Vitamin D3 Supplementation in Overweight/Obese Pregnant Women: No Effects on the Maternal or Fetal Lipid Profile and Body Fat Distribution—A Secondary Analysis of the Multicentric, Randomized, Controlled Vitamin D and Lifestyle for Gestational Diabetes Prevention Trial (DALI)
Abstract
1. Introduction
2. Materials and Methods
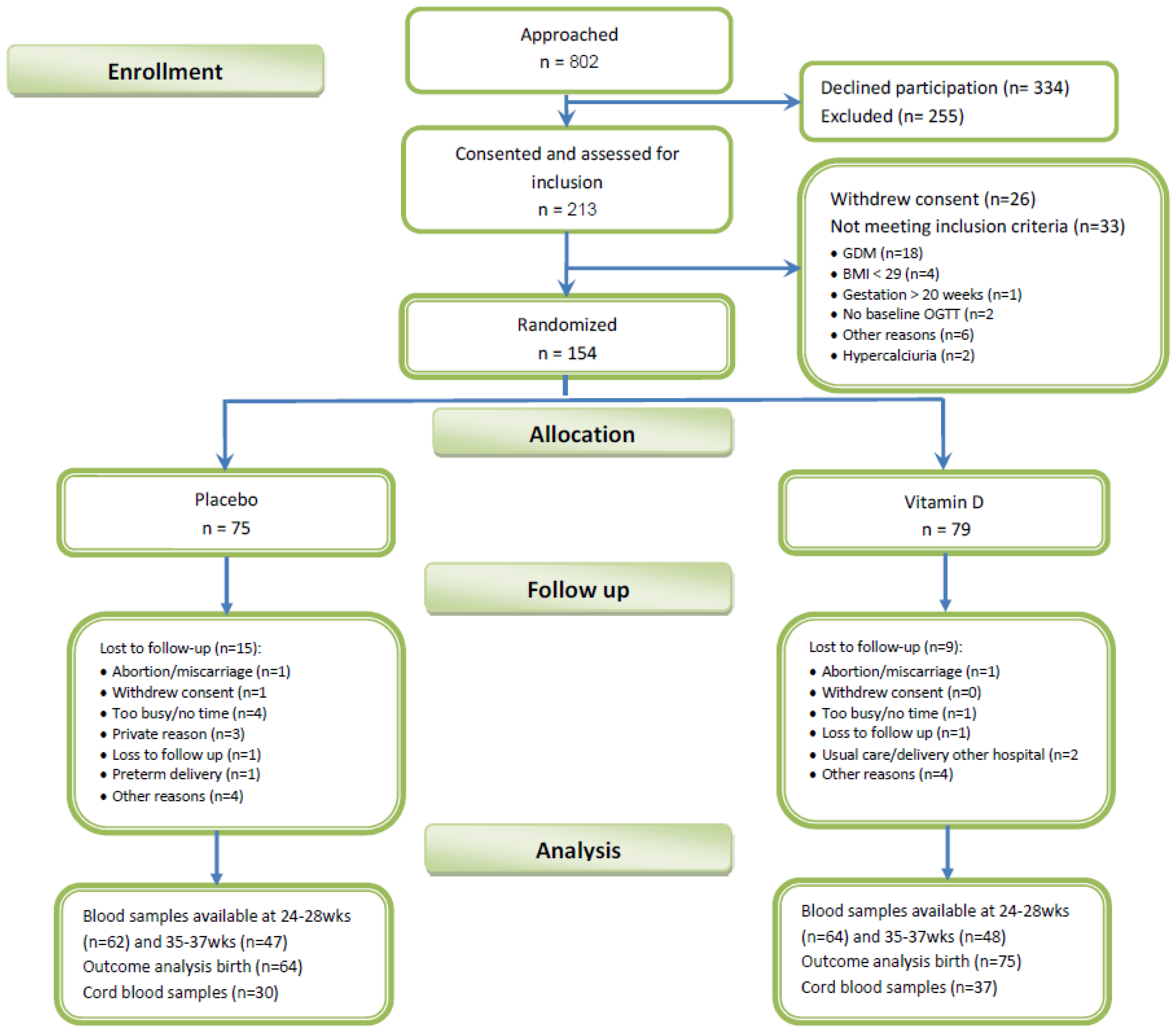
2.1. Study Design and Participants
2.2. Study Procedures and Study Intervention
2.3. Assessments
2.4. Behaviour Assessment
2.5. Laboratory Analyses
2.6. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Intervention Effects on Maternal Vitamin D and Lipid Levels
3.3. Cord Blood Lipid and Vitamin D Levels and Birth Outcomes
3.4. Correlation Analysis
4. Discussion
4.1. Maternal Outcomes
4.2. Birth Outcomes
4.3. Limitations and Strengths
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rosen, C.J.; Adams, J.S.; Bikle, D.D.; Black, D.M.; Demay, M.B.; Manson, J.E.; Murad, M.H.; Kovacs, C.S. The nonskeletal effects of vitamin D: An endocrine society scientific statement. Endocr. Rev. 2012, 33, 456–492. [Google Scholar] [PubMed]
- Hollis, B.W.; Wagner, C.L. New insights into the vitamin D requirements during pregnancy. Bone Res. 2017, 5, 17030. [Google Scholar] [CrossRef] [PubMed]
- Palacios, C.; Trak-Fellermeier, M.A.; Martinez, R.X.; Lopez-Perez, L.; Lips, P.; Salisi, J.A.; John, J.C.; Pena-Rosas, J.P. Regimens of vitamin D supplementation for women during pregnancy. Cochrane Database Syst. Rev. 2019, 10, CD013446. [Google Scholar] [CrossRef] [PubMed]
- Bodnar, L.M.; Catov, J.M.; Roberts, J.M.; Simhan, H.N. Prepregnancy obesity predicts poor vitamin D status in mothers and their neonates. J. Nutr. 2007, 137, 2437–2442. [Google Scholar] [CrossRef] [PubMed]
- Josefson, J.L.; Feinglass, J.; Rademaker, A.W.; Metzger, B.E.; Zeiss, D.M.; Price, H.E.; Langman, C.B. Maternal obesity and vitamin d sufficiency are associated with cord blood vitamin D insufficiency. J. Clin. Endocrinol. Metab. 2013, 98, 114–119. [Google Scholar] [CrossRef] [PubMed]
- Geraghty, A.A.; Alberdi, G.; O’Sullivan, E.J.; O’Brien, E.C.; Crosbie, B.; Twomey, P.J.; McAuliffe, F.M. Maternal and fetal blood lipid concentrations during pregnancy differ by maternal body mass index: Findings from the ROLO study. BMC Pregnancy Childbirth 2017, 17, 360. [Google Scholar] [CrossRef] [PubMed]
- Harreiter, J.; Simmons, D.; Desoye, G.; Corcoy, R.; Adelantado, J.M.; Devlieger, R.; van Assche, A.; Galjaard, S.; Damm, P.; Mathiesen, E.R.; et al. IADPSG and WHO 2013 gestational diabetes mellitus criteria identify obese women with marked insulin resistance in early pregnancy. Diabetes Care 2016, 39, e90–e92. [Google Scholar] [CrossRef]
- Akbari, M.; Moosazaheh, M.; Lankarani, K.B.; Tabrizi, R.; Samimi, M.; Karamali, M.; Jamilian, M.; Kolahdooz, F.; Asemi, Z. The effects of vitamin D supplementation on glucose metabolism and lipid profiles in patients with gestational diabetes: A systematic review and meta-analysis of randomized controlled trials. Horm. Metab. Res. 2017, 49, 647–653. [Google Scholar]
