Conventional and Virtual Reality Mirror Therapies in Upper Obstetric Brachial Palsy: A Randomized Pilot Study
Abstract
1. Introduction
2. Materials and Methods
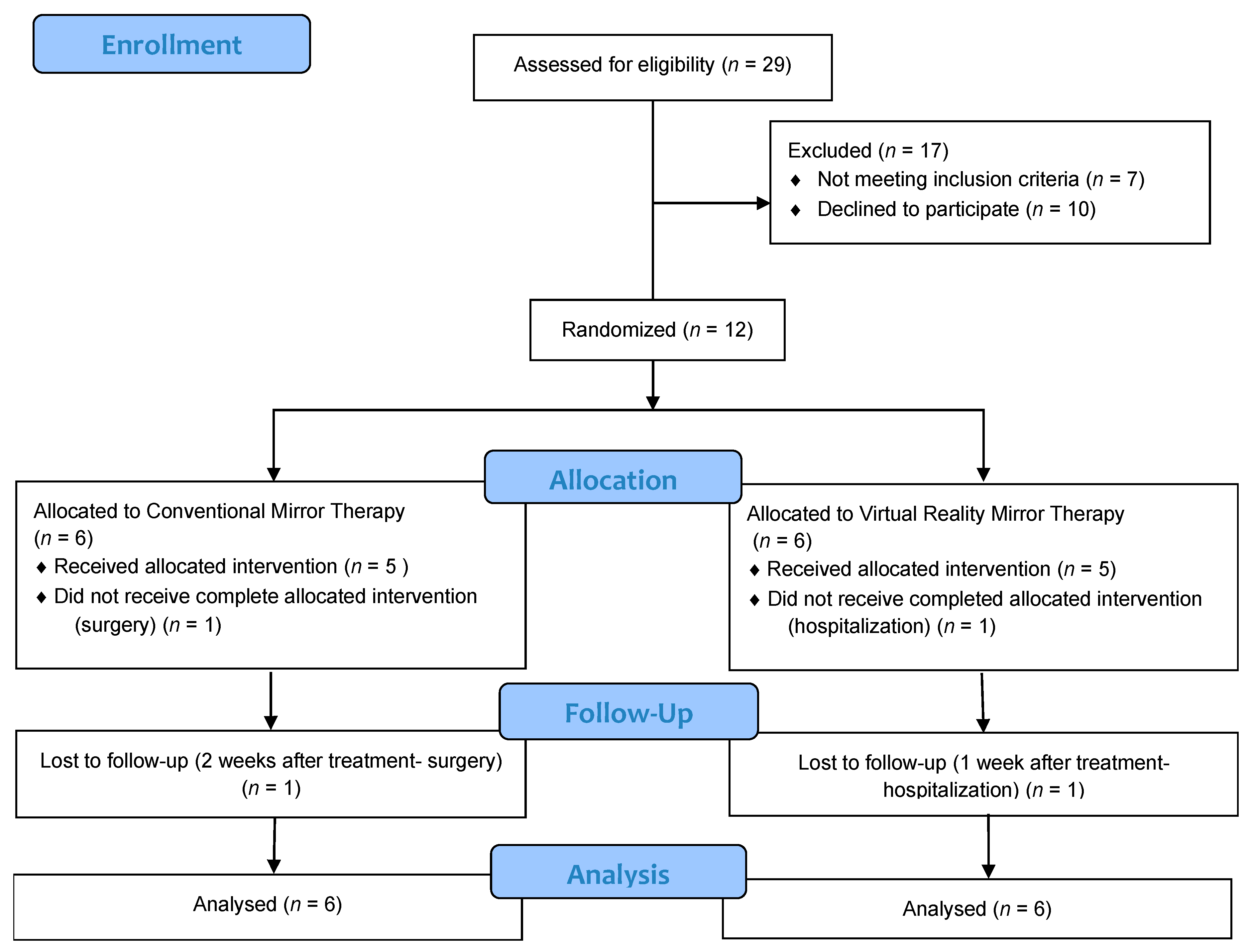
2.1. Participants and Recruitment
2.2. Inclusion and Exclusion Criteria
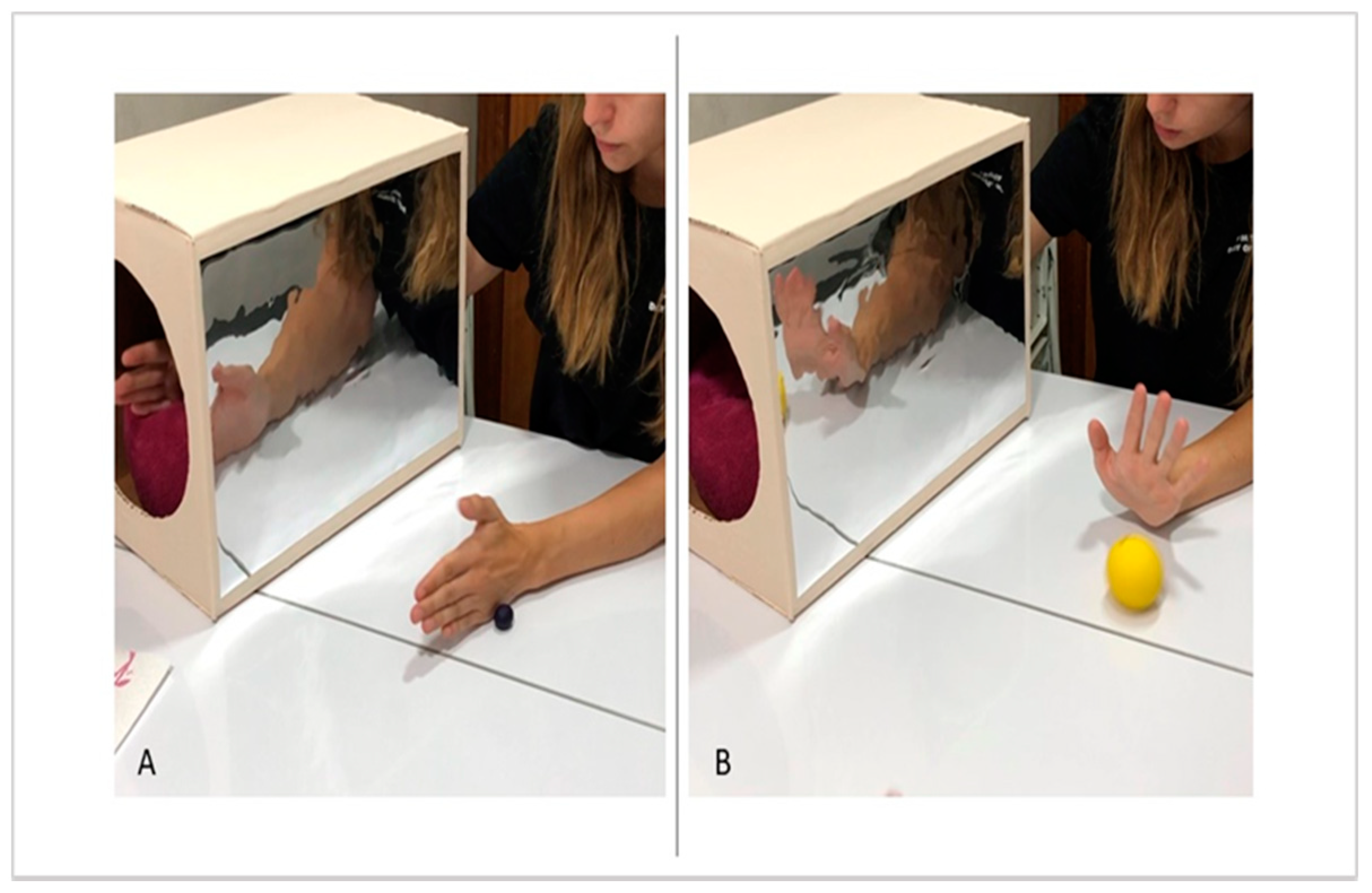
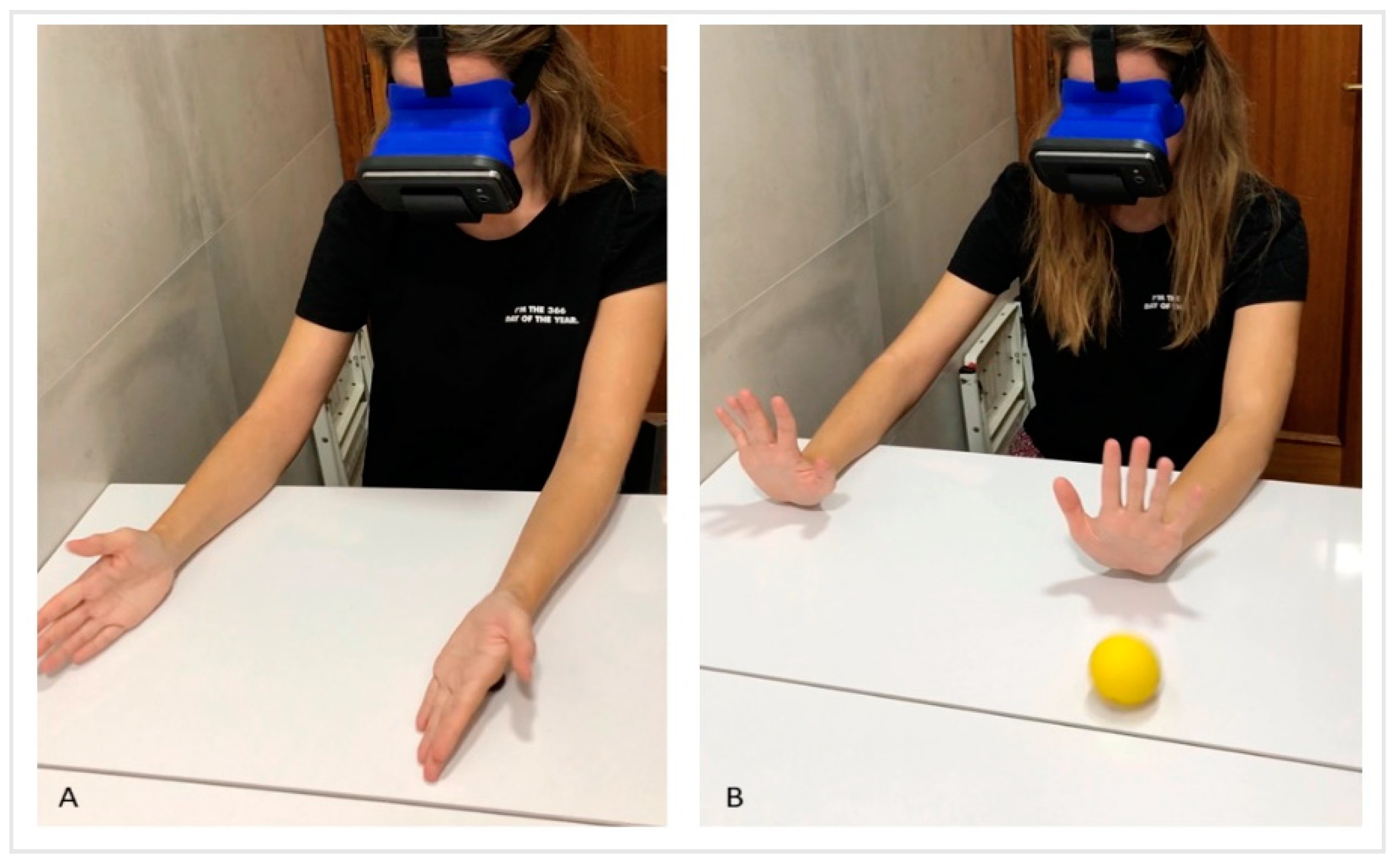
2.3. Intervention and Follow-Up
2.4. Outcome Measures
2.4.1. Primary Measures: Affected Upper Limb Spontaneous Use
2.4.2. Secondary Measures: Quality of Life
2.5. Statistical Analysis
3. Results
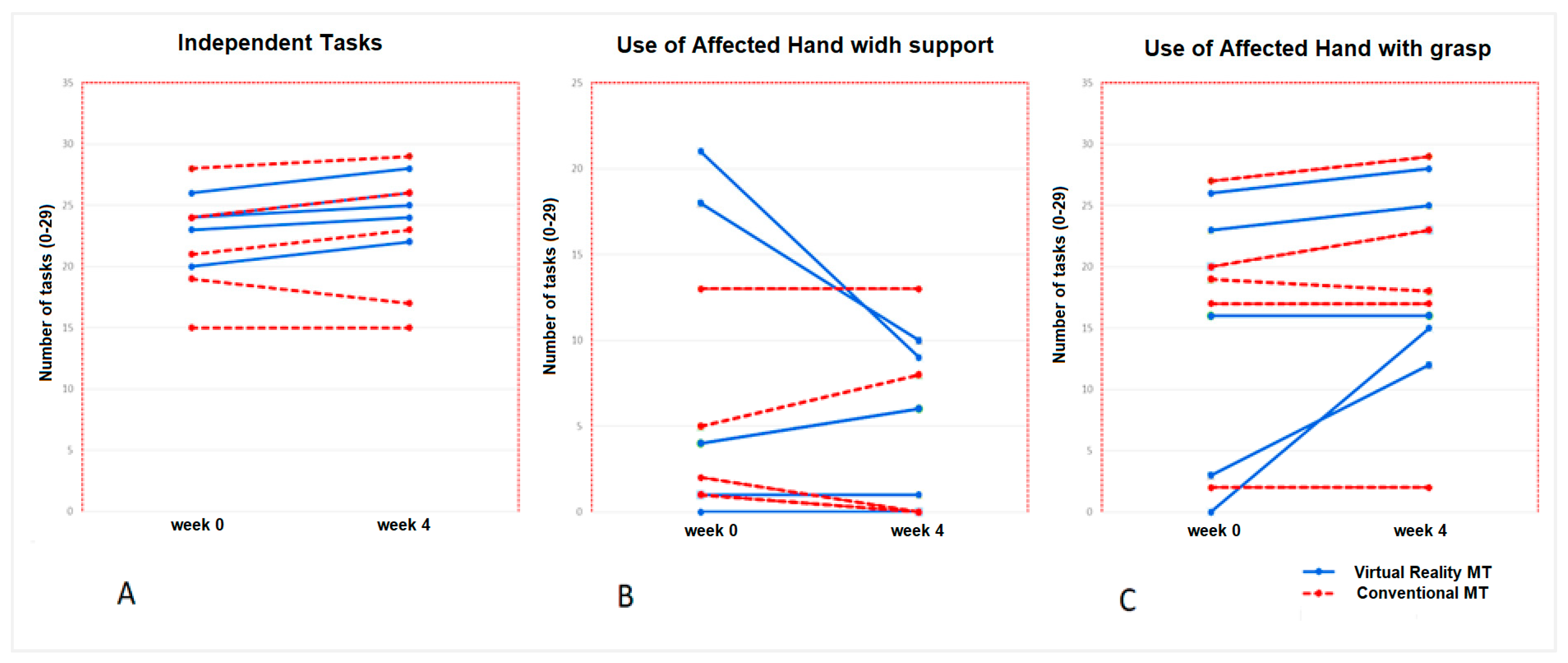
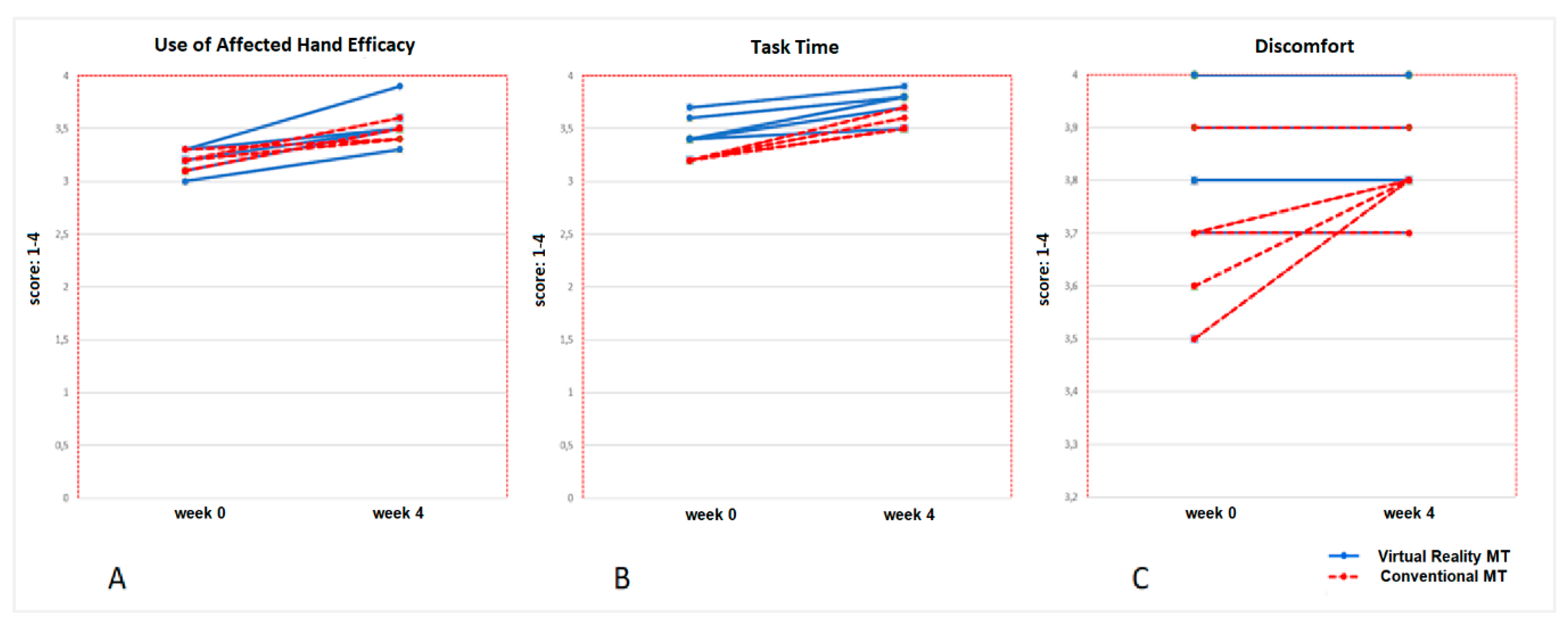
3.1. Primary Results: Spontaneous Use of the Affected Upper Limb (Measured with CHEQ)
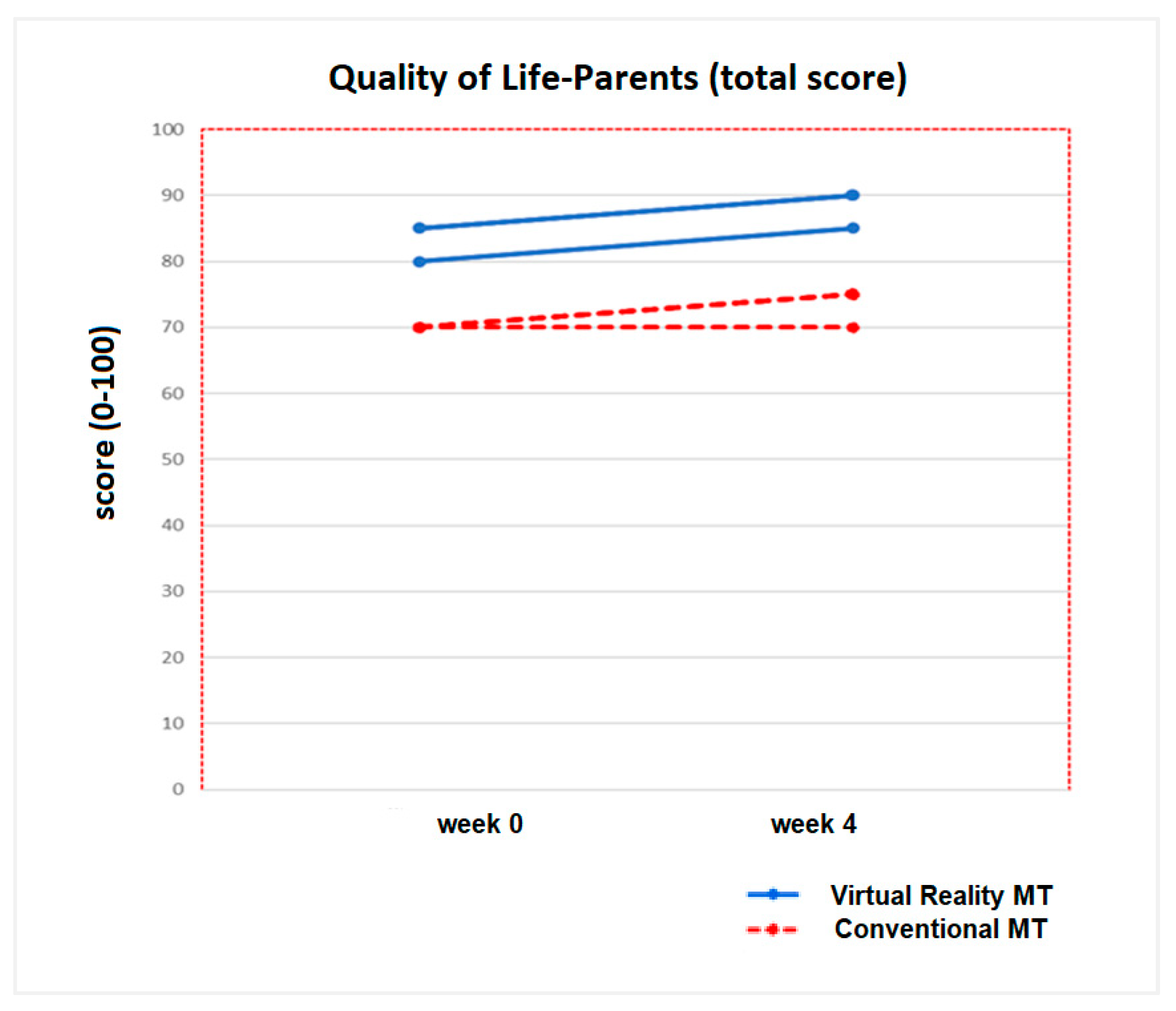
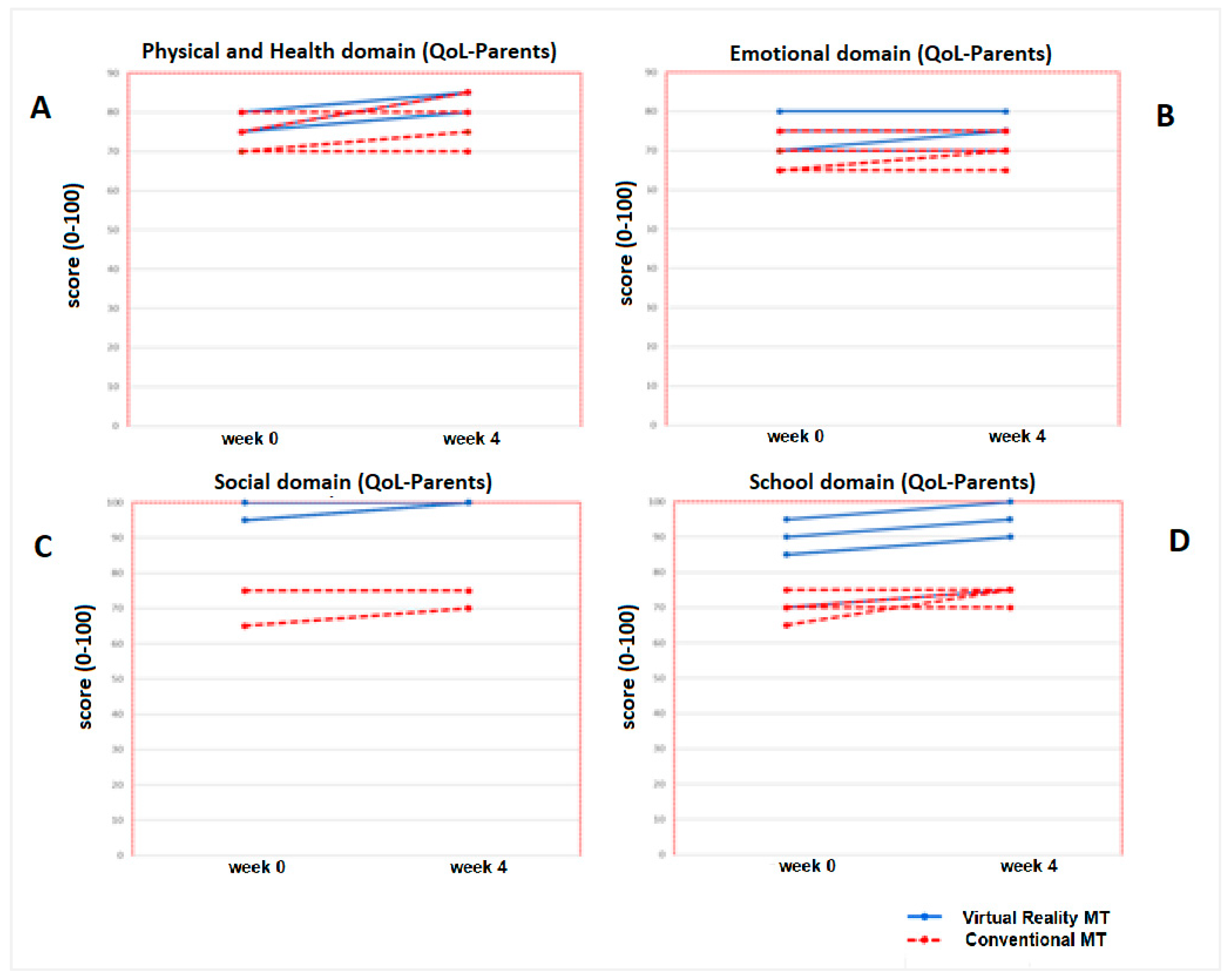
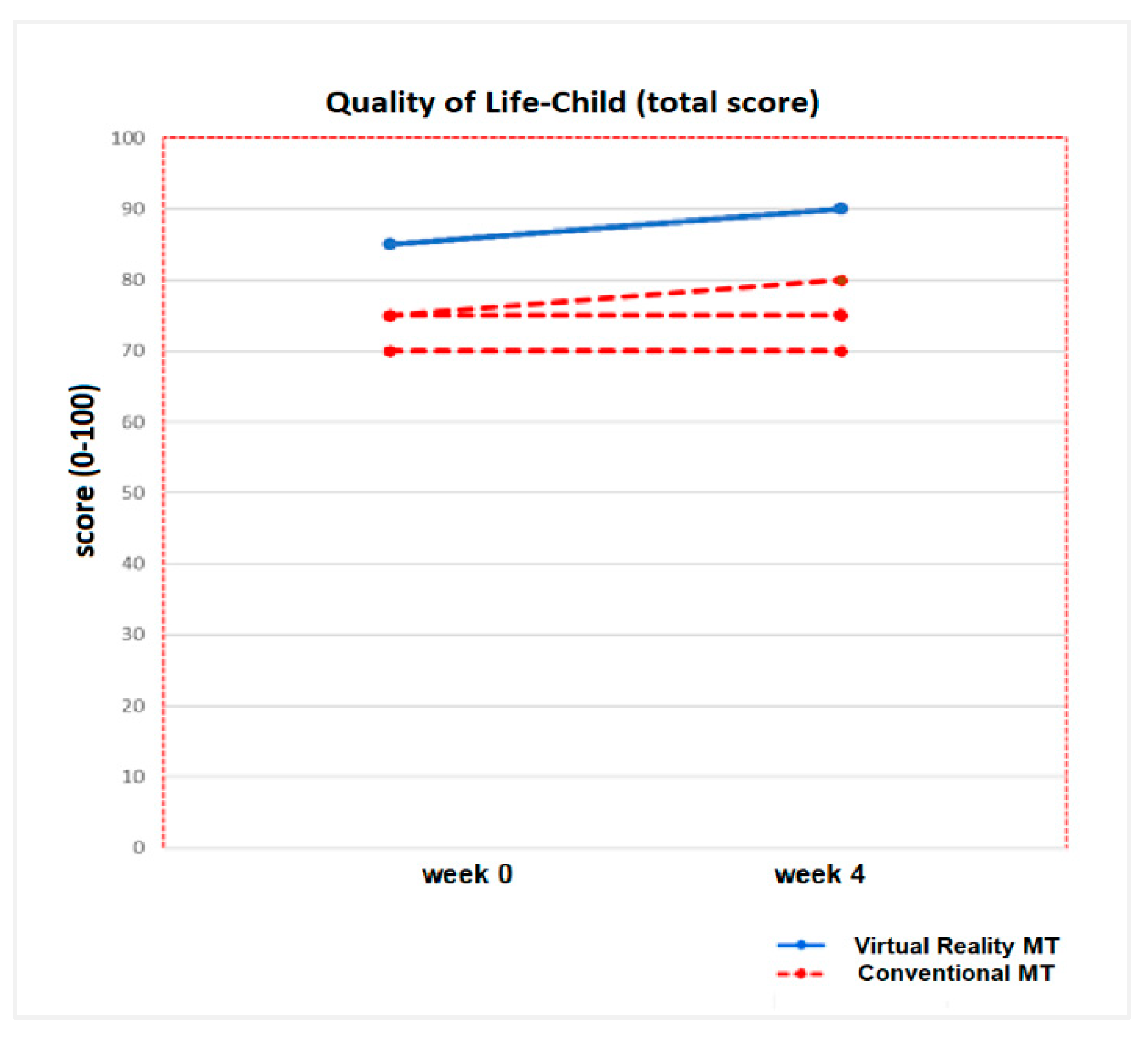
3.2. Secondary Results: Quality of Life (Measured with PedsQL TM 4.0)
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Galbiatti, J.A.; Cardoso, F.L.; Galbiatti, M.G.P. Obstetric Paralysis: Who is to blame? A systematic literature review. Rev. Bras. Ortop. 2020, 55, 139–146. [Google Scholar]
- Zafeiriou, D.I.; Psychogiou, K. Obstetrical brachial plexus palsy. Pediatr. Neurol. 2008, 38, 235–242. [Google Scholar] [CrossRef] [PubMed]
- Srofenyoh, E.K.; Seffah, J.D. Prenatal, labor and delivery characteristics of mothers with macrosomic babies. Int. J. Gynaecol. Obstet. 2006, 93, 49–50. [Google Scholar] [CrossRef] [PubMed]
- Piasek, G.; Starzewski, J.; Chil, A.; Wrona-Cyranowska, A. Analysis of labour and perinatal complications in case of foetus weight over 4000 g. Wiad Lek. 2006, 59, 326–331. [Google Scholar] [PubMed]
- Gilbert, A. Long-term evaluation of brachial plexus surgery in obstetrical palsy. Hand Clin. 1995, 11, 583–594. [Google Scholar]
- Strömbeck, C. Long-term follow-up of children with obstetric brachial plexus palsy I: Functional aspects. Dev. Med. Child. Neurol. 2007, 49, 198–203. [Google Scholar] [CrossRef]
- Al-Quattan, M.M.; Clarke, H.M. A historical note on the intermediate type of obstetrical brachial plexus palsy. J. Hand Surg. 1994, 19, 673. [Google Scholar]
- Shenaq, S.M.; Berzin, E.; Lee, R.; Laurent, J.P.; Nath, R.; Nelson, M.R. Brachial plexus birth injuries and current management. Clin. Plast. Surg. 1998, 25, 527–536. [Google Scholar] [CrossRef]
- Narakas, A.O. Injuries to the brachial plexus. In The Pediatric Upper Extremity: Diagnosis and Management; Bora, F.W., Jr., Ed.; W.B. Saunders: Philadelphia, PA, USA, 1986; pp. 247–258. [Google Scholar]
- Narakas, A.O. Obstetrical brachial plexus injuries. In The Paralysed Hand: The Hand and Upper Limb; Lamb, D.W., Ed.; Churchill Livingstone: Edinburgh, UK, 1987; Volume 2, pp. 116–135. [Google Scholar]
- Gherman, R.B.; Ouzounian, J.G.; Goodwin, T.M. Obstetric maneuvers for shoulder dystocia and associated fetal morbidity. Am. J. Obstet. Gynecol. 1998, 178, 1126–1130. [Google Scholar] [CrossRef]
- Ho, E.S.; Curtis, C.G.; Clarke, H.M. Pediatric Evaluation of Disability Inventory: Its application to children with obstetric brachial plexus palsy. J. Hand Surg. Am. 2006, 31, 197–202. [Google Scholar] [CrossRef]
