Effectiveness of Interventions for Managing Acute Malnutrition in Children under Five Years of Age in Low-Income and Middle-Income Countries: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Objective
- To evaluate the effectiveness of community-based strategies, such as community-based mobilization, screening, follow-up, counselling, and education; to improve screening, identification, and management of SAM and MAM;
- To evaluate the effectiveness of facility-based strategies, such as facility-based screening, management, and periodic follow-up, to improve screening and management of SAM and MAM;
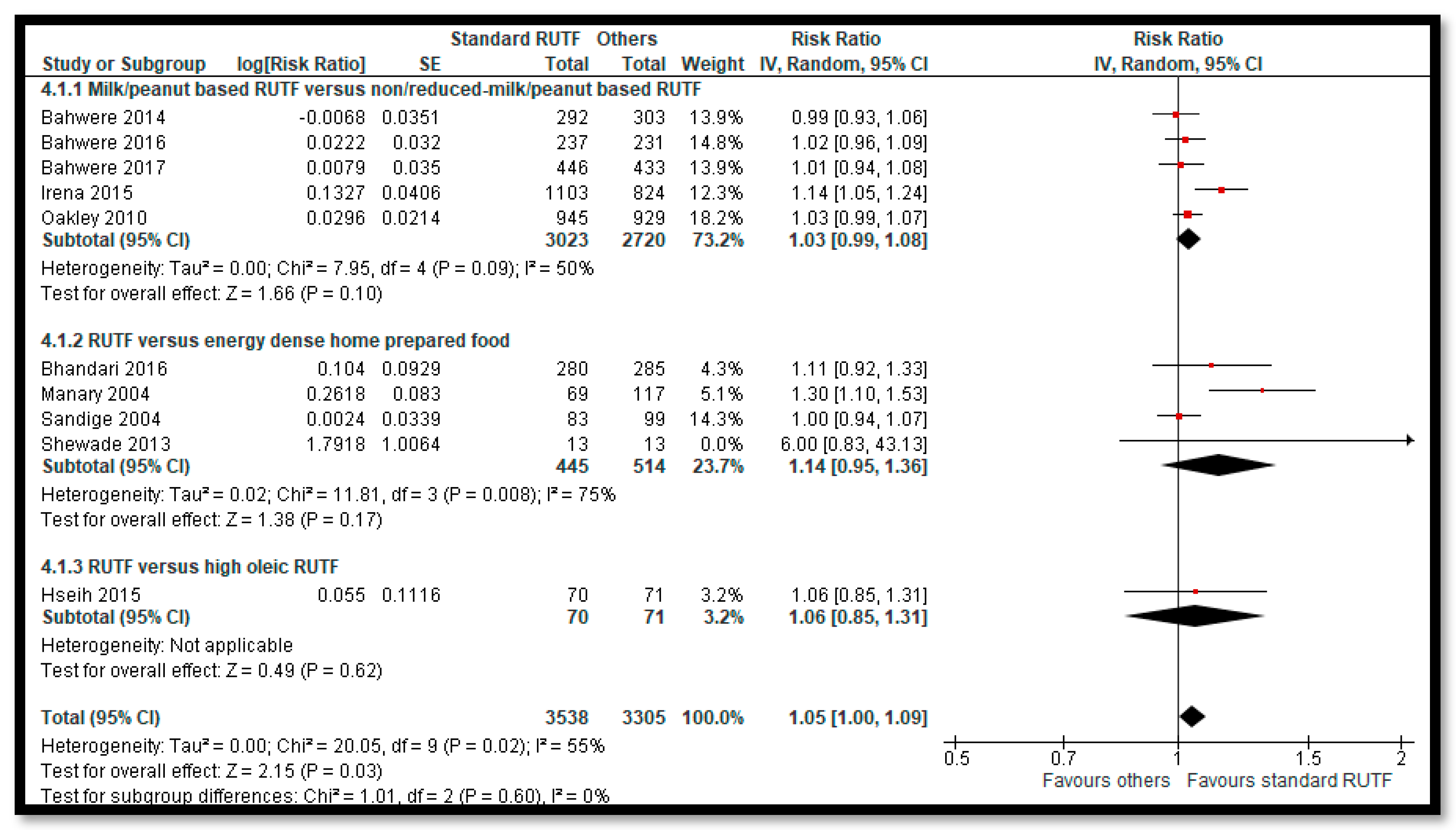
- To evaluate the effectiveness and relative effectiveness of various RUTF and RUSF for the management of SAM and MAM;
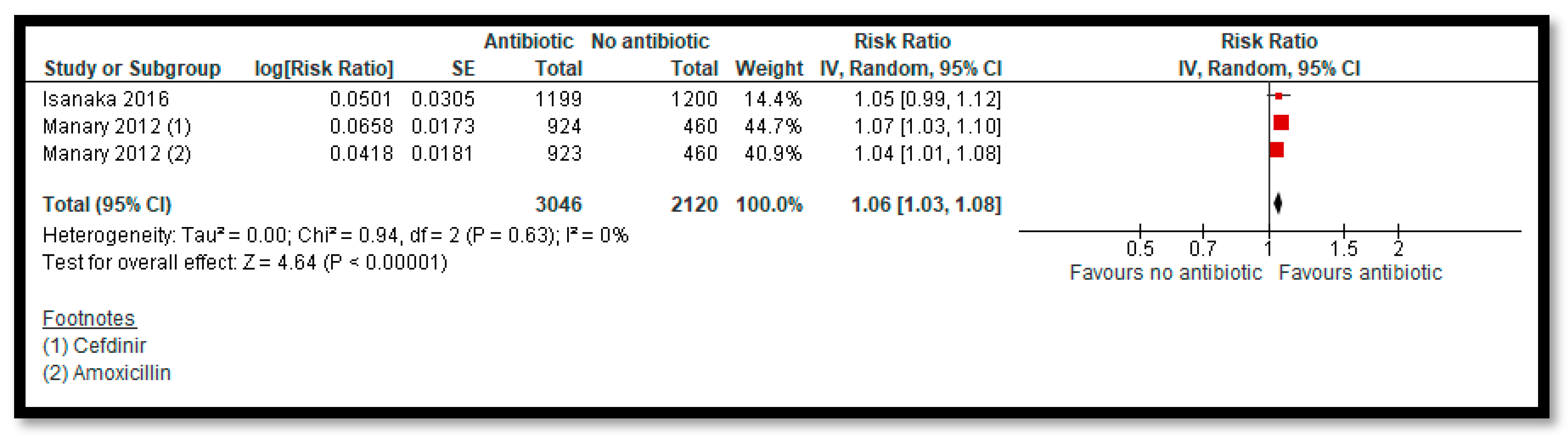
- To evaluate the effectiveness of prophylactic use of antibiotic to manage uncomplicated SAM;
- To evaluate the effectiveness of various doses of vitamin A supplement to manage children with SAM and MAM.