- Hashemipour, S.; Ziaee, A.; Javadi, A.; Movahed, F.; Elmizadeh, K.; Javadi, E.H.; Lalooha, F. Effect of treatment of vitamin D deficiency and insufficiency during pregnancy on fetal growth indices and maternal weight gain: A randomized clinical trial. Eur. J. Obstet. Gynecol. Reprod. Biol. 2014, 172, 15–19. [Google Scholar] [CrossRef]
- Zhang, Q.; Zhang, C.; Wang, Y.; Zhao, J.; Li, H.; Shen, Q.; Wang, X.; Ni, M.; Ouyang, F.; Vinturache, A.; et al. Relationship of maternal obesity and vitamin D concentrations with fetal growth in early pregnancy. Eur. J. Nutr. 2022, 61, 915–924. [Google Scholar] [CrossRef]
- Chen, W.; Li, Y.; Gao, B.; Li, J.; Zheng, M.; Chen, X. Serum 25-hydroxyvitamin D levels in relation to lipids and clinical outcomes in pregnant women with gestational diabetes mellitus: An observational cohort study. BMJ Open 2020, 10, e039905. [Google Scholar] [CrossRef]
- Yazdchi, R.; Gargari, B.P.; Asghari-Jafarabadi, M.; Sahhaf, F. Effects of vitamin D supplementation on metabolic indices and hs-CRP levels in gestational diabetes mellitus patients: A randomized, double-blinded, placebo-controlled clinical trial. Nutr. Res. Pract. 2016, 10, 328–335. [Google Scholar] [CrossRef][Green Version]
- Barbour, L.A.; Hernandez, T.L. Maternal non-glycemic contributors to fetal growth in obesity and gestational diabetes: Spotlight on lipids. Curr. Diab. Rep. 2018, 18, 37. [Google Scholar] [CrossRef]
- Barrett, H.L.; Gatford, K.L.; Houda, C.M.; De Blasio, M.J.; McIntyre, H.D.; Callaway, L.K.; Dekker Nitert, M.; Coat, S.; Owens, J.A.; Hague, W.M.; et al. Maternal and neonatal circulating markers of metabolic and cardiovascular risk in the metformin in gestational diabetes (MIG) trial: Responses to maternal metformin versus insulin treatment. Diabetes Care 2013, 36, 529–536. [Google Scholar] [CrossRef]
- Miliku, K.; Vinkhuyzen, A.; Blanken, L.M.; McGrath, J.J.; Eyles, D.W.; Burne, T.H.; Hofman, A.; Tiemeier, H.; Steegers, E.A.; Gaillard, R.; et al. Maternal vitamin D concentrations during pregnancy, fetal growth patterns, and risks of adverse birth outcomes. Am. J. Clin. Nutr. 2016, 103, 1514–1522. [Google Scholar] [CrossRef]
- Jelsma, J.G.; van Poppel, M.N.; Galjaard, S.; Desoye, G.; Corcoy, R.; Devlieger, R.; van Assche, A.; Timmerman, D.; Jans, G.; Harreiter, J.; et al. DALI: Vitamin D and lifestyle intervention for gestational diabetes mellitus (GDM) prevention: An european multicentre, randomised trial-study protocol. BMC Pregnancy Childbirth 2013, 13, 142. [Google Scholar] [CrossRef]
- Simmons, D.; Devlieger, R.; van Assche, A.; Jans, G.; Galjaard, S.; Corcoy, R.; Adelantado, J.M.; Dunne, F.; Desoye, G.; Harreiter, J.; et al. Effect of physical activity and/or healthy eating on GDM risk: The DALI lifestyle study. J. Clin. Endocrinol. Metab. 2017, 102, 903–913. [Google Scholar] [CrossRef]
- Harreiter, J.; Simmons, D.; Desoye, G.; Corcoy, R.; Adelantado, J.M.; Devlieger, R.; Galjaard, S.; Damm, P.; Mathiesen, E.R.; Jensen, D.M.; et al. Nutritional lifestyle intervention in obese pregnant women, including lower carbohydrate intake, is associated with increased maternal free fatty acids, 3-beta-hydroxybutyrate, and fasting glucose concentrations: A secondary factorial analysis of the european multicenter, randomized controlled DALI lifestyle intervention trial. Diabetes Care 2019, 42, 1380–1389. [Google Scholar]
