719 | 2.474 ± 1.514 | 0.009 | 3.668 ± 1.995 | 2.652 ± 1.663 | 0.003 | 0.210 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Siener, R.; Ernsten, C.; Bitterlich, N.; Alteheld, B.; Metzner, C. Effect of Two Different Dietary Weight Loss Strategies on Risk Factors for Urinary Stone Formation and Cardiometabolic Risk Profile in Overweight Women. Nutrients 2022, 14, 5054. https://doi.org/10.3390/nu14235054
Siener R, Ernsten C, Bitterlich N, Alteheld B, Metzner C. Effect of Two Different Dietary Weight Loss Strategies on Risk Factors for Urinary Stone Formation and Cardiometabolic Risk Profile in Overweight Women. Nutrients. 2022; 14(23):5054. https://doi.org/10.3390/nu14235054
Chicago/Turabian StyleSiener, Roswitha, Charlotte Ernsten, Norman Bitterlich, Birgit Alteheld, and Christine Metzner. 2022. "Effect of Two Different Dietary Weight Loss Strategies on Risk Factors for Urinary Stone Formation and Cardiometabolic Risk Profile in Overweight Women" Nutrients 14, no. 23: 5054. https://doi.org/10.3390/nu14235054






