Tailored Surgical Stabilization of Rib Fractures Matters More Than the Number of Fractured Ribs
Abstract
1. Introduction
2. Materials and Methods
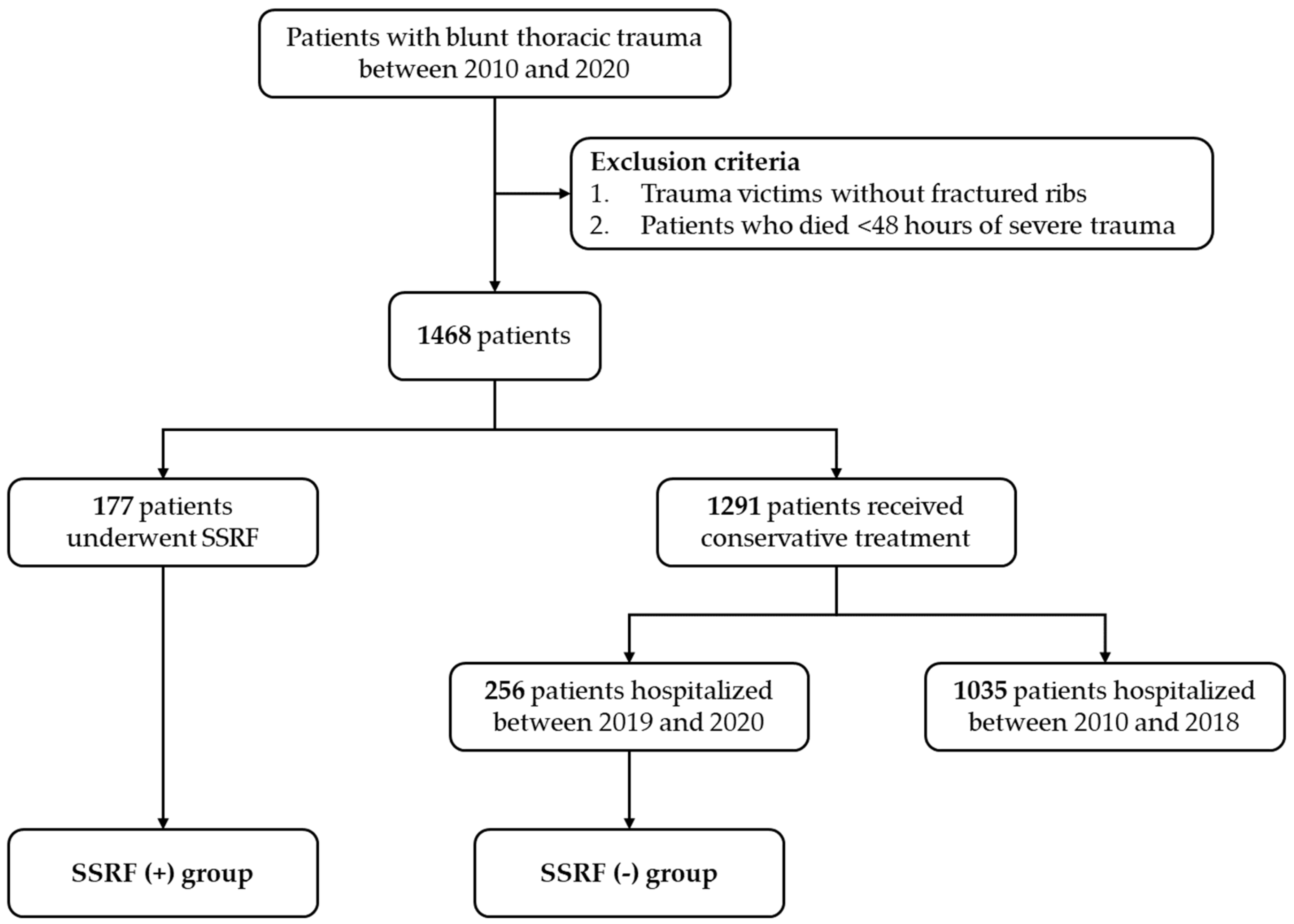
2.1. Patient Enrollment and Data Collection
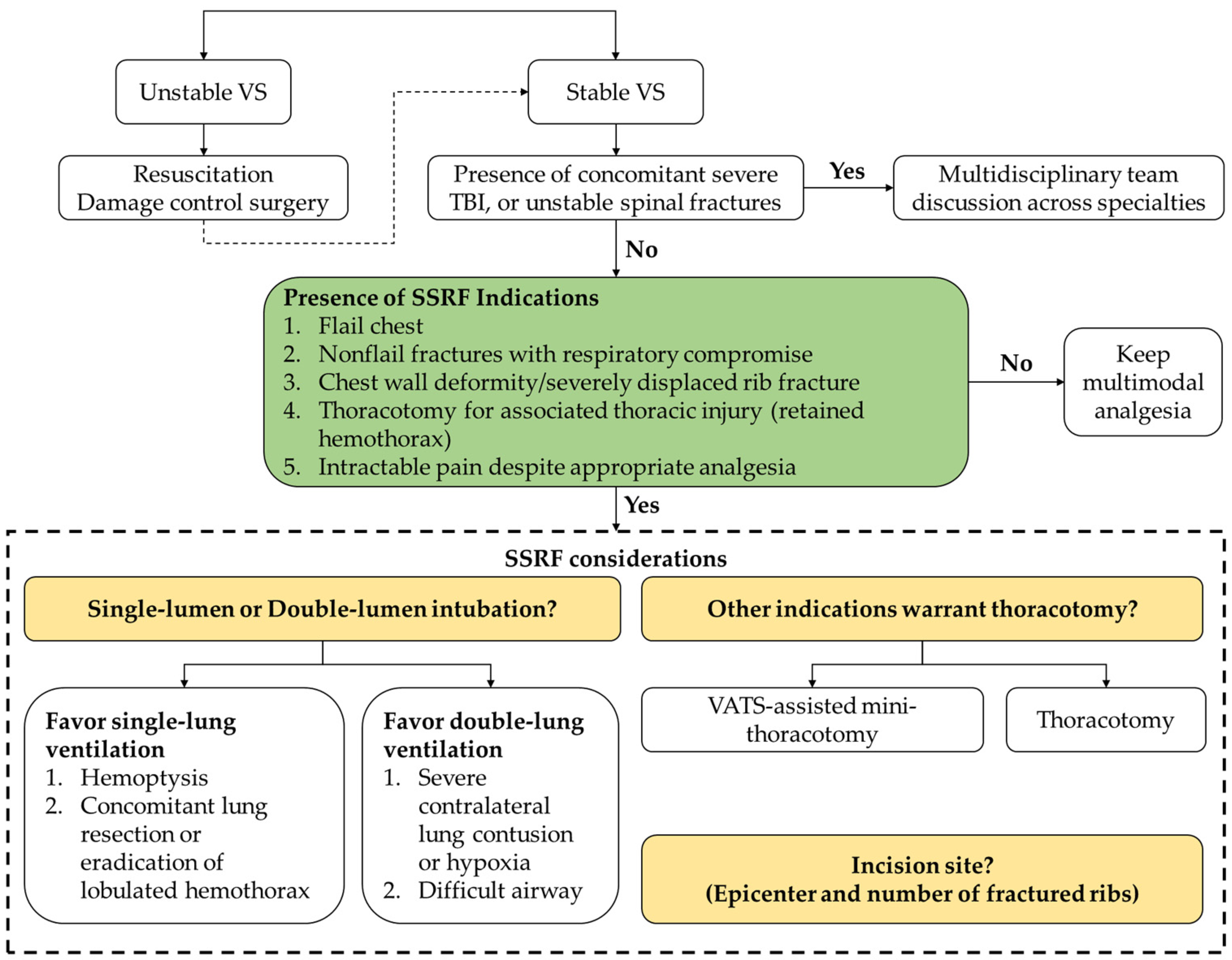
2.2. Algorithmic Approach with Tailored Surgical Planning
2.3. Outcomes
2.4. Statistical Analyses
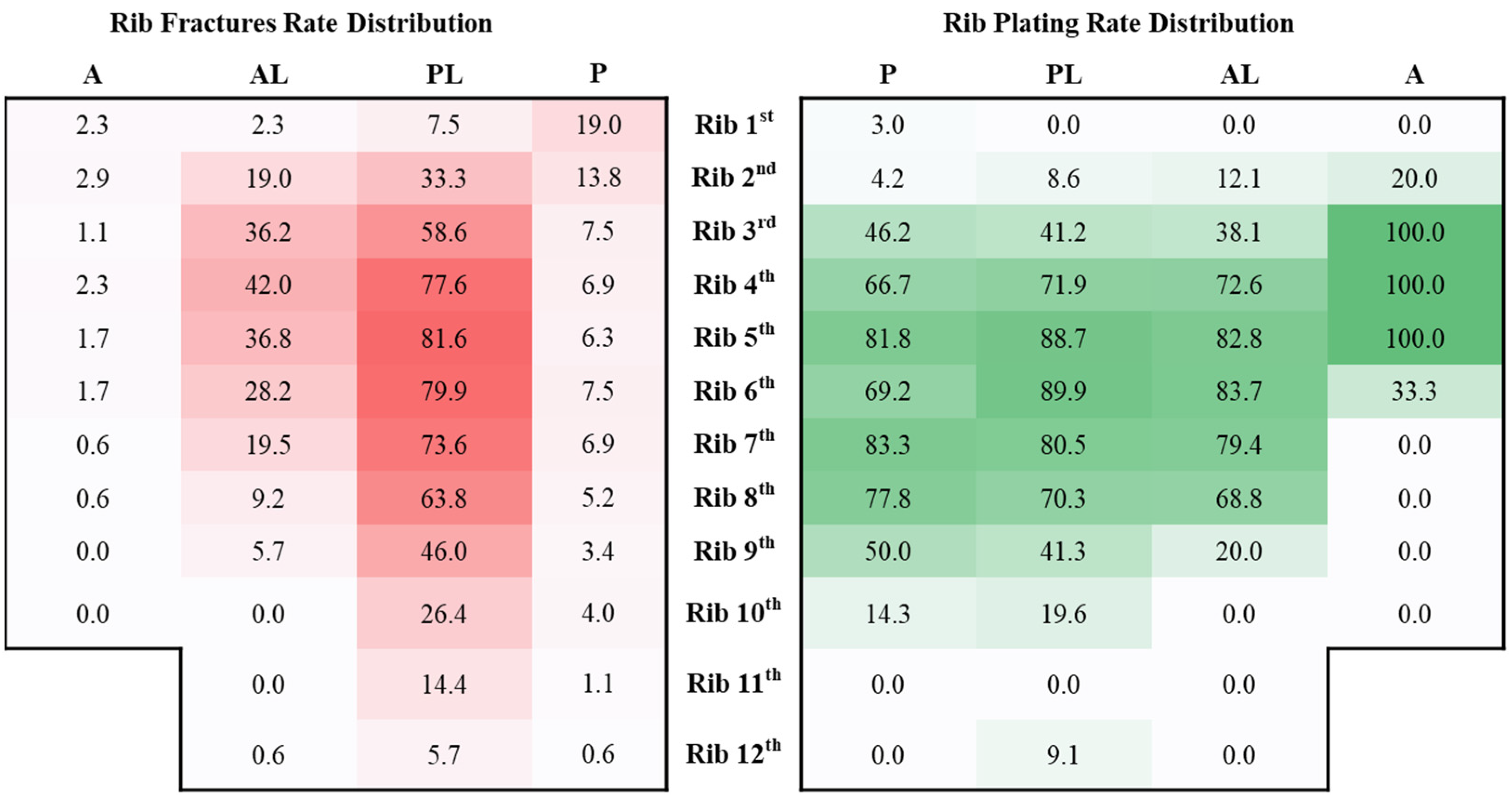
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chalya, P.L.; Dass, R.M.; McHembe, M.D.; Mbelenge, N.; Ngayomela, I.H.; Chandika, A.B.; Gilyoma, J.M.; Mabula, J.B. Citywide trauma experience in Mwanza, Tanzania: A need for urgent intervention. J. Trauma Manag. Outcomes 2013, 7, 9. [Google Scholar] [CrossRef] [PubMed]
- Ziegler, D.W.; Agarwal, N.N. The morbidity and mortality of rib fractures. J. Trauma 1994, 37, 975–979. [Google Scholar] [CrossRef] [PubMed]
- Bulger, E.M.; Arneson, M.A.; Mock, C.N.; Jurkovich, G.J. Rib fractures in the elderly. J. Trauma 2000, 48, 1040–1046; discussion 1046–1047. [Google Scholar] [CrossRef] [PubMed]
- Flagel, B.T.; Luchette, F.A.; Reed, R.L.; Esposito, T.J.; Davis, K.A.; Santaniello, J.M.; Gamelli, R.L. Half-a-dozen ribs: The breakpoint for mortality. Surgery 2005, 138, 717–723; discussion 723–725. [Google Scholar] [CrossRef]
- Lien, Y.C.; Chen, C.H.; Lin, H.C. Risk factors for 24-hour mortality after traumatic rib fractures owing to motor vehicle accidents: A nationwide population-based study. Ann. Thorac. Surg. 2009, 88, 1124–1130. [Google Scholar] [CrossRef]
- Narayanan, R.; Kumar, S.; Gupta, A.; Bansal, V.K.; Sagar, S.; Singhal, M.; Mishra, B.; Bhoi, S.; Gupta, B.; Gamangatti, S.; et al. An Analysis of Presentation, Pattern and Outcome of Chest Trauma Patients at an Urban Level 1 Trauma Center. Indian J. Surg. 2018, 80, 36–41. [Google Scholar] [CrossRef]
- Bergeron, E.; Lavoie, A.; Clas, D.; Moore, L.; Ratte, S.; Tetreault, S.; Lemaire, J.; Martin, M. Elderly trauma patients with rib fractures are at greater risk of death and pneumonia. J. Trauma 2003, 54, 478–485. [Google Scholar] [CrossRef]
- Bolliger, C.T.; Van Eeden, S.F. Treatment of multiple rib fractures. Randomized controlled trial comparing ventilatory with nonventilatory management. Chest 1990, 97, 943–948. [Google Scholar] [CrossRef]
- Wu, C.L.; Jani, N.D.; Perkins, F.M.; Barquist, E. Thoracic epidural analgesia versus intravenous patient-controlled analgesia for the treatment of rib fracture pain after motor vehicle crash. J. Trauma 1999, 47, 564–567. [Google Scholar] [CrossRef]
- Yang, Y.; Young, J.B.; Schermer, C.R.; Utter, G.H. Use of ketorolac is associated with decreased pneumonia following rib fractures. Am. J. Surg. 2014, 207, 566–572. [Google Scholar] [CrossRef]
