Dietary Phosphorus as a Marker of Mineral Metabolism and Progression of Diabetic Kidney Disease
Abstract
:1. Phosphate Homeostasis
2. Abnormalities of Phosphate Homeostasis in Chronic Kidney Disease (CKD)
3. Interactions between Glucose and Phosphate Homeostasis
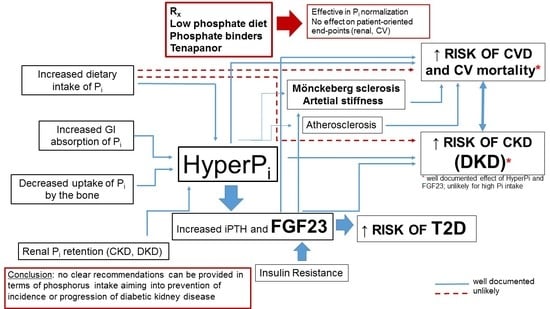
4. Impact of Phosphate on CV Disease and Outcome in General Population, CKD and Diabetes
5. Impact of Phosphorus on Development and Progression of Non-Diabetic and Diabetic CKD
6. Therapeutic Interventions to Lower Serum Phosphorus for Cardio- and Nephroprotection
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| CKD | chronic kidney disease |
| CKD-MBD | mineral ad bone disorders of chronic kidney disease |
| CV | cardiovascular |
| CVD | cardiovascular disease |
| DKD | diabetic kidney disease |
| ECM | extracelular matrix |
| ESRD | end-stage renal disease |
| FGF | fibroblast growth factor |
| GFR | glomerular filtration rate |
| GI | gastrointestinal tract |
| GLP1 | glucagon-like peptide 1 |
| HOMA-IR | Homeostatic Model Assessment for Insulin Resistance |
| IGF1 | insulin-like growth fatcor 1 |
| IL | interleukin |
| KDIGO | Kidney Disease: Improving Global Outcomes |
| KEEP | Kidney Early Evaluation Program |
| MDRD | Modification of Diet in Renal Disease |
| NHE3 | sodium-hydrogen exchanger3 |
| NHANES | National Health and Nutrition Examination Survey |
| PTH | parathyroid hormone |
| SGLT2i | sodium-glucose co-transporter type 1 |
| sFRp-4 | soluble Frizzled-related protein 4 |
| T2D | type 2 diabetes |
| VSMC | vascular smooth muscle cells |
References
- Calvo, M.S.; Lamberg-Allardt, C.J. Phosphorus. Adv. Nutr. 2015, 6, 860–862. [Google Scholar] [CrossRef] [Green Version]
- Lederer, E. Regulation of serum phosphate. J. Physiol. 2014, 592, 3985–3995. [Google Scholar] [CrossRef]
- Serna, J.; Bergwitz, C. Importance of Dietary Phosphorus for Bone Metabolism and Healthy Aging. Nutr. 2020, 12, 3001. [Google Scholar] [CrossRef] [PubMed]
- Marks, J.; Debnam, E.S.; Unwin, R.J. The role of the gastrointestinal tract in phosphate homeostasis in health and chronic kidney disease. Curr. Opin. Nephrol. Hypertens. 2013, 22, 481–487. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lederer, E. Renal phosphate transporters. Curr. Opin. Nephrol. Hypertens. 2014, 23, 502–506. [Google Scholar] [CrossRef] [PubMed]
- Wagner, C.A.; Hernando, N.; Forster, I.C.; Biber, J. The SLC34 family of sodium-dependent phosphate transporters. Pflügers Archiv Eur. J. Physiol. 2013, 466, 139–153. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Drüeke, T.B.; Massy, Z.A. Changing bone patterns with progression of chronic kidney disease. Kidney Int. 2016, 89, 289–302. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gutierrez, O.; Isakova, T.; Rhee, E.; Shah, A.; Holmes, J.; Collerone, G.; Jüppner, H.; Wolf, M. Fibroblast Growth Factor-23 Mitigates Hyperphosphatemia but Accentuates Calcitriol Deficiency in Chronic Kidney Disease. J. Am. Soc. Nephrol. 2005, 16, 2205–2215. [Google Scholar] [CrossRef] [PubMed]
- Faul, C. Fibroblast growth factor 23 and the heart. Curr. Opin. Nephrol. Hypertens. 2012, 21, 369–375. [Google Scholar] [CrossRef]
- Kalantar-Zadeh, K.; Gutekunst, L.; Mehrotra, R.; Kovesdy, C.P.; Bross, R.; Shinaberger, C.S.; Noori, N.; Hirschberg, R.; Benner, D.; Nissenson, A.R.; et al. Understanding Sources of Dietary Phosphorus in the Treatment of Patients with Chronic Kidney Disease. Clin. J. Am. Soc. Nephrol. 2010, 5, 519–530. [Google Scholar] [CrossRef]
