Effectiveness of a Motivational Nutritional Intervention through Social Networks 2.0 to Increase Adherence to the Mediterranean Diet and Improve Lung Function in Active Smokers: The DIET Study, a Randomized, Controlled and Parallel Clinical Trial in Primary Care
Abstract
:1. Introduction
2. Materials and Methods
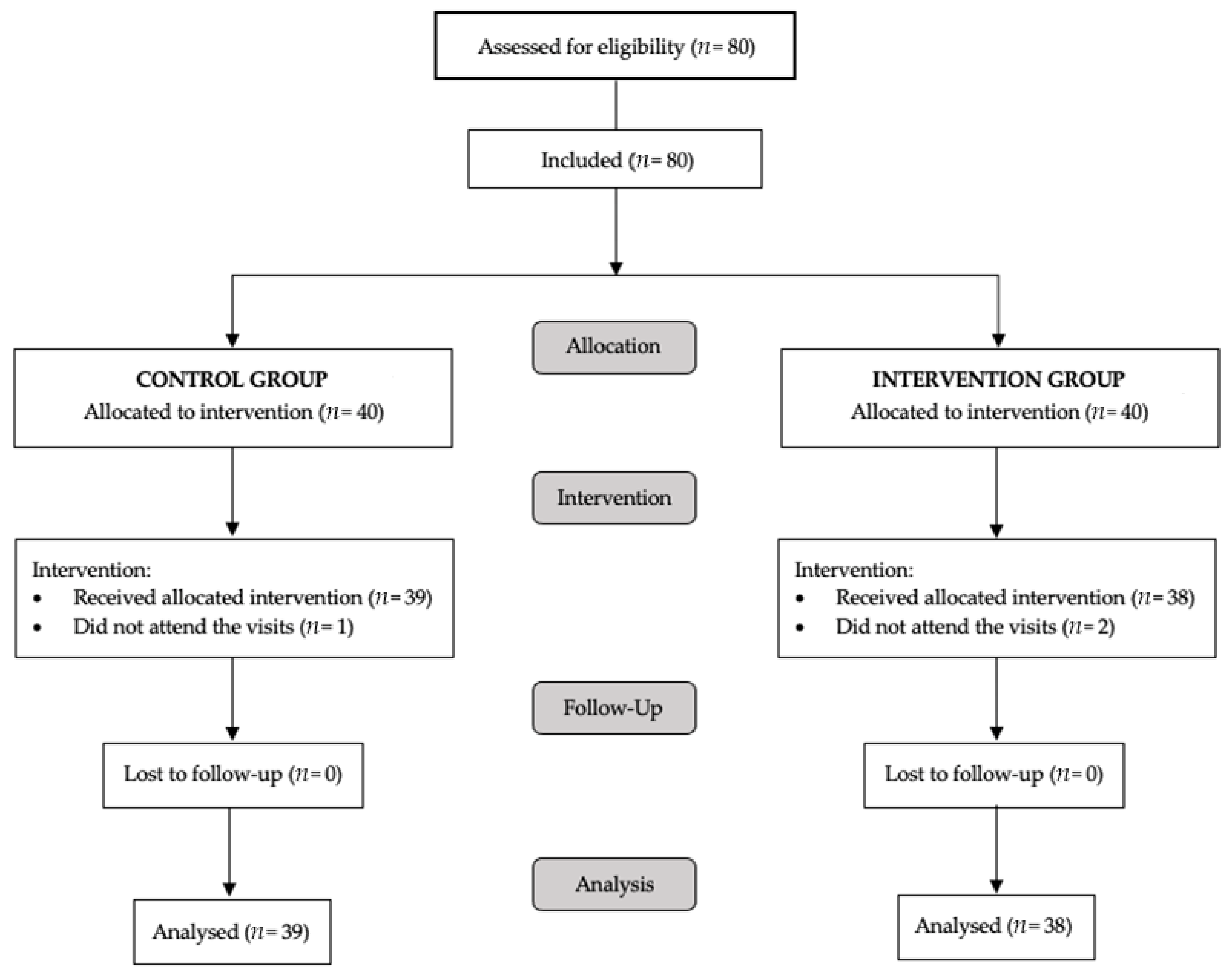
2.1. Study Design
2.2. Selection of Participants and Randomization
2.3. Procedures
2.4. Intervention Group
2.5. Control Group
2.6. Study Variables
2.7. Statistical Analyses
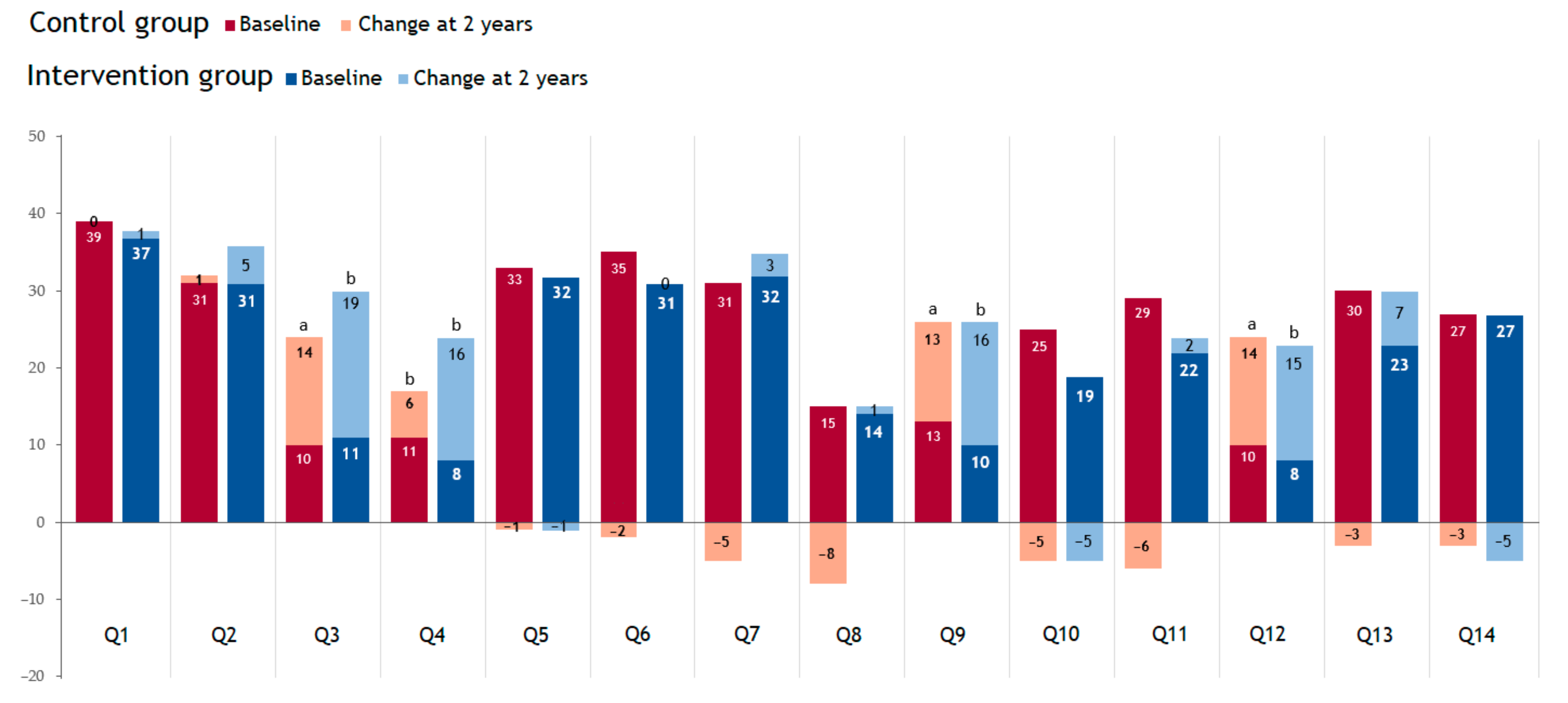
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Schulze, M.B.; Martínez-González, M.A.; Fung, T.T.; Lichtenstein, A.H.; Forouhi, N. Food based dietary patterns and chronic disease prevention. BMJ 2018, 361, k2396. [Google Scholar] [CrossRef] [Green Version]
- Berthon, B.S.; Wood, L.G. Nutrition and Respiratory Health—Feature Review. Nutrients 2015, 7, 1618–1643. [Google Scholar] [CrossRef] [PubMed]
- Rabe, K.F.; Watz, H. Chronic obstructive pulmonary disease. Lancet 2017, 389, 1931–1940. [Google Scholar] [CrossRef]
- Papassotiriou, I.; Islam, S.M.S. Adherence to Mediterranean Diet Is Associated With Lung Function in Older Adults: Data from the Health and Retirement Study. J. Am. Coll. Nutr. 2021, 40, 119–124. [Google Scholar] [CrossRef] [PubMed]
- Bach-Faig, A.; Geleva, D.; Carrasco, J.; Ribas-Barba, L.; Serra-Majem, L. Evaluating associations between Mediterranean diet adherence indexes and biomarkers of diet and disease. Public Health Nutr. 2006, 9, 1110–1117. [Google Scholar] [CrossRef]
- Ochs-Balcom, H.M.; Grant, B.J.B.; Muti, P.; Sempos, C.T.; Freudenheim, J.L.; Browne, R.W.; McCann, S.E.; Trevisan, M.; Cassano, P.A.; Iacoviello, L.; et al. Antioxidants, oxidative stress, and pulmonary func-tion in individuals diagnosed with asthma or COPD. Eur. J. Clin. Nutr. 2006, 60, 991–999. [Google Scholar] [CrossRef]
- Hanson, C.; Lyden, E.; Furtado, J.; Campos, H.; Sparrow, D.; Vokonas, P.; Litonjua, A.A. Serum tocopherol levels and vitamin E intake are associated with lung function in the normative aging study. Clin. Nutr. 2016, 35, 169–174. [Google Scholar] [CrossRef] [Green Version]
- Sharma, G.; Goodwin, J. Effect of aging on respiratory system physiology and immunology. Clin. Interv. Aging 2006, 1, 253–260. [Google Scholar] [CrossRef]
- Kaluza, J.; Larsson, S.; Orsini, N.; Linden, A.; Wolk, A. Fruit and vegetable consumption and risk of COPD: A prospective cohort study of men. Thorax 2017, 72, 500–509. [Google Scholar] [CrossRef]
- Whyand, T.; Hurst, J.R.; Beckles, M.; Caplin, M.E. Pollution and respiratory disease: Can diet or supplements help? A review. Respir. Res. 2018, 19, 79. [Google Scholar] [CrossRef] [Green Version]
- Zhai, T.; Li, S.; Hu, W.; Li, D.; Leng, S. Potential Micronutrients and Phytochemicals against the Pathogenesis of Chronic Obstructive Pulmonary Disease and Lung Cancer. Nutrients 2018, 10, 813. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dreher, M.L. Whole Fruits and Fruit Fiber Emerging Health Effects. Nutrients 2018, 10, 1833. [Google Scholar] [CrossRef] [Green Version]
