5-Year Follow-Up of a Telephone Intervention to Increase Fruit and Vegetable Consumption in Preschoolers: The ‘Healthy Habits’ Cluster Randomised Trial
Abstract
1. Introduction
2. Materials and Methods
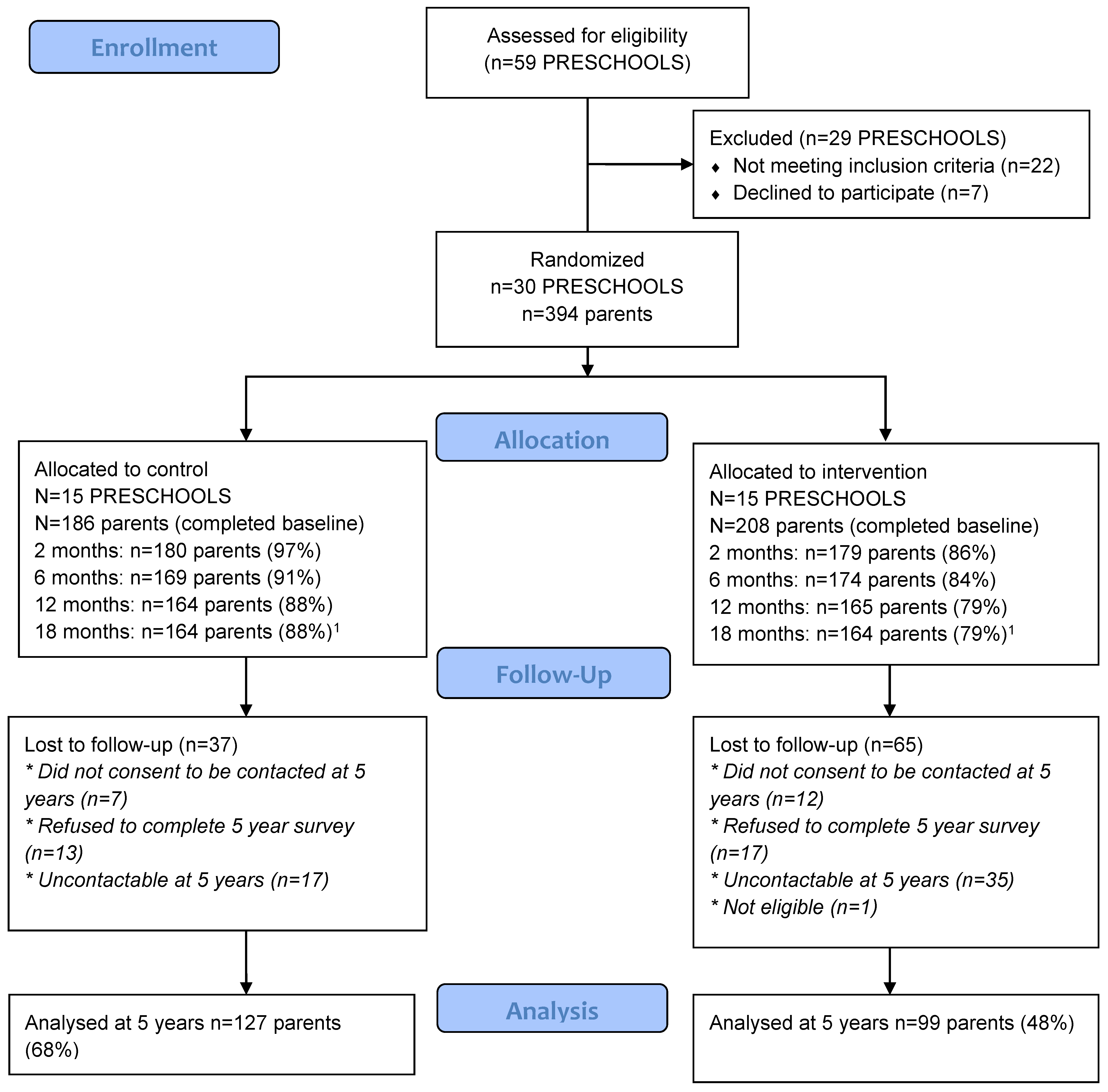
2.1. Design
2.2. Sample
2.3. Randomisation and Masking
2.4. Procedures
2.5. Data Collection
2.6. Outcomes
2.7. Sample Size Calculation
2.8. Statistical Analysis
3. Results
3.1. Primary Outcome: F&V-CDQ Score
3.2. Other Outcomes
3.3. Subgroup
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Availability of Data and Materials
References
- Afshin, A.; Sur, P.J.; Fay, K.A.; Cornaby, L.; Ferrara, G.; Salama, J.S.; Mullany, E.C.; Abate, K.H.; Abbafati, C.; Abebe, Z.; et al. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 393, 1958–1972. [Google Scholar] [CrossRef]
- World Health Organization. Increasing Fruit and Vegetable Consumption to Reduce the Risk of Noncommunicable Diseases. Available online: https://www.who.int/elena/titles/fruit_vegetables_ncds/en/ (accessed on 26 March 2020).
