Dietary Management in Pediatric Patients with Crohn’s Disease
Abstract
:1. Introduction
2. Materials and Methods
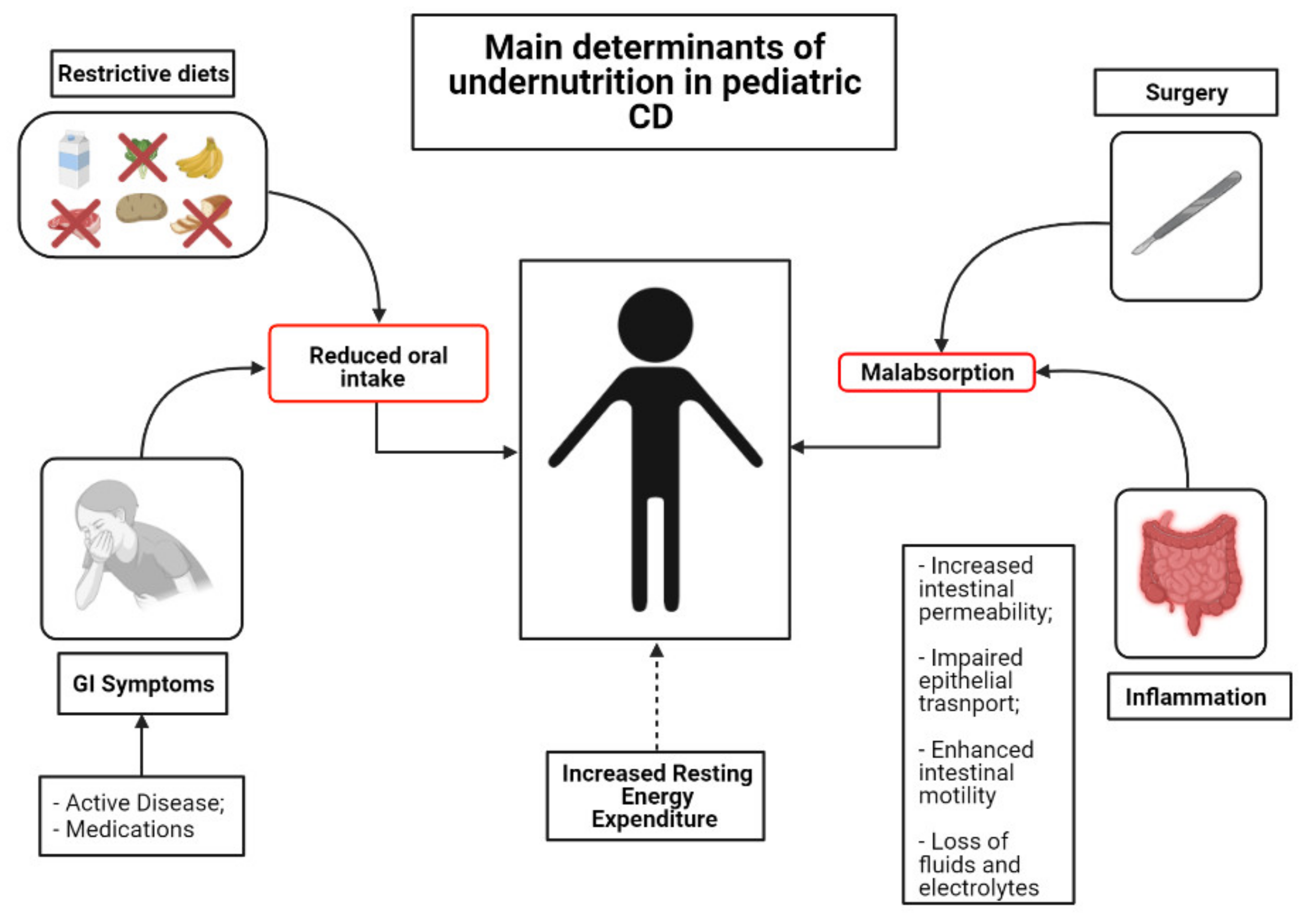
3. Mechanisms and Clinical Implications of Undernutrition in Children with CD
4. Nutritional Assessment and Supplementation
4.1. Macronutrients
4.2. Micronutrients
4.2.1. Iron
4.2.2. Vitamin B12 and Folate
4.2.3. Calcium and Vitamin D
4.3. Dietary Fiber
5. Nutritional Therapies
5.1. EEN
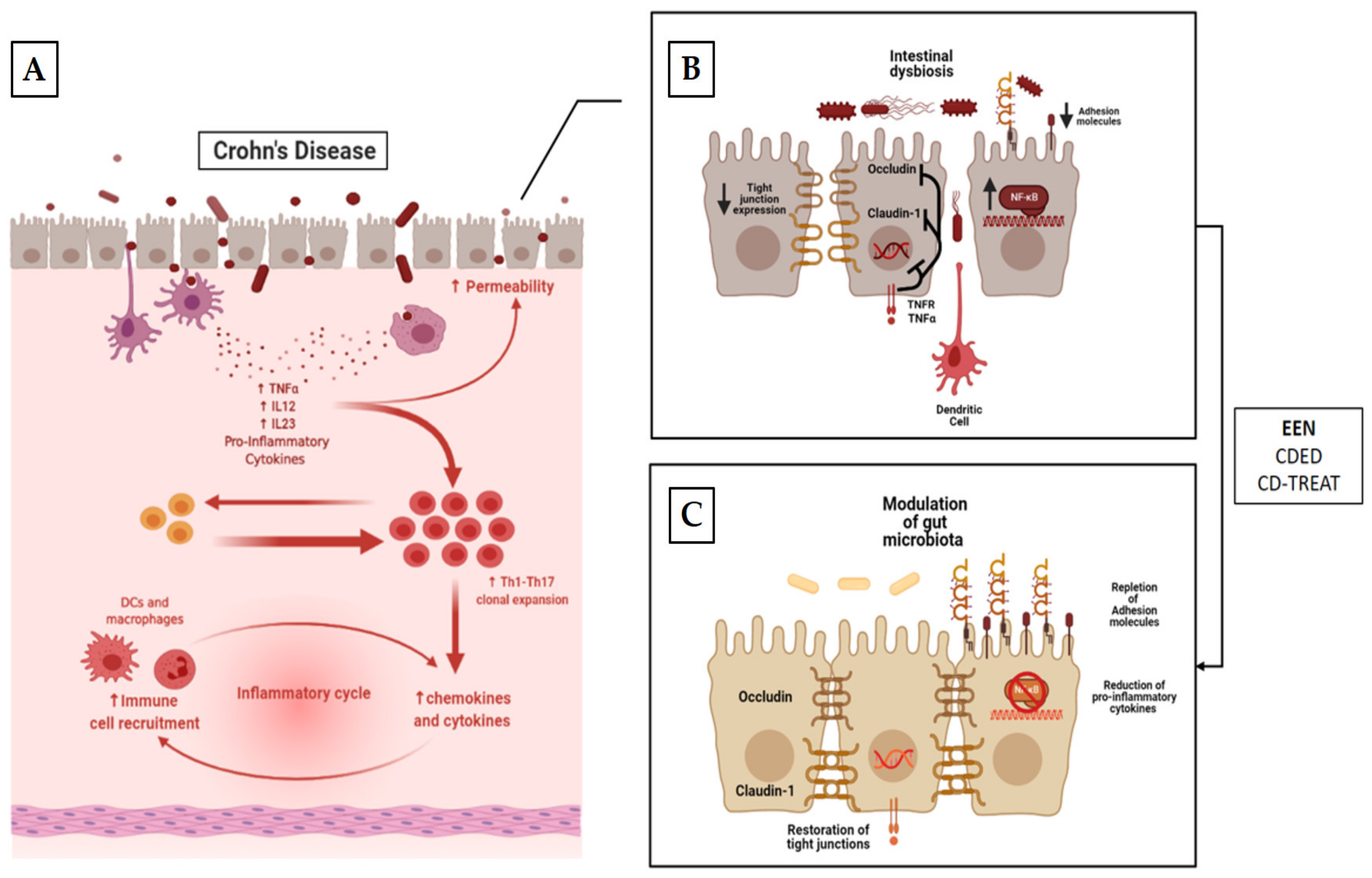
5.1.1. Mechanism of Action
5.1.2. EEN for Induction of Remission in CD
5.1.3. EEN for Preoperative Nutritional Optimization in Children with CD
5.1.4. EEN’s Effects on Body Mass Composition in Children with CD
5.2. Partial Enteral Nutrition (PEN) in CD
5.2.1. PEN for the Induction of Remission in CD
5.2.2. Maintenance of Enteral Nutrition (MEN) in CD
5.3. Food-Based Therapies in CD
5.3.1. Crohn’s Disease Exclusion Diet (CDED)
5.3.2. CD Treatment-with-Eating (CD-TREAT)
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fumery, M.; Pariente, B.; Sarter, H.; Savoye, G.; Spyckerelle, C.; Djeddi, D.; Mouterde, O.; Bouguen, G.; Ley, D.; Peneau, A.; et al. Long-term outcome of pediatric-onset Crohn’s disease: A population-based cohort study. Dig. Liver Dis. 2019, 51, 496–502. [Google Scholar] [CrossRef] [PubMed]
- Duricova, D.; Fumery, M.; Annese, V.; Lakatos, P.L.; Peyrin-Biroulet, L.; Gower-Rousseau, C. The natural history of Crohn’s disease in children: A review of population-based studies. Eur. J. Gastroenterol. Hepatol. 2017, 29, 10. [Google Scholar] [CrossRef] [PubMed]
- Ghione, S.; Sarter, H.; Fumery, M.; Armengol-Debeir, L.; Savoye, G.; Ley, D.; Spyckerelle, C.; Pariente, B.; Peyrin-Biroulet, L.; Turck, D.; et al. Dramatic Increase in Incidence of Ulcerative Colitis and Crohn’s Disease (1988–2011): A Population-Based Study of French Adolescents. Am. J. Gastroenterol. 2018, 113, 265–272. [Google Scholar] [CrossRef] [PubMed]
- E Roberts, S.; Thorne, K.; Thapar, N.; Broekaert, I.; A Benninga, M.; Dolinsek, J.; Mas, E.; Miele, E.; Orel, R.; Pienar, C.; et al. A Systematic Review and Meta-analysis of Paediatric Inflammatory Bowel Disease Incidence and Prevalence Across Europe. J. Crohn’s Colitis 2020, 14, 1119–1148. [Google Scholar] [CrossRef]
- Van Limbergen, J.; Russell, R.K.; Drummond, H.E.; Aldhous, M.C.; Round, N.K.; Nimmo, E.R.; Smith, L.; Gillett, P.M.; McGrogan, P.; Weaver, L.T.; et al. Definition of Phenotypic Characteristics of Childhood-Onset Inflammatory Bowel Disease. Gastroenterology 2008, 135, 1114–1122. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Duricova, D.; Burisch, J.; Jess, T.; Gower-Rousseau, C.; Lakatos, P.L. Age-related differences in presentation and course of inflammatory bowel disease: An update on the population-based literature. J. Crohn’s Colitis 2014, 8, 1351–1361. [Google Scholar] [CrossRef]
- Jakobsen, C.; Bartek, J., Jr.; Wewer, V.; Vind, I.; Munkholm, P.; Groen, R.; Paerregaard, A. Differences in phenotype and disease course in adult and paediatric inflammatory bowel disease—A population-based study: Differences between paediatric and adult IBD. Aliment. Pharmacol. Ther. 2011, 34, 1217–1224. [Google Scholar] [CrossRef]
- Kelsen, J.; Baldassano, R.N. Inflammatory bowel disease: The difference between children and adults. Inflamm. Bowel Dis. 2008, 14, S9–S11. [Google Scholar] [CrossRef]
- Torres, J.; Mehandru, S.; Colombel, J.-F.; Peyrin-Biroulet, L. Crohn’s disease. Lancet 2017, 389, 1741–1755. [Google Scholar] [CrossRef]
- Huang, H.; International Inflammatory Bowel Disease Genetics Consortium; Fang, M.; Jostins, L.; Mirkov, M.U.; Boucher, G.; Anderson, C.A.; Andersen, V.; Cleynen, I.; Cortes, A.; et al. Fine-mapping inflammatory bowel disease loci to single-variant resolution. Nat. Cell Biol. 2017, 547, 173–178. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, J.-H.; Wacholder, S.; Gail, M.H.; Peters, U.; Jacobs, K.B.; Chanock, S.J.; Chatterjee, N. Estimation of effect size distribution from genome-wide association studies and implications for future discoveries. Nat. Genet. 2010, 42, 570–575. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- A Peters, L.; Perrigoue, J.; Mortha, A.; Iuga, A.; Song, W.-M.; Neiman, E.M.; Llewellyn, S.R.; Di Narzo, A.; A Kidd, B.; E Telesco, S.; et al. A functional genomics predictive network model identifies regulators of inflammatory bowel disease. Nat. Genet. 2017, 49, 1437–1449. [Google Scholar] [CrossRef]
- Levine, A.; Boneh, R.S.; Wine, E. Evolving role of diet in the pathogenesis and treatment of inflammatory bowel diseases. Gut 2018, 67, 1726–1738. [Google Scholar] [CrossRef]
- Kaplan, G.G.; Windsor, J.W. The four epidemiological stages in the global evolution of inflammatory bowel disease. Nat. Rev. Gastroenterol. Hepatol. 2021, 18, 56–66. [Google Scholar] [CrossRef] [PubMed]
- De Filippo, C.; Cavalieri, D.; Di Paola, M.; Ramazzotti, M.; Poullet, J.B.; Massart, S.; Collini, S.; Pieraccini, G.; Lionetti, P. Impact of diet in shaping gut microbiota revealed by a comparative study in children from Europe and rural Africa. Proc. Natl. Acad. Sci. USA 2010, 107, 14691–14696. [Google Scholar] [CrossRef] [Green Version]
- De Filippo, C.; Di Paola, M.; Ramazzotti, M.; Albanese, D.; Pieraccini, G.; Banci, E.; Miglietta, F.; Cavalieri, D.; Lionetti, P. Diet, Environments, and Gut Microbiota. A Preliminary Investigation in Children Living in Rural and Urban Burkina Faso and Italy. Front. Microbiol. 2017, 8, 1979. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Desai, M.S.; Seekatz, A.M.; Koropatkin, N.M.; Kamada, N.; Hickey, C.A.; Wolter, M.; Pudlo, N.A.; Kitamoto, S.; Terrapon, N.; Muller, A.; et al. A Dietary Fiber-Deprived Gut Microbiota Degrades the Colonic Mucus Barrier and Enhances Pathogen Susceptibility. Cell 2016, 167, 1339–1353.e21. [Google Scholar] [CrossRef] [Green Version]
- Martinez-Medina, M.; Denizot, J.; Dreux, N.; Robin, F.; Billard, E.; Bonnet, R.; Barnich, N. Western diet induces dysbiosis with increased E coli in CEABAC10 mice, alters host barrier function favouring AIEC colonisation. Gut 2014, 63, 116–124. [Google Scholar] [CrossRef]
- Statovci, D.; Aguilera, M.; MacSharry, J.; Melgar, S. The Impact of Western Diet and Nutrients on the Microbiota and Immune Response at Mucosal Interfaces. Front. Immunol. 2017, 8, 838. [Google Scholar] [CrossRef] [Green Version]
- Dong, J.; Chen, Y.; Tang, Y.; Xu, F.; Yu, C.; Li, Y.; Pankaj, P.; Dai, N. Body Mass Index Is Associated with Inflammatory Bowel Disease: A Systematic Review and Meta-Analysis. PLoS ONE 2015, 10, e0144872. [Google Scholar] [CrossRef] [Green Version]
- Yerushalmy-Feler, A.; Galai, T.; Moran-Lev, H.; Ben-Tov, A.; Dali-Levy, M.; Weintraub, Y.; Amir, A.; Cohen, S. BMI in the lower and upper quartiles at diagnosis and at 1-year follow-up is significantly associated with higher risk of disease exacerbation in pediatric inflammatory bowel disease. Eur. J. Nucl. Med. Mol. Imaging 2021, 180, 21–29. [Google Scholar] [CrossRef]
- Nguyen, G.C.; Munsell, M.; Harris, M.L. Nationwide prevalence and prognostic significance of clinically diagnosable protein-calorie malnutrition in hospitalized inflammatory bowel disease patients. Inflamm. Bowel Dis. 2008, 14, 1105–1111. [Google Scholar] [CrossRef] [PubMed]