2.2. Type of Studies and Participants
2.3. Type of Interventions
2.4. Type of Outcomes
2.5. Search Methods
2.6. Data Collection and Analysis
2.7. Quality Assessment
3. Results
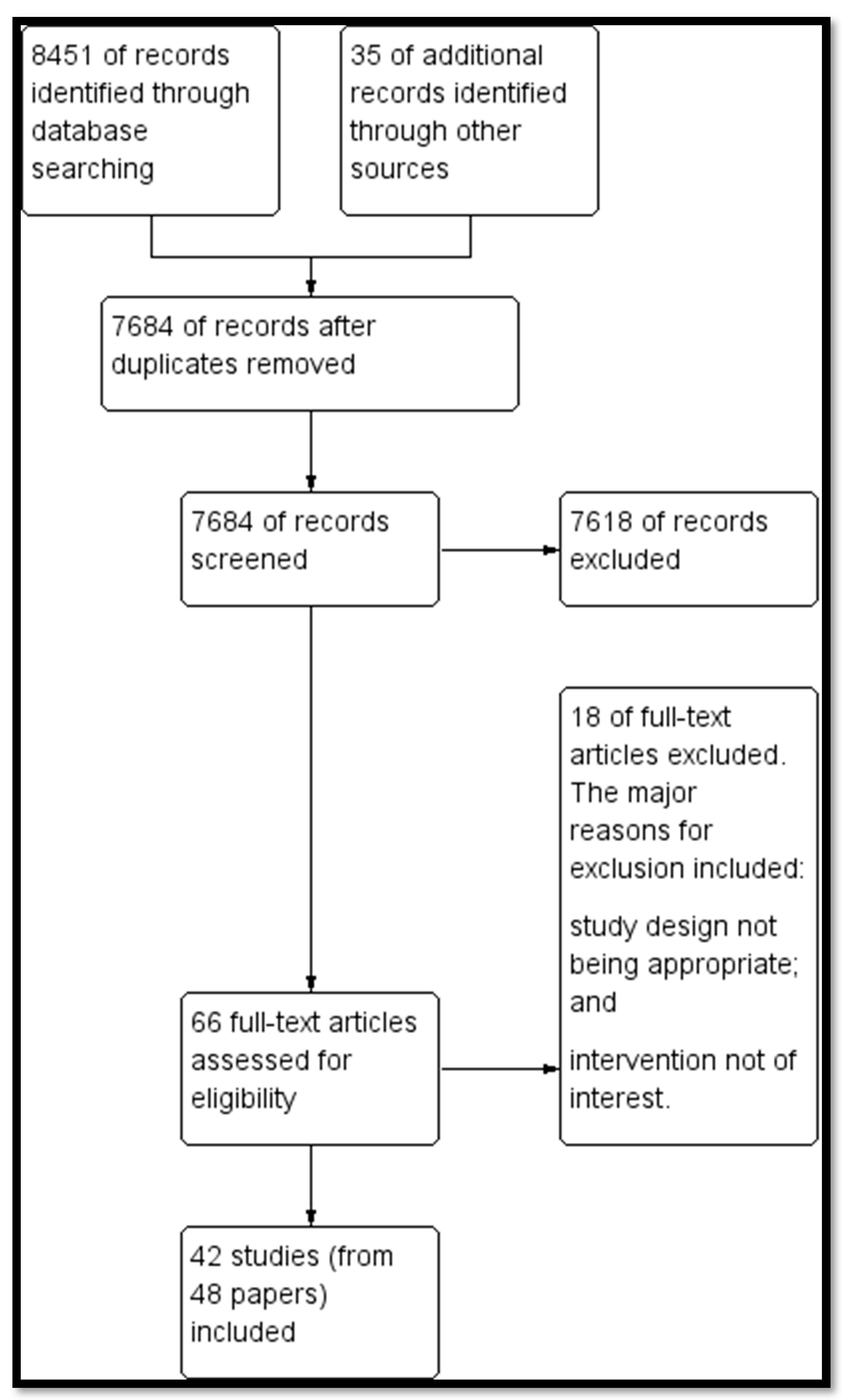
3.1. Results of the Search
3.2. Description of Included Studies
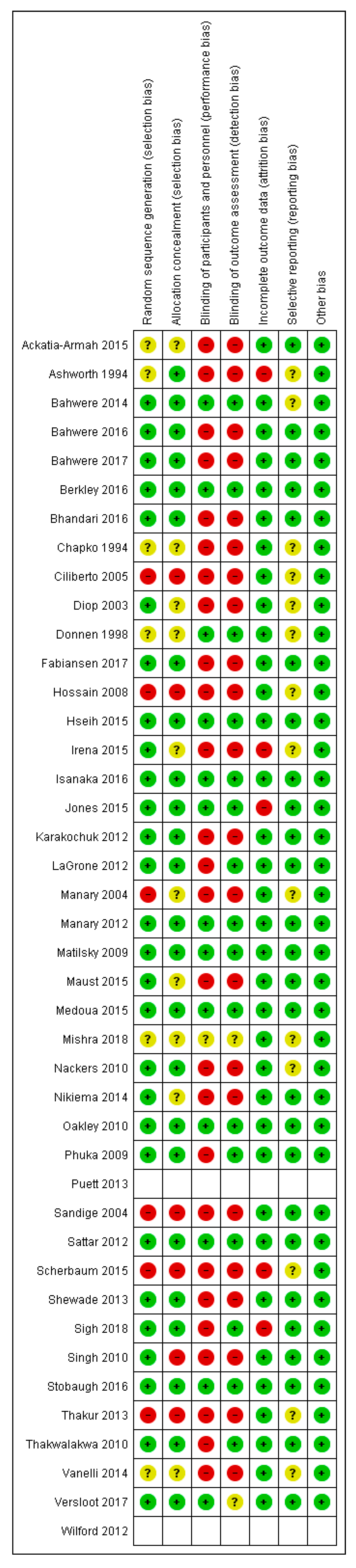
3.3. Risk of Bias
3.4. Effects of Intervention
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Appendix A. Search Strategy
Appendix B. Reasons for Exclusion for Excluded Studies
| Study | Reason for Exclusion |
| Agha 2004 [67] | This study did not have an appropriate control group. |
| Aguayo 2018 [68] | The study design was not appropriate. |
| Ahmed 1999 [69] | The study design was not appropriate. |
| Ashworth 2004 [70] | The study design was not appropriate. |
| Bachou 2008 [71] | The study design was not appropriate. |
| Badaloo 1999 [72] | This study did not assess the intervention of interest; study compared high protein formula with low protein formula. |
| Baker 1978 [73] | The study did not assess the intervention of interest; study compared milk diet with soy-maize-porridge diet. |
| Bhandari 2001 [74] | The study did not assess the intervention of interest; study compared food supplementation with counselling with nutritional counselling alone. |
| Burza 2016 [75] | The study design was not appropriate. |
| Donnen 2007 [76] | This study included children up to 14 years of age |
| Dubray 2008 [77] | This study compared two different antibiotics (ceftriaxone vs amoxicillin) in children with SAM and did not have an appropriate control group (no antibiotic/placebo). |
| Javan 2017 [78] | This study was conducted in Upper Middle Income Country. |
| Linneman 2007 [79] | This study did not have an appropriate control group. |
| Nagar 2016 [80] | This study did not have an appropriate control group. |
| Roy 2005 [81] | The study did not assess the intervention of interest; study compared supplementary feeding with education to feeding alone. |
| Simpore 2006 [82] | This study did not have an appropriate control group. |
| Zongo 2013 [83] | The study did not assess the intervention of interest; the study compared Moringa leaf in addition to the usual porridge diet. |
References
- World Health Organization (WHO). Malnutrition. Fact Sheet. 2017. Available online: https://www.who.int/news-room/fact-sheets/detail/malnutrition (accessed on 5 December 2019).
- UNICEF. Types of Undernutrition: Growthz Failure-UNICEF. 2009. Available online: https://www.unicef.org/nutrition/training/2.3/contents.html (accessed on 5 December 2019).
- Hawkes, C. Global Nutrition Report 2017: Nourishing the SDGs. Development Initiatives. 2017. Available online: https://data.unicef.org/resources/global-nutrition-report-2017-nourishing-sdgs/ (accessed on 5 December 2019).
- UNICEF; WHO. International Bank for Reconstruction and Development/The World Bank, Levels and Trends in Child Malnutrition: Key Findings of the 2019 Edition of the Joint Child Malnutrition Estimates; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- Black, R.E.; Victora, C.G.; Walker, S.P.; Bhutta, Z.A.; Christian, P.; de Onis, M.; Ezzati, M.; Grantham-McGregor, S.; Katz, J.; Martorell, R.; et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013, 382, 427–451. [Google Scholar] [CrossRef]
- Bhutta, Z.A.; Das, J.K.; Rizvi, A.; Gaffey, M.F.; Walker, N.; Horton, S.; Webb, P.; Lartey, A.; Black, R.E.; The Lancet Nutrition Interventions Review Group; et al. Evidence-based interventions for improvement of maternal and child nutrition: What can be done and at what cost? Lancet 2013, 382, 452–477. [Google Scholar] [CrossRef]
- Ruel, M.T.; Alderman, H.; Maternal and Child Nutrition Study Group. Nutrition-sensitive interventions and programmes: How can they help to accelerate progress in improving maternal and child nutrition? Lancet 2013, 382, 536–551. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Guideline: Updates on the Management of Severe Acute Malnutrition in Infants and Children; World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- Picot, J.; Hartwell, D.; Harris, P.; Mendes, D.; Clegg, A.J.; Takeda, A. The Effectiveness of Interventions to Treat Severe Acute Malnutrition in Young Children: A Systematic Review; Health Technology Assessment: Winchester, UK, 2012; Volume 16, p. 1. [Google Scholar]
- Lenters, L.M.; Wazny, K.; Webb, P.; Ahmed, T.; Bhutta, Z.A. Treatment of Severe and Moderate Acute Malnutrition in Low-and Middle-Income Settings: A Systematic Review, Meta-Analysis and Delphi Process. BMC Public Health 2013, 13, S23. [Google Scholar] [CrossRef]
- Alcoba, G.; Kerac, M.; Breysse, S.; Salpeteur, C.; Galetto-Lacour, A.; Briend, A.; Gervaix, A. Do children with uncomplicated severe acute malnutrition need antibiotics? A systematic review and meta-analysis. PLoS ONE 2013, 8, e53184. [Google Scholar] [CrossRef]
- Gera, T. Efficacy and safety of therapeutic nutrition products for home based therapeutic nutrition for severe acute malnutrition: A systematic review. Indian Pediatr. 2010, 47, 709–718. [Google Scholar] [CrossRef]
- Lazzerini, M.; Tickell, D. Antibiotics in severely malnourished children: Systematic review of efficacy, safety and pharmacokinetics. Bull. World Health Organ. 2011, 89, 593–606. [Google Scholar] [CrossRef]
- Schoonees, A.; Lombard, M.J.; Musekiwa, A.; Nel, E.; Volmink, J. Ready-to-use therapeutic food (RUTF) for home-based nutritional rehabilitation of severe acute malnutrition in children from six months to five years of age. Cochrane Database Syst. Rev. 2019, 5, CD009000. [Google Scholar] [CrossRef]
- Kristjansson, E.; Francis, D.K.; Liberato, S.; Benkhalti Jandu, M.; Welch, V.; Batal, M.; Greenhalgh, T.; Rader, T.; Noonan, E.; Shea, B.; et al. Food supplementation for improving the physical and psychosocial health of socio-economically disadvantaged children aged three months to five years. Cochrane Database Syst. Rev. 2015, CD009924. [Google Scholar] [CrossRef]
- Visser, J.; McLachlan, M.H.; Fergusson, P.; Volmink, J.; Garner, P. Supplementary feeding for food insecure, vulnerable and malnourished populations-an overview of systematic reviews. Cochrane Database Syst. Rev. 2013, 6. [Google Scholar] [CrossRef]
- Manary, M.; Iannotti, L.; Trehan, I. Systematic Review of Vitamin A Supplementation in the Treatment of Children with Severe Acute Malnutrition; World Health Organization: Geneva, Switzerland, 2012. [Google Scholar]
- Review Manager; The Nordic Cochrane Centre, The Cochrane Collaboration: Copenhagen, Denmark, 2014.
