The Clinical Application of Machine Learning-Based Models for Early Prediction of Hemorrhage in Trauma Intensive Care Units
Abstract
1. Introduction
2. Materials and Methods
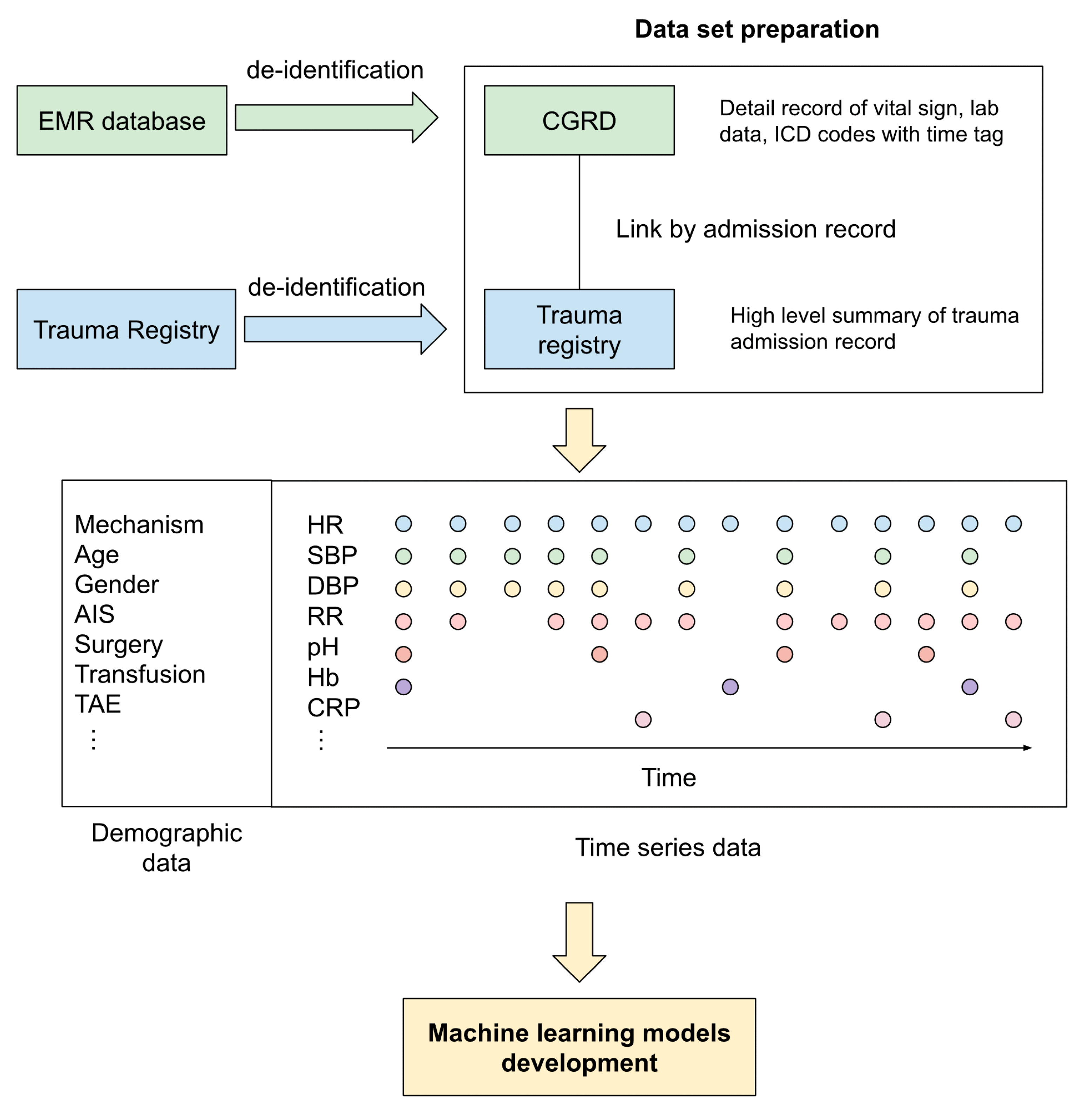
2.1. Database
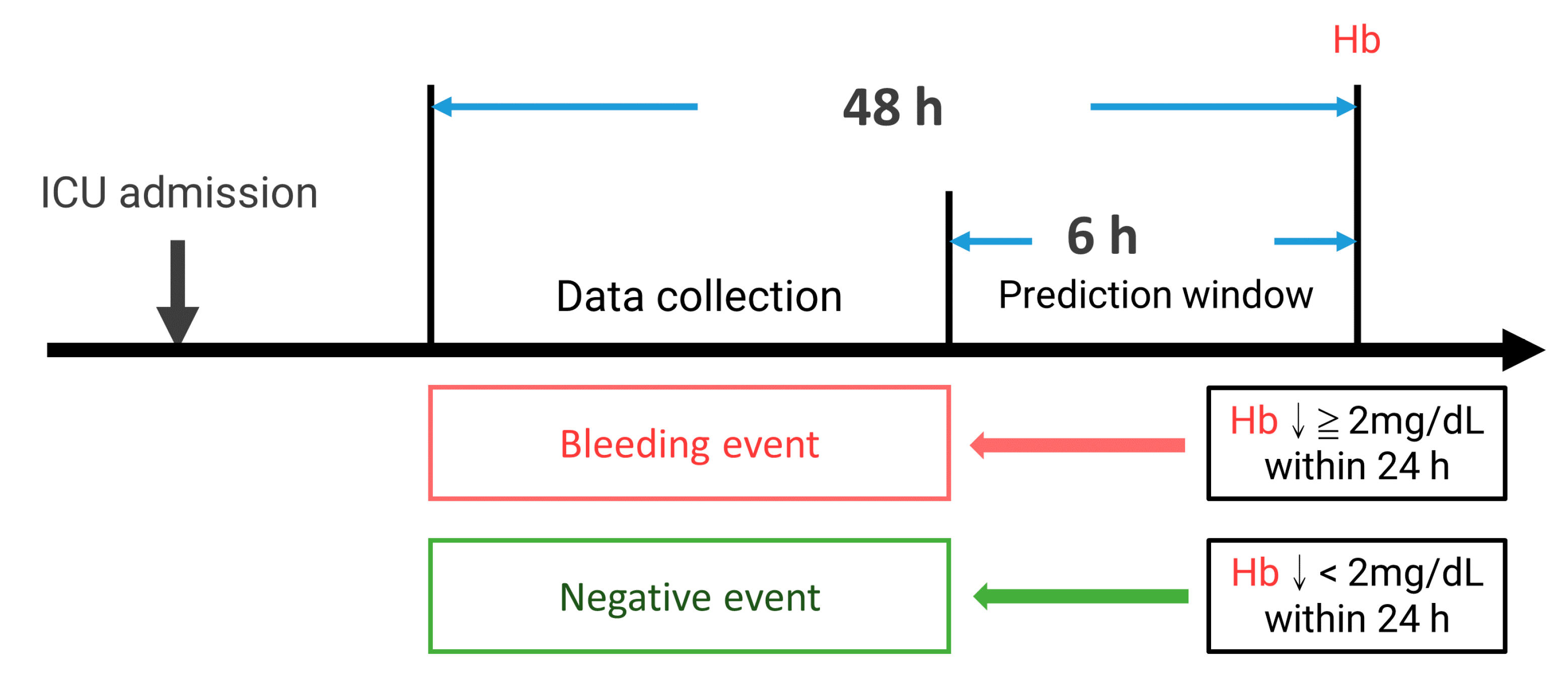
2.2. Data Selection and Inclusion Criteria
2.3. Features Generation and Data Preprocessing
2.4. Model Development
2.5. Statistical Analysis
3. Results
3.1. Demographics and Clinical Characteristics
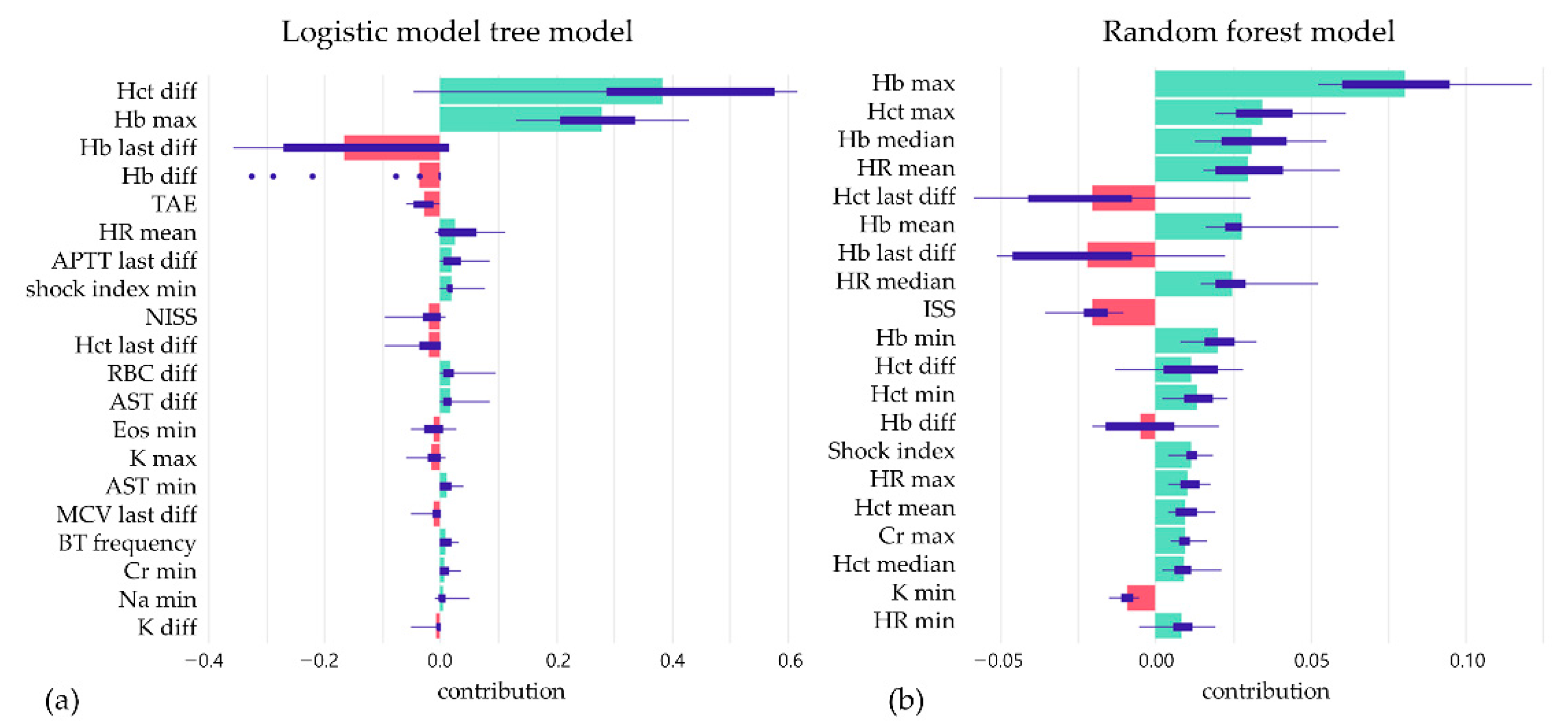
3.2. Feature Selection Outcome
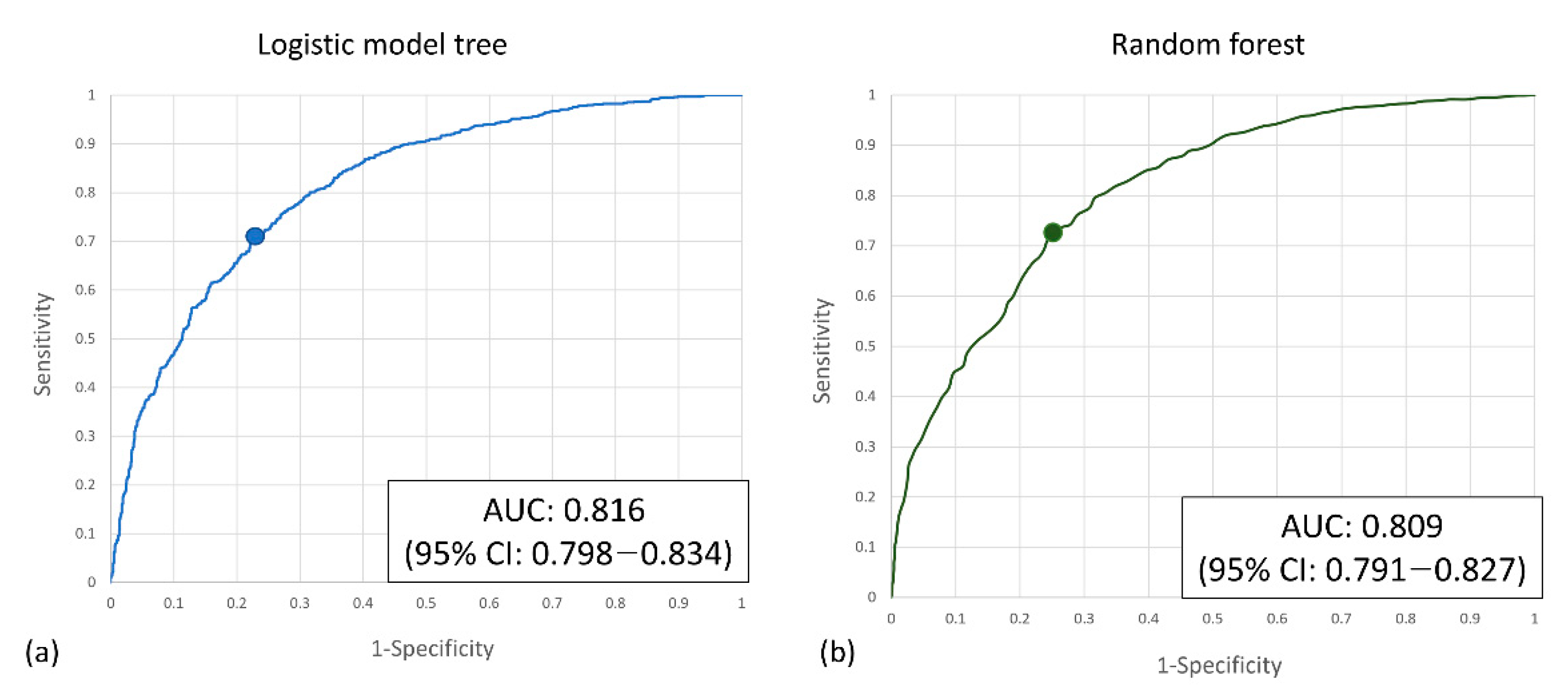
3.3. The Performance of Prediction Models
4. Discussion
5. Limitation
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Spahn, D.R.; Bouillon, B.; Cerny, V.; Duranteau, J.; Filipescu, D.; Hunt, B.J.; Komadina, R.; Maegele, M.; Nardi, G.; Riddez, L.; et al. The European Guideline on Management of Major Bleeding and Coagulopathy Following Trauma: Fifth Edition. Crit. Care 2019, 23, 98. [Google Scholar] [CrossRef] [PubMed]
- Parimi, N.; Hu, P.F.; Mackenzie, C.F.; Yang, S.; Bartlett, S.T.; Scalea, T.M.; Stein, D.M. Automated Continuous Vital Signs Predict Use of Uncrossed Matched Blood and Massive Transfusion Following Trauma. J. Trauma Acute Care Surg. 2016, 80, 897–906. [Google Scholar] [CrossRef] [PubMed]
- Liu, N.T.; Holcomb, J.B.; Wade, C.E.; Batchinsky, A.I.; Cancio, L.C.; Darrah, M.I.; Salinas, J. Development and Validation of a Machine Learning Algorithm and Hybrid System to Predict the Need for Life-Saving Interventions in Trauma Patients. Med. Biol. Eng. Comput. 2014, 52, 193–203. [Google Scholar] [CrossRef] [PubMed]