- Van Rheenen, P.F.; Aloi, M.; Assa, A.; Bronsky, J.; Escher, J.C.; Fagerberg, U.L.; Gasparetto, M.; Gerasimidis, K.; Griffiths, A.; Henderson, P.; et al. The Medical Management of Paediatric Crohn’s Disease: An ECCO-ESPGHAN Guideline Update. J. Crohn’s Colitis 2021, 15, 171–194. [Google Scholar] [CrossRef] [PubMed]
- Kugathasan, S.; A Denson, L.; Walters, T.D.; Kim, M.-O.; Marigorta, U.M.; Schirmer, M.; Mondal, K.; Liu, C.; Griffiths, A.; Noe, J.D.; et al. Prediction of complicated disease course for children newly diagnosed with Crohn’s disease: A multicentre inception cohort study. Lancet 2017, 389, 1710–1718. [Google Scholar] [CrossRef] [Green Version]
- Ford, A.C.; Peyrin-Biroulet, L. Opportunistic Infections With Anti-Tumor Necrosis Factor-α Therapy in Inflammatory Bowel Disease: Meta-Analysis of Randomized Controlled Trials. Am. J. Gastroenterol. 2013, 108, 1268–1276. [Google Scholar] [CrossRef]
- Magro, F.; Peyrin-Biroulet, L.; Sokol, H.; Aldeger, X.; Costa, A.; Higgins, P.D.; Joyce, J.C.; Katsanos, K.H.; Lopez, A.; De Xaxars, T.M.; et al. Extra-intestinal malignancies in inflammatory bowel disease: Results of the 3rd ECCO Pathogenesis Scientific Workshop (III). J. Crohn’s Colitis 2014, 8, 31–44. [Google Scholar] [CrossRef] [Green Version]
- Cohen-Dolev, N.; Sladek, M.; Hussey, S.; Turner, D.; Veres, G.; Koletzko, S.; Levine, A. Differences in Outcomes Over Time with Exclusive Enteral Nutrition Compared With Steroids in Children With Mild to Moderate Crohn’s Disease: Results From the GROWTH CD Study. J. Crohn’s Colitis 2018, 12, 306–312. [Google Scholar] [CrossRef] [Green Version]
- Grover, Z.; Lewindon, P. Two-Year Outcomes After Exclusive Enteral Nutrition Induction Are Superior to Corticosteroids in Pediatric Crohn’s Disease Treated Early with Thiopurines. Dig. Dis. Sci. 2015, 60, 3069–3074. [Google Scholar] [CrossRef] [PubMed]
- Scarallo, L. Mucosal and Histologic Healing in children with Inflammatory Bowel Disease treated with anti-Tumor Necrosis Factor-alpha. J. Pediatr. Gastroenterol. Nutr. 2021, 72, 728–735. [Google Scholar] [CrossRef] [PubMed]
- Qiu, Y.; Chen, B.-L.; Mao, R.; Zhang, S.-H.; He, Y.; Zeng, Z.-R.; Ben-Horin, S.; Chen, M.-H. Systematic review with meta-analysis: Loss of response and requirement of anti-TNFα dose intensification in Crohn’s disease. J. Gastroenterol. 2017, 52, 535–554. [Google Scholar] [CrossRef] [PubMed]
- Rubio, A. The efficacy of exclusive nutritional therapy in paediatric Crohn’s disease, comparing fractionated oral vs. continuous enteral feeding: Oral vs. continuous enteral nutrition for CD in children. Aliment. Pharmacol. Ther. 2011, 33, 1332–1339. [Google Scholar] [CrossRef] [PubMed]
- Gerasimidis, K. Impact of exclusive enteral nutrition on body composition and circulating micronutrients in plasma and erythrocytes of children with active Crohn’s disease. Inflamm. Bowel Dis. 2012, 18, 1672–1681. [Google Scholar] [CrossRef]
- Stewart, M.; Day, A.S.; Otley, A. Physician Attitudes and Practices of Enteral Nutrition as Primary Treatment of Paediatric Crohn Disease in North America. J. Pediatr. Gastroenterol. Nutr. 2011, 52, 38–42. [Google Scholar] [CrossRef] [PubMed]
- Levine, A.; Wine, E.; Assa, A.; Boneh, R.S.; Shaoul, R.; Kori, M.; Cohen, S.; Peleg, S.; Shamaly, H.; On, A.; et al. Crohn’s Disease Exclusion Diet Plus Partial Enteral Nutrition Induces Sustained Remission in a Randomized Controlled Trial. Gastroenterology 2019, 157, 440–450.e8. [Google Scholar] [CrossRef] [Green Version]
- Svolos, V.; Hansen, R.; Nichols, B.; Quince, C.; Ijaz, U.Z.; Papadopoulou, R.T.; Edwards, C.A.; Watson, D.; Alghamdi, A.; Brejnrod, A.; et al. Treatment of Active Crohn’s Disease With an Ordinary Food-based Diet That Replicates Exclusive Enteral Nutrition. Gastroenterology 2019, 156, 1354–1367.e6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hartman, C.; Eliakim, R.; Shamir, R. Nutritional status and nutritional therapy in inflammatory bowel diseases. World J. Gastroenterol. 2009, 15, 2570–2578. [Google Scholar] [CrossRef] [PubMed]
- Goh, J.; O’Morain, C.A. Nutrition and adult inflammatory bowel disease. Aliment. Pharm. Ther. 2003, 14, 307–320. [Google Scholar] [CrossRef]
- Balestrieri, P.; Ribolsi, M.; Guarino, M.P.L.; Emerenziani, S.; Altomare, A.; Cicala, M. Nutritional Aspects in Inflammatory Bowel Diseases. Nutrients 2020, 12, 372. [Google Scholar] [CrossRef] [Green Version]
- Sanderson, I.R. Growth problems in children with IBD. Nat. Rev. Gastroenterol. Hepatol. 2014, 11, 601–610. [Google Scholar] [CrossRef] [PubMed]
- Vasudevan, A.; Parthasarathy, N.; Con, D.; Nicolaides, S.; Apostolov, R.; Chauhan, A.; Bishara, M.; Luber, R.P.; Joshi, N.; Wan, A.; et al. Thiopurines vs methotrexate: Comparing tolerability and discontinuation rates in the treatment of inflammatory bowel disease. Aliment. Pharmacol. Ther. 2020, 52, 1174–1184. [Google Scholar] [CrossRef] [PubMed]
- Jowett, S.L.; Seal, C.J.; Phillips, E.; Gregory, W.; Barton, J.; Welfare, M.R. Dietary beliefs of people with ulcerative colitis and their effect on relapse and nutrient intake. Clin. Nutr. 2004, 23, 161–170. [Google Scholar] [CrossRef]
- Guerreiro, C.S.; Cravo, M.; Costa, A.R.; Miranda, A.; Tavares, L.; Moura-Santos, P.; Marquesvidal, P.; Leitão, C.N. A Comprehensive Approach to Evaluate Nutritional Status in Crohn’s Patients in the Era of Biologic Therapy: A Case-Control Study. Am. J. Gastroenterol. 2007, 102, 2551–2556. [Google Scholar] [CrossRef]
- Martini, E.; Krug, S.M.; Siegmund, B.; Neurath, M.F.; Becker, C. Mend Your Fences. Cell. Mol. Gastroenterol. Hepatol. 2017, 4, 33–46. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miele, E.; Shamir, R.; Aloi, M.; Assa, A.; Braegger, C.; Bronsky, J.; de Ridder, L.; Escher, J.C.; Hojsak, I.; Kolaček, S.; et al. Nutrition in Pediatric Inflammatory Bowel Disease: A Position Paper on Behalf of the Porto Inflammatory Bowel Disease Group of the European Society of Pediatric Gastroenterology, Hepatology and Nutrition. J. Pediatr. Gastroenterol. Nutr. 2018, 66, 687–708. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Varille, V.; Cézard, J.P.; De Lagausie, P.; Bellaiche, M.; Tounian, P.; Besnard, M.; Faure, C.; Aigrain, Y.; Girardet, J.P.; Navarro, J. Resting Energy Expenditure before and after Surgical Resection of Gut Lesions in Pediatric Crohn’s Disease. J. Pediatr. Gastroenterol. Nutr. 1996, 23, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Wiskin, A.E.; Wootton, S.A.; Culliford, D.J.; Afzal, N.A.; Jackson, A.A.; Beattie, R.M. Impact of disease activity on resting energy expenditure in children with inflammatory bowel disease. Clin. Nutr. 2009, 28, 652–656. [Google Scholar] [CrossRef]
- A Sentongo, T.; Semeao, E.J.; A Piccoli, D.; A Stallings, V.; Zemel, B.S. Growth, Body Composition, and Nutritional Status in Children and Adolescents With Crohn’s Disease. J. Pediatr. Gastroenterol. Nutr. 2000, 31, 33–40. [Google Scholar] [CrossRef]
- Kanof, M.E.; Lake, A.M.; Bayless, T.M. Decreased Height Velocity in Children and Adolescents Before the Diagnosis of Crohn’s Disease. Gastroenterology 1988, 95, 1523–1527. [Google Scholar] [CrossRef]
- Vasseur, F.; Gower-Rousseau, C.; Vernier-Massouille, G.; Dupas, J.L.; Merle, V.; Merlin, B.; Lerebours, E.; Savoye, G.; Salomez, J.L.; Cortot, A.; et al. Nutritional Status and Growth in Pediatric Crohn’s Disease: A Population-Based Study. Am. J. Gastroenterol. 2010, 105, 1893–1900. [Google Scholar] [CrossRef]