- Galvagno, S.M., Jr.; Smith, C.E.; Varon, A.J.; Hasenboehler, E.A.; Sultan, S.; Shaefer, G.; To, K.B.; Fox, A.D.; Alley, D.E.; Ditillo, M.; et al. Pain management for blunt thoracic trauma: A joint practice management guideline from the Eastern Association for the Surgery of Trauma and Trauma Anesthesiology Society. J. Trauma Acute Care Surg. 2016, 81, 936–951. [Google Scholar] [CrossRef] [PubMed]
- Williams, A.; Bigham, C.; Marchbank, A. Anaesthetic and surgical management of rib fractures. BJA Educ. 2020, 20, 332–340. [Google Scholar] [CrossRef] [PubMed]
- Yeying, G.; Liyong, Y.; Yuebo, C.; Yu, Z.; Guangao, Y.; Weihu, M.; Liujun, Z. Thoracic paravertebral block versus intravenous patient-controlled analgesia for pain treatment in patients with multiple rib fractures. J. Int. Med. Res. 2017, 45, 2085–2091. [Google Scholar] [CrossRef] [PubMed]
- Forero, M.; Adhikary, S.D.; Lopez, H.; Tsui, C.; Chin, K.J. The Erector Spinae Plane Block: A Novel Analgesic Technique in Thoracic Neuropathic Pain. Reg. Anesth. Pain Med. 2016, 41, 621–627. [Google Scholar] [CrossRef]
- Rose, P.; Ramlogan, R.; Sullivan, T.; Lui, A. Serratus anterior plane blocks provide opioid-sparing analgesia in patients with isolated posterior rib fractures: A case series. Can. J. Anaesth. 2019, 66, 1263–1264. [Google Scholar] [CrossRef]
- Caragounis, E.C.; Fagevik Olsen, M.; Pazooki, D.; Granhed, H. Surgical treatment of multiple rib fractures and flail chest in trauma: A one-year follow-up study. World J. Emerg. Surg. 2016, 11, 27. [Google Scholar] [CrossRef]
- Fokin, A.A.; Hus, N.; Wycech, J.; Rodriguez, E.; Puente, I. Surgical Stabilization of Rib Fractures: Indications, Techniques, and Pitfalls. JBJS Essent Surg. Tech. 2020, 10, e0032. [Google Scholar] [CrossRef]
- Lin, H.L.; Tarng, Y.W.; Wu, T.H.; Huang, F.D.; Huang, W.Y.; Chou, Y.P. The advantages of adding rib fixations during VATS for retained hemothorax in serious blunt chest trauma—A prospective cohort study. Int. J. Surg. 2019, 65, 13–18. [Google Scholar] [CrossRef]
- Granetzny, A.; Abd El-Aal, M.; Emam, E.; Shalaby, A.; Boseila, A. Surgical versus conservative treatment of flail chest. Evaluation of the pulmonary status. Interact. Cardiovasc. Thorac. Surg. 2005, 4, 583–587. [Google Scholar] [CrossRef]
- Marasco, S.F.; Davies, A.R.; Cooper, J.; Varma, D.; Bennett, V.; Nevill, R.; Lee, G.; Bailey, M.; Fitzgerald, M. Prospective randomized controlled trial of operative rib fixation in traumatic flail chest. J. Am. Coll. Surg. 2013, 216, 924–932. [Google Scholar] [CrossRef]
- Kasotakis, G.; Hasenboehler, E.A.; Streib, E.W.; Patel, N.; Patel, M.B.; Alarcon, L.; Bosarge, P.L.; Love, J.; Haut, E.R.; Como, J.J. Operative fixation of rib fractures after blunt trauma: A practice management guideline from the Eastern Association for the Surgery of Trauma. J. Trauma Acute Care Surg. 2017, 82, 618–626. [Google Scholar] [CrossRef] [PubMed]