- Pounis, G.; Arcari, A.; Costanzo, S.; Di Castelnuovo, A.; Bonaccio, M.; Persichillo, M.; Donati, M.B.; de Gaetano, G.; Iacoviello, L. Favorable association of polyphenol-rich diets with lung function: Cross-sectional findings from the Moli-sani study. Respir. Med. 2018, 136, 48–57. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Atlantis, E.; Cochrane, B. The association of dietary intake and supplementation of specific polyunsaturated fatty acids with inflammation and functional capacity in chronic obstructive pulmonary disease: A systematic review. Int. J. Evid. Based Healthc. 2016, 14, 53–63. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fulton, A.S.; Hill, A.M.; Williams, M.T.; Howe, P.R.; Coates, A.M. Paucity of evidence for a relationship between long-chain omega-3 fatty acid intake and chronic obstructive pulmonary disease: A systematic review. Nutr. Rev. 2015, 73, 612–623. [Google Scholar] [CrossRef]
- Cornell, K.; Alam, M.; Lyden, E.; Wood, L.; LeVan, T.D.; Nordgren, T.M.; Bailey, K.; Hanson, C. Saturated Fat Intake Is Associated with Lung Function in Individuals with Airflow Obstruction: Results from NHANES 2007–2012. Nutrients 2019, 11, 317. [Google Scholar] [CrossRef] [Green Version]
- Johnson, I. The cancer risk related to meat and meat products. Br. Med Bull. 2017, 121, 73–81. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kaluza, J.; Larsson, S.; Linden, A.; Wolk, A. Consumption of Unprocessed and Processed Red Meat and the Risk of Chronic Obstructive Pulmonary Disease: A Prospective Cohort Study of Men. Am. J. Epidemiol. 2016, 184, 829–836. [Google Scholar] [CrossRef]
- Kaluza, J.; Harris, H.; Linden, A.; Wolk, A. Long-term unprocessed and processed red meat consumption and risk of chronic obstructive pulmonary disease: A prospective cohort study of women. Eur. J. Nutr. 2019, 58, 665–672. [Google Scholar] [CrossRef] [Green Version]
- Salari-Moghaddam, A.; Milajerdi, A.; Larijani, B.; Esmaillzadeh, A. Processed red meat intake and risk of COPD: A systematic review and dose-response meta-analysis of prospective cohort studies. Clin. Nutr. 2019, 38, 1109–1116. [Google Scholar] [CrossRef]
- Arvers, P. Alcool et poumon: Des liaisons dangereuses [Alcohol consumption and lung damage: Dangerous relationships]. Rev. Mal. Respir. 2018, 35, 1039–1049. [Google Scholar] [CrossRef] [PubMed]
- Yeligar, S.M.; Chen, M.M.; Kovacs, E.J.; Sisson, J.H.; Burnham, E.L.; Brown, L.A.S. Alcohol and lung injury and immunity. Alcohol 2016, 55, 51–59. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mehta, A.J.; Guidot, D.M. Alcohol and the Lung. Alcohol Res. 2017, 38, 243–254. [Google Scholar] [PubMed]
- Traphagen, N.; Tian, Z.; Allengipson, D.S. Chronic Ethanol Exposure: Pathogenesis of Pulmonary Disease and Dysfunction. Biomolecules 2015, 5, 2840–2853. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sorli-Aguilar, M.; Martin-Lujan, F.; Flores-Mateo, G.; Arija-Val, V.; Basora-Gallisa, J.; Sola-Alberich, R.; RESET Study Group Investigators. Dietary patterns are associated with lung function among Spanish smokers without respiratory disease. BMC Pulm. Med. 2016, 16, 162. [Google Scholar] [CrossRef] [Green Version]
