Access to Genetic Counselors in the Southern United States
Abstract
1. Introduction
2. Materials & Methods
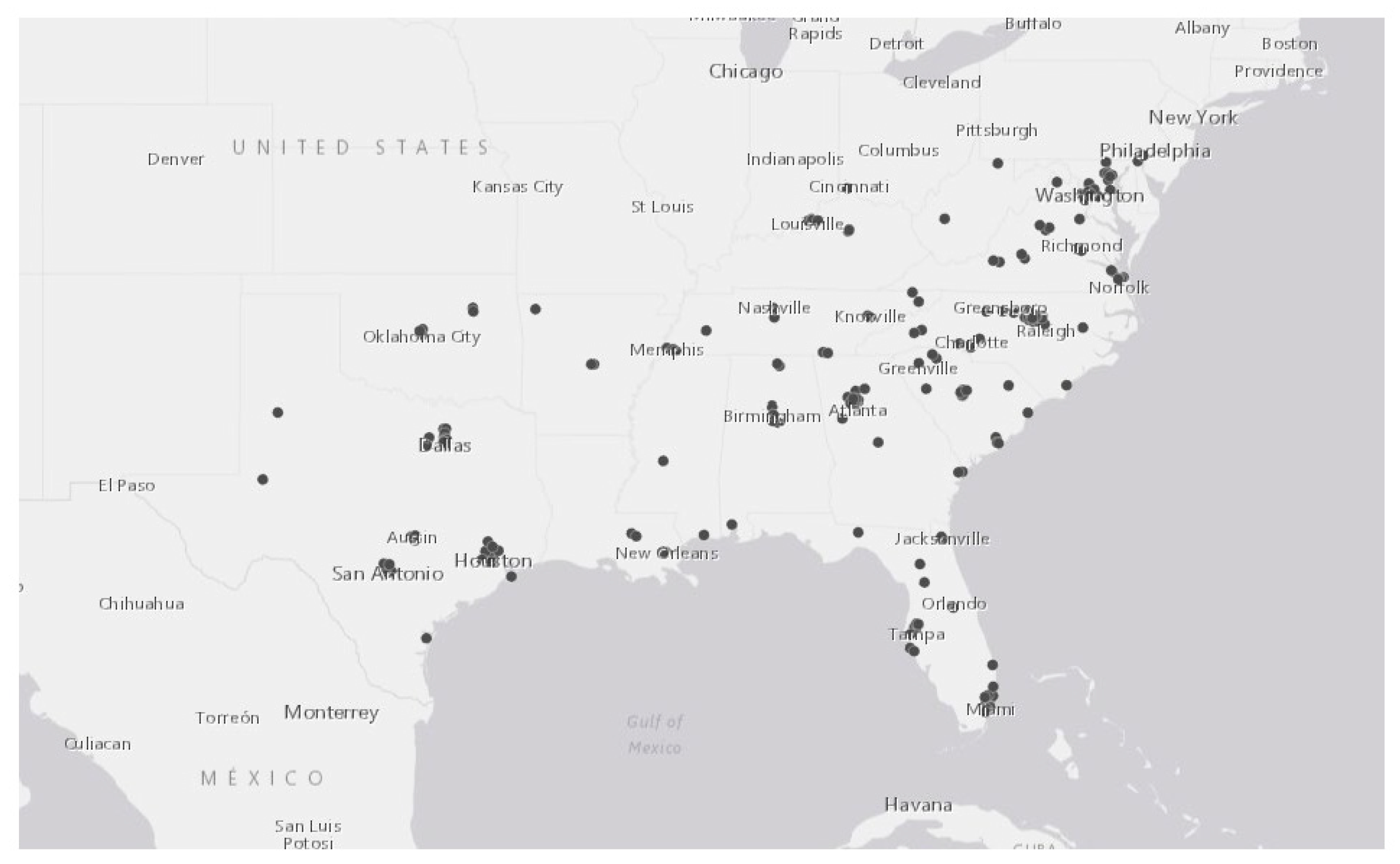
3. Results
4. Discussion
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Institute of Medicine. Implications of Genomics for Public Health: Workshop Summary; National Academies Press: Washington, DC, USA, 2005. [Google Scholar]
- Smedley, B.D.; Stith, A.Y.; Nelson, A.R.; Institute of Medicine (U.S.) Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care; National Academy Press: Washington, DC, USA, 2003; p. 764. [Google Scholar]
- American Board of Genetic Counselors. Mission & History. Available online: https://www.abgc.net/about-abgc/mission-history/ (accessed on 18 November 2018).