- Corcoy, R.; Mendoza, L.C.; Simmons, D.; Desoye, G.; Adelantado, J.M.; Chico, A.; Devlieger, R.; van Assche, A.; Galjaard, S.; Timmerman, D.; et al. The DALI vitamin D randomized controlled trial for gestational diabetes mellitus prevention: No major benefit shown besides vitamin d sufficiency. Clin. Nutr. 2020, 39, 976–984. [Google Scholar] [CrossRef]
- Hollis, B.W.; Johnson, D.; Hulsey, T.C.; Ebeling, M.; Wagner, C.L. Vitamin D supplementation during pregnancy: Double-blind, randomized clinical trial of safety and effectiveness. J. Bone Miner. Res. 2011, 26, 2341–2357. [Google Scholar] [CrossRef]
- Chasan-Taber, L.; Schmidt, M.D.; Roberts, D.E.; Hosmer, D.; Markenson, G.; Freedson, P.S. Development and validation of a pregnancy physical activity questionnaire. Med. Sci. Sports Exerc. 2004, 36, 1750–1760. [Google Scholar] [CrossRef]
- Simmons, D.; Mandell, C.; Fleming, C.; Gatland, B.; Leakehe, L. Evaluation of a diabetes knowledge and behaviour (DKB) questionnaire. Asia Pac. J. Clin. Nutr. 1994, 3, 193–200. [Google Scholar]
- Alvarez, J.J.; Montelongo, A.; Iglesias, A.; Lasuncion, M.A.; Herrera, E. Longitudinal study on lipoprotein profile, high density lipoprotein subclass, and postheparin lipases during gestation in women. J. Lipid Res. 1996, 37, 299–308. [Google Scholar] [CrossRef]
- Desoye, G.; Schweditsch, M.O.; Pfeiffer, K.P.; Zechner, R.; Kostner, G.M. Correlation of hormones with lipid and lipoprotein levels during normal pregnancy and postpartum. J. Clin. Endocrinol. Metab. 1987, 64, 704–712. [Google Scholar] [CrossRef]
- Motamed, S.; Nikooyeh, B.; Kashanian, M.; Chamani, M.; Hollis, B.W.; Neyestani, T.R. Evaluation of the efficacy of two doses of vitamin D supplementation on glycemic, lipidemic and oxidative stress biomarkers during pregnancy: A randomized clinical trial. BMC Pregnancy Childbirth 2020, 20, 619. [Google Scholar] [CrossRef]
- Li, Q.; Xing, B. Vitamin D3-supplemented yogurt drink improves insulin resistance and lipid profiles in women with gestational diabetes mellitus: A randomized double blinded clinical trial. Ann. Nutr. Metab. 2016, 68, 285–290. [Google Scholar] [CrossRef]
- Al-Ajlan, A.; Krishnaswamy, S.; Alokail, M.S.; Aljohani, N.J.; Al-Serehi, A.; Sheshah, E.; Alshingetti, N.M.; Fouda, M.; Turkistani, I.Z.; Al-Daghri, N.M. Vitamin D deficiency and dyslipidemia in early pregnancy. BMC Pregnancy Childbirth 2015, 15, 314. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Perichart-Perera, O.; Avila-Sosa, V.; Solis-Paredes, J.M.; Montoya-Estrada, A.; Reyes-Munoz, E.; Rodriguez-Cano, A.M.; Gonzalez-Leyva, C.P.; Sanchez-Martinez, M.; Estrada-Gutierrez, G.; Irles, C. Vitamin D deficiency, excessive gestational weight gain, and oxidative stress predict small for gestational age newborns using an artificial neural network model. Antioxidants 2022, 11, 574. [Google Scholar] [CrossRef] [PubMed]
- Perez-Lopez, F.R.; Pasupuleti, V.; Mezones-Holguin, E.; Benites-Zapata, V.A.; Thota, P.; Deshpande, A.; Hernandez, A.V. Effect of vitamin D supplementation during pregnancy on maternal and neonatal outcomes: A systematic review and meta-analysis of randomized controlled trials. Fertil. Steril. 2015, 103, 1278–1288.e4. [Google Scholar] [CrossRef] [PubMed]