- Sorli-Aguilar, M.; Martin-Lujan, F.; Santigosa-Ayala, A.; Piñol-Moreso, J.L.; Flores-Mateo, G.; Basora-Gallisá, J.; Arija-Val, V.; Solà-Alberich, R. Effects of Mediterranean diet on lung function in smokers: A randomised, parallel and controlled protocol. BMC Public Health 2015, 15, 74. [Google Scholar] [CrossRef] [Green Version]
- Chen, Y.; Perez-Cueto, F.; Giboreau, A.; Mavridis, I.; Hartwell, H. The Promotion of Eating Behaviour Change through Digital Interventions. Int. J. Environ. Res. Public Health 2020, 17, 7488. [Google Scholar] [CrossRef]
- Miller, M.R.; Hankinson, J.; Brusasco, V.; Burgos, F.; Casaburi, R.; Coates, A.; Crapo, R.; Enright, P.; Van Der Grinten, C.P.M.; Gustafsson, P.; et al. Standardisation of spirometry. Eur. Respir. J. 2005, 26, 319–338. [Google Scholar] [CrossRef] [Green Version]
- Schröder, H.; Fitó, M.; Estruch, R.; Martínez-González, M.A.; Corella, D.; Salas-Salvadó, J.; Lamuela-Raventós, R.; Ros, E.; Salaverría, I.; Fiol, M.; et al. A Short Screener Is Valid for Assessing Mediterranean Diet Adherence among Older Spanish Men and Women. J. Nutr. 2011, 141, 1140–1145. [Google Scholar] [CrossRef] [Green Version]
- Trinidad, I.; Fernandez, J.; Cucó, G.; Biarnés, E.; Arija, V. Validation of a short questionnaire on frequency of dietary intake: Re-producibility and validity. Nutr Hosp. 2008, 23, 242–252. [Google Scholar]
- Elosua, R.; Marrugat, J.; Molina, L.; Pons, S.; Pujol, E. Validation of the Minnesota leisure time physical activity questionnaire in spanish men. The MARATHOM investigators. Am. J. Epidemiol. 1994, 139, 1197–1209. [Google Scholar] [CrossRef]
- Román Viñas, B.; Ribas Barba, L.; Ngo, J.; Serra Majem, L. Validity of the international physical activity questionnaire in the Catalan population (Spain). Gac. Sanit. 2013, 27, 254–257. [Google Scholar] [CrossRef] [Green Version]
- Bach-Faig, A.; Berry, E.M.; Lairon, D.; Reguant, J.; Trichopoulou, A.; Dernini, S.; Medina, F.X.; Battino, M.; Belahsen, R.; Miranda, G.; et al. Mediterranean Diet Foundation Expert Group. Mediterranean diet pyramid today. Science and cultural updates. Public Health Nutr. 2011, 14, 2274–2284. [Google Scholar] [CrossRef] [Green Version]
- Estruch, R.; Ros, E.; Salas-Salvadó, J.; Covas, M.-I.; Corella, D.; Arós, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V.; Fiol, M.; Lapetra, J.; et al. Primary Prevention of Cardiovascular Disease with a Mediterranean Diet. N. Engl. J. Med. 2013, 368, 1279–1290. [Google Scholar] [CrossRef] [Green Version]
- Graham, B.L.; Steenbruggen, I.; Miller, M.R.; Barjaktarevic, I.Z.; Cooper, B.G.; Hall, G.L.; Hallstrand, T.S.; Kaminsky, D.A.; McCarthy, K.; McCormack, M.C.; et al. Standardization of Spirometry 2019 Update. An Official American Thoracic Society and European Respiratory Society Technical Statement. Am. J. Respir. Crit. Care Med. 2019, 200, e70–e88. [Google Scholar] [CrossRef]
- Campbell, M.; Grimshaw, J.; Steen, N. Sample size calculations for cluster randomised trials. Changing Professional Practice in Europe Group (EU BIOMED II Concerted Action). J. Health Serv. Res. Policy 2000, 5, 12–16. [Google Scholar] [CrossRef] [PubMed]
