Stunting and Anemia in Children from Urban Poor Environments in 28 Low and Middle-income Countries: A Meta-analysis of Demographic and Health Survey Data
Abstract
:1. Introduction
2. Data and Methods
2.1. Data
2.2. Variables
2.3. Methods
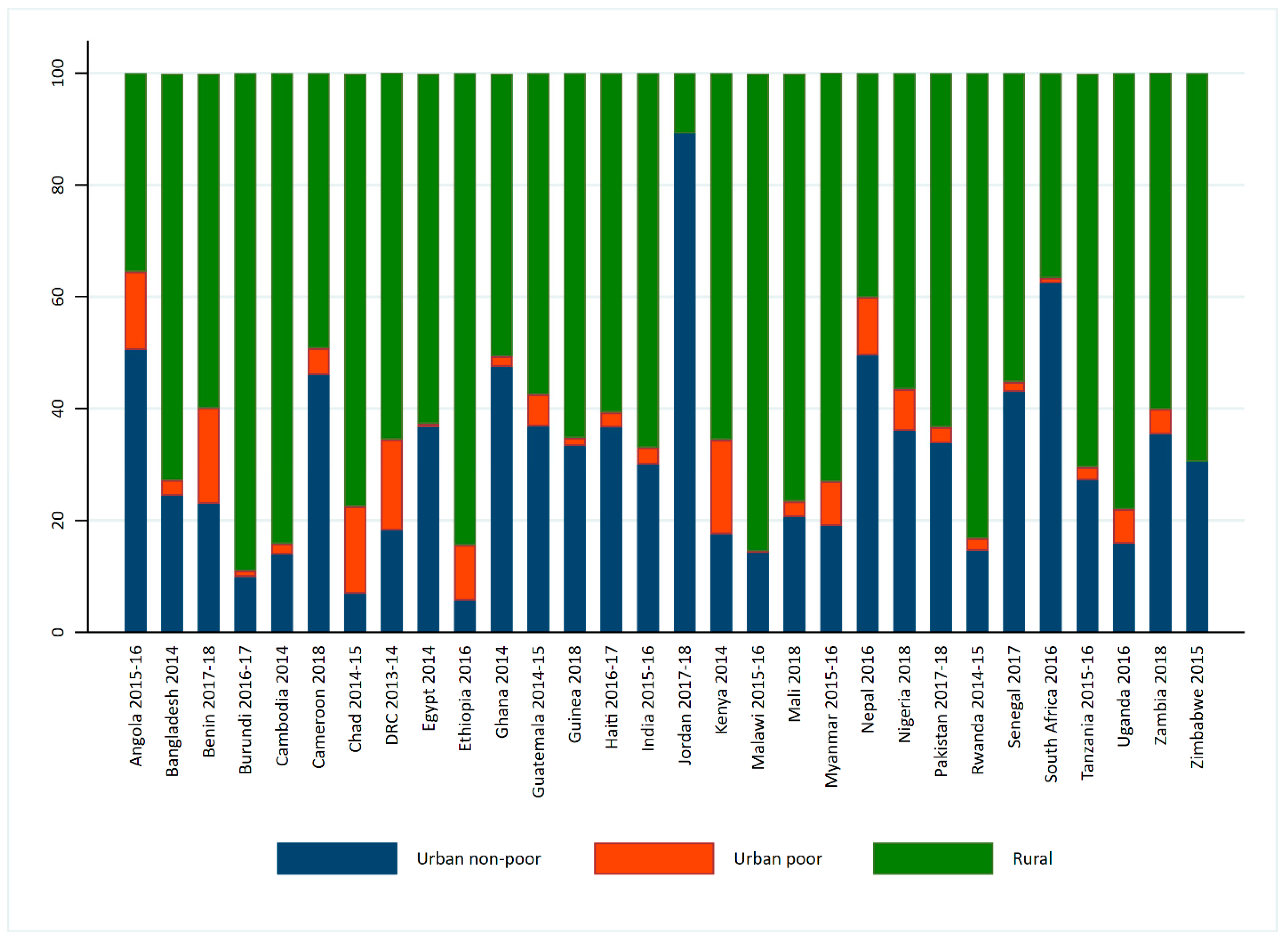
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A
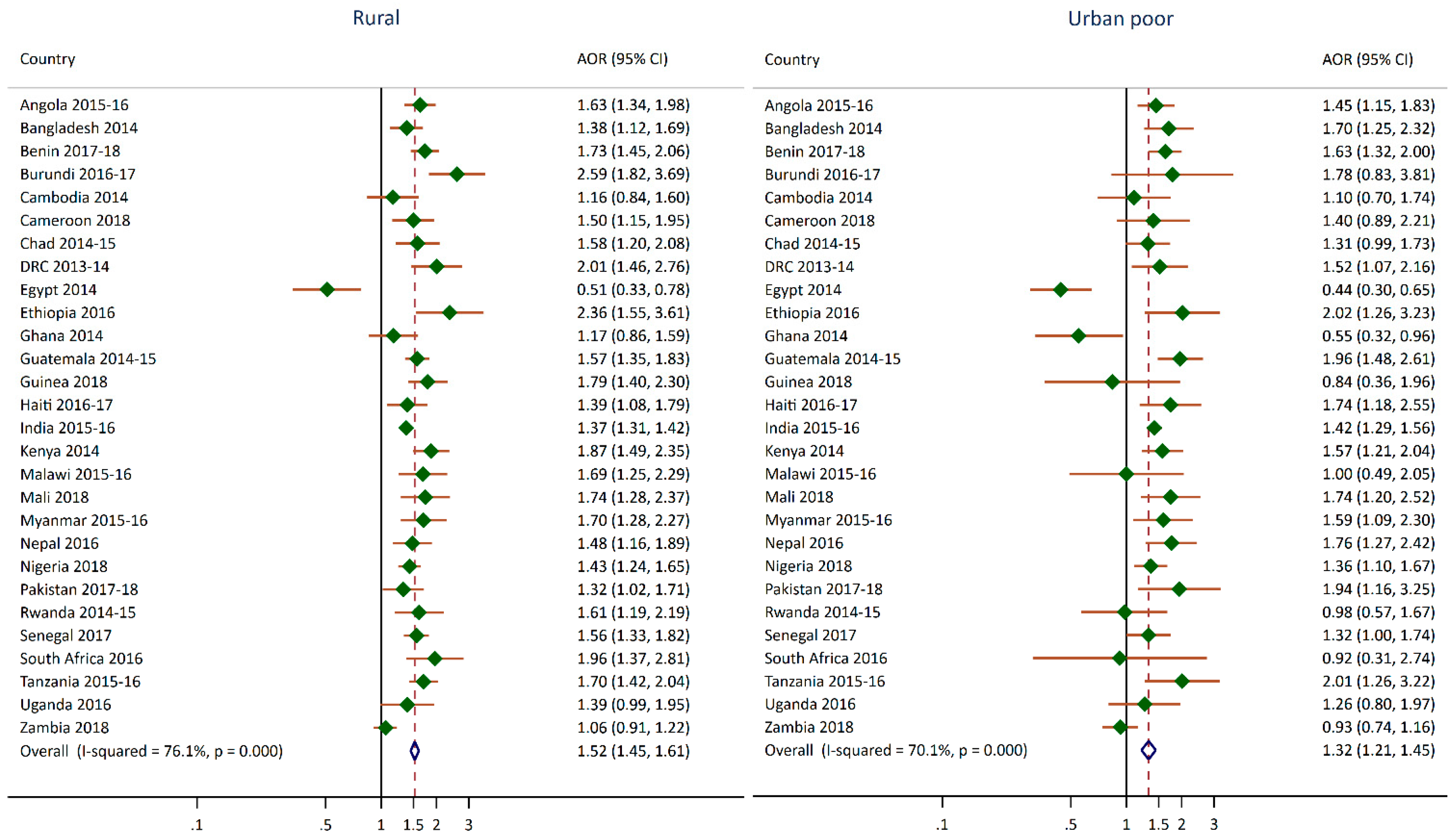
| Survey | Rural | Urban Poor |
|---|---|---|
| Angola 2015–2016 | 1.63 *** (1.34,1.98) | 1.45 ** (1.15,1.83) |
| Bangladesh 2014 | 1.38 ** (1.12,1.69) | 1.70 ** (1.25,2.32) |
| Benin 2017–2018 | 1.73 *** (1.45,2.06) | 1.63 *** (1.32,2) |
| Burundi 2016–2017 | 2.59 *** (1.82,3.69) | 1.78 (0.83,3.81) |
| Cameroon 2018 | 1.5 ** (1.15,1.95) | 1.40 (0.89,2.21) |
| Cambodia 2014 | 1.16 (0.84,1.6) | 1.10 (0.7,1.74) |
| Chad 2014–2015 | 1.58 ** (1.2,2.08) | 1.31 (0.99,1.73) |
| Congo Democratic Republic 2013–2014 | 2.01 *** (1.46,2.76) | 1.52 * (1.07,2.16) |
| Egypt 2014 | 0.51 ** (0.33,0.78) | 0.44 *** (0.3,0.65) |
| Ethiopia 2016 | 2.36 *** (1.55,3.61) | 2.02 ** (1.26,3.23) |
| Ghana 2014 | 1.17 (0.86,1.59) | 0.55 * (0.32,0.96) |
| Guatemala 2014–2015 | 1.57 *** (1.35,1.83) | 1.96 *** (1.48,2.61) |
| Guinea 2018 | 1.79 *** (1.4,2.3) | 0.84 (0.36,1.96) |
| Haiti 2016–2017 | 1.39 * (1.08,1.79) | 1.74 ** (1.18,2.55) |
| India 2015–2016 | 1.37 *** (1.31,1.42) | 1.42 *** (1.29,1.56) |
| Kenya 2014 | 1.87 *** (1.49,2.35) | 1.57 ** (1.21,2.04) |
| Malawi 2015–2016 | 1.69 ** (1.25,2.29) | 1.00 (0.49,2.05) |
| Mali 2018 | 1.74 *** (1.28,2.37) | 1.74 ** (1.2,2.52) |
| Myanmar 2015–2016 | 1.7 *** (1.28,2.27) | 1.59 * (1.09,2.3) |
| Nepal 2016 | 1.48 ** (1.16,1.89) | 1.76 ** (1.27,2.42) |
| Nigeria 2018 | 1.43 *** (1.24,1.65) | 1.36 ** (1.1,1.67) |
| Pakistan 2017–2018 | 1.32 * (1.02,1.71) | 1.94 * (1.16,3.25) |
| Rwanda 2014–2015 | 1.61 ** (1.19,2.19) | 0.98 (0.57,1.67) |
| Senegal 2017 | 1.56 *** (1.33,1.82) | 1.32 * (1,1.74) |
| South Africa 2016 | 1.96 *** (1.37,2.81) | 0.92 (0.31,2.74) |