- Crozier, S.R.; Harvey, N.C.; Inskip, H.M.; Godfrey, K.M.; Cooper, C.; Robinson, S.M.; Group, S.W.S.S. Maternal vitamin D status in pregnancy is associated with adiposity in the offspring: Findings from the southampton women’s survey. Am. J. Clin. Nutr. 2012, 96, 57–63. [Google Scholar] [PubMed]
- Razaghi, M.; Gharibeh, N.; Vanstone, C.A.; Sotunde, O.F.; Wei, S.Q.; McNally, D.; Rauch, F.; Jones, G.; Weiler, H.A. Maternal excess adiposity and serum 25-hydroxyvitamin D <50 nmol/L are associated with elevated whole body fat mass in healthy breastfed neonates. BMC Pregnancy Childbirth 2022, 22, 83. [Google Scholar]
- Tint, M.T.; Chong, M.F.; Aris, I.M.; Godfrey, K.M.; Quah, P.L.; Kapur, J.; Saw, S.M.; Gluckman, P.D.; Rajadurai, V.S.; Yap, F.; et al. Association between maternal mid-gestation vitamin D status and neonatal abdominal adiposity. Int. J. Obes. 2018, 42, 1296–1305. [Google Scholar] [CrossRef]
- Archer, E. The childhood obesity epidemic as a result of nongenetic evolution: The maternal resources hypothesis. Mayo Clin. Proc. 2015, 90, 77–92. [Google Scholar] [CrossRef]
- Wen, J.; Hong, Q.; Wang, X.; Zhu, L.; Wu, T.; Xu, P.; Fu, Z.; You, L.; Wang, X.; Ji, C.; et al. The effect of maternal vitamin D deficiency during pregnancy on body fat and adipogenesis in rat offspring. Sci. Rep. 2018, 8, 365. [Google Scholar] [CrossRef]
- Cannell, J.J.; Grant, W.B.; Holick, M.F. Vitamin D and inflammation. Dermatoendocrinology 2014, 6, e983401. [Google Scholar] [CrossRef]
| Vitamin D N = 79 | Placebo N = 75 | p | Total N = 154 | Excluded N = 33 | p | |
|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |||
| Age (year) | 32.8 (5.4) | 32.2 (5.2) | ns | 32.5 (5.3) | 33.5 (4.6) | ns |
| Height (cm) | 165.1 (6.6) | 164.7 (7.4) | ns | 164.9 (7.0) | 163.2 (4.9) | ns |
| Pre-pregnancy weight (kg) | 92.0 (13.8) | 90.3 (13.4) | ns | 91.2 (13.7) | 91.4 (16.1) | ns |
| Pre pregnancy BMI (kg/m2) | 33.7 (4.3) | 33.3 (4.3) | ns | 33.5 (4.3) | 34.3 (6.0) | ns |
| Weight gain until 1st visit (kg) | 2.3 (4.8) | 1.3 (3.4) | ns | 1.8 (4.2) | 2.4 (3.5) | ns |
| Gestational week at enrollment (weeks) | 15.0 (2.9) | 15.4 (2.5) | ns | 15.2 (2.7) | 15.3 (2.8) | ns |
| N (%) | N (%) | N (%) | N (%) | |||
| European descent | 72/79 (91.1) | 59/75 (78.7%) | <0.05 | 131/154 (85.1) | 30/33 (90.9) | ns |
| Higher education | 50/78 (64.1) | 45/75 (60.0) | ns | 95/153 (62.1) | 18/33 (54.5) | ns |
| Multiparity | 48/79 (60.8) | 46/75 (61.3) | ns | 94/154 (61.0) | 21/33 (63.6) | ns |
| Diabetes in family | 12/79 (15.2) | 17/75 (22.7) | ns | 29/154 (18.8) | 11/32 (34.4) | ns |
| History of GDM | 7/46 (15.2) | 7/46 (15.2) | ns | 14/92 (15.2) | 4/19 (21.1) | ns |
| Previous unexplained stillbirth | 5/45 (13.3) | 3/46 (6.5) | ns | 9/91 (9.9) | 2/19 (10.5) | ns |
| History of malformation | 4/47 (8.5) | 1/45 (2.2) | ns | 5/92 (5.4) | 1/19 (5.2) | ns |
| Prev. macrosomia | 15/47 (31.9) | 11/46 (23.9) | ns | 26/93 (28.0) | 6/19 (31.6) | ns |
| PCOS | 10/79 (12.7) | 11/74 (14.9) | ns | 21/153 (13.7) | 6/33 (18.2) | ns |
| Chronic hypertension | 14/79 (17.7) | 9/74 (12.2) | ns | 23/153 (15.0) | 7/33 (21.1) | ns |
| Smoking | 17/79 (22.5) | 14/75 (18.7 | ns | 31/154 (20.1) | 7/33 (21.2) | ns |