- Lee, P.N.; Fry, J.S. Systematic review of the evidence relating FEV1decline to giving up smoking. BMC Med. 2010, 8, 84. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scoditti, E.; Massaro, M.; Garbarino, S.; Toraldo, D.M. Role of Diet in Chronic Obstructive Pulmonary Disease Prevention and Treatment. Nutrients 2019, 11, 1357. [Google Scholar] [CrossRef] [Green Version]
- Olson, C.M. Behavioral Nutrition Interventions Using e- and m-Health Communication Technologies: A Narrative Review. Annu. Rev. Nutr. 2016, 36, 647–664. [Google Scholar] [CrossRef] [PubMed]
- Hamulka, J.; Wadolowska, L.; Hoffmann, M.; Kowalkowska, J.; Gutkowska, K. Effect of an Education Program on Nutrition Knowledge, Attitudes toward Nutrition, Diet Quality, Lifestyle, and Body Composition in Polish Teenagers. The ABC of Healthy Eating Project: Design, Protocol, and Methodology. Nutrients 2018, 10, 1439. [Google Scholar] [CrossRef] [Green Version]
- Dinu, M.; Pagliai, G.; Casini, A.; Sofi, F. Mediterranean diet and multiple health outcomes: An umbrella review of meta-analyses of observational studies and randomised trials. Eur. J. Clin. Nutr. 2018, 72, 30–43. [Google Scholar] [CrossRef] [PubMed]
- Livingstone, K.M.; Celis-Morales, C.; Navas-Carretero, S.; San-Cristobal, R.; Macready, A.L.; Fallaize, R.; Forster, H.; Woolhead, C.; O’Donovan, C.B.; Marsaux, C.F.; et al. Food4Me Study. Effect of an Internet-based, personalized nutrition randomized trial on dietary changes associated with the Mediterranean diet: The Food4Me Study. Am. J. Clin. Nutr. 2016, 104, 288–297. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jahangiry, L.; Montazeri, A.; Najafi, M.; Yaseri, M.; Farhangi, M.A. An interactive web-based intervention on nutritional status, physical activity and health-related quality of life in patient with metabolic syndrome: A randomized-controlled trial (The Red Ruby Study). Nutr. Diabetes 2017, 7, e240. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lisón, J.F.; Palomar, G.; Mensorio, M.S.; Baños, R.M.; Cebolla-Martí, A.; Botella, C.; Benavent-Caballer, V.; Rodilla, E. Impact of a Web-Based Exercise and Nutritional Education Intervention in Patients Who Are Obese With Hypertension: Randomized Wait-List Controlled Trial. J. Med. Internet Res. 2020, 22, e14196. [Google Scholar] [CrossRef]
- Sorgente, A.; Pietrabissa, G.; Manzoni, G.M.; Rethlefsen, M.; Simpson, S.; Perona, S.; Rossi, A.; Cattivelli, R.; Innamorati, M.; Jackson, J.B.; et al. Web-Based Interventions for Weight Loss or Weight Loss Maintenance in Overweight and Obese People: A Systematic Review of Systematic Reviews. J. Med. Internet Res. 2017, 19, e229. [Google Scholar] [CrossRef] [PubMed]
- Watson, S.; Woodside, J.V.; Ware, L.J.; Hunter, S.J.; McGrath, A.; Cardwell, C.R.; Appleton, K.M.; Young, I.S.; McKinley, M.C. Effect of a Web-Based Behavior Change Program on Weight Loss and Cardiovascular Risk Factors in Overweight and Obese Adults at High Risk of Developing Cardiovascular Disease: Randomized Controlled Trial. J. Med. Internet Res. 2015, 17, e177. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Z.; Monro, J.; Venn, B.J. Development and Evaluation of an Internet-Based Diabetes Nutrition Education Resource. Nutrients 2019, 11, 1217. [Google Scholar] [CrossRef] [Green Version]
