Is School Gardening Combined with Physical Activity Intervention Effective for Improving Childhood Obesity? A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Databases and Search Criteria
2.2. Study Selection
2.3. Data Selection and Extraction
2.4. Study Quality Assessment
2.5. Statistical Analysis
3. Results
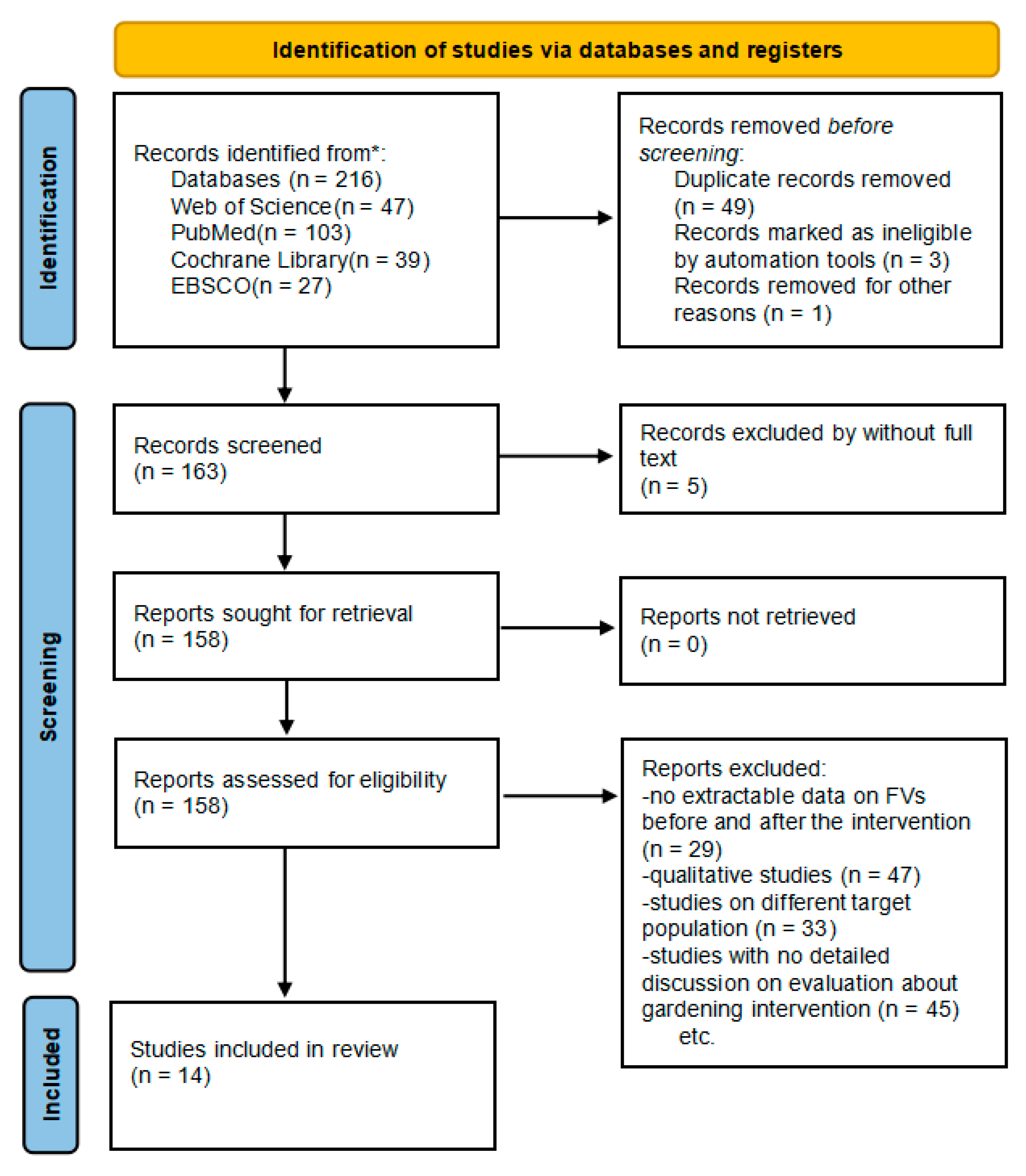
3.1. Search Findings
3.2. Characteristics of the Included Studies
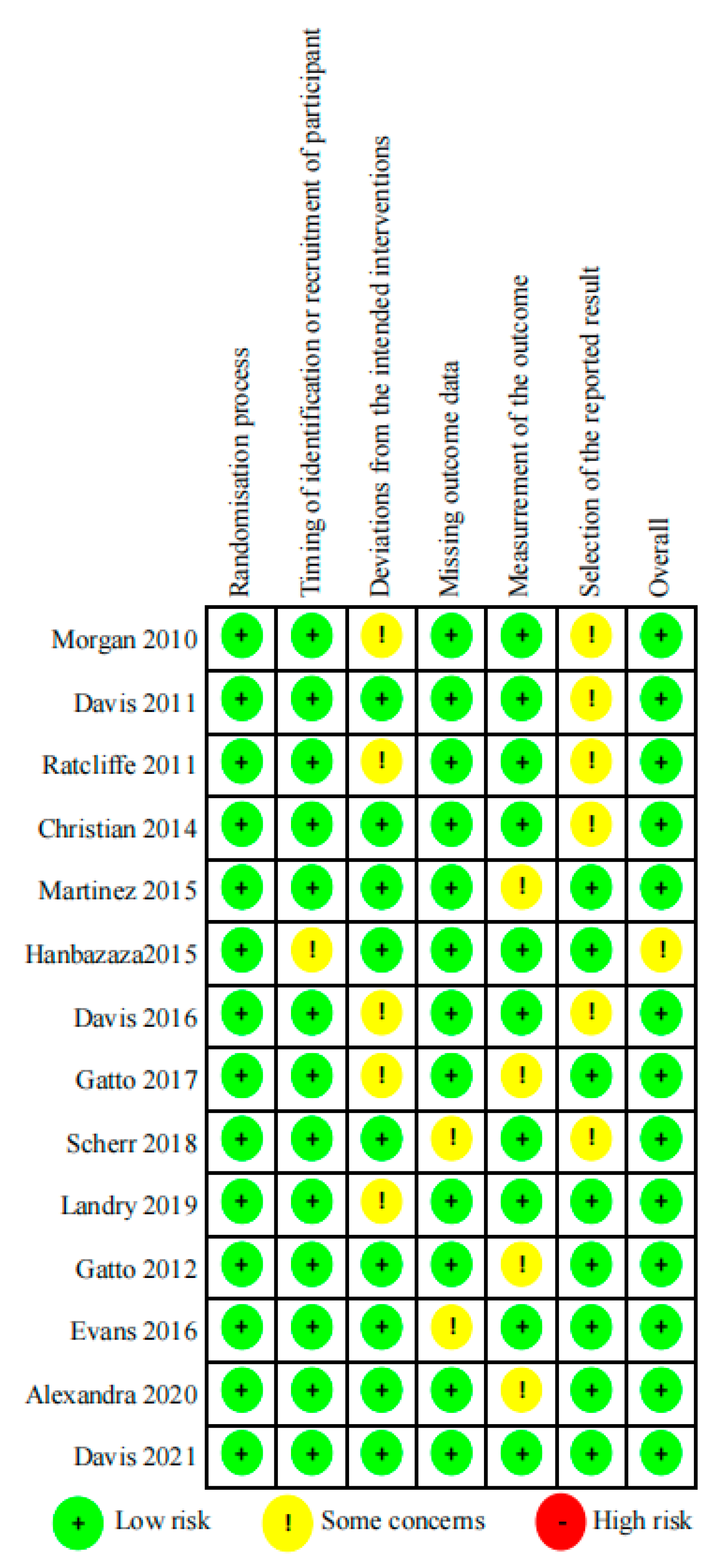
3.3. Quality Assessment
3.4. FVs
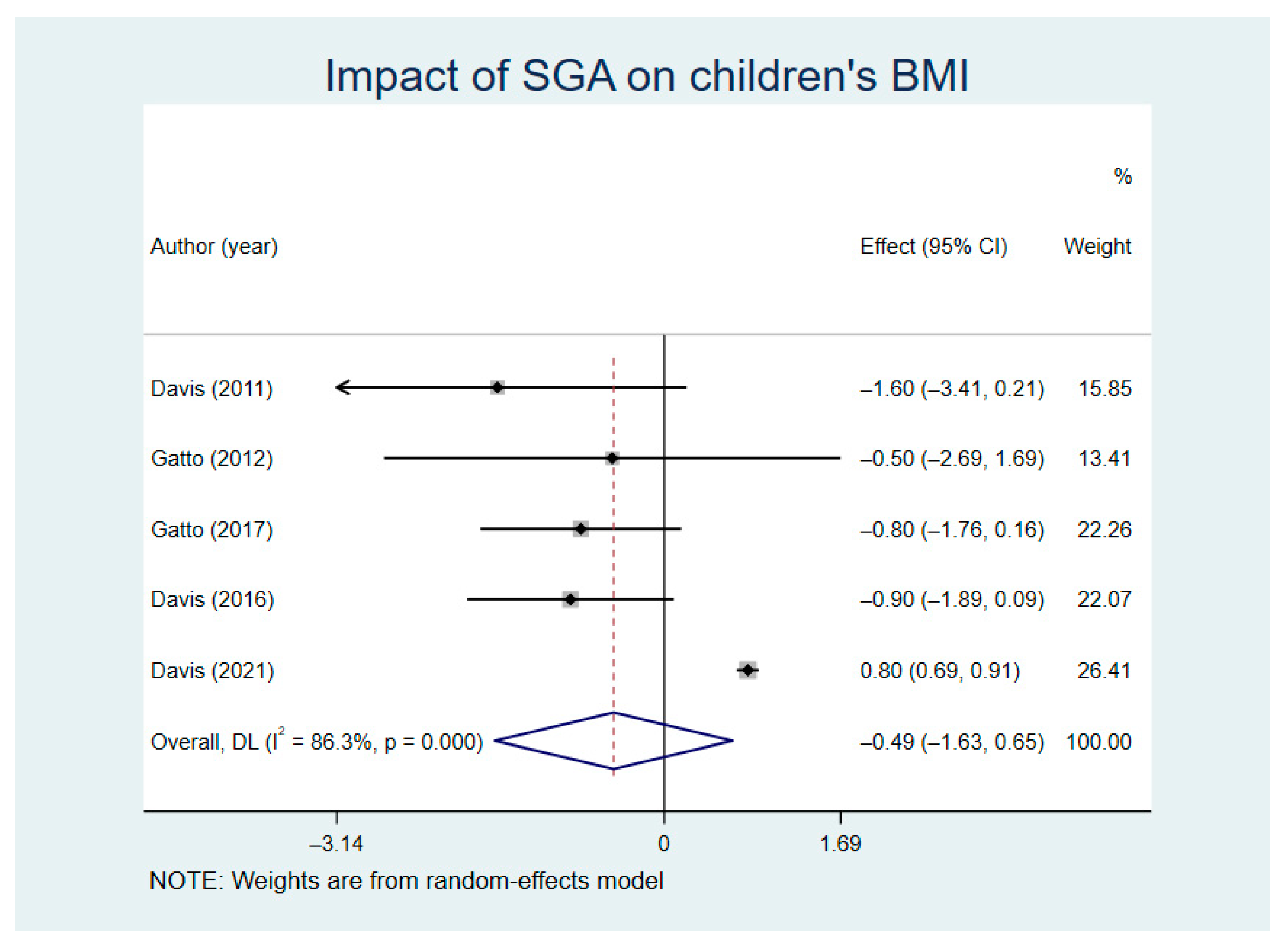
3.5. BMI
3.6. BMI z-Score
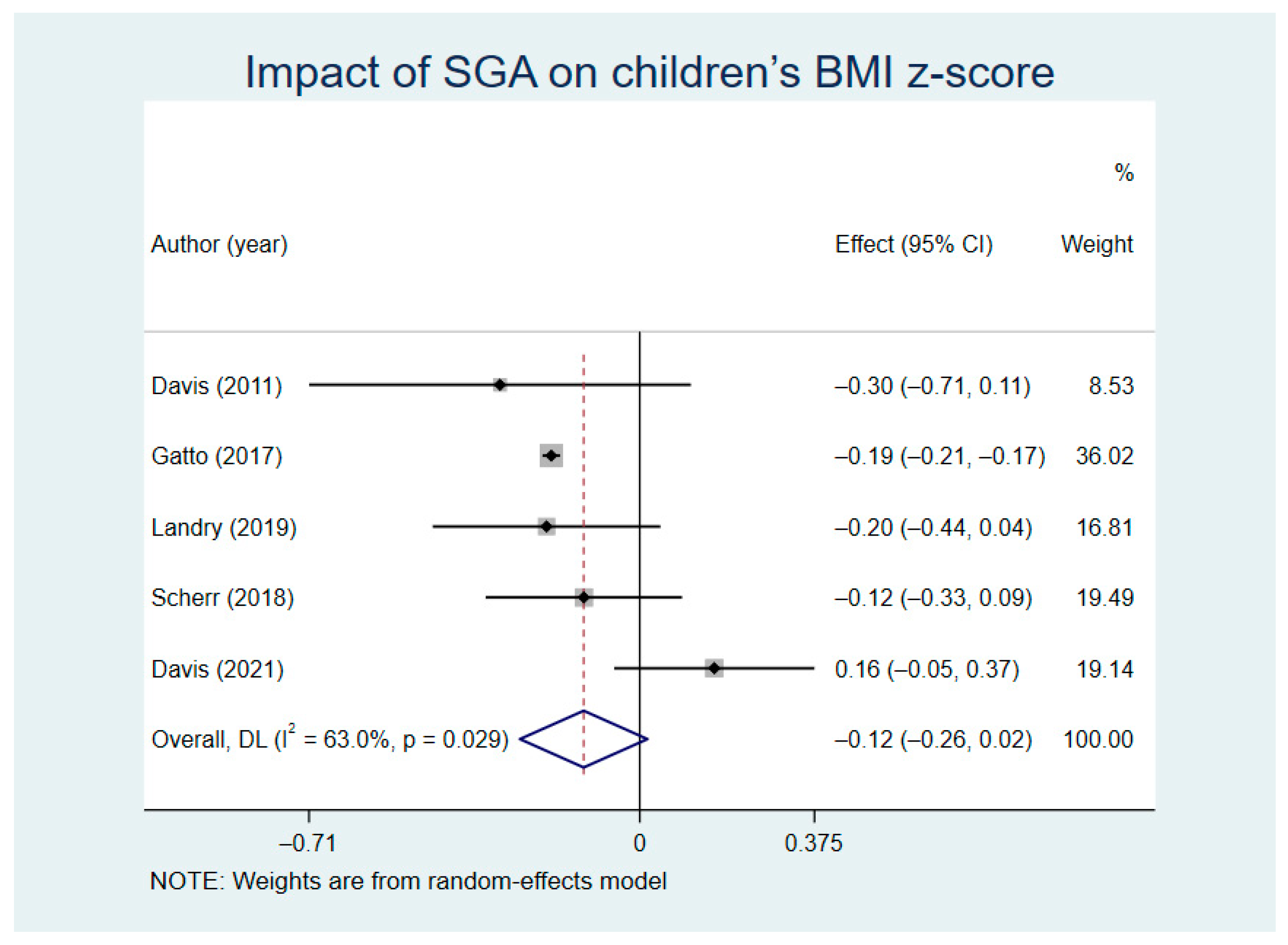