- Yngve, A.; Wolf, A.; Poortvliet, E.; Elmadfa, I.; Brug, J.; Ehrenblad, B.; Franchini, B.; Haraldsdóttir, J.; Krølner, R.; Maes, L.; et al. Fruit and Vegetable Intake in a Sample of 11-Year-Old Children in 9 European Countries: The Pro Children Cross-Sectional Survey. Ann. Nutr. Metab. 2005, 49, 236–245. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. CDC Healthy Schools: Obesity. Available online: https://www.cdc.gov/healthyschools/obesity/facts.htm (accessed on 1 May 2018).
- The Australian Bureau of Statistics. Australian Health Survey: Consumption of Food Groups from the Australian Dietary Guidelines, 2011–2012. Available online: https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/4364.0.55.012main+features12011-12 (accessed on 1 May 2018).
- Public Health England. NDNS Results from Years 5 and 6 Combined of the Rolling Programme for 2012 and 2013 to 2013 and 2014. Available online: https://assets.publishing.service.gov.auk/government/uploads/system/uploads/attachment_data/file/551352/NDNS_Y5_6_UK_Main_Text.pdf (accessed on 9 April 2020).
- Maynard, M. Fruit, vegetables, and antioxidants in childhood and risk of adult cancer: The Boyd Orr cohort. J. Epidemiol. Commun. Health 2003, 57, 218–225. [Google Scholar] [CrossRef]
- Ness, A.; Maynard, M.; Frankel, S.; Smith, G.D.; Frobisher, C.; Leary, S.D.; Emmett, P.M.; Gunnell, D. Diet in childhood and adult cardiovascular and all cause mortality: The Boyd Orr cohort. Heart 2005, 91, 894–898. [Google Scholar] [CrossRef]
- Australian Institute of Health and Welfare. Childhood Overweight and Obesity; Australia’s Health Series; Australian Institute of Health and Welfare: Canberra, Australia, 2014.
- World Health Organisation. Consideration of The Evidence on Childhood Obesity for the Commission on Ending Childhood Obesity: Report of the Ad Hoc Working Group on Science and Evidence for Ending Childhood Obesity; World Health Organisation: Geneva, Switzerland, 2016. [Google Scholar]
- Charles Perkins Centre. The University of Sydney Inquiry into Childhood Overweight and Obesity; Charles Perkins Centre: Camperdown, NSW, Australia, 2016. [Google Scholar]
- Donnelly, J.E.; Goetz, J.; Gibson, C.; Sullivan, D.K.; Lee, R.; Smith, B.K.; Lambourne, K.; Mayo, M.S.; Hunt, S.; Lee, J.H.; et al. Equivalent weight loss for weight management programs delivered by phone and clinic. Obesity 2013, 21, 1951–1959. [Google Scholar] [CrossRef]
- Havas, S.; Anliker, J.; Damron, D.; Langenberg, P.; Ballesteros, M.; Feldman, R. Final results of the Maryland WIC 5-A-Day Promotion Program. Am. J. Public Health 1998, 88, 1161–1167. [Google Scholar] [CrossRef] [PubMed]
- Australian Communications and Media Authority. Communications Report, 2018–2019; Australian Communications and Media Authority: Pyrmont, NSW, Australia, 2020.