- Pfefferkorn, M.; Burke, G.; Griffiths, A.; Markowitz, J.; Rosh, J.; Mack, D.; Otley, A.; Kugathasan, S.; Evans, J.; Bousvaros, A.; et al. Growth Abnormalities Persist in Newly Diagnosed Children With Crohn Disease Despite Current Treatment Paradigms. J. Pediatr. Gastroenterol. Nutr. 2009, 48, 168–174. [Google Scholar] [CrossRef]
- Lee, J.; Escher, J.; Shuman, M.; Forbes, P.; Delemarre, L.; Harr, B.; Kruijer, M.; Moret, M.; Allende-Richter, S.; Grand, R. Final adult height of children with inflammatory bowel disease is predicted by parental height and patient minimum height Z-score. Inflamm. Bowel Dis. 2010, 16, 1669–1677. [Google Scholar] [CrossRef] [PubMed]
- Yerushalmy-Feler, A.; Ben-Tov, A.; Weintraub, Y.; Amir, A.; Galai, T.; Moran-Lev, H.; Cohen, S. High and low body mass index may predict severe disease course in children with inflammatory bowel disease. Scand. J. Gastroenterol. 2018, 53, 708–713. [Google Scholar] [CrossRef] [PubMed]
- Thangarajah, D.; Hyde, M.J.; Konteti, V.K.S.; Santhakumaran, S.; Frost, G.; Fell, J.M.E. Systematic review: Body composition in children with inflammatory bowel disease. Aliment. Pharmacol. Ther. 2015, 42, 142–157. [Google Scholar] [CrossRef] [Green Version]
- Houttu, N.; Kalliomäki, M.; Grönlund, M.-M.; Niinikoski, H.; Nermes, M.; Laitinen, K. Body composition in children with chronic inflammatory diseases: A systematic review. Clin. Nutr. 2020, 39, 2647–2662. [Google Scholar] [CrossRef] [PubMed]
- Ward, L.M.; Ma, J.; Rauch, F.; Benchimol, E.I.; Hay, J.; Leonard, M.B.; Matzinger, M.A.; Shenouda, N.; Lentle, B.; Cosgrove, H.; et al. Musculoskeletal health in newly diagnosed children with Crohn’s disease. Osteoporos. Int. 2017, 28, 3169–3177. [Google Scholar] [CrossRef]
- Sylvester, F.A.; Leopold, S.; Lincoln, M.; Hyams, J.S.; Griffiths, A.M.; Lerer, T. A Two-Year Longitudinal Study of Persistent Lean Tissue Deficits in Children With Crohn’s Disease. Clin. Gastroenterol. Hepatol. 2009, 7, 452–455. [Google Scholar] [CrossRef]
- Werkstetter, K.J.; Ullrich, J.; Schatz, S.B.; Prell, C.; Koletzko, B.; Koletzko, S. Lean body mass, physical activity and quality of life in paediatric patients with inflammatory bowel disease and in healthy controls. J. Crohn’s Coliti 2012, 6, 665–673. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wolfe, R.R. The underappreciated role of muscle in health and disease. Am. J. Clin. Nutr. 2006, 84, 475–482. [Google Scholar] [CrossRef]
- Gerasimidis, K.; McGrogan, P.; Edwards, C.A. The aetiology and impact of malnutrition in paediatric inflammatory bowel disease. J. Hum. Nutr. Diet. 2011, 24, 313–326. [Google Scholar] [CrossRef]
- Holt, D.Q.; Varma, P.; Strauss, B.J.G.; Rajadurai, A.S.; Moore, G.T. Low muscle mass at initiation of anti-TNF therapy for inflammatory bowel disease is associated with early treatment failure: A retrospective analysis. Eur. J. Clin. Nutr. 2017, 71, 773–777. [Google Scholar] [CrossRef]
- Murthy, S.K.; Begum, J.; I Benchimol, E.; Bernstein, C.N.; Kaplan, G.G.; McCurdy, J.D.; Singh, H.; Targownik, L.; Taljaard, M. Introduction of anti-TNF therapy has not yielded expected declines in hospitalisation and intestinal resection rates in inflammatory bowel diseases: A population-based interrupted time series study. Gut 2020, 69, 274–282. [Google Scholar] [CrossRef] [PubMed]
- Alves, A.; Panis, Y.; Bouhnik, Y.; Pocard, M.; Vicaut, E.; Valleur, P. Risk Factors for Intra-Abdominal Septic Complications After a First Ileocecal Resection for Crohn’s Disease: A Multivariate Analysis in 161 Consecutive Patients. Dis. Colon Rectum 2007, 50, 331–336. [Google Scholar] [CrossRef] [PubMed]
- Ryan, E. Sarcopenia and Inflammatory Bowel Disease: A Systematic Review. Inflamm. Bowel Dis. 2019, 25, 67–73. [Google Scholar] [CrossRef]
- Limdi, J.K.; Aggarwal, D.; McLaughlin, J.T. Dietary Practices and Beliefs in Patients with Inflammatory Bowel Disease. Inflamm. Bowel Dis. 2016, 22, 164–170. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hartman, C.; Marderfeld, L.; Davidson, K.; Mozer-Glassberg, Y.; Poraz, I.; Silbermintz, A.; Zevit, N.; Shamir, R. Food Intake Adequacy in Children and Adolescents With Inflammatory Bowel Disease. J. Pediatr. Gastroenterol. Nutr. 2016, 63, 437–444. [Google Scholar] [CrossRef]
- Thomas, A.G.; Miller, V.; Taylor, F.; Maycock, P.; Scrimgeour, C.M.; Rennie, M.J. Whole body protein turnover in childhood Crohn’s disease. Gut 1992, 33, 675–677. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Steiner, S.J.; Noe, J.D.; Denne, S.C. Corticosteroids Increase Protein Breakdown and Loss in Newly Diagnosed Pediatric Crohn Disease. Pediatr. Res. 2011, 70, 484–488. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Steiner, S.J.; Pfefferkorn, M.D.; Fitzgerald, J.F.; Denne, S.C. Protein and energy metabolism response to the initial dose of infliximab in children with Crohn’s disease. Inflamm. Bowel Dis. 2007, 13, 737–744. [Google Scholar] [CrossRef]
- Wiskin, A.E.; Fleming, B.J.; Wootton, S.A.; Beattie, R.M. Anaemia and iron deficiency in children with inflammatory bowel disease. J. Crohn’s Colitis 2012, 6, 687–691. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goyal, A.; Zheng, Y.; Albenberg, L.G.; Stoner, N.L.; Hart, L.; Alkhouri, R.; Hampson, K.; Ali, S.; Cho-Dorado, M.; Goyal, R.K.; et al. Anemia in Children With Inflammatory Bowel Disease: A Position Paper by the IBD Committee of the North American Society of Pediatric Gastroenterology, Hepatology and Nutrition. J. Pediatr. Gastroenterol. Nutr. 2020, 71, 563–582. [Google Scholar] [CrossRef] [PubMed]
- Pels, L.P.; Van de Vijver, E.; Waalkens, H.J.; Uitentuis, J.; Jong, G.G.-D.; van Overbeek, L.A.; Norbruis, O.F.; Rings, E.H.; van Rheenen, P.F. Slow Hematological Recovery in Children With IBD-associated Anemia in Cases of “Expectant Management. ” J. Pediatr. Gastroenterol. Nutr. 2010, 51, 708–713. [Google Scholar] [CrossRef] [PubMed]
- Gerasimidis, K. The Epidemiology of Anemia in Pediatric Inflammatory Bowel Disease: Prevalence and Associated Factors at Diagnosis and Follow-up and the Impact of Exclusive Enteral Nutrition. Inflamm. Bowel Dis. 2013, 19, 2411–2422. [Google Scholar] [CrossRef] [PubMed]
- Goodhand, J.R.; Kamperidis, N.; Rao, A.; Laskaratos, F.; McDermott, A.; Wahed, M.; Naik, S.; Croft, N.M.; Lindsay, J.O.; Sanderson, I.R.; et al. Prevalence and management of anemia in children, adolescents, and adults with inflammatory bowel disease. Inflamm. Bowel Dis. 2012, 18, 513–519. [Google Scholar] [CrossRef] [PubMed]
- Sjöberg, D. Anemia in a population-based IBD cohort (ICURE): Still high prevalence after 1 year, especially among pediatric patients. Inflamm. Bowel Dis. 2014, 20, 2266–2270. [Google Scholar] [CrossRef]
- Carvalho, F.S.G.; de Medeiros, I.A.; Antunes, H. Prevalence of iron deficiency anemia and iron deficiency in a pediatric population with inflammatory bowel disease. Scand. J. Gastroenterol. 2017, 52, 1099–1103. [Google Scholar] [CrossRef] [PubMed]
- Stein, J.; Hartmann, F.; Dignass, A.U. Diagnosis and management of iron deficiency anemia in patients with IBD. Nat. Rev. Gastroenterol. Hepatol. 2010, 7, 599–610. [Google Scholar] [CrossRef] [PubMed]
- Aljomah, G.; Baker, S.S.; Schmidt, K.; Alkhouri, R.; Kozielski, R.; Zhu, L.; Baker, R.D. Anemia in Pediatric Inflammatory Bowel Disease. J. Pediatr. Gastroenterol. Nutr. 2018, 67, 351–355. [Google Scholar] [CrossRef]