3.7. WC
3.8. Results Impacted by SGA Combined with PA
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ng, M.; Fleming, T.; Robinson, M.; Thomson, B.; Graetz, N.; Margono, C.; Mullany, E.C.; Biryukov, S.; Abbafati, C.; Abera, S.F.; et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014, 384, 766–781. [Google Scholar] [CrossRef]
- Wang, Y.; Lobstein, T. Worldwide trends in childhood overweight and obesity. Int. J. Pediatr. Obes. 2006, 1, 11–25. [Google Scholar] [CrossRef]
- Ogden, C.L.; Carroll, M.D.; Kit, B.K.; Flegal, K.M. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 2014, 311, 806–814. [Google Scholar] [CrossRef] [PubMed]
- Jie, G.A.Q.J. Interpretation of the 2017 U.S. Preventive Services Working Group’s Recommendations for Screening Obesity in Children and Adolescents. J. Chin. Gen. Pract. 2017, 20, 3195–3198. [Google Scholar]
- National Center for Health Statistics. U.S. Health, United States, 2011: With Special Features on Socioeconomic Status and Health. National Center for Health Statistics: Hyattsville, MD, USA, 2012. Available online: https://www.ncbi.nlm.nih.gov/books/NBK98752/ (accessed on 27 July 2021).
