Functional Health Literacy: Psychometric Properties of the Newest Vital Sign for Portuguese Adolescents (NVS-PTeen)
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Sampling and Participants
2.3. Instruments of Data Collection
2.4. Statistical Analysis
2.5. Ethical Considerations
3. Results
3.1. Sample Characterization
3.2. Functional Health Literacy among Adolescents
3.3. Internal Consistency and Test-Retest Reliability
3.4. Convergent Validity of the NVS-PTeen
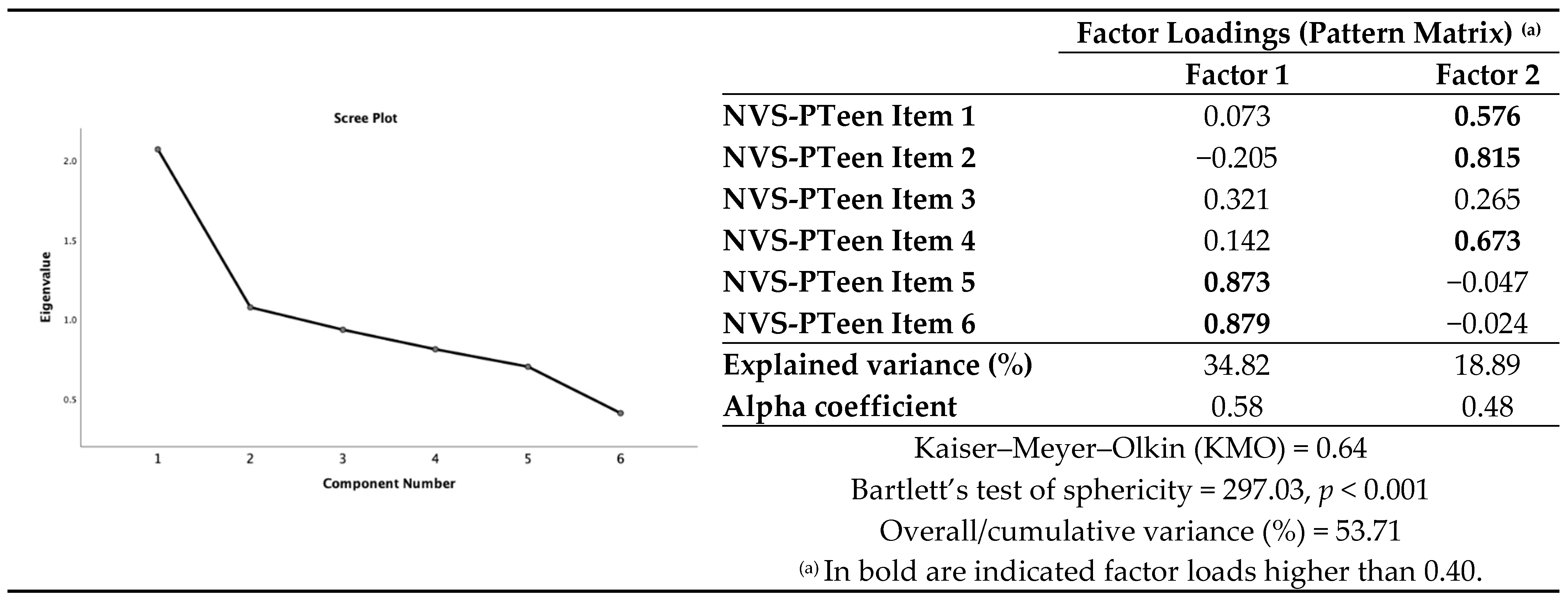
3.5. Construct Validity-Dimensionality
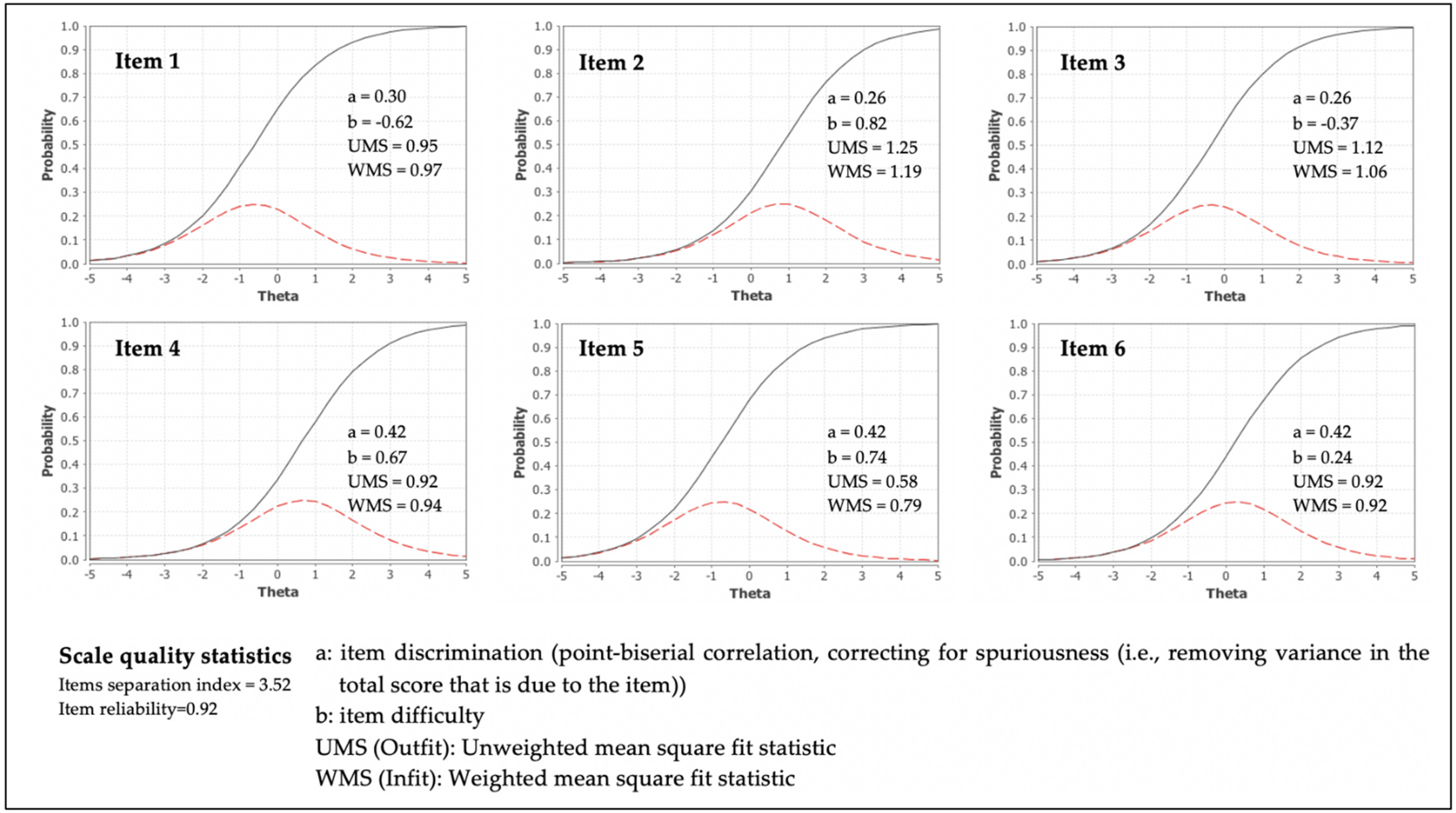
3.6. Item Response Theory (IRT): Item Difficulty, Discrimination, and Fit
4. Discussion
4.1. Prevalence of Adequate Health Literacy in the Adolescent Sample under Study
4.2. Psychometric Properties of the NVS-PTeen
4.3. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sørensen, K.; Van den Broucke, S.; Fullam, J.; Doyle, G.; Pelikan, J.; Slonska, Z.; Brand, H. Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health 2012, 12, 80. [Google Scholar] [CrossRef] [PubMed]
- Ratzan, S.C.; Parker, R.M. Health literacy - identification and response. J. Health Commun. 2006, 11, 713–715. [Google Scholar] [CrossRef]
- Nutbeam, D.; McGill, B.; Premkumar, P. Improving health literacy in community populations: A review of progress. Health Promot. Int. 2018, 33, 901–911. [Google Scholar] [CrossRef] [PubMed]
- Nutbeam, D. Health literacy as a public health goal: A challenge for contemporary health education and communication strategies into the 21st century. Health Promot. Int. 2000, 15, 259–267. [Google Scholar] [CrossRef]
- Chinn, D. Critical health literacy: A review and critical analysis. Soc. Sci. Med. 2011, 73, 60–67. [Google Scholar] [CrossRef]
- Eichler, K.; Wieser, S.; Brügger, U. The costs of limited health literacy: A systematic review. Int. J. Public Health 2009, 54, 313–324. [Google Scholar] [CrossRef]
- Weishaar, H.; Hurrelmann, K.; Okan, O.; Horn, A.; Schaeffer, D. Framing health literacy: A comparative analysis of national action plans. Health Policy 2019, 123, 11–20. [Google Scholar] [CrossRef] [PubMed]
- Sørensen, K.; Pelikan, J.M.; Röthlin, F.; Ganahl, K.; Slonska, Z.; Doyle, G.; Fullam, J.; Kondilis, B.; Agrafiotis, D.; Uiters, E.; et al. Health literacy in Europe: Comparative results of the European Health Literacy Survey (HLS-EU). Eur. J. Public Health 2015, 25, 1053–1058. [Google Scholar] [CrossRef]