- Chang, J.-F.; Feng, Y.-F.; Peng, Y.-S.; Hsu, S.-P.; Pai, M.-F.; Chen, H.-Y.; Wu, H.-Y.; Yang, J.-Y. Combined Alkaline Phosphatase and Phosphorus Levels as a Predictor of Mortality in Maintenance Hemodialysis Patients. Med. 2014, 93, e106. [Google Scholar] [CrossRef]
- Moe, S.M.; Zidehsarai, M.P.; Chambers, M.A.; Jackman, L.A.; Radcliffe, J.S.; Trevino, L.L.; Donahue, S.E.; Asplin, J.R. Vegetarian Compared with Meat Dietary Protein Source and Phosphorus Homeostasis in Chronic Kidney Disease. Clin. J. Am. Soc. Nephrol. 2010, 6, 257–264. [Google Scholar] [CrossRef] [Green Version]
- Isakova, T.; Gutiérrez, O.M.; Smith, K.; Epstein, M.; Keating, L.K.; Jüppner, H.; Wolf, M. Pilot study of dietary phosphorus restriction and phosphorus binders to target fibroblast growth factor 23 in patients with chronic kidney disease. Nephrol. Dial. Transplant. 2010, 26, 584–591. [Google Scholar] [CrossRef] [PubMed]
- Selamet, U.; Tighiouart, H.; Sarnak, M.J.; Beck, G.J.; Levey, A.S.; A Block, G.; Ix, J.H. Relationship of dietary phosphate intake with risk of end-stage renal disease and mortality in chronic kidney disease stages 3–5: The Modification of Diet in Renal Disease Study. Kidney Int. 2016, 89, 176–184. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Knöpfel, T.; Pastor-Arroyo, E.M.; Schnitzbauer, U.; Kratschmar, D.V.; Odermatt, A.; Pellegrini, G.; Hernando, N.; Wagner, C.A. The intestinal phosphate transporter NaPi-IIb (Slc34a2) is required to protect bone during dietary phosphate restriction. Sci. Rep. 2017, 7, 11018. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fouque, D.; Vervloet, M.; Ketteler, M. Targeting Gastrointestinal Transport Proteins to Control Hyperphosphatemia in Chronic Kidney Disease. Drugs 2018, 78, 1171–1186. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Block, G.A.; Rosenbaum, D.P.; Yan, A.; Chertow, G.M. Efficacy and Safety of Tenapanor in Patients with Hyperphosphatemia Receiving Maintenance Hemodialysis: A Randomized Phase 3 Trial. J. Am. Soc. Nephrol. 2019, 30, 641–652. [Google Scholar] [CrossRef]
- Cianciolo, G.; De Pascalis, A.; Capelli, I.; Gasperoni, L.; Di Lullo, L.; Bellasi, A.; La Manna, G. Mineral and Electrolyte Disorders With SGLT2i Therapy. JBMR Plus 2019, 3, e10242. [Google Scholar] [CrossRef] [Green Version]
- Hou, Y.-C.; Zheng, C.-M.; Yen, T.-H.; Lu, K.-C. Molecular Mechanisms of SGLT2 Inhibitor on Cardiorenal Protection. Int. J. Mol. Sci. 2020, 21, 7833. [Google Scholar] [CrossRef]
- Wanner, C.; Inzucchi, S.E.; Lachin, J.M.; Fitchett, D.; Von Eynatten, M.; Mattheus, M.; Johansen, O.E.; Woerle, H.J.; Broedl, U.C.; Zinman, B. Empagliflozin and Progression of Kidney Disease in Type 2 Diabetes. N. Engl. J. Med. 2016, 375, 323–334. [Google Scholar] [CrossRef]
- Zelniker, T.A.; Braunwald, E. Clinical Benefit of Cardiorenal Effects of Sodium-Glucose Cotransporter 2 Inhibitors. J. Am. Coll. Cardiol. 2020, 75, 435–447. [Google Scholar] [CrossRef]
- Wiviott, S.D.; Raz, I.; Bonaca, M.P.; Mosenzon, O.; Kato, E.T.; Cahn, A.; Silverman, M.G.; Zelniker, T.A.; Kuder, J.F.; Murphy, S.A.; et al. Dapagliflozin and Cardiovascular Outcomes in Type 2 Diabetes. N. Engl. J. Med. 2019, 380, 347–357. [Google Scholar] [CrossRef] [PubMed]