- O’Berry, P.; Brown, M.; Phillips, L.; Evans, S.H. Obstetrical Brachial Plexus Palsy. Curr. Probl. Pediatr. Adolesc. Health Care 2017, 47, 151–155. [Google Scholar] [CrossRef] [PubMed]
- Shah, A.S.; Kalish, L.A.; Bae, D.S.; Peljovich, A.E.; Cornwall, R.; Bauer, A.S.; Waters, P.M. Early Predictors of Microsurgical Reconstruction in Brachial Plexus Birth Palsy. Iowa Orthop. J. 2019, 39, 37–43. [Google Scholar] [PubMed]
- Palomo, R.; Sánchez, R. Physiotherapy applied to the upper extremity in 0 to 10-year-old children with obstetric brachial palsy: A systematic review]. Rev. Neurol. 2020, 71, 1–10. [Google Scholar] [PubMed]
- Buesch, F.E.; Schlaepfer, B.; de Bruin, E.D.; Wohlrab, G.; Ammann-Reiffer, C.; Meyer-Heim, A. Constraint-induced movement therapy for children with obstetric brachial plexus palsy: Two single-case series. Int. J. Rehabil. Res. 2010, 33, 187–192. [Google Scholar] [CrossRef]
- Vaz, D.V.; Mancini, M.C.; do Amaral, M.F.; de Brito Brandão, M.; de França Drummond, A.; da Fonseca, S.T. Clinical changes during an intervention based on constraint-induced movement therapy principles on use of the affected arm of a child with obstetric brachial plexus injury: A case report. Occup. Ther. Int. 2010, 17, 159–167. [Google Scholar] [CrossRef]
- Donnelly, V.; Foran, A.; Murphy, J.; McParland, P.; Keane, D.; O’Herlihy, C. Neonatal brachial plexus palsy: An unpredictable injury. Am. J. Obstet. Gynecol. 2002, 187, 1209–1212. [Google Scholar] [CrossRef]
- Arad, E.; Stephens, D.; Curtis, C.G.; Clarke, H.M. Botulinum toxin for the treatment of motor imbalance in obstetrical brachial plexus palsy. Plast. Reconstr. Surg. 2013, 131, 1307–1315. [Google Scholar] [CrossRef]
- Santamato, A.; Panza, F.; Ranieri, M.; Fiore, P. Effect of botulinum toxin type A and modified constraint-induced movement therapy on motor function of upper limb in children with obstetrical brachial plexus palsy. Childs Nerv. Syst. 2011, 27, 2187–2192. [Google Scholar] [CrossRef]
- Kendall, B.E. Some directions in ecological theory. Ecology 2015, 96, 3117–3125. [Google Scholar] [CrossRef]
- Tzeng, Y.F.; Gau, B.S. Nursing care of a school-age child with asthma: An ecological system theory approach. Hu Li Za Zhi 2012, 59, 96–103. [Google Scholar]
- Ramachandran, V.S.; Altschuler, E.L. The use of visual feedback, in particular mirror visual feedback, in restoring brain function. Brain 2009, 132, 1693–1710. [Google Scholar] [CrossRef] [PubMed]
- Thieme, H.; Mehrholz, J.; Pohl, M.; Behrens, J.; Dohle, C. Mirror therapy for improving motor function after stroke. Cochrane Database Syst. Rev. 2018, 7, CD008449. [Google Scholar] [CrossRef] [PubMed]
- Gygax, M.J.; Schneider, P.; Newman, C.J. Mirror therapy in children with hemiplegia: A pilot study. Dev. Med. Child. Neurol. 2011, 53, 473–476. [Google Scholar] [CrossRef] [PubMed]
- Grunt, S.; Newman, C.J.; Saxer, S.; Steinlin, M.; Weisstanner, C.; Kaelin-Lang, A. The Mirror Illusion Increases Motor Cortex Excitability in Children with and without Hemiparesis. Neurorehabil. Neural Repair 2017, 31, 280–289. [Google Scholar] [CrossRef] [PubMed]