- Love, J.C.; Derrick, S.M.; Wiersema, J.M.; Pinto, D.C.; Greeley, C.; Donaruma-Kwoh, M.; Bista, B. Novel classification system of rib fractures observed in infants. J. Forensic. Sci. 2013, 58, 330–335. [Google Scholar] [CrossRef] [PubMed]
- Thorax. J. Orthop. Trauma 2018, 32 (Suppl. 1), S161–S166. [CrossRef] [PubMed]
- Marasco, S.; Liew, S.; Edwards, E.; Varma, D.; Summerhayes, R. Analysis of bone healing in flail chest injury: Do we need to fix both fractures per rib? J. Trauma Acute Care Surg. 2014, 77, 452–458. [Google Scholar] [CrossRef]
- La Padula, S.; Hersant, B.; Meningaud, J.P. Intraoperative use of indocyanine green angiography for selecting the more reliable perforator of the anterolateral thigh flap: A comparison study. Microsurgery 2018, 38, 738–744. [Google Scholar] [CrossRef]
- Tanaka, H.; Yukioka, T.; Yamaguti, Y.; Shimizu, S.; Goto, H.; Matsuda, H.; Shimazaki, S. Surgical stabilization of internal pneumatic stabilization? A prospective randomized study of management of severe flail chest patients. J. Trauma 2002, 52, 727–732; discussion 732. [Google Scholar] [CrossRef]
- Shelat, V.G.; Eileen, S.; John, L.; Teo, L.T.; Vijayan, A.; Chiu, M.T. Chronic pain and its impact on quality of life following a traumatic rib fracture. Eur. J. Trauma Emerg. Surg. 2012, 38, 451–455. [Google Scholar] [CrossRef]
- Fabricant, L.; Ham, B.; Mullins, R.; Mayberry, J. Prolonged pain and disability are common after rib fractures. Am. J. Surg. 2013, 205, 511–515; discusssion 515–516. [Google Scholar] [CrossRef]
- Doben, A.R.; Eriksson, E.A.; Denlinger, C.E.; Leon, S.M.; Couillard, D.J.; Fakhry, S.M.; Minshall, C.T. Surgical rib fixation for flail chest deformity improves liberation from mechanical ventilation. J. Crit. Care 2014, 29, 139–143. [Google Scholar] [CrossRef]
- Rabiou, S.; Ouadnouni, Y.; Lakranbi, M.; Traibi, A.; Antoini, F.; Smahi, M. Chronic chest pain after rib fracture: It can cause a disability? Rev. Pneumol. Clin. 2018, 74, 89–95. [Google Scholar] [CrossRef]
- Knoll, H.; Ziegeler, S.; Schreiber, J.U.; Buchinger, H.; Bialas, P.; Semyonov, K.; Graeter, T.; Mencke, T. Airway injuries after one-lung ventilation: A comparison between double-lumen tube and endobronchial blocker: A randomized, prospective, controlled trial. Anesthesiology 2006, 105, 471–477. [Google Scholar] [CrossRef] [PubMed]
- Casos, S.R.; Richardson, J.D. Role of thoracoscopy in acute management of chest injury. Curr. Opin. Crit. Care 2006, 12, 584–589. [Google Scholar] [CrossRef] [PubMed]
- Liebsch, C.; Seiffert, T.; Vlcek, M.; Beer, M.; Huber-Lang, M.; Wilke, H.J. Patterns of serial rib fractures after blunt chest trauma: An analysis of 380 cases. PLoS ONE 2019, 14, e0224105. [Google Scholar] [CrossRef] [PubMed]
| (N = 177) | |
|---|---|
| Age at time of surgery, y | 56.0 (45.5–64.5) |
| Sex (male) | 106 (59.9) |
| Transferal | 59 (33.9) |