- Pan, X.F.; Wang, L.M.; Pan, A. Epidemiology and determinants of obesity in China. Lancet Diabetes Endocrinol. 2021, 9, 373–392. [Google Scholar] [CrossRef]
- Serdula, M.K. Do obese children become obese adults? A review of the literature. Prev. Med. 1993, 22, 167–177. [Google Scholar] [CrossRef]
- Liu, W.; Li, Q.; Li, H.; Li, J.; Wang, H.J.; Li, B. 20-year trends in prevalence of overweight and obesity among children aged 0–6 in Harbin, China: A multiple cross-sectional study. PLoS ONE 2018, 13, e0198032. [Google Scholar] [CrossRef]
- Micic, D.D.; Polovina, S.; Micic, D.D. Does Obesity Cause Type 2 Diabetes? Int. C Interd. Manag. D 2020, 11, 379–381. [Google Scholar]
- Liang, Y.J.; Hou, D.Q.; Zhao, X.Y.; Wang, L.; Hu, Y.H.; Liu, J.T.; Cheng, H.; Yang, P.Y.; Shan, X.K.; Yan, Y.; et al. Childhood obesity affects adult metabolic syndrome and diabetes. Endocrine 2015, 50, 87–92. [Google Scholar] [CrossRef]
- Beilin, L.; Huang, R.C. Childhood obesity, hypertension, the metabolic syndrome and adult cardiovascular disease. Clin. Exp. Pharm. Physiol. 2008, 35, 409–411. [Google Scholar] [CrossRef]
- Burgess, J.A.; Walters, E.H.; Byrnes, G.B.; Jenkins, M.A.; Giles, G.G.; Abramson, M.J.; Hopper, J.L.; Dharmage, S.C. Childhood obesity predicts current incident asthma in adult women. Thorax 2005, 60, Ii32–Ii33. [Google Scholar]
- Loke, K.Y. Early Influences in Childhood Obesity Implications for Adult Metabolic Disease. Ann. Acad. Med. Singap. 2014, 43, 57–58. [Google Scholar]
- Wang, Z.Q.; Peng, Y.; Liu, M.N. Age Variation in the Association Between Obesity and Mortality in Adults. Obesity 2017, 25, 2137–2141. [Google Scholar] [CrossRef]
- Nolan, G.A.; McFarland, A.L.; Zajicek, J.M.; Waliczek, T.M. The Effects of Nutrition Education and Gardening on Attitudes, Preferences, and Knowledge of Minority Second to Fifth Graders in the Rio Grande Valley Toward Fruit and Vegetables. Horttechnology 2012, 22, 299–304. [Google Scholar] [CrossRef]
- Langellotto, G.A.; Gupta, A. Gardening Increases Vegetable Consumption in School-aged Children: A Meta-analytical Synthesis. Horttechnology 2012, 22, 430–445. [Google Scholar] [CrossRef]
- Rosenstock, I.M.; Strecher, V.J.; Becker, M.H. Social learning theory and the Health Belief Model. Health Educ. Q. 1988, 15, 175–183. [Google Scholar] [CrossRef] [PubMed]
- Ozer, E.J. The effects of school gardens on students and schools: Conceptualization and considerations for maximizing healthy development. Health Educ. Behav. 2007, 34, 846–863. [Google Scholar] [CrossRef] [PubMed]
- Christian, M.S.; Evans, C.E.L.; Conner, M.; Ransley, J.K.; Cade, J.E. Study protocol: Can a school gardening intervention improve children’s diets? BMC Public Health 2012, 12, 304. [Google Scholar] [CrossRef]
- Molitor, F.; Doerr, C. Dietary Behaviors and Obesity of Children From Low-Income Households by Gender of Caregiver and Child. Am. J. Health Promot. 2021, 35, 434–437. [Google Scholar] [CrossRef]
- Savage, J.S.; Fisher, J.O.; Birch, L.L. Parental influence on eating behavior: Conception to adolescence. J. Law Med. Ethics. 2007, 35, 22–34. [Google Scholar] [CrossRef]
- Davis, J.N.; Ventura, E.E.; Cook, L.T.; Gyllenhammer, L.E.; Gatto, N.M. LA Sprouts: A Gardening, Nutrition, and Cooking Intervention for Latino Youth Improves Diet and Reduces Obesity. J. Am. Diet. Assoc. 2011, 111, 1224–1230. [Google Scholar] [CrossRef]
- Christian, M.S.; El Evans, C.; Nykjaer, C.; Hancock, N.; Cade, J.E. Evaluation of the impact of a school gardening intervention on children’s fruit and vegetable intake: A randomised controlled trial. Int. J. Behav. Nutr. Phy. 2014, 11, 99. [Google Scholar] [CrossRef]
- Castro, D.C.; Samuels, M.; Harman, A.E. Growing Healthy Kids A Community Garden-Based Obesity Prevention Program. Am. J. Prev. Med. 2013, 44, S193–S199. [Google Scholar] [CrossRef]