- Rizzolatti, G.; Sinigaglia, C. The mirror mechanism: A basic principle of brain function. Nat. Rev. Neurosci. 2016, 17, 757–765. [Google Scholar] [CrossRef]
- Buccino, G.; Solodkin, A.; Small, S.L. Functions of the mirror neuron system: Implications for neurorehabilitation. Cogn. Behav. Neurol. 2006, 19, 55–63. [Google Scholar] [CrossRef]
- Pomeroy, V.M.; Clark, C.A.; Miller, J.S.G.; Baron, J.C.; Markus, H.S.; Tallis, R.C. The potential for utilizing the “mirror neurone system” to enhance recovery of the severely affected upper limb early after stroke: A review and hypothesis. Neurorehabil. Neural Repair 2005, 19, 4–13. [Google Scholar] [CrossRef]
- Rizzolatti, G.; Fogassi, L.; Gallese, V. Neurophysiological mechanisms underlying the understanding and imitation of action. Nat. Rev. Neurosci. 2001, 2, 661–670. [Google Scholar] [CrossRef]
- Kilner, J.M.; Paulignan, Y.; Blakemore, S.J. An interference effect of observed biological movement on action. Curr. Biol. 2003, 13, 522–525. [Google Scholar] [CrossRef]
- Calvo-Merino, B.; Grèzes, J.; Glaser, D.E.; Passingham, R.E.; Haggard, P. Seeing or doing? Influence of visual and motor familiarity in action observation. Curr. Biol. 2006, 16, 1905–1910. [Google Scholar] [CrossRef]
- Sgandurra, G.; Ferrari, A.; Cossu, G.; Guzzetta, A.; Fogassi, L.; Cioni, G. Randomized trial of observation and execution of upper extremity actions versus action alone in children with unilateral cerebral palsy. Neurorehabil. Neural Repair 2013, 27, 808–815. [Google Scholar] [CrossRef]
- Buccino, G.; Molinaro, A.; Ambrosi, C.; Arisi, D.; Mascaro, L.; Pinardi, C.; Rossi, A.; Gasparotti, R.; Fazzi, E.; Galli, J. Action Observation Treatment Improves Upper Limb Motor Functions in Children with Cerebral Palsy: A Combined Clinical and Brain Imaging Study. Neural. Plast. 2018, 2018, 4843985. [Google Scholar] [CrossRef]
- Nuara, A.; Avanzini, P.; Rizzolatti, G.; Fabbri-Destro, M. Efficacy of a home-based platform for child-to-child interaction on hand motor function in unilateral cerebral palsy. Dev. Med. Child Neurol. 2019, 61, 1314–1322. [Google Scholar] [CrossRef] [PubMed]
- Galvin, J.; McDonald, R.; Catroppa, C.; Anderson, V. Does intervention using virutal reality improve upper limb function in children with neurological impairment: A systematic review of the evidence. Brain Inj. 2011, 25, 435–442. [Google Scholar] [CrossRef] [PubMed]
- Sisto, S.A.; Forrest, G.F.; Glendinning, D. Virtual reality applications for motor rehabilitation after stroke. Top. Stroke Rehabil. 2002, 8, 11–23. [Google Scholar] [CrossRef] [PubMed]
- Broeren, J.; Bjorkdahl, A.; Pascher, R.; Rydmark, M. Virtual reality and haptics as an assessment device in the post acute phase after stroke. Cyber Psychol. Behav. 2002, 25, 207–211. [Google Scholar] [CrossRef]
- Crosbie, J.H.; Lennon, S.; Basford, J.R.; McDonough, S.M. Virtual reality in stroke rehabilitation: Still more virtual than real. Disabil. Rehabil. 2007, 29, 1139–1146. [Google Scholar] [CrossRef]