- Olaussen, A.; Blackburn, T.; Mitra, B.; Fitzgerald, M. Review Article: Shock Index for Prediction of Critical Bleeding Post-Trauma: A Systematic Review. Emerg. Med. Australas. 2014, 26, 223–228. [Google Scholar] [CrossRef]
- Convertino, V.A.; Moulton, S.L.; Grudic, G.Z.; Rickards, C.A.; Hinojosa-Laborde, C.; Gerhardt, R.T.; Blackbourne, L.H.; Ryan, K.L. Use of Advanced Machine-Learning Techniques for Noninvasive Monitoring of Hemorrhage. J. Trauma 2011, 71, S25–S32. [Google Scholar] [CrossRef]
- Shillan, D.; Sterne, J.A.C.; Champneys, A.; Gibbison, B. Use of Machine Learning to Analyse Routinely Collected Intensive Care Unit Data: A Systematic Review. Crit. Care 2019, 23, 284. [Google Scholar] [CrossRef]
- Awad, A.; Bader-El-Den, M.; McNicholas, J.; Briggs, J.; El-Sonbaty, Y. Predicting Hospital Mortality for Intensive Care Unit Patients: Time-Series Analysis. Health Inform. J. 2020, 26, 1043–1059. [Google Scholar] [CrossRef]
- Kizzier-Carnahan, V.; Artis, K.A.; Mohan, V.; Gold, J.A. Frequency of Passive EHR Alerts in the ICU: Another Form of Alert Fatigue? J. Patient Saf. 2019, 15, 246–250. [Google Scholar] [CrossRef]
- Huddar, V.; Desiraju, B.K.; Rajan, V.; Bhattacharya, S.; Roy, S.; Reddy, C.K. Predicting Complications in Critical Care Using Heterogeneous Clinical Data. IEEE Access 2016, 4, 7988–8001. [Google Scholar] [CrossRef]
- Syed, M.; Syed, S.; Sexton, K.; Syeda, H.B.; Garza, M.; Zozus, M.; Syed, F.; Begum, S.; Syed, A.U.; Sanford, J.; et al. Application of Machine Learning in Intensive Care Unit (ICU) Settings Using MIMIC Dataset: Systematic Review. Informatics 2021, 8, 16. [Google Scholar] [CrossRef]