- Perkovic, V.; Jardine, M.J.; Neal, B.; Bompoint, S.; Heerspink, H.J.; Charytan, D.M.; Edwards, R.; Agarwal, R.; Bakris, G.; Bull, S.; et al. Canagliflozin and Renal Outcomes in Type 2 Diabetes and Nephropathy. N. Engl. J. Med. 2019, 380, 2295–2306. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peled, H.; Dau, N.-Q.; Borghi, C.; Cicero, A.F.G.; Vieira, J.L.; Mehra, M.R.; McMurray, J.J.V.; Docherty, K.F.; Jhund, P.S. Dapagliflozin in Patients with Heart Failure and Reduced Ejection Fraction. N. Engl. J. Med. 2020, 382, 972–973. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Packer, M.; Anker, S.D.; Butler, J.; Filippatos, G.; Pocock, S.J.; Carson, P.; Januzzi, J.; Verma, S.; Tsutsui, H.; Brueckmann, M.; et al. Cardiovascular and Renal Outcomes with Empagliflozin in Heart Failure. N. Engl. J. Med. 2020, 383, 1413–1424. [Google Scholar] [CrossRef]
- Heerspink, H.J.; Stefánsson, B.V.; Correa-Rotter, R.; Chertow, G.M.; Greene, T.; Hou, F.-F.; Mann, J.F.; McMurray, J.J.; Lindberg, M.; Rossing, P.; et al. Dapagliflozin in Patients with Chronic Kidney Disease. N. Engl. J. Med. 2020, 383, 1436–1446. [Google Scholar] [CrossRef] [PubMed]
- Wheeler, D.C.; Stefansson, B.V.; Batiushin, M.; Bilchenko, O.; I Cherney, D.Z.; Chertow, G.M.; Douthat, W.; Dwyer, J.P.; Escudero, E.; Pecoits-Filho, R.; et al. The dapagliflozin and prevention of adverse outcomes in chronic kidney disease (DAPA-CKD) trial: baseline characteristics. Nephrol. Dial. Transplant. 2020, 35, 1700–1711. [Google Scholar] [CrossRef]
- Wheeler, D.C.; Stefánsson, B.V.; Jongs, N.; Chertow, G.M.; Greene, T.; Hou, F.F.; McMurray, J.J.V.; Correa-Rotter, R.; Rossing, P.; Toto, R.D.; et al. Effects of dapagliflozin on major adverse kidney and cardiovascular events in patients with diabetic and non-diabetic chronic kidney disease: a prespecified analysis from the DAPA-CKD trial. Lancet Diabetes Endocrinol. 2021, 9, 22–31. [Google Scholar] [CrossRef]
- Donath, M.Y.; Shoelson, S.E. Type 2 diabetes as an inflammatory disease. Nat. Rev. Immunol. 2011, 11, 98–107. [Google Scholar] [CrossRef] [PubMed]
- Bär, L.; Feger, M.; Fajol, A.; Klotz, L.-O.; Zeng, S.; Lang, F.; Hocher, B.; Föller, M. Insulin suppresses the production of fibroblast growth factor 23 (FGF23). Proc. Natl. Acad. Sci. 2018, 115, 5804–5809. [Google Scholar] [CrossRef] [Green Version]
- Garland, J.S.; Holden, R.M.; Ross, R.; Adams, M.A.; Nolan, R.L.; Hopman, W.M.; Morton, A.R. Insulin resistance is associated with Fibroblast Growth Factor-23 in stage 3–5 chronic kidney disease patients. J. Diabetes Its Complicat. 2014, 28, 61–65. [Google Scholar] [CrossRef]
- Hanks, L.J.; Casazza, K.; Judd, S.E.; Jenny, N.S.; Gutiérrez, O.M. Associations of Fibroblast Growth Factor-23 with Markers of Inflammation, Insulin Resistance and Obesity in Adults. PLOS ONE 2015, 10, e0122885. [Google Scholar] [CrossRef] [PubMed]
- Castillo, M.; Campillo, J.-E.; Valdivia, M.M.; Osório, C. Effect of phosphate omission on the glucose-induced insulin releasein vitro in fed and fasted rats. Acta Diabetol. 1982, 19, 281–283. [Google Scholar] [CrossRef] [PubMed]
- Haap, M.; Heller, E.; Thamer, C.; Tschritter, O.; Stefan, N.; Fritsche, A. Association of serum phosphate levels with glucose tolerance, insulin sensitivity and insulin secretion in non-diabetic subjects. Eur. J. Clin. Nutr. 2006, 60, 734–739. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mancini, F.R.; Affret, A.; Dow, C.; Balkau, B.; Clavel-Chapelon, F.; Bonnet, F.; Boutron-Ruault, M.-C.; Fagherazzi, G. High dietary phosphorus intake is associated with an increased risk of type 2 diabetes in the large prospective E3N cohort study. Clin. Nutr. 2018, 37, 1625–1630. [Google Scholar] [CrossRef]
- Cheng, H.-T.; Xu, X.; Lim, P.S.; Hung, K.-Y. Worldwide Epidemiology of Diabetes-Related End-Stage Renal Disease, 2000–2015. Diabetes Care 2021, 44, 89–97. [Google Scholar] [CrossRef]