- El-Shamy, S.; Alsharif, R. Effect of virtual reality versus conventional physiotherapy on upper extremity function in children with obstetric brachial plexus injury. J. Musculoskelet Neuronal. Interact. 2017, 17, 319–326. [Google Scholar]
- Chen, Y.P.; Lee, S.Y.; Howard, A.M. Effect of virtual reality on upper extremity function in children with cerebral palsy: A meta-analysis. Pediatr. Phys. Ther. 2014, 26, 289–300. [Google Scholar] [CrossRef]
- Olivieri, I.; Chiappedi, M.; Meriggi, P.; Mazzola, M.; Grandi, A.; Angelini, L. Rehabilitation of children with hemiparesis: A pilot study on the use of virtual reality. Biomed. Res. Int. 2013, 2013, 1–5. [Google Scholar] [CrossRef]
- Kassee, C.; Hunt, C.; Holmes, M.W.R.; Lloyd, M. Home-based Nintendo Wii training to improve upper-limb function in children ages 7 to 12 with spastic hemiplegic cerebral palsy. J. Pediatr. Rehabil. Med. 2017, 10, 145–154. [Google Scholar] [CrossRef]
- World Health Organization. International Classification of Functioning, Disability, and Health; World Health Organization: Geneva, Switzerland, 2001. [Google Scholar]
- Gilmore, R.; Sakzewski, L.; Boyd, R. Upper limb activity measures for 5- to 16-year-old children with congenital hemiplegia: A systematic review. Dev. Med. Child Neurol. 2010, 52, 14–21. [Google Scholar] [CrossRef]
- Wagner, L.V.; Davids, J.R. Assessment tools and classification systems used for the upper extremity in children with cerebral palsy. Clin. Orthop. Relat. Res. 2012, 470, 1257–1271. [Google Scholar] [CrossRef]
- Bruchez, R.; Jequier Gygax, M.; Roches, S.; Fluss, J.; Jacquier, D.; Ballabeni, P.; Grunt, S.; Newman, C.J. Mirror therapy in children with hemiparesis: A randomized observer-blinded trial. Dev. Med. Child Neurol. 2016, 58, 970–978. [Google Scholar] [CrossRef]
- Ferre, C.L.; Brandão, M.; Surana, B.; Dew, A.P.; Moreau, N.G.; Gordon, A.M. Caregiver-directed home-based intensive bimanual training in young children with unilateral spastic cerebral palsy: A randomized trial. Dev. Med. Child Neurol. 2017, 59, 497–504. [Google Scholar] [CrossRef]
- Sköld, A.; Hermansson, L.N.; Krumlinde-Sundholm, L.; Eliasson, A.C. Development and evidence of validity for the Children’s Hand-use Experience Questionnaire (CHEQ). Dev. Med. Child Neurol. 2011, 53, 436–442. [Google Scholar] [CrossRef]
- Ryll, U.C.; Eliasson, A.C.; Bastiaenen, C.H.; Green, D. To Explore the Validity of Change Scores of the Children’s Hand-Use Experience Questionnaire (CHEQ) in Children with Unilateral Cerebral Palsy. Phys. Occup. Ther. Pediatr. 2019, 39, 168–180. [Google Scholar] [CrossRef]
- Varni, J. The PedsQL TM. (Adaptación española). 1998. Available online: https://www.pedsql.org/about_pedsql.html (accessed on 7 August 2020).
- Tantilipikorn, P.; Watter, P.; Prasertsukdee, S. Comparison between utility of the Thai pediatric quality of life inventory 4.0 generic core scales and 3.0 cerebral palsy module. Int. J. Rehabil. Res. 2013, 36, 21–29. [Google Scholar] [CrossRef]