- Badnjević, A.; Avdihodžić, H.; Gurbeta Pokvić, L. Artificial Intelligence in Medical Devices: Past, Present and Future. Psychiatr. Danub. 2021, 33, S336–S341. [Google Scholar] [CrossRef] [PubMed]
- Rajkomar, A.; Dean, J.; Kohane, I. Machine Learning in Medicine. N. Engl. J. Med. 2019, 380, 1347–1358. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.Y.; Kim, S.; Cho, J.; Kim, Y.S.; Sol, I.S.; Sung, Y.; Cho, I.; Park, M.; Jang, H.; Kim, Y.H.; et al. A Deep Learning Model for Real-Time Mortality Prediction in Critically Ill Children. Crit. Care 2019, 23, 279. [Google Scholar] [CrossRef] [PubMed]
- Shahi, N.; Shahi, A.K.; Phillips, R.; Shirek, G.; Bensard, D.; Moulton, S.L. Decision-Making in Pediatric Blunt Solid Organ Injury: A Deep Learning Approach to Predict Massive Transfusion, Need for Operative Management, and Mortality Risk. J. Pediatr. Surg. 2021, 56, 379–384. [Google Scholar] [CrossRef]
- Gutierrez, G. Artificial Intelligence in the Intensive Care Unit. Crit. Care 2020, 24, 101. [Google Scholar] [CrossRef]
- Zheng, H.; Shi, D. Using a LSTM-RNN Based Deep Learning Framework for ICU Mortality Prediction. In Proceedings of the Web Information Systems and Applications; Springer: Cham, Switzerland, 2018; pp. 60–67. [Google Scholar]
- Vezzoli, M.; Inciardi, R.M.; Oriecuia, C.; Paris, S.; Murillo, N.H.; Agostoni, P.; Ameri, P.; Bellasi, A.; Camporotondo, R.; Canale, C.; et al. Machine learning for prediction of in-hospital mortality in coronavirus disease 2019 patients: Results from an Italian multicenter study. J. Cardiovasc. Med. 2022, 23, 439–446. [Google Scholar] [CrossRef]