- Esposito, K.; Maiorino, M.I.; Bellastella, G.; Chiodini, P.; Panagiotakos, D.B.; Giugliano, D. A journey into a Mediterranean diet and type 2 diabetes: A systematic review with meta-analyses. BMJ Open 2015, 5, e008222. [Google Scholar] [CrossRef] [Green Version]
- Yu, Q.; Xu, L.; Li, L.; Zhi, M.; Gu, Y.; Wang, X.; Guo, H.; Li, Y.; Fan, Y.; Yang, B.; et al. Internet and WeChat used by patients with Crohn’s disease in China: A multi-center questionnaire survey. BMC Gastroenterol. 2019, 19, 97. [Google Scholar] [CrossRef] [Green Version]
- Long, M.D.; Kappelman, M.D.; Martin, C.F.; Lewis, J.D.; Mayer, L.; Kinneer, P.M.; Sandler, R.S. Development of an internet-based cohort of patients with inflammatory bowel diseases (CCFA Partners): Methodology and initial results. Inflamm. Bowel Dis. 2012, 18, 2099–2106. [Google Scholar] [CrossRef]
- Singh, D.; Agusti, A.; Anzueto, A.; Barnes, P.J.; Bourbeau, J.; Celli, B.R.; Criner, G.J.; Frith, P.; Halpin, D.M.G.; Han, M.; et al. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease: The GOLD science committee report 2019. Eur. Respir. J. 2019, 53, 1900164. [Google Scholar] [CrossRef] [PubMed]
- Yazdanpanah, L.; Paknahad, Z.; Moosavi, A.J.; Maracy, M.R.; Zaker, M.M. The relationship between different diet quality indices and severity of airflow obstruction among COPD patients. Med. J. Islam. Repub. Iran 2016, 30, 380. [Google Scholar] [PubMed]
- Rennard, S.I.; Drummond, M.B. Early chronic obstructive pulmonary disease: Definition, assessment, and prevention. Lancet 2015, 385, 1778–1788. [Google Scholar] [CrossRef] [Green Version]
- Verduci, E.; Martelli, A.; Miniello, V.; Landi, M.; Mariani, B.; Brambilla, M.; Diaferio, L.; Peroni, D. Nutrition in the first 1000 days and respiratory health: A descriptive review of the last five years’ literature. Allergol. Immunopathol. 2017, 45, 405–413. [Google Scholar] [CrossRef] [PubMed]
- Joo, J.; Williamson, S.A.; I Vazquez, A.; Fernandez, J.R.; Bray, M.S. Advanced Dietary Patterns Analysis Using Sparse Latent Factor Models in Young Adults. J. Nutr. 2018, 148, 1984–1992. [Google Scholar] [CrossRef] [PubMed]
- Hinnig, P.D.F.; Monteiro, J.S.; De Assis, M.A.A.; Levy, R.B.; Peres, M.A.; Perazi, F.M.; Porporatti, A.L.; Canto, G.D.L. Dietary Patterns of Children and Adolescents from High, Medium and Low Human Development Countries and Associated Socioeconomic Factors: A Systematic Review. Nutrients 2018, 10, 436. [Google Scholar] [CrossRef] [Green Version]
- Burggraf, C.; Teuber, R.; Brosig, S.; Meier, T. Review of a priori dietary quality indices in relation to their construction criteria. Nutr. Rev. 2018, 76, 747–764. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hlaing-Hlaing, H.; Pezdirc, K.; Tavener, M.; James, E.L.; Hure, A. Diet Quality Indices Used in Australian and New Zealand Adults: A Systematic Review and Critical Appraisal. Nutrients 2020, 12, 3777. [Google Scholar] [CrossRef]