| Charlson Comorbidity Index | 2.0 (0.0–3.0) |
| Medication required hypertension | 51 (28.8) |
| Coronary artery disease | 13 (7.3) |
| Atrial fibrillation | 5 (2.8) |
| Peripheral artery disease | 2 (1.1) |
| Heart failure (ACC/AHA ≥ stage C) | 1 (0.6) |
| Medication required diabetes mellitus | 37 (20.9) |
| Chronic kidney disease (eGFR < 60 mL/min) | 5 (2.8) |
| Liver cirrhosis | 3 (1.7) |
| Connective tissue disease | 3 (1.7) |
| Chronic obstructive pulmonary disease/Asthma | 2 (1.1) |
| Psychiatric disorders | 7 (4.0) |
| Malignancy | 11 (6.2) |
| 2010–2018 N = 93 | 2019–2020 N = 84 | 2010–2020 N = 177 | |
|---|---|---|---|
| Glasgow Coma Scale | 15 (15–15) | 15 (15–15) | 15 (15–15) |
| Trauma mechanism | |||
| Vehicle-to-vehicle collision | 60 (64.5) | 52 (61.9) | 112 (63.3) |
| Vehicle-to-pedestrian collision | 3 (3.2) | 3 (3.6) | 6 (3.4) |
| Single-vehicle collision | 15 (16.1) | 17 (20.2) | 32 (18.1) |
| Fall | 15 (16.1) | 11 (13.1) | 26 (14.7) |
| Crush | 0 (0.0) | 1 (1.2) | 1 (0.6) |
| Injury Severity Score | 20 (14–25) | 17 (13–22) | 17 (13–24) |
| Head/Neck | |||
| Median (IQR) | 0 (0–2) | 0 (0–2) | 0 (0–2) |
| AIS ≥ 3 | 16 (17.2) | 14 (16.7) | 30 (16.9) |
| Face | |||
| Median (IQR) | 0 (0–0) | 0 (0–0) | 0 (0–0) |
| AIS ≥ 3 | 1 (1.1) | 0 (0.0) | 1 (0.6) |
| Thorax | |||
| Median (IQR) | 3 (3–4) | 3 (3–3) | 3 (3–3) |
| AIS ≥ 3 | 93 (100.0) | 84 (100.0) | 177 (100.0) |
| Abdomen | |||
| Median (IQR) | 0 (0–2) | 0 (0–2) | 0 (0–2) |
| AIS ≥ 3 | 15 (16.1) | 11 (13.1) | 26 (14.7) |
| Extremity | |||
| Median (IQR) | 2 (0–2) | 2 (0–2) | 2 (0–2) |
| AIS ≥ 3 | 15 (16.1) | 9 (10.7) | 24 (13.6) |
| External | |||
| Median (IQR) | 0 (0–0) | 0 (0–0) | 0 (0–0) |
| AIS ≥ 3 | 1 (1.1) | 1 (1.2) | 2 (1.1) |
| Pattern of rib fractures | |||
| Number of ribs broken | 7 (5–9) | 6 (5–8) | 7 (5–9) |
| Presence of a flail segment radiologically | 37 (39.8) | 35 (41.7) | 72 (40.7) |
| Requiring mechanical ventilation | 15 (16.1) | 11 (13.1) | 26 (14.7) |
| Fractured side | |||
| Right | 34 (36.6) | 35 (41.7) | 69 (39.0) |
| Left | 43 (46.2) | 40 (47.6) | 83 (46.9) |
| Both | 16 (17.2) | 9 (10.7) | 25 (14.1) |
| Position on involved ribs (total fractured site = 1502) | |||
| Anterior | 2 (0.2) | 21 (3.1) | 23 (1.5) |
| Anterolateral | 209 (25.5) | 137 (20.1) | 346 (23.0) |
| Posterolateral | 534 (65.1) | 456 (66.9) | 990 (65.9) |
| Posterior | 75 (9.1) | 68 (10.0) | 143 (9.5) |
| Associated injuries | |||
| Lung contusion/laceration | 40 (43.0) | 28 (33.3) | 68 (38.4) |
| Pneumothorax | 51 (54.8) | 43 (51.2) | 94 (53.1) |
| Hemothorax | 81 (87.1) | 70 (83.3) | 151 (85.3) |
| Cardiac injury | 2 (2.2) | 0 (0.0) | 2 (1.1) |
| Great vessels | 0 (0.0) | 1 (1.2) | 1 (0.6) |
| Soft tissue | 21 (22.6) | 22 (26.2) | 43 (24.3) |
| Concurrent sternal fracture | 4 (4.3) | 4 (4.8) | 8 (4.5) |