- Ratcliffe, M.M.; Merrigan, K.A.; Rogers, B.L.; Goldberg, J.P. The effects of school garden experiences on middle school-aged students’ knowledge, attitudes, and behaviors associated with vegetable consumption. Health Promot. Pract. 2011, 12, 36–43. [Google Scholar] [CrossRef]
- Morgan, P.J.; Warren, J.M.; Lubans, D.R.; Saunders, K.L.; Quick, G.I.; Collins, C.E. The impact of nutrition education with and without a school garden on knowledge, vegetable intake and preferences and quality of school life among primary-school students. Public. Health Nutr. 2010, 13, 1931–1940. [Google Scholar] [CrossRef] [PubMed]
- Gatto, N.M.; Martinez, L.C.; Spruijt-Metz, D.; Davis, J.N. LA sprouts randomized controlled nutrition, cooking and gardening programme reduces obesity and metabolic risk in Hispanic/Latino youth. Pediatr. Obes. 2017, 12, 28–37. [Google Scholar] [CrossRef]
- Utter, J.; Denny, S.; Dyson, B. School gardens and adolescent nutrition and BMI: Results from a national, multilevel study. Prev. Med. 2016, 83, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Liang, J.; Lu, B.; Hao, L. Effect of resistance training on body composition, blood lipids and serum leptin of obese children. J. Chin. Sch. Health 2017, 38, 1379–1381+1384. [Google Scholar]
- Liang, J.a.L.H. Effects of high intensity intermittent exercise on body composition, blood pressure and serum Chemerin in obese children. J. Chin. Sch. Health 2018, 39, 1729–1732. [Google Scholar]
- Jeyanthi, S.; Arumugam, N.; Parasher, R.K. Effect of physical exercises on attention, motor skill and physical fitness in children with attention deficit hyperactivity disorder: A systematic review. Atten. Defic Hyperact. Disord. 2019, 11, 125–137. [Google Scholar] [CrossRef]
- Ng, Q.X.; Ho, C.Y.X.; Chan, H.W.; Yong, B.Z.J.; Yeo, W.S. Managing childhood and adolescent attention-deficit/hyperactivity disorder (ADHD) with exercise: A systematic review. Complement Ther. Med. 2017, 34, 123–128. [Google Scholar] [CrossRef] [PubMed]
- Contreras-Osorio, F.; Campos-Jara, C.; Martinez-Salazar, C.; Chirosa-Rios, L.; Martinez-Garcia, D. Effects of Sport-Based Interventions on Children’s Executive Function: A Systematic Review and Meta-Analysis. Brain Sci. 2021, 11, 755. [Google Scholar] [CrossRef]
- Ganjeh, P.; Meyer, T.; Hagmayer, Y.; Kuhnert, R.; Ravens-Sieberer, U.; von Steinbuechel, N.; Rothenberger, A.; Becker, A. Physical Activity Improves Mental Health in Children and Adolescents Irrespective of the Diagnosis of Attention Deficit Hyperactivity Disorder (ADHD)-A Multi-Wave Analysis Using Data from the KiGGS Study. Int. J. Environ. Res. Public Health 2021, 18, 2207. [Google Scholar] [CrossRef] [PubMed]
- Story, M. School-based approaches for preventing and treating obesity. Int. J. Obesity 1999, 23, S43–S51. [Google Scholar] [CrossRef]
- Flattum, C.; Friend, S.; Story, M.; Neumark-Sztainer, D. Evaluation of an Individualized Counseling Approach as Part of a Multicomponent School-Based Program to Prevent Weight-Related Problems among Adolescent Girls. J. Am. Diet. Assoc. 2011, 111, 1218–1223. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Basch, C.E. Physical Activity and the Achievement Gap Among Urban Minority Youth. J. Sch. Health 2011, 81, 626–634. [Google Scholar] [CrossRef]
- Rausch, J.C.; Berger-Jenkins, E.; Nieto, A.R.; McCord, M.; Meyer, D. Effect of a School-Based Intervention on Parents’ Nutrition and Exercise Knowledge, Attitudes, and Behaviors. Am. J. Health Educ. 2015, 46, 33–39. [Google Scholar] [CrossRef]
- Grasten, A. School-based physical activity interventions for children and youth: Keys for success. J. Sport Health Sci. 2017, 6, 290–291. [Google Scholar] [CrossRef]
- Messiah, S.E.; Arheart, K.L.; Lipshultz, S.E.; Miller, T.L. Body mass index, waist circumference, and cardiovascular risk factors in adolescents. J. Pediatr. 2008, 153, 845–850. [Google Scholar] [CrossRef]