- Abate, G.; Vezzoli, M.; Polito, L.; Guaita, A.; Albani, D.; Marizzoni, M.; Garrafa, E.; Marengoni, A.; Forloni, G.; Frisoni, G.B.; et al. A Conformation Variant of p53 Combined with Machine Learning Identifies Alzheimer Disease in Preclinical and Prodromal Stages. J. Pers. Med. 2020, 11, 14. [Google Scholar] [CrossRef]
- Schulman, S.; Kearon, C.; Subcommittee on Control of Anticoagulation of the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis. Definition of Major Bleeding in Clinical Investigations of Antihemostatic Medicinal Products in Non-Surgical Patients. J. Thromb. Haemost. JTH 2005, 3, 692–694. [Google Scholar] [CrossRef]
- Liu, N.T.; Salinas, J. Machine Learning for Predicting Outcomes in Trauma. Shock 2017, 48, 504–510. [Google Scholar] [CrossRef]
- Wang, I.-J.; Bae, B.-K.; Park, S.-W.; Cho, Y.-M.; Lee, D.-S.; Min, M.-K.; Ryu, J.-H.; Kim, G.-H.; Jang, J.-H. Pre-Hospital Modified Shock Index for Prediction of Massive Transfusion and Mortality in Trauma Patients. Am. J. Emerg. Med. 2020, 38, 187–190. [Google Scholar] [CrossRef]
- Stewart, C.L.; Mulligan, J.; Grudic, G.Z.; Convertino, V.A.; Moulton, S.L. Detection of Low-Volume Blood Loss: Compensatory Reserve versus Traditional Vital Signs. J. Trauma Acute Care Surg. 2014, 77, 892–897; discussion 897–898. [Google Scholar] [CrossRef] [PubMed]
- Minne, L.; Ludikhuize, J.; de Jonge, E.; de Rooij, S.; Abu-Hanna, A. Prognostic Models for Predicting Mortality in Elderly ICU Patients: A Systematic Review. Intensive Care Med. 2011, 37, 1258–1268. [Google Scholar] [CrossRef] [PubMed]