- Tolkien, Z.; Stecher, L.; Mander, A.P.; Pereira, D.I.A.; Powell, J.J. Ferrous Sulfate Supplementation Causes Significant Gastrointestinal Side-Effects in Adults: A Systematic Review and Meta-Analysis. PLoS ONE 2015, 10, e0117383. [Google Scholar] [CrossRef] [Green Version]
- Gargallo-Puyuelo, C.J.; Alfambra, E.; García-Erce, J.A.; Gomollon, F. Iron Treatment May Be Difficult in Inflammatory Diseases: Inflammatory Bowel Disease as a Paradigm. Nutrients 2018, 10, 1959. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jaeggi, T.; Kortman, G.A.M.; Moretti, D.; Chassard, C.; Holding, P.; Dostal, A.; Boekhorst, J.; Timmerman, H.M.; Swinkels, D.W.; Tjalsma, H.; et al. Iron fortification adversely affects the gut microbiome, increases pathogen abundance and induces intestinal inflammation in Kenyan infants. Gut 2015, 64, 731–742. [Google Scholar] [CrossRef]
- Weiss, G. Dietary iron supplementation: A proinflammatory attack on the intestine? Gut 2014, 64, 696–697. [Google Scholar] [CrossRef] [PubMed]
- Cummings, J.F.; Fraser, A.; Stansfield, C.; Beales, I.; Sebastian, S.; Hoque, S. Ferric maltol Real-world Effectiveness Study in Hospital practice (FRESH): Clinical characteristics and outcomes of patients with inflammatory bowel disease receiving ferric maltol for iron-deficiency anaemia in the UK. BMJ Open Gastroenterol. 2021, 8, e000530. [Google Scholar] [CrossRef]
- Lee, T.; Clavel, T.; Smirnov, K.; Schmidt, A.; Lagkouvardos, I.; Walker, A.; Lucio, M.; Michalke, B.; Schmitt-Kopplin, P.; Fedorak, R.; et al. Oral versus intravenous iron replacement therapy distinctly alters the gut microbiota and metabolome in patients with IBD. Gut 2016, 66, 863–871. [Google Scholar] [CrossRef] [PubMed]
- Rampton, D.S.; Goodhand, J.R.; Joshi, N.M.; Karim, A.-B.; Koodun, Y.; Barakat, F.M.; Macken, L.; Ward, D.G.; Iqbal, T.H.; Epstein, J.; et al. Oral Iron Treatment Response and Predictors in Anaemic Adolescents and Adults with IBD: A Prospective Controlled Open-Label Trial. J. Crohn’s Colitis 2016, 11, 706–715. [Google Scholar] [CrossRef] [PubMed]
- Chertow, G.M.; Mason, P.D.; Vaage-Nilsen, O.; Ahlmén, J. Update on adverse drug events associated with parenteral iron. Nephrol. Dial. Transplant. 2006, 21, 378–382. [Google Scholar] [CrossRef] [PubMed]
- Mamula, P.; Piccoli, D.A.; Peck, S.N.; Markowitz, J.E.; Baldassano, R.N. Total Dose Intravenous Infusion of Iron Dextran for Iron-Deficiency Anemia in Children With Inflammatory Bowel Disease. J. Pediatr. Gastroenterol. Nutr. 2002, 34, 286–290. [Google Scholar] [CrossRef]
- Stein, R.E.; Plantz, K.; Maxwell, E.C.; Mamula, P.; Baldassano, R.N. Intravenous Iron Sucrose for Treatment of Iron Deficiency Anemia in Pediatric Inflammatory Bowel Disease. J. Pediatr. Gastroenterol. Nutr. 2018, 66, e51–e55. [Google Scholar] [CrossRef]
- Papadopoulos, M. Safety and efficacy of parenteral iron in children with inflammatory bowel disease: Safety and efficacy of parenteral iron in children with IBD. Br. J. Clin. Pharmacol. 2018, 84, 694–699. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carman, N.; Muir, R.; Lewindon, P. Ferric carboxymaltose in the treatment of iron deficiency in pediatric inflammatory bowel disease. Transl. Pediatr. 2019, 8, 28–34. [Google Scholar] [CrossRef] [PubMed]
- Powers, J.M.; Shamoun, M.; McCavit, T.L.; Adix, L.; Buchanan, G.R. Intravenous Ferric Carboxymaltose in Children with Iron Deficiency Anemia Who Respond Poorly to Oral Iron. J. Pediatr. 2017, 180, 212–216. [Google Scholar] [CrossRef] [PubMed]
- Savage, D.G.; Lindenbaum, J.; Stabler, S.P.; Allen, R.H. Sensitivity of serum methylmalonic acid and total homocysteine determinations for diagnosing cobalamin and folate deficiencies. Am. J. Med. 1994, 96, 239–246. [Google Scholar] [CrossRef]
- Battat, R.; Kopylov, U.; Szilagyi, A.; Saxena, A.; Rosenblatt, D.S.; Warner, M.; Bessissow, T.; Seidman, E.; Bitton, A. Vitamin B12 Deficiency in Inflammatory Bowel Disease. Inflamm. Bowel Dis. 2014, 20, 1120–1128. [Google Scholar] [CrossRef]
- Fritz, J.; Walia, C.; Elkadri, A.; Pipkorn, R.; Dunn, R.K.; Sieracki, R.; Goday, P.S.; Cabrera, J.M. A Systematic Review of Micronutrient Deficiencies in Pediatric Inflammatory Bowel Disease. Inflamm. Bowel Dis. 2018, 25, 445–459. [Google Scholar] [CrossRef] [PubMed]
- Yakut, M.; Üstün, Y.; Kabaçam, G.; Soykan, I. Serum vitamin B12 and folate status in patients with inflammatory bowel diseases. Eur. J. Intern. Med. 2010, 21, 320–323. [Google Scholar] [CrossRef]
- Vagianos, K.; Bernstein, C.N. Homocysteinemia and B vitamin status among adult patients with inflammatory bowel disease: A one-year prospective follow-up study. Inflamm. Bowel Dis. 2012, 18, 718–724. [Google Scholar] [CrossRef] [PubMed]
- Bermejo, F.; Algaba, A.; Guerra, I.; Chaparro, M.; De-La-Poza, G.; Valer, P.; Piqueras, B.; Bermejo, A.; García-Alonso, J.; Pérez, M.-J.; et al. Should we monitor vitamin B12and folate levels in Crohn’s disease patients? Scand. J. Gastroenterol. 2013, 48, 1272–1277. [Google Scholar] [CrossRef] [PubMed]
- Lopes, M.B.; Rocha, R.; Lyra, A.C.; Oliveira, V.R.; Coqueiro, F.G.; Almeida, N.S.; Valois, S.S.; Santana, G.O. Restriction of dairy products; a reality in inflammatory bowel disease patients. Nutr. Hosp. 2014, 29, 575–581. [Google Scholar] [CrossRef]
- Filippi, J.; Al-Jaouni, R.; Wiroth, J.-B.; Hébuterne, X.; Schneider, S.M. Nutritional deficiencies in patients with Crohn’s disease in remission. Inflamm. Bowel Dis. 2006, 12, 185–191. [Google Scholar] [CrossRef] [PubMed]
- Paganelli, M.; Albanese, C.V.; Borrelli, O.; Civitelli, F.; Canitano, N.; Viola, F.; Passariello, R.; Cucchiara, S. Inflammation Is The Main Determinant of Low Bone Mineral Density in Pediatric Inflammatory Bowel Disease. Inflamm. Bowel Dis. 2007, 13, 416–423. [Google Scholar] [CrossRef]
- Lopes, L.H.C.; Sdepanian, V.L.; Szejnfeld, V.L.; De Morais, M.B.; Fagundes-Neto, U. Risk Factors for Low Bone Mineral Density in Children and Adolescents with Inflammatory Bowel Disease. Dig. Dis. Sci. 2008, 53, 2746–2753. [Google Scholar] [CrossRef]
- Nobile, S.; Grand, R.J.; Pappa, H.M. Risk factors for low bone mineral density in pediatric inflammatory bowel disease: The positive role of physical activity. Eur. J. Gastroenterol. Hepatol. 2018, 30, 471–476. [Google Scholar] [CrossRef] [PubMed]
- Sigurdsson, G.V.; Schmidt, S.; Mellström, D.; Ohlsson, C.; Kindblom, J.M.; Lorentzon, M.; Saalman, R. Bone Mass Development from Childhood into Young Adulthood in Patients with Childhood-onset Inflammatory Bowel Disease. Inflamm. Bowel Dis. 2017, 23, 2215–2226. [Google Scholar] [CrossRef] [Green Version]
- Guz-Mark, A.; Rinawi, F.; Egotubov, O.; Shimon, I.; Shamir, R.; Assa, A. Pediatric-onset inflammatory bowel disease poses risk for low bone mineral density at early adulthood. Dig. Liver Dis. 2017, 49, 639–642. [Google Scholar] [CrossRef] [PubMed]
- A Sentongo, T.; Semaeo, E.J.; Stettler, N.; A Piccoli, D.; A Stallings, V.; Zemel, B.S. Vitamin D status in children, adolescents, and young adults with Crohn disease. Am. J. Clin. Nutr. 2002, 76, 1077–1081. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Levin, A.D.; Wadhera, V.; Leach, S.T.; Woodhead, H.J.; Lemberg, D.A.; Mendoza-Cruz, A.C.; Day, A.S. Vitamin D Deficiency in Children with Inflammatory Bowel Disease. Dig. Dis. Sci. 2011, 56, 830–836. [Google Scholar] [CrossRef]