- Hoskovec, J.M.; Bennett, R.L.; Carey, M.E.; DaVanzo, J.E.; Dougherty, M.; Hahn, S.E.; LeRoy, B.S.; O’Neal, S.; Richardson, J.G.; Wicklund, C.A. Projecting the supply and demand for certified genetic counselors: A workforce study. J. Genet. Couns. 2018, 27, 16–20. [Google Scholar] [CrossRef] [PubMed]
- National Society of Genetic Counselors. 2018 Professional Status Survey: Executive Summary. Available online: https://www.nsgc.org/p/cm/ld/fid=68 (accessed on 11 May 2018).
- National Society of Genetic Counselors. 2008 Professional Status Survey: Executive Summary; National Society of Genetic Counselors: Chicago, IL, USA, 2008. [Google Scholar]
- National Society of Genetic Counselors. 2019 Professional Status Survey: Executive Summary. Available online: https://www.nsgc.org/d/do/9099 (accessed on 28 May 2019).
- Burns, K.; Swanson, A.; Hoskovec, J.; Leonhard, J.; Hahn, S.; Stein, Q.P. Genetic counseling job market in the United States and Canada: An analysis of job advertisements 2014–2016. J. Genet. Couns. 2019. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.A.; Tucker, M.E. Movement of genetic counselors from clinical to non-clinical positions: Identifying driving forces. J. Genet. Couns. 2018, 27, 792–799. [Google Scholar] [CrossRef] [PubMed]
- Cooksey, J.A.; Forte, G.; Benkendorf, J.; Blitzer, M.G. The state of the medical geneticist workforce: Findings of the 2003 survey of American Board of Medical Genetics certified geneticists. Genet. Med. Off. J. Am. Coll. Med. Genet. 2005, 7, 439–443. [Google Scholar] [CrossRef]
- Institute of Medicine Roundtable on Translating Genomic-Based Research. Innovations in Service Delivery in the Age of Genomics: Workshop Summary; National Academies Press: Washington, DC, USA, 2009. [Google Scholar]
- Wicklund, C.; Trepanier, A. Adapting genetic counseling training to the genomic era: More an evolution than a revolution. J. Genet. Couns. 2014, 23, 452–454. [Google Scholar] [CrossRef] [PubMed]
- Radford, C.; Prince, A.; Lewis, K.; Pal, T. Factors Which impact the delivery of genetic risk assessment services focused on inherited cancer genomics: Expanding the role and reach of certified genetics professionals. J. Genet. Couns. 2014, 23, 522–530. [Google Scholar] [CrossRef]
- Cohen, S.A.; Tucker, M.E.; Delk, P. Genetic counselor workforce issues: A survey of genetic counselors licensed in the State of Indiana. J. Genet. Couns. 2017, 26, 567–575. [Google Scholar] [CrossRef]
- U.S. Census Bureau. Available online: https://www.census.gov/popclock/data_tables.php?component=growth (accessed on 18 November 2017).
- Artiga, S.; Damico, A. Health and Health Coverage in the South: A Data Update. Available online: http://kff.org/disparities-policy/issue-brief/health-and-health-coverage-in-the-south-a-data-update/ (accessed on 18 November 2016).
- Radley, D.C.; McCarthy, D.; Hayes, S.L. Aiming Higher: Results from the Commonwealth Fund Scorecard on State Health System Performance; The Commonwealth Fund: New York, NY, USA, 2017. [Google Scholar]
- Health Resources & Services Administration. Medically Underserved Areas/Populations (MUA/P). State Summary of Designated MUA/P. Available online: https://ersrs.hrsa.gov/ReportServer?/HGDW_Reports/BCD_MUA/BCD_MUA_State_Statistics&rs:Format=PDF (accessed on 18 November 2018).