| Tanzania 2015–2016 | 1.7 *** (1.42,2.04) | 2.01 ** (1.26,3.22) |
| Uganda 2016 | 1.39 (0.99,1.95) | 1.26 (0.8,1.97) |
| Zambia 2018 | 1.06 (0.91,1.22) | 0.93 (0.74,1.16) |
Appendix B
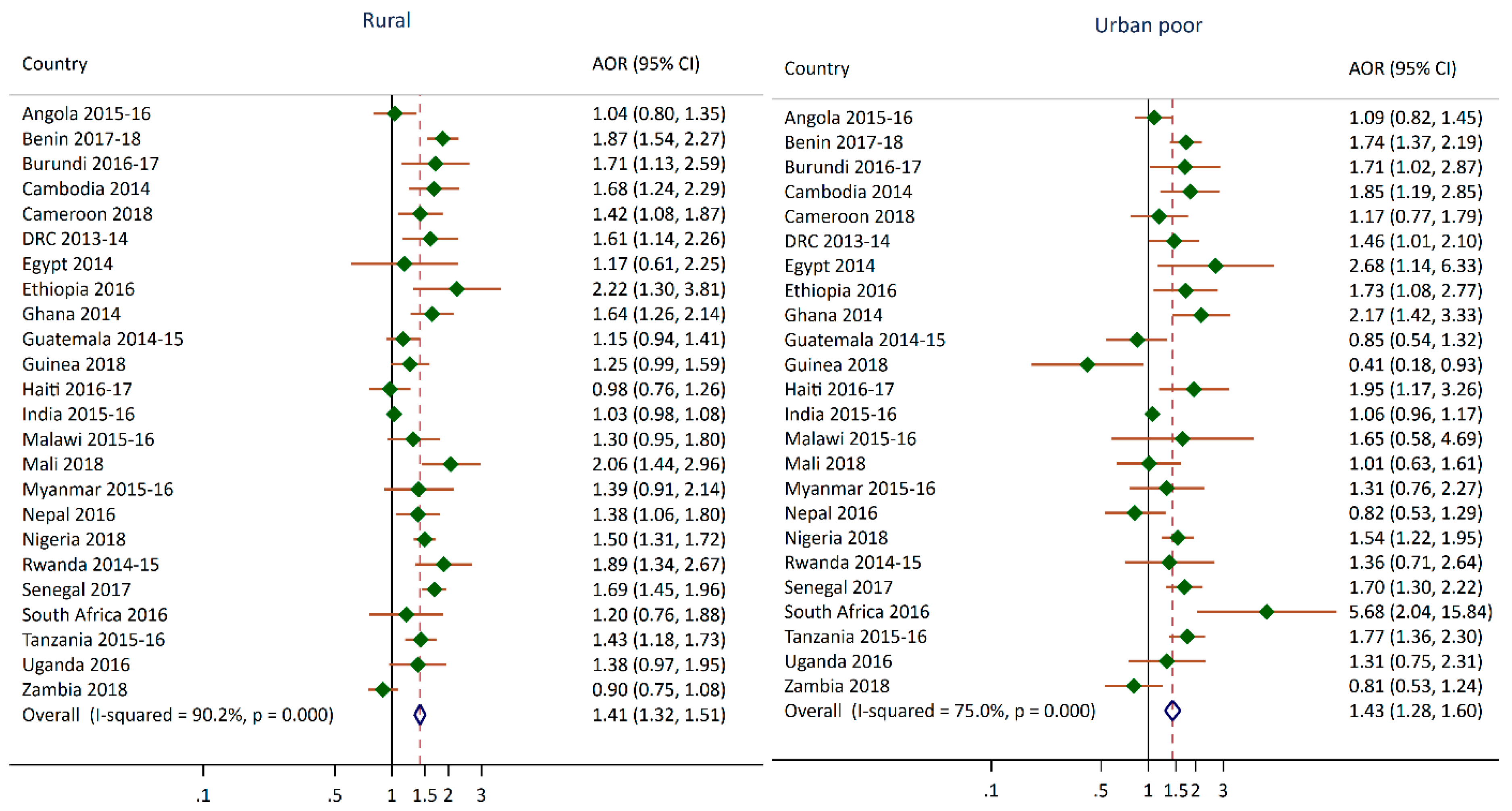
| Survey | Rural | Urban Poor |
|---|---|---|
| Angola 2015–2016 | 1.04 (0.8,1.35) | 1.09 (0.82,1.45) |
| Bangladesh 2014 | NA | NA |
| Benin 2017–2018 | 1.87 *** (1.54,2.27) | 1.74 *** (1.37,2.19) |
| Burundi 2016–2017 | 1.71 * (1.13,2.59) | 1.71 * (1.02,2.87) |
| Cameroon 2018 | 1.42 * (1.08,1.87) | 1.17 (0.77,1.79) |
| Cambodia 2014 | 1.68 ** (1.24,2.29) | 1.85 ** (1.19,2.85) |
| Chad 2014–2015 | NA | NA |
| Congo Democratic Republic 2013–2014 | 1.61 ** (1.14,2.26) | 1.46 * (1.01,2.1) |
| Egypt 2014 | 1.17 (0.61,2.25) | 2.68 * (1.14,6.33) |
| Ethiopia 2016 | 2.22 ** (1.3,3.81) | 1.73 * (1.08,2.77) |
| Ghana 2014 | 1.64 *** (1.26,2.14) | 2.17 *** (1.42,3.33) |
| Guatemala 2014–2015 | 1.15 (0.94,1.41) | 0.85 (0.54,1.32) |
| Guinea 2018 | 1.25 (0.99,1.59) | 0.41 * (0.18,0.93) |
| Haiti 2016–2017 | 0.98 (0.76,1.26) | 1.95 * (1.17,3.26) |
| India 2015–2016 | 1.03 (0.98,1.08) | 1.06 (0.96,1.17) |
| Kenya 2014 | NA | NA |
| Malawi 2015–2016 | 1.3 (0.95,1.8) | 1.65 (0.58,4.69) |
| Mali 2018 | 2.06 *** (1.44,2.96) | 1.01 (0.63,1.61) |
| Myanmar 2015–2016 | 1.39 (0.91,2.14) | 1.31 (0.76,2.27) |
| Nepal 2016 | 1.38 * (1.06,1.8) | 0.82 (0.53,1.29) |
| Nigeria 2018 | 1.5 *** (1.31,1.72) | 1.54 *** (1.22,1.95) |
| Pakistan 2017–2018 | NA | NA |
| Rwanda 2014–2015 | 1.89 *** (1.34,2.67) | 1.36 (0.71,2.64) |
| Senegal 2017 | 1.69 *** (1.45,1.96) | 1.7 *** (1.3,2.22) |
| South Africa 2016 | 1.2 (0.76,1.88) | 5.68 ** (2.04,15.84) |
| Tanzania 2015–2016 | 1.43 *** (1.18,1.73) | 1.77 *** (1.36,2.3) |
| Uganda 2016 | 1.38 (0.97,1.95) | 1.31 (0.75,2.31) |
| Zambia 2018 | 0.9 (0.75,1.08) | 0.81 (0.53,1.24) |
References
- UNICEF. The State of the World’s Children 2019. Children, Food and Nutrition: Growing Well in a Changing World; UNICEF: New York, NY, USA, 2019. [Google Scholar]
