‘Joining the Dots’: Individual, Sociocultural and Environmental Links between Alcohol Consumption, Dietary Intake and Body Weight—A Narrative Review
Abstract
1. Introduction
2. Materials and Methods
3. Results
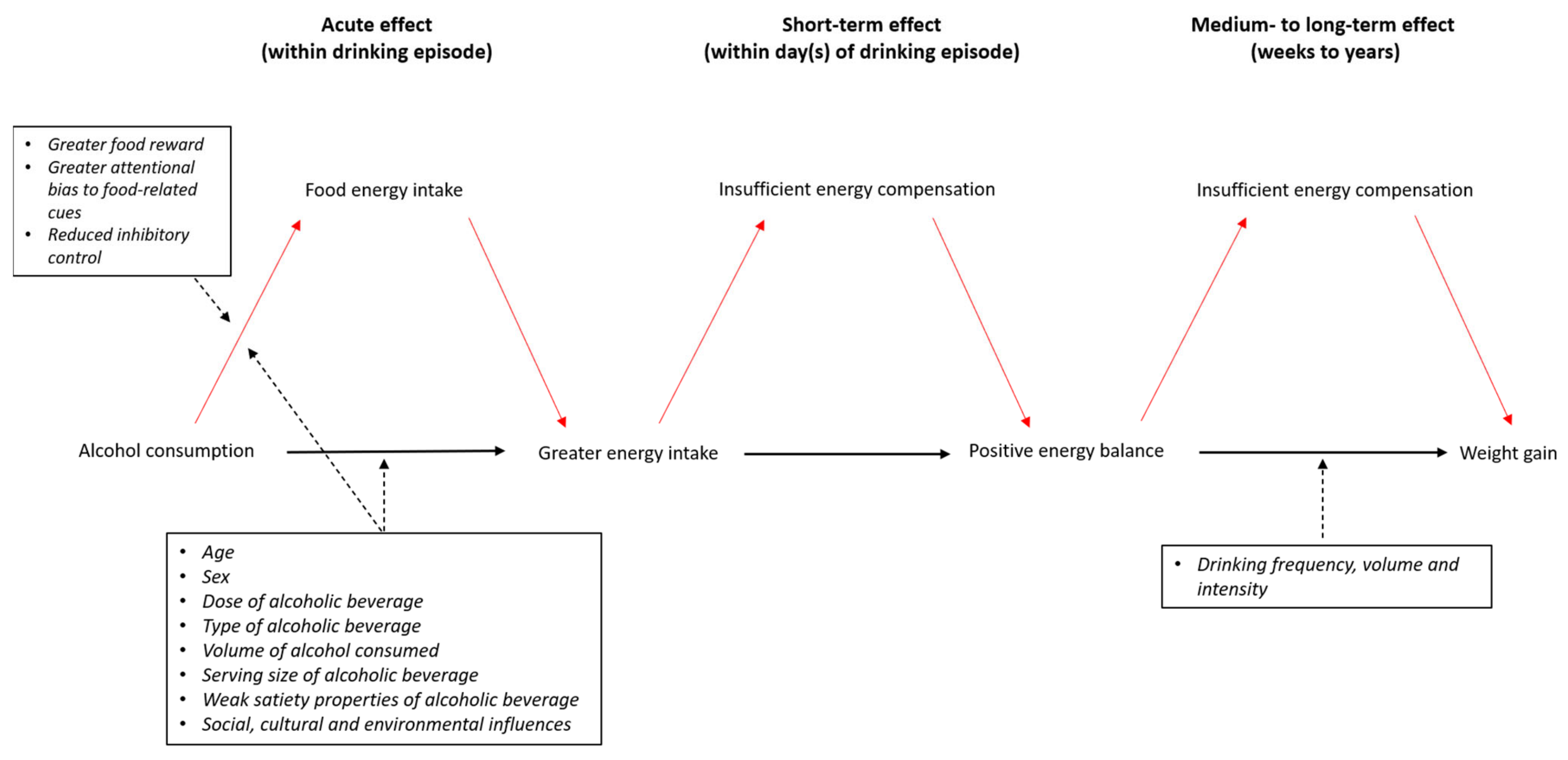
3.1. Alcohol and Dietary Intake
3.2. Alcohol and Body Weight
3.3. Alcohol and Weight Loss
3.4. Indiviudal-Level Mechanisms Linking Alcohol and Food Intake
3.4.1. Appetite, Hunger and Satiety
3.4.2. Inhibitory Control
3.4.3. Food-Related Reward and Attentional-Bias
3.5. Social, Cultural and Environmental Influences on Food and Alcohol Intake
3.5.1. The Interconnected Role of Food and Alcohol in Social and Cultural Life
3.5.2. Role of the Environment
3.5.3. The Role of Food and Alcohol Industries
4. Discussion
4.1. Appraising the Evidence
4.2. Strengths and Limitations
4.3. Policy and Practice Implications
4.4. Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organisation. Overweight and Obesity 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 2 April 2021).
- Office for National Statistics. Adult Drinking Habits in Great Britain 2018. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/drugusealcoholandsmoking/datasets/adultdrinkinghabits (accessed on 7 June 2021).
- Burgoine, T.; Forouhi, N.G.; Griffin, S.J.; Brage, S.; Wareham, N.J.; Monsivais, P. Does neighborhood fast-food outlet exposure amplify inequalities in diet and obesity? A cross-sectional study. Am. J. Clin. Nutr. 2016, 103, 1540–1547. [Google Scholar] [CrossRef] [PubMed]
- Katikireddi, S.V.; Whitley, E.; Lewsey, J.; Gray, L.; Leyland, A.H. Socioeconomic status as an effect modifier of alcohol consumption and harm: Analysis of linked cohort data. Lancet Public Health 2017, 2, e267–e276. [Google Scholar] [CrossRef]
- Dai, H.; Alsalhe, T.A.; Chalghaf, N.; Riccò, M.; Bragazzi, N.L.; Wu, J. The global burden of disease attributable to high body mass index in 195 countries and territories, 1990–2017: An analysis of the Global Burden of Disease Study. PLoS Med. 2020, 17, e1003198. [Google Scholar] [CrossRef]
- Boyd, J.; Bambra, C.; Purshouse, R.C.; Holmes, J. Beyond Behaviour: How Health Inequality Theory Can Enhance Our Under-standing of the ‘Alcohol-Harm Paradox’. Int. J. Environ. Res. Public Health 2021, 18, 6025. [Google Scholar] [CrossRef]
- Beard, E.; Brown, J.; West, R.; Angus, C.; Brennan, A.; Holmes, J.; Kaner, E.; Meier, P.; Michie, S. Deconstructing the Alcohol Harm Paradox: A Population Based Survey of Adults in England. PLoS ONE 2016, 11, e0160666. [Google Scholar] [CrossRef]
- Mourao, D.M.; Bressan, J.; Campbell, W.W.; Mattes, R.D. Effects of food form on appetite and energy intake in lean and obese young adults. Int. J. Obes. 2007, 31, 1688–1695. [Google Scholar] [CrossRef]
- Houchins, J.A.; Tan, S.Y.; Campbell, W.W.; Mattes, R.D. Effects of fruit and vegetable, consumed in solid vs beverage forms, on acute and chronic appetitive responses in lean and obese adults. Int. J. Obes. 2012, 37, 1109–1115. [Google Scholar] [CrossRef] [PubMed]
- Wiessing, K.R.; Xin, L.; Budgett, S.C.; Poppitt, S.D. No evidence of enhanced satiety following whey protein- or sucrose-enriched water beverages: A dose response trial in overweight women. Eur. J. Clin. Nutr. 2015, 69, 1238–1243. [Google Scholar] [CrossRef] [PubMed]
- Fong, M.; Li, A.; Hill, A.J.; Cunich, M.; Skilton, M.R.; Madigan, C.D.; Caterson, I.D. Modelling the Association between Core and Discretionary Energy Intake in Adults with and without Obesity. Nutrients 2019, 11, 683. [Google Scholar] [CrossRef]
- McKiernan, F.; Hollis, J.; Mattes, R. Short-term dietary compensation in free-living adults. Physiol. Behav. 2008, 93, 975–983. [Google Scholar] [CrossRef] [PubMed]
- Arif, A.A.; Rohrer, J.E. Patterns of alcohol drinking and its association with obesity: Data from the third national health and nutrition examination survey, 1988–1994. BMC Public Health 2005, 5, 126. [Google Scholar] [CrossRef]
- Public Health England. National Diet and Nutrition Survey (NDNS) from Years 1 to 9: Data Tables 201. Available online: https://www.gov.uk/government/statistics/ndns-time-trend-and-income-analyses-for-years-1-to-9 (accessed on 7 June 2021).