- U.S. Census Bureau. Census Bureau Regions and Divisions with State FIPS Codes. Available online: https://www2.census.gov/geo/docs/maps-data/maps/reg_div.txt (accessed on 18 November 2018).
- National Society of Genetic Counselors. In Person—Find a Genetic Counselor. Available online: https://www.nsgc.org/page/find-a-gc-search (accessed on 18 November 2018).
- American Board of Genetic Counselors. Find a Certified Genetic Counselor. Available online: https://www.abgc.net/about-genetic-counseling/find-a-certified-counselor.aspx/ (accessed on 18 November 2018).
- Healthgrades. Find a Doctor. Available online: https://www.healthgrades.com/find-a-doctor (accessed on 18 November 2018).
- U.S. Census Bureau. American Community Survey (ACS). Available online: https://www.census.gov/programs-surveys/acs/ (accessed on 21 December 2018).
- Joseph, K.S.; Allen, A.C.; Dodds, L.; Turner, L.A.; Scott, H.; Liston, R. The perinatal effects of delayed childbearing. Obstet. Gynecol. 2005, 105, 1410–1418. [Google Scholar] [CrossRef]
- Prysak, M.; Lorenz, R.P.; Kisly, A. Pregnancy outcome in nulliparous women 35 years and older. Obstet. Gynecol. 1995, 85, 65–70. [Google Scholar] [CrossRef]
- Jacobsson, B.; Ladfors, L.; Milsom, I. Advanced maternal age and adverse perinatal outcome. Obstet. Gynecol. 2004, 104, 727–733. [Google Scholar] [CrossRef]
- Kean, N.; Turner, J.; Flatley, C.; ClinEpi, M.; Kumar, S. Maternal age potentiates the impact of operative birth on serious neonatal outcomes. J. Matern. Fetal Neonatal Med. 2018, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Driscoll, D.A.; Gross, S. Clinical practice. Prenatal screening for aneuploidy. N. Engl. J. Med. 2009, 360, 2556–2562. [Google Scholar] [CrossRef] [PubMed]
- Pan, V.; Yashar, B.M.; Pothast, R.; Wicklund, C. Expanding the genetic counseling workforce: Program directors’ views on increasing the size of genetic counseling graduate programs. Genet. Med. 2016, 18, 842–848. [Google Scholar] [CrossRef] [PubMed]
- Kozhimannil, K.B.; Hardeman, R.R.; Henning-Smith, C. Maternity care access, quality, and outcomes: A systems-level perspective on research, clinical, and policy needs. Semin. Perinatol. 2017, 41, 367–374. [Google Scholar] [CrossRef] [PubMed]
- The American Congress of Obstetrics and Gynecology. The Obstetrician-Gynecologist Workforce in the United States: Facts, Figures, and Implications. 2017. Available online: https://m.acog.org/~/media/BB3A7629943642ADA47058D0BDCD1521.pdf (accessed on 28 May 2017).
- Davis, M.A.; Anthopolos, R.; Tootoo, J.; Titler, M.; Bynum, J.P.W.; Shipman, S.A. Supply of healthcare providers in relation to county socioeconomic and health status. J. Gen. Intern. Med. 2018, 33, 412–414. [Google Scholar] [CrossRef]
- Goldstein, J.T.; Hartman, S.G.; Meunier, M.R.; Panchal, B.; Pecci, C.C.; Zink, N.M.; Shields, S.G. Supporting family physician maternity care providers. Fam. Med. 2018, 50, 662–671. [Google Scholar] [CrossRef] [PubMed]
- Moaddab, A.; Dildy, G.A.; Brown, H.L.; Bateni, Z.H.; Belfort, M.A.; Sangi-Haghpeykar, H.; Clark, S.L. Health care disparity and pregnancy-related mortality in the United States, 2005–2014. Obstet. Gynecol. 2018, 131, 707–712. [Google Scholar] [CrossRef]
- U.S. Centers for Disease Control and Prevention. Mean Age of Mothers is on the Rise: 2000–2014. Available online: https://www.cdc.gov/nchs/data/databriefs/db232.htm (accessed on 18 November 2018).