- Global Nutrition Report. 2020 Global Nutrition Report: Action on Equity to End Malnutrition; Development Initiatives: Bristol, UK, 2020. [Google Scholar]
- Gardner, W.; Kassebaum, N. Global, Regional, and National Prevalence of Anemia and Its Causes in 204 Countries and Territories, 1990–2019. Curr. Dev. Nutr. 2020, 4, 830. [Google Scholar] [CrossRef]
- Stevens, G.A.; Finucane, M.M.; De-Regil, L.M.; Paciorek, C.J.; Flaxman, S.R.; Branca, F.; Peña-Rosas, J.P.; Bhutta, Z.A.; Ezzati, M.; Nutrition Impact Model Study Group. Global, regional, and national trends in haemoglobin concentration and prevalence of total and severe anaemia in children and pregnant and non-pregnant women for 1995–2011: A systematic analysis of population-representative data. Lancet Glob. Health 2013, 1, e16–e25. [Google Scholar] [CrossRef] [Green Version]
- Grantham-McGregor, S.; Cheung, Y.B.; Cueto, S.; Glewwe, P.; Richter, L.; Strupp, B.; International Child Development Steering Group. Developmental potential in the first 5 years for children in developing countries. Lancet 2007, 369, 60–70. [Google Scholar] [CrossRef] [Green Version]
- WHO. Stunted Growth and Development: Context, Causes and Consequences; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Grantham-McGregor, S.; Smith, J. The Effect of Malnutrition and Micronutrient Deficiency on Children’s Mental Health. Ment. Health Illn. Child. Adolesc. 2020, 1–20. [Google Scholar] [CrossRef]
- Prado, E.L.; Dewey, K.G. Nutrition and brain development in early life. Nutr. Rev. 2014, 72, 267–284. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- United Nations Human Settlements Programme. State of the World’s Cities 2008/2009: Harmonious Cities; UN-HABITAT: Sterling, VA, USA, 2008. [Google Scholar]
- Lucci, P.; Bhatkal, T.; Khan, A. Are we underestimating urban poverty? World Dev. 2018, 103, 297–310. [Google Scholar] [CrossRef]