- Espanha, R.; Ávila, P. Health Literacy Survey Portugal: A contribution for the knowledge on health and communications. Procedia Comput. Sci. 2016, 100, 1033–1041. [Google Scholar] [CrossRef]
- Pedro, A.R.; Amaral, O.; Escoval, A. Literacia em saúde, dos dados à ação: Tradução, validação e aplicação do European Health Literacy Survey em Portugal. Rev. Port. Saude Publica 2016, 34, 259–275. [Google Scholar] [CrossRef]
- Guo, S.; Armstrong, R.; Waters, E.; Sathish, T.; Alif, S.M.; Browne, G.R.; Yu, X. Quality of health literacy instruments used in children and adolescents: A systematic review. BMJ Open 2018, 8, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Manganello, J. Health literacy and adolescents: A framework and agenda for future research. Health Educ. Res. 2008, 23, 840–847. [Google Scholar] [CrossRef]
- Ormshaw, M.J.; Paakkari, L.T.; Kannas, L.K. Measuring child and adolescent health literacy: A systematic review of literature. Health Educ. 2013, 113, 433–455. [Google Scholar] [CrossRef]
- Perry, E.L. Health literacy in adolescents: An integrative review. J. Spec. Pediatr. Nurs. 2014, 19, 210–218. [Google Scholar] [CrossRef] [PubMed]
- Sansom-Daly, U.M.; Lin, M.; Robertson, E.G.; Wakefield, C.E.; McGill, B.C.; Girgis, A.; Cohn, R.J. Health literacy in adolescents and young adults: An updated review. J. Adolesc. Young Adult Oncol. 2016, 5, 106–118. [Google Scholar] [CrossRef] [PubMed]
- Chari, R.; Warsh, J.; Ketterer, T.; Hossain, J.; Sharif, I. Association between health literacy and child and adolescent obesity. Patient Educ. Couns. 2014, 94, 61–66. [Google Scholar] [CrossRef]
- Morrison, A.K.; Schapira, M.M.; Gorelick, M.H.; Hoffmann, R.G.; Brousseau, D.C. Low caregiver health literacy is associated with higher pediatric emergency department use and nonurgent visits. Acad. Pediatr. 2014, 14, 309–314. [Google Scholar] [CrossRef]
- Feldman, S.S.; Elliott, G.R. At the Threshold: The Developing Adolescent; Harvard University Press: Cambridge, MA, USA, 1990. [Google Scholar]
- Yurgelun-Todd, D. Emotional and cognitive changes during adolescence. Curr. Opin. Neurobiol. 2007, 17, 251–257. [Google Scholar] [CrossRef] [PubMed]
- Sisk, C.L.; Zehr, J.L. Pubertal hormones organize the adolescent brain and behavior. Front. Neuroendocrinol. 2005, 26, 163–174. [Google Scholar] [CrossRef] [PubMed]
