Implementation of WHO Recommended Policies and Interventions on Healthy Diet in the Countries of the Eastern Mediterranean Region: From Policy to Action
Abstract
1. Introduction
- Reduce the prevalence of overweight in children under five to not more than 3%
- Halt the rise in diabetes and obesity in adults
- Halt the rise in overweight in school-age children and adolescents 5–18 years old
- Reduce mean population intake of salt/sodium by 30%, and
- Virtually eliminate industrially-produced trans-fatty acids from the food supply.
- Progressively reduce intakes of salt, sugars and saturated fats by improving the nutritional quality of foods through government-led reformulation programmes
- Implement a tax on sugar-sweetened beverages and use other taxes and subsidies to promote healthy diets
- Review food subsidy programmes and progressively eliminate subsidies for all types of fats/oils and sugars
- Implement mandatory standards for ingredient listing, back-of-pack nutrient declarations and simplified front-of-pack labelling for all pre-packaged foods
- Introduce and enforce mandatory guidelines for provision of healthy food in public institutions, and
- Implement the WHO Set of recommendations on marketing of foods and non-alcoholic beverages to children.
2. Materials and Methods
- governance, including multisectoral coordination
- inclusion of promotion of healthy diet and prevention of obesity and diet-related NCDs in recent policies, strategies or plans
- school nutrition and health
- education and information
- nutrition labelling
- elimination of industrially-produced trans-fatty acids from the food supply
- reducing levels of salt, sugars and saturated fats in the food supply
- marketing restrictions
- fiscal measures (taxes and subsidies), and