- DESA. World Urbanization Prospects: The 2018 Revision; Department of Economic and Social Affairs, Population Division, United Nations: New York, NY, USA, 2018. [Google Scholar]
- Assaf, S.; Kothari, M.T.; Pullum, T. An Assessment of the Quality of DHS Anthropometric Data, 2005-2014; ICF International: Rockville, MA, USA, 2015. [Google Scholar]
- Assaf, S.; Pullum, T. Levels and Trends in Maternal and Child Health Disparities by Wealth and Region in Eleven Countries with DHS Surveys; ICF International: Rockville, MA, USA, 2016. [Google Scholar]
- Eckert, S.; Kohler, S. Urbanization and health in developing countries: A systematic review. World Health Popul. 2014, 15, 7–20. [Google Scholar] [CrossRef]
- Rutstein, S.O.; Staveteig, S.; Winter, R.; Yourkavitch, J. Urban Child Poverty, Health, and Survival in Low- and Middle-Income Countries; ICF International: Rockville, MA, USA, 2016. [Google Scholar]
- Van de Poel, E.; Hosseinpoor, A.R.; Speybroeck, N.; Van Ourti, T.; Vega, J. Socioeconomic inequality in malnutrition in developing countries. Bull. World Health Organ. 2008, 86, 282–291. [Google Scholar] [CrossRef] [Green Version]
- Baye, K.; Laillou, A.; Chitweke, S. Socio-Economic Inequalities in Child Stunting Reduction in Sub-Saharan Africa. Nutrients 2020, 12, 253. [Google Scholar] [CrossRef] [Green Version]
- Van de Poel, E.; O’Donnell, O.; Van Doorslaer, E. Are urban children really healthier? Evidence from 47 developing countries. Soc. Sci. Med. 2007, 65, 1986–2003. [Google Scholar] [CrossRef]
- Ezeh, A.; Oyebode, O.; Satterthwaite, D.; Chen, Y.-F.; Ndugwa, R.; Sartori, J.; Mberu, B.; Melendez-Torres, G.J.; Haregu, T.; Watson, S.I. The history, geography, and sociology of slums and the health problems of people who live in slums. Lancet 2017, 389, 547–558. [Google Scholar] [CrossRef]
- Fink, G.; Günther, I.; Hill, K. Slum residence and child health in developing countries. Demography 2014, 51, 1175–1197. [Google Scholar] [CrossRef] [PubMed]