- Adams, G.R.; Berzonsky, M.D. Blackwell Handbook of Adolescence; Blackwell Publishing Ltd.: Malden, MA, USA, 2006. [Google Scholar]
- Dahl, R.E.; Forbes, E.E. Pubertal development and behavior: Hormonal activation of social and motivational tendencies. Brain Cogn. 2010, 72, 66–72. [Google Scholar] [CrossRef]
- Viner, R.M.; Ozer, E.M.; Denny, S.; Marmot, M.; Resnick, M.; Fatusi, A.; Currie, C. Adolescence and the social determinants of health. Lancet 2012, 379, 1641–1652. [Google Scholar] [CrossRef]
- Yang, T.-C.; Chen, I.-C.; Choi, S.-W.; Kurtulus, A. Linking perceived discrimination during adolescence to health during mid-adulthood: Self-esteem and risk-behavior mechanisms. Soc. Sci. Med. 2019, 232, 434–443. [Google Scholar] [CrossRef] [PubMed]
- Landstedt, E.; Hammarstrom, A.; Winefield, H. How well do parental and peer relationships in adolescence predict health in adulthood? Scand. J. Public Health 2015, 43, 460–468. [Google Scholar] [CrossRef]
- Begoray, D.L.; Wharf-Higgins, J.; MacDonald, M. High school health curriculum and health literacy: Canadian student voices. Glob. Health Promot. 2009, 16, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Kilgour, L.; Matthews, N.; Christian, P.; Shire, J. Health literacy in schools: Prioritising health and well-being issues through the curriculum. Sport. Educ. Soc. 2015, 20, 485–500. [Google Scholar] [CrossRef]
- Leger, L.S. Schools, health literacy and public health: Possibilities and challenges. Health Promot. Int. 2001, 16, 197–205. [Google Scholar] [CrossRef]
- Okan, O.; Lopes, E.; Bollweg, T.M.; Bröder, J.; Messer, M.; Bruland, D.; Bond, E.; Carvalho, G.S.; Sørensen, K.; Saboga-Nunes, L.; et al. Generic health literacy measurement instruments for children and adolescents: A systematic review of the literature. BMC Public Health 2018, 18, 166. [Google Scholar] [CrossRef] [PubMed]
- Bröder, J.; Okan, O.; Bauer, U.; Bruland, D.; Schlupp, S.; Bollweg, T.M.; Saboga-Nunes, L.; Bond, E.; Sørensen, K.; Bitzer, E.-M.; et al. Health literacy in childhood and youth: A systematic review of definitions and models. BMC Public Health 2017, 17, 361. [Google Scholar] [CrossRef]
- Parker, R.M.; Baker, D.W.; Willia, M.V.; Nurss, J.R. The Test of Functional Health Literacy in adults: A new instrument for measuring patients’ literacy skills. J. Gen. Intern. Med. 1995, 10, 537–541. [Google Scholar] [CrossRef]