- Yang, X.; Xiao, N.; Yan, J. The PedsQL in Pediatric cerebral palsy: Reliability and validity of the Chinese version Pediatric Quality of life inventory 4.0 Generic core scales and 3.0 cerebral palsy module. Qual. Life Res. 2011, 20, 243–252. [Google Scholar] [CrossRef]
- Sarmento, L.A.; Pinto, J.S.; da Silva, A.P.; Cabral, C.M.; Chiavegato, L.D. Effect of conventional physical therapy and pilates in functionality, respiratory muscle strength and ability to exercise in hospitalized chronic renal patients: A randomized controlled trial. Clin. Rehabil. 2017, 31, 508. [Google Scholar] [CrossRef]
- Youssef, E.F.; Elhameed, A.A. Supervised versus home exercise training programs on functional balance in older subjects. Malays. J. Med. Sci. 2016, 23, 83. [Google Scholar] [CrossRef] [PubMed]
- Poulsen, A.A.; Rodger, S.; Ziviani, J.M. Understanding children’s motivation from a self-determination theoretical perspective: Implications for practice. Aust. Occup. Ther. J. 2006, 53, 78–86. [Google Scholar] [CrossRef]
- Deci, E.L.; Ryan, R.M. Facilitating optimal motivation and psychological well-being across life’s domains. Can. Psychol. 2008, 49, 14–23. [Google Scholar] [CrossRef]
- Miller, L.; Ziviani, J.; Ware, R.S.; Boyd, R.N. Mastery Motivation as a predictor of occupational performance following upper limb intervention for school-aged children with congenital hemiplegia. Dev. Med. Child Neurol. 2014, 56, 976–983. [Google Scholar] [CrossRef]
- Inguaggiato, E.; Sgandurra, G.; Perazza, S.; Guzzetta, A.; Cioni, G. Brain reorganization following intervention in children with congenital hemiplegia: A systematic review. Neural Plast. 2013, 2013, 1–8. [Google Scholar] [CrossRef]
- Chiang, V.C.L.; Lo, K.H.; Choi, K.S. Rehabilitation of activities of daily living in virtual environments with intuitive user interface and force feedback. Disabil. Rehabil. Assist. Technol. 2017, 12, 672–680. [Google Scholar] [CrossRef]
- Golomb, M.R.; Mcdonald, B.C.; Warden, S.J.; Yonkman, J.; Saykin, A.J.; Shirley, B.; Huber, M.; Rabin, B.; Abdelbaky, M.; Nwosu, M.E.; et al. In-Home Virtual Reality Videogame Telerehabilitation in Adolescents with Hemiplegic Cerebral Palsy. Arch. Phys. Med. Rehabil. 2010, 91, 1–8.e1. [Google Scholar] [CrossRef]
- You, S.H.; Jang, S.H.; Kim, Y.H.; Kwon, Y.H.; Barrow, I.; Hallett, M. Cortical reorganization induced by virtual reality therapy in a child with hemiparetic cerebral palsy. Dev. Med. Child Neurol. 2005, 47, 628–635. [Google Scholar] [CrossRef]
- Majnemer, A.; Shevell, M.; Law, M.; Poulin, C.; Rosenbaum, P. Reliability in the ratings of quality of life between parents and their children of school age with cerebral palsy. Qual. Life Res. 2008, 17, 1163–1171. [Google Scholar] [CrossRef]
- Upton, P.; Lawford, J.; Eiser, C. Parent-child agreement across child health-related quality of life instruments: A review of the literature. Qual. Life Res. 2008, 17, 895–913. [Google Scholar] [CrossRef]
- Eiser, C.; Morse, R. Can parents rate their child’s health-related quality of life? Results from a systematic review. Qual. Life Res. 2001, 10, 347–357. [Google Scholar] [CrossRef] [PubMed]