- Silver, L. Smartphone Ownership is Growing Rapidly around the World, But Not Always Equally. Available online: https://www.pewresearch.org/global/2019/02/05/smartphone-ownership-is-growing-rapidly-around-the-world-but-not-always-equally/ (accessed on 26 March 2020).
- Graves, N.; Barnett, A.; Halton, K.; Veerman, J.L.; Winkler, E.; Owen, N.; Reeves, M.M.; Marshall, A.L.; Eakin, E.G. Cost-Effectiveness of a Telephone-Delivered Intervention for Physical Activity and Diet. PLoS ONE 2009, 4, e7135. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Eakin, E.G.; Lawler, S.P.; Vandelanotte, C.; Owen, N. Telephone Interventions for Physical Activity and Dietary Behavior Change. Am. J. Prev. Med. 2007, 32, 419–434. [Google Scholar] [CrossRef] [PubMed]
- O’Hara, B.J.; Phongsavan, P.; Venugopal, K.; Bauman, A.E. Characteristics of participants in Australia’s Get Healthy telephone-based lifestyle information and coaching service: Reaching disadvantaged communities and those most at need. Health Educ. Res. 2011, 26, 1097–1106. [Google Scholar] [CrossRef]
- Misericordia Health Centre. Dial-a-Dietitian. Available online: https://misericordia.mb.ca/programs/phcc/dial-a-dietitian/ (accessed on 12 May 2020).
- HealthLink BC. About 8-1-1. Available online: https://www.healthlinkbc.ca/about-8-1-1 (accessed on 12 May 2020).
- Llewellyn-Bennett, R.; Bowman, L.; Bulbulia, R. Post-trial follow-up methodology in large randomized controlled trials: A systematic review protocol. Syst. Rev. 2016, 5, 214. [Google Scholar] [CrossRef]
- Goode, A.D.; Reeves, M.M.; Eakin, E.G. Telephone-Delivered Interventions for Physical Activity and Dietary Behavior Change. Am. J. Prev. Med. 2012, 42, 81–88. [Google Scholar] [CrossRef] [PubMed]
- Hodder, R.; O’Brien, K.; Tzelepis, F.; Wyse, R.; Wolfenden, L. Interventions for increasing fruit and vegetable consumption in children aged five years and under. Cochrane Database Syst. Rev. 2020, 5, CD008552. [Google Scholar] [PubMed]
- Wolfenden, L.; Wyse, R.; Campbell, E.; Brennan, L.; Campbell, K.J.; Fletcher, A.; Wiggers, J.; Bowman, J.; Heard, T.R. Randomized controlled trial of a telephone-based intervention for child fruit and vegetable intake: Long-term follow-up. Am. J. Clin. Nutr. 2014, 99, 543–550. [Google Scholar] [CrossRef] [PubMed]
- Dave, J.M. Assessing long-term impact of dietary interventions: Important but challenging. Am. J. Clin. Nutr. 2019, 109, 5–6. [Google Scholar] [CrossRef]
- Yavuz-Muren, H.M.; Van Ijzendoorn, M.H.; Mesman, J.; Van Der Veek, S. Interventions aimed at reducing obesity in early childhood: A meta-analysis of programs that involve parents. J. Child Psychol. Psychiatry 2014, 56, 677–692. [Google Scholar] [CrossRef]
- Albani, V.; Butler, L.T.; Traill, W.B.; Kennedy, O.B. Fruit and vegetable intake: Change with age across childhood and adolescence. Br. J. Nutr. 2017, 117, 759–765. [Google Scholar] [CrossRef]