- Kyu, H.H.; Shannon, H.S.; Georgiades, K.; Boyle, M.H. Association of urban slum residency with infant mortality and child stunting in low and middle income countries. Biomed Res. Int. 2013. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- UNICEF; WHO; World Bank. Levels and Trends in Child Malnutrition: Key Findings of the 2018 Edition of the Joint Child Malnutrition Estimates; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- WHO. The Double Burden of Malnutrition: Policy Brief; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- WHO. Report of the Commission on Ending Childhood Obesity; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- Akombi, B.J.; Chitekwe, S.; Sahle, B.W.; Renzaho, A. Estimating the Double Burden of Malnutrition among 595,975 Children in 65 Low-and Middle-Income Countries: A Meta-Analysis of Demographic and Health Surveys. Int. J. Environ. Res. Public Health 2019, 16, 2886. [Google Scholar] [CrossRef] [Green Version]
- Popkin, B.M.; Corvalan, C.; Grummer-Strawn, L.M. Dynamics of the double burden of malnutrition and the changing nutrition reality. Lancet 2020, 395, 65–74. [Google Scholar] [CrossRef]
- Tzioumis, E.; Kay, M.C.; Bentley, M.E.; Adair, L.S. Prevalence and trends in the childhood dual burden of malnutrition in low-and middle-income countries, 1990–2012. Public Health Nutr. 2016, 19, 1375–1388. [Google Scholar] [CrossRef] [Green Version]
- Popkin, B.M. Nutrition transition and the global diabetes epidemic. Curr. Diabetes Rep. 2015, 15, 64. [Google Scholar] [CrossRef]
- Ruel, M.T.; Garrett, J.; Yosef, S.; Olivier, M. Urbanization, food security and nutrition. In Nutrition and Health in a Developing World; Springer: New York, NY, USA, 2017; pp. 705–735. [Google Scholar]
- United Nations, Department of Economic and Social Affairs Population Dynamics, Population Division. World Population Prospects 2019, Online Edition. Rev. 1. Available online: https://population.un.org/wpp/ (accessed on 11 September 2020).