- Asghari, G.; Mirmiran, P.; Yuzbashian, E.; Azizi, F. A systematic review of diet quality indices in relation to obesity. Br. J. Nutr. 2017, 117, 1055–1065. [Google Scholar] [CrossRef] [Green Version]
- Zheng, P.-F.; Shu, L.; Si, C.-J.; Zhang, X.-Y.; Yu, X.-L.; Gao, W. Dietary Patterns and Chronic Obstructive Pulmonary Disease: A Meta-analysis. COPD 2016, 13, 515–522. [Google Scholar] [CrossRef]
- Saussereau, J.; Guillien, A.; Soumagne, T.; Laplante, J.-J.; Laurent, L.; Bouhaddi, M.; Rocchi, S.; Annesi-Maesano, I.; Roche, N.; Dalphin, J.-C.; et al. Dietary Patterns and Prevalence of Post-bronchodilator Airway Obstruction in Dairy Farmers Exposed to Organic Dusts. COPD 2019, 16, 118–125. [Google Scholar] [CrossRef]
- Steinemann, N.; Grize, L.; Pons, M.; Rothe, T.; Stolz, D.; Turk, A.; Schindler, C.; Brombach, C.; Probst-Hensch, N. Associations between Dietary Patterns and Post-Bronchodilation Lung Function in the SAPALDIA Cohort. Respiration 2018, 95, 454–463. [Google Scholar] [CrossRef]
- Fischer, A.; Johansson, I.; Blomberg, A.; Sundström, B. Adherence to a Mediterranean-like Diet as a Protective Factor Against COPD: A Nested Case-Control Study. COPD 2019, 16, 272–277. [Google Scholar] [CrossRef] [Green Version]
- Schwingshackl, L.; Schwedhelm, C.; Hoffmann, G.; Lampousi, A.-M.; Knüppel, S.; Iqbal, K.; Bechthold, A.; Schlesinger, S.; Boeing, H. Food groups and risk of all-cause mortality: A systematic review and meta-analysis of prospective studies. Am. J. Clin. Nutr. 2017, 105, 1462–1473. [Google Scholar] [CrossRef] [Green Version]
- GBD 2017 Diet Collaborators. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 393, 1958–1972. [Google Scholar] [CrossRef] [Green Version]
- Guilleminault, L.; Williams, E.J.; Scott, H.A.; Berthon, B.S.; Jensen, M.; Wood, L.G. Diet and Asthma: Is It Time to Adapt Our Message? Nutrients 2017, 9, 1227. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hosseini, B.; Berthon, B.S.; Wark, P.; Wood, L.G. Effects of Fruit and Vegetable Consumption on Risk of Asthma, Wheezing and Immune Responses: A Systematic Review and Meta-Analysis. Nutrients 2017, 9, 341. [Google Scholar] [CrossRef] [PubMed]
- Hosseini, B.; Berthon, B.S.; Saedisomeolia, A.; Starkey, M.R.; Collison, A.; Wark, P.A.B.; Wood, L.G. Effects of fruit and vegetable consumption on inflammatory biomarkers and immune cell populations: A systematic literature review and meta-analysis. Am. J. Clin. Nutr. 2018, 108, 136–155. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arigliani, M.; Spinelli, A.M.; Liguoro, I.; Cogo, P. Nutrition and Lung Growth. Nutrients 2018, 10, 919. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wypych, T.; Marsland, B.J.; Ubags, N.D.J. The Impact of Diet on Immunity and Respiratory Diseases. Ann. Am. Thorac. Soc. 2017, 14 (Suppl. 5), S339–S347. [Google Scholar] [CrossRef]
- Ministry of Health Government of Spain. Statistical Portal: Primary Care Information System (SIAP). Available online: https://pestadistico.inteligenciadegestion.mscbs.es/publicoSNS/S/sistema-de-informacion-de-atencion-primaria-siap (accessed on 30 September 2021).