- Hill, J.O.; Wyatt, H.R.; Reed, G.W.; Peters, J.C. Obesity and the environment: Where do we go from here? Science 2003, 299, 853–855. [Google Scholar] [CrossRef] [PubMed]
- Sozio, M.; Crabb, D.W. Alcohol and lipid metabolism. Am. J. Physiol. Endocrinol. Metab. 2008, 295, E10–E16. [Google Scholar] [CrossRef]
- Yeomans, M.R. Alcohol, appetite and energy balance: Is alcohol intake a risk factor for obesity? Physiol. Behav. 2010, 100, 82–89. [Google Scholar] [CrossRef]
- Traversy, G.; Chaput, J.-P. Alcohol Consumption and Obesity: An Update. Curr. Obes. Rep. 2015, 4, 122–130. [Google Scholar] [CrossRef] [PubMed]
- Erol, A.; Karpyak, V.M. Sex and gender-related differences in alcohol use and its consequences: Contemporary knowledge and future research considerations. Drug Alcohol Depend. 2015, 156, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Wilsnack, R.W.; Wilsnack, S.C. Gender and Alcohol: Consumption and Consequences. Alcohol: Science, Policy, and Public Health; Oxford University Press: New York, NY, USA, 2013; pp. 153–160. [Google Scholar]
- Baraona, E.; Abittan, C.S.; Dohmen, K.; Moretti, M.; Pozzato, G.; Chayes, Z.W.; Schaefer, C.; Lieber, C.S. Gender differences in pharmacokinetics of alcohol. Alcohol Clin. Exp. Res. 2001, 25, 502–507. [Google Scholar] [CrossRef] [PubMed]
- Thomasson, H.R. Gender Differences in Alcohol Metabolism. In Recent Developments in Alcoholism; Springer: Boston, MA, USA, 2002; Volume 12. [Google Scholar]
- Fone, D.L.; Farewell, D.; White, J.; Lyons, R.A.; Dunstan, F.D. Socioeconomic patterning of excess alcohol consumption and binge drinking: A cross-sectional study of multilevel associations with neighbourhood deprivation. BMJ Open 2013, 3, e002337. [Google Scholar] [CrossRef] [PubMed]
- Beard, E.; Brown, J.; West, R.; Kaner, E.; Meier, P.; Michie, S. Associations between socio-economic factors and alcohol con-sumption: A population survey of adults in England. PLoS ONE 2019, 14, e0209442. [Google Scholar]
- Scott, S.; Shucksmith, J.; Baker, R.; Kaner, E. ‘Hidden Habitus’: A Qualitative Study of Socio-Ecological Influences on Drinking Practices and Social Identity in Mid-Adolescence. Int. J. Environ. Res. Public Health 2017, 14, 611. [Google Scholar] [CrossRef]
- Brierley-Jones, L.; Ling, J.; McCabe, K.E.; Wilson, G.B.; Crosland, A.; Kaner, E.F.; Haighton, C.A. Habitus of home and traditional drinking: A qualitative analysis of reported middle-class alcohol use. Soc. Health Illn. 2014, 36, 1054–1076. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Villegas, A.; Toledo, E.; Bes-Rastrollo, M.; Martín-Moreno, J.; Tortosa, A.; Martinez-Gonzalez, M.A. Association between dietary and beverage consumption patterns in the SUN (Seguimiento Universidad de Navarra) cohort study. Public Health Nutr. 2008, 12, 351–358. [Google Scholar] [CrossRef] [PubMed]
- Ruidavets, J.-B.; Bataille, V.; Dallongeville, J.; Simon, C.; Bingham, A.; Amouyel, P.; Arveiler, M.; Ducimetière, P.; Ferrières, J. Alcohol intake and diet in France, the prominent role of lifestyle. Eur. Heart J. 2004, 25, 1153–1162. [Google Scholar] [CrossRef]
- De Timary, P.; Cani, P.D.; Duchemin, J.; Neyrinck, A.M.; Gihousse, D.; Laterre, P.-F.; Badaoui, A.; Leclercq, S.; Delzenne, N.M.; Stärkel, P. The loss of metabolic control on alcohol drinking in heavy drinking alcohol-dependent subjects. PLoS ONE 2012, 7, e38682. [Google Scholar] [CrossRef]
- Ross, L.J.; Wilson, M.; Banks, M.; Rezannah, F.; Daglish, M. Prevalence of malnutrition and nutritional risk factors in patients undergoing alcohol and drug treatment. Nutrition 2012, 28, 738–743. [Google Scholar] [CrossRef] [PubMed]
- Kwok, A.; Dordevic, A.L.; Paton, G.; Page, M.J.; Truby, H. Effect of alcohol consumption on food energy intake: A systematic review and meta-analysis. Br. J. Nutr. 2019, 121, 481–495. [Google Scholar] [CrossRef]
- Grech, A.; Rangan, A.; Allman-Farinelli, M. Increases in Alcohol Intakes Are Concurrent with Higher Energy Intakes: Trends in Alcohol Consumption in Australian National Surveys from 1983, 1995 and 2012. Nutrients 2017, 9, 944. [Google Scholar] [CrossRef] [PubMed]
- Ebbeling, C.B.; Swain, J.F.; Feldman, H.A.; Wong, W.W.; Hachey, D.L.; Garcia-Lago, E.; Ludwig, D.S. Effects of Dietary Composition on Energy Expenditure During Weight-Loss Maintenance. JAMA 2012, 307, 2627–2634. [Google Scholar] [CrossRef] [PubMed]
- Cummings, J.R.; Gearhardt, A.N.; Ray, L.A.; Choi, A.K.; Tomiyama, A.J. Experimental and observational studies on alcohol use and dietary intake: A systematic review. Obes Rev. 2020, 21, e12950. [Google Scholar] [CrossRef] [PubMed]
- Parekh, N.; Lin, Y.; Chan, M.; Juul, F.; Makarem, N. Longitudinal dimensions of alcohol consumption and dietary intake in the Framingham Heart Study Offspring Cohort (1971–2008). Br. J. Nutr. 2020, 125, 685–694. [Google Scholar] [CrossRef] [PubMed]
- Beulens, J.W.; van Beers, R.M.; Stolk, R.P.; Schaafsma, G.; Hendriks, H.F. The effect of moderate alcohol consumption on fat dis-tribution and adipocytokines. Obesity 2006, 14, 60–66. [Google Scholar] [CrossRef]
- Cordain, L.; Bryan, E.D.; Melby, C.L.; Smith, M.J. Influence of moderate daily wine consumption on body weight regulation and metabolism in healthy free-living males. J. Am. Coll. Nutr. 1997, 16, 134–139. [Google Scholar] [CrossRef] [PubMed]