- Murphy, P.W.; Davis, T.C.; Long, S.W.; Jackson, R.H.; Decker, B.C. Rapid Estimate of Adult Literacy in Medicine (REALM): A quick reading test for patients. J. Read. 1993, 37, 124–130. [Google Scholar]
- Weiss, B.D.; Mays, M.Z.; Martz, W.; Castro, K.M.; DeWalt, D.A.; Pignone, M.P.; Mockbee, J.; Hale, F.A. Quick assessment of literacy in primary care: The Newest Vital Sign. Ann. Fam. Med. 2005, 3, 514–522. [Google Scholar] [CrossRef] [PubMed]
- Rowlands, G.; Khazaezadeh, N.; Oteng-Ntim, E.; Seed, P.; Barr, S.; Weiss, B.D. Development and validation of a measure of health literacy in the UK: The Newest Vital Sign. BMC Public Health 2013, 13, 116. [Google Scholar] [CrossRef] [PubMed]
- Johnson, K.; Weiss, B.D. How long does it take to assess literacy skills in clinical practice? J. Am. Board Fam. Med. 2008, 21, 211–214. [Google Scholar] [CrossRef]
- Santos, O.; Oliveira, A.; Carvalho, C.; Lunet, N.; Azevedo, A.; Paiva, D.; do Carmo, I. Self-administration of the Newest Vital Sign in Portuguese young adults: Study of its internal reliability. In Proceedings of the Abstracts from the ICBM 2012 Meeting, Budapeste, Hungary, 29 August–1 September 2021; p. S189. [Google Scholar]
- Paiva, D.; Silva, S.; Severo, M.; Moura-Ferreira, P.; Lunet, N.; Azevedo, A. Limited health literacy in Portugal assessed with the Newest Vital Sign. Acta Med. Port. 2017, 30, 861–869. [Google Scholar] [CrossRef] [PubMed]
- Anthoine, E.; Moret, L.; Regnault, A.; Sbille, V.; Hardouin, J.B. Sample size used to validate a scale: A review of publications on newly-developed patient reported outcomes measures. Health Qual. Life Outcomes 2014, 12, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Salgado, T.M.; Ramos, S.B.; Sobreira, C.; Canas, R.; Cunha, I.; Benrimoj, S.I.; Fernandez-Llimos, F. Newest Vital Sign as a proxy for medication adherence in older adults. J. Am. Pharm. Assoc. 2013, 53, 611–617. [Google Scholar] [CrossRef]
- Martins, A.C.; Andrade, I.M. Cross-cultural adaptation and validation of the Portuguese version of the Newest Vital Sign. Rev. Enferm. Ref. 2014, IV, 75–83. [Google Scholar] [CrossRef]
- Aaronson, N.; Alonso, J.; Burnam, A.; Lohr, K.; Patrick, D.; Perrin, E.; Stein, R. Assessing health status and quality-of-life instruments: Attributes and review criteria. Qual. Life Res. 2002, 11, 193–205. [Google Scholar] [CrossRef]