- Theunissen, N.C.M.; Vogels, T.G.C.; Koopman, H.M.; Verrips, G.H.; Zwinderman, A.H.; Verloove-Vanhorick, S.P.; Wit, J.M. The proxy problem: Child report versus parent report in health-related quality of life research. Qual. Life Res. 1998, 7, 387–397. [Google Scholar] [CrossRef] [PubMed]
- Ferre, C.L.; Gordon, A.M. Coaction of individual and environmental factors: A review of intensive therapy paradigms for children with unilateral spastic cerebral palsy. Dev. Med. Child Neurol. 2017, 59, 1139–1145. [Google Scholar] [CrossRef] [PubMed]
- Hadders-Algra, M.; Boxum, A.G.; Hielkema, T.; Hamer, E.G. Effect of early intervention in infants at very high risk of cerebral palsy: A systematic review. Dev. Med. Child Neurol. 2017, 59, 246–258. [Google Scholar] [CrossRef] [PubMed]

| Forearm Prone-Supination Exercises | |
|---|---|
| Sound Bottle | -Material: fill a bottle with beads, chickpeas, lentils, or grains of rice, stick chopsticks so that it takes longer to move the inner contents/rain stick. -Exercise: make forearm prono-supination so that the content falls from one side to the other inside the bottle.  |
| Cookies | -Material: small plasticine balls. -Exercise: with your forearm resting on the table, from a neutral prone-supination position, make supination to crush the plasticine balls with the back of your hand.  |
| The Tower | -Material: small plasticine balls. -Exercise: with your forearm in supination resting on the table, gradually place the plasticine balls on the palm of your hand to form a tower. 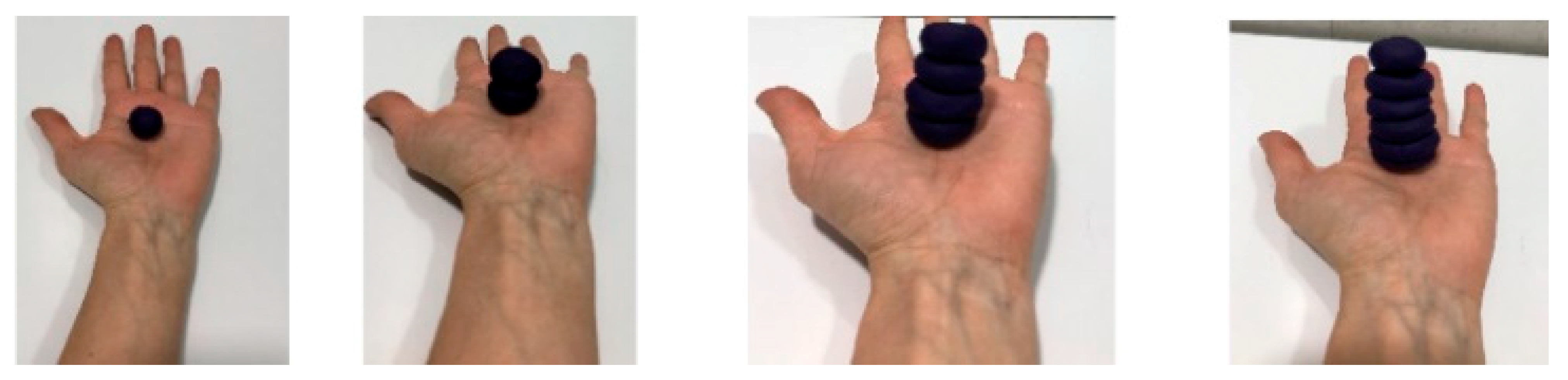 |
| Flexo-Extension Wrist Exercises | |
| Ball Wheel | -Material: small ball, i.e.,: tennis ball. -Exercise: with your forearm resting on the table, slowly throw the ball and try to stop it by making wrist extension. 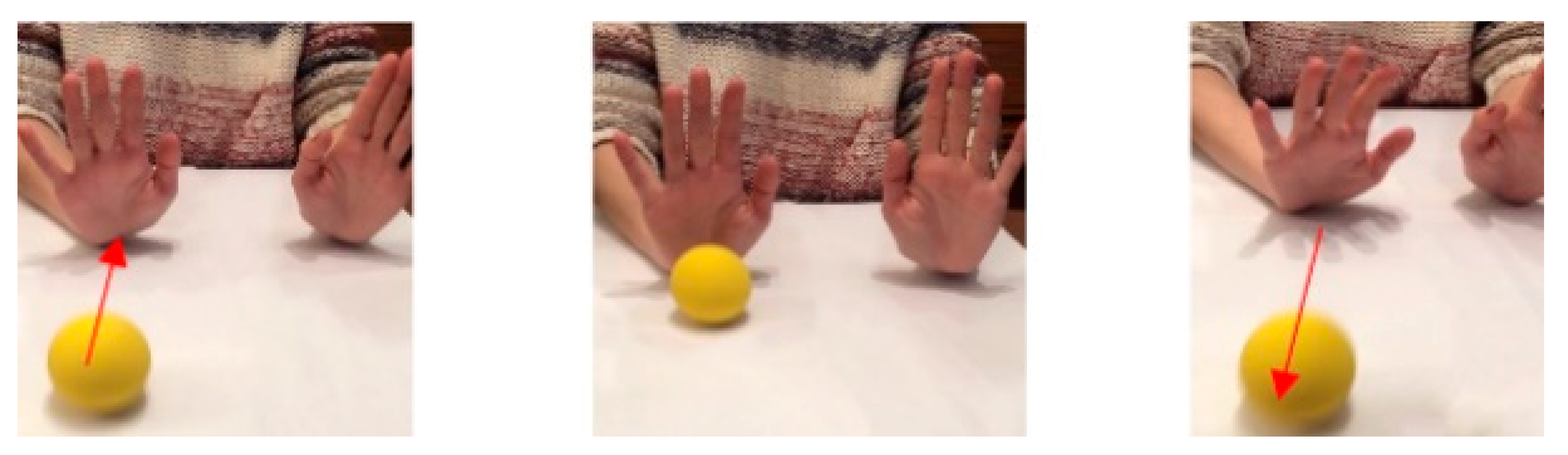 |
| Doughnuts | -Material: make small plasticine rings. -Exercise: with your forearm resting on the table, do wrist extension and place the doughnuts on your fingers while keeping your wrist in extension. You can stop and rest when you are tired.  |
| The Marble | -Material: a small ball of plasticine. -Exercise: put a small ball on the back of your hand and make wrist extension to keep the ball from falling (move the small ball on the back of your hand).  |
| Protocol: 4 Weeks Dose: 20 min per/day | Day 1 | Day 2 | Day 3 |
|---|---|---|---|
| 5 min (morning) | Forearm Prone-supination 1-Sound Bottle | Wrist flexion-extension 5-Doughnuts | Forearm Prono-supination 3-Tower |
| 5 min (morning) | Forearm Prone-supination 2-Cookies | Wrist flexion-extension 6-The Marble | Wrist flexion-extension 4-Ball Wheel |
| 5 min (afternoon) | Forearm Prone-supination 3-Tower | Forearm Prone-supination 1-Sound Bottle. | Wrist flexion-extension 5-Doughnuts |
| 5 min (afternoon) | Wrist flexion-extension 4- Ball Wheel | Forearm Prone-supination 2-Cookies | Wrist flexion-extension 6-The Marble |
| VARIABLES | Total (n = 12) | Virtual Reality MT (n = 6) | Conventional MT (n = 6) | p-Value |