- Messiah, S.E. BMI, waist circumference, and selected cardiovascular disease risk factors among preschool-age children. Obesity 2012, 20, 1942–1949. [Google Scholar] [CrossRef]
- Magnussen, C.G.; Koskinen, J.; Chen, W.; Thomson, R.; Schmidt, M.D.; Srinivasan, S.R.; Kivimaki, M.; Mattsson, N.; Kahonen, M.; Laitinen, T.; et al. Pediatric Metabolic Syndrome Predicts Adulthood Metabolic Syndrome, Subclinical Atherosclerosis, and Type 2 Diabetes Mellitus but Is No Better Than Body Mass Index Alone The Bogalusa Heart Study and the Cardiovascular Risk in Young Finns Study. Circulation 2010, 122, 1604–U1134. [Google Scholar] [CrossRef]
- Soltero, E.G.; Parker, N.H.; Mama, S.K.; Ledoux, T.A.; Lee, R.E. Lessons Learned from Implementing of Garden Education Program in Early Child Care. Health Promot. Pract. 2021, 22, 266–274. [Google Scholar] [CrossRef] [PubMed]
- Kegler, M.C.; Prakash, R.; Hermstad, A.; Williamson, D.; Anderson, K.; Haardorfer, R. Home gardening and associations with fruit and vegetable intake and BMI. Public Health Nutr. 2020, 23, 3417–3422. [Google Scholar] [CrossRef]
- Skelton, K.; Herbert, A.; Benjamin-Neelon, S.E. Garden-based interventions and early childhood health: A protocol for an umbrella review. Syst. Rev. 2019, 8, 310. [Google Scholar] [CrossRef]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; Grp, P.-P. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef]
- Hanbazaza, M.A.; Triador, L.; Ball, G.D.C.; Farmer, A.; Maximova, K.; Nation, A.F.; Willows, N.D. The Impact of School Gardening on Cree Children’s Knowledge and Attitudes toward Vegetables and Fruit. Can. J. Diet. Pract. Res. 2015, 76, 133–139. [Google Scholar] [CrossRef] [PubMed]
- Davis, J.N.; Martinez, L.C.; Spruijt-Metz, D.; Gatto, N.M. LA Sprouts: A 12-Week Gardening, Nutrition, and Cooking Randomized Control Trial Improves Determinants of Dietary Behaviors. J. Nutr. Educ. Behav. 2016, 48, 2–11.e11. [Google Scholar] [CrossRef] [PubMed]
- Landry, M.J.; Markowitz, A.K.; Asigbee, F.M.; Gatto, N.M.; Spruijt-Metz, D.; Davis, J.N. Cooking and Gardening Behaviors and Improvements in Dietary Intake in Hispanic/Latino Youth. Child. Obes. 2019, 15, 262–270. [Google Scholar] [CrossRef]
- Martinez, L.C.; Gatto, N.M.; Spruijt-Metz, D.; Davis, J.N. Design and methodology of the LA Sprouts nutrition, cooking and gardening program for Latino youth: A randomized controlled intervention. Contemp. Clin. Trials 2015, 42, 219–227. [Google Scholar] [CrossRef]
- Scherr, R.E.; Linnell, J.D.; Dharmar, M.; Beccarelli, L.M.; Bergman, J.J.; Briggs, M.; Brian, K.M.; Feenstra, G.; Hillhouse, J.C.; Keen, C.L.; et al. A Multicomponent, School-Based Intervention, the Shaping Healthy Choices Program, Improves Nutrition-Related Outcomes. J. Nutr. Educ. Behav. 2017, 49, 368–379.e1. [Google Scholar] [CrossRef] [PubMed]
- Gatto, N.M.; Ventura, E.E.; Cook, L.T.; Gyllenhammer, L.E.; Davis, J.N. LA Sprouts: A garden-based nutrition intervention pilot program influences motivation and preferences for fruits and vegetables in Latino youth. J. Acad. Nutr. Diet. 2012, 112, 913–920. [Google Scholar] [CrossRef] [PubMed]
- Davis, J.N.; Perez, A.; Asigbee, F.M.; Landry, M.J.; Vandyousefi, S.; Ghaddar, R.; Hoover, A.; Jeans, M.; Nikah, K.; Fischer, B.; et al. School-based gardening, cooking and nutrition intervention increased vegetable intake but did not reduce BMI: Texas sprouts—a cluster randomized controlled trial. Int. J. Behav. Nutr. Phy. 2021, 18, 18. [Google Scholar] [CrossRef] [PubMed]
- Evans, A.; Ranjit, N.; Hoelscher, D.; Jovanovic, C.; Lopez, M.; McIntosh, A.; Ory, M.; Whittlesey, L.; McKyer, L.; Kirk, A.; et al. Impact of school-based vegetable garden and physical activity coordinated health interventions on weight status and weight-related behaviors of ethnically diverse, low-income students: Study design and baseline data of the Texas, Grow! Eat! Go! (TGEG) cluster-randomized controlled trial. BMC Public. Health 2016, 16, 973. [Google Scholar] [CrossRef]