- food and nutrition surveillance and food composition data.
3. Results
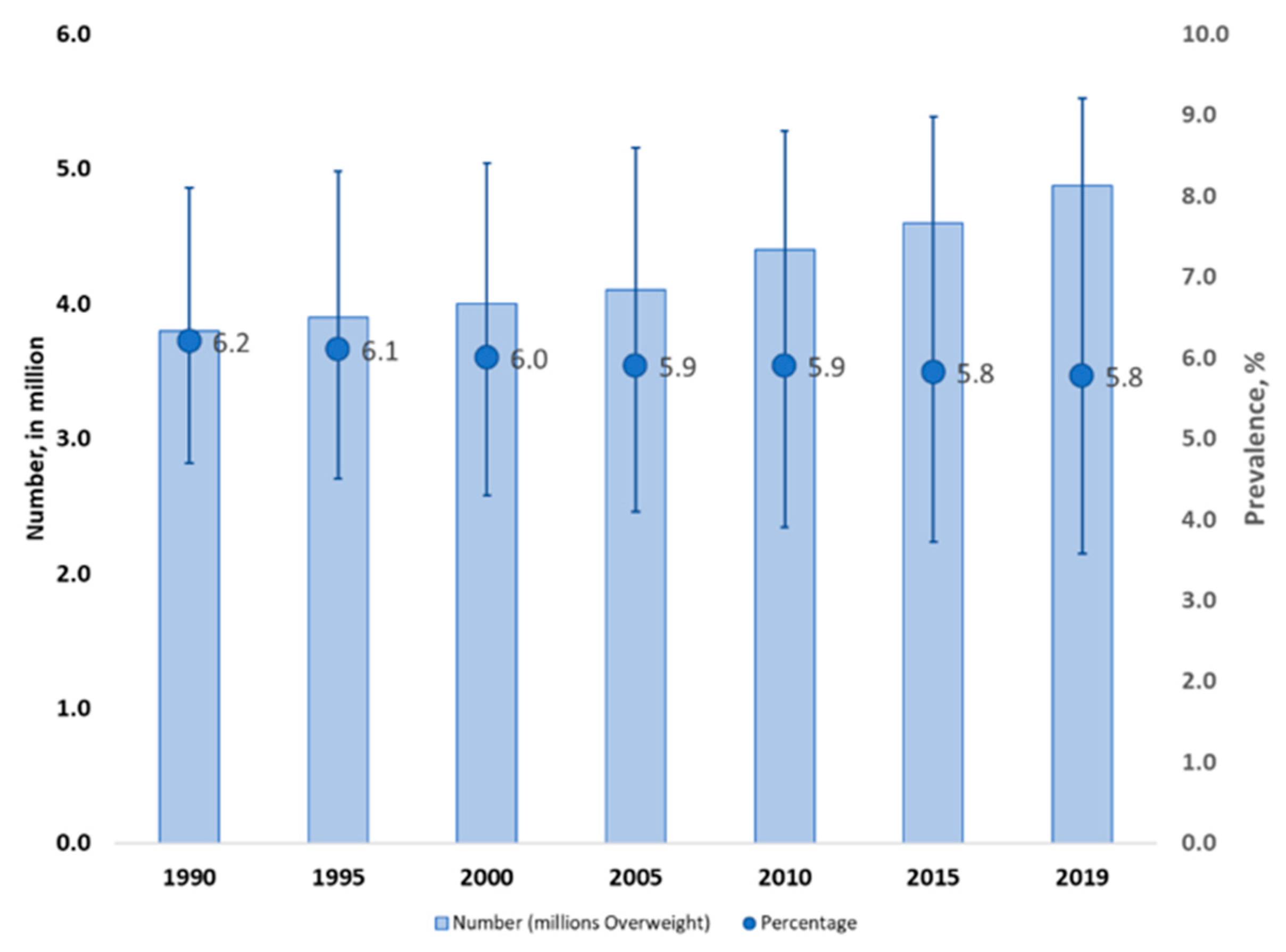
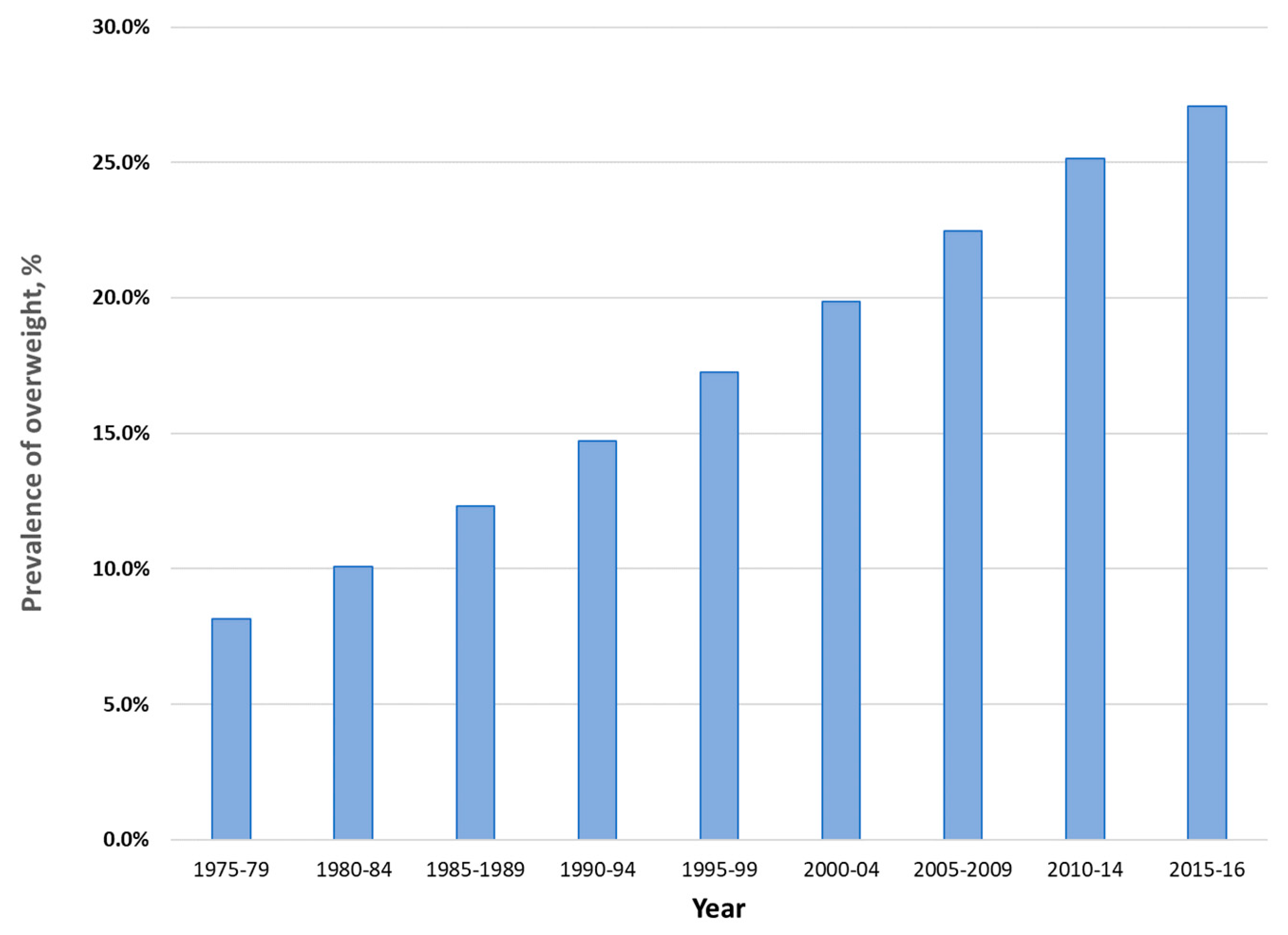
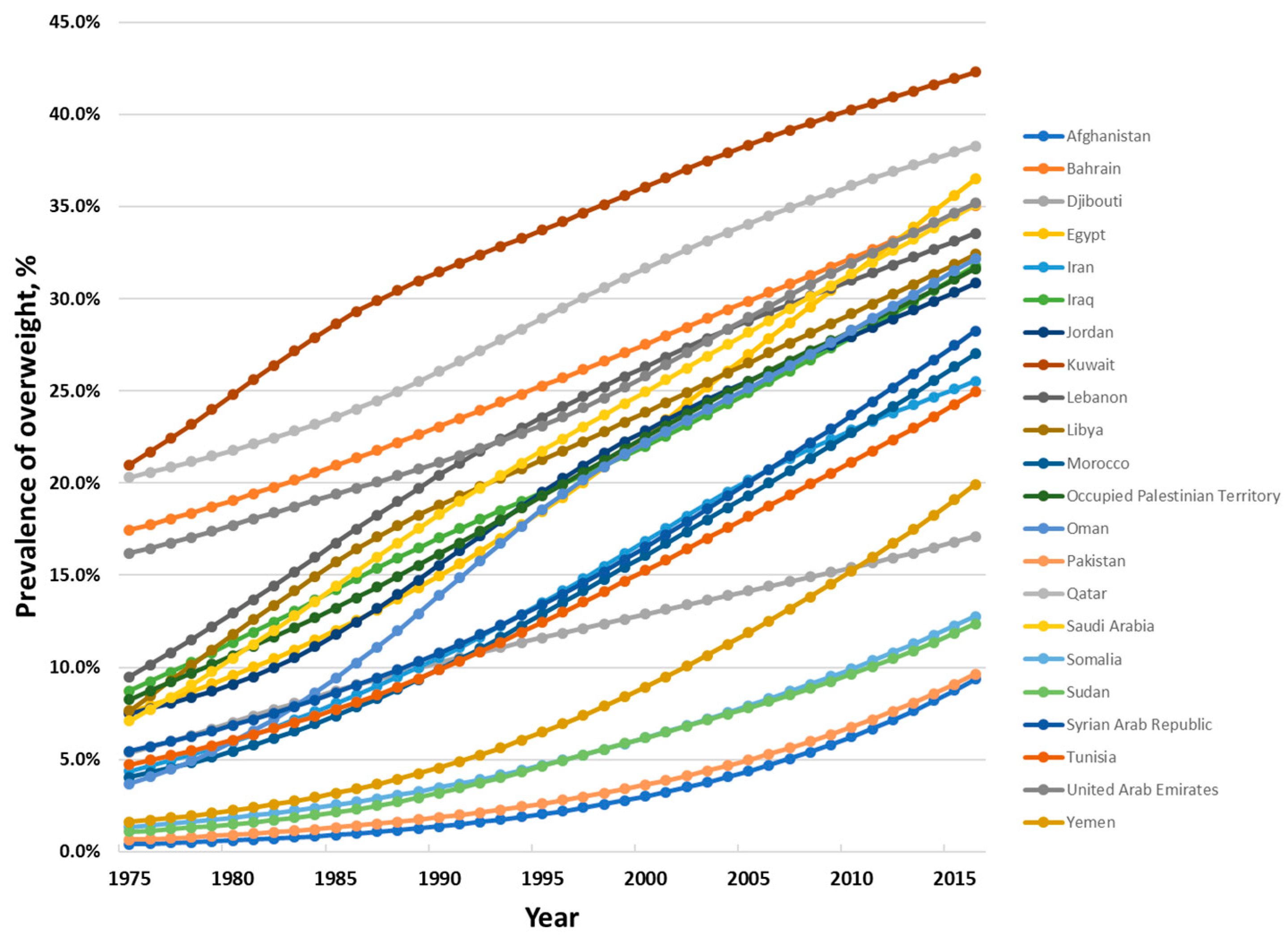
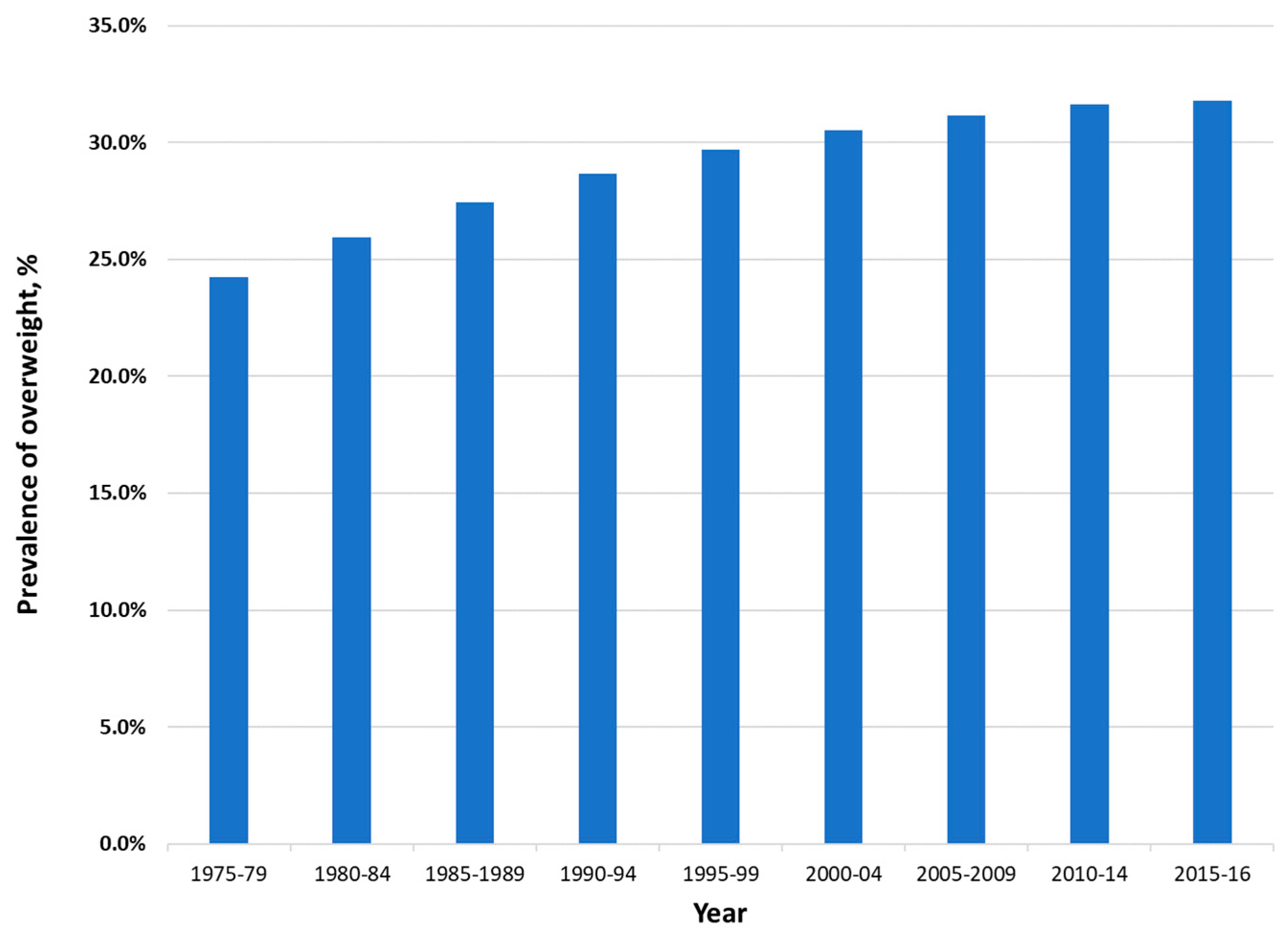
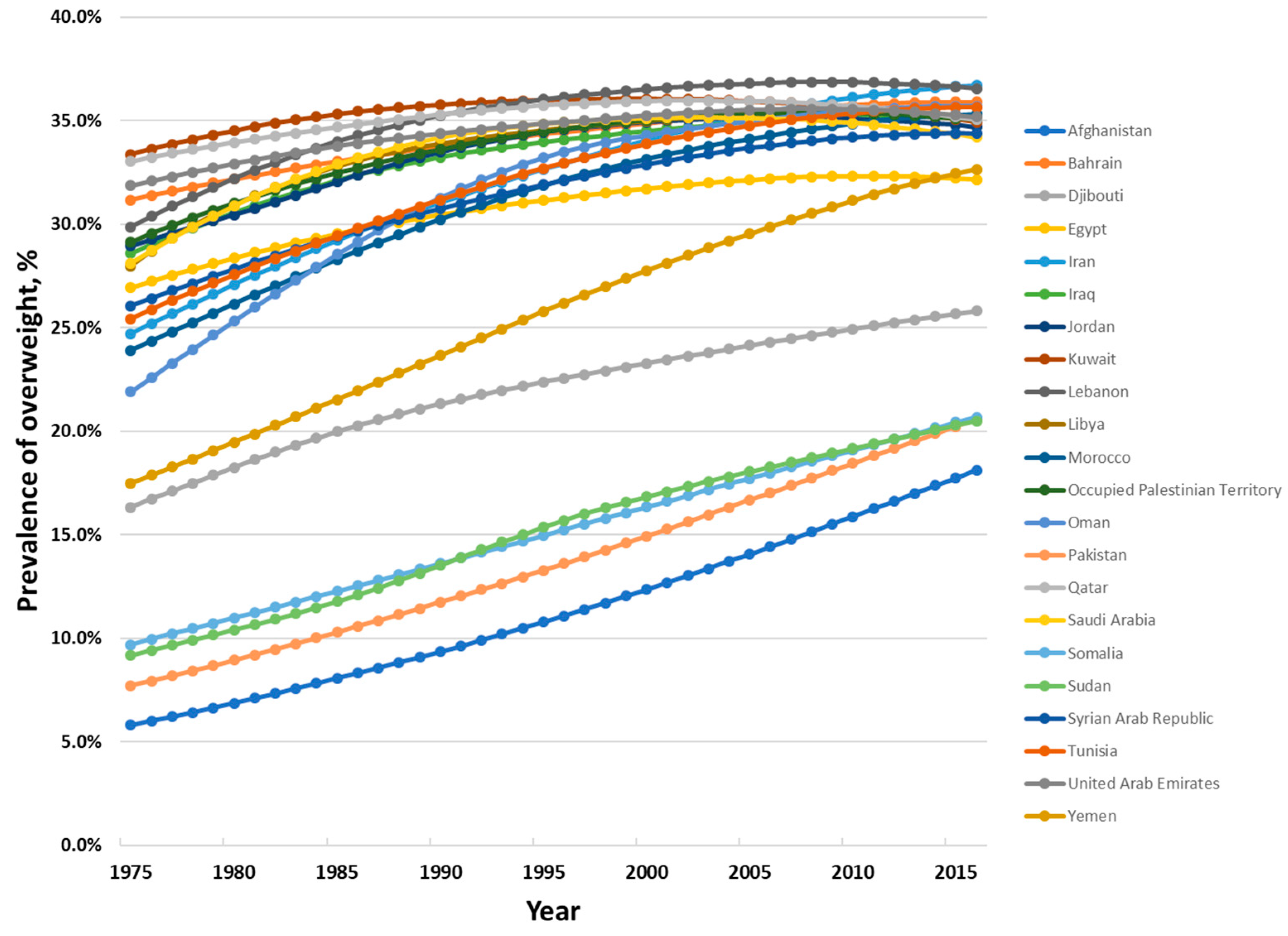
3.1. Overweight and Obesity in the Eastern Mediterranean Region
3.2. Implementation of Policies to Tackle Unhealthy Diet
3.2.1. Nutrition Governance, Multisectoral Coordination and Capacity
3.2.2. Inclusion of Healthy Diet Promotion and Policy for Prevention of Obesity and Diet-Related NCDs
3.2.3. School Nutrition and Health
3.2.4. Education and Information
3.2.5. Nutrition Labelling
3.2.6. Elimination of Industrially-Produced Trans-Fatty Acids from the Food Supply
3.2.7. Reducing Levels of Salt, Sugars and Saturated Fats in the Food Supply
3.2.8. Marketing Restrictions
3.2.9. Fiscal Measures—Taxes and Subsidies
3.2.10. Food and Nutrition Surveillance and Food Composition Data
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Disclaimer
References
- World Health Organization Regional Office for the Mediterranean. Strategy on Nutrition for the Eastern Mediterranean Region 2020–2030; WHO: Cairo, Egypt, 2019. [Google Scholar]
- Al-Jawaldeh, A.; Taktouk, M.; Nasreddine, L. Food consumption patterns and nutrient intakes of children and adolescents in the Eastern Mediterranean Region: A call for policy action. Nutrients 2020, 12, 3345. [Google Scholar] [CrossRef]
- Nasreddine, L.; Ayoub, J.L.; Al-Jawaldeh, A. Review of the nutrition situation in the Eastern Mediterranean Region. East. Mediterr. Health J. 2018, 24, 77–91. [Google Scholar] [CrossRef]
- World Health Organization. Healthy Diet. 2020. Available online: https://www.who.int/news-room/fact-sheets/detail/healthy-diet (accessed on 2 October 2020).