- Chen, F.; Liu, P.; Gu, Y.; Zhu, Z.; Nanisetti, A.; Lan, Z.; Huang, Z.; Liu, S.J.; Kang, X.; Deng, Y.; et al. Isolation and Whole Genome Sequencing of fetal cells from maternal blood towards the ultimate non-invasive prenatal testing. Prenat. Diagn. 2017, 37, 1311–1321. [Google Scholar] [CrossRef]
- Committee on Practice Bulletins—Obstetrics, Committee on Genetics, and the Society for Maternal-Fetal Medicine. Practice Bulletin No. 163: Screening for Fetal Aneuploidy. Obstet. Gynecol. 2016, 127, e123–e137. [Google Scholar] [CrossRef]
- Iwarsson, E.; Jacobsson, B.; Dagerhamn, J.; Davidson, T.; Bernabe, E.; Heibert Arnlind, M. Analysis of cell-free fetal DNA in maternal blood for detection of trisomy 21, 18 and 13 in a general pregnant population and in a high risk population—A systematic review and meta-analysis. Acta Obstet. Gynecol. Scand. 2017, 96, 7–18. [Google Scholar] [CrossRef]
- McLennan, A.; Palma-Dias, R.; da Silva Costa, F.; Meagher, S.; Nisbet, D.L.; Scott, F. Noninvasive prenatal testing in routine clinical practice—An audit of NIPT and combined first-trimester screening in an unselected Australian population. Aust. N. Z. J. Obstet. Gynaecol. 2016, 56, 22–28. [Google Scholar] [CrossRef] [PubMed]
- D’Agincourt-Canning, L.; McGillivray, B.; Panabaker, K.; Scott, J.; Pearn, A.; Ridge, Y.; Portigal-Todd, C. Evaluation of genetic counseling for hereditary cancer by videoconference in British Columbia. BC Med. J. 2008, 50, 554–559. [Google Scholar]
- McDonald, E.; Lamb, A.; Grillo, B.; Lucas, L.; Miesfeldt, S. Acceptability of telemedicine and other cancer genetic counseling models of service delivery in geographically remote settings. J. Genet. Couns. 2014, 23, 221–228. [Google Scholar] [CrossRef] [PubMed]
- Hilgart, J.S.; Hayward, J.A.; Coles, B.; Iredale, R. Telegenetics: A systematic review of telemedicine in genetic services. Genet. Med. 2012, 14, 756–776. [Google Scholar] [CrossRef] [PubMed]
- Kane, C.J.; Gillis, K. The use of telemedicine by physicians: Still the exception rather than the rule. Health Aff. (Project Hope) 2018, 37. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.A.; Huziak, R.C.; Gustafson, S.; Grubs, R.E. Analysis of advantages, limitations, and barriers of genetic counseling service delivery models. J. Genet. Couns. 2016, 25, 1010–1018. [Google Scholar] [CrossRef]
- Schwartz, M.D.; Valdimarsdottir, H.B.; Peshkin, B.N.; Mandelblatt, J.; Nusbaum, R.; Huang, A.-T.; Chang, Y.; Graves, K.; Isaacs, C.; Wood, M.; et al. Randomized noninferiority trial of telephone versus in-person genetic counseling for hereditary breast and ovarian cancer. J. Clin. Oncol. 2014, 32, 618–626. [Google Scholar] [CrossRef] [PubMed]
- Weissman, S.M.; Zellmer, K.; Gill, N.; Wham, D. Implementing a virtual health telemedicine program in a community setting. J. Genet. Couns. 2018, 27, 323–325. [Google Scholar] [CrossRef]
- Zierhut, H.A.; MacFarlane, I.M.; Ahmed, Z.; Davies, J. Genetic counselors’ experiences and interest in telegenetics and remote counseling. J. Genet. Couns. 2018, 27, 329–338. [Google Scholar] [CrossRef]
- Buchanan, A.H.; Datta, S.K.; Sknner, C.S.; Hollowell, G.P.; Beresford, H.F.; Freeland, T.; Rogers, B.; Boling, J.; Marcom, P.K.; Adams, M.B. Randomized trial of telegenetics vs. in-person cancer genetic counseling: Cost, patient satisfaction and attendance. J. Genet. Couns. 2015, 24, 961–970. [Google Scholar] [CrossRef]