- Higgins, J.P.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions; John Wiley & Sons: New York, NY, USA, 2011; Volume 4. [Google Scholar]
- EPOC. Resources for Review Authors 2017. Available online: Epoc.cochrane.org/resources/epoc-resources-review-authors (accessed on 5 December 2019).
- Guyatt, G.H.; Oxman, A.D.; Vist, G.E.; Kunz, R.; Falck-Ytter, Y.; Alonso-Coello, P.; Schunemann, H.J.; Group, G.W. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008, 336, 924–926. [Google Scholar] [CrossRef]
- Balshem, H.; Helfand, M.; Schunemann, H.J.; Oxman, A.D.; Kunz, R.; Brozek, J.; Vist, G.E.; Falck-Ytter, Y.; Meerpohl, J.; Norris, S.; et al. GRADE guidelines: 3. Rating the quality of evidence. J. Clin. Epidemiol. 2011, 64, 401–406. [Google Scholar] [CrossRef] [PubMed]
- Ackatia-Armah, R.S.; McDonald, C.M.; Doumbia, S.; Erhardt, J.G.; Hamer, D.H.; Brown, K.H. Malian children with moderate acute malnutrition who are treated with lipid-based dietary supplements have greater weight gains and recovery rates than those treated with locally produced cereal-legume products: A community-based, cluster-randomized trial. Am. J. Clin. Nutr. 2015, 101, 632–645. [Google Scholar] [CrossRef] [PubMed]
- Ashworth, A.; Huttly, S.; Khanum, S. Controlled trial of three approaches to the treatment of severe malnutrition. Lancet 1994, 344, 1728–1732. [Google Scholar] [CrossRef]
- Bahwere, P.; Akomo, P.; Mwale, M.; Murakami, H.; Banda, C.; Kathumba, S.; Banda, C.; Jere, S.; Sadler, K.; Collins, S. Soya, maize, and sorghum–based ready-to-use therapeutic food with amino acid is as efficacious as the standard milk and peanut paste–based formulation for the treatment of severe acute malnutrition in children: A noninferiority individually randomized controlled efficacy clinical trial in Malawi. Am. J. Clin. Nutr. 2017, 106, 1100–1112. [Google Scholar] [PubMed]
- Bahwere, P.; Balaluka, B.; Wells, J.C.K.; Mbiribindi, C.N.; Sadler, K.; Akomo, P.; Dramaix-Wilmet, M.; Collins, S. Cereals and pulse-based ready-to-use therapeutic food as an alternative to the standard milk-and peanut paste–based formulation for treating severe acute malnutrition: A noninferiority, individually randomized controlled efficacy clinical trial. Am. J. Clin. Nutr. 2016, 103, 1145–1161. [Google Scholar] [CrossRef]
- Bahwere, P.; Banda, T.; Sadler, K.; Nyirenda, G.; Owino, V.; Shaba, B.; Dibari, F.; Collins, S. Effectiveness of milk whey protein-based ready-to-use therapeutic food in treatment of severe acute malnutrition in M alawian under-5 children: A randomised, double-blind, controlled non-inferiority clinical trial. Matern. Child Nutr. 2014, 10, 436–451. [Google Scholar] [CrossRef]
- Berkley, J.A.; Ngari, M.; Thitiri, J.; Mwalekwa, L.; Timbwa, M.; Hamid, F.; Ali, R.; Shangala, J.; Mturi, N.; Jones, K.D.; et al. Daily co-trimoxazole prophylaxis to prevent mortality in children with complicated severe acute malnutrition: A multicentre, double-blind, randomised placebo-controlled trial. Lancet Glob. Health 2016, 4, e464–e473. [Google Scholar] [CrossRef]
- Bhandari, N.; Mohan, S.B.; Bose, A.; Iyengar, S.D.; Taneja, S.; Mazumder, S.; Pricilla, R.A.; Iyengar, K.; Sachdev, H.S.; Mohan, V.R.; et al. Efficacy of three feeding regimens for home-based management of children with uncomplicated severe acute malnutrition: A randomised trial in India. BMJ Glob. Health 2016, 1, e000144. [Google Scholar] [CrossRef]
- Chapko, M.K.; Prual, A.; Gamatie, Y.; Maazou, A.A. Randomized clinical trial comparing hospital to ambulatory rehabilitation of malnourished children in Niger. J. Trop. Pediatr. 1994, 40, 225–230. [Google Scholar] [CrossRef]
- Ciliberto, M.A.; Sandige, H.; Ndekha, M.J.; Ashorn, P.; Briend, A.; Ciliberto, H.M.; Manary, M.J. Comparison of home-based therapy with ready-to-use therapeutic food with standard therapy in the treatment of malnourished Malawian children: A controlled, clinical effectiveness trial. Am. J. Clin. Nutr. 2005, 81, 864–870. [Google Scholar] [CrossRef] [PubMed]
- Diop, E.H.I.; Dossou, N.I.; Ndour, M.M.; Briend, A.; Wade, S. Comparison of the efficacy of a solid ready-to-use food and a liquid, milk-based diet for the rehabilitation of severely malnourished children: A randomized trial. Am. J. Clin. Nutr. 2003, 78, 302–307. [Google Scholar] [CrossRef] [PubMed]
- Donnen, P.; Dramaix, M.; Brasseur, D.; Bitwe, R.; Vertongen, F.; Hennart, P. Randomized placebo-controlled clinical trial of the effect of a single high dose or daily low doses of vitamin A on the morbidity of hospitalized, malnourished children. Am. J. Clin. Nutr. 1998, 68, 1254–1260. [Google Scholar] [CrossRef] [PubMed]
- Fabiansen, C.; Yameogo, C.W.; Iuel-Brockdorf, A.S.; Cichon, B.; Rytter, M.J.H.; Kurpad, A.; Wells, J.C.; Ritz, C.; Ashorn, P.; Filteau, S.; et al. Effectiveness of food supplements in increasing fat-free tissue accretion in children with moderate acute malnutrition: A randomised 2 × 2 × 3 factorial trial in Burkina Faso. PLoS Med. 2017, 14, e1002387. [Google Scholar] [CrossRef] [PubMed]
- Hossain, M.M.; Hassan, M.Q.; Rahman, M.H.; Kabir, A.R.; Hannan, A.H.; Rahman, A.K. Hospital management of severely malnourished children: Comparison of locally adapted protocol with WHO protocol. Indian Pediatr. 2009, 46, 213–217. [Google Scholar] [PubMed]
- Hsieh, J.-C.; Liu, L.; Zeilani, M.; Ickes, S.; Trehan, I.; Maleta, K.; Craig, C.; Thakwalakwa, C.; Singh, L.; Brenna, J.T. High oleic ready-to-use therapeutic food maintains docosahexaenoic acid status in severe malnutrition: A randomized, blinded trial. J. Pediatr. Gastroenterol. Nutr. 2015, 61, 138. [Google Scholar] [CrossRef]
- Irena, A.H.; Bahwere, P.; Owino, V.O.; Diop, E.I.; Bachmann, M.O.; Mbwili-Muleya, C.; Dibari, F.; Sadler, K.; Collins, S. Comparison of the effectiveness of a milk-free soy-maize-sorghum-based ready-to-use therapeutic food to standard ready-to-use therapeutic food with 25% milk in nutrition management of severely acutely malnourished Z ambian children: An equivalence non-blinded cluster randomised controlled trial. Matern. Child Nutr. 2015, 11, 105–119. [Google Scholar]
- Isanaka, S.; Langendorf, C.; Berthe, F.; Gnegne, S.; Li, N.; Ousmane, N.; Harouna, S.; Hassane, H.; Schaefer, M.; Adehossi, E.; et al. Routine amoxicillin for uncomplicated severe acute malnutrition in children. N. Engl. J. Med. 2016, 374, 444–453. [Google Scholar] [CrossRef]
- Jones, K.D.J.; Ali, R.; Khasira, M.A.; Odera, D.; West, A.L.; Koster, G.; Akomo, P.; Talbert, A.W.A.; Goss, V.M.; Ngari, M.; et al. Ready-to-use therapeutic food with elevated n-3 polyunsaturated fatty acid content, with or without fish oil, to treat severe acute malnutrition: A randomized controlled trial. BMC Med. 2015, 13, 93. [Google Scholar] [CrossRef]
- Karakochuk, C.; van den Briel, T.; Stephens, D.; Zlotkin, S. Treatment of moderate acute malnutrition with ready-to-use supplementary food results in higher overall recovery rates compared with a corn-soya blend in children in southern Ethiopia: An operations research trial. Am. J. Clin. Nutr. 2012, 96, 911–916. [Google Scholar] [CrossRef]