- Lee, R.; Maltz, R.M.; Crandall, W.V.; Plogsted, S.W.; Shaikhkhalil, A.K.; Bowden, S.A.; Mezoff, E.A. Single High-dose Vitamin D3 Supplementation in Pediatric Patients With Inflammatory Bowel Disease and Hypovitaminosis D. J. Pediatr. Gastroenterol. Nutr. 2020, 70, e77–e80. [Google Scholar] [CrossRef] [PubMed]
- Alshahrani, F.; Aljohani, N. Vitamin D: Deficiency, Sufficiency and Toxicity. Nutrients 2013, 5, 3605–3616. [Google Scholar] [CrossRef] [Green Version]
- Nielsen, O.H.; Rejnmark, L.; Moss, A.C. Role of Vitamin D in the Natural History of Inflammatory Bowel Disease. J. Crohn’s Colitis 2018, 12, 742–752. [Google Scholar] [CrossRef] [PubMed]
- Gubatan, J.; Chou, N.D.; Nielsen, O.H.; Moss, A.C. Systematic review with meta-analysis: Association of vitamin D status with clinical outcomes in adult patients with inflammatory bowel disease. Aliment. Pharmacol. Ther. 2019, 50, 1146–1158. [Google Scholar] [CrossRef]
- El Amrousy, D.; El Ashry, H.; Hodeib, H.; Hassan, S. Vitamin D in Children With Inflammatory Bowel Disease. J. Clin. Gastroenterol. 2020. [Google Scholar] [CrossRef]
- Guzman-Prado, Y.; Samson, O.; Segal, J.P.; Limdi, J.K.; Hayee, B. Vitamin D Therapy in Adults With Inflammatory Bowel Disease: A Systematic Review and Meta-Analysis. Inflamm. Bowel Dis. 2020, 26, 1819–1830. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, H.; Mander, I.; Zhang, Z.; Armstrong, D.; Wine, E. Not All Fibers Are Born Equal; Variable Response to Dietary Fiber Subtypes in IBD. Front. Pediatr. 2021, 8, 620189. [Google Scholar] [CrossRef] [PubMed]
- Ríos-Covián, D.; Ruas-Madiedo, P.; Margolles, A.; Gueimonde, M.; Reyes-Gavilán, C.G.D.L.; Salazar, N. Intestinal Short Chain Fatty Acids and their Link with Diet and Human Health. Front. Microbiol. 2016, 7, 185. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sokol, H.; Lay, C.; Seksik, P.; Tannock, G.W. Analysis of bacterial bowel communities of IBD patients: What has it revealed? Inflamm. Bowel Dis. 2008, 14, 858–867. [Google Scholar] [CrossRef]
- Pituch-Zdanowska, A.; Albrecht, P.; Banasiuk, M.; Banaszkiewicz, A. Dietary Fiber Intake in Children With Inflammatory Bowel Disease. J. Pediatr. Gastroenterol. Nutr. 2018, 66, 624–629. [Google Scholar] [CrossRef] [PubMed]
- Costa, C.O.P.C.; Carrilho, F.J.; Nunes, V.S.; Sipahi, A.M.; Rodrigues, M. A snapshot of the nutritional status of Crohn’s disease among adolescents in Brazil: A prospective cross-sectional study. BMC Gastroenterol. 2015, 15, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Levine, A.; Rhodes, J.M.; Lindsay, J.O.; Abreu, M.T.; Kamm, M.A.; Gibson, P.R.; Gasche, C.; Silverberg, M.S.; Mahadevan, U.; Boneh, R.S.; et al. Dietary Guidance From the International Organization for the Study of Inflammatory Bowel Diseases. Clin. Gastroenterol. Hepatol. 2020, 18, 1381–1392. [Google Scholar] [CrossRef] [PubMed]
- Adamina, M.; Gerasimidis, K.; Sigall-Boneh, R.; Zmora, O.; Overstraeten, A.D.B.V.; Campmans-Kuijpers, M.; Ellul, P.; Katsanos, K.; Kotze, P.; Noor, N.; et al. DOP05 Perioperative Dietary Therapy in inflammatory bowel disease. J. Crohn’s Colitis 2020, 14, S044. [Google Scholar] [CrossRef]
- Lochs, H.; Allison, S.; Meier, R.; Pirlich, M.; Kondrup, J.; Schneider, S.; Berghe, G.V.D.; Pichard, C. Introductory to the ESPEN Guidelines on Enteral Nutrition: Terminology, Definitions and General Topics. Clin. Nutr. 2006, 25, 180–186. [Google Scholar] [CrossRef] [Green Version]
- Narula, N.; Dhillon, A.; Zhang, D.; E Sherlock, M.; Tondeur, M.; Zachos, M. Enteral nutritional therapy for induction of remission in Crohn’s disease. Cochrane Database Syst. Rev. 2018, 4, CD000542. [Google Scholar] [CrossRef]
- Knight, C.; El-Matary, W.; Spray, C.; Sandhu, B.K. Long-term outcome of nutritional therapy in paediatric Crohn’s disease. Clin. Nutr. 2005, 24, 775–779. [Google Scholar] [CrossRef]
- Akobeng, A.K.; Thomas, A.G. Refeeding Syndrome Following Exclusive Enteral Nutritional Treatment in Crohn Disease. J. Pediatr. Gastroenterol. Nutr. 2010, 51, 364–366. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, J.S.V. ASPEN Consensus Recommendations for Refeeding Syndrome. Nutr. Clin. Pract. 2020, 35, 178–195. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McCole, D.F. IBD Candidate Genes and Intestinal Barrier Regulation. Inflamm. Bowel Dis. 2014, 20, 1829–1849. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kleessen, B.; Kroesen, A.J.; Buhr, H.J.; Blaut, M. Mucosal and Invading Bacteria in Patients with Inflammatory Bowel Disease Compared with Controls. Scand. J. Gastroenterol. 2002, 37, 1034–1041. [Google Scholar] [CrossRef] [PubMed]
- Zaidi, D.; Bording-Jorgensen, M.; Huynh, H.Q.; Carroll, M.W.; Turcotte, J.-F.; Sergi, C.; Liu, J.; Wine, E. Increased Epithelial Gap Density in the Noninflamed Duodenum of Children With Inflammatory Bowel Diseases. J. Pediatr. Gastroenterol. Nutr. 2016, 63, 644–650. [Google Scholar] [CrossRef]
- Fell, J.M.; Paintin, M.; Arnaud-Battandier, F.; Beattie, R.M.; Hollis, A.; Kitching, P.; Donnet-Hughes, A.; Macdonald, T.T.; Walker-Smith, J.A. Mucosal healing and a fall in mucosal pro-inflammatory cytokine mRNA induced by a specific oral polymeric diet in paediatric Crohn’s disease. Aliment. Pharmacol. Ther. 2000, 14, 281–289. [Google Scholar] [CrossRef]
- Yamamoto, T.; Nakahigashi, M.; Umegae, S.; Kitagawa, T.; Matsumoto, K. Impact of elemental diet on mucosal inflammation in patients with active Crohn’s disease: Cytokine production and endoscopic and histological findings. Inflamm. Bowel Dis. 2005, 11, 580–588. [Google Scholar] [CrossRef] [PubMed]
- De Jong, N.S.H.; Leach, S.T.; Day, A.S. Polymeric Formula Has Direct Anti-Inflammatory Effects on Enterocytes in an in VitroModel of Intestinal Inflammation. Dig. Dis. Sci. 2007, 52, 2029–2036. [Google Scholar] [CrossRef]
- Nahidi, L.; Corley, S.M.; Wilkins, M.R.; Wei, J.; Alhagamhmad, M.; Day, A.S.; Lemberg, D.A.; Leach, S.T. The major pathway by which polymeric formula reduces inflammation in intestinal epithelial cells: A microarray-based analysis. Genes Nutr. 2015, 10, 29. [Google Scholar] [CrossRef] [Green Version]
- Alhagamhmad, M.H. Enteral Nutrition in the Management of Crohn’s Disease: Reviewing Mechanisms of Actions and Highlighting Potential Venues for Enhancing the Efficacy. Nutr. Clin. Pr. 2018, 33, 483–492. [Google Scholar] [CrossRef] [PubMed]
- Schwerd, T.; Frivolt, K.; Clavel, T.; Lagkouvardos, I.; Katona, G.; Mayr, D.; Uhlig, H.H.; Haller, D.; Koletzko, S.; Bufler, P. Exclusive enteral nutrition in active pediatric Crohn disease: Effects on intestinal microbiota and immune regulation. J. Allergy Clin. Immunol. 2016, 138, 592–596. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wedrychowicz, A.; Kowalska-Duplaga, K.; Jedynak-Wasowicz, U.; Pieczarkowski, S.; Sladek, M.; Tomasik, P.; Fyderek, K. Serum Concentrations of VEGF and TGF-β1 During Exclusive Enteral Nutrition in IBD. J. Pediatr. Gastroenterol. Nutr. 2011, 53, 150–155. [Google Scholar] [CrossRef]
- Hahm, K.-B.; Im, Y.-H.; Parks, T.W.; Park, S.H.; Markowitz, S.D.; Jung, H.-Y.; Green, J.; Kim, S.J. Loss of transforming growth factor beta signalling in the intestine contributes to tissue injury in inflammatory bowel disease. Gut 2001, 49, 190–198. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Triantafillidis, J.K.; Tzouvala, M.; Triantafyllidi, E. Enteral Nutrition Supplemented with Transforming Growth Factor-β, Colostrum, Probiotics, and Other Nutritional Compounds in the Treatment of Patients with Inflammatory Bowel Disease. Nutrients 2020, 12, 1048. [Google Scholar] [CrossRef] [Green Version]