- Provenzano, M.; Coppolino, G.; De Nicola, L.; Serra, R.; Garofalo, C.; Andreucci, M.; Bolignano, D. Unraveling Cardiovascular Risk in Renal Patients: A New Take on Old Tale. Front. Cell Dev. Biol. 2019, 7, 314. [Google Scholar] [CrossRef] [Green Version]
- Haynes, R.; Staplin, N.; Emberson, J.; Herrington, W.G.; Tomson, C.; Agodoa, L.; Tesar, V.; Levin, A.; Lewis, D.; Reith, C.; et al. Evaluating the Contribution of the Cause of Kidney Disease to Prognosis in CKD: Results From the Study of Heart and Renal Protection (SHARP). Am. J. Kidney Dis. 2014, 64, 40–48. [Google Scholar] [CrossRef] [Green Version]
- Davignon, J.; Ganz, P. Role of Endothelial Dysfunction in Atherosclerosis. Circulation 2004, 109 (Suppl. 1), III-27. [Google Scholar] [CrossRef] [Green Version]
- Haidara, M.; Yassin, H.; Rateb, M.; Ammar, H.; Zorkani, M. Role of Oxidative Stress in Development of Cardiovascular Complications in Diabetes Mellitus. Curr. Vasc. Pharmacol. 2006, 4, 215–227. [Google Scholar] [CrossRef] [PubMed]
- Gerich, J.E. Postprandial Hyperglycemia and Cardiovascular Disease. Endocr. Pr. 2006, 12, 47–51. [Google Scholar] [CrossRef] [PubMed]
- Roumeliotis, S.; Mallamaci, F.; Zoccali, C. Endothelial Dysfunction in Chronic Kidney Disease, from Biology to Clinical Outcomes: A 2020 Update. J. Clin. Med. 2020, 9, 2359. [Google Scholar] [CrossRef]
- Stompór, T.P.; Pasowicz, M.; Sułowicz, W.; Dembińska-Kieć, A.; Janda, K.; Wójcik, K.; Tracz, W.; Zdzienicka, A.; Konieczyńska, M.; Klimeczek, P.; et al. Trends and dynamics of changes in calcification score over the 1-year observation period in patients on peritoneal dialysis. Am. J. Kidney Dis. 2004, 44, 517–528. [Google Scholar] [CrossRef]
- Stompór, T.; Pasowicz, M.; Sulłowicz, W.; Dembińska-Kieć, A.; Janda, K.; Wójcik, K.; Tracz, W.; Zdzienicka, A.; Klimeczek, P.; Janusz-Grzybowska, E. An association between coronary artery calcification score, lipid profile, and selected markers of chronic inflammation in ESRD patients treated with peritoneal dialysis. Am. J. Kidney Dis. 2003, 41, 203–211. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Zhou, P.; Chen, W.; Peng, D. Combined effects of hyperphosphatemia and hyperglycemia on the calcification of cultured human aortic smooth muscle cells. Exp. Ther. Med. 2018, 17, 863–868. [Google Scholar] [CrossRef] [PubMed]
- Shanahan, C.M.; Crouthamel, M.H.; Kapustin, A.; Giachelli, C.M. Arterial Calcification in Chronic Kidney Disease: Key Roles for Calcium and Phosphate. Circ. Res. 2011, 109, 697–711. [Google Scholar] [CrossRef] [Green Version]
- Yamada, S.; Giachelli, C.M. Vascular calcification in CKD-MBD: Roles for phosphate, FGF23, and Klotho. Bone 2017, 100, 87–93. [Google Scholar] [CrossRef]
- Reynolds, J.L.; Joannides, A.J.; Skepper, J.N.; McNair, R.; Schurgers, L.J.; Proudfoot, D.; Jahnen-Dechent, W.; Weissberg, P.L.; Shanahan, C.M. Human Vascular Smooth Muscle Cells Undergo Vesicle-Mediated Calcification in Response to Changes in Extracellular Calcium and Phosphate Concentrations: A Potential Mechanism for Accelerated Vascular Calcification in ESRD. J. Am. Soc. Nephrol. 2004, 15, 2857–2867. [Google Scholar] [CrossRef] [Green Version]
- Tabas, I.; Bornfeldt, K.E. Macrophage Phenotype and Function in Different Stages of Atherosclerosis. Circ. Res. 2016, 118, 653–667. [Google Scholar] [CrossRef] [Green Version]
- Mehrotra, R.; Peralta, C.A.; Chen, S.-C.; Li, S.; Sachs, M.; Shah, A.; Norris, K.; Saab, G.; Whaley-Connell, A.; Kestenbaum, B.; et al. No independent association of serum phosphorus with risk for death or progression to end-stage renal disease in a large screen for chronic kidney disease. Kidney Int. 2013, 84, 989–997. [Google Scholar] [CrossRef] [Green Version]