- Knaus, W.A.; Wagner, D.P.; Draper, E.A.; Zimmerman, J.E.; Bergner, M.; Bastos, P.G.; Sirio, C.A.; Murphy, D.J.; Lotring, T.; Damiano, A. The APACHE III Prognostic System. Risk Prediction of Hospital Mortality for Critically Ill Hospitalized Adults. Chest 1991, 100, 1619–1636. [Google Scholar] [CrossRef] [PubMed]
- Gülcher, S.S.; Bruins, N.A.; Kingma, W.P.; Boerma, E.C. Elevated C-Reactive Protein Levels at ICU Discharge as a Predictor of ICU Outcome: A Retrospective Cohort Study. Ann. Intensive Care 2016, 6, 5. [Google Scholar] [CrossRef]
- Islam, M.M.; Nasrin, T.; Walther, B.A.; Wu, C.-C.; Yang, H.-C.; Li, Y.-C. Prediction of Sepsis Patients Using Machine Learning Approach: A Meta-Analysis. Comput. Methods Programs Biomed. 2019, 170, 1–9. [Google Scholar] [CrossRef] [PubMed]
| Group | Positive | Negative | p Value |
|---|---|---|---|
| No. | 1036 | 1182 | |
| Gender, male, n (%) | 782 (75.5) | 790 (66.8) | <0.001 |
| Age, median (IQR) | 37 (23–54) | 37 (225–6) | 0.914 |
| ED arrival GCS, median (IQR) | 15 (11–15) | 15 (13–15) | 0.843 |
| ED leave GCS, median (IQR) | 15 (11–15) | 15 (11–15) | 0.805 |
| AIS head, median (IQR) | 0 (0–2) | 0 (0–1) | 0.87 |
| AIS chest, median (IQR) | 3 (0–4) | 2.5 (0–4) | 0.864 |
| AIS abdomen, median (IQR) | 2 (0–3) | 3 (0–4) | 0.868 |
| ISS, median (IQR) | 22 (16–29) | 20 (13–29) | 0.634 |
| NISS, median (IQR) | 26 (173–4) | 22 (14–29) | 0.598 |
| TAE, n (%) | 399 (38.5) | 371 (31.4) | <0.001 |
| CPR, n (%) | 14 (1.4) | 15 (1.3) | 0.865 |
| Trauma team activation, n (%) | 514 (49.6) | 466 (39.4) | <0.001 |