- Wyse, R.; Wolfenden, L.; Campbell, E.; Brennan, L.; Campbell, K.J.; Fletcher, A.; Bowman, J.; Heard, T.; Wiggers, J. A cluster randomised trial of a telephone-based intervention for parents to increase fruit and vegetable consumption in their 3- to 5-year-old children: Study protocol. BMC Public Health 2010, 10, 216. [Google Scholar] [CrossRef]
- Wyse, R.; Wolfenden, L.; Campbell, E.; Campbell, K.J.; Wiggers, J.; Brennan, L.; Fletcher, A.; Bowman, J.; Heard, T.R. A cluster randomized controlled trial of a telephone-based parent intervention to increase preschoolers’ fruit and vegetable consumption123. Am. J. Clin. Nutr. 2012, 96, 102–110. [Google Scholar] [CrossRef]
- Campbell, K.J.; Crawford, D.; Jackson, M.; Cashel, K.; Worsley, A.; Gibbons, K.; Birch, L.L. Family food environments of 5−6-year-old-children: Does socioeconomic status make a difference? Asia Pac. J. Clin. Nutr. 2002, 11, S553–S561. [Google Scholar] [CrossRef]
- Golan, M.; Weizman, A. Familial Approach to The Treatment of Childhood Obesity: Conceptual Model. J. Nutr. Educ. 2001, 33, 102–107. [Google Scholar] [CrossRef]
- Pearson, N.; Biddle, S.J.H.; Gorely, T. Family correlates of fruit and vegetable consumption in children and adolescents: A systematic review. Public Health Nutr. 2009, 12, 267–283. [Google Scholar] [CrossRef] [PubMed]
- Abraham, C.; Michie, S. A taxonomy of behavior change techniques used in interventions. Health Psychol. 2008, 27, 379–387. [Google Scholar] [CrossRef] [PubMed]
- Magarey, A.; Golley, R.K.; Spurrier, N.J.; Goodwin, E.J.; Ong, F. Reliability and validity of the Children’s Dietary Questionnaire; A new tool to measure children’s dietary patterns. Pediatr. Obes. 2009, 4, 257–265. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Statistics. National Nutrition Survey Users’ Guide 1995; Australian Bureau of Statistics: Canberra, Australia, 1998.
- White, I.R.; Horton, N.J.; Carpenter, J.; Pocock, S.J. Strategy for intention to treat analysis in randomised trials with missing outcome data. BMJ 2011, 342, d40. [Google Scholar] [CrossRef] [PubMed]
- Fjeldsoe, B.; Neuhaus, M.; Winkler, E.; Eakin, E. Systematic review of maintenance of behavior change following physical activity and dietary interventions. Health Psychol. 2011, 30, 99. [Google Scholar] [CrossRef] [PubMed]
- Magarey, A.; Mauch, C.; Mallan, K.; Perry, R.; Elovaris, R.; Meedeniya, J.; Byrne, R.; Daniels, L. Child dietary and eating behavior outcomes up to 3.5 years after an early feeding intervention: The NOURISH RCT. Obesity 2016, 24, 1537–1545. [Google Scholar] [CrossRef]
- Watt, R.G.; Tull, K.I.; Hardy, R.; Wiggins, M.; Kelly, Y.; Molloy, B.; Dowler, E.; Apps, J.; McGlone, P. Effectiveness of a social support intervention on infant feeding practices: Randomised controlled trial. J. Epidemiol. Commun. Health 2008, 63, 156–162. [Google Scholar] [CrossRef]