- World Health Organization Regional Office for the Eastern Mediterranean. Nutrition Advice for Adults during the COVID-19 Outbreak. Available online: http://www.emro.who.int/nutrition/nutrition-infocus/nutrition-advice-for-adults-during-the-covid-19-outbreak.html (accessed on 2 October 2020).
- World Health Organization Regional Office for the Eastern Mediterranean Region. Regional Strategy on Nutrition 2010–2019 and Plan of Action; WHO: Cairo, Egypt, 2011. [Google Scholar]
- World Health Organization Regional Office for the Eastern Mediterranean. Framework for Action to Implement the United Nations Political Declaration on Noncommunicable Diseases (NCDs), Including Indicators to Assess Country Progress by 2030; Updated October 2019; WHO: Cairo, Egypt, 2019. [Google Scholar]
- World Health Organization Regional Office for the Eastern Mediterranean. Regional Framework for Action on Obesity Prevention 2019–2023; WHO: Cairo, Egypt, 2018. [Google Scholar]
- World Health Organization Regional Office for the Eastern Mediterranean. Proposed Policy Priorities for Preventing Obesity and Diabetes in the Eastern Mediterranean Region; WHO: Cairo, Egypt, 2017. [Google Scholar]
- World Health Organization. Comprehensive Implementation Plan for Maternal, Infant and Young Child Nutrition; WHO: Geneva, Switzerland, 2012. [Google Scholar]
- World Health Organization. Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013–2020; WHO: Geneva, Switzerland, 2013. [Google Scholar]
- Fouad, H.; Latif, N.; Ingram, R.; Hammerich, A. Scaling up prevention and control of noncommunicable diseases in the WHO Eastern Mediterranean Region. East. Mediterr. Health J. 2018, 24, 52–62. [Google Scholar] [CrossRef]
- United Nation’s Children’s Fund; World Health Organization; The World Bank. Joint Malnutrition Estimates Regional and Global Estimates. March 2020 Edition; WHO: Geneva, Switzerland, 2020. [Google Scholar]
- World Health Organization Multicentre Growith Reference Study Group. WHO Child Growth Standards: Length/Height-For-Age, Weight-For-Age, Weight-For-Length, Weight-For-Height and Body Mass Index-For Age: Methods and Development; WHO: Geneva, Switzerland, 2006. [Google Scholar]
- United Nation’s Children’s Fund; World Health Organization; The World Bank. UNICEF-WHO-World Bank Joint Child Malnutrition Estimates; UNICEF: New York, NY, USA; WHO: Geneva, Switzerland; World Bank: Washington, DC, USA, 2012. [Google Scholar]
- United Nations Children’s Fund; World Health Organization. Global Nutrition Monitoring Framework: Operational Guidance for Tracking Progress in Meeting Targets for 2025; WHO: Geneva, Switzerland, 2017. [Google Scholar]
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef]
- World Health Organization. Growth Reference 5–19 Years. Available online: https://www.who.int/growthref/who2007_bmi_for_age/en/ (accessed on 26 August 2020).
- De Onis, M.; Onyango, A.; Borghi, E.; Siyam, A.; Nishida, C.; Siekmann, J. Development of a WHO growth reference for school-aged children and adolescents. Bull. World Health Organ. 2007, 85, 660–667. [Google Scholar] [CrossRef]
- World Health Organization. Global Health Observatory. Available online: https://www.who.int/data/gho (accessed on 19 August 2020).
- World Health Organization Regional Office for the Eastern Mediterranean. Regional Health Observatory. Available online: http://www.emro.who.int/entity/statistics/regional-health-observatory.html (accessed on 19 August 2020).
- World Health Organization. Global Nutrition Policy Review 2016–2017; WHO: Geneva, Switzerland, 2018. [Google Scholar]
- World Health Organization; UNICEF; IBFAN. Marketing of Breast-Milk Substitutes: National Implementation of the International Code Status Report 2020; World Health Organization: Geneva, Switzerland; UNICEF: Geneva, Switzerland; IBFAN: Geneva, Switzerland, 2020. [Google Scholar]
- World Health Organization. National Implementation of the Baby-Friendly Hospital Initiativei; WHO: Geneva, Switzerland, 2017. [Google Scholar]
- Global Database on the Implementation of Nutrition Action (GINA). Available online: https://www.who.int/nutrition/gina/en/ (accessed on 29 November 2020).