- Abrams, D.J.; Geier, M.R. A Comparison of patient satisfaction with telehealth and on-site consultations: A pilot study for prenatal genetic counseling. J. Genet. Couns. 2006, 15, 199–205. [Google Scholar] [CrossRef] [PubMed]
- Solomons, N.M.; Lamb, A.E.; Lucas, F.L.; McDonald, E.F.; Miesfeldt, S. Examination of the patient-focused impact of cancer telegenetics among a rural population: Comparison with traditional in-person services. Telemed. J. E-Health Off. J. Am. Telemed. Assoc. 2018, 24, 130–138. [Google Scholar] [CrossRef] [PubMed]
- Zilliacus, E.M.; Meiser, B.; Lobb, E.A.; Kelly, P.J.; Barlow-Stewart, K.; Kirk, J.A.; Spigelman, A.D.; Warwick, L.J.; Tucker, K.M. Are videoconferenced consultations as effective as face-to-face consultations for hereditary breast and ovarian cancer genetic counseling? Genet. Med. 2011, 13, 933–941. [Google Scholar] [CrossRef] [PubMed]
- Doughty Rice, C.; Ruscham, J.G.; Martin, L.J.; Manders, J.B.; Miller, E. Retrospective comparison of patient outcomes after in-person and telephone results disclosure counseling for BRCA1/2 genetic testing. Fam. Cancer 2010, 9, 203–212. [Google Scholar] [CrossRef] [PubMed]
- Kinney, A.Y.; Steffen, L.E.; Brumbach, B.H.; Kohlmann, W.; Du, R.; Lee, J.-H.; Gammon, A.; Butler, K.; Buys, S.S.; Stroup, A.M.; et al. Randomized noninferiority trial of telephone delivery of BRCA1/2 genetic counseling compared with in-person counseling: 1-Year follow-up. J. Clin. Oncol. 2016, 34. [Google Scholar] [CrossRef] [PubMed]
- Boothe, E.; Kaplan, J. Using telemedicine in Mississippi to improve patient access to genetic services. J. Genet. Couns. 2018, 27, 320–322. [Google Scholar] [CrossRef] [PubMed]
- Reiser, C.; Van Vreede, V.; Petty, E.M. Genetic counselor workforce generational diversity: Millennials to Baby Boomers. J. Genet. Couns. 2019. [Google Scholar] [CrossRef]
- Gammon, B.L.; Otto, L.; Wick, M.; Borowski, K.; Allyse, M. Implementing group prenatal counseling for expanded noninvasive screening options. J. Genet. Couns. 2017, 27, 894–901. [Google Scholar] [CrossRef]
- Cloutier, M.; Gallagher, L.; Goldsmith, C.; Akiki, S.; Barrowman, N.; Morrison, S. Group genetic counseling: An alternate service delivery model in a high risk prenatal screening population. Prenat. Diagn. 2017, 37, 1112–1119. [Google Scholar] [CrossRef]
- Pirzadeh-Miller, S.; Robinson, L.S.; Read, P.; Ross, T.S. Genetic counseling assistants: An integral piece of the evolving genetic counseling service delivery model. J. Genet. Couns. 2017, 26, 716–727. [Google Scholar] [CrossRef]
- Chan, W.V.; Johnson, J.A.; Wilson, R.D.; Metcalfe, A. Obstetrical provider knowledge and attitudes towards cell-free DNA screening: Results of a cross-sectional national survey. BMC Pregnancy Childbirth 2018, 18, 40. [Google Scholar] [CrossRef] [PubMed]
- Brewer, J.; Demers, L.; Musci, T. Survey of US obstetrician opinions regarding NIPT use in general practice: Implementation and barriers. J. Matern. Fetal Neonatal Med. 2017, 30, 1793–1796. [Google Scholar] [CrossRef] [PubMed]