- Menon, V.; Greene, T.; Pereira, A.A.; Wang, X.; Beck, G.J.; Kusek, J.W.; Collins, A.J.; Levey, A.S.; Sarnak, M.J. Relationship of Phosphorus and Calcium-Phosphorus Product With Mortality in CKD. Am. J. Kidney Dis. 2005, 46, 455–463. [Google Scholar] [CrossRef]
- Palmer, S.C.; Hayen, A.; Macaskill, P.; Pellegrini, F.; Craig, J.C.; Elder, G.J.; Strippoli, G.F.M. Serum Levels of Phosphorus, Parathyroid Hormone, and Calcium and Risks of Death and Cardiovascular Disease in Individuals With Chronic Kidney Disease. JAMA 2011, 305, 1119–1127. [Google Scholar] [CrossRef] [PubMed]
- Kestenbaum, B.; Sampson, J.N.; Rudser, K.D.; Patterson, D.J.; Seliger, S.L.; Young, B.; Sherrard, D.J.; Andress, D.L. Serum Phosphate Levels and Mortality Risk among People with Chronic Kidney Disease. J. Am. Soc. Nephrol. 2004, 16, 520–528. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tonelli, M.; Sacks, F.; Pfeffer, M.; Gao, Z.; Curhan, G. Relation Between Serum Phosphate Level and Cardiovascular Event Rate in People With Coronary Disease. Circ. 2005, 112, 2627–2633. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gutiérrez, O.M. Increased serum phosphate and adverse clinical outcomes: Unraveling mechanisms of disease. Curr. Opin. Nephrol. Hypertens. 2011, 20, 224–228. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Parra, E.; Tuñón, J.; Egido, J.; Ortiz, A. Phosphate: a stealthier killer than previously thought? Cardiovasc. Pathol. 2012, 21, 372–381. [Google Scholar] [CrossRef]
- Singh, M.; Sharma, P.K.; Garg, V.K.; Mondal, S.C.; Singh, A.K.; Kumar, N. Role of fetuin-A in atherosclerosis associated with diabetic patients. J. Pharm. Pharmacol. 2012, 64, 1703–1708. [Google Scholar] [CrossRef]
- Yilmaz, A.; Yilmaz, T.; Gunay, M. Elevated serum fetuin-A levels are associated with grades of retinopathy in type 2 diabetic patients. Int. Ophthalmol. 2017, 38, 2445–2450. [Google Scholar] [CrossRef]
- Orellana, J.M.; Kampe, K.; Schulze, F.; Sieber, J.; Jehle, A.W. Fetuin-A aggravates lipotoxicity in podocytes via interleukin-1 signaling. Physiol. Rep. 2017, 5, e13287. [Google Scholar] [CrossRef]
- Sato, M.; Kamada, Y.; Takeda, Y.; Kida, S.; Ohara, Y.; Fujii, H.; Akita, M.; Mizutani, K.; Yoshida, Y.; Yamada, M.; et al. Fetuin-A negatively correlates with liver and vascular fibrosis in nonalcoholic fatty liver disease subjects. Liver Int. 2014, 35, 925–935. [Google Scholar] [CrossRef] [PubMed]
- Chang, A.R.; Lazo, M.; Appel, L.J.; Gutiérrez, O.M.; E Grams, M. High dietary phosphorus intake is associated with all-cause mortality: Results from NHANES III. Am. J. Clin. Nutr. 2013, 99, 320–327. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murtaugh, M.A.; Filipowicz, R.; Baird, B.C.; Wei, G.; Greene, T.; Beddhu, S. Dietary phosphorus intake and mortality in moderate chronic kidney disease: NHANES III. Nephrol. Dial. Transplant. 2011, 27, 990–996. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yamamoto, K.T.; Robinson-Cohen, C.; De Oliveira, M.C.; Kostina, A.; Nettleton, J.A.; Ix, J.H.; Nguyen, H.; Eng, J.; Lima, J.A.; Siscovick, D.S.; et al. Dietary phosphorus is associated with greater left ventricular mass. Kidney Int. 2013, 83, 707–714. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Itkonen, S.T.; Karp, H.J.; E Kemi, V.; Kokkonen, E.M.; Saarnio, E.M.; Pekkinen, M.H.; Kärkkäinen, M.U.; A Laitinen, E.K.; I Turanlahti, M.; Lamberg-Allardt, C.J. Associations among total and food additive phosphorus intake and carotid intima-media thickness—A cross-sectional study in a middle-aged population in Southern Finland. Nutr. J. 2013, 12, 94. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vorum, H.; Ditzel, J. Disturbance of Inorganic Phosphate Metabolism in Diabetes Mellitus: Its Relevance to the Pathogenesis of Diabetic Retinopathy. J. Ophthalmol. 2014, 2014, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Ditzel, J.; Lervang, H.-H. Disturbance of inorganic phosphate metabolism in diabetes mellitus: Its impact on the development of diabetic late complications. Curr. Diabetes Rev. 2010, 6, 323–333. [Google Scholar] [CrossRef]
- Ditzel, J.; Lervang, H.H. Disturbance of inorganic phosphate metabolism in diabetes mellitus: Temporary therapeutic inter-vention trials. Diabetes Metab. Syndr. Obes. 2009, 2, 173–177. [Google Scholar]
- O’Seaghdha, C.M.; Hwang, S.-J.; Muntner, P.; Melamed, M.L.; Fox, C.S. Serum phosphorus predicts incident chronic kidney disease and end-stage renal disease. Nephrol. Dial. Transplant. 2011, 26, 2885–2890. [Google Scholar] [CrossRef] [Green Version]
- Chang, W.X.; Xu, N.; Kumagai, T.; Shiraishi, T.; Kikuyama, T.; Omizo, H.; Sakai, K.; Arai, S.; Tamura, Y.; Ota, T.; et al. The Impact of Normal Range of Serum Phosphorus on the Incidence of End-Stage Renal Disease by A Propensity Score Analysis. PLoS ONE 2016, 11, e0154469. [Google Scholar] [CrossRef]
- Xu, D.; Lv, J.; Wang, J.; Zhang, L. The association between plasma phosphorus and renal outcome - a prospective cohort of patients majorly with glomerulonephritis. Nephrol. 2016, 22, 43–48. [Google Scholar] [CrossRef]
- Da, J.; Xie, X.; Wolf, M.; Disthabanchong, S.; Wang, J.; Zha, Y.; Lv, J.; Zhang, L.; Wang, H. Serum Phosphorus and Progression of CKD and Mortality: A Meta-analysis of Cohort Studies. Am. J. Kidney Dis. 2015, 66, 258–265. [Google Scholar] [CrossRef]
- Xiang, H.; Zhang, H.; Zhou, M.; Jiang, S.; Zhang, L.; Chen, D.; Liu, Z. Phosphorus is an independent risk factor for the progression of diabetic nephropathy. Adv. Clin. Exp. Med. 2018, 27, 1239–1245. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Li, X.; Yue, R.; Ren, X.; Zhang, X.; Ni, A. The effects of diabetes mellitus and diabetic nephropathy on bone and mineral metabolism in T2DM patients. Diabetes Res. Clin. Pract. 2013, 100, 272–276. [Google Scholar] [CrossRef] [PubMed]
- Brandenburg, V.M.; Kleber, M.E.; Vervloet, M.G.; Tomaschitz, A.; Pilz, S.; Stojakovic, T.; Delgado, G.; Grammer, T.B.; Marx, N.; März, W.; et al. Fibroblast growth factor 23 (FGF23) and mortality: The Ludwigshafen Risk and Cardiovascular Health Study. Atheroscler. 2014, 237, 53–59. [Google Scholar] [CrossRef]
- Emrich, I.E.; Brandenburg, V.; Sellier, A.B.; Schauerte, J.; Wiedenroth, J.; Untersteller, K.; Lennartz, C.S.; Seiler-Mussler, S.; Wagenpfeil, S.; Fliser, D.; et al. Strength of Fibroblast Growth Factor 23 as a Cardiovascular Risk Predictor in Chronic Kidney Disease Weaken by ProBNP Adjustment. Am. J. Nephrol. 2019, 49, 203–211. [Google Scholar] [CrossRef] [PubMed]
- Stöhr, R.; Brandenburg, V.M.; Heine, G.H.; Maeder, M.T.; Leibundgut, G.; Schuh, A.; Jeker, U.; Pfisterer, M.; Wijk, S.S.; Rocca, H.B. Limited role for fibroblast growth factor 23 in assessing prognosis in heart failure patients: Data from the TIME-CHF trial. Eur. J. Hear. Fail. 2020, 22, 701–709. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chonchol, M.; Gitomer, B.; Isakova, T.; Cai, X.; Salusky, I.; Pereira, R.; Abebe, K.; Torres, V.; Steinman, T.I.; Grantham, J.J.; et al. Fibroblast Growth Factor 23 and Kidney Disease Progression in Autosomal Dominant Polycystic Kidney Disease. Clin. J. Am. Soc. Nephrol. 2017, 12, 1461–1469. [Google Scholar] [CrossRef] [PubMed]