- Van den Berg, A.; Warren, J.L.; McIntosh, A.; Hoelscher, D.; Ory, M.G.; Jovanovic, C.; Lopez, M.; Whittlesey, L.; Kirk, A.; Walton, C.; et al. Impact of a Gardening and Physical Activity Intervention in Title 1 Schools: The TGEG Study. Child. Obes. 2020, 16, S44–S54. [Google Scholar] [CrossRef]
- Knapp, M.B.; Hall, M.T.; Mundorf, A.R.; Partridge, K.L.; Johnson, C.C. Perceptions of School-Based Kitchen Garden Programs in Low-Income, African American Communities. Health Promot. Pract. 2019, 20, 667–674. [Google Scholar] [CrossRef] [PubMed]
- Leuven, J.R.F.W.; Rutenfrans, A.H.M.; Dolfing, A.G.; Leuven, R.S.E.W. School gardening increases knowledge of primary school children on edible plants and preference for vegetables. Food Sci. Nutr. 2018, 6, 1960–1967. [Google Scholar] [CrossRef] [PubMed]
- Taylor, C.; Symon, E.B.; Dabbs, A.; Way, A.; Thompson, O.M. Assessing a School Gardening Program as an Integrated Component of a Pilot Farm-to-school Initiative Based in South Carolina. Horttechnology 2017, 27, 228–234. [Google Scholar] [CrossRef]
- Schreinemachers, P.; Bhattarai, D.R.; Subedi, G.D.; Acharya, T.P.; Chen, H.P.; Yang, R.Y.; Kashichhawa, N.K.; Dhungana, U.; Luther, G.C.; Mecozzi, M. Impact of school gardens in Nepal: A cluster randomised controlled trial. J. Dev. Effect. 2017, 9, 329–343. [Google Scholar] [CrossRef]
- Nishida, C.; Ko, G.T.; Kumanyika, S. Body fat distribution and noncommunicable diseases in populations: Overview of the 2008 WHO Expert Consultation on Waist Circumference and Waist-Hip Ratio. Eur. J. Clin. Nutr. 2010, 64, 2–5. [Google Scholar] [CrossRef]
- Blair, D. The Child in the Garden: An Evaluative Review of the Benefits of School Gardening. J. Environ. Educ. 2009, 40, 15–38. [Google Scholar] [CrossRef]
- Katz, D.L.; O’Connell, M.; Njike, V.Y.; Yeh, M.C.; Nawaz, H. Strategies for the prevention and control of obesity in the school setting: Systematic review and meta-analysis. Int. J. Obes. 2008, 32, 1780–1789. [Google Scholar] [CrossRef]
- Katz, D.L. School-Based Interventions for Health Promotion and Weight Control: Not Just Waiting on the World to Change. Annu. Rev. Publ. Health 2009, 30, 253–272. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Suarez, C.; Worley, A.; Grimmer-Somers, K.; Dones, V. School-Based Interventions on Childhood Obesity A Meta-Analysis. Am. J. Prev. Med. 2009, 37, 418–427. [Google Scholar] [CrossRef]
- McGuire, S. Institute of Medicine. 2012. Accelerating Progress in Obesity Prevention: Solving the Weight of the Nation. Washington, DC: The National Academies Press. Adv. Nutr. 2012, 3, 708–709. [Google Scholar] [CrossRef] [PubMed]
- Sa, G.D.; Neves, V.D.; Fraga, S.R.D.; Souza-Mello, V.; Barbosa-da-Silva, S. High-intensity interval training has beneficial effects on cardiac remodeling through local renin-angiotensin system modulation in mice fed high-fat or high-fructose diets. Life Sci. 2017, 189, 8–17. [Google Scholar] [CrossRef]
- Smith, K.E.; Mason, T.B.; O’Connor, S.M.; Wang, S.; Dzubur, E.; Crosby, R.D.; Wonderlich, S.A.; Salvy, S.J.; Feda, D.M.; Roemmich, J.N. Bi-Directional Associations Between Real-Time Affect and Physical Activity in Weight-Discordant Siblings. J. Pediatr. Psychol 2021, 46, 443–453. [Google Scholar] [CrossRef] [PubMed]
- Paduano, S.; Greco, A.; Borsari, L.; Salvia, C.; Tancredi, S.; Pinca, J.; Midili, S.; Tripodi, A.; Borella, P.; Marchesi, I. Physical and Sedentary Activities and Childhood Overweight/Obesity: A Cross-Sectional Study among First-Year Children of Primary Schools in Modena, Italy. Int. J. Environ. Res. Public Health 2021, 18, 3221. [Google Scholar] [CrossRef]
- Imierska, M.; Kurianiuk, A.; Blachnio-Zabielska, A. The Influence of Physical Activity on the Bioactive Lipids Metabolism in Obesity-Induced Muscle Insulin Resistance. Biomolecules 2020, 10, 1665. [Google Scholar] [CrossRef] [PubMed]