- I Keenan, J.; Hooper, E.M.; Tyrer, P.C.; Day, A.S. Influences of enteral nutrition upon CEACAM6 expression by intestinal epithelial cells. Innate Immun. 2013, 20, 848–856. [Google Scholar] [CrossRef]
- Budd, G.R.; Aitchison, A.; Day, A.S.; I Keenan, J. The effect of polymeric formula on enterocyte differentiation. Innate Immun. 2017, 23, 240–248. [Google Scholar] [CrossRef] [PubMed]
- Nahidi, L.; Day, A.S.; Lemberg, D.A.; Leach, S.T. Differential effects of nutritional and non-nutritional therapies on intestinal barrier function in an in vitro model. J. Gastroenterol. 2011, 47, 107–117. [Google Scholar] [CrossRef]
- Hansen, R.; Russell, R.K.; Reiff, C.; Louis, P.; McIntosh, F.; Berry, S.H.; Mukhopadhya, I.; Bisset, M.W.; Barclay, A.R.; Bishop, J.; et al. Microbiota of De-Novo Pediatric IBD: Increased Faecalibacterium Prausnitzii and Reduced Bacterial Diversity in Crohn’s But Not in Ulcerative Colitis. Am. J. Gastroenterol. 2012, 107, 1913–1922. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hedin, C.R.; E McCarthy, N.; Louis, P.; Farquharson, F.M.; McCartney, S.; Taylor, K.; Prescott, N.J.; Murrells, T.; Stagg, A.J.; Whelan, K.; et al. Altered intestinal microbiota and blood T cell phenotype are shared by patients with Crohn’s disease and their unaffected siblings. Gut 2014, 63, 1578–1586. [Google Scholar] [CrossRef]
- Treem, W.R.; Ahsan, N.; Shoup, M.; Hyams, J.S. Fecal Short-Chain Fatty Acids in Children with Inflammatory Bowel Disease. J. Pediatr. Gastroenterol. Nutr. 1994, 18, 159–164. [Google Scholar] [CrossRef]
- Bjerrum, J.T.; Wang, Y.; Hao, F.; Coskun, M.; Ludwig, C.; Günther, U.; Nielsen, O.H. Metabonomics of human fecal extracts characterize ulcerative colitis, Crohn’s disease and healthy individuals. Metabolomics 2015, 11, 122–133. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Duboc, H.; Rajca, S.; Rainteau, D.; Benarous, D.; Maubert, M.-A.; Quervain, E.; Thomas, G.; Barbu, V.; Humbert, L.; Despras, G.; et al. Connecting dysbiosis, bile-acid dysmetabolism and gut inflammation in inflammatory bowel diseases. Gut 2013, 62, 531–539. [Google Scholar] [CrossRef] [PubMed]
- Diederen, K.; Li, J.V.; Donachie, G.E.; De Meij, T.G.; De Waart, D.R.; Hakvoort, T.B.M.; Kindermann, A.; Wagner, J.; Auyeung, V.; Velde, A.A.T.; et al. Exclusive enteral nutrition mediates gut microbial and metabolic changes that are associated with remission in children with Crohn’s disease. Sci. Rep. 2020, 10, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Lionetti, P.; Callegari, M.L.; Ferrari, S.; Cavicchi, M.C.; Pozzi, E.; De Martino, M.; Morelli, L. Enteral Nutrition and Microflora in Pediatric Crohn’s Disease. J. Parenter. Enter. Nutr. 2005, 29, S173–S178. [Google Scholar] [CrossRef] [PubMed]
- Gerasimidis, K.; Bertz, M.; Hanske, L.; Junick, J.; Biskou, O.; Aguilera, M.; Garrick, V.; Russell, R.K.; Blaut, M.; McGrogan, P.; et al. Decline in Presumptively Protective Gut Bacterial Species and Metabolites Are Paradoxically Associated with Disease Improvement in Pediatric Crohn’s Disease During Enteral Nutrition. Inflamm. Bowel Dis. 2014, 20, 861–871. [Google Scholar] [CrossRef]
- Logan, M.; Gkikas, K.; Svolos, V.; Nichols, B.; Milling, S.; Gaya, D.R.; Seenan, J.P.; Macdonald, J.; Hansen, R.; Ijaz, U.Z.; et al. Analysis of 61 exclusive enteral nutrition formulas used in the management of active Crohn’s disease-new insights into dietary disease triggers. Aliment. Pharmacol. Ther. 2020, 51, 935–947. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Quince, C.; Ijaz, U.Z.; Loman, N.; A Eren, M.; Saulnier, D.; Russell, J.; Haig, S.J.; Calus, S.T.; Quick, J.; Barclay, A.; et al. Extensive Modulation of the Fecal Metagenome in Children With Crohn’s Disease During Exclusive Enteral Nutrition. Am. J. Gastroenterol. 2015, 110, 1718–1729. [Google Scholar] [CrossRef] [Green Version]
- Voitk, A.J. Experience With Elemental Diet in the Treatment of Inflammatory Bowel Disease: Is This Primary Therapy? Arch. Surg. 1973, 107, 329. [Google Scholar] [CrossRef] [PubMed]
- Morin, C.L.; Roulet, M.; Roy, C.C.; Weber, A. Continuous elemental enteral alimentation in children with Crohn’s disease and growth failure. Gastroenterology 1980, 79, 1205–1210. [Google Scholar] [CrossRef]
- Sanderson, I.R.; Udeen, S.; Davies, P.S.; O Savage, M.; A Walker-Smith, J. Remission induced by an elemental diet in small bowel Crohn’s disease. Arch. Dis. Child. 1987, 62, 123–127. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Swaminath, A.; Feathers, A.; Ananthakrishnan, A.; Falzon, L.; Ferry, S.L. Systematic review with meta-analysis: Enteral nutrition therapy for the induction of remission in paediatric Crohn’s disease. Aliment. Pharmacol. Ther. 2017, 46, 645–656. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Levine, A. Comparison of Outcomes Parameters for Induction of Remission in New Onset Pediatric Crohn’s Disease: Evaluation of the Porto IBD Group “Growth Relapse and Outcomes with Therapy” (GROWTH CD) Study. Inflamm. Bowel Dis. 2014, 20, 278–285. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.; Baldassano, R.N.; Otley, A.R.; Albenberg, L.; Griffiths, A.M.; Compher, C.; Chen, E.Z.; Lindsey, A.; Gilroy, E.; Nessel, L.; et al. Comparative Effectiveness of Nutritional and Biological Therapy in North American Children with Active Crohn’s Disease. Inflamm. Bowel Dis. 2015, 21, 1786–1793. [Google Scholar] [CrossRef] [PubMed]
- Shah, S.C.; Colombel, J.-F.; E Sands, B.; Narula, N. Systematic review with meta-analysis: Mucosal healing is associated with improved long-term outcomes in Crohn’s disease. Aliment. Pharmacol. Ther. 2016, 43, 317–333. [Google Scholar] [CrossRef]
- Grover, Z.; Muir, R.; Lewindon, P. Exclusive enteral nutrition induces early clinical, mucosal and transmural remission in paediatric Crohn’s disease. J. Gastroenterol. 2014, 49, 638–645. [Google Scholar] [CrossRef] [PubMed]
- Borrelli, O.; Cordischi, L.; Cirulli, M.; Paganelli, M.; Labalestra, V.; Uccini, S.; Russo, P.M.; Cucchiara, S. Polymeric Diet Alone Versus Corticosteroids in the Treatment of Active Pediatric Crohn’s Disease: A Randomized Controlled Open-Label Trial. Clin. Gastroenterol. Hepatol. 2006, 4, 744–753. [Google Scholar] [CrossRef]
- Grover, Z.; Burgess, C.; Muir, R.; Reilly, C.; Lewindon, P.J. Early Mucosal Healing with Exclusive Enteral Nutrition is Associated with Improved Outcomes in Newly Diagnosed Children with Luminal Crohn’s disease. J. Crohn’s Colitis 2016, 10, 1159–1164. [Google Scholar] [CrossRef] [Green Version]
- Buchanan, E.; Gaunt, W.W.; Cardigan, T.; Garrick, V.; McGrogan, P.; Russell, R.K. The use of exclusive enteral nutrition for induction of remission in children with Crohn’s disease demonstrates that disease phenotype does not influence clinical remission. Aliment. Pharmacol. Ther. 2009, 30, 501–507. [Google Scholar] [CrossRef] [PubMed]
- Afzal, N.A.; Davies, S.; Paintin, M.; Arnaud-Battandier, F.; Walker-Smith, J.A.; Murch, S.; Heuschkel, R.; Fell, J. Colonic Crohn’s Disease in Children Does Not Respond Well to Treatment with Enteral Nutrition If the Ileum Is Not Involved. Dig. Dis. Sci. 2005, 50, 1471–1475. [Google Scholar] [CrossRef]