- Oxenford, K.; Daley, R.; Lewis, C.; Hill, M.; Chitty, L.S. Development and evaluation of training resources to prepare health professionals for counselling pregnant women about non-invasive prenatal testing for Down syndrome: A mixed methods study. BMC Pregnancy Childbirth 2017, 17, 132. [Google Scholar] [CrossRef] [PubMed]
- Adam, S.; Birch, P.H.; Coe, R.R.; Bansback, N.; Jones, A.L.; Connolly, M.B.; Demos, M.K.; Toyota, E.B.; Farrer, M.J.; Friedman, J.M. Assessing an interactive online tool to support parents’ genomic testing decisions. J. Genet. Couns. 2018, 28, 10–17. [Google Scholar] [CrossRef] [PubMed]
- Birch, P.H. Interactive e-counselling for genetics pre-test decisions: Where are we now? Clin. Genet. 2015, 87, 209–217. [Google Scholar] [CrossRef] [PubMed]
- Beulen, L.; van den Berg, M.; Faas, B.H.; Feenstra, I.; Hageman, M.; van Vugt, J.M.; Bekker, M.N. The effect of a decision aid on informed decision-making in the era of non-invasive prenatal testing: A randomised controlled trial. Eur. J. Hum. Genet. EJHG 2016, 24, 1409–1416. [Google Scholar] [CrossRef] [PubMed]
- Lepine, J.; Leiva Portocarrero, M.E.; Delanoe, A.; Robitaille, H.; Levesque, I.; Rousseau, F.; Wilson, B.J.; Giguere, A.M.; Legare, F. What factors influence health professionals to use decision aids for Down syndrome prenatal screening? BMC Pregnancy Childbirth 2016, 16, 262. [Google Scholar] [CrossRef]
- Emmet, M.; Stein, Q.; Thorpe, E.; Campion, M. Experiences of genetic counselors practicing in rural areas. J. Genet. Couns. 2018, 27, 140–154. [Google Scholar] [CrossRef]
- Williamson, L.; LeBlanc, D.B. A genetic services practice model: Advanced practice nurse and genetic counselor team. Newborn Infant Nurs. Rev. 2009, 8, 30–35. [Google Scholar] [CrossRef]
- Kubendran, S.; Sivamurthy, S.; Schaefer, G.B. A novel approach in pediatric telegenetic services: Geneticist, pediatrician and genetic counselor team. Genet. Med. Off. J. Am. Coll. Med. Genet. 2017, 19, 1260–1267. [Google Scholar] [CrossRef]
- Senier, L.; Kearney, M.; Orne, J. Using public-private partnerships to mitigate disparities in access to genetic services: Lessons from Wisconsin. Adv. Med. Sociol. 2015, 16, 269–305. [Google Scholar] [CrossRef] [PubMed]
- Texas Health and Human Services. Non-Invasive Prenatal Testing. Available online: https://hhs.texas.gov/about-hhs/communications-events/news/2016/03/non-invasive-prenatal-testing (accessed on 28 May 2016).
- Accreditation Council for Genetic Counseling. Program Directory. Available online: https://www.gceducation.org/program-directory/ (accessed on 28 May 2018).
- American Association of Medical Colleges. Key Facts from the 2015 State Data Book. Available online: https://www.aamc.org/download/464578/data/keyfactsfromthe2015statedatabook.pdf (accessed on 11 May 2015).
- Mittman, I.S.; Downs, K. Diversity in genetic counseling: Past, present and future. J. Genet. Couns. 2008, 17, 301–313. [Google Scholar] [CrossRef] [PubMed]
- Atiyeh, B.S.; Rubeiz, M.T.; Hayek, S.N. Aesthetic/Cosmetic surgery and ethical challenges. Aesthet. Plast. Surg. 2008, 32, 829–839; discussion 840–841. [Google Scholar] [CrossRef] [PubMed]
- Marrast, L.M.; Zallman, L.; Woolhandler, S.; Bor, D.H.; McCormick, D. Minority physicians’ role in the care of underserved patients: Diversifying the physician workforce may be key in addressing health disparities. JAMA Intern. Med. 2014, 174, 289–291. [Google Scholar] [CrossRef] [PubMed]