- Martín-Luján, F.; Catalin, R.-E.; Salamanca-González, P.; Sorlí-Aguilar, M.; Santigosa-Ayala, A.; Valls-Zamora, R.M.; Martín-Vergara, N.; Canela-Armengol, T.; Arija-Val, V.; Solà-Alberich, R. A clinical trial to evaluate the effect of the Mediterranean diet on smokers lung function. NPJ Prim. Care Respir. Med. 2019, 29, 40. [Google Scholar] [CrossRef] [PubMed]
| Baseline | Change at 2 Years | |||
|---|---|---|---|---|
| Control Group | Intervention Group | Control Group | Intervention Group | |
| (n = 39) | (n = 38) | (n = 39) | (n = 38) | |
| Health habits | ||||
| Physical activity, hours/week | 6.50 [3.12;11.6] | 5.25 [2.36;11.0] | 0.82 (6.35) | 2.09 (5.48) |
| Current smoking (%) | 100 | 100 | 2 (5.13) | 5 (13.2) |
| Current consumption, cigarettes/day | 15.0 (10.0; 20.0) | 12.0 (10.0; 20.0) | 0.00 [0.00; 0.00] | 0.00 [0.00; 0.00] |
| Mediterranean Diet Adherence Score (MEDAS) b | 8.6 (2,9) | 7.9 (1,6) | 0.69 (2.14) | 2.05 (2.03) |
| Anthropometrics variables | ||||
| Height, cm a | 158 (7.7) | 163 (10.1) | - | - |
| Weight, kg | 68.2 (12.2) | 71.4 (15.1) | −1.69(6.18) | 1.98(4.89) |
| BMI, kg/m | 27.2 (4.5) | 26.9 (5.01) | −0.80 (2.22) | −0.93 (1.78) |
| Waist circumference, cm | 87.2 (10.5) | 88.3 (12.0) | −0.79 (8.46) | −3.66 (6.64) |
| Clinical variables | ||||
| SBP, mmHg | 129 (26.7) | 128 (14.5) | 0.18 (24.2) | −0.03 (16.4) |
| DBP, mmHg a | 80.0 (7.5) | 75.4 (8.6) | −0.39 (6.83) | 3.08 (11.5) |
| Biochemical variables | ||||
| Total Cholesterol, mg/dL b | 209 (49.20) | 197 (35.10) | 0.65 [−35.13; 15.5] | −8.85 [−15.08; 14.7] |
| HDL—Cholesterol mg/dL | 61.1 (19.4) | 55.2 (15.0) | 1.05 [−5.47; 8.98] | 2.80 [−4.20; 7.00] |
| LDL—Cholesterol, mg/dL b | 131 (36.6) | 116 (34.1) | −5.51 [−40.92; 8.12] | −10.37 [−20.07; 3.92] |
| Triglycerides, mg/dL | 129 (64.3) | 132 (91.9) | 3.00 [−7.00; 28.0] | −9.50 [−37.50; 51.0] |
| Glucose, mg/dL | 90.8 (23.0) | 98.8 (33.1) | 2.00 [−1.00; 13.0] | −1.00 [−8.00; 12.0] |
| Pulmonary function variables | ||||
| FVC, mL | 3340 (850) | 3590 (1000) | −120 [−180; −50] | −70 [−320; 10] |
| FVC, (%) | 97.7 (16.2) | 93.3 (16.5) | 0.00 [−2.50; 0.00] | 0.00 [−6.00; 1.00] |
| FEV1, mL/min | 2630 (600) | 2820 (890) | −140 [−210; −50] | −90 [−210; 10] |
| FEV1, (%) | 103 (16.4) | 95.7 (19.0) | 0.00 [−7.00; 0.00] | 0.00 [−4.00; 1.00] |
| FEV1/FVC ratio, (%) | 79.3 (6.26) | 78. (6.42) | −0.68 [−1.15; −0.25] | −0.55 [−0.84; −0.16] |
| Baseline | Change at 2 Years | |||
|---|---|---|---|---|
| Control Group | Intervention Group | Control Group | Intervention Group | |
| (n = 39) | (n = 38) | (n = 39) | (n = 38) | |
| Cereals, nuts and legumes | ||||
| Legumes (g/day) | 10.0 [10.0; 20.0] | 10.0 [10.0; 20.0] | 10.0 [0.00; 20.0] | 10.0 [0.00; 20.0] |
| Nuts (g/day) | 4.29 [0.00; 10.7] | 4.29 [0.00; 12.9] | 0.00 [0.00; 12.9] | 12.9 [0.00; 19.6] |
| Cereals (g/day) | 163 (62.6) | 181 (63.4) | −0.72 (63.0) | −13.29 (70.1) |
| Fruits and vegetables | ||||
| Vegetable (g/day) | 194 (119) | 152 (68.2) | 21.4 [0.00; 72.9] | 55.0 [14.3; 103] |
| Fruits (g/day) a,b | 300 [150; 300] | 136 [66.1; 236] | 12.7 (167) | 121 (178) |
| Milk and dairy products | ||||
| Dairy products (g/day) | 261 [225; 475] | 282 [226; 475] | 35.7 [0.00; 135] | 36.8 [0.00; 177] |
| Meat, fish and eggs | ||||
| White meat (g/day) | 32.9 [16.4; 49.3] | 32.9 [16.4; 49.3] | 0.00 [0.00; 8.21] | 0.00 [−16.43; 0.00] |
| Red meat (g/day) | 20.7 [17.5; 35.0] | 31.4 [20.7; 43.0] | 0.00 [−6.43; 2.14] | 0.00 [−13.75; 5.89] |
| Processed meat (g/day) | 16.4 [6.34; 20.7] | 18.6 [15.0; 22.3] | 4.29 [−5.00; 18.6] | 1.07 [−7.50; 9.55] |
| White fish (g/day) | 38.6 [19.3; 38.6] | 38.6 [38.6; 38.6] | 0.00 [0.00; 0.00] | 0.00 [0.00; 0.00] |
| Blue fish (g/day) | 38.6 [19.3; 38.6] | 38.6 [19.3; 38.6] | 0.00 [0.00; 0.00] | 0.00 [0.00; 0.00] |