| Intubation, n (%) | 145 (14.0) | 100 (8.5) | <0.001 |
| Demographic Feature | Gain Ratio | Hematology | Gain Ratio | Biochemistry | Gain Ratio |
|---|---|---|---|---|---|
| NISS | 0.0140824 | HB last diff | 0.060502 | ALT max | 0.0217857 |
| ED intubation | 0.0111678 | HB max | 0.057131 | AST mean | 0.0217508 |
| ISS | 0.0105278 | Hct max | 0.055303 | AST median | 0.0217508 |
| ED trauma blue | 0.0076397 | Hct last diff | 0.049209 | AST min | 0.0191412 |
| Gender | 0.0075227 | HB median | 0.044343 | AST max | 0.0171591 |
| ED leave GCS | 0.0054404 | Hb mean | 0.044343 | Cre min | 0.0157679 |
| TAE | 0.0043155 | Hct median | 0.041516 | Cre frequency | 0.0153933 |
| ED CPR | 0.0000937 | Hct mean | 0.041516 | Cre max | 0.0130096 |
| Hb diff | 0.03215 | Cre median | 0.0126784 | ||
| Vital signs | Gain Ratio | Hct diff | 0.031456 | Cre mean | 0.0126784 |
| HR median | 0.017608 | Hct min | 0.029003 | ALT min | 0.0120391 |
| HR mean | 0.017608 | RBC max | 0.028482 | ALT median | 0.0117981 |
| HR max | 0.0142613 | Hb min | 0.027336 | ALT mean | 0.0117981 |
| HR min | 0.013361 | MCV min | 0.020603 | K diff | 0.01081 |
| BT min | 0.0107972 | RBC mean | 0.019859 | ||
| SI median | 0.0094917 | RBC median | 0.019859 | ||
| SI mean | 0.0094917 | RBC min | 0.016197 | ||
| SI min | 0.0094543 | MCV max | 0.016045 | ||
| SI max | 0.0077304 | MCV median | 0.015736 | ||
| BT frequency | 0.0073078 | MCV mean | 0.015736 | ||
| SBP frequency | 0.0071975 | Platelets frequency | 0.013502 |
| Algorithm | Positive (Pred) | Negative (Ped) | Sensitivity | Specificity | F-Measure | AUC | |
|---|---|---|---|---|---|---|---|