| Concurrent ipsilateral clavicular fracture | 38 (40.9) | 45 (53.6) | 83 (46.9) |
| Concurrent ipsilateral scapular fracture | 19 (20.4) | 18 (21.4) | 37 (20.9) |
| Surgery-related factors | |||
| Indication | |||
| Flail chest | 37 (39.8) | 35 (41.7) | 72 (40.7) |
| nonflail fractures with respiratory compromise | 8 (8.6) | 6 (7.3) | 14 (7.9) |
| Chest wall deformity/severely displaced | 5 (5.4) | 6 (7.3) | 11 (6.2) |
| Thoracotomy for associated thoracic injury (e.g., hemothorax, lung laceration) | 77 (82.8) | 42 (50.0) | 119 (67.2) |
| Intractable pain despite appropriate analgesia | 58 (62.4) | 61 (74.4) | 119 (67.2) |
| Time from trauma to rib fixation, d | 4.0 (2.0–6.0) | 3.0 (1.3–5.0) | 4.0 (2.5–7.0) |
| Number of surgically fixated rib fractures | 4 (3–5) | 4 (3–5) | 4 (3–5) |
| Fracture fixation ratio | 0.6 (0.4–0.8) | 0.6 (0.5–0.8) | 0.6 (0.5–0.8) |
| Mechanical ventilation during anesthesia (N = 169) | |||
| Single lung ventilation | 69 (80.2) | 54 (65.1) | 123 (69.5) |
| Double lung ventilation | 17 (19.8) | 29 (34.9) | 46 (26.0) |
| Approach side | |||
| Right | 46 (49.5) | 40 (47.6) | 86 (48.6) |
| Left | 45 (48.4) | 44 (52.4) | 89 (50.3) |
| Both | 2 (2.2) | 0 (0.0) | 2 (1.1) |
| Incision | |||
| Thoracotomy | 27 (29.0) | 21 (25.0) | 48 (27.1) |
| Video-assisted minithoracotomy | 66 (71.0) | 63 (75.0) | 129 (72.9) |
| Combined operation | 45 (48.4) | 45 (53.6) | 90 (50.8) |
| Operation time, min | 144 (123–204) | 154 (125–198) | 145 (124–198) |
| Blood loss, mL | 100 (0–200) | 100 (0–188) | 100 (0–200) |
| N = 177 | |
|---|---|
| Ventilator days, d (N = 70) | 5.0 (2.0–9.0) |
| Postoperative ventilator days, d (N = 70) | 2.0 (1.0–4.0) |
| Length of ICU stay, d (N = 93) | 6.0 (3.0–12.0) |
| Postoperative ICU stay, d (N = 93) | 4.0 (2.0–7.0) |
| Length of hospital stay, d | 13.0 (9.0–19.5) |
| Postoperative hospital stay, d | 8.0 (5.0–13.0) |
| Time from trauma to ambulation, d | 3.0 (1.0–7.5) |
| Time from rib fixation to ambulation, d | 2.0 (1.0–4.0) |
| Procedure-related complication | |
| Surgical site infection/chest wall abscess | 2 (1.1) |
| Empyema | 1 (0.6) |
| Implant breakage | 1 (0.6) |
| Implant dislodgement | 1 (0.6) |
| Nonprocedure-related pulmonary complication | 13 (7.3) |
| Tracheostomy | 0 (0.0) |
| Mortality | 0 (0.0) |
| Fractured Ribs ≤ 6 N = 85 | Fractured Ribs > 6 N = 92 | p | |
|---|---|---|---|
| Ventilator days, d | 0.0 (0.0–0.0) | 1.0 (0.0–6.0) | <0.01 |
| Postoperative ventilator days, d | 0.0 (0.0–0.0) | 0.0 (0.0–2.0) | <0.01 |
| Length of ICU stay, d | 0.0 (0.0–3.0) | 4.0 (0.0–11.0) | <0.01 |
| Postoperative ICU stay, d | 0.0 (0.0–2.0) | 2.0 (0.0–5.0) | <0.01 |
| Length of hospital stay, d | 10.0 (7.7–15.5) | 15.0 (11.0–21.8) | <0.01 |
| Postoperative hospital stay, d | 6.0 (4.5–10.0) | 9.0 (7.0–16.0) | <0.01 |
| Time from trauma to ambulation, d | 2.0 (1.0–5.0) | 4.0 (2.0–10.0) | <0.01 |