- Cordain, L.; Melby, C.L.; Hamamoto, A.E.; O’Neill, D.; Cornier, M.-A.; Barakat, H.A.; Israel, R.G.; Hill, J.O. Influence of moderate chronic wine consumption on insulin sensitivity and other correlates of syndrome X in moderately obese women. Metabolism 2000, 49, 1473–1478. [Google Scholar] [CrossRef] [PubMed]
- Sayon-Orea, C.; Martinez-Gonzalez, M.A.; Bes-Rastrollo, M. Alcohol consumption and body weight: A systematic review. Nutr. Rev. 2011, 69, 419–431. [Google Scholar] [CrossRef] [PubMed]
- Shelton, N.J.; Knott, C.S. Association Between Alcohol Calorie Intake and Overweight and Obesity in English Adults. Am. J. Public Health 2014, 104, 629–631. [Google Scholar] [CrossRef]
- Bendsen, N.T.; Christensen, R.; Bartels, E.M.; Kok, F.J.; Sierksma, A.; Raben, A.; Astrup, A. Is beer consumption related to measures of abdominal and general obesity? A systematic review and meta-analysis. Nutr. Rev. 2012, 71, 67–87. [Google Scholar] [CrossRef]
- Golzarand, M.; Salari-Moghaddam, A.; Mirmiran, P. Association between alcohol intake and overweight and obesity: A sys-tematic review and dose-response meta-analysis of 127 observational studies. Crit. Rev. Food Sci. Nutr. 2021, 1–21. [Google Scholar] [CrossRef]
- Guyatt, G.H.; Oxman, A.D.; Vist, G.E.; Kunz, R.; Falck-Ytter, Y.; Alonso-Coello, P.; Schünemann, H.J. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008, 336, 924–926. [Google Scholar] [CrossRef]
- Flechtner-Mors, M.; Biesalski, H.K.; Jenkinson, C.P.; Adler, G.; Ditschuneit, H.H. Effects of moderate consumption of white wine on weight loss in overweight and obese subjects. Int. J. Obes. 2004, 28, 1420–1426. [Google Scholar] [CrossRef]
- Carels, R.A.; Young, K.M.; Coit, C.; Clayton, A.M.; Spencer, A.; Wagner, M. Skipping meals and alcohol consumption: The regulation of energy intake and expenditure among weight loss participants. Appetite 2008, 51, 538–545. [Google Scholar] [CrossRef]
- Chao, A.M.; Wadden, T.A.; Tronieri, J.S.; Berkowitz, R.I. Alcohol Intake and Weight Loss During Intensive Lifestyle Intervention for Adults with Overweight or Obesity and Diabetes. Obesity 2018, 27, 30–40. [Google Scholar] [CrossRef]
- Kase, C.A.; Piers, A.D.; Schaumberg, K.; Forman, E.M.; Butryn, M.L. The relationship of alcohol use to weight loss in the context of behavioral weight loss treatment. Appetite 2016, 99, 105–111. [Google Scholar] [CrossRef]
- Eiler, W.J., 2nd; Džemidžić, M.; Case, K.R.; Soeurt, C.M.; Armstrong, C.L.; Mattes, R.D.; O’Connor, S.J.; Harezlak, J.; Acton, A.J.; Considine, R.V.; et al. The apéritif effect: Alcohol’s effects on the brain’s response to food aromas in women. Obesity 2015, 23, 1386–1393. [Google Scholar] [CrossRef]
- Koopmann, A.; Schuster, R.; Kiefer, F. The impact of the appetite-regulating, orexigenic peptide ghrelin on alcohol use disorders: A systematic review of preclinical and clinical data. Biol. Psychol. 2016, 131, 14–30. [Google Scholar] [CrossRef]
- Rose, A.; Hardman, C.; Christiansen, P. The effects of a priming dose of alcohol and drinking environment on snack food intake. Appetite 2015, 95, 341–348. [Google Scholar] [CrossRef] [PubMed]
- Mattes, R.D.; Campbell, W.W. Effects of Food Form and Timing of Ingestion on Appetite and Energy Intake in Lean Young Adults and in Young Adults with Obesity. J. Am. Diet Assoc. 2009, 109, 430–437. [Google Scholar] [CrossRef]
- Glasbrenner, B.; Pieramico, O.; Brecht-Krau, D.; Baur, M.; Malfertheiner, P. Gastric emptying of solids and liquids in obesity. J. Mol. Med. 1993, 71. [Google Scholar] [CrossRef]
- Hoad, C.; Rayment, P.; Spiller, R.C.; Marciani, L.; Alonso, B.D.C.; Traynor, C.; Mela, D.; Peters, H.P.F.; Gowland, P.A. In Vivo Imaging of Intragastric Gelation and Its Effect on Satiety in Humans. J. Nutr. 2004, 134, 2293–2300. [Google Scholar] [CrossRef] [PubMed]
- Lavin, J.; French, S.; Ruxton, C.; Read, N. An investigation of the role of oro-sensory stimulation in sugar satiety? Int. J. Obes. 2002, 26, 384–388. [Google Scholar] [CrossRef]
- French, S.J.; Cecil, J.E. Oral, gastric and intestinal influences on human feeding. Physiol. Behav. 2001, 74, 729–734. [Google Scholar] [CrossRef]
- Cassady, B.A.; Considine, R.V.; Mattes, R.D. Beverage consumption, appetite, and energy intake: What did you expect? Am. J. Clin. Nutr. 2012, 95, 587–593. [Google Scholar] [CrossRef] [PubMed]
- Leidy, H.J.; Apolzan, J.; Mattes, R.D.; Campbell, W.W. Food Form and Portion Size Affect Postprandial Appetite Sensations and Hormonal Responses in Healthy, Nonobese, Older Adults. Obesity 2010, 18, 293–299. [Google Scholar] [CrossRef] [PubMed]
- DiMeglio, D.; Mattes, R. Liquid versus solid carbohydrate: Effects on food intake and body weight. Int. J. Obes. 2000, 24, 794–800. [Google Scholar] [CrossRef] [PubMed]
- Diamond, A. Executive Functions. Ann. Rev. Psychol. 2013, 64, 135–168. [Google Scholar] [CrossRef]
- Field, M.; Wiers, R.; Christiansen, P.; Fillmore, M.T.; Verster, J.C. Acute Alcohol Effects on Inhibitory Control and Implicit Cognition: Implications for Loss of Control Over Drinking. Alcohol. Clin. Exp. Res. 2010, 34, 1346–1352. [Google Scholar] [CrossRef]
- Christiansen, P.; Rose, A.; Randall-Smith, L.; Hardman, C.A. Alcohol’s acute effect on food intake is mediated by inhibitory control impairments. Health Psychol. 2016, 35, 518–522. [Google Scholar] [CrossRef]