| LMT | Positive (Act) | 740 | 296 | 71.40% | 75.90% | 0.718 | 0.816 |
| Negative (Act) | 285 | 897 | |||||
| RF | Positive (Act) | 762 | 274 | 73.60% | 73.70% | 0.723 | 0.809 |
| Negative (Act) | 311 | 871 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, S.-W.; Kung, H.-C.; Huang, J.-F.; Hsu, C.-P.; Wang, C.-C.; Wu, Y.-T.; Wen, M.-S.; Cheng, C.-T.; Liao, C.-H. The Clinical Application of Machine Learning-Based Models for Early Prediction of Hemorrhage in Trauma Intensive Care Units. J. Pers. Med. 2022, 12, 1901. https://doi.org/10.3390/jpm12111901
Lee S-W, Kung H-C, Huang J-F, Hsu C-P, Wang C-C, Wu Y-T, Wen M-S, Cheng C-T, Liao C-H. The Clinical Application of Machine Learning-Based Models for Early Prediction of Hemorrhage in Trauma Intensive Care Units. Journal of Personalized Medicine. 2022; 12(11):1901. https://doi.org/10.3390/jpm12111901
Chicago/Turabian StyleLee, Shih-Wei, His-Chun Kung, Jen-Fu Huang, Chih-Po Hsu, Chia-Cheng Wang, Yu-Tung Wu, Ming-Shien Wen, Chi-Tung Cheng, and Chien-Hung Liao. 2022. "The Clinical Application of Machine Learning-Based Models for Early Prediction of Hemorrhage in Trauma Intensive Care Units" Journal of Personalized Medicine 12, no. 11: 1901. https://doi.org/10.3390/jpm12111901
APA StyleLee, S.-W., Kung, H.-C., Huang, J.-F., Hsu, C.-P., Wang, C.-C., Wu, Y.-T., Wen, M.-S., Cheng, C.-T., & Liao, C.-H. (2022). The Clinical Application of Machine Learning-Based Models for Early Prediction of Hemorrhage in Trauma Intensive Care Units. Journal of Personalized Medicine, 12(11), 1901. https://doi.org/10.3390/jpm12111901