| Alcohol in pregnancy | 6/76 (7.9 | 5/74 (6.8) | ns | 11/150 (7.3) | 2/33 (6.1) | ns |
| Taking pregnancy vitamins | 68/79 (86.1%) | 63/75 (84.0%) | ns | 131/154 (85.1) | 32/33 (97.0) | ns |
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |||
| BP sys (mmHg) | 115.6 (11.6) | 114.9 (12.0) | ns | 115.2 (11.7) | 118.9 (11.2) | ns |
| BP dia (mmHg) | 72.4 (9.3) | 71.4 (9.2) | ns | 71.9 (9.2) | 75.0 (8.6) | ns |
| Heart rate (bpm) | 79.2 (10.3) | 79.1 (9.7) | ns | 79.2 (10.0) | 82.4 (11.7) | ns |
| Triglycerides (mmol/L) | 1.32 (0.41) | 1.41 (0.55) | ns | 1.36 (0.48) | 1.40 (0.64) | ns |
| LDL-C (mmol/L) | 3.21 (0.72) | 2.96 (0.73) | <0.05 | 3.08 (0.74) | 3.04 (0.70) | ns |
| HDL-C (mmol/L) | 1.37 (0.23) | 1.33 (0.28) | ns | 1.35 (0.26) | 1.40 (0.22) | ns |
| FFA (mmol/L) | 0.62 (0.23) | 0.64 (0.29) | ns | 0.64 (0.26) | 0.68 (0.22) | ns |
| 3BHB (mmol/L) | 0.067 (0.085) | 0.057 (0.074) | ns | 0.062 (0.080) | 0.087 (0.096) | ns |
| Leptin (ng/dL) | 34.5 (17.6) | 33.7 (17.6) | ns | 34.0 (17.1) | 36.9 (20.3) | ns |
| Calcium (mmol/L) | 2.2 (0.3) | 2.2 (0.4) | ns | 2.2 (0.3) | 2.3 (0.1) | ns |
| Albumin (g/L) | 36.5 (3.6) | 36.1 (3.9) | ns | 36.3 (3.8) | 37.0 (4.5) | ns |
| Albumin-corrected Calcium (mmol/L) | 2.2 (0.3) | 2.2 (0.4) | ns | 2.2 (0.4 | 2.3 (0.1) | ns |
| 25OH D2 (nmol/L) | 4.2 (4.6) | 3.0 (4.3) | ns | 3.6 (4.5) | 3.6 (4.6) | ns |
| 25OH D3 (nmol/L) | 69.3 (26.8) | 66.7 (26.8) | ns | 68.0 (26.7) | 63.3 (25.4) | ns |
| 25OH D total (nmol/L) | 73.40 (26.8) | 69.8 (26.9) | ns | 71.6 (26.8) | 66.9 (25.9) | ns |
| Skinfold biceps (mm) | 20.1 (7.9) | 19.8 (6.4) | ns | 20.0 (7.2) | 17.1 (7.2) | <0.05 |
| Skinfold triceps (mm) | 28.2 (6.6) | 28.1 (6.0) | ns | 28.1 (6.3) | 26.9 (5.7) | ns |
| Skinfold subscapular (mm) | 28.6 (7.4) | 30.3 (9.4) | ns | 29.4 (8.4) | 30.5 (6.8) | ns |
| Skinfold supra-iliac (mm) | 34.3 (7.8) | 33.3 (8.8) | ns | 33.8 (8.3) | 31.8 (7.1) | ns |
| Sum of skinfolds (mm) | 111.3 (20.5) | 111.5 (24.2) | ns | 111.4 (22.3) | 106.3 (19.6) | ns |
| Fat percentage (%) | 31.1 (2.9) | 31.2 (3.2) | ns | 31.1 (3.0) | 30.8 (2.3) | ns |
| Neck circumference (cm) | 36.3 (2.3) | 36.4 (2.0) | ns | 36.4 (2.2) | 36.6 (2.6) | ns |
| Vitamin D n = 77 | Placebo n = 67 | Vit.D vs. Placebo $ | Vit.D vs. Placebo $$ | |||
|---|---|---|---|---|---|---|
| 24–28 weeks | Mean | SD | Mean | SD | mean difference (95% CI) | Adjusted mean difference (95% CI) |
| Gestational age, weeks | 26.5 | 1.4 | 26.3 | 1.6 | 0.3 (−0.2; 0.8) | 0.3 (−0.2; 0.8) |
| Triglyceride, mmol/L | 1.86 | 0.56 | 1.82 | 0.59 | 0.08 (−0.08; 0.24) | 0.05 (−0.13; 0.22) |
| LDL-C, mmol/L | 3.99 * | 0.96 | 3.55 * | 0.83 | 0.20 (−0.03; 0.43) | 0.20 (−0.05; 0.44) |
| HDL-C, mmol/L | 1.47 | 0.21 | 1.45 | 0.28 | 0.00 (−0.05; 0.05) | 0.01 (−0.05; 0.06) |
| FFA, mmol/L | 0.54 | 0.22 | 0.52 | 0.17 | 0.014 (−0.047; 0.076) | 0.015 (−0.053; 0.083) |
| 3BHB, mmol/L | 0.087 | 0.097 | 0.053 | 0.084 | 0.018 (−0.012; 0.048) | 0.007 (−0.027; 0.040) |
| Leptin, ng/dL | 33.0 | 17.5 | 33.0 | 15.3 | −0.4 (−5.1; 4.3) | 0.9 (−3.6; 5.4) |
| Calcium, mmol/L | 2.1 | 0.3 | 2.1 | 0.4 | 0.02 (−0.07; 0.10) | −0.02 (−0.08; 0.05) |
| Albumin-corrected Calcium, mmol/L | 2.2 | 0.4 | 2.2 | 0.5 | 0.04 (−0.08; 0.15) | −0.01 (−0.03; 0.05) |