- United Nations Human Settlements Programme. UN-HABITAT State of the World’s Cities 2006/7; UN-HABITAT: Nairobi, Kenya, 2007. [Google Scholar]
- UN-Habitat. Slum Almanac 2015/2016. Tracking Improvement in the Lives of Slum Dwellers; UN-Habitat: Nairobi, Kenya, 2016. [Google Scholar]
- Harris, R.J.; Deeks, J.J.; Altman, D.G.; Bradburn, M.J.; Harbord, R.M.; Sterne, J.A. Metan: Fixed-and random-effects meta-analysis. Stata J. 2008, 8, 3–28. [Google Scholar] [CrossRef] [Green Version]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [Green Version]
- Assaf, S.; Juan, C. Variations in Health Outcomes with Alternative Measures of Urbanicity, Using Demographic and Health Surveys 2013-18; ICF: Rockville, MA, USA, 2020. [Google Scholar]
- Menon, P.; Ruel, M.T.; Morris, S.S. Socio-economic differentials in child stunting are consistently larger in urban than in rural areas. Food Nutr. Bull. 2000, 21, 282–289. [Google Scholar] [CrossRef] [Green Version]
- Mberu, B.U.; Haregu, T.N.; Kyobutungi, C.; Ezeh, A.C. Health and health-related indicators in slum, rural, and urban communities: A comparative analysis. Glob. Health Action 2016, 9, 33163. [Google Scholar] [CrossRef] [PubMed]
- World Bank Group. Scaling Up Nutrition in the Arab Republic of Egypt: Investing in a Healthy Future; Herbst, C.H., Elshalakani, A., Kakietek, J., Hafiz, A., Petrovic, O., Eds.; World Bank: Washington, DC, USA, 2020. [Google Scholar]
- Hassan, H.; Moussa, W.; Ismail, I. Assessment of dietary changes and their health implications in countries facing the double burden of malnutrition: Egypt, 1980 to 2005. Double Burd. Malnutrition 2006, 43, 22. [Google Scholar]
- Atsu, B.K.; Guure, C.; Laar, A.K. Determinants of overweight with concurrent stunting among Ghanaian children. BMC Pediatrics 2017, 17, 177. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cyril, S.; Oldroyd, J.C.; Renzaho, A. Urbanisation, urbanicity, and health: A systematic review of the reliability and validity of urbanicity scales. BMC Public Health 2013, 13, 513. [Google Scholar] [CrossRef] [Green Version]
- Unger, A.; Riley, L.W. Slum health: From understanding to action. PLoS Med. 2007, 4, e295. [Google Scholar] [CrossRef] [Green Version]
- Tacoli, C. Food security in rapidly urbanising, low-income contexts. Int. J. Environ. Res. Public Health 2017, 14, 1554. [Google Scholar] [CrossRef] [Green Version]
- Fish, T.D.; Janocha, B.; Dontamsetti, T.; Mayala, B.K. Geospatial Covariates: Proxies for Mapping Urban-Related Indicators; ICF: Rockville, MA, USA, 2020. [Google Scholar]
- Jones, A.D.; Acharya, Y.; Galway, L.P. Urbanicity gradients are associated with the household-and individual-level double burden of malnutrition in sub-Saharan Africa. J. Nutr. 2016, 146, 1257–1267. [Google Scholar] [CrossRef] [Green Version]
| Country | DHS Survey | Number of Households Interviewed | Projected Population in 2020 (Thousands) * |
|---|---|---|---|
| Angola | 2015–2016 | 16,109 | 32,866 |
| Bangladesh | 2014 | 17,300 | 164,689 |
| Benin | 2017–2018 | 14,156 | 12,123 |
| Burundi | 2016–2017 | 15,977 | 11,891 |
| Cameroon | 2018 | 11,710 | 26,546 |
| Cambodia | 2014 | 15,825 | 16,719 |
| Chad | 2014–2015 | 17,233 | 16,426 |
| DRC | 2013–2014 | 18,171 | 89,561 |
| Egypt | 2014 | 28,175 | 102,334 |
| Ethiopia | 2016 | 16,650 | 114,964 |
| Ghana | 2014 | 11,835 | 31,073 |
| Guatemala | 2014–2015 | 21,383 | 17,916 |
| Guinea | 2018 | 7912 | 13,133 |
| Haiti | 2016–2017 | 13,405 | 11,403 |
| India | 2015–2016 | 601,509 | 1,380,004 |
| Jordan | 2017–2018 | 18,802 | 10,203 |