- Caton, S.J.; Nolan, L.J.; Hetherington, M.M. Alcohol, Appetite and Loss of Restraint. Curr. Obes. Rep. 2015, 4, 99–105. [Google Scholar] [CrossRef]
- Luce, K.H.; Crowther, J.H.; Leahey, T.; Buchholz, L.J. Do restrained eaters restrict their caloric intake prior to drinking alcohol? Eat Behav. 2013, 14, 361–365. [Google Scholar] [CrossRef]
- Jones, A.; Robinson, E.; Duckworth, J.; Kersbergen, I.; Clarke, N.; Field, M. The effects of exposure to appetitive cues on inhibitory control: A meta-analytic investigation. Appetite 2018, 128, 271–282. [Google Scholar] [CrossRef]
- Schrieks, I.C.; Stafleu, A.; Griffioen-Roose, S.; de Graaf, C.; Witkamp, R.; Boerrigter-Rijneveld, R.; Hendriks, H.F. Moderate alcohol consumption stimulates food intake and food reward of savoury foods. Appetite 2015, 89, 77–83. [Google Scholar] [CrossRef]
- Gough, T.; Christiansen, P.; Rose, A.K.; Hardman, C.A. The effect of alcohol on food-related attentional bias, food reward and intake: Two experimental studies. Appetite 2021, 162, 105173. [Google Scholar] [CrossRef]
- Castellanos, E.H.; Charboneau, E.; Dietrich, M.S.; Park, S.; Bradley, B.; Mogg, K.; Cowan, R.L. Obese adults have visual attention bias for food cue images: Evidence for altered reward system function. Int. J. Obes. 2009, 33, 1063–1073. [Google Scholar] [CrossRef] [PubMed]
- Adams, S.; Wijk, E. Effects of Acute Alcohol Consumption on Food Intake and Pictorial Stroop Response to High-Calorie Food Cues. Alcohol Alcohol. 2020, 56, 275–283. [Google Scholar] [CrossRef] [PubMed]
- Monem, R.; Fillmore, M.T. Alcohol administration reduces attentional bias to alcohol-related but not food-related cues: Evi-dence for a satiety hypothesis. Psychol. Addict. Behav. 2019, 33, 677–684. [Google Scholar] [CrossRef]
- Karyadi, K.A.; Cyders, M.A. Preliminary support for the role of alcohol cues in food cravings and attentional biases. J. Health Psychol. 2017, 24, 812–822. [Google Scholar] [CrossRef]
- Scott, S.; Elamin, W.; Giles, E.L.; Hillier-Brown, F.; Byrnes, K.; Connor, N.; Newbury-Birch, D.; Ells, L. Socio-Ecological Influences on Adolescent (Aged 10–17) Alcohol Use and Unhealthy Eating Behaviours: A Systematic Review and Synthesis of Qualitative Studies. Nutrients 2019, 11, 1914. [Google Scholar] [CrossRef] [PubMed]
- Scott, S.; Muir, C.; Stead, M.; Fitzgerald, N.; Kaner, E.; Bradley, J.; Wrieden, W.; Power, C.; Adamson, A. Exploring the links between unhealthy eating behaviour and heavy alcohol use in the social, emotional and cultural lives of young adults (aged 18–25): A qualitative research study. Appetite 2019, 144, 104449. [Google Scholar] [CrossRef] [PubMed]
- Nelson, M.C.; Kocos, R.; Lytle, L.A.; Perry, C.L. Understanding the Perceived Determinants of Weight-related Behaviors in Late Adolescence: A Qualitative Analysis among College Youth. J. Nutr. Educ. Behav. 2009, 41, 287–292. [Google Scholar] [CrossRef]
- Ayuka, F.; Barnett, R.; Pearce, J. Neighbourhood availability of alcohol outlets and hazardous alcohol consumption in New Zealand. Health Place 2014, 29, 186–199. [Google Scholar] [CrossRef]
- Weitzman, E.R.; Folkman, A.; Folkman, M.K.L.; Wechsler, H. The relationship of alcohol outlet density to heavy and frequent drinking and drinking-related problems among college students at eight universities. Health Place 2002, 9, 1–6. [Google Scholar] [CrossRef]
- Burgoine, T.; Sarkar, C.; Webster, C.J.; Monsivais, P. Examining the interaction of fast-food outlet exposure and income on diet and obesity: Evidence from 51,361 UK Biobank participants. Int. J. Behav. Nutr. Phys. Activity 2018, 15, 71. [Google Scholar] [CrossRef] [PubMed]
- Maguire, E.R.; Burgoine, T.; Monsivais, P. Area deprivation and the food environment over time: A repeated cross-sectional study on takeaway outlet density and supermarket presence in Norfolk, UK, 1990–2008. Health Place 2015, 33, 142–147. [Google Scholar] [CrossRef] [PubMed]
- Public Health England. Obesity and the Environment. Density of Fast Food Outlets at 31 December 2017. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/741555/Fast_Food_map.pdf (accessed on 23 July 2021).
- Berke, E.M.; Tanski, S.E.; Demidenko, E.; Alford-Teaster, J.; Shi, X.; Sargent, J.D. Alcohol Retail Density and Demographic Predictors of Health Disparities: A Geographic Analysis. Am. J. Public Health 2010, 100, 1967–1971. [Google Scholar] [CrossRef]
- Huckle, T.; Parker, K.; Romeo, J.S.; Casswell, S. Online alcohol delivery is associated with heavier drinking during the first New Zealand COVID -19 pandemic restrictions. Drug Alcohol Rev. 2020, 40, 826–834. [Google Scholar] [CrossRef] [PubMed]
- Mojica-Perez, Y.; Callinan, S.; Livingston, M. Alcohol Home Delivery Services: An Investigation of Use and Risk 2019. Available online: https://fare.org.au/wp-content/uploads/Alcohol-home-delivery-services.pdf (accessed on 23 July 2021).
- Keeble, M.; Adams, J.; Sacks, G.; Vanderlee, L.; White, C.M.; Hammond, D.; Burgoine, T. Use of Online Food Delivery Services to Order Food Prepared Away-From-Home and Associated Sociodemographic Characteristics: A Cross-Sectional, Multi-Country Analysis. Int. J. Environ. Res. Public Health 2020, 17, 5190. [Google Scholar] [CrossRef]
- NHS Digital. Expenditure and Affordability 2020. Available online: https://digital.nhs.uk/data-and-information/publications/statistical/statistics-on-alcohol/2020/part-7 (accessed on 23 July 2021).