- Day, A.S.; E Whitten, K.; A Lemberg, D.; Clarkson, C.; Vitug-Sales, M.; Jackson, R.; Bohane, T.D. Exclusive enteral feeding as primary therapy for Crohn’s disease in Australian children and adolescents: A feasible and effective approach. J. Gastroenterol. Hepatol. 2006, 21, 1609–1614. [Google Scholar] [CrossRef] [PubMed]
- Belli, D.; Seidman, E.; Bouthillier, L.; Weber, A.; Roy, C.; Pletincx, M.; Beaulieu, M.; Morin, C. Chronic intermittent elemental diet improves growth failure in children with Crohn’s disease. Gastroenterology 1988, 94, 603–610. [Google Scholar] [CrossRef]
- Polk, D.B.; Hattner, J.A.T.; Kerner, J.A. Improved Growth and Disease Activity After Intermittent Administration of a Defined Formula Diet in Children With Crohn’s Disease. J. Parenter. Enter. Nutr. 1992, 16, 499–504. [Google Scholar] [CrossRef]
- Patel, K.V.; Darakhshan, A.A.; Griffin, N.; Williams, A.B.; Sanderson, J.D.; Irving, P.M. Patient optimization for surgery relating to Crohn’s disease. Nat. Rev. Gastroenterol. Hepatol. 2016, 13, 707–719. [Google Scholar] [CrossRef]
- Heerasing, N.; Thompson, B.; Hendy, P.; Heap, G.A.; Walker, G.; Bethune, R.; Mansfield, S.; Calvert, C.; Kennedy, N.A.; Ahmad, T.; et al. Exclusive enteral nutrition provides an effective bridge to safer interval elective surgery for adults with Crohn’s disease. Aliment. Pharmacol. Ther. 2017, 45, 660–669. [Google Scholar] [CrossRef] [Green Version]
- Ge, X.; Tang, S.; Yang, X.; Liu, W.; Ye, L.; Yu, W.; Xu, H.; Cao, Q.; Zhou, W.; Cai, X. The role of exclusive enteral nutrition in the preoperative optimization of laparoscopic surgery for patients with Crohn’s disease: A cohort study. Int. J. Surg. 2019, 65, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Grass, F.; Pache, B.; Martin, D.; Hahnloser, D.; Demartines, N.; Hübner, M. Preoperative Nutritional Conditioning of Crohn’s Patients-Systematic Review of Current Evidence and Practice. Nutrients 2017, 9, 562. [Google Scholar] [CrossRef] [Green Version]
- Jacobson, S. Early postoperative complications in patients with Crohn’s disease given and not given preoperative total parenteral nutrition. Scand. J. Gastroenterol. 2012, 47, 170–177. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Zuo, L.; Zhao, J.; Dong, J.; Li, Y.; Gu, L.; Gong, J.; Liu, Q.; Zhu, W. Impact of Preoperative Exclusive Enteral Nutrition on Postoperative Complications and Recurrence After Bowel Resection in Patients with Active Crohn’s Disease. World J. Surg. 2016, 40, 1993–2000. [Google Scholar] [CrossRef]
- Li, Y.; Zuo, L.; Zhu, W.; Gong, J.; Zhang, W.; Gu, L.; Guo, Z.; Cao, L.; Li, N.; Li, J. Role of Exclusive Enteral Nutrition in the Preoperative Optimization of Patients With Crohn’s Disease Following Immunosuppressive Therapy. Medicine 2015, 94, e478. [Google Scholar] [CrossRef]
- Li, G.; Ren, J.; Wang, G.; Hu, D.; Gu, G.; Liu, S.; Ren, H.; Wu, X.; Li, J. Preoperative exclusive enteral nutrition reduces the postoperative septic complications of fistulizing Crohn’s disease. Eur. J. Clin. Nutr. 2014, 68, 441–446. [Google Scholar] [CrossRef]
- Harris, R.E.; Duncan, H.; Buchanan, E.; Cardigan, T.; Garrick, V.; Curtis, L.; Gervais, L.; Barclay, A.; Haddock, G.; Hansen, R.; et al. Prehabilitation: The Impact of Preoperative Exclusive Enteral Nutrition on Paediatric Patients With Crohn Disease. J. Pediatr. Gastroenterol. Nutr. 2020, 70, 503–507. [Google Scholar] [CrossRef] [PubMed]
- Whitten, K.E.; Leach, S.T.; Bohane, T.D.; Woodhead, H.J.; Day, A.S. Effect of exclusive enteral nutrition on bone turnover in children with Crohn’s disease. J. Gastroenterol. 2009, 45, 399–405. [Google Scholar] [CrossRef]
- Strisciuglio, C.; Scarpato, E.; Cenni, S.; Serra, M.; Giugliano, F.; Mainolfi, C.; Dolce, P.; Martinelli, M.; Staiano, A.; Miele, E. Improvement of body composition and bone mineral density after enteral nutrition in pediatric Crohn disease. Dig. Liver Dis. 2020, 52, 630–636. [Google Scholar] [CrossRef]
- Lev-Tzion, R.; Ben-Moshe, T.; Abitbol, G.; Ledder, O.; Peleg, S.; Millman, P.; Shaoul, R.; Kori, M.; Assa, A.; Cohen, S.; et al. The Effect of Nutritional Therapy on Bone Mineral Density and Bone Metabolism in Pediatric Crohn’s Disease. J. Pediatr. Gastroenterol. Nutr. 2021. [Google Scholar] [CrossRef] [PubMed]
- Johnson, T.; Macdonald, S.; Hill, S.M.; Thomas, A.; Murphy, M.S. Treatment of active Crohn’s disease in children using partial enteral nutrition with liquid formula: A randomised controlled trial. Gut 2006, 55, 356–361. [Google Scholar] [CrossRef] [Green Version]
- Gupta, K.; Noble, A.; Kachelries, K.E.; Albenberg, L.; Kelsen, J.R.; Grossman, A.B.; Baldassano, R.N. A Novel Enteral Nutrition Protocol for the Treatment of Pediatric Crohn’s Disease. Inflamm. Bowel Dis. 2013, 19, 1374–1378. [Google Scholar] [CrossRef]
- Wilschanski, M.; Sherman, P.; Pencharz, P.; Davis, L.; Corey, M.; Griffiths, A. Supplementary enteral nutrition maintains remission in paediatric Crohn’s disease. Gut 1996, 38, 543–548. [Google Scholar] [CrossRef]
- Duncan, H.; Buchanan, E.; Cardigan, T.; Garrick, V.; Curtis, L.; McGrogan, P.; Barclay, A.; Russell, R.K. A retrospective study showing maintenance treatment options for paediatric CD in the first year following diagnosis after induction of remission with EEN: Supplemental enteral nutrition is better than nothing! BMC Gastroenterol. 2014, 14, 50. [Google Scholar] [CrossRef] [Green Version]
- Schulman, J.M.; Pritzker, L.; Shaoul, R. Maintenance of Remission with Partial Enteral Nutrition Therapy in Pediatric Crohn’s Disease: A Retrospective Study. Can. J. Gastroenterol. Hepatol. 2017, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Gavin, J.; Ashton, J.J.; Heather, N.; Marino, L.V.; Beattie, R.M. Nutritional support in paediatric Crohn’s disease: Outcome at 12 months. Acta Paediatr. 2017, 107, 156–162. [Google Scholar] [CrossRef]
- Logan, M.; Clark, C.M.; Ijaz, U.Z.; Gervais, L.; Duncan, H.; Garrick, V.; Curtis, L.; Buchanan, E.; Cardigan, T.; Armstrong, L.; et al. The reduction of faecal calprotectin during exclusive enteral nutrition is lost rapidly after food re-introduction. Aliment. Pharmacol. Ther. 2019, 50, 664–674. [Google Scholar] [CrossRef]
- Takagi, S.; Utsunomiya, K.; Kuriyama, S.; Yokoyama, H.; Takahashi, S.; Iwabuchi, M.; Kinouchi, Y.; Hiwatashi, N.; Funayama, Y.; Sasaki, I.; et al. Effectiveness of an ’half elemental diet’ as maintenance therapy for Crohn’s disease: A randomized-controlled trial. Aliment. Pharmacol. Ther. 2006, 24, 1333–1340. [Google Scholar] [CrossRef] [PubMed]
- Hanai, H.; Iida, T.; Takeuchi, K.; Arai, H.; Arai, O.; Abe, J.; Tanaka, T.; Maruyama, Y.; Ikeya, K.; Sugimoto, K.; et al. Nutritional therapy versus 6-mercaptopurine as maintenance therapy in patients with Crohn’s disease. Dig. Liver Dis. 2012, 44, 649–654. [Google Scholar] [CrossRef]
- Hirai, F.; Takeda, T.; Takada, Y.; Kishi, M.; Beppu, T.; Takatsu, N.; Miyaoka, M.; Hisabe, T.; Yao, K.; Ueki, T. Efficacy of enteral nutrition in patients with Crohn’s disease on maintenance anti-TNF-alpha antibody therapy: A meta-analysis. J. Gastroenterol. 2020, 55, 133–141. [Google Scholar] [CrossRef] [Green Version]
- Gkikas, K.; Gerasimidis, K.; Milling, S.; Ijaz, U.Z.; Hansen, R.; Russell, R.K. Dietary Strategies for Maintenance of Clinical Remission in Inflammatory Bowel Diseases: Are We There Yet? Nutrients 2020, 12, 2018. [Google Scholar] [CrossRef]