| Kenya | 2014 | 36,430 | 53,771 |
| Malawi | 2015–2016 | 26,361 | 19,130 |
| Mali | 2018 | 9510 | 20,251 |
| Myanmar | 2015–2016 | 12,500 | 54,410 |
| Nepal | 2016 | 11,040 | 29,137 |
| Nigeria | 2018 | 40,427 | 206,140 |
| Pakistan | 2017–2018 | 11,869 | 220,892 |
| Philippines | 2017 | 27,496 | 109,581 |
| Rwanda | 2014–2015 | 12,699 | 12,952 |
| Senegal | 2017 | 8380 | 16,744 |
| South Africa | 2016 | 11,083 | 59,309 |
| Tanzania | 2015–2016 | 12,563 | 59,734 |
| Uganda | 2016 | 19,588 | 45,741 |
| Zambia | 2018 | 12,831 | 18,384 |
| Zimbabwe | 2015 | 10,534 | 14,863 |
| Survey | Total | Urban non-Poor | Urban Poor | Rural | p-Value |
|---|---|---|---|---|---|
| Angola 2015–2016 | 37.6 (35.7,39.5) | 28.2 (24.5,32.3) | 41.4 (37.8,45.0) | 45.7 (43.5,47.9) | 0.001 |
| Bangladesh 2014 | 36.1 (34.4,37.9) | 28.5 (25.0,32.2) | 47.6 (40.1,55.2) | 37.9 (35.9,39.9) | 0.001 |
| Benin 2017–2018 | 32.2 (30.9,33.4) | 21.7 (19.6,23.9) | 33.9 (31.2,36.8) | 35.2 (33.7,36.8) | 0.001 |
| Burundi 2016–2017 | 55.9 (54.2,57.7) | 25.7 (20.1,32.2) | 45.1 (24.8,67.1) | 58.8 (57.0,60.5) | 0.001 |
| Cameroon 2018 | 28.9 (27.1,30.8) | 18.1 (15.7,20.8) | 32.7 (23.0,44.2) | 36.2 (33.7,38.8) | 0.001 |
| Cambodia 2014 | 32.4 (30.6,34.3) | 22.5 (18.9,26.6) | 30.9 (24.2,38.5) | 33.8 (31.8,35.9) | 0.001 |
| Chad 2014–2015 | 39.9 (38.4,41.3) | 25.0 (21.3,29.1) | 35.0 (31.7,38.5) | 41.6 (39.9,43.4) | 0.001 |
| Democratic Republic of the Congo 2013–2014 | 42.7 (40.9,44.5) | 25.1 (20.5,30.3) | 39.0 (35.3,42.9) | 47.1 (44.9,49.4) | 0.001 |
| Egypt 2014 | 21.4 (20.1,22.9) | 23.1 (20.5,26.0) | 15.9 (12.3,20.4) | 20.7 (19.1,22.4) | 0.112 |
| Ethiopia 2016 | 38.4 (36.5,40.3) | 14.6 (11.5,18.4) | 29.8 (23.6,36.7) | 39.9 (37.9,42.0) | 0.001 |
| Ghana 2014 | 18.8 (17.0,20.6) | 14.8 (12.4,17.6) | 15.1 (11.4,19.8) | 22.1 (19.7,24.7) | 0.001 |
| Guatemala 2014–2015 | 46.5 (44.8,48.2) | 30.0 (27.8,32.3) | 55.1 (47.5,62.4) | 53.0 (50.8,55.1) | 0.001 |
| Guinea 2018 | 30.3 (28.6,32.1) | 21.7 (18.9,24.9) | 21.3 (10.5,38.5) | 33.8 (31.8,35.9) | 0.001 |
| Haiti 2016–2017 | 21.9 (20.5,23.5) | 16.8 (14.6,19.2) | 29.4 (22.0,38.1) | 23.9 (22.0,25.9) | 0.001 |
| India 2015–2016 | 38.4 (38.1,38.7) | 29.4 (28.6,30.2) | 42.6 (40.8,44.5) | 41.2 (40.8,41.5) | 0.001 |
| Kenya 2014 | 26.0 (25.1,27.0) | 16.3 (13.6,19.4) | 23.2 (21.1,25.4) | 29.1 (27.9,30.2) | 0.001 |
| Malawi 2015–2016 | 37.1 (35.6,38.7) | 25.0 (20.7,29.8) | (24.3) (16.0,35.2) | 38.9 (37.2,40.6) | 0.001 |
| Mali 2018 | 26.9 (25.6,28.2) | 15.4 (13.6,17.5) | 27.8 (21.2,35.5) | 29.4 (27.9,30.9) | 0.001 |
| Myanmar 2015–2016 | 29.2 (27.3,31.1) | 17.0 (13.9,20.6) | 25.1 (19.8,31.3) | 31.6 (29.5,33.9) | 0.001 |
| Nepal 2016 | 35.8 (33.5,38.3) | 28.3 (25.0,31.7) | 44.1 (37.6,50.8) | 40.2 (36.6,43.9) | 0.001 |
| Nigeria 2018 | 36.8 (35.6,38.1) | 24.2 (22.3,26.3) | 39.6 (35.7,43.6) | 44.8 (43.2,46.3) | 0.001 |
| Pakistan 2017–2018 | 37.6 (34.8,40.6) | 28.4 (24.9,32.2) | 55.7 (44.5,66.4) | 40.9 (37.1,44.9) | 0.001 |
| Rwanda 2014–2015 | 37.9 (36.1,39.6) | 22.7 (19.0,26.9) | 28.9 (15.8,47.0) | 40.6 (38.6,42.6) | 0.001 |
| Senegal 2017 | 16.5 (15.6,17.5) | 9.5 (8.3,10.8) | 23.3 (18.6,28.8) | 20.2 (19.0,21.4) | 0.001 |
| South Africa 2016 | 27.4 (24.3,30.7) | 26.0 (20.9,31.7) | ND | 29.2 (25.8,32.8) | 0.338 |
| Tanzania 2015–2016 | 34.4 (33.0,35.9) | 22.8 (20.5,25.3) | 39.5 (24.1,57.3) | 37.8 (36.1,39.4) | 0.001 |
| Uganda 2016 | 28.9 (27.3,30.5) | 20.0 (16.5,24.1) | 31.6 (25.6,38.2) | 30.2 (28.4,32.0) | 0.001 |
| Zambia 2018 | 34.6 (33.4,35.8) | 31.9 (29.6,34.4) | 33.8 (28.9,39.1) | 35.9 (34.4,37.3) | 0.016 |