- Alcohol Health Alliance. Small Change: Alcohol at Pocket Money Prices. AHA Pricing Survey. 2020. Available online: https://ahauk.org/wp-content/uploads/2021/04/Small-change-Final-04_2021-compressed.pdf (accessed on 23 July 2021).
- Petticrew, M.; Maani, N.; Pettigrew, L.; Rutter, H.; VAN Schalkwyk, M.C. Dark Nudges and Sludge in Big Alcohol: Behavioral Economics, Cognitive Biases, and Alcohol Industry Corporate Social Responsibility. Milbank Q. 2020, 98, 1290–1328. [Google Scholar] [CrossRef]
- Smith, R.; Kelly, B.; Yeatman, H.; Boyland, E. Food Marketing Influences Children’s Attitudes, Preferences and Consumption: A Systematic Critical Review. Nutrients 2019, 11, 875. [Google Scholar] [CrossRef]
- Viacava, K.R.; Weydmann, G.J.; De Vasconcelos, M.F.; Jaboinski, J.; Batista, G.D.; De Almeida, R.M.M.; Bizarro, L. It is pleasant and heavy: Convergence of visual contents in tobacco, alcohol and food marketing in Brazil. Health Promot. Int. 2015, 31, 674–683. [Google Scholar] [CrossRef][Green Version]
- Miller, D.; Harkins, C. Corporate strategy, corporate capture: Food and alcohol industry lobbying and public health. Crit. Soc. Policy 2010, 30, 564–589. [Google Scholar] [CrossRef]
- Livonen, K. Defensive responses to strategic sustainability paradoxes: Have your coke and drink it too! J. Bus. Ethics 2018, 148, 309–327. [Google Scholar] [CrossRef]
- Rinaldi, C.; van Schalkwyk, M.C.; Egan, M.; Petticrew, M. A Framing Analysis of Consultation Submissions on the WHO Global Strategy to Reduce the Harmful Use of Alcohol: Values and Interests. Int. J. Health Policy Manag. 2021, in press. [Google Scholar] [CrossRef]
- Campbell, N.; Mialon, M.; Reilly, K.; Browne, S.; Finucane, F.M. How are frames generated? Insights from the industry lobby against the sugar tax in Ireland. Soc. Sci. Med. 2020, 264, 113215. [Google Scholar] [CrossRef]
- Lauber, K.; Ralston, R.; Mialon, M.; Carriedo, A.; Gilmore, A. Non-communicable disease governance in the era of the sustainable development goals: A qualitative analysis of food industry framing in WHO consultations. Glob. Health 2020, 16, 76. [Google Scholar] [CrossRef]
- Petticrew, M.; Katikireddi, S.V.; Knai, C.; Cassidy, R.; Maani Hessari, N.; Thomas, J.; Weishaar, H. Nothing can be done until eve-rything is done: The use of complexity arguments by food, beverage, alcohol and gambling industries. J. Epidemiol. Community Health 2017, 71, 1078–1083. [Google Scholar]
- Martino, F.; Brooks, R.; Browne, J.; Carah, N.; Zorbas, C.; Corben, K.; Saleeba, E.; Martin, J.; Peeters, A.; Backholer, K. The Nature and Extent of Online Marketing by Big Food and Big Alcohol During the COVID-19 Pandemic in Australia: Content Analysis Study. JMIR Public Health Surveill. 2021, 7, e25202. [Google Scholar] [CrossRef]
- Schoenmakers, T.; Wiers, R. Craving and Attentional Bias Respond Differently to Alcohol Priming: A Field Study in the Pub. Eur. Addict. Res. 2010, 16, 9–16. [Google Scholar] [CrossRef]
- Bush, K.; Kivlahan, D.R.; McDonell, M.B.; Fihn, S.D.; Bradley, K.A. The AUDIT Alcohol Consumption Questions (AUDIT-C) An Effective Brief Screening Test for Problem Drinking. Arch. Intern. Med. 1998, 158, 1789–1795. [Google Scholar] [CrossRef]
- McKenna, H.; Treanor, C.; O’Reilly, D.; Donnelly, M. Evaluation of the psychometric properties of self-reported measures of alcohol consumption: A COSMIN systematic review. Subst. Abus. Treat. Prev. Policy 2018, 13, 6. [Google Scholar] [CrossRef]
- Gmel, G.; Daeppen, J.B. Recall bias for seven-day recall measurement of alcohol consumption among emergency department patients: Implications for case-crossover designs. J. Stud. Alcohol Drugs. 2007, 68, 303–310. [Google Scholar] [CrossRef]
- Cherpitel, C.J.; Ye, Y.; Stockwell, T.; Vallance, K.; Chow, C. Recall bias across 7 days in self-reported alcohol consumption prior to injury among emergency department patients. Drug Alcohol Rev. 2017, 37, 382–388. [Google Scholar] [CrossRef]
- Davis, C.G.; Thake, J.; Vilhena, N. Social desirability biases in self-reported alcohol consumption and harms. Addict. Behav. 2010, 35, 302–311. [Google Scholar] [CrossRef]
- Devos-Comby, L.; Lange, J.E. My Drink is Larger than Yours? A Literature Review of Self-Defined Drink Sizes and Standard Drinks. Curr. Drug Abus. Rev. 2008, 1, 162–176. [Google Scholar] [CrossRef]
- Gilligan, C.; Anderson, K.G.; Ladd, B.O.; Yong, Y.M.; David, M. Inaccuracies in survey reporting of alcohol consumption. BMC Public Health 2019, 19, 1639. [Google Scholar] [CrossRef]
- Dodge, T.; Clarke, P.; Dwan, R. The Relationship Between Physical Activity and Alcohol Use Among Adults in the United States. Am. J. Health Promot. 2016, 31, 97–108. [Google Scholar] [CrossRef] [PubMed]
- Piazza-Gardner, A.K.; Barry, A.E. Examining physical activity levels and alcohol consumption: Are people who drink more active? Am. J. Health Promot. 2012, 26, e95–e104. [Google Scholar] [CrossRef]
- Matley, F.A.I.; Davies, E.L. Resisting temptation: Alcohol specific self-efficacy mediates the impacts of compensatory health beliefs and behaviours on alcohol consumption. Psychol. Health Med. 2017, 23, 259–269. [Google Scholar] [CrossRef]
- Bray, G.A.; Flatt, J.-P.; Volaufova, J.; Delany, J.P.; Champagne, C.M. Corrective responses in human food intake identified from an analysis of 7-d food-intake records. Am. J. Clin. Nutr. 2008, 88, 1504–1510. [Google Scholar] [CrossRef] [PubMed]
- Eisenberg, M.; Fitz, C.C. “Drunkorexia”: Exploring the Who and Why of a Disturbing Trend in College Students’ Eating and Drinking Behaviors. J. Am. Coll. Health 2014, 62, 570–577. [Google Scholar] [CrossRef]