- Scheiwe, A.; Hardy, R.; Watt, R.G. Four-year follow-up of a randomized controlled trial of a social support intervention on infant feeding practices. Matern. Child. Nutr. 2010, 6, 328–337. [Google Scholar] [CrossRef]
- Emmett, P.M.; Jones, L.R. Diet, growth, and obesity development throughout childhood in the Avon Longitudinal Study of Parents and Children. Nutr. Rev. 2015, 73, 175–206. [Google Scholar] [CrossRef]
- Wyse, R.; Wolfenden, L.; Bisquera, A. Characteristics of the home food environment that mediate immediate and sustained increases in child fruit and vegetable consumption: Mediation analysis from the Healthy Habits cluster randomised controlled trial. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 1–9. [Google Scholar] [CrossRef]
- Poelman, A.; Delahunty, C.M.; Broch, M.; De Graaf, C. Multiple vs Single Target Vegetable Exposure to Increase Young Children’s Vegetable Intake. J. Nutr. Educ. Behav. 2019, 51, 985–992. [Google Scholar] [CrossRef] [PubMed]
- Crutzen, R.; Viechtbauer, W.; Spigt, M.; Kotz, D. Differential attrition in health behaviour change trials: A systematic review and meta-analysis. Psychol. Health 2014, 30, 122–134. [Google Scholar] [CrossRef] [PubMed]
- Bell, M.L.; Kenward, M.G.; Fairclough, D.L.; Horton, N.J. Differential dropout and bias in randomised controlled trials: When it matters and when it may not. BMJ 2013, 346, e8668. [Google Scholar] [CrossRef] [PubMed]
- Byers, T.; Trieber, F.; Gunter, E.; Coates, R.; Sowell, A.; Leonard, S.; Mokdad, A.; Jewell, S.; Miller, D.; Serdula, M. The accuracy of parental reports of their children’s intake of fruits and vegetables: Validation of a food frequency questionnaire with serum levels of carotenoids and vitamins C, A, and E. Epidemiology 1993, 4, 350–355. [Google Scholar] [CrossRef] [PubMed]
- Linneman, C.; Hessler, K.; Nanney, M.S.; Steger-May, K.; Huynh, A.; Haire-Joshu, D. Parents Are Accurate Reporters of Their Preschoolers’ Fruit and Vegetable Consumption under Limited Conditions. J. Nutr. Educ. Behav. 2004, 36, 305–308. [Google Scholar] [CrossRef]
- Hammersley, M.L.; Wyse, R.J.; Jones, R.A.; Wolfenden, L.; Yoong, S.; Stacey, F.; Eckermann, S.; Okely, A.D.; Innes-Hughes, C.; Li, V.; et al. Translation of two healthy eating and active living support programs for parents of 2-6 year old children: A parallel partially randomised preference trial protocol (the ’time for healthy habits’ trial). BMC Public Health 2020, 20, 636. [Google Scholar] [CrossRef]
| Key Theme | Content | Behaviour Change Technique | Application of Behaviour Change Technique |
|---|---|---|---|
| WEEK 1 Availability and Accessibility |
| ||
|
|
| |
| |||
|
|
| |
| WEEK 2 Availability and Accessibility, Supportive Family Eating Routines |
|
|
|
|
|
| |
|
|
| |
| |||
|
|
| |
| WEEK 3 Parental role-modelling, Supportive Family Eating Routines |
|
|
|
|
|
| |
|
| ||
|
|
| |