| Survey | Total | Urban non-Poor | Urban Poor | Rural | p-Value |
|---|---|---|---|---|---|
| Angola 2015–2016 | 34.1 (32.2,36.1) | 32.6 (29.7,35.7) | 35.3 (31.1,39.7) | 35.1 (32.0,38.3) | 0.419 |
| Bangladesh 2014 | NA | NA | NA | NA | |
| Benin 2017–2018 | 43.9 (42.2,45.6) | 28.9 (26.1,31.9) | 47.5 (43.5,51.6) | 47.8 (45.6,50.0) | 0.001 |
| Burundi 2016–2017 | 36.3 (34.6,38.1) | 23.6 (17.8,30.7) | 31.7 (26.2,37.9) | 37.5 (35.6,39.3) | 0.001 |
| Cameroon 2018 | 31.0 (29.1,33.0) | 25.5 (22.8,28.5) | 30.7 (23.9,38.5) | 34.8 (32.0,37.8) | 0.001 |
| Cambodia 2014 | 25.7 (24.0,27.5) | 15.7 (12.6,19.3) | 29.2 (24.2,34.9) | 27.0 (25.0,29.0) | 0.001 |
| Chad 2014–2015 | NA | NA | NA | NA | |
| Democratic Republic of the Congo 2013–2014 | 34.8 (32.5,37.1) | 26.6 (23.3,30.1) | 35.5 (30.3,41.1) | 36.2 (33.1,39.3) | 0.005 |
| Egypt 2014 | 9.5 (8.3,10.7) | 6.2 (4.8,7.9) | (14.0) (4.0,38.7) | 11.0 (9.5,12.7) | 0.001 |
| Ethiopia 2016 | 32.0 (29.5,34.6) | 21.7 (16.1,28.5) | 26.2 (20.8,32.4) | 32.8 (30.0,35.6) | 0.011 |
| Ghana 2014 | 39.1 (36.3,41.9) | 29.6 (25.9,33.6) | 52.2 (37.5,66.5) | 46.2 (42.6,49.8) | 0.001 |
| Guatemala 2014–2015 | 12.1 (11.3,13.0) | 9.3 (8.1,10.6) | 9.1 (6.8,12.1) | 13.6 (12.5,14.8) | 0.001 |
| Guinea 2018 | 43.8 (41.6,46.0) | 40.4 (36.7,44.3) | 23.9 (14.3,37.2) | 45.7 (43.0,48.3) | 0.001 |
| Haiti 2016–2017 | 37.5 (35.7,39.3) | 36.4 (33.0,40.0) | 54.4 (42.1,66.2) | 37.2 (35.1,39.3) | 0.005 |
| India 2015–2016 | 30.7 (30.4,31.0) | 28.7 (27.9,29.5) | 32.8 (31.0,34.7) | 31.3 (30.9,31.7) | 0.001 |
| Kenya 2014 | NA | NA | NA | NA | |
| Malawi 2015–2016 | 36.1 (34.2,38.1) | 29.4 (23.9,35.6) | ND | 37.1 (35.0,39.2) | 0.020 |
| Mali 2018 | 56.7 (54.6,58.8) | 45.1 (41.2,49.2) | 43.1 (31.4,55.5) | 59.7 (57.2,62.1) | 0.001 |
| Myanmar 2015–2016 | 26.7 (24.7,28.9) | 20.3 (15.5,26.2) | 27.4 (19.9,36.4) | 27.6 (25.3,30.1) | 0.087 |
| Nepal 2016 | 26.4 (24.0,29.1) | 21.5 (18.4,24.9) | 24.0 (17.3,32.2) | 31.2 (27.5,35.2) | 0.001 |
| Nigeria 2018 | 41.1 (39.7,42.5) | 31.6 (29.5,33.9) | 48.6 (43.4,53.8) | 46.4 (44.5,48.2) | 0.001 |
| Pakistan 2017–2018 | NA | NA | NA | NA | |
| Rwanda 2014–2015 | 15.8 (14.4,17.2) | 9.0 (7.0,11.6) | 13.4 (5.8,27.8) | 16.9 (15.4,18.5) | 0.001 |
| Senegal 2017 | 41.8 (40.2,43.4) | 29.7 (27.3,32.2) | 48.9 (42.9,54.8) | 48.1 (46.2,50.0) | 0.001 |
| South Africa 2016 | 37.0 (32.9,41.3) | 41.2 (34.0,48.9) | ND | 32.9 (29.1,36.9) | 0.108 |
| Tanzania 2015–2016 | 31.3 (29.6,33.0) | 26.0 (23.8,28.3) | 38.8 (25.1,54.6) | 32.6 (30.6,34.7) | 0.001 |
| Uganda 2016 | 29.1 (27.3,31.1) | 24.2 (20.1,28.8) | 25.4 (17.9,34.6) | 30.2 (28.1,32.4) | 0.060 |
| Zambia 2018 | 29.5 (28.1,30.9) | 30.3 (27.8,32.9) | 29.9 (24.1,36.5) | 29.1 (27.4,30.8) | 0.694 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Assaf, S.; Juan, C. Stunting and Anemia in Children from Urban Poor Environments in 28 Low and Middle-income Countries: A Meta-analysis of Demographic and Health Survey Data. Nutrients 2020, 12, 3539. https://doi.org/10.3390/nu12113539
Assaf S, Juan C. Stunting and Anemia in Children from Urban Poor Environments in 28 Low and Middle-income Countries: A Meta-analysis of Demographic and Health Survey Data. Nutrients. 2020; 12(11):3539. https://doi.org/10.3390/nu12113539
Chicago/Turabian StyleAssaf, Shireen, and Christina Juan. 2020. "Stunting and Anemia in Children from Urban Poor Environments in 28 Low and Middle-income Countries: A Meta-analysis of Demographic and Health Survey Data" Nutrients 12, no. 11: 3539. https://doi.org/10.3390/nu12113539