- Pysna, J.; Pysny, L.; Cihlar, D.; Petru, D.; Skopek, M. Effect of Physical Activity on Obesity in Second Stage Pupils of Elementary Schools in Northwest Bohemia. Sustainability 2020, 12, 42. [Google Scholar] [CrossRef]
- Smith, K.E.; O’Connor, S.M.; Mason, T.B.; Wang, S.; Dzubur, E.; Crosby, R.D.; Wonderlich, S.A.; Salvy, S.J.; Feda, D.M.; Roemmich, J.N. Associations between objective physical activity and emotional eating among adiposity-discordant siblings using ecological momentary assessment and accelerometers. Pediatr. Obes. 2021, 16, e12720. [Google Scholar] [CrossRef] [PubMed]
- Schwarzfischer, P.; Gruszfeld, D.; Stolarczyk, A.; Ferre, N.; Escribano, J.; Rousseaux, D.; Moretti, M.; Mariani, B.; Verduci, E.; Koletzko, B.; et al. Physical Activity and Sedentary Behavior From 6 to 11 Years. Pediatrics 2019, 143, e20180994. [Google Scholar] [CrossRef] [PubMed]
- Riso, E.M.; Kull, M.; Mooses, K.; Jurimae, J. Physical activity, sedentary time and sleep duration: Associations with body composition in 10-12-year-old Estonian schoolchildren. BMC Public Health 2018, 18, 496. [Google Scholar] [CrossRef] [PubMed]


| First Author | Year | Sample Size | Age | Interventions | Study Duration | Control Group | Outcomes | Results |
|---|---|---|---|---|---|---|---|---|
| Davis [22] | 2011 | 114 | 7–12 | Gardening | 12 weeks | No intervention | BMIz BMI WC | BMI↓ BMIz↓ WC↓ |
| Christian [23] | 2014 | 641 | 7–11 | Gardening | 72 weeks | No intervention | FVs | FVs↑ |
| Ratcliffe [25] | 2011 | 320 | 12 | Gardening | 13 weeks | No intervention | FVs | FVs - |
| Morgan [26] | 2010 | 127 | 11–12 | Gardening | 10 weeks | No intervention | FVs | FVs↑ |
| Gatto [27] | 2017 | 319 | 9–11 | Gardening | 12 weeks | No intervention | BMI BMIz WC | BMI↓ BMIz↓ WC↓ |
| Hanbazaza [47] | 2015 | 116 | 7–12 | Gardening | 72 weeks | No intervention | FVs | FVs↑ |
| Davis [48] | 2016 | 304 | 9–11 | Gardening | 12 weeks | No intervention | BMI | BMI↓ |
| Landry [49] | 2019 | 290 | 9–11 | Gardening | 12 weeks | No intervention | BMIz WC | BMIz↓ WC↓ |
| Martinez [50] | 2015 | 364 | 9–11 | Gardening | 12 weeks | No intervention | WC | WC↓ |
| Scherr [51] | 2018 | 409 | 9–10 | Gardening | 48 weeks | No intervention | BMIz | BMIz↓ |
| Gatto [52] | 2012 | 104 | 9–11 | Gardening | 12 weeks | No intervention | WC BMI | WC↓ BMI↓ |
| Davis [53] | 2021 | 3153 | 9–11 | Gardening | 36 weeks | No intervention | FVs BMIz BMI WC | FVs↑ BMIz↑ BMI↑ WC↑ |
| Evans [54] | 2016 | 1600 | 7–9 | Gardening and Physical Activity | 48 weeks | No intervention | others | |
| Alexandra [55] | 2020 | 1326 | 9–12 | Gardening and Physical Activity | 24 weeks | No intervention | others |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Qi, Y.; Hamzah, S.H.; Gu, E.; Wang, H.; Xi, Y.; Sun, M.; Rong, S.; Lin, Q. Is School Gardening Combined with Physical Activity Intervention Effective for Improving Childhood Obesity? A Systematic Review and Meta-Analysis. Nutrients 2021, 13, 2605. https://doi.org/10.3390/nu13082605
Qi Y, Hamzah SH, Gu E, Wang H, Xi Y, Sun M, Rong S, Lin Q. Is School Gardening Combined with Physical Activity Intervention Effective for Improving Childhood Obesity? A Systematic Review and Meta-Analysis. Nutrients. 2021; 13(8):2605. https://doi.org/10.3390/nu13082605
Chicago/Turabian StyleQi, Yufei, Sareena Hanim Hamzah, Erya Gu, Haonan Wang, Yue Xi, Minghui Sun, Siyu Rong, and Qian Lin. 2021. "Is School Gardening Combined with Physical Activity Intervention Effective for Improving Childhood Obesity? A Systematic Review and Meta-Analysis" Nutrients 13, no. 8: 2605. https://doi.org/10.3390/nu13082605
APA StyleQi, Y., Hamzah, S. H., Gu, E., Wang, H., Xi, Y., Sun, M., Rong, S., & Lin, Q. (2021). Is School Gardening Combined with Physical Activity Intervention Effective for Improving Childhood Obesity? A Systematic Review and Meta-Analysis. Nutrients, 13(8), 2605. https://doi.org/10.3390/nu13082605