- Jones, V.A. Comparison of total parenteral nutrition and elemental diet in induction of remission of Crohn’s disease. Dig. Dis. Sci. 1987, 32, S100–S107. [Google Scholar] [CrossRef] [PubMed]
- Woolner, J.T.; Parker, T.J.; Kirby, G.A.; Hunter, J.O. The development and evaluation of a diet for maintaining remission in Crohn’s disease. J. Hum. Nutr. Diet. 1998, 11, 1–11. [Google Scholar] [CrossRef]
- Faiman, A.; Mutalib, M.; Moylan, A.; Morgan, N.; Crespi, D.; Furman, M.; Kader, A. Standard versus rapid food reintroduction after exclusive enteral nutritional therapy in paediatric Crohn’s disease. Eur. J. Gastroenterol. Hepatol. 2014, 26, 276–281. [Google Scholar] [CrossRef] [PubMed]
- Levine, A.; Wine, E. Effects of enteral nutrition on Crohn’s disease: Clues to the impact of diet on disease pathogenesis. Inflamm. Bowel. Dis. 2013, 19, 1322–1329. [Google Scholar] [CrossRef]
- Nickerson, K.P.; Chanin, R.; McDonald, C. Deregulation of intestinal anti-microbial defense by the dietary additive, maltodextrin. Gut Microbes 2015, 6, 78–83. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chassaing, B.; Koren, O.; Goodrich, J.K.; Poole, A.C.; Srinivasan, S.; Ley, R.E.; Gewirtz, A.T. Dietary emulsifiers impact the mouse gut microbiota promoting colitis and metabolic syndrome. Nat. Cell Biol. 2015, 519, 92–96. [Google Scholar] [CrossRef] [Green Version]
- Nickerson, K.P.; Homer, C.R.; Kessler, S.P.; Dixon, L.J.; Kabi, A.; Gordon, I.O.; Johnson, E.E.; De La Motte, C.A.; McDonald, C. The Dietary Polysaccharide Maltodextrin Promotes Salmonella Survival and Mucosal Colonization in Mice. PLoS ONE 2014, 9, e101789. [Google Scholar] [CrossRef] [Green Version]
- Herrador-López, M.; Martín-Masot, R.; Navas-López, V.M. EEN Yesterday and Today CDED Today and Tomorrow. Nutrients 2020, 12, 3793. [Google Scholar] [CrossRef]
- Sigall-Boneh, R.; Pfeffer-Gik, T.; Segal, I.; Zangen, T.; Boaz, M.; Levine, A. Partial enteral nutrition with a Crohn’s disease exclusion diet is effective for induction of remission in children and young adults with Crohn’s disease. Inflamm. Bowel Dis. 2014, 20, 1353–1360. [Google Scholar] [CrossRef] [PubMed]
- Boneh, R.S.; Van Limbergen, J.; Wine, E.; Assa, A.; Shaoul, R.; Milman, P.; Cohen, S.; Kori, M.; Peleg, S.; On, A.; et al. Dietary Therapies Induce Rapid Response and Remission in Pediatric Patients With Active Crohn’s Disease. Clin. Gastroenterol. Hepatol. 2021, 19, 752–759. [Google Scholar] [CrossRef] [PubMed]
- Debruyn, J.C.; Jacobson, K.; El-Matary, W.; Carroll, M.; Wine, E.; Wrobel, I.; Van Woudenberg, M.; Huynh, H.Q. Long-term Outcomes of Infliximab Use for Pediatric Crohn Disease: A Canadian Multicenter Clinical Practice Experience. J. Pediatr. Gastroenterol. Nutr. 2018, 66, 268–273. [Google Scholar] [CrossRef]
- Faubion, W.A.; Dubinsky, M.; Ruemmele, F.M.; Escher, J.; Rosh, J.; Hyams, J.S.; Lazar, A. Long-term Efficacy and Safety of Adalimumab in Pediatric Patients with Crohn’s Disease. Inflamm. Bowel Dis. 2017, 23, 453–460. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boneh, R.S.; Shabat, C.S.; Yanai, H.; Chermesh, I.; Ben Avraham, S.; Boaz, M.; Levine, A. Dietary Therapy With the Crohn’s Disease Exclusion Diet is a Successful Strategy for Induction of Remission in Children and Adults Failing Biological Therapy. J. Crohn’s Colitis 2017, 11, 1205–1212. [Google Scholar] [CrossRef] [Green Version]
- Turner, D.; Griffiths, A.M.; Wilson, D.; Mould, D.R.; Baldassano, R.N.; Russell, R.K.; Dubinsky, M.; Heyman, M.B.; De Ridder, L.; Hyams, J.; et al. Designing clinical trials in paediatric inflammatory bowel diseases: A PIBDnet commentary. Gut 2020, 69, 32–41. [Google Scholar] [CrossRef] [PubMed]
- Seyed Tabib, N.S.; Madgwick, M.; Sudhakar, P.; Verstockt, B.; Korcsmaros, T.; Vermeire, S. Big data in IBD: Big progress for clinical practice. Gut 2020, 69, 1520–1532. [Google Scholar] [CrossRef] [PubMed]
| First Author | Study Design | Population | Intervention (Duration) | Control Group | Key Findings |
|---|---|---|---|---|---|
| Morin [139] | R | 4 CD with growth failure | Elemental formula (6 weeks) | N/A |
|
| Sanderson [140] | P/RCT | 8 pts with active CD | Elemental formula (6 weeks) | 8 CD patients treated with CS |
|
| Cohen-Dolev [24] | P/O | 60 patients with newly diagnosed CD | Any formula (6–8 weeks) | 87 matched patients treated with CS |
|
| Levine [142] | P/O | 43 patients with newly diagnosed CD | Any formula (6–8 weeks) | 114 patients treated with CS 29 with 5-ASA |
|
| Lee [143] | P/O | 22 patients with active CD | Any formula (6–8 weeks) | 52 patients treated with anti-TNF-α 16 pts with PEN + unrestricted diet |
|
| Grover [145] | P/O | 26 patients with active CD | Any formula (6 weeks) | N/A |
|
| Borrelli [146] | P/RCT | 19 patients with active CD | Polymeric formula (10 weeks) | 18 patients treated with CS |
|
| Grover [147] | P/O | 54 patients with active disease | Any formula (6 weeks) | N/A |
|
| Rubio [148] | R | 45 patients with CD who received oral EEN | Polymeric formula (8 weeks) | 61 patients treated with continuous EEN |
|
| Buchanan [149] | R | 110 patients with CD | Polymeric/ Elemental formula (8 weeks) | N/A |
|
| Afzal [150] | R | 65 patients with active CD | Polymeric formula (8 weeks) | N/A |
|
| Belli [152] | P | 8 patients with active CD and growth failure | Polymeric formula (intermittent administration over 1 year) | 4 matched CD patients not treated with EEN |
|
| First Author | Study Design | Population | Intervention (Duration) | Control Group | Key Findings |
|---|---|---|---|---|---|
| Sigall-Boneh [183] | R | 47 children and young adult pts with active CD | CDED + PEN (12 weeks, n = 40) CDED weeks, n = 7) | N/A | Clinical remission achieved in 24/34 children and 9/13 adults at wk 6 and maintained in 27/33 patients at week 12; Significant fall in clinical disease activity and inflammatory markers. |
| Sigall-Boneh [187] | R | 21 children and young adult pts with treatment-refractory CD | CDED + PEN (12 weeks, n = 12) CDED (12 weeks, n = 4) Mod. EEN + CDED (2 + 12 weeks, n = 5) | N/A | 13/21 pts refractory to biologic treatment achieved clinical remission; 9/17 of patients failing double biologic therapy achieved clinical remission; Significant decrease in serum markers of inflammation. |
| Levine [32] | P/RCT | 40 pts with mild-to-moderate CD | CDED + PEN (12 weeks) | 34 pts with mild-to-moderate CD treated with EEN | CDED+PEN was equally as effective as EEN in inducing remission at week 6; CDED+PEN was superior to EEN in maintaining remission at week 12; CDED+PEN was able to induce rapid remission (3 weeks); |
| Svolos [33] | OL | 5 pts with active CD (PCDAI ≥ 12.5) | CD-TREAT (8 weeks) | N/A | CD-TREAT was able to induce clinical response in 80% and remission in 60% of patients; 80% of pts showed decrease in fecal calprotectin |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scarallo, L.; Lionetti, P. Dietary Management in Pediatric Patients with Crohn’s Disease. Nutrients 2021, 13, 1611. https://doi.org/10.3390/nu13051611
Scarallo L, Lionetti P. Dietary Management in Pediatric Patients with Crohn’s Disease. Nutrients. 2021; 13(5):1611. https://doi.org/10.3390/nu13051611
Chicago/Turabian StyleScarallo, Luca, and Paolo Lionetti. 2021. "Dietary Management in Pediatric Patients with Crohn’s Disease" Nutrients 13, no. 5: 1611. https://doi.org/10.3390/nu13051611