| 25-OH-D2, nmol/L | 2.9 | 4.3 | 3.3 | 4.7 | −0.6 (−2.0; 0.8) | −0.7 (−2.3; 0.9) |
| 25-OH-D3, nmol/L | 116.6 *** | 35.2 | 78.7 *** | 39.3 | 35.1 (23.3; 46.9) *** | 34.3 (22.5; 46.2) *** |
| 25-OH-D total, nmol/L | 119.5 *** | 35.5 | 82.0 *** | 39.4 | 34.3 (22.4; 46.1) *** | 33.4 (21.5; 45.2) *** |
| Neck circumference, cm | 36.6 | 2.2 | 36.6 | 2.0 | 0.1 (−0.2; 0.5) | 0.1 (−0.3; 0.4) |
| Weight gain, kg | 4.1 | 3.1 | 3.9 | 2.6 | 0.2 (−0.7; 1.1) | −0.4 (−1.3; 0.6) |
| Vitamin D n = 70 | Placebo n = 59 | Vit.D vs. Placebo $ | Vit.D vs. Placebo $$ | |||
| 35–37 weeks | Mean | SD | Mean | SD | mean difference (95% CI) | Adjusted mean difference (95% CI) |
| Gestational age, wks | 35.9 | 0.8 | 35.9 | 0.9 | 0.0 (−0.3; 0.3) | 0.0 (−0.3; 0.3) |
| Triglyceride, mmol/L | 2.49 | 0.73 | 2.29 | 0.80 | 0.19 (−0.08; 0.46) | 0.11 (−0.18; 0.39) |
| LDL-C, mmol/L | 4.06 | 1.01 | 3.68 | 0.93 | 0.17 (−0.14; 0.48) | 0.17 (−0.14; 0.48) |
| HDL-C, mmol/L | 1.41 | 0.25 | 1.44 | 0.30 | −0.00 (−0.08; 0.07) | −0.00 (−0.09; 0.08) |
| FFA, mmol/L | 0.54 | 0.19 | 0.54 | 0.20 | −0.01 (−0.08; 0.07) | −0.04 (−0.12; 0.05) |
| 3BHB, mmol/L | 0.079 | 0.058 | 0.062 | 0.074 | 0.016 (−0.012; 0.043) | 0.012 (−0.019; 0.042) |
| Leptin, ng/dL | 32.7 | 14.3 | 31.7 | 13.0 | 0.38 (−4.6; 5.4) | 1.2 (−3.9; 6.4) |
| Calcium, mmol/L | 2.2 | 0.2 | 2.1 | 0.4 | 0.10 (−0.22; 0.41) | 0.00 (−0.05; 0.05) |
| Albumin-corrected Calcium, mmol/L | 2.3 | 0.3 | 2.2 | 0.4 | 0.04 (−0.08; 0.15) | −0.25 (−0.12; 0.07) |
| 25-OH-D2, µg/L | 2.3 | 4.1 | 2.9 | 4.5 | −1.1 (−2.5; 0.3) | −1.3 (−2.8; 0.3) |
| 25-OH-D3, µg/L | 120.7 *** | 38.9 | 81.7 *** | 40.3 | 38.9 (24.6; 53.1) *** | 36.2 (19.9; 52.5) *** |
| 25-OH- D total, µg/L | 123.0 *** | 38.8 | 84.6 *** | 39.8 | 37.9 (23.8; 51.9) *** | 34.9 (18.8; 51.0) *** |
| Skinfold biceps, mm | 21.0 | 9.0 | 20.8 | 8.0 | −0.1 (−2.9; 2.9) | 0.2 (−3.2; 3.5) |
| Skinfold triceps, mm | 27.4 | 7.1 | 27.7 | 8.1 | −0.4 (−2.7; 1.9) | −1.0 (−3.6; 1.7) |
| Skinfold subscapular, mm | 29.6 | 8.4 | 29.7 | 10.2 | 0.8 (−2.0; 3.6) | −0.2 (−3.5; 3.2) |
| Skinfold supra-iliac, mm | 34.7 | 13.6 | 33.7 | 11.7 | −0.4 (−4.1; 3.3) | −3.3 (−7.6, 1.2) |
| Sum of skinfolds, cm | 112.7 | 28.1 | 111.9 | 30.4 | −0.5 (−9.0; 8.0) | −5.6 (−15.5; 4.3) |
| Fat percentage, % | 31.3 | 3.0 | 31.3 | 3.9 | 0.0 (−1.0; 1.0) | −0.6 (−1.8; 0.6) |
| Neck circumference, cm | 36.8 | 2.6 | 36.8 | 2.1 | 0.1 (−0.2; 0.5) | 0.1 (−0.3; 0.4) |
| Weight gain, kg § | 7.7 | 4.6 | 8.0 | 6.1 | −0.3 (−2.1; 1.5) | −1.6 (−3.2; 0.1) |
| Vit D N = 77 | Placebo N = 62 | ||
|---|---|---|---|
| Before 20 weeks of gestation | Mean (SD) | Mean (SD) | |
| Sugar drinks (n/week) | 7.7 (12.0) | 5.3 (7.1) | |
| Fiber (n/week) | 29.6 (31.4) | 25.6 (12.2) | |
| Protein (n/week) | 8.8 (10.0) | 8.5 (6.1) | |
| Fat (n/week) | 6.6 (6.0) | 5.9 (4.8) | |
| Carbohydrates (n/week) | 39.0 (38.8) | 32.9 (15.7) | |
| Portion size (n/week) | 20.1 (14.3) | 17.5 (11.2) | |
| Total PA (MET.h/week) | 175.1 (84.2) | 195.8 (116.3) | |
| MVPA (MET.h/week) | 58.2 (53.7) * | 81.0 (77.6) * | |
| Sedentary time (MET.h/week) | 13.5 (10.5) | 13.3 (8.5) | |
| 24–28 weeks of gestation | Vit D N = 70 | Placebo N = 62 | Adjusted mean differences Vit D vs. Placebo |