- Kuder, G.F.; Richardson, M.W. The theory of the estimation of test reliability. Psychometrika 1937, 2, 151–160. [Google Scholar] [CrossRef]
- Nunnally, J.C.; Bernstein, I.H. Psychometric Theory; McGraw-Hill, Inc.: New York, NY, USA, 1994. [Google Scholar]
- Huang, Y.M.; Shiyanbola, O.O.; Smith, P.D.; Chan, H.Y. Quick screen of patients’ numeracy and document literacy skills: The factor structure of the Newest Vital Sign. Patient Prefer. Adherence 2018, 12, 853–859. [Google Scholar] [CrossRef]
- Meyer, P. Applied measurement with Jmetrik; Rutledge: New York, NY, USA, 2014; ISBN 9780203115190. [Google Scholar]
- World Medical Association (WMA) World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [CrossRef] [PubMed]
- Rasu, R.; Bawa, W.A.; Suminski, R.; Snella, K.; Warady, B. Health literacy impact on national healthcare utilization and expenditure. Int. J. Heal. Policy Manag. 2015, 4, 747–755. [Google Scholar] [CrossRef]
- MacLeod, S.; Musich, S.; Gulyas, S.; Cheng, Y.; Tkatch, R.; Cempellin, D.; Bhattarai, G.R.; Hawkins, K.; Yeh, C.S. The impact of inadequate health literacy on patient satisfaction, healthcare utilization, and expenditures among older adults. Geriatr. Nurs. 2017, 38, 334–341. [Google Scholar] [CrossRef] [PubMed]
- Shieh, C.; Halstead, J.A. Understanding the impact of health literacy on women’s health. J. Obstet. Gynecol. Neonatal Nurs. 2009, 38, 601–612. [Google Scholar] [CrossRef]
- Baker, D.W. The meaning and the measure of health literacy. J. Gen. Intern. Med. 2006, 21, 878–883. [Google Scholar] [CrossRef] [PubMed]
- Weiss, B.D. The use of the Newest Vital Sign in children. HLRP Heal. Lit. Res. Pract. 2019, 3, e19. [Google Scholar] [CrossRef] [PubMed]
- Keating, D.P. Cognitive and brain development in adolescence. Enfance 2012, 3, 267–279. [Google Scholar] [CrossRef]
- Rosa, A.; Loureiro, L.; Sequeira, C. Literacia em saúde mental sobre depressão: Um estudo com adolescentes portugueses. Rev. Port. Enferm. Saúde Ment. 2019, 21, 40–46. [Google Scholar] [CrossRef]
- Manganello, J.A.; DeVellis, R.F.; Davis, T.C.; Schottler-Thal, C. Development of the Health Literacy Assessment Scale for Adolescents (HAS-A). J. Commun. Healthc. 2015, 8, 172–184. [Google Scholar] [CrossRef]
- Público Comunicação Social SA Ranking das Escolas. 2017. Available online: https://www.publico.pt/ranking-das-escolas-2017/lista (accessed on 30 December 2020).