- Knight, A.; Castelnuovo, G.; Pietrabissa, G.; Manzoni, G.M.; Simpson, S. Drunkorexia: An Empirical Investigation among Australian Female University Students. Aust. Psychol. 2017, 52, 414–423. [Google Scholar] [CrossRef]
- Lupi, M.; Martinotti, G.; Di Giannantonio, M. Drunkorexia: An emerging trend in young adults. Eat. Weight. Disord. Stud. Anorex. Bulim. Obes. 2017, 22, 619–622. [Google Scholar] [CrossRef]
- Wilkerson, A.H.; Hackman, C.L.; Rush, S.E.; Usdan, S.L.; Smith, C.S. “Drunkorexia”: Understanding eating and physical activity be-haviors of weight conscious drinkers in a sample of college students. J. Am. Coll. Health 2017, 65, 492–501. [Google Scholar] [CrossRef]
- Albani, V.; Bradley, J.; Wrieden, W.L.; Scott, S.; Muir, C.; Power, C.; Fitzgerald, N.; Stead, M.; Kaner, E.; Adamson, A.J. Examining Associations between Body Mass Index in 18–25 Year-Olds and Energy Intake from Alcohol: Findings from the Health Survey for England and the Scottish Health Survey. Nutrients 2018, 10, 1477. [Google Scholar] [CrossRef]
- Thern, E.; Landberg, J. Understanding the differential effect of alcohol consumption on the relation between socio-economic position and alcohol-related health problems: Results from the Stockholm Public Health Cohort. Addiction 2020, 116, 799–808. [Google Scholar] [CrossRef]
- Boniface, S.; Lewer, D.; Hatch, S.; Goodwin, L. Associations between interrelated dimensions of socio-economic status, higher risk drinking and mental health in South East London: A cross-sectional study. PLoS ONE 2020, 15, e0229093. [Google Scholar] [CrossRef] [PubMed]
- Sadler, S.; Angus, C.; Gavens, L.; Gillespie, D.; Holmes, J.; Hamilton, J.; Brennan, A.; Meier, P. Understanding the alcohol harm paradox: An analysis of sex- and condition-specific hospital admissions by socio-economic group for alcohol-associated conditions in England. Addiction 2017, 112, 808–817. [Google Scholar] [CrossRef]
- Bellis, M.A.; Hughes, K.; Nicholls, J.; Sheron, N.; Gilmore, I.; Jones, L. The alcohol harm paradox: Using a national survey to explore how alcohol may disproportionately impact health in deprived individuals. BMC Public Health 2016, 16, 111. [Google Scholar] [CrossRef] [PubMed]
- Adan, A.; Forero, D.; Navarro, J.F. Personality Traits Related to Binge Drinking: A Systematic Review. Front. Psychiatry 2017, 8, 134. [Google Scholar] [CrossRef] [PubMed]
- Bénard, M.; Bellisle, F.; Kesse-Guyot, E.; Julia, C.; Andreeva, V.A.; Etilé, F.; Reach, G.; Dechelotte, P.; Tavolacci, M.-P.; Hercberg, S.; et al. Impulsivity is associated with food intake, snacking, and eating disorders in a general population. Am. J. Clin. Nutr. 2018, 109, 117–126. [Google Scholar] [CrossRef]
- World Obesity. Sugar-Sweetened Beverage Tax: Systematic Reviews 2019. Available online: https://www.worldobesity.org/resources/policy-dossiers/pd-1/systematic-reviews (accessed on 23 July 2021).
- World Obesity. Sugar-Sweetened Beverage Tax: Case Studies 2019. Available online: https://www.worldobesity.org/resources/policy-dossiers/pd-1/case-studies (accessed on 23 July 2021).
- Lhachimi, S.K.; Pega, F.; Heise, T.L.; Fenton, C.; Gartlehner, G.; Griebler, U.; Sommer, I.; Bombana, M.; Katikireddi, S. Taxation of the fat content of foods for reducing their consumption and preventing obesity or other adverse health outcomes. Cochrane Database Syst Rev. 2020, 9, CD012415. [Google Scholar] [CrossRef][Green Version]
- Boniface, S.; Scannell, J.W.; Marlow, S. Evidence for the effectiveness of minimum pricing of alcohol: A systematic review and assessment using the Bradford Hill criteria for causality. BMJ Open 2017, 7, e013497. [Google Scholar] [CrossRef]
- Anderson, P.; O’Donnell, A.; Kaner, E.; Llopis, E.J.; Manthey, J.; Rehm, J. Impact of minimum unit pricing on alcohol purchases in Scotland and Wales: Controlled interrupted time series analyses. Lancet Public Health 2021, 6, e557–e565. [Google Scholar] [CrossRef]
- Llopis, E.J.; O’Donnell, A.; Anderson, P. Impact of price promotion, price, and minimum unit price on household purchases of low and no alcohol beers and ciders: Descriptive analyses and interrupted time series analysis of purchase data from 70, 303 British households, 2015–2018 and first half of 2020. Soc. Sci. Med. 2021, 270, 113690. [Google Scholar] [CrossRef] [PubMed]
- Nelson, J.P.; McNall, A.D. Alcohol prices, taxes, and alcohol-related harms: A critical review of natural experiments in alcohol policy for nine countries. Health Policy 2016, 120, 264–272. [Google Scholar] [CrossRef] [PubMed]
- Elder, R.W.; Lawrence, B.; Ferguson, A.; Naimi, T.; Brewer, R.D.; Chattopadhyay, S.K.; Toomey, T.L.; Fielding, J.E. The Effectiveness of Tax Policy Interventions for Reducing Excessive Alcohol Consumption and Related Harms. Am. J. Prev. Med. 2010, 38, 217–229. [Google Scholar] [CrossRef] [PubMed]
- Boyland, E.J.; Nolan, S.N.; Kelly, B.; Tudur-Smith, C.; Jones, A.; Halford, J.C.; Robinson, E. Advertising as a cue to consume: A systematic review and meta-analysis of the effects of acute exposure to unhealthy food and nonalcoholic beverage advertising on intake in children and adults. Am. J. Clin. Nutr. 2016, 103, 519–533. [Google Scholar] [CrossRef]
- Obesity Health Alliance. The Need for a Comprehensive 9pm Watershed on All Junk Food Adverts Shown on All Types of Media 2021. Available online: http://obesityhealthalliance.org.uk/wp-content/uploads/2019/03/The-need-for-a-comprehensive-9pm-watershed-Briefing.pdf (accessed on 23 July 2021).