| Sugar drinks (n/week) | 4.2 (4.4) | 4.4 (8.2) | −0.6 (−2.9; 1.7) |
| Fiber (n/week) | 31.7 (19.4) | 35.4 (31.8) | −5.8 (−14.8; 3.3) |
| Protein (n/week) | 7.5 (3.8) | 8.6 (6.4) | −1.4 (−3.2; 0,4) |
| Fat (n/week) | 6.0 (5.6) | 6.5 (7.2) | −0.1 (−2.2; 2.1) |
| Carbohydrates (n/week) | 32.4 (21.4) | 36.6 (40.0) | −6.3 (−12.7; 1.7) |
| Portion size (n/week) | 17.4 (12.4) | 17.0 (21.1) | 0 (−6.2; 6.1) |
| Total PA (MET.h/week) | 163.6 (66.1) | 172.5 (90.2) | −1.3 (−22.2; 19.6) |
| MVPA (MET.h/week) | 58.0 (50.9) | 68.6 (64.3) | −3.1 (−19.7; 13.4) |
| Sedentary time (MET.h/week) | 11.5 (8.1) | 11.8 (7.7) | 2.3 (−0.4; 5.0) |
| 35–37 weeks of gestation | Vit DN = 67 | PlaceboN = 57 | Adjusted mean differences Vit D vs. Placebo |
| Sugar drinks (n/week) | 4.1 (4.9) | 3.6 (4.0) | 0.4 (−1.4; 2.1) |
| Fiber (n/week) | 31.0 (25.5) | 33.9 (20.1) | −4.3 (−12.6; 4.0) |
| Protein (n/week) | 7.9 (6.5) | 8.4 (5.6) | −0.8 (−3.0; 1.3) |
| Fat (n/week) | 7.4 (8.8) | 7.9 (8.6) | 0.3 (−2.5; 3.0) |
| Carbohydrates (n/week) | 30.1 (17.9) | 33.9 (21.7) | −5.5 (−18.2; 5.6) |
| Portion size (n/week) | 18.3 (12.7) | 17.8 (16.7) | −0.2 (−5.5; 5.1) |
| Total PA (MET.h/week) | 133.9 (54.5) | 147.8 (78.3) | −7.0 (−28.1; 14.1) |
| MVPA (MET.h/week) | 37.4 (30.6) | 51.2 (48.8) | −8.3 (−20.9; 4.4) |
| Sedentary time (MET.h/week) | 13.8 (9.2) | 11.5 (7.5) | −0.4 (−2.9; 2.0) |
| Birth and Fetal Cord Blood Outcomes | Vitamin D n = 75 | Placebo n = 64 | Mean Difference (95% CI) Vit.D vs. Placebo † | Adjusted Mean Difference (95% CI) Vit.D vs. Placebo †† | ||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| Gestational age at birth, weeks | 39.6 | 1.6 | 39.8 | 1.9 | −0.10 (−0.69; 0.49) | 0.22 (−0.38; 0.82) |
| Birth weight, g | 3461.2 | 419.7 | 3504.5 | 458.9 | −38.4 (−183.6; 106.9) | −49.9 (−203.3; 103.5) |
| Height, cm | 52.1 | 3.1 | 52.0 | 3.1 | 0.2 (−0.9; 1.3) | 0.1 (−1.0; 1.1) |
| Triglyceride, mmol/L | 0.50 | 0.26 | 0.49 | 0.46 | 0.01 (−0.16; 0.18) | 0.07 (−0.09; 0.24 |
| LDL-C, mmol/L | 0.94 | 0.38 | 0.96 | 0.50 | −0.02 (−0.23; 0.20) | −0.22 (−0.24; 0.20)) |
| HDL-C, mmol/L | 0.57 | 0.17 | 0.64 | 0.21 | −0.06 (−0.15; 0.02) | −0.06 (−0.16; 0.04) |
| FFA, mmol/L | 0.261 | 0.163 | 0.264 | 0.259 | −0.006 (−0.107; 0.095 | 0.023 (−0.084; 0.130) |
| 3BHB, mmol/L | 0.26 | 0.24 | 0.207 | 0.24 | 0.053 (−0.068; 0.174) | 0.046 (−0.079; 0.171) |
| Leptin, ng/dL | 10.1 | 8.1 | 9.6 | 8.3 | 0.5 (−3.5; 4.6) | −2.3 (−6.1; 1.5) |
| 25-OH-D2, nmol/L | 1.3 | 3.2 | 1.8 | 3.7 | −0.4 (−1.4; 2.3) | −0.8 (−2.7; 1.1) |
| 25-OH-D3, nmol/L | 74.2 *** | 22.1 | 51.0 *** | 21.1 | 23.0 (11.3; 34.7) *** | 22.3 (10.8; 33.8) *** |
| 25-OH-D total, nmol/L | 75.5 *** | 21.9 | 52.8 *** | 20.8 | 22.6 (11.0; 34.2) *** | 21.3 (10.1; 32.6) *** |
| Skinfold triceps, mm | 5.0 | 1.0 | 5.0 | 1.4 | 0.0 (−0.5; 0.4) | 0.0 (−0.6; 0.5) |
| Skinfold subscapular, mm | 5.1 | 1.4 | 4.9 | 1.1 | 0.2 (−0.3; 0.7) | 0.2 (−0.4; 0.7) |
| Skinfold supra-iliac, mm | 5.1 | 1.5 | 4.6 | 1.1 | 0.5 (−0.1; 1.0) | 0.5 (−0.1; 1.1) |
| Skinfold thigh, mm | 6.5 | 1.4 | 6.4 | 1.7 | 0.1 (−0.5; 0.7) | 0.1 (−0.6; 0.8) |
| Neonatal sum of skinfolds, mm | 21.8 | 4.4 | 21.0 | 4.3 | 0.7 (−1.0; 2.5) | 0.9 (−1.0; 2.8) |