- Al-Jawaldeh, A.; Rayner, M.; Julia, C.; Elmadfa, I.; Hammerich, A.; McColl, K. Improving nutrition information in the Eastern Mediterranean Region: Implementation of Front-of-Pack Nutrition Labelling. Nutrients 2020, 12, 330. [Google Scholar] [CrossRef]
- Al Jawaldeh, A.; Al-Khamaiseh, M. Assessment of salt concentration in bread commonly consumed in the Eastern Mediterranean Region. East. Mediterr. Health J. 2018, 24, 18–22. [Google Scholar] [CrossRef] [PubMed]
- Al-Jawaldeh, A. The role of WHO Regional Office in the Eastern Mediterranean Region for translating the WHO policies to actions using the technical package for healthy diet tools (powerpoint). In Proceedings of the WHO Global Meeting to Accelerate Progress on SDG Target 3.4 on NCDs and Mental Health, Muscat, Oman, 9–12 December 2019. [Google Scholar]
- Alfawaz, R. Policies to promote healthy diets in Saudi Arabia. In Proceedings of the WHO Second Global Meeting on National NCD and Mental Health Directors and Focal Points, Muscat, Oman, 9–12 December 2019. [Google Scholar]
- Alhamad, N.; Elmat, E.; Alamir, N.; Subhakaran, M. An overview of salt intake reduction efforts in the Gulf Cooperation Council countries. Cardiovasc. Diagn. Ther. 2015, 5, 172–177. [Google Scholar] [PubMed]
- Aluskait, R.; Wilde, P.; Bleich, S.; Singh, G.; Folta, S. Impact of Saudi Arabia’s sugary drink tax on purchases. Curr. Dev. Nutr. 2019, 3 (Suppl. 1), P10-066-19. [Google Scholar]
- Finglas, P.; Warthon-Medina, M.; Plumb, J. Capacity Building in Dietary Monitoring and Public Health Nutrition in the Eastern Mediterranean Region; Quadram Institute; WHO Regional Office for the Eastern Mediterranean; EURO FIR: Norwich, UK, 2019. [Google Scholar]
- Jafri, A.; Elkardi, Y.; Derouiche, A. Sodium chloride composition of commercial white bread in Morocco. East. Mediterr. Health J. 2017, 23, 10. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Planning, Development and Reform and World Food Programme. Pakistan Multi-Sectoral Nutrition Strategy (PMNS 2018–25); Government of Pakistan: Islamabad, Pakistan, 2018. [Google Scholar]
- Ministry of Health and Prevention. National Action Plan in Nutrition (2017–2021); United Arab Emirates Government: Abu Dhabi, UAE, 2017. [Google Scholar]
- Montagnese, C.; Santarpia, L.; Ivavarone, F.; Strangio, F.; Sangiovanni, B.; Buonifacio, M.; Caldara, A.; Silvestri, E.; Contaldo, F.; Pasanisi, F. Food-based dietary guidelines around the world: Eastern Mediterranean and Middle-Eastern Countries. Nutrients 2019, 11, 1325. [Google Scholar] [CrossRef] [PubMed]
- Moslemi, M.; Kheirandish, M.; Mazaheri, N.; Hosseini, H.; Jannat, B.; Mofid, V.; Fooladi, M.; Karimian, N. National food policies in the Islamic Republic of Iran aimed at control and prevention of noncommunicable disease. East. Mediterr. Health J. 2020, in press. [Google Scholar] [CrossRef]
- Saghafi, Z.; Zargaraan, A.; Tabibiazar, M.; Hosseini, H. Is Trans fatty acid still an issue for policy makers in Iran? A technical report. Nutr. Food Sci. Res. 2018, 5, 47–51. [Google Scholar] [CrossRef][Green Version]
- Saudi Food and Drug Authority. Saudi Technical Regulation No. SFDA 2483/2018 Trans Fatty Acids (Trans Fats); Saudi Food and Drug Authority: Riyadh, Saudi Arabia, 2018.
- Saudi Food and Drug Authority. SFDA Prevents “Partially Hydrogenated Oils” (PHOs) in the Food Industry and Gives a Period to the Manufactuers to Comply with the Saudi Technical Regulations. 2018. Available online: https://www.sfda.gov.sa/en/food/news/Pages/f6-12-2018a2.aspx (accessed on 11 May 2020).
- Saudi Food and Drug Authority. Strategy of Regulating Healthy Food; Saudi Food and Drug Authority: Riyadh, Saudi Arabia, 2018. [Google Scholar]
- State of Qatar Supreme Council of Health. Qatar National Nutrition and Physical Activity Action Plan 2017–2022; Ministry of Public Health: Doha, Qatar, 2017.
- World Health Organization Regional Office for the Eastern Mediterranean. The Work of WHO in the Eastern Mediterranean Region: Annual Report of the Regional Director 2017; WHO: Cairo, Egypt, 2018. [Google Scholar]
- World Health Organization Regional Office for the Eastern Mediterranean. Food and Nutrition Surveillance Systems: Technical Guide for the Development of a Food and Nutrition Surveillance System; WHO: Cairo, Egypt, 2013. [Google Scholar]
- World Health Organization Regional Office for the Eastern Mediterranean. Implementing the WHO Recommendations on the Marketing of Food and Non-Alcoholic Beverages to Children in the Eastern Mediterranean Region; WHO: Cairo, Egypt, 2018. [Google Scholar]
- World Health Organization Regional Office for the Eastern Mediterranean. Progress in Implementing Nutrition Policy in the Eastern Mediterranean Region; WHO: Cairo, Egypt, 2020; Forthcoming. [Google Scholar]
- World Health Organization Regional Office for the Eastern Mediterranean Region. Cutting into Trans Fat Consumption in Iran. 2018. Available online: https://www.who.int/news-room/feature-stories/detail/cutting-into-trans-fat-consumption-in-iran (accessed on 18 May 2020).
- World Health Organization Regional Office for the Eastern Mediterranean. Summary Report of the Regional Meeting to Standardize and Update Food Composition Tables, Reflecting Sugar, Trans Fat, Saturated Fat and Salt Contents, Rabat, Morocco 20–22 September 2016; WHO: Cairo, Egypt, 2018. [Google Scholar]
- World Bank. World Bank Country and Lending Groups. Available online: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups (accessed on 4 August 2020).
- FAO; WHO. Framework for Action: Outcome Document of the Second International Conference on Nutrition; FAO: Rome, Italy, 2014. [Google Scholar]
- World Health Organization. Tackling NCDS: ‘Best Buys’ and Other Recommended Interventions for the Prevention and Control of Noncommunicable Diseases; WHO: Geneva, Switzerlands, 2017. [Google Scholar]
- Government of Egypt. Egypt National Multisectoral Action Plan for Prevention and Control on Noncommunicable Diseases 2017–2021; Government of Egypt: Cairo, Egypt, 2017. [Google Scholar]
- General Directorate Nutrition. National Nutrition Policy, Strategies and Action Plan 2017–2022; Palestinian Ministry of Public Health: Ramallah, West Bank, 2016.