- LaGrone, L.N.; Trehan, I.; Meuli, G.J.; Wang, R.J.; Thakwalakwa, C.; Maleta, K.; Manary, M.J. A novel fortified blended flour, corn-soy blend ‘plus-plus,’is not inferior to lipid-based ready-to-use supplementary foods for the treatment of moderate acute malnutrition in Malawian children. Am. J. Clin. Nutr. 2011, 95, 212–219. [Google Scholar] [CrossRef] [PubMed]
- Manary, M.J.; Ndkeha, M.J.; Ashorn, P.; Maleta, K.; Briend, A. Home based therapy for severe malnutrition with ready-to-use food. Arch. Dis. Child. 2004, 89, 557–561. [Google Scholar] [CrossRef] [PubMed]
- Matilsky, D.K.; Maleta, K.; Castleman, T.; Manary, M.J. Supplementary feeding with fortified spreads results in higher recovery rates than with a corn/soy blend in moderately wasted children. J. Nutr. 2009, 139, 773–778. [Google Scholar] [CrossRef] [PubMed]
- Maust, A.; Koroma, A.S.; Abla, C.; Molokwu, N.; Ryan, K.N.; Singh, L.; Manary, M.J. Severe and moderate acute malnutrition can be successfully managed with an integrated protocol in Sierra Leone. J. Nutr. 2015, 145, 2604–2609. [Google Scholar] [CrossRef] [PubMed]
- Medoua, G.N.; Ntsama, P.M.; Ndzana, A.C.; Essa’a, V.J.; Tsafack, J.J.; Dimodi, H.T. Recovery rate of children with moderate acute malnutrition treated with ready-to-use supplementary food (RUSF) or improved corn–soya blend (CSB+): A randomized controlled trial. Public Health Nutr. 2016, 19, 363–370. [Google Scholar] [CrossRef] [PubMed]
- Nackers, F.; Broillet, F.; Oumarou, D.; Djibo, A.; Gaboulaud, V.; Guerin, P.J.; Rusch, B.; Grais, R.F.; Captier, V. Effectiveness of ready-to-use therapeutic food compared to a corn/soy-blend-based pre-mix for the treatment of childhood moderate acute malnutrition in Niger. J. Trop. Pediatr. 2010, 56, 407–413. [Google Scholar] [CrossRef]
- Nikiema, L.; Huybregts, L.; Kolsteren, P.; Lanou, H.; Tiendrebeogo, S.; Bouckaert, K.; Kouanda, S.; Sondo, B.; Roberfroid, D. Treating moderate acute malnutrition in first-line health services: An effectiveness cluster-randomized trial in Burkina Faso. Am. J. Clin. Nutr. 2014, 100, 241–249. [Google Scholar] [CrossRef]
- Oakley, E.; Reinking, J.; Sandige, H.; Trehan, I.; Kennedy, G.; Maleta, K.; Manary, M. A ready-to-use therapeutic food containing 10% milk is less effective than one with 25% milk in the treatment of severely malnourished children. J. Nutr. 2010, 140, 2248–2252. [Google Scholar] [CrossRef]
- Phuka, J.; Thakwalakwa, C.; Maleta, K.; Cheung, Y.B.; Briend, A.; Manary, M.; Ashorn, P. Supplementary feeding with fortified spread among moderately underweight 6–18-month-old rural Malawian children. Matern. Child Nutr. 2009, 5, 159–170. [Google Scholar] [CrossRef]
- Puett, C.; Sadler, K.; Alderman, H.; Coates, J.; Fiedler, J.L.; Myatt, M. Cost-effectiveness of the community-based management of severe acute malnutrition by community health workers in southern Bangladesh. Health Policy Plan. 2012, 28, 386–399. [Google Scholar] [CrossRef]
- Sandige, H.; Ndekha, M.J.; Briend, A.; Ashorn, P.; Manary, M.J. Home-based treatment of malnourished Malawian children with locally produced or imported ready-to-use food. J. Pediatr. Gastroenterol. Nutr. 2004, 39, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Sattar, S.; Ahmed, T.; Rasul, C.H.; Saha, D.; Salam, M.A.; Hossain, M.I. Efficacy of a high-dose in addition to daily low-dose vitamin A in children suffering from severe acute malnutrition with other illnesses. PLoS ONE 2012, 7, e33112. [Google Scholar] [CrossRef] [PubMed]
- Scherbaum, V.; Purwestri, R.C.; Stuetz, W.; Inayati, D.A.; Suryantan, J.; Bloem, M.A.; Biesalski, H.K. Locally produced cereal/nut/legume-based biscuits versus peanut/milk-based spread for treatment of moderately to mildly wasted children in daily programmes on Nias Island, Indonesia: An issue of acceptance and compliance? Asia Pac. J. Clin. Nutr. 2015, 24, 152. [Google Scholar] [PubMed]
- Shewade, H.D.; Patro, B.K.; Bharti, B.; Soundappan, K.; Kaur, A.; Taneja, N. Effectiveness of indigenous ready-to-use therapeutic food in community-based management of uncomplicated severe acute malnutrition: A randomized controlled trial from India. J. Trop. Pediatr. 2013, 59, 393–398. [Google Scholar] [CrossRef] [PubMed]
- Sigh, S.; Roos, N.; Chamnan, C.; Laillou, A.; Prak, S.; Wieringa, F.T. Effectiveness of a locally produced, fish-based food product on weight gain among Cambodian children in the treatment of acute malnutrition: A randomized controlled trial. Nutrients 2018, 10, 909. [Google Scholar] [CrossRef]
- Singh, A.S.; Kang, G.; Ramachandran, A.; Sarkar, R.; Peter, P.; Bose, A. Locally made ready-to-use therapeutic food for treatment of malnutrition: A randomized controlled trial. Indian Pediatr. 2010, 47, 679–686. [Google Scholar] [CrossRef]
- Sm, M.; Rai, P.; Swain, A.S.B. Locally prepared ready to use therapeutic food for the treatment of children with severe acute malnutrition: A randomised controlled trial. World J. Pharm. Med. Res. 2019, 5, 159–164. [Google Scholar]
- Stobaugh, H.C.; Ryan, K.N.; Kennedy, J.A.; Grise, J.B.; Crocker, A.H.; Thakwalakwa, C.; Litkowski, P.E.; Maleta, K.M.; Manary, M.J.; Trehan, I. Including whey protein and whey permeate in ready-to-use supplementary food improves recovery rates in children with moderate acute malnutrition: A randomized, double-blind clinical trial. Am. J. Clin. Nutr. 2016, 103, 926–933. [Google Scholar] [CrossRef]
- Thakur, G.S.; Singh, H.; Patel, C. Locally-prepared ready-to-use therapeutic food for children with severe acute malnutrition: A controlled trial. Indian Pediatr. 2013, 50, 295–299. [Google Scholar] [CrossRef]
- Thakwalakwa, C.; Ashorn, P.; Phuka, J.; Cheung, Y.B.; Briend, A.; Puumalainen, T.; Maleta, K. A lipid-based nutrient supplement but not corn-soy blend modestly increases weight gain among 6-to 18-month-old moderately underweight children in rural Malawi. J. Nutr. 2010, 140, 2008–2013. [Google Scholar] [CrossRef][Green Version]
- Vanelli, M.; Virdis, R.; Contini, S.; Corradi, M.; Cremonini, G.; Marchesi, M.; Mele, A.; Monti, F.; Pagano, B.; Proietti, I.; et al. A hand-made supplementary food for malnourished children. Acta Bio Med. Atenei Parm. 2014, 85, 236–242. [Google Scholar]
- Versloot, C.J.; Voskuijl, W.; van Vliet, S.J.; van den Heuvel, M.; Carter, J.C.; Phiri, A.; Kerac, M.; Heikens, G.T.; van Rheenen, P.F.; Bandsma, R.H.J. Effectiveness of three commonly used transition phase diets in the inpatient management of children with severe acute malnutrition: A pilot randomized controlled trial in Malawi. BMC Pediatr. 2017, 17, 112. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wilford, R.; Golden, K.; Walker, D.G. Cost-effectiveness of community-based management of acute malnutrition in Malawi. Health Policy Plan. 2011, 27, 127–137. [Google Scholar] [CrossRef] [PubMed]
- Trehan, I.; Goldbach, H.S.; LaGrone, L.N.; Meuli, G.J.; Wang, R.J.; Maleta, K.M.; Manary, M.J. Research Article (New England Journal of Medicine) Antibiotics as part of the management of severe acute malnutrition. Malawi Med. J. 2016, 28, 123–130. [Google Scholar] [PubMed]