| Abdominal circumference, cm | 33.4 | 2. 5 | 33.4 | 2.0 | 0.1 (−0.8; 1.0) | 0.1 (−0.9; 1.1) |
| Head circumference, cm | 34.8 | 1.4 | 35.1 | 1.7 | −0.2 (−0.8; 0.3) | −0.1 (−0.7; 0.5) |
| N | % | N | % | OR (95%CI) | OR (95%CI) | |
| Male sex, n, % | 33/74 | 44.6 | 33/64 | 51.6 | 0.78 (0.40; 1.53) | 0.67 (0.32; 1.39) |
| LGA, n, % | 7/73 | 9.6 | 9/60 | 15.0 | 1.57 (0.55; 4.54) | 1.65 (0.51; 5.36) |
| Birth weight above 4000 g, n, % | 7/73 | 9.6 | 9/60 | 15.0 | 1.57 (0.55; 4.54) | 1.65 (0.51; 5.36) |
| SGA, n, % | 0/75 | 0 | 2/61 | 3.3 | N/A | N/A |
| Birth weight below 2500 g, n, % | 0/75 | 0 | 1/64 | 1.6 | N/A | N/A |
| Preeclampsia, n, % | 1/66 | 1.5 | 3/58 | 5.2 | 4.00 (0.36; 44.30) | 4.85 (0.26; 89.67) |
| Preterm birth, n, % | 4/75 | 5.3 | 2/63 | 3.2 | 0.12 (0.01; 1.07) | 0.13 (0.01; 1.20) |
| C-section, n, % | 36/75 | 48.0 | 28/64 | 43.8 | 0.75 (0.37; 1.49) | 0.56 (0.26; 1.25) |
| NICU, n, % | 7/71 | 9.9 | 1/59 | 1.7 | 0.12 (0.01; 0.82) | 0.13 (0.01; 1.20) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Harreiter, J.; Mendoza, L.C.; Simmons, D.; Desoye, G.; Devlieger, R.; Galjaard, S.; Damm, P.; Mathiesen, E.R.; Jensen, D.M.; Andersen, L.L.T.; et al. Vitamin D3 Supplementation in Overweight/Obese Pregnant Women: No Effects on the Maternal or Fetal Lipid Profile and Body Fat Distribution—A Secondary Analysis of the Multicentric, Randomized, Controlled Vitamin D and Lifestyle for Gestational Diabetes Prevention Trial (DALI). Nutrients 2022, 14, 3781. https://doi.org/10.3390/nu14183781
Harreiter J, Mendoza LC, Simmons D, Desoye G, Devlieger R, Galjaard S, Damm P, Mathiesen ER, Jensen DM, Andersen LLT, et al. Vitamin D3 Supplementation in Overweight/Obese Pregnant Women: No Effects on the Maternal or Fetal Lipid Profile and Body Fat Distribution—A Secondary Analysis of the Multicentric, Randomized, Controlled Vitamin D and Lifestyle for Gestational Diabetes Prevention Trial (DALI). Nutrients. 2022; 14(18):3781. https://doi.org/10.3390/nu14183781
Chicago/Turabian StyleHarreiter, Jürgen, Lilian C. Mendoza, David Simmons, Gernot Desoye, Roland Devlieger, Sander Galjaard, Peter Damm, Elisabeth R. Mathiesen, Dorte M. Jensen, Lise Lotte T. Andersen, and et al. 2022. "Vitamin D3 Supplementation in Overweight/Obese Pregnant Women: No Effects on the Maternal or Fetal Lipid Profile and Body Fat Distribution—A Secondary Analysis of the Multicentric, Randomized, Controlled Vitamin D and Lifestyle for Gestational Diabetes Prevention Trial (DALI)" Nutrients 14, no. 18: 3781. https://doi.org/10.3390/nu14183781
APA StyleHarreiter, J., Mendoza, L. C., Simmons, D., Desoye, G., Devlieger, R., Galjaard, S., Damm, P., Mathiesen, E. R., Jensen, D. M., Andersen, L. L. T., Dunne, F., Lapolla, A., Dalfra, M. G., Bertolotto, A., Wender-Ozegowska, E., Zawiejska, A., Hill, D., Jelsma, J. G. M., Snoek, F. J., ... on behalf of the DALI Core Investigator Group. (2022). Vitamin D3 Supplementation in Overweight/Obese Pregnant Women: No Effects on the Maternal or Fetal Lipid Profile and Body Fat Distribution—A Secondary Analysis of the Multicentric, Randomized, Controlled Vitamin D and Lifestyle for Gestational Diabetes Prevention Trial (DALI). Nutrients, 14(18), 3781. https://doi.org/10.3390/nu14183781