- Driessnack, M.; Chung, S.; Perkhounkova, E.; Hein, M. Using the “Newest Vital Sign” to assess health literacy in children. J. Pediatr. Heal. Care 2014, 28, 165–171. [Google Scholar] [CrossRef] [PubMed]
- Kogure, T.; Sumitani, M.; Suka, M.; Ishikawa, H.; Odajima, T.; Igarashi, A.; Kusama, M.; Okamoto, M.; Sugimori, H.; Kawahara, K. Validity and reliability of the Japanese version of the Newest Vital Sign: A preliminary study. PLoS One 2014, 9, e94582. [Google Scholar] [CrossRef] [PubMed]
- Mansfield, E.D.; Wahba, R.; Gillis, D.E.; Weiss, B.D.; L’Abbé, M. Canadian adaptation of the Newest Vital Sign©, a health literacy assessment tool. Public Health Nutr. 2018, 21, 2038–2045. [Google Scholar] [CrossRef]
- Tseng, H.-M.; Liao, S.-F.; Wen, Y.-P.; Chuang, Y.-J. Adaptation and validation of a measure of health literacy in Taiwan: The Newest Vital Sign. Biomed. J. 2018, 41, 273–278. [Google Scholar] [CrossRef] [PubMed]
- Welch, V.L.; VanGeest, J.B.; Caskey, R. Time, costs, and clinical utilization of screening for health literacy: A case study using the Newest Vital Sign (NVS) instrument. J. Am. Board Fam. Med. 2011, 24, 281–289. [Google Scholar] [CrossRef]
- Hoffman, S.; Marsiglia, F.F.; Lambert, M.C.; Porta, M. A psychometric assessment of the Newest Vital Sign among youth in Guatemala city. J. Child Adolesc. Behav. 2015, 3, 190. [Google Scholar] [CrossRef]
- Warsh, J.; Chari, R.; Badaczewski, A.; Hossain, J.; Sharif, I. Can the Newest Vital Sign be used to assess health literacy in children and adolescents? Clin. Pediatr. 2014, 53, 141–144. [Google Scholar] [CrossRef] [PubMed]
- Tavakol, M.; Dennick, R. Making sense of Cronbach’s alpha. Int. J. Med. Educ. 2011, 2, 53–55. [Google Scholar] [CrossRef] [PubMed]
- Schmitt, N. Uses and abuses of coefficient alpha. Psychol. Assess. 1995, 8, 350–353. [Google Scholar] [CrossRef]
- Cruvinel, A.F.P.; Méndez, D.A.C.; Chaves, G.C.; Gutierres, E.; Lotto, M.; Oliveira, T.M.; Cruvinel, T. The Brazilian validation of a health literacy instrument: The Newest Vital Sign. Acta Odontol. Scand. 2018, 1–8. [Google Scholar] [CrossRef]
- Zotti, P.; Cocchi, S.; Polesel, J.; Mis, C.C.; Bragatto, D.; Cavuto, S.; Conficconi, A.; Costanzo, C.; De Giorgi, M.; Drace, C.A.; et al. Cross-cultural validation of health literacy measurement tools in Italian oncology patients. BMC Health Serv. Res. 2017, 17, 410. [Google Scholar] [CrossRef]
- Fransen, M.P.; Leenaars, K.E.F.; Rowlands, G.; Weiss, B.D.; Maat, H.P.; Essink-Bot, M.L. International application of health literacy measures: Adaptation and validation of the Newest Vital Sign in The Netherlands. Patient Educ. Couns. 2014, 97, 403–409. [Google Scholar] [CrossRef] [PubMed]
- Fransen, M.P.; Van Schaik, T.M.; Twickler, T.B.; Essink-Bot, M.L. Applicability of internationally available health literacy measures in the Netherlands. J. Health Commun. 2011, 16, 134–149. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, R.; De Andrade, S.M.; González, A.D.; Birolim, M.M.; Mesas, A.E. Cross-cultural adaptation and validation of the Newest Vital Sign (NVS) health literacy instrument in general population and highly educated samples of Brazilian adults. Public Health Nutr. 2017, 20, 1907–1913. [Google Scholar] [CrossRef] [PubMed]