- Ministere de la Santé. Stratégie Nationale de prévention des différentes formes de la malnutrition à Djibouti, 2018–2022; UNICEF: Djibouti City, Djibouti, 2018. [Google Scholar]
- Adib, S.M.; Rady, A. Non-communicable disease prevention and control plan (NCD-PCP) for Lebanon 2015–2020; WHO: Beirut, Lebanon, 2014. [Google Scholar]
- Ministry of Health, Government of Pakistan; World Health Organization Pakistan Country Office; Heartfile. National Action Plan for Prevention and Control on Non-Communicable Diseases and Health Promotion in Pakistan: A Public-Private Partnership in Health; Ministry of Health, Government of Pakistan: Islamabad, Pakistan, 2004.
- World Health Organization. Report of the Commission on Ending Childhood Obesity; WHO: Geneva, Switzerland, 2016. [Google Scholar]
- World Health Organization. Nutrition-Friendly Schools Initiative. Available online: https://www.who.int/nutrition/topics/nutrition_friendly_schools_initiative/en/ (accessed on 26 August 2020).
- Food and Agriculture Organization of the United Nations. Food-Based Dietary Guidelines—United Arab Emirates. Available online: http://www.fao.org/nutrition/education/food-dietary-guidelines/regions/countries/united-arab-emirates/en/ (accessed on 21 September 2020).
- World Cancer Research Fund International. Building Momentum: Lessons on Implementing a Robust Front-Of-Pack Food Label; WCRF: London, UK, 2019. [Google Scholar]
- Tehran Times. ‘Traffic light’ labels to guide Iranians towards healthier food. Tehran Times 2017, 9, 6.
- World Health Organization. Countdown to 2023: WHO Report on Global Trans Fat Elimination 2020; WHO: Geneva, Switzerland, 2020. [Google Scholar]
- World Cancer Research Fund. 2020. Available online: https://www.wcrf.org/int/policy/nourishing-database (accessed on 31 October 2020).
- World Health Organization Regional Office for the Eastern Mediterranean. Summary Report of the Virtual Meeting on Implementation of Trans Fatty Acid Elimination in the Eastern Mediterranean Report 10–11 August 2020; WHO: Cairo, Egypt, Forthcoming.
- GCC Standardization Organization. Trans Fatty Acids GSO 2483/2015 (E); GSO: Riyadh, Saudi Arabia, 2015. [Google Scholar]
- World Health Organization. Global Database on the Implementation of Nutrition Action: Kuwaiti Technical Regulation of Trans Fatty Acids (KWS GSO 2483/2017). 2017. Available online: https://extranet.who.int/nutrition/gina/en/node/38174 (accessed on 14 September 2020).
- Sadeghirad, B.; Dunahey, T. Influence of unhealthy food and beverage marketing on children’s dietary intake and preferences: A systematic review and meta-analysis of randomized trials. Obes. Rev. 2016, 17, 945–959. [Google Scholar] [CrossRef]
- World Health Organization. Set of Recommendations on the Marketing of Foods and Non-Alcoholic Beverages to Children; WHO: Geneva, Switzerland, 2010. [Google Scholar]
- WHO Regional Office for the Eastern Mediterranean. Nutrient Profile Model for the Marketing of Food and Non-Alcoholic Beverages to Children in the WHO Eastern Mediterranean Region; WHO: Cairo, Egypt, 2017. [Google Scholar]
- World Health Assembly. Resolution WHA 66.10. Follow-Up to the Political Declaration of the High-Level Meeting of the General Assembly on the Prevention and Control of Non-Communicable Diseases; WHO: Geneva, Switzerland, 2014. [Google Scholar]
- World Health Organization. Thirteenth General Programme of Work 2019–2023; WHO: Geneva, Switzerland, 2019. [Google Scholar]
- Stuckler, D.; Nestle, M. Big food, food systems and global health. PLoS Med. 2012, 9, e1001242. [Google Scholar] [CrossRef]
- UNICEF; FAO; WFP; WHO. Statement on Nutrition during the COVID-19 Pandemic in the Middle East and North Africa, Eastern Mediterranean and Arab Regions; WHO: Cairo, Egypt; FAO: Cairo, Egypt; UNICEF: Cairo, Egypt; WFP: Cairo, Egypt, 2020. [Google Scholar]
- Kass, D.; Duggal, P.; Cingolani, O. Obesity could shift severe COVID-19 disease to younger ages. Lancet 2020, 395, 1544–1545. [Google Scholar] [CrossRef]
- Zadori, N.; Vancsa, S.; Farkas, N.; Hegyi, P.; Eross, B. The negative impact of comorbidities on the disease course of COVID-19. Intensive Care Med. 2020, 46, 1784–1786. [Google Scholar] [CrossRef]
- Kluge, H.; Wickramasinghe, K.; Rippin, H.; Mendes, R.; Peters, D.; Kontsevaya, A.; Breda, J. Prevention and control of non-communicable diseases in the COVID-19 response. Lancet 2020, 835, 1678–1680. [Google Scholar] [CrossRef]
- Wang, B.L.R.; Lu, Z.; Huang, Y. Does comorbidity increase the risk of patients with COVID-19: Evidence from meta-analysis. Aging 2020, 12, 6049–6057. [Google Scholar] [CrossRef] [PubMed]
- UN Secretary General. The Impact of COVID-19 on Food Security and Nutrition. Policy Brief; United Nations: New York, NY, USA, 2020. [Google Scholar]
- FAO; IFAD; UNICEF; WFP; WHO. The State of Food Security and Nutrition in the World 2020: Transforming Food Systems for Affordable Healthy Diets; FAO: Rome, Italy, 2020. [Google Scholar]
- World Health Organization Regional Office for the Eastern Mediterranean. Promoting a Healthy Diet for the WHO Eastern Mediterranean Region: User-Friendly Guide; WHO: Cairo, Egypt, 2012. [Google Scholar]
- Horta, B.; de Mola, C.L.; Victora, C. Long-term consequences of breastfeeding on cholesterol, obesity, systolic blood pressure and type 2 diabetes: A systematic review and meta-analysis. Acta Paediatr. 2015, 104, 30–37. [Google Scholar] [CrossRef] [PubMed]
- Chowdhury, R.; Sinha, B.; Sankar, M.J.; Taneja, S.; Bhandari, N.; Rollins, N.; Bahl, R.; Martines, J. Breastfeeding and maternal health outcomes: A systematic review and meta-analysis. Acta Paediatr. 2015, 104, 96–113. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization Regional Office for the Eastern Mediterranean. Breastfeeding Advice during the COVID-19 Outbreak. 2020. Available online: http://www.emro.who.int/nutrition/nutrition-infocus/breastfeeding-advice-during-covid-19-outbreak.html (accessed on 2 October 2020).