- Roberfroid, D.; Hammami, N.; Mehta, P.; Lachat, C.; Verstraeten, R.; Weise Prinzo, Z.; Huybregts, L.; Kolsteren, P. Management of Oedematous Malnutrition in Infants and Children Aged> 6 Months: A Systematic Review of the Evidence; WHO: Geneva, Switzerland, 2013. [Google Scholar]
- Williams, P.C.; Berkley, J.A. Guidelines for the treatment of severe acute malnutrition: A systematic review of the evidence for antimicrobial therapy. Paediatr. Int. Child Health 2018, 38, S32–S49. [Google Scholar] [CrossRef] [PubMed]
- Agha, S. Supplementary Feeding of Malnourished Children in Northern Iraq. East Mediterr Health J. 2004, 10, 12. [Google Scholar]
- Aguayo, V.M.; Badgaiyan, N.; Qadir, S.S.; Bugti, A.N.; Alam, M.M.; Nishtar, N.; Galvin, M. Community management of acute malnutrition (CMAM) programme in Pakistan effectively treats children with uncomplicated severe wasting. Matern. Child Nutr. 2018, 14, e12623. [Google Scholar] [CrossRef]
- Ahmed, T.; Ali, M.; Choudhary, I.A.; Haque, M.E.; Salam, M.A.; Rabbani, G.H.; Suskind, R.M.; Fuchs, G.J. Mortality in severely malnourished children with diarrhoea and use of a standardised management protocol. Lancet 1999, 353, 1919–1922. [Google Scholar] [CrossRef]
- Ashworth, A.; Chopra, M.; McCoy, D.; Sanders, D.; Jackson, D.; Karaolis, N.; Sogaula, N.; Schofield, C. WHO guidelines for management of severe malnutrition in rural South African hospitals: Effect on case fatality and the influence of operational factors. Lancet 2004, 363, 1110–1115. [Google Scholar] [CrossRef]
- Bachou, H.; Tumwine, J.K.; Mwadime, R.K.; Ahmed, T.; Tylleskar, T. Reduction of unnecessary transfusion and intravenous fluids in severely malnourished children is not enough to reduce mortality. Ann. Trop. Paediatr. 2008, 28, 23–33. [Google Scholar] [CrossRef][Green Version]
- Badaloo, A.; Boyne, M.; Reid, M.; Persaud, C.; Forrester, T.; Millward, D.J.; Jackson, A.A. Dietary protein, growth and urea kinetics in severely malnourished children and during recovery. J. Nutr. 1999, 129, 969–979. [Google Scholar] [CrossRef] [PubMed]
- Baker, R.; Baker, S.; Margo, G.; Reuter, H. Successful use of a soya-maize mixture in the treatment of kwashiorkor. S. Afr. Med. J. 1978, 53, 674–677. [Google Scholar] [PubMed]
- Bhandari, N.; Bahl, R.; Nayyar, B.; Khokhar, P.; Rohde, J.E.; Bhan, M.K. Food supplementation with encouragement to feed it to infants from 4 to 12 months of age has a small impact on weight gain. J. Nutr. 2001, 131, 1946–1951. [Google Scholar] [CrossRef] [PubMed]
- Burza, S.; Mahajan, R.; Marino, E.; Sunyoto, T.; Shandilya, C.; Tabrez, M.; Kumar, K.; Jha, A.; Mathew, P.; Salse, N.; et al. Seasonal effect and long-term nutritional status following exit from a community-based management of severe acute malnutrition program in Bihar, India. Eur. J. Clin. Nutr. 2016, 70, 437. [Google Scholar] [CrossRef] [PubMed]
- Donnen, P.; Sylla, A.; Dramaix, M.; Sall, G.; Kuakuvi, N.; Hennart, P. Effect of daily low dose of vitamin A compared with single high dose on morbidity and mortality of hospitalized mainly malnourished children in senegal: A randomized controlled clinical trial. Eur. J. Clin. Nutr. 2007, 61, 1393. [Google Scholar] [CrossRef] [PubMed]
- Dubray, C.; Ibrahim, S.A.; Abdelmutalib, M.; Guerin, P.J.; Dantoine, F.; Belanger, F.; Legros, D.; Pinoges, L.; Brown, V. Treatment of severe malnutrition with 2-day intramuscular ceftriaxone vs 5-day amoxicillin. Ann. Trop. Paediatr. 2008, 28, 13–22. [Google Scholar] [CrossRef]
- avan, R.; Kooshki, A.; Afzalaghaee, M.; Aldaghi, M.; Yousefi, M. Effectiveness of supplementary blended flour based on chickpea and cereals for the treatment of infants with moderate acute malnutrition in Iran: A randomized clinical trial. Electron. Phys. 2017, 9, 6078. [Google Scholar]
- Linneman, Z.; Matilsky, D.; Ndekha, M.; Manary, M.J.; Maleta, K.; Manary, M.J. A large-scale operational study of home-based therapy with ready-to-use therapeutic food in childhood malnutrition in Malawi. Matern. Child Nutr. 2007, 3, 206–215. [Google Scholar] [CrossRef]
- Nagar, R.P.; Nagar, T.; Gupta, B.D. Treatment outcome in patients with severe acute malnutrition managed with protocolised care at malnutrition treatment corner in Rajasthan, India: A prospective observational study (quasi-experimental). Int. J. Res. Med. Sci. 2016, 4, 238–245. [Google Scholar] [CrossRef]
- Roy, S.K.; Fuchs, G.J.; Mahmud, Z.; Ara, G.; Islam, S.; Shafique, S.; Akter, S.S.; Chakraborty, B. Intensive nutrition education with or without supplementary feeding improves the nutritional status of moderately-malnourished children in Bangladesh. J. Health Popul. Nutr. 2005, 23, 320–330. [Google Scholar]
- Simpore, J.; Kabore, F.; Zongo, F.; Dansou, D.; Bere, A.; Pignatelli, S.; Biondi, D.M.; Ruberto, G.; Musumeci, S. Nutrition rehabilitation of undernourished children utilizing Spiruline and Misola. Nutr. J. 2006, 5, 3. [Google Scholar] [CrossRef]
- Zongo, U.; Zoungrana, S.L.; Savadogo, A.; Traoré, A.S. Nutritional and clinical rehabilitation of severely malnourished children with Moringa oleifera Lam. leaf powder in Ouagadougou (Burkina Faso). Food Nutr. Sci. 2013, 4, 991. [Google Scholar] [CrossRef]

| Study | Study Design | Setting | Participants | Intervention/Control | Outcomes |
|---|---|---|---|---|---|
| Comparison 1: Community-based strategies to screen, identify, and manage SAM and MAM compared to standard care | |||||
| Maust 2015 | cRCT | Study carried out in 10 centers in Sierra Leone treating global acute malnutrition in children | 1957 children aged 6–59 months | Group 1: Integrated (N = 1100) Children with SAM were given RUTF (175 kcal/kg/day) and amoxicillin every 2 weeks for 12 weeks. Children with MAM were given RUTF (75 kcal/kg/day) every 2 weeks for 12 weeks. Group 2: Standard (N = 857) Children with SAM were given RUTF (200 kcal/kg/day) and amoxicillin every 2 weeks for 12 weeks. Children with MAM were given super cereal plus (a fortified flour of CSB with oil and milk powder (1250 kcal/day)) every 2 weeks for 12 weeks | Coverage and recovery rate, duration of treatment, rates of weight and MUAC gain, clinical status. and cost of foodstuffs used |
| Wilford 2012 | Cost-effectiveness study | District Dowa, Central Malawi | - | The study assessed the cost-effectiveness of community-based management of acute malnutrition (CMAM) to prevent deaths due to SAM | Costs and cost-effectiveness |
| Comparison 2: Facility-based strategies to screen and manage uncomplicated SAM according to the WHO protocol compared to other standards of care | |||||