- Ireland, R.; Chambers, S.; Bunn, C. Exploring the relationship between Big Food corporations and professional sports clubs: A scoping review. Public Health Nutr. 2019, 22, 1888–1897. [Google Scholar] [CrossRef]
- Smith, M.; Signal, L.; Edwards, R.; Hoek, J. Children’s and parents’ opinions on the sport-related food environment: A systematic review. Obes. Rev. 2017, 18, 1018–1039. [Google Scholar] [CrossRef]
- Stautz, K.; Brown, K.G.; King, S.E.; Shemilt, I.; Marteau, T.M. Immediate effects of alcohol marketing communications and media portrayals on consumption and cognition: A systematic review and meta-analysis of experimental studies. BMC Public Health 2016, 16, 465. [Google Scholar] [CrossRef]
- Courtney, A.L.; Rapuano, K.M.; Sargent, J.D.; Heatherton, T.F.; Kelley, W.M. Reward System Activation in Response to Alcohol Advertisements Predicts College Drinking. J. Stud Alcohol Drugs 2018, 79, 29–38. [Google Scholar] [CrossRef]
- Westberg, K.; Stavros, C.; Smith, A.C.; Munro, G.; Argus, K. An examination of how alcohol brands use sport to engage consumers on social media. Drug Alcohol Rev. 2016, 37, 28–35. [Google Scholar] [CrossRef]
- Jones, S. When does alcohol sponsorship of sport become sports sponsorship of alcohol? A case study of developments in sport in Australia. Int. J. Sports Mark. Spons. 2010, 11, 67–78. [Google Scholar] [CrossRef]
- Williams, J.; Scarborough, P.; Matthews, A.; Cowburn, G.; Foster, C.; Roberts, N.; Rayner, M. A systematic review of the influence of the retail food environment around schools on obesity-related outcomes. Obes. Rev. 2014, 15, 359–374. [Google Scholar] [CrossRef] [PubMed]
- Keeble, M.; Burgoine, T.; White, M.; Summerbell, C.; Cummins, S.; Adams, J. How does local government use the planning system to regulate hot food takeaway outlets? A census of current practice in England using document review. Health Place 2019, 57, 171–178. [Google Scholar] [CrossRef] [PubMed]
- Keeble, M.; Adams, J.; White, M.; Summerbell, C.; Cummins, S.; Burgoine, T. Correlates of English local government use of the planning system to regulate hot food takeaway outlets: A cross-sectional analysis. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 127. [Google Scholar] [CrossRef] [PubMed]
- Goffe, L.; Uwamahoro, N.S.; Dixon, C.J.; Blain, A.P.; Danielsen, J.; Kirk, D.; Adamson, A.J. Supporting a Healthier Takeaway Meal Choice: Creating a Universal Health Rating for Online Takeaway Fast-Food Outlets. Int. J. Environ. Res. Public Health 2020, 17, 9260. [Google Scholar] [CrossRef]
- Popova, S.; Giesbrecht, N.; Bekmuradov, D.; Patra, J. Hours and Days of Sale and Density of Alcohol Outlets: Impacts on Alcohol Consumption and Damage: A Systematic Review. Alcohol Alcohol. 2009, 44, 500–516. [Google Scholar] [CrossRef]
- Campbell, C.A.; Hahn, R.A.; Elder, R.; Brewer, R.; Chattopadhyay, S.; Fielding, J.; Naimi, T.; Toomey, T.; Lawrence, B.; Middleton, J.C. The Effectiveness of Limiting Alcohol Outlet Density as a Means of Reducing Excessive Alcohol Consumption and Alcohol-Related Harms. Am. J. Prev. Med. 2009, 37, 556–569. [Google Scholar] [CrossRef]
- Hahn, R.A.; Kuzara, J.L.; Elder, R.; Brewer, R.; Chattopadhyay, S.; Fielding, J.; Naimi, T.S.; Toomey, T.; Middleton, J.C.; Lawrence, B. Effectiveness of policies restricting hours of alcohol sales in preventing excessive alcohol consumption and related harms. Am. J. Prev Med. 2010, 39, 590–604. [Google Scholar] [CrossRef]
- Colbert, S.; Wilkinson, C.; Thornton, L.; Feng, X.; Richmond, R. Online alcohol sales and home delivery: An international policy review and systematic literature review. Health Policy 2021, in press. [Google Scholar] [CrossRef]
- Gupta, A.; Billich, N.; George, N.A.; Blake, M.R.; Huse, O.; Backholer, K.; Boelsen-Robinson, T.; Peeters, A. The effect of front-of-package labels or point-of-sale signage on consumer knowledge, attitudes and behavior regarding sugar-sweetened beverages: A systematic review. Nutr. Rev. 2020, in press. [Google Scholar] [CrossRef]
- Chan, J.; McMahon, E.; Brimblecombe, J. Point-of-sale nutrition information interventions in food retail stores to promote healthier food purchase and intake: A systematic review. Obes. Rev. 2021, in press. [Google Scholar] [CrossRef]
- Watt, T.L.S.; Beckert, W.; Smith, R.D.; Cornelsen, L. Reducing consumption of unhealthy foods and beverages through banning price promotions: What is the evidence and will it work? Public Health Nutr. 2020, 23, 2228–2233. [Google Scholar] [CrossRef]
- Carter, P.; Bignardi, G.; Hollands, J.; Marteau, T.M. Information-based cues at point of choice to change selection and consumption of food, alcohol and tobacco products: A systematic review. BMC Public Health 2018, 18, 418. [Google Scholar] [CrossRef]
- Meier, P.; Booth, A.; Stockwell, T.; Sutton, A.; Wilkerson, A.; Wong, R. Independent Review of the Effects of Alcohol Pricing and Promotion; University of Sheffield: Sheffield, UK, 2008. [Google Scholar]
- Jackson, R.; Johnson, M.; Campbell, F.; Messina, J.; Guillaume, L.; Meier, P.; Goyder, E.; Chilcott, J.; Payne, N. Interventions on Control of Alcohol Price, Promotion and Availability for Prevention of Alcohol Use Disorders in Adults and Young People; University of Sheffield: Sheffield, UK, 2010. [Google Scholar]
- Gressier, M.; Swinburn, B.; Frost, G.; Segal, A.B.; Sassi, F. What is the impact of food reformulation on individuals’ behaviour, nutrient intakes and health status? A systematic review of empirical evidence. Obes. Rev. 2020, 22, e13139. [Google Scholar] [CrossRef]
- Hashem, K.M.; He, F.J.; A MacGregor, G. Effects of product reformulation on sugar intake and health—A systematic review and meta-analysis. Nutr. Rev. 2019, 77, 181–196. [Google Scholar] [CrossRef]
- Rehm, J.; Lachenmeier, D.W.; Llopis, E.J.; Imtiaz, S.; Anderson, P. Evidence of reducing ethanol content in beverages to reduce harmful use of alcohol. Lancet Gastroenterol. Hepatol. 2016, 1, 78–83. [Google Scholar] [CrossRef]
- Rosenblatt, D.H.; Bode, S.; Dixon, H.; Murawski, C.; Summerell, P.; Ng, A.; Wakefield, M. Health warnings promote healthier dietary decision making: Effects of positive versus negative message framing and graphic versus text-based warnings. Appetite 2018, 127, 280–288. [Google Scholar] [CrossRef] [PubMed]