|---|---|---|---|---|
| AGE years, mean (SD) | 8.42 (3.4) | 8.5 (3.5) | 8.4 (3.3) | 0.9 |
| SEX | ||||
| Male. Num (%) | 6 (50) | 3 (50) | 3 (50) | 1.00 |
| Female. Num (%) | 6 (50) | 3 (50) | 3 (50) | |
| AFFECTED UPPER LIMB | ||||
| Left. Num (%) | 4 (33.3) | 1 (16.7) | 3 (50) | 0.04 * |
| Right. Num (%) | 8 (66.7) | 5 (83.3) | 3 (50) |
| Ch | Age | Sex | Injured B.P. Roots | Aff. UL | Aff. Muscles/m.S.S | Narakas Classf. | Risk Factor PBO | BTX-A | Performed Therapy |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 12 | F | C5–C6 | R | -Shoulder: Flexors: 4− Ext.rot: 4− -Elbow: Biceps and Extensors: 3+/3 -Forearm: Supinators: 3+ | I | >4 kg born | Pectoralis major Biceps brachii | Virtual Reality MT |
| 2 | 11 | M | C5–C6 | R | -Shoulder: Flexors: 4 Ext.rot: 4 -Elbow: Bicepsand extensors: 4/3+ -Forearm: Supinators: 3+ | I | >4 kg born | Pectoralis major Biceps brachii | Conventional MT |
| 3 | 8 | F | C5–C6–C7 | R | -Shoulder: Flexors: 4− Ext.rot: 4 -Elbow: Biceps and extensors: 4/3+ -Forearm: Supinators: 3+ -Wrist: Extensors: 4 | II | >4 kg born | Pectoralis major Biceps brachii | Conventional MT |
| 4 | 7 | F | C5–C6 | L | -Shoulder: Flexors: 4 Ext.rot: 3+ -Elbow: Biceps and extensors: 3+/3+ -Forearm: Supinators: 3+ | I | Instrument. delivery | No | Conventional MT |
| 5 | 7 | M | C5–C6–C7 | R | -Shoulder: Flexors: 4− Ext.rot: 3+ -Elbow: Biceps and extensors: 4/3+ -Forearm: Supinators: 3+ -Wrist: Extensors: 4 | II | Instrument. delivery | No | Virtual Reality MT |
| 6 | 9 | M | C5–C6–C7 | L | -Shoulder: Flexors: 4 Ext.rot: 4 -Elbow: Biceps and extensors: 4−/3+ -Forearm: Supinators: 3+ -Wrist: Extensors: 4 | II | >4 kg born | No | Conventional MT |
| 7 | 6 | F | C5–C6–C7 | R | -Shoulder: Flexors: 4 Ext.rot: 3+ -Elbow: Biceps and extensors: 4/3+ -Forearm: Supinators: 3+ -Wrist: Extensors: 4 | II | Instrument. delivery | Biceps brachii Pronators | Conventional MT |
| 8 | 8 | M | C5–C6–C7 | R | -Shoulder: Flexors: 4 Ext.rot: 4 -Elbow: Biceps and extensors: 4/4 -Forearm: Supinators: 4 -Wrist: Extensors: 4 | II | Instrument. delivery | Pectoralis major | Virtual Reality MT |
| 9 | 8 | F | C5–C6–C7 | L | -Shoulder: Flexors: 4 Ext.rot: 3+ -Elbow: Biceps and extensors: 3+/3+ -Forearm: Supinators: 3+ -Wrist: Extensors: 4 | II | Instrument. delivery | Biceps brachii pronators | Virtual Reality MT |
| 10 | 10 | M | C4–C5–C6–C7 | R | -Shoulder: Flexors: 4− Ext.rot: 4− -Elbow: Biceps and extensors: 3+/3+ -Forearm: Supinators: 3+ -Wrist: Extensors: 3+ | II | >4 kg born | No | Virtual Reality MT |
| * 11 | 6 | F | C5–C6–C7 | R | -Shoulder: Flexors: 4 Ext.rot: 4 -Elbow: Biceps and extensors: 4/3+ -Forearm: Supinators: 3+ -Wrist: Extensors: 4− | II | Instrument. delivery | No | Virtual Reality MT |
| * 12 | 9 | M | C5–C6–C7 | L | -Shoulder: Flexors: 4 Ext.rot: 3+ -Elbow: Biceps and extensors: 4/3+ -Forearm: Supinators: 3+ -Wrist: Extensors: 4− | II | Instrument. delivery | Pectoralis major | Conventional MT |
| Spontaneous USe | Total Sample (n = 12) | +p Value | Virtual Reality MT (n = 6) | p Value | Conventional MT (n = 6) | p Value |