| Time from rib fixation to ambulation, d | 2.0 (1.0–3.0) | 2.0 (1.0–5.8) | <0.01 |
| Procedure-related complication | NA | ||
| Surgical site infection/chest wall abscess | 0 (0.0) | 2 (2.2) | |
| Empyema | 0 (0.0) | 1 (1.1) | |
| Implant breakage | 1 (1.2) | 0 (0.0) | |
| Implant dislodgement | 1 (1.2) | 0 (0.0) | |
| Nonprocedure-related pulmonary complication | 3 (3.5) | 10 (10.9) | 0.06 |
| Tracheostomy | 0 (0.0) | 0 (0.0) | NA |
| Mortality | 0 (0.0) | 0 (0.0) | NA |
| Variables | Unstandardized Coefficients | Standardized Coefficients Beta | t | Sig. | 95% CI for B | ||
|---|---|---|---|---|---|---|---|
| B | Std. Error | Lower | Upper | ||||
| GCS | −0.072 | 0.032 | −0.243 | −2.264 | 0.028 | −0.135 | −0.008 |
| ISS | 0.012 | 0.009 | 0.164 | 1.410 | 0.164 | −0.005 | 0.030 |
| Flail chest requiring mechanical ventilation | 0.492 | 0.206 | 0.271 | 2.387 | 0.020 | 0.079 | 0.904 |
| Time from trauma to SSRF | 0.053 | 0.023 | 0.248 | 2.302 | 0.025 | 0.007 | 0.099 |
| Video-assisted vs. Thoracotomy | −0.438 | 0.206 | −0.238 | −2.122 | 0.038 | −0.852 | −0.024 |
| Blood loss during SSRF | 0.001 | <0.001 | 0.196 | 1.700 | 0.095 | <0.001 | 0.001 |
| Number of ribs broken | 0.018 | 0.035 | 0.059 | 0.502 | 0.617 | −0.053 | 0.088 |
| Variables | Unstandardized Coefficients | Standardized Coefficients Beta | t | Sig. | 95% CI for B | ||
|---|---|---|---|---|---|---|---|
| B | Std. Error | Lower | Upper | ||||
| GCS | −0.075 | 0.027 | −0.225 | −2.736 | 0.008 | −0.129 | −0.020 |
| ISS | 0.022 | 0.007 | 0.279 | 3.110 | 0.003 | 0.008 | 0.037 |
| Bilateral vs. unilateral rib fractures | 0.379 | 0.196 | 0.177 | 1.935 | 0.057 | −0.011 | 0.768 |
| Flail chest requiring mechanical ventilation | 0.680 | 0.171 | 0.344 | 3.984 | <0.001 | 0.340 | 1.019 |
| Lung contusion/laceration | 0.123 | 0.150 | 0.074 | 0.825 | 0.412 | −0.174 | 0.421 |
| Time from trauma to SSRF | 0.052 | 0.019 | 0.223 | 2.784 | 0.007 | 0.015 | 0.089 |
| Video-assisted vs. Thoracotomy | −0.177 | 0.158 | −0.094 | −1.121 | 0.265 | −0.492 | 0.137 |
| Blood loss during SSRF | <0.001 | <0.001 | 0.082 | 0.948 | 0.346 | <0.001 | 0.001 |
| Number of ribs broken | −0.021 | 0.030 | −0.070 | −0.713 | 0.478 | −0.080 | 0.038 |
| Variables | Unstandardized Coefficients | Standardized Coefficients Beta | t | Sig. | 95% CI for B | ||
|---|---|---|---|---|---|---|---|
| B | Std. Error | Lower | Upper | ||||
| GCS | −0.049 | 0.023 | −0.145 | −2.107 | 0.037 | −0.096 | −0.003 |
| ISS | 0.023 | 0.005 | 0.366 | 4.636 | <0.001 | 0.013 | 0.032 |
| Bilateral vs. unilateral rib fractures | 0.012 | 0.117 | 0.007 | 0.104 | 0.917 | −0.219 | 0.243 |
| Presence of a flail segment radiologically | 0.095 | 0.089 | 0.080 | 1.071 | 0.286 | −0.081 | 0.271 |
| Flail chest requiring mechanical ventilation | 0.247 | 0.125 | 0.144 | 1.982 | 0.049 | 0.001 | 0.493 |