| WEEK 4 Availability and Accessibility, Parental role-modelling, Supportive Family Eating Routines |
|
|
|
|
|
| |
|
|
|
| Parents Characteristics Reported at Baseline [24,29] Mean, (SD) a | Baseline All Participants (n = 394) | Baseline Control (n = 186) | Baseline Intervention (n = 208) | 5-Year Follow up All Participants (n = 226) | 5-Year Follow up Control (n = 127) | 5-Year Follow up Intervention (n = 99) |
|---|---|---|---|---|---|---|
| Age in years at baseline | 35.5 (5.4) | 35.7 (5.0) | 35.2 (5.6) | 36.2 (4.6) | 36.2 (4.5) | 36.2 (4.9) |
| Gender - female, (%) | 95.9% (n = 378) | 96.8% (n = 180) | 95.2% (n = 198) | 95.6% (n = 216) | 96.1% (n = 122) | 95.0% (n = 94) |
| Household income, ≥AU$100,000, (%) | 41.4% (n = 137) | 39.6% (n = 72) | 41.0% (n = 84) | 45.7% (n = 102) | 44.4% (n = 55) | 47.5% (n = 47) |
| University education, (%) | 47.2% (n = 186) | 49.5% (n = 92) | 45.2% (n = 94) | 53.1% (n = 120) | 52.8% (n = 67) | 53.5% (n = 53) |
| Aboriginal &/or Torres Strait Islander, (%) | 2.0% (n = 8) | 3.2% (n = 6) | 1.0% (n = 2) | 1.8% (n = 4) | 2.4% (n = 3) | 1.0% (n = 1) |
| Number of children <16 years | 2.3 (0.8) | 2.3 (0.7) | 2.3 (0.8) | 2.3 (0.7) | 2.4 (0.7) | 2.3 (0.8) |
| Number of fruit servings per day | 1.8 (1.1) | 1.8 (1.0) | 1.8 (1.1) | 1.9 (1.1) | 1.8 (1.1) | 2.0 (1.2) |
| Number of vegetable servings per day | 3.2 (1.3) | 3.1 (1.3) | 3.3 (1.3) | 3.2 (1.4) | 3.1 (1.4) | 3.3 (1.2) |
| CHILD CHARACTERISTICS REPORTED AT BASELINE | ||||||
| Age in years at baseline | 4.3 (0.6) | 4.3 (0.6) | 4.3 (0.6) | 4.3 (0.6) | 4.4 (0.6) | 4.3 (0.6) |
| Gender—female, (%) | 48.5% (n = 191) | 45.7% (n = 85) | 51.0% (n = 106) | 51.3% (n = 116) | 47.2% (n = 60) | 56.6% (n = 56) |
| Aboriginal &/or Torres Strait Islander, (%) | 2.8% (n = 11) | 4.8% (n = 9) | 1.0% (n = 2) | 1.8% (n = 4) | 1.6% (n = 2) | 2.0% (n = 2) |
| Daily servings of fruit b | 2.3 (1.0) | 2.2 (1.0) | 2.3 (1.0) | 2.3 (1.1) | 2.2 (1.0) | 2.3 (1.2) |
| Daily servings of vegetables b | 2.1 (1.2) | 2.0 (1.2) | 2.1 (1.1) | 2.2 (1.1) | 2.1 (1.2) | 2.3 (1.1) |
| Baseline [24,29] | 5 Year Follow-up | Complete-Case a: between Group Difference at 5 Years b (95% CI) n = 226 | p-Value | Sensitivity analysis: between Group Difference b—Imputed Values c (95% CI) n = 394 | p-Value | |||
|---|---|---|---|---|---|---|---|---|
| Control Mean (SD) n = 127 | Intervention Mean (SD) n = 99 | Control Mean (SD) n = 127 | Intervention Mean (SD) n = 99 | |||||
| Child consumption | ||||||||
| F&V-CDQ score d | 14.7 (4.6) | 15.2 (4.5) | 16.1 (4.4) | 17.5 (3.8) | 1.1 (−0.03 to 2.2) | 0.06 | 1.1 (−0.05 to 2.3) | 0.06 |
| Daily ‘child’ servings of fruit e | 2.2 (1.0) | 2.3 (1.2) | 2.6 (1.1) | 2.8 (1.3) | 0.2 (−0.2 to 0.5) | 0.26 | 0.1 (−0.4 to 0.6) | 0.64 |
| Daily ‘child’ servings of vegetables e | 2.1 (1.2) | 2.3 (1.1) | 2.9 (1.6) | 3.5 (1.5) | 0.5 (0.09 to 0.9) | 0.02 | 0.5 (−0.09 to 1.1) | 0.10 |