| Ashworth 1994 | RCT | The Children’s Nutrition Unit in central Dhaka, Bangladesh | 573 children aged 12–60 months | Group 1: Inpatient: (N = 200) Children were admitted with their mothers and were resident until they reached 80% weight/height Group 2: Daycare (N = 200) Children came with their mothers from 0800 to 1700 every day except Friday, until 80% weight/height was reached Group 3: Care at home (N = 173) Children were treated in the daycare facility for 7 days (or up to 9 days if poor appetite or poor clinical outcome) | Cost-effectiveness, mortality, rate of edema loss, weight gain, and days taken to achieve 80% edema-free weight/height |
| Chapko 1994 | RCT | Niger’s National Hospital, Niamey, Niger | 100 malnourished children | Group 1 (N = 53) Hospital-based rehabilitation Group 2 (N = 47) Ambulatory-based rehabilitation | Cost of care, mortality, and anthropometric measures |
| Hossain 2008 | Quasi-experimental | Urban setting in Dhaka, Bangladesh | 60 children aged 2–59 months | Group 1 (N = 30) Children were managed as per the WHO protocol Group 2 (N = 30) Children were managed as per the Institute of Child and Mother Health (ICMH) protocol | Clinical determinants, improved appetite, disappearance of edema, improvement of other associated medical conditions. Catch-up growth |
| Puett 2013 | Cost-effectiveness study | Rural setting in Bhola district, Bangladesh | - | The cost-effectiveness of community-based management for severe acute malnutrition (SAM) was compared with the “standard of care” for SAM (i.e., inpatient treatment), augmented with community surveillance by CHWs to detect cases in a neighboring area | Cost-effectiveness |
| Comparison 3: Facility-based strategies to screen and manage uncomplicated SAM according to the WHO protocol compared to other standards of care (inpatient treatment with RUTF compared to F100) | |||||
| Mishra 2018 | RCT | Pediatrics ward of SCB Medical College, Cuttack, India | 120 children aged 6–60 months | Group 1: Locally prepared ready-to-use therapeutic food (N = 60) Group 2: F100 (N = 60) | Weight gain, recovery rate and length of stay, anthropometric determinants (weight, height, MUAC), clinical determinants (wasting, edema, death) |
| Thakur 2013 | Quasi-experimental | Urban setting in Maharashtra, India | 98 children ages 6–60 months | Group 1: L-RUTF (N = 50) Groundnut, milk powder, vegetable oil was given as 4 meals/day (12 g/kg/day), along with 4 meals from family pot Group 2: F100-L (N = 54) F100 locally produced was given as 60 mL/kg/day in 4 quarters + 4 meals from family food (total 120 kcal/kg/day). | Weight gain, duration of hospital stay |
| Versloot 2017 | RCT | Blantyre, Malawi | 74 children aged 6–60 months | Group 1: RUTF-F75 (N = 26) Low protein milk-based formula diet given daily for 7 days (135 kcal/kg/day) Group 2: F100 (N = 25) F100 milk diet given daily for 7 days (135 kcal/kg/day) Group 3: RUTF (N = 23) RUTF given daily for 7 days (135 kcal/kg/day) | Fecal pH, duration of stay, days with diarrhea, duration of edema, weight at discharge, hypo- and hypernatremia, reversion to F75 diet, and mortality |
| Comparison 4: Community-based management of children with uncomplicated SAM as outpatients with RUTF compared to standard diet, fortified blended flours (FBFs) or other locally produced foods | |||||
| Bahwere 2014 | RCT | Lilong Health District, Central Malawi | 600 children aged 6–59 months of age | Group 1 (N = 308) Whey protein concentrate 34% (replacing dried skimmed milk (DSM)) was given weekly. One-week ratio N = 175 kcal/kg Group 2 (N = 292) Peanut-based RUTF (P-RUTF) was given weekly | Average weight gain and recovery rate, length of stay (LOS) |
| Bahwere 2016 | RCT | Study was carried out in a rural setting in Kabare administrative zone of South Kivu province, Democratic Republic of Congo | 886 children; 6–23 months (N = 414), 24–59 months (N = 472) | Group 1 (N = 445) Soya–maize–sorghum RUTF Group 2 (N = 441) Standard peanut-paste-based RUTF | Recovery rate; mean daily weight gain; mean length of stay; hemoglobin change; differences in fat mass, body fat percentage, and fat mass index; fat-free mass and fat-free mass index; bio-electrical impedance analysis; illness marker and plasma concentrations of 8 key amino acids |
| Bahwere 2017 | RCT | Study was carried out in 3 districts: Lilongwe, Dedza, Mchinji of Malawi; 21 clusters in each district | 1347 children; N = 823 (6–23 months), N = 524 (24–59 months) | Group 1: Peanut butter RUTF (N = 454) Peanut butter, milk powder, sugar, vegetable oil, vit/min was given daily (0800 to 1600) until discharged or weight was gained Group 2: Amino-acid enriched milk-free, soya, maize, sorghum (N = 458) Amino-acid enriched milk-free soya, maize, sorghum was given daily (0800–1600 h) until discharged or weight was gained Group 3: Amino acid enriched low cow milk (N = 435) Amino acid enriched low-fat cow’s milk (9.3%), soya, maize, sorghum given daily (0800–1600 h) until discharged or weight was gained | Recovery rate, mean length of stay, mean daily weight gain, hemoglobin levels, body iron stores, RUTF intake, and morbidity |
| Bhandari 2016 | RCT | Study was carried out in a mixed setting of Rajasthan, Delhi, and Tamil Nadu areas of India | 906 children aged 6–59 months | Group 1: RUTF (Commercial) (N = 298) Commercial peanut paste, sugar, milk solids, vegetable oil, min/vit mix given weekly for 16 weeks Group 2: RUTF (Local) (N = 307) Local peanut paste, sugar, milk solids, vegetable oil, min/vit mix given weekly for 16 weeks Control: Energy dense home prepared food (N = 301) Cereals, pulses, sugar, oil, milk, eggs, min/vit mix given weekly for 16 weeks | Recovery weight gain, time to recovery, prevalence of diarrhea, acute lower respiratory tract infection (ALRI) and fever, mortality, and hospitalizations |
| Ciliberto 2005 | Quasi-experimental | Study was carried out in a rural setting in South Malawi | 1178 children aged 10–60 months | Group 1 (N = 992) Home-based therapy with RUTF (HBT-RUTF) Group 2 (N = 186) F100 standard inpatient therapy | Case fatality rate, successful recovery, relapse or death, rates of growth in body weight, MUAC, and length. Number of days of fever, cough, and diarrhea |
| Diop 2003 | RCT | Urban setting in Rebuss, Dakar, Senegal | 70 children aged 6–36 months | Group 1: RUTF (N = 35) Peanut-butter-based (Nutriset) given 3 times/day until discharged Control: F100 (N = 35) Skim milk-based (Nutriset) given 3 times/day until discharged | Weight gain, food intake |
| Hseih 2015 | RCT | Rural setting in Katana health district, South Kivu, Democratic Republic of Congo | 141 children aged 6–59 months | Group 1: High oleic RUTF: (N = 71) High oleic peanuts, palm oil, and linseed oil given every 2 weeks for 12 weeks Group 2: RUTF (N = 70) Peanuts, palm oil, soy oil given every 2 week for 12 weeks | Change in plasma DHA and EPA content, rates of recovery length and weight gain, and change in plasma content of arachidonic acid |
| Irena 2015 | cRCT | Health care clinics run by the Lusaka District Health Management Team in Lusaka, Zambia | 1927 children aged 6–59 months | Group 1: Standard RUTF (N = 1103) Standard peanut-based RUTF given daily until discharged Group 2: Soybean, maize, and sorghum RUTF (N = 824) Soybean, maize, and sorghum grains given weekly until discharged | Recovery (cure), death, default, transfer out of the catchment area, and non-recovery |