- Frost, M.H.; Reeve, B.B.; Liepa, A.M.; Stauffer, J.W.; Hays, R.D.; Sloan, J.A. What is sufficient evidence for the reliability and validity of patient-reported outcome measures? Value Heal. 2007, 10, S94–S105. [Google Scholar] [CrossRef]
- Kipping, R.R.; Campbell, R.M.; MacArthur, G.J.; Gunnell, D.J.; Hickman, M. Multiple risk behaviour in adolescence. J. Public Health 2012, 34, i1–i2. [Google Scholar] [CrossRef] [PubMed]
- Kupersmidt, J.B.; Scull, T.M.; Austin, E.W. Media literacy education for elementary school substance use prevention: Study of media detective. Pediatrics 2010, 126, 525–531. [Google Scholar] [CrossRef]
- Winkelman, T.N.A.; Caldwell, M.T.; Bertram, B.; Davis, M.M. Promoting health literacy for children and adolescents. Pediatrics 2016, 138, e20161937. [Google Scholar] [CrossRef]
| Female (n = 191) | Male (n = 195) | Total (N = 386) | p-Value 1 | ||
|---|---|---|---|---|---|
| Age (years) | 12 | 14 (7.3%) | 14 (7.2%) | 28 (7.3%) | 0.672 |
| 13 | 49 (25.7%) | 45 (23.1%) | 94 (24.4%) | ||
| 14 | 39 (20.4%) | 54 (27.7%) | 93 (24.1%) | ||
| 15 | 35 (18.3%) | 30 (15.4%) | 65 (16.8%) | ||
| 16 | 33 (17.3%) | 34 (17.4%) | 67 (17.4%) | ||
| 17 | 21 (11.0%) | 18 (9.2%) | 39 (10.1%) | ||
| Mean (±SD) | 14.46 (1.49) | 14.41 (1.43) | 14.43 (1.46) | 0.791 | |
| Median | 14.00 | 14.00 | 14.00 | ||
| Educational level | Grade 8 | 66 (34.6%) | 60 (30.8%) | 126 (32.6%) | |
| Grade 9 | 43 (22.5%) | 61 (31.3%) | 104 (26.9%) | ||
| Grade 10 | 29 (15.2%) | 21 (10.8%) | 50 (13.0%) | 0.321 | |
| Grade 11 | 35 (18.3%) | 36 (18.5%) | 71 (18.4%) | ||
| Grade 12 | 18 (9.4%) | 17 (8.7%) | 35 (9.1%) |
| NVS-PTeen Items (I) | NVS Total Score (Range: 0–6; Mean ± SD) | Health Literacy Level | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| I1 (%) | I2 (%) | I3 (%) | I4 (%) | I5 (%) | I6 (%) | Inadequate (Score 0–1; %) | Limited (Score 2–3; %) | Adequate (Score 4–6; %) | |||
| Sex | Female (n = 191) | 84.3 | 71.2 | 83.2 | 71.2 | 90.6 | 79.1 | 4.72 ± 1.41 | 3.7 | 15.7 | 80.6 |
| Male (n = 195) | 92.3 | 71.3 | 88.7 | 75.4 | 88.2 | 79.0 | 4.86 ± 1.27 | 2.1 | 11.3 | 86.7 | |
| p-value 1 | 0.014 | 0.987 | 0.121 | 0.353 | 0.450 | 0.984 | 0.526 | 0.259 | |||
| Educational level | Grade 8 (n = 126) | 84.1 | 61.1 | 86.5 | 57.1 | 84.9 | 63.5 | 4.27 ± 1.47 | 4.8 | 23.8 | 72.2 |
| Grade 9 (n = 104) | 85.6 | 73.1 | 76.9 | 64.4 | 86.5 | 78.8 | 4.50 ± 1.31 | 3.8 | 16.3 | 79.8 | |
| Grade 10 (n = 50) | 94.0 | 94.0 | 96.0 | 96.0 | 96.0 | 92.0 | 5.68 ± 0.89 | 2.0 | 2.0 | 96.0 | |
| Grade 11 (n = 71) | 90.1 | 73.2 | 88.7 | 88.7 | 95.8 | 91.0 | 5.28 ± 1.03 | 0.0 | 5.6 | 94.4 | |
| Grade 12 (n = 35) | 100.0 | 65.7 | 91.4 | 97.1 | 91.4 | 94.3 | 5.29 ± 0.83 | 0.0 | 2.9 | 97.1 | |
| p-value 2 | 0.053 | 0.001 | 0.013 | <0.001 | 0.060 | <0.001 | <0.001 | <0.001 | |||
| Total (N = 386) | 88.3 | 71.2 | 86.0 | 73.3 | 89.4 | 79.0 | 4.79 ± 1.34 | 2.8 | 13.5 | 83.4 | |
| Item 2 | Item 3 | Item 4 | Item 5 | Item 6 | NVS-PTeen Total Score | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| rho | OR (95% CI) | rho | OR (95% CI) | rho | OR (95% CI) | rho | OR (95% CI) | rho | OR (95% CI) | rho | |
| Item 1:If you eat the whole container of ice cream, how many calories are you going to consume? | 0.197 ** | 3.33 (1.77–6.29) | 0.179 ** | 3.40 (1.67–6.93) | 0.201 ** | 3.41 (1.81–6.44) | 0.163 ** | 3.35 (1.54–7.29) | 0.170 ** | 2.94 (1.53–5.67) | 0.445 ** |