- Fliser, D.; Kollerits, B.; Neyer, U.; Ankerst, D.P.; Lhotta, K.; Lingenhel, A.; Ritz, E.; Kronenberg, F. Fibroblast Growth Factor 23 (FGF23) Predicts Progression of Chronic Kidney Disease: The Mild to Moderate Kidney Disease (MMKD) Study. J. Am. Soc. Nephrol. 2007, 18, 2600–2608. [Google Scholar] [CrossRef]
- Scialla, J.J.; Astor, B.C.; Isakova, T.; Xie, H.; Appel, L.J.; Wolf, M. Mineral Metabolites and CKD Progression in African Americans. J. Am. Soc. Nephrol. 2013, 24, 125–135. [Google Scholar] [CrossRef] [Green Version]
- Isakova, T.; Craven, T.E.; Lee, J.; Scialla, J.J.; Xie, H.; Wahl, P.; Marcovina, S.M.; Byington, R.P.; Wolf, M. Fibroblast Growth Factor 23 and Incident CKD in Type 2 Diabetes. Clin. J. Am. Soc. Nephrol. 2014, 10, 29–38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Titan, S.M.; Zatz, R.; Graciolli, F.G.; Dos Reis, L.M.; Barros, R.T.; Jorgetti, V.; Moyses, R.M.A. FGF-23 as a Predictor of Renal Outcome in Diabetic Nephropathy. Clin. J. Am. Soc. Nephrol. 2010, 6, 241–247. [Google Scholar] [CrossRef] [Green Version]
- Agarwal, R.; Duffin, K.L.; Laska, D.A.; Voelker, J.R.; Breyer, M.D.; Mitchell, P.G. A prospective study of multiple protein biomarkers to predict progression in diabetic chronic kidney disease. Nephrol. Dial. Transplant. 2014, 29, 2293–2302. [Google Scholar] [CrossRef] [Green Version]
- De Seigneux, S.; Courbebaisse, M.; Rutkowski, J.M.; Wilhelm-Bals, A.; Metzger, M.; Khodo, S.N.; Hasler, U.; Chehade, H.; Dizin, E.; Daryadel, A.; et al. Proteinuria Increases Plasma Phosphate by Altering Its Tubular Handling. J. Am. Soc. Nephrol. 2014, 26, 1608–1618. [Google Scholar] [CrossRef] [Green Version]
- Yoon, C.-Y.; Park, J.T.; Jhee, J.H.; Noh, J.; Kee, Y.K.; Seo, C.; Lee, M.; Cha, M.-U.; Kim, H.; Park, S.; et al. High dietary phosphorus density is a risk factor for incident chronic kidney disease development in diabetic subjects: A community-based prospective cohort study. Am. J. Clin. Nutr. 2017, 106, 311–321. [Google Scholar] [CrossRef] [Green Version]
- Tonelli, M. Serum phosphorus in people with chronic kidney disease: You are what you eat. Kidney Int. 2013, 84, 871–873. [Google Scholar] [CrossRef] [PubMed]
- Ketteler, M.; Block, G.A.; Evenepoel, P.; Fukagawa, M.; Herzog, C.A.; McCann, L.; Moe, S.M.; Shroff, R.; Tonelli, M.A.; Toussaint, N.D.; et al. Executive summary of the 2017 KDIGO Chronic Kidney Disease–Mineral and Bone Disorder (CKD-MBD) Guideline Update: What’s changed and why it matters. Kidney Int. 2017, 92, 26–36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- KDIGO 2017 Clinical Practice Guideline Update for the Diagnosis, Evaluation, Prevention, and Treatment of Chronic Kidney Disease–Mineral and Bone Disorder (CKD-MBD). Kidney Int. Suppl. 2017, 7, 1–59. [CrossRef] [PubMed] [Green Version]
- Block, G.A.; Wheeler, D.C.; Persky, M.S.; Kestenbaum, B.; Ketteler, M.; Spiegel, D.M.; Allison, M.A.; Asplin, J.; Smits, G.; Hoofnagle, A.N.; et al. Effects of Phosphate Binders in Moderate CKD. J. Am. Soc. Nephrol. 2012, 23, 1407–1415. [Google Scholar] [CrossRef]