| Jones 2015 | RCT | Rural setting in Kilifi county, Kenya | 60 children aged 6–50 months | Group 1: Standard peanut-based RUTF (N = 21) Group 2: Flax seed oil-containing RUTF (N = 20) Flax seed oil-based RUTF given weekly, except oil was given for 2 weeks only, followed by RUTF alone Group 3: Flax seed oil-containing RUTF with additional fish oil capsules (N = 20) Given weekly | Erythrocyte n-3 PUFA content, safety, and acceptability of the intervention; recovery and growth |
| Manary 2004 | Quasi-experimental | Nutrition unit in Blantyre, Malawi | 282 children aged 12–59 months | Group 1: RTUF plus supplement (N = 96) High energy diet + supplement Group 2: Maize-Soy (N = 117) Group 3: RTUF (N = 69) High Energy diet | Recovery rate, dropout, mortality, relapse, weight gain, height gain, MUAC gain |
| Oakley 2010 | RCT | Rural setting in southern region of Malawi | 1874 children aged 6–59 months | Group 1: RUTF-10% (N = 929) Skimmed milk (10%), whole soy flour (15%), peanut paste, min/vit mix was provided every 2 weeks for 8 weeks Group 2: RUTF-25% (N = 945) Skim milk (25%), peanut paste, min/vit mix was given weekly for 8 weeks | Recovery, rate of weight gain, and height gain |
| Sandige 2004 | Quasi-experimental | Blantyre, Malawi | 182 children aged 1–5 years | Group 1: Local RUTF (N = 99) Local RUTF composed of full fat milk powder, icing sugar, cotton seed oil, peanut butter and a mineral/vitamin mixture was given every 2 weeks for 16 weeks or until target weight was achieved Group 2: Imported RUTF (N = 83) Imported Plumpy’Nut (Nutriset) was given every 2 weeks for 16 weeks or until target weight was achieved | Recovery, weight gain, statural growth, growth in MUAC, anthropometric status, and the prevalence of fever, cough, and diarrhea |
| Shewade 2013 | RCT | Urban setting in Chandigarh, India | 26 children aged 6 months to 5 years | Intervention group: (N = 13) RUTF Groundnut-based diet prepared by program staff was provided on weekly basis for 12 weeks. Diet supplied 200 kcal/kg/d Control group: (N = 13) Supplementary nutrition from the anganwadi as per guidelines for management for malnutrition under the Integrated Child Development Scheme (ICDS) | Weight gain, WHZ, HAZ, WAZ, consumption |
| Sigh 2018 | RCT | National Pediatric Hospital in Phnom Penh, Cambodia | 121 children aged 6–59 months | Group 1: NumTrey fish-based RUTF: (N = 60) Two week rations of fish-based RUTF wafers (160 and 180 kcal/kg) based on weight were provided at each follow-up visit Group 2: Milk based RUTF (BP100) (N = 61) Two week rations of a standard product BP-100™ (160 and 180 kcal/kg) | Weight gain, height, MUAC, WHZ, WAZ, and HAZ |
| Comparison 5: RUSF for MAM compared to standard diet, FBF, or other locally produced foods | |||||
| Ackatia-Armah 2015 | cRCT | Twelve community health centers in rural setting in Diola health district, Bamako, Mali | 1264 children aged 6–35 months | Group 1: Ready-to-use supplementary food (RUSF) (N = 344) Group 2: Corn soy blend (CSB++) (N = 349) Group 3: Misoloa (MI) (N = 307) Group 4: Locally milled flours + micronutrient powder (LMF) (N = 284) | Adherence to treatment, MUAC, body weight and length, WHZ, HAZ, anemia, iron deficiency, iron deficiency anemia, hemoglobin, plasma ferritin, retinol binding protein, transferrin receptor, body iron stores, plasma zinc |
| Fabiansen 2017 | RCT | Province de Passore, Burkina Faso | 1609 children aged 6–23 months | Group 1: LNS (N = 809) Lipid-based nutrient supplement was given every 2 weeks for 12 weeks Group 2: CSB (N = 800) Corn/soy blend was given every 2 weeks for 12 weeks | Fat free mass index, recovery rate, anthropometric measures |
| Karakochul 2012 | cRCT | 10 health centers and health posts in the northern region of the Sidama zone, Ethiopia | 1125 children aged 6–60 months | Group 1: RUSF (N = 375) Supplementary Plumpy’Nut (Nutriset) was given biweekly for 16 weeks Group 2: CSB (N = 750) CSB: Corn/soy blend + vegetable oil (premix) was given biweekly for 16 weeks | Recovery, default, transport, non-response, mortality |
| La Grone 2012 | RCT | Rural setting in South TFC, Malawi | 2890 children aged 6–59 months | Group 1: CSB++ (N = 948) Group 2: Soy RUSF (N = 964) Group 3: Soy/whey RUSF (N = 978) | Recovered and developed SAM, remaining MAM, death, default time to recovery, rate of adverse events, and rates of gain in weight, length, and MUAC |
| Matilsky 2009 | RCT | Rural setting in southern region of Malawi | 1362 children aged 6–60 months | Group 1: Milk/peanut fortified spread (Nutriset) (N = 465) Given every 2 weeks for 8 weeks Group 2: Soy/peanut fortified spread (Nutriset) (N = 450) Given every 2 weeks for 8 weeks Group 3: Corn-Soy Blend (N = 447) Given every 2 weeks for 8 weeks | Recovery; rates of gain in weight, stature, and mid-upper arm circumference (MUAC); and adverse outcomes |
| Medoua 2015 | RCT | Health districts of Mvog-Beti and Evodoula in the central region of Cameroon | 81 children aged 6–59 months | Group 1: CSB+ (N = 41) Improved corn/soy blend: corn, soya, sugar, min/vit + soy oil was given every 2 weeks for 16 weeks. Treatment diet provided 40 kcal/kg/d Group 2: RUSF (N = 40) Ready-to-use supplementary food: soya, corn flour, peanut paste, sugar, soy oil, min/vit was given every 2 weeks for 16 weeks. Control diet provided 40 kcal/kg/d | Recovery rate, time to recovery; and rates of gain in weight and mid-upper arm circumference |
| Nackers 2010 | RCT | Two supplementary feeding centers (SFCs) in the remote and difficult-to-access villages of Mallawa and Bangaza (Magaria department, Zinder region, South of Niger) | 807 children aged 6–59 months | Group 1: CSB (N = 406) Corn/soy blend premix + vegetable oil + sugar was given weekly for 16 weeks Group 2: RUTF-Nutriset (N = 401) (Plumpy’Nut) Peanut, powder milk, vegetable oil, vit/min mix was given weekly for 16 weeks | Weight gain and the recovery rate, mortality, non-responder and defaulter rates, length of stay, MUAC gain and hemoglobin gain, relapse and height gain |
| Nikiema 2014 | cRCT | Rural setting in Hounde, Burkina Faso | 1974 children aged 6–24 months of age | Group 1: Child centered counselling (N = 605) Only education counselling was given weekly for 12 weeks. No supplementation was provided Group 2: Corn soy blend (CSB++) (N = 675) Maize, soybean, milk, soy oil, vit/min mix diet was provided weekly for 12 weeks Group 3: RUSF (N = 694) Peanut butter, vegetable oil, whole soybean, shea butter, micronutrient-based diet was provided weekly for 12 weeks | Recovery, death, or drop-out; attendance; time to recovery; weight; length; daily MUAC gains |
| Phuka 2009 | RCT | Rural setting in Lungwena, Mangochi District, Malawi | 176 children aged 6–18 months | Group 1: LP fortified (N = 86) Maize flour, soya flour, micronutrient diet was given (71 g/d) weekly for 12 weeks Group 2: RUSF (N = 90) Maize flour-peanut butter, milk, vegetable oil, micronutrient diet was given (50 g/d) weekly for 12 weeks | Weight gain, length gain, mean change in anthropometric indices WAZ, LAZ, WLZ, recovery, change in MUAC, change in blood hemoglobin |