- Clarke, N.; Pechey, E.; Kosīte, D.; König, L.M.; Mantzari, E.; Blackwell, A.K.; Marteau, T.M.; Hollands, G.J. Impact of health warning labels on selection and consumption of food and alcohol products: Systematic review with meta-analysis. Health Psychol. Rev. 2020, 1–24. [Google Scholar] [CrossRef] [PubMed]
- Robinson, E.; Humphreys, G.; Jones, A. Alcohol, calories, and obesity: A rapid systematic review and meta-analysis of consumer knowledge, support, and behavioral effects of energy labeling on alcoholic drinks. Obes Rev. 2021, 22, e13198. [Google Scholar] [CrossRef] [PubMed]
- Stautz, K.; Marteau, T.M. Viewing alcohol warning advertising reduces urges to drink in young adults: An online experiment. BMC Public Health 2016, 16, 530. [Google Scholar] [CrossRef] [PubMed]
- Steenhuis, I.H.M.; Vermeer, W.M. Portion size: Review and framework for interventions. Int. J. Behav. Nutr. Phys. Activity 2009, 6, 58. [Google Scholar] [CrossRef]
- Marteau, T.M.; Hollands, G.; Shemilt, I.; Jebb, S.A. Downsizing: Policy options to reduce portion sizes to help tackle obesity. BMJ 2015, 351, h5863. [Google Scholar] [CrossRef] [PubMed]
- Kersbergen, I.; Oldham, M.; Jones, A.; Field, M.; Angus, C.; Robinson, E. Reducing the standard serving size of alcoholic beverages prompts reductions in alcohol consumption. Addiction 2018, 113, 1598–1608. [Google Scholar] [CrossRef] [PubMed]
- Pilling, M.; Clarke, N.; Pechey, R.; Hollands, G.; Marteau, T. The effect of wine glass size on volume of wine sold: A mega-analysis of studies in bars and restaurants. Addiction 2020, 115, 1660–1667. [Google Scholar] [CrossRef] [PubMed]
- Vasiljevic, M.; Couturier, D.-L.; Marteau, T.M. What are the perceived target groups and occasions for wines and beers labelled with verbal and numerical descriptors of lower alcohol strength? An experimental study. BMJ Open 2019, 9, e024412. [Google Scholar] [CrossRef] [PubMed]
- Cummings, J.R.; Ray, L.A.; Tomiyama, A.J. Food-alcohol competition: As young females eat more food, do they drink less alcohol? J. Health Psychol. 2017, 22, 674–683. [Google Scholar] [CrossRef] [PubMed]
- Farhat, T.; Iannotti, R.J.; Simons-Morton, B.G. Overweight, obesity, youth, and health-risk behaviors. Am. J. Prev. Med. 2010, 38, 258–267. [Google Scholar] [CrossRef] [PubMed]
- Pasch, K.E.; Nelson, M.C.; Lytle, L.A.; Moe, S.G.; Perry, C.L. Adoption of Risk-Related Factors Through Early Adolescence: Associations with Weight Status and Implications for Causal Mechanisms. J. Adolesc. Health 2008, 43, 387–393. [Google Scholar] [CrossRef] [PubMed]
- Peralta, R.L.; Barr, P.B. Gender orientation and alcohol-related weight control behavior among male and female college students. J. Am. Coll. Health 2016, 65, 229–242. [Google Scholar] [CrossRef]
- Simpson, R.F.; Hermon, C.; Liu, B.; Green, J.; Reeves, G.K.; Beral, V.; Floud, S. Alcohol drinking patterns and liver cirrhosis risk: Analysis of the prospective UK Million Women Study. Lancet Public Health 2018, 4, e41–e48. [Google Scholar] [CrossRef]
- Jani, B.D.; McQueenie, R.; Nicholl, B.I.; Field, R.; Hanlon, P.; Gallacher, K.I.; Mair, F.S.; Lewsey, J. Association between patterns of alcohol consumption (beverage type, frequency and consumption with food) and risk of adverse health outcomes: A prospective cohort study. BMC Med. 2021, 19, 8. [Google Scholar] [CrossRef] [PubMed]
- Puddephatt, J.-A.; Keenan, G.; Fielden, A.; Reaves, D.; Halford, J.C.; Hardman, C.A. ‘Eating to survive’: A qualitative analysis of factors influencing food choice and eating behaviour in a food-insecure population. Appetite 2019, 147, 104547. [Google Scholar] [CrossRef] [PubMed]
- Reitzel, L.R.; Chinamuthevi, S.; Daundasekara, S.S.; Hernandez, D.C.; Chen, T.-A.; Harkara, Y.; Obasi, E.M.; Kendzor, D.E.; Businelle, M.S. Association of Problematic Alcohol Use and Food Insecurity among Homeless Men and Women. Int. J. Environ. Res. Public Health 2020, 17, 3631. [Google Scholar] [CrossRef] [PubMed]
- Bergmans, R.S.; Coughlin, L.; Wilson, T.; Malecki, K. Cross-sectional associations of food insecurity with smoking cigarettes and heavy alcohol use in a population-based sample of adults. Drug Alcohol Depend. 2019, 205, 107646. [Google Scholar] [CrossRef] [PubMed]
- Tan, J.; Johns, G. Drinking and Eating; Alcohol Change UK: London, UK, 2019. [Google Scholar]
- Wray, T.B.; Merrill, J.E.; Monti, P.M. Using Ecological Momentary Assessment (EMA) to Assess Situation-Level Predictors of Alcohol Use and Alcohol-Related Consequences. Alcohol Res. Curr. Rev. 2014, 36, 19–27. [Google Scholar]
- Oldham, M.; Callinan, S.; Whitaker, V.; Fairbrother, H.; Curtis, P.; Meier, P.; Livingston, M.; Holmes, J. The decline in youth drinking in England—is everyone drinking less? A quantile regression analysis. Addiction 2019, 115, 230–238. [Google Scholar] [CrossRef]
- Vashishtha, R.; Pennay, A.; Dietze, P.; Marzan, M.B.; Room, R.; Livingston, M. Trends in adolescent drinking across 39 high-income countries: Exploring the timing and magnitude of decline. Eur. J. Public Health 2020, 31, 424–431. [Google Scholar] [CrossRef]
| Target of Policy/Strategy | Foods and Non-Alcoholic Beverages | Alcoholic Beverages |
|---|---|---|
| Fiscal policy | ||
| Mass media and marketing | ||
| Sales availability |
|
|
| Product server setting |
|
|
| Product reformulation | ||
| Product labelling |
|
|
| Standard serving sizes |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fong, M.; Scott, S.; Albani, V.; Adamson, A.; Kaner, E. ‘Joining the Dots’: Individual, Sociocultural and Environmental Links between Alcohol Consumption, Dietary Intake and Body Weight—A Narrative Review. Nutrients 2021, 13, 2927. https://doi.org/10.3390/nu13092927
Fong M, Scott S, Albani V, Adamson A, Kaner E. ‘Joining the Dots’: Individual, Sociocultural and Environmental Links between Alcohol Consumption, Dietary Intake and Body Weight—A Narrative Review. Nutrients. 2021; 13(9):2927. https://doi.org/10.3390/nu13092927
Chicago/Turabian StyleFong, Mackenzie, Stephanie Scott, Viviana Albani, Ashley Adamson, and Eileen Kaner. 2021. "‘Joining the Dots’: Individual, Sociocultural and Environmental Links between Alcohol Consumption, Dietary Intake and Body Weight—A Narrative Review" Nutrients 13, no. 9: 2927. https://doi.org/10.3390/nu13092927
APA StyleFong, M., Scott, S., Albani, V., Adamson, A., & Kaner, E. (2021). ‘Joining the Dots’: Individual, Sociocultural and Environmental Links between Alcohol Consumption, Dietary Intake and Body Weight—A Narrative Review. Nutrients, 13(9), 2927. https://doi.org/10.3390/nu13092927