| Shellfish (g/day) | 4.82 [0.00; 19.3] | 19.3 [1.21; 19.3] | 0.00 [0.00; 19.3] | 0.00 [0.00; 19.3] |
| Eggs (g/day) | 25.7 [12.9; 38.6] | 25.7 [12.9; 25.7] | 12.9 [0.00; 12.9] | 12.9 [0.00; 12.9] |
| Processed products | 15.7 [5.71; 21.4] | 15.7 [10.0; 21.1] | 1.43 [−6.96; 15.2] | 0.00 [−9.64; 9.29] |
| Pastries products | 24.3 [14.6; 41.2] | 30.0 [12.9; 83.9] | −4.29 [−14.82; 4.55] | −4.64 [−41.92; 7.14] |
| Carbonated drinks | ||||
| Sugary and light drinks (mL/day) | 0.00 [0.00; 157] | 28.6 [0.00; 78.6] | 0.00 [0.00; 0.00] | 0.00 [−28.57; 0.00] |
| Alcohol drinks | ||||
| Wine (mL/day) | 28.6 [0.00; 100] | 14.3 [0.00; 71.4] | 0.00 [0.00; 14.3] | 0.00 [−14.29; 0.00] |
| Fermented drinks (mL/day) | 28.6 [0.00; 100] | 14.3 [0.00; 67.9] | 0.00 [0.00; 14.3] | 0.00 [−14.29; 0.00] |
| Unadjusted | Age/Sex-Adjusted | Multivariable-Adjusted | ||||
|---|---|---|---|---|---|---|
| β (95% CI) | p-Value | β (95% CI) | p-Value | β (95% CI) | p-Value | |
| Mediterranean Diet Adherence 1 | 1.36 (0.35; 2.37) | 0.009 | 1.15 (0.05; 2.25) | 0.040 | 1.17 (0.02; 2.31) | 0.046 * |
| Pulmonary Function | ||||||
| FVC | 2.18 (−2.46; 6.84) | 0.352 | 1.65 (−3.40; 6.71) | 0.517 | 1.22 (−4.17; 6.61) | 0.652 |
| FEV1 | 2.70 (−1.56; 6.95) | 0.211 | 2.24 (−2.36; 6.85) | 0.335 | 1.93 (−3.00; 6.86) | 0.437 |
| Ratio FVC/FEV1 | −0,09 (−2.66; 2.48) | 0.944 | 0.08 (−2,70; 2.87) | 0.953 | 0.52 (−2.48; 3.52) | 0.730 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Salamanca-González, P.; Valls-Zamora, R.M.; Pedret-Figuerola, A.; Sorlí-Aguilar, M.; Santigosa-Ayala, A.; Catalin, R.-E.; Pallejà-Millán, M.; Solà-Alberich, R.; Martin-Lujan, F.; the CENIT Research Group Investigators. Effectiveness of a Motivational Nutritional Intervention through Social Networks 2.0 to Increase Adherence to the Mediterranean Diet and Improve Lung Function in Active Smokers: The DIET Study, a Randomized, Controlled and Parallel Clinical Trial in Primary Care. Nutrients 2021, 13, 3597. https://doi.org/10.3390/nu13103597
Salamanca-González P, Valls-Zamora RM, Pedret-Figuerola A, Sorlí-Aguilar M, Santigosa-Ayala A, Catalin R-E, Pallejà-Millán M, Solà-Alberich R, Martin-Lujan F, the CENIT Research Group Investigators. Effectiveness of a Motivational Nutritional Intervention through Social Networks 2.0 to Increase Adherence to the Mediterranean Diet and Improve Lung Function in Active Smokers: The DIET Study, a Randomized, Controlled and Parallel Clinical Trial in Primary Care. Nutrients. 2021; 13(10):3597. https://doi.org/10.3390/nu13103597
Chicago/Turabian StyleSalamanca-González, Patricia, Rosa Maria Valls-Zamora, Anna Pedret-Figuerola, Mar Sorlí-Aguilar, Antoni Santigosa-Ayala, Roxana-Elena Catalin, Meritxell Pallejà-Millán, Rosa Solà-Alberich, Francisco Martin-Lujan, and the CENIT Research Group Investigators. 2021. "Effectiveness of a Motivational Nutritional Intervention through Social Networks 2.0 to Increase Adherence to the Mediterranean Diet and Improve Lung Function in Active Smokers: The DIET Study, a Randomized, Controlled and Parallel Clinical Trial in Primary Care" Nutrients 13, no. 10: 3597. https://doi.org/10.3390/nu13103597
APA StyleSalamanca-González, P., Valls-Zamora, R. M., Pedret-Figuerola, A., Sorlí-Aguilar, M., Santigosa-Ayala, A., Catalin, R.-E., Pallejà-Millán, M., Solà-Alberich, R., Martin-Lujan, F., & the CENIT Research Group Investigators. (2021). Effectiveness of a Motivational Nutritional Intervention through Social Networks 2.0 to Increase Adherence to the Mediterranean Diet and Improve Lung Function in Active Smokers: The DIET Study, a Randomized, Controlled and Parallel Clinical Trial in Primary Care. Nutrients, 13(10), 3597. https://doi.org/10.3390/nu13103597