| Scherbaum 2015 | Quasi-experimental | Nias Island, Indonesia | 129 children under five years of age | Group 1: Peanut/milk-based spreads program (N = 44) Peanut/milk-based spread was given for 4 to 6 weeks or until recovered Group 2: CNL-B: Cereal/nut/legume-based biscuits program (N = 47) Cereal/nut/legume-based biscuits were given for 4 to 6 weeks or until recovered Group 3: CNL-B and intensive nutrition education (INE) (N = 38) Cereal/nut/legume-based biscuits + intensive nutrition education were given for 4 to 6 weeks or until recovered | Weight, height, WHZ, recovery, compliance |
| Singh 2010 | RCT | Rural setting in Vellore, India | 118 children aged 18–60 months | Group 1: RUTF (N = 61) Group 2: High caloric cereal meal (N = 57) High calorie cereal milk (HCCM) supplement | Recovery; changes in vitamin B12, plasma Zinc, serum albumin levels, and iron status |
| Stobough 2016 | RCT | Rural setting in South Malawi/Mozambique border residents | 2259 children aged 6–59 months of age | Group 1: Whey protein RUSF: (N = 1144) A dairy-based, whey protein, whey permeate concentrate (75 kcal/kg/day) was given every 2 weeks for 12 weeks Group 2: soy-flour RUSF (N = 2086) Extruded soy flour (75 kcal/kg/day) was given every 2 weeks for 12 weeks | Recovery; changes in MUAC, weight, and length; time to recovery; any adverse events |
| Thakwalakwa 2010 | RCT | Rural setting of Lungwena, Mangochi district of Malawi | 189 children aged 6–15 months | Group 1: CSB (N = 67) Corn/soy blend given weekly for 12 weeks Group 2: LNS (N = 66) Peanut paste, dry skim milk, vegetable oil, sugar, min/vit mix given weekly for 12 weeks Group 3: Control (N = 59) Infants breastfed only | Weight change, length change, hemoglobin, WLZ, LAZ, MUAC, head circumference, adverse events |
| Vanelli 2014 | RCT | Makeni, Northern region, Sierra Leonne | 332 children aged 6–60 months | Group 1: Feeding Program supplementations (N = 177) Group 2 (N = 159) 100 g servings of “Parma pap” equal to the weekly requirement containing peanut, palm oil, milk, mineral/vitamin mix given weekly for 12 weeks | Weight, length, WHZ |
| Comparison 6: Prophylactic use of antibiotics in children with uncomplicated SAM compared to no antibiotics | |||||
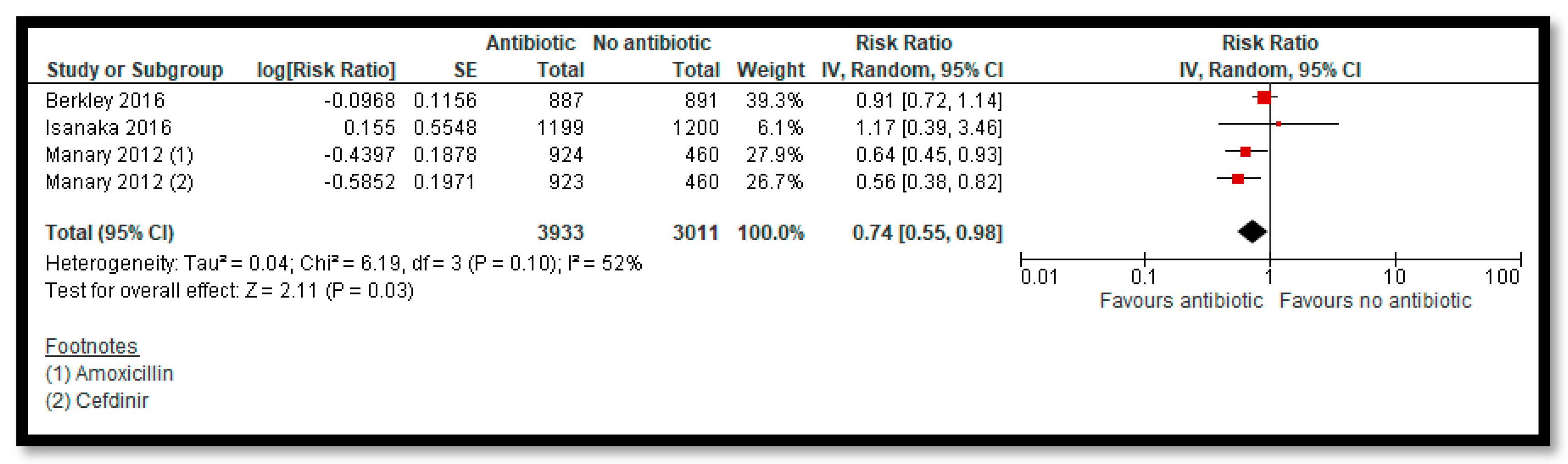
| Berkley 2016 | RCT | Study was carried out in four hospitals in Kenya (two rural hospitals in Kilifi and Malindi, and two urban hospitals in Mombasa and Nairobi) | 1781 children aged 60 days to 59 months | Group 1 (N = 887) Daily treatment with water dispersible co-trimoxazole tablets for 6 months Group 2 (N = 891) Placebo given daily for 6 months | Mortality, frequency of non-fatal illness episodes resulting in readmission to hospital outpatient attendance; the clinical syndromes associated with death or illness; pathogens detected from blood culture, urine culture, and malaria testing; suspected toxic effects during the period that investigational products were received; and changes in MUAC, weight-for-height, weight-for-length, weight-for-age, height-for-age, length-for-age, head circumference-for-age, and hematological indices |
| Isanaka 2016 | RCT | Rural setting in Madarounfa, Niger | 2412 children aged 6–59 months | Intervention (N = 1210) Twice daily treatment with a split-dose of 80 mg/kg of body weight with amoxicillin. Duration of treatment was 1 week. Control (N = 1202) Placebo administered two times per day for 1 week | Nutritional recovery by 8 weeks, non-response at 8 weeks, death from any cause, default, and transfer to inpatient care |
| Manary 2012 | RCT | 18 feeding clinics in rural Malawi | 2767 children aged 6–59 months | Group 1: Amoxicillin (N = 924) Daily treatment with amoxicillin suspension of 80–90 mg/kg for initial 7 days of the therapy Group 2: Cefdinir (N = 923) Daily treatment with 14 mg/kg Cefdinir suspension for initial 7 days of the therapy Group 3: Placebo (N = 920) Placebo administered daily for initial 7 days of the therapy | Recovery rate, mortality, weight gain, length gain, antibiotics rates of adverse events, and time to recovery |
| Comparison 7: Vitamin A supplementation in the management of SAM and MAM with various doses and frequency of administration | |||||
| Donnen 1998 | RCT | Rural setting in Katana health district, South Kivu, Democratic Republic of Congo | 900 hospitalized preschool children aged 0–72 months | Group 1 (N = 300) High dose Vitamin A (200,000 IU or 100, 000 IU (age < 12 months)) on day of admission followed by placebo for every subsequent day until discharge Group 2 (N = 298) Low dose Vitamin A (5000 IU) on day of admission followed by placebo for every subsequent day until discharge Control (N = 302) Placebo administered until discharge | Morbidity, mortality, duration of hospitalization |
| Sattar 2012 | RCT | Urban/peri-urban setting in Dhaka, Bangladesh | 260 children aged 6–59 months | Group 1: High dose Vitamin A (N = 130) 200,000 IU or 100, 000 IU if aged < 12 months on day of admission followed by low dose (5000 IU) on each subsequent day for 15 days Group 2: Placebo (N = 130) Administered on day of admission followed by low dose vitamin A (5000 IU) each day for 15 days | Clinical success, adverse events; clinical features of vitamin A toxicity, changes in serum retinol and RBP levels, duration of resolution of diarrhea, ALRI, edema, dermatosis, other illness, changes in weight and length or height, nosocomial morbidities and mortality |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Das, J.K.; Salam, R.A.; Saeed, M.; Kazmi, F.A.; Bhutta, Z.A. Effectiveness of Interventions for Managing Acute Malnutrition in Children under Five Years of Age in Low-Income and Middle-Income Countries: A Systematic Review and Meta-Analysis. Nutrients 2020, 12, 116. https://doi.org/10.3390/nu12010116
Das JK, Salam RA, Saeed M, Kazmi FA, Bhutta ZA. Effectiveness of Interventions for Managing Acute Malnutrition in Children under Five Years of Age in Low-Income and Middle-Income Countries: A Systematic Review and Meta-Analysis. Nutrients. 2020; 12(1):116. https://doi.org/10.3390/nu12010116
Chicago/Turabian StyleDas, Jai K., Rehana A. Salam, Marwah Saeed, Faheem Ali Kazmi, and Zulfiqar A. Bhutta. 2020. "Effectiveness of Interventions for Managing Acute Malnutrition in Children under Five Years of Age in Low-Income and Middle-Income Countries: A Systematic Review and Meta-Analysis" Nutrients 12, no. 1: 116. https://doi.org/10.3390/nu12010116
APA StyleDas, J. K., Salam, R. A., Saeed, M., Kazmi, F. A., & Bhutta, Z. A. (2020). Effectiveness of Interventions for Managing Acute Malnutrition in Children under Five Years of Age in Low-Income and Middle-Income Countries: A Systematic Review and Meta-Analysis. Nutrients, 12(1), 116. https://doi.org/10.3390/nu12010116