| Lung contusion/laceration | 0.036 | 0.085 | 0.030 | 0.431 | 0.667 | −0.131 | 0.204 |
| Time from trauma to SSRF | 0.019 | 0.010 | 0.117 | 1.873 | 0.063 | −0.001 | 0.039 |
| Video-assisted vs. Thoracotomy | −0.052 | 0.092 | −0.039 | −0.571 | 0.569 | −0.234 | 0.129 |
| Double lumen vs. Single lumen intubation | −0.083 | 0.083 | −0.064 | −1.005 | 0.316 | −0.247 | 0.080 |
| Number of surgically fixated rib fractures | 0.022 | 0.033 | 0.057 | 0.670 | 0.504 | −0.043 | 0.087 |
| Operation time | 0.001 | 0.001 | 0.112 | 1.370 | 0.173 | <0.001 | 0.003 |
| Blood loss during SSRF | <0.001 | <0.001 | 0.037 | 0.521 | 0.603 | <0.001 | <0.001 |
| Number of ribs broken | 0.007 | 0.019 | 0.032 | 0.378 | 0.706 | −0.030 | 0.044 |
| Variables | Univariate Model Results | Multivariate Model Results | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | |
| Age, y | 1.050 | 1.006–1.095 | 0.025 | 1.097 | 1.025–1.173 | 0.007 |
| GCS | 0.662 | 0.541–0.810 | <0.001 | 0.648 | 0.499–0.843 | 0.001 |
| Flail chest requiring mechanical ventilation | 8.904 | 2.707–29.286 | <0.001 | 4.643 | 0.748–28.827 | 0.135 |
| Number of surgically fixated rib fractures | 1.416 | 1.012–1.982 | 0.042 | 1.514 | 0.667–3.438 | 0.322 |
| Operation time | 1.009 | 1.001–1.017 | 0.023 | 1.004 | 0.990–1.018 | 0.600 |
| Blood loss during SSRF | 1.002 | 1.000–1.005 | 0.018 | 1.002 | 0.999–1.004 | 0.176 |
| Number of ribs broken | 1.099 | 0.903–1.337 | 0.347 | 0.734 | 0.444–1.211 | 0.226 |
| Video-assisted vs. Thoracotomy | 0.569 | 0.176–1.833 | 0.344 | 0.232 | 0.038–1.417 | 0.113 |
| SSRF (−) N = 106 | SSRF (+) N = 106 | p | |
|---|---|---|---|
| Age, y | 58.5 (43.5–70.0) | 56.5 (46.8–64.3) | 0.37 |
| Male/Female | 69/37 | 64/42 | 0.48 |
| Transferal | 32 (30.2) | 35 (33.0) | 0.66 |
| Charlson Comorbidity Index | 2.0 (0.0–4.0) | 2.0 (0.0–3.0) | 0.50 |
| Trauma mechanism | 0.50 | ||
| Vehicle-to-vehicle collision | 59 (55.7) | 68 (64.2) | |
| Vehicle-to-pedestrian collision | 4 (3.8) | 5 (4.7) | |
| Single-vehicle collision | 25 (23.6) | 17 (16.0) | |
| Fall | 18 (17.0) | 16 (15.1) | |
| Crush | 0 (0.0) | 0 (0.0) | |
| Assault | 0 (0.0) | 0 (0.0) | |
| Glasgow Coma Scale | 15.0 (15.0–15.0) | 15.0 (15.0–15.0) | 0.95 |
| Injury Severity Score | 17.0 (13.0–22.5) | 17.0 (13.0–22.0) | 0.30 |
| Head/Neck | |||
| Median (IQR) | 0.0 (0.0–2.0) | 0.0 (0.0–2.0) | 0.51 |
| AIS ≥ 3 | 23 (21.7) | 24 (22.6) | 0.87 |
| Face | |||
| Median (IQR) | 0.0 (0.0–0.0) | 0.0 (0.0–0.0) | 0.34 |
| AIS ≥ 3 | 1 (0.9) | 0 (0.0) | >0.99 |
| Thorax | |||
| Median (IQR) | 3.0 (3.0–3.0) | 3.0 (3.0–3.0) | 0.29 |
| AIS ≥ 3 | 99 (93.4) | 106 (100.0) | 0.02 |
| Abdomen | |||
| Median (IQR) | 0.0 (0.0–2.0) | 0.0 (0.0–2.0) | 0.49 |
| AIS ≥ 3 | 15 (14.2) | 12 (11.3) | 0.54 |
| Extremity | |||
| Median (IQR) | 2.0 (0.0–2.0) | 2.0 (0.0–2.0) | 0.82 |