| State | Number of Practicing CGCs | Number of CGCs per 100,000 People | Number of Counties with a CGC/total Number of Counties | Percentage of Population Residing in Counties with a CGC (%) |
|---|---|---|---|---|
| Alabama | 19 | 0.39 | 4/67 | 33.66 |
| Arkansas | 11 | 0.37 | 2/75 | 20.61 |
| Delaware | 11 | 1.18 | 1/3 | 59.06 |
| District of Columbia | 16 | 2.43 | 1/1 | 100.00 |
| Florida | 52 | 0.26 | 11/67 | 58.32 |
| Georgia | 46 | 0.46 | 7/159 | 38.57 |
| Kentucky | 20 | 0.45 | 3/120 | 27.98 |
| Louisiana | 12 | 0.13 | 3/64 | 27.20 |
| Maryland | 101 | 1.70 | 4/23 | 50.89 |
| Mississippi | 5 | 0.17 | 2/82 | 14.83 |
| North Carolina | 105 | 1.06 | 11/100 | 43.93 |
| Oklahoma | 14 | 0.36 | 2/77 | 35.98 |
| South Carolina | 35 | 0.72 | 8/46 | 48.51 |
| Tennessee | 47 | 0.72 | 8/95 | 45.83 |
| Texas | 115 | 0.43 | 12/254 | 56.31 |
| Virginia | 72 | 0.87 | 15/95 | 39.46 |
| West Virginia | 2 | 0.11 | 2/55 | 15.84 |
| State | Median Household Income ($) of Counties without a CGC | Median Household Income ($) of Counties with a CGC | Percentage Difference in Median Household Income |
|---|---|---|---|
| Alabama | $37,557 | $53,685 | 30.04 |
| Arkansas | $36,032 | $46,272 | 22.13 |
| Delaware | $54,701 | $66,283 | 17.47 |
| Florida | $42,561 | $49,196 | 13.49 |
| Georgia | $38,436 | $58,851 | 34.69 |
| Kentucky | $39,479 | $50,661 | 22.07 |
| Louisiana | $40,771 | $49,457 | 17.56 |
| Maryland | $64,666 | $80,454 | 19.62 |
| Mississippi | $34,744 | $40,934 | 15.12 |
| North Carolina | $40,260 | $51,232 | 21.42 |
| Oklahoma | $44,216 | $49,820 | 11.25 |
| South Carolina | $37,362 | $48,059 | 22.26 |
| Tennessee | $38,854 | $48,144 | 19.30 |
| Texas | $45,557 | $59,354 | 23.25 |
| Virginia | $49,160 | $50,727 | 3.09 |
| West Virginia | $38,703 | $46,794 | 17.29 |
| State | Number of Practicing Prenatal CGCs Listed in the NSGC | Percentage of High Risk Births (%) | Number of Prenatal CGCs per 5000 High Risk Births |
|---|---|---|---|
| Alabama | 1 | 13.81 | 0.61 |
| Arkansas | 3 | 12.86 | 2.93 |
| Delaware | 1 | 23.57 | 1.90 |
| District of Columbia | 7 | 32.47 | 11.31 |
| Florida | 12 | 23.11 | 1.20 |
| Georgia | 9 | 20.32 | 1.58 |
| Kentucky | 3 | 15.71 | 1.71 |
| Louisiana | 2 | 14.06 | 1.17 |
| Maryland | 24 | 26.31 | 6.10 |
| Mississippi | 1 | 13.90 | 0.94 |
| North Carolina | 23 | 19.90 | 4.70 |
| Oklahoma | 3 | 14.43 | 1.98 |
| South Carolina | 12 | 17.40 | 5.81 |
| Tennessee | 4 | 15.40 | 1.59 |
| Texas | 35 | 18.90 | 2.33 |
| Virginia | 19 | 23.14 | 3.84 |
| West Virginia | 1 | 12.85 | 2.03 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Villegas, C.; Haga, S.B. Access to Genetic Counselors in the Southern United States. J. Pers. Med. 2019, 9, 33. https://doi.org/10.3390/jpm9030033
Villegas C, Haga SB. Access to Genetic Counselors in the Southern United States. Journal of Personalized Medicine. 2019; 9(3):33. https://doi.org/10.3390/jpm9030033
Chicago/Turabian StyleVillegas, Catalina, and Susanne B. Haga. 2019. "Access to Genetic Counselors in the Southern United States" Journal of Personalized Medicine 9, no. 3: 33. https://doi.org/10.3390/jpm9030033
APA StyleVillegas, C., & Haga, S. B. (2019). Access to Genetic Counselors in the Southern United States. Journal of Personalized Medicine, 9(3), 33. https://doi.org/10.3390/jpm9030033