| Item 2:If you could eat 60 g of carbohydrates, what quantity of ice cream would you be able to eat? | 0.057 | 1.42 (0.77–2.60) | 0.315 ** | 4.37 (2.69–7.09) | 0.115 * | 2.12 (1.10–4.11) | 0.094 | 1.63 (0.97–2.73) | 0.596 ** | ||
| Item 3:Your doctor has advised you to reduce the amount of saturated fat in your diet. You generally eat 42 g of saturated fat per day, which includes one portion of ice cream. If you were to stop eating ice cream, how many grams of saturated fat would you be consuming per day? | 0.213 ** | 3.37 (1.86–6.09) | 0.176 ** | 3.44 (1.65–7.17) | 0.196 * | 3.18 (1.73–5.86) | 0.447 ** | ||||
| Item 4:If you generally eat 2500 calories per day, what percentage of the daily value of calories would you be consuming if you ate one portion of ice cream? | 0.210 ** | 3.77 (1.95–7.32) | 0.264 ** | 3.75 (2.24–6.28) | 0.662 ** | ||||||
| Item 5:Is it safe for you to eat this ice cream? | 0.586 * | 63.28 (21.51–186.15) | 0.498 ** | ||||||||
| Item 6 (asked if the participant answered no to item 5): Why not? | 0.599 ** | ||||||||||
| Coefficient α If Item Deleted (N = 386) | Item Difficulty: % of Students Answering the Item Correctly (N = 386) | Temporal Reliability | ||
|---|---|---|---|---|
| % of Test-Retest Accuracy (n = 127) | % of Test-Retest Score Improvement (n = 127) | |||
| Item 1 | 0.58 | 88.3% | 96.9% | 0.8% |
| Item 2 | 0.60 | 71.2% | 66.1% | 27.6% |
| Item 3 | 0.59 | 86.0% | 78.7% | 7.1% |
| Item 4 | 0.52 | 73.3% | 81.9% | 6.3% |
| Item 5 | 0.53 | 89.4% | 92.9% | 3.1% |
| Item 6 | 0.53 | 79.0% | 86.6% | 10.2% |
| Pearson’s r | |
|---|---|
| Age (N = 386) | 0.19 * |
| Educational level (N = 386) | 0.31 ** |
| Final classification: Portuguese 1 (N = 386) | 0.28 ** |
| Final classification: mathematics 1 (N = 358) | 0.31 ** |
| Average final classification: Portuguese and mathematics 1 (N = 358) | 0.39 ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Santos, O.; Stefanovska-Petkovska, M.; Virgolino, A.; Miranda, A.C.; Costa, J.; Fernandes, E.; Cardoso, S.; Vaz Carneiro, A. Functional Health Literacy: Psychometric Properties of the Newest Vital Sign for Portuguese Adolescents (NVS-PTeen). Nutrients 2021, 13, 790. https://doi.org/10.3390/nu13030790
Santos O, Stefanovska-Petkovska M, Virgolino A, Miranda AC, Costa J, Fernandes E, Cardoso S, Vaz Carneiro A. Functional Health Literacy: Psychometric Properties of the Newest Vital Sign for Portuguese Adolescents (NVS-PTeen). Nutrients. 2021; 13(3):790. https://doi.org/10.3390/nu13030790
Chicago/Turabian StyleSantos, Osvaldo, Miodraga Stefanovska-Petkovska, Ana Virgolino, Ana Cristina Miranda, Joana Costa, Elisabete Fernandes, Susana Cardoso, and António Vaz Carneiro. 2021. "Functional Health Literacy: Psychometric Properties of the Newest Vital Sign for Portuguese Adolescents (NVS-PTeen)" Nutrients 13, no. 3: 790. https://doi.org/10.3390/nu13030790
APA StyleSantos, O., Stefanovska-Petkovska, M., Virgolino, A., Miranda, A. C., Costa, J., Fernandes, E., Cardoso, S., & Vaz Carneiro, A. (2021). Functional Health Literacy: Psychometric Properties of the Newest Vital Sign for Portuguese Adolescents (NVS-PTeen). Nutrients, 13(3), 790. https://doi.org/10.3390/nu13030790