- Isakova, T.; Gutiérrez, O.M.; Chang, Y.; Shah, A.; Tamez, H.; Smith, K.; Thadhani, R.; Wolf, M. Phosphorus Binders and Survival on Hemodialysis. J. Am. Soc. Nephrol. 2008, 20, 388–396. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Andía, J.B.C.; Martín, J.L.F.; Locatelli, F.; London, G.; Gorriz, J.L.; Floege, J.; FerreKetteler, M.; Ferreira, A.; Covic, A.; Rutkowski, B.; et al. Use of phosphate-binding agents is associated with a lower risk of mortality. Kidney Int. 2013, 84, 998–1008. [Google Scholar] [CrossRef] [Green Version]
- A Jamal, S.; VanderMeer, B.; Raggi, P.; Mendelssohn, D.C.; Chatterley, T.; Dorgan, M.; E Lok, C.; Fitchett, D.; Tsuyuki, R.T. Effect of calcium-based versus non-calcium-based phosphate binders on mortality in patients with chronic kidney disease: An updated systematic review and meta-analysis. Lancet 2013, 382, 1268–1277. [Google Scholar] [CrossRef]
- Patel, L.; Bernard, L.M.; Elder, G.J. Sevelamer Versus Calcium-Based Binders for Treatment of Hyperphosphatemia in CKD: A Meta-Analysis of Randomized Controlled Trials. Clin. J. Am. Soc. Nephrol. 2015, 11, 232–244. [Google Scholar] [CrossRef] [Green Version]
- Floege, J. Phosphate binders in chronic kidney disease: An updated narrative review of recent data. J. Nephrol. 2019, 33, 497–508. [Google Scholar] [CrossRef]
- Luo, Q.; Lao, C.; Huang, C.; Xia, Y.; Ma, W.; Liu, W.; Chen, Z. Iron Overload Resulting from the Chronic Oral Administration of Ferric Citrate Impairs Intestinal Immune and Barrier in Mice. Biol. Trace Element Res. 2021, 199, 1027–1036. [Google Scholar] [CrossRef] [PubMed]
- Peter, W.L.S.; Wazny, L.D.; Weinhandl, E.; Cardone, K.E.; Hudson, J.Q. A Review of Phosphate Binders in Chronic Kidney Disease: Incremental Progress or Just Higher Costs? Drugs 2017, 77, 1155–1186. [Google Scholar] [CrossRef] [PubMed]
- Ruospo, M.; Palmer, S.C.; Natale, P.; Craig, J.C.; Vecchio, M.; Elder, G.J.; Strippoli, G.F. Phosphate binders for preventing and treating chronic kidney disease-mineral and bone disorder (CKD-MBD). Cochrane Database Syst. Rev. 2018, 8, CD006023. [Google Scholar] [CrossRef] [PubMed]
- Di Iorio, B.; Bellasi, A.; Russo, D. On behalf of the INDEPENDENT study investigators Mortality in Kidney Disease Patients Treated with Phosphate Binders: A Randomized Study. Clin. J. Am. Soc. Nephrol. 2012, 7, 487–493. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jean, G.; Vanel, T.; Terrat, J.; Hurot, J.; Lorriaux, C.; Mayor, B.; Chazot, C. Treating mineral metabolism disorders in patients undergoing long hemodialysis: A search for an optimal strategy. Hemodial. Int. 2009, 13, 526–532. [Google Scholar] [CrossRef]
- de Boer, I.H.; Caramori, M.L.; Chan, J.C.; Heerspink, H.J.; Hurst, C.; Khunti, K.; Liew, A.; Michos, E.D.; Navaneethan, S.D.; Olowu, W.A.; et al. KDIGO 2020 Clinical Practice Guideline for Diabetes Management in Chronic Kidney Disease. Kidney Int. 2020, 98, S1–S115. [Google Scholar] [CrossRef]
- American Diabetes Association. Standards of medical care in diabetes-2021. Diabetes Care 2021, 44, S1–S232. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Winiarska, A.; Filipska, I.; Knysak, M.; Stompór, T. Dietary Phosphorus as a Marker of Mineral Metabolism and Progression of Diabetic Kidney Disease. Nutrients 2021, 13, 789. https://doi.org/10.3390/nu13030789
Winiarska A, Filipska I, Knysak M, Stompór T. Dietary Phosphorus as a Marker of Mineral Metabolism and Progression of Diabetic Kidney Disease. Nutrients. 2021; 13(3):789. https://doi.org/10.3390/nu13030789
Chicago/Turabian StyleWiniarska, Agata, Iwona Filipska, Monika Knysak, and Tomasz Stompór. 2021. "Dietary Phosphorus as a Marker of Mineral Metabolism and Progression of Diabetic Kidney Disease" Nutrients 13, no. 3: 789. https://doi.org/10.3390/nu13030789