| Country | Trained Nutritionists or Dieticians per 100,000 Population |
|---|---|
| Low-income countries | |
| Afghanistan | 0.1 |
| Somalia | n.d. |
| Sudan | 2 |
| Syria | 10.7 |
| Yemen | 0.4 |
| Lower-middle income countries | |
| Djibouti | 0.8 |
| Egypt | n.d. |
| Morocco | 1.1 |
| Pakistan | n.d. |
| occupied Palestinian Territory | n.d. |
| Tunisia | 8 |
| Upper-middle income countries | |
| Iran | 20.2 |
| Iraq | 0 |
| Jordan | 19.9 |
| Lebanon | n.d. |
| Libya | 3.5 |
| High-income countries | |
| Bahrain | 1 |
| Kuwait | 5.8 |
| Oman | 5 |
| Qatar | 6 |
| Saudi Arabia | 6.6 |
| United Arab Emirates | 7.6 |
| Countries | Any Policies on Marketing of Food to Children 1 | Any Policies to Reduce Salt Consumption 1 | National Policies on Saturated Fatty Acids/Trans-Fatty Acids 1 | National Policies on Saturated Fats 1 | National Policies on Trans-Fatty Acid Elimina-tion 1 | Specific Measure to Ban or Virtually Eliminate Industrial Trans-Fatty Acids 2 | Tax on Sugar-Sweetened Beverages (Level of Tax Levied) 3 |
|---|---|---|---|---|---|---|---|
| Low-income countries | |||||||
| Afghanistan | x | x | ✔ | x | x | x | x |
| Somalia | n.d. | n.d. | x | n.d. | x | x | x |
| Sudan | x | x | x | x | x | x 5 | x |
| Syria | x | x | x | x | x | x | n.d. |
| Yemen | x | x | x | x | x | x | n.d. |
| Lower-middle income countries | |||||||
| Djibouti | n.d. | x | x | x | x | x | x |
| Egypt | x | ✔ | x | x | x | x 4,5 | n.d. |
| Morocco | ✔ | ✔ | ✔ | ✔ | ✔ | x 4 | ✔ (50%) |
| Pakistan | x | x | x | x | x | x 8 | x |
| Occupied Palestinian Territory 6 | x | ✔ | ✔ | n.d. | x | x 4,5 | x |
| Tunisia | x | ✔ | ✔ | ✔ | ✔ | x 4,8 | ✔ |
| Upper-middle income countries | |||||||
| Iran | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ (20%) |
| Iraq | x | ✔ | ✔ | ✔ | n.d. | x | x |
| Jordan | x | ✔ | ✔ | x | ✔ | x 8 | x |
| Lebanon | x | x | x | x | x | x | x |
| Libya | x | x | x | x | x | x | x |
| High-income countries | |||||||
| Bahrain | ✔ | ✔ | ✔ | ✔ | ✔ | ✔7 | ✔ (50%) |
| Kuwait | x | ✔ | ✔ | ✔ | ✔ | ✔7 | x |
| Oman | ✔ | ✔ | ✔ | ✔ | ✔ | x 5,7,8 | ✔ (50%) |
| Qatar | x | ✔ | ✔ | ✔ | ✔ | x 5,7 | ✔ (50%) |
| Saudi Arabia | x | ✔ | ✔ | ✔ | ✔ | ✔ 7 | ✔ (50%) |
| UAE | x | ✔ | ✔ | ✔ | ✔ | x 5,7 | ✔ (50%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Jawaldeh, A.; Hammerich, A.; Doggui, R.; Engesveen, K.; Lang, K.; McColl, K. Implementation of WHO Recommended Policies and Interventions on Healthy Diet in the Countries of the Eastern Mediterranean Region: From Policy to Action. Nutrients 2020, 12, 3700. https://doi.org/10.3390/nu12123700
Al-Jawaldeh A, Hammerich A, Doggui R, Engesveen K, Lang K, McColl K. Implementation of WHO Recommended Policies and Interventions on Healthy Diet in the Countries of the Eastern Mediterranean Region: From Policy to Action. Nutrients. 2020; 12(12):3700. https://doi.org/10.3390/nu12123700
Chicago/Turabian StyleAl-Jawaldeh, Ayoub, Asmus Hammerich, Radhouene Doggui, Kaia Engesveen, Krista Lang, and Karen McColl. 2020. "Implementation of WHO Recommended Policies and Interventions on Healthy Diet in the Countries of the Eastern Mediterranean Region: From Policy to Action" Nutrients 12, no. 12: 3700. https://doi.org/10.3390/nu12123700
APA StyleAl-Jawaldeh, A., Hammerich, A., Doggui, R., Engesveen, K., Lang, K., & McColl, K. (2020). Implementation of WHO Recommended Policies and Interventions on Healthy Diet in the Countries of the Eastern Mediterranean Region: From Policy to Action. Nutrients, 12(12), 3700. https://doi.org/10.3390/nu12123700