| AIS ≥ 3 | 20 (18.9) | 11 (10.4) | 0.12 |
| External | |||
| Median (IQR) | 0.0 (0.0–1.0) | 0.0 (0.0–0.0) | 0.60 |
| AIS ≥ 3 | 0 (0.0) | 0 (0.0) | NA |
| Number of ribs broken | 5.0 (3.0–8.0) | 6.0 (5.0–8.0) | 0.02 |
| Fractured side | 0.24 | ||
| Unilateral | 88 (83.0) | 94 (88.7) | |
| Bilateral | 18 (17.0) | 12 (11,3) | |
| Presence of a flail segment radiologically | 35 (33.0) | 35 (33.0) | NA |
| Requiring mechanical ventilation | 10 (9.4) | 6 (5.7) | 0.30 |
| Associated intrathoracic injury | |||
| Lung contusion/laceration | 50 (47.2) | 39 (36.8) | 0.13 |
| Pneumothorax | 44 (41.5) | 57 (53.8) | 0.07 |
| Hemothorax | 72 (67.9) | 83 (78.3) | 0.09 |
| Cardiac injury | 3 (2.8) | 1 (0.9) | 0.62 |
| Great vessels | 2 (1.9) | 1 (0.9) | >0.99 |
| Soft tissue | 13 (12.3) | 18 (17.0) | 0.33 |
| Concurrent sternal fracture | 2 (1.9) | 4 (3.8) | 0.69 |
| Concurrent ipsilateral clavicular fracture | 38 (35.8) | 45 (42.5) | 0.33 |
| Concurrent ipsilateral scapular fracture | 17 (16.0) | 20 (18.9) | 0.59 |
| SSRF (−) N = 106 | SSRF (+) N = 106 | p | |
|---|---|---|---|
| Ventilator days, d | 0.0 (0.0–9.8) | 2.0 (0.0–6.0) | 0.877 |
| N = 52 | N = 52 | ||
| Length of ICU stay, d | 3.0 (0.0–7.5) | 3.0 (0.0–8.0) | 0.914 |
| N = 69 | N = 69 | ||
| Length of hospital stay, d | 8.0 (5.0–20.0) | 11.5 (8.0–18.0) | 0.195 |
| Time from trauma to ambulation, d | 4.0 (3.0–10.0) | 3.0 (1.0–6.0) | 0.002 |
| Nonprocedure-related pulmonary complication | 18 (17.0) | 7 (6.6) | 0.019 |
| Tracheostomy | 4 (3.8) | 0 (0.0) | 0.121 |
| Mortality | 1 (0.9) | 0 (0.0) | >0.999 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tang, W.-R.; Chang, C.-C.; Wang, C.-J.; Yang, T.-H.; Hung, K.-S.; Wu, C.-H.; Yen, Y.-T.; Tseng, Y.-L.; Shan, Y.-S. Tailored Surgical Stabilization of Rib Fractures Matters More Than the Number of Fractured Ribs. J. Pers. Med. 2022, 12, 1844. https://doi.org/10.3390/jpm12111844
Tang W-R, Chang C-C, Wang C-J, Yang T-H, Hung K-S, Wu C-H, Yen Y-T, Tseng Y-L, Shan Y-S. Tailored Surgical Stabilization of Rib Fractures Matters More Than the Number of Fractured Ribs. Journal of Personalized Medicine. 2022; 12(11):1844. https://doi.org/10.3390/jpm12111844
Chicago/Turabian StyleTang, Wen-Ruei, Chao-Chun Chang, Chih-Jung Wang, Tsung-Han Yang, Kuo-Shu Hung, Chun-Hsien Wu, Yi-Ting Yen, Yau-Lin Tseng, and Yan-Shen Shan. 2022. "Tailored Surgical Stabilization of Rib Fractures Matters More Than the Number of Fractured Ribs" Journal of Personalized Medicine 12, no. 11: 1844. https://doi.org/10.3390/jpm12111844
APA StyleTang, W.-R., Chang, C.-C., Wang, C.-J., Yang, T.-H., Hung, K.-S., Wu, C.-H., Yen, Y.-T., Tseng, Y.-L., & Shan, Y.-S. (2022). Tailored Surgical Stabilization of Rib Fractures Matters More Than the Number of Fractured Ribs. Journal of Personalized Medicine, 12(11), 1844. https://doi.org/10.3390/jpm12111844