| Parent consumption | ||||||||
| Daily servings of fruit | 1.8 (1.1) | 2.0 (1.2) | 1.8 (1.5) | 2.0 (1.1) | 0.2 (−0.2 to 0.5) | 0.30 | 0.3 (−0.09 to 0.6) | 0.15 |
| Daily servings of vegetables | 3.1 (1.4) | 3.3 (1.2) | 3.5 (1.6) | 3.8 (1.4) | 0.2 (−0.2 to 0.6) | 0.27 | 0.2 (−0.3 to 0.8) | 0.44 |
| Baseline | 5 Year Follow-up | Group by Time Differential Effect (95% CI) | p-Value | Group by Time by Sub-Group Differential Effect (95% CI) | p-Value | |||
|---|---|---|---|---|---|---|---|---|
| Control Mean (SD) n = 127 | Intervention Mean (SD) n = 99 | Control Mean (SD) n = 127 | Intervention Mean (SD) n = 99 | |||||
| Child F&V-CDQ score | ||||||||
| Mtg dietary guidelines at baseline | ||||||||
| <14 (n = 82) | 10.0 (3.4) | 10.2 (2.9) | 13.6 (5.0) | 15.4 (3.9) | 1.5 (−0.2 to 3.1) | 0.08 | −0.7 (−2.6 to 1.1) | 0.50 |
| 14 or above (n = 144) | 17.4 (2.6) | 18.0 (2.4) | 17.5 (3.2) | 18.7 (3.3) | 0.7 (−0.6 to 2.1) | 0.30 | ||
| Education | ||||||||
| No university (n = 106) | 13.9 (5.0) | 14.3 (4.9) | 15.5 (5.1) | 16.9 (4.1) | 1.1 (−0.4 to 2.5) | 0.10 | 0.02 (−1.8 to 1.9) | 1.0 |
| University (n = 120) | 15.4 (4.2) | 16.0 (4.0) | 16.6 (3.5) | 18.1 (3.5) | 1.1 (−0.3 to 2.5) | 0.10 | ||
| Income | ||||||||
| <AU$100,000 (n = 121) | 14.5 (4.5) | 14.3 (5.0) | 16.4 (4.2) | 16.9 (4.1) | 0.4 (−0.9 to 1.8) | 0.50 | −1.3 (−3.1 to 0.6) | 0.18 |
| ≥AU$100,000 (n = 102) | 14.9 (4.5) | 16.2 (3.7) | 15.9 (4.3) | 18.2 (3.5) | 1.7 (0.2 to 3.2) | 0.03 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wyse, R.; Stacey, F.; Campbell, L.; Yoong, S.; Lecathelinais, C.; Wiggers, J.; Campbell, K.; Wolfenden, L. 5-Year Follow-Up of a Telephone Intervention to Increase Fruit and Vegetable Consumption in Preschoolers: The ‘Healthy Habits’ Cluster Randomised Trial. Nutrients 2020, 12, 3702. https://doi.org/10.3390/nu12123702
Wyse R, Stacey F, Campbell L, Yoong S, Lecathelinais C, Wiggers J, Campbell K, Wolfenden L. 5-Year Follow-Up of a Telephone Intervention to Increase Fruit and Vegetable Consumption in Preschoolers: The ‘Healthy Habits’ Cluster Randomised Trial. Nutrients. 2020; 12(12):3702. https://doi.org/10.3390/nu12123702
Chicago/Turabian StyleWyse, Rebecca, Fiona Stacey, Libby Campbell, Serene Yoong, Christophe Lecathelinais, John Wiggers, Karen Campbell, and Luke Wolfenden. 2020. "5-Year Follow-Up of a Telephone Intervention to Increase Fruit and Vegetable Consumption in Preschoolers: The ‘Healthy Habits’ Cluster Randomised Trial" Nutrients 12, no. 12: 3702. https://doi.org/10.3390/nu12123702
APA StyleWyse, R., Stacey, F., Campbell, L., Yoong, S., Lecathelinais, C., Wiggers, J., Campbell, K., & Wolfenden, L. (2020). 5-Year Follow-Up of a Telephone Intervention to Increase Fruit and Vegetable Consumption in Preschoolers: The ‘Healthy Habits’ Cluster Randomised Trial. Nutrients, 12(12), 3702. https://doi.org/10.3390/nu12123702