|---|---|---|---|---|---|---|
| Indep. Task | ||||||
| Week 0 | 23.5 (15, 28) | 0.12 | 24 (21, 28) | 20 (15, 27) | ||
| Week 4 | 24.5 (15, 29) | 0.02 * | 26 (23, 29) | 0.02 * | 19.5 (15, 24) | 0.78 |
| No indep. Task | ||||||
| Week 0 | 2 (0, 9) | 0.10 | 1 (0, 8) | 4 (2, 9) | ||
| Week 4 | 2.5 (0, 7) | 0.19 | 0.5 (0, 5) | 0.18 | 5 (0, 7) | 0.28 |
| No rel. Task | ||||||
| Week 0 | 2.5 (0, 8) | 0.75 | 5 (0, 7) | 2 (0, 8) | ||
| Week 4 | 1.5 (0, 8) | 0.14 | 3 (0, 3) | 0.13 | 6.5 (0, 8) | 0.28 |
| Non-use AH | ||||||
| Week 0 | 0 (0, 3) | 0.90 | 0 (0, 3) | 0 (0, 2) | ||
| Week 4 | 0 (0, 3) | 0.41 | 0 (0, 3) | 1.00 | 0 (0, 0) | 0.32 |
| Use AH support | ||||||
| Week 0 | 2 (0, 21) | 0.37 | 1 (0, 18) | 4 (0, 21) | ||
| Week 4 | 3.5 (0, 13) | 0.32 | 0.5 (0, 10) | 0.46 | 7.5 (0, 13) | 0. 41 |
| Use AH grasp | ||||||
| Week 0 | 19 (0, 27) | 0.14 | 20 (3, 27) | 16 (0, 27) | ||
| Week 4 | 17.5 (0, 29) | 0.04 * | 24 (12, 29) | 0.04 * | 15.5 (2, 17) | 0.32 |
| Efficacy | ||||||
| Week 0 | 3.3 (2,3, 4) | 0.74 | 3.2 (2.3, 3.8) | 3.3 (3.1, 4) | ||
| Week 4 | 3.5 (2.3, 4) | 0.59 | 3.7 (2.3, 4) | 0.79 | 3.5 (2.9, 4) | 0.70 |
| Task time | ||||||
| Week 0 | 3.4 (1.9, 4) | 0.19 | 3.5 (3.2, 4) | 3.3 (1.9, 4) | ||
| Week 4 | 3.7 (1.7, 4) | 0.39 | 3.8 (3.1, 4) | 0.58 | 3.6 (1.7, 4) | 0.45 |
| Disconfort | ||||||
| Week 0 | 3.9 (2.9, 4) | 0.55 | 3.9 (3.6, 4) | 3.7 (2.9, 4) | ||
| Week 4 | 3.9 (2.9, 4) | 0.17 | 3.9 (3.5, 4) | 0.85 | 3.9 (2.9, 4) | 0.32 |
| Quality of Life | Total Sample (n = 12) | p Value | Virtual Reality MT (n = 6) | p Value | Conventional MT (n = 6) | p Value |
|---|---|---|---|---|---|---|
| PhysD (Ch) | ||||||
| Week 0 | 76.6 (50, 100) | 0.29 | 87.5 (53.1, 96.9) | 0.07 | 75 (50, 100) | 0.18 |
| Week 4 | 85.9 (56.2, 96.9) | 0.16 | 92.2 (56.2, 96.9) | 75 (56.2, 93.7) | ||
| PhysD (P) | ||||||
| Week 0 | 74.1 (46.9, 96.9) | 0.57 | 75 (46.9, 96.9) | 72.9 (59.4, 93.7) | ||
| Week 4 | 81.2 (65.6, 100) | 0.04 * | 82.8 (71.9, 100) | 0.03+ | 73.9 (65.6, 90.6) | 0.14 |
| EmD (Ch) | ||||||
| Week 0 | 71.5 (50,100) | 0.45 | 80 (45, 100) | 60 (60, 100) | ||
| Week 4 | 74.5 (45, 100) | 0.62 | 82.5 (50, 100) | 0.46 | 65 (90, 50) | 0.28 |
| EmD (P) | ||||||
| Week 0 | 75 (50, 100) | 0.37 | 75 (65, 100) | 65 (50, 80) | ||
| Week 4 | 75 (50, 100) | 0.08 | 75 (65, 100) | 0.59 | 65 (50, 70) | 0.41 |
| SocD (Ch) | ||||||
| Week 0 | 90 (40, 100) | 0.06 | 95 (70, 100) | 70 (40, 90) | ||
| Week 4 | 90 (40, 100) | 0.06 | 97.5 (80, 100) | 0.1 | 77.5 (40, 90) | 0.11 |
| SocD (P) | ||||||
| Week 0 | 87.5 (55, 100) | 0.06 | 100 (55, 100) | 70 (60, 90) | ||
| Week 4 | 90 (60, 100) | 0.07 | 100 (90, 100) | 0.28 | 70 (60, 90) | 0.1 |
| SchD (Ch) | ||||||
| Week 0 | 75 (60, 100) | 0.06 | 82.5 (65, 95) | 65 (60, 80) | ||
| Week 4 | 80 (50, 95) | 0.2 | 85 (60, 100) | 0.52 | 72.5 (50, 90) | 0.32 |
| SchD (P) | ||||||
| Week 0 | 77.6 (45, 100) | 0.12 | 85 (45, 100) | 70 (55, 70) | ||
| Week 4 | 85 (60, 95) | 0.23 | 87.5 (75, 95) | 0.07 | 71.5 (60, 90) | 0.1 |
| Total QoL (Ch) | ||||||
| Week 0 | 81 (52.5, 96.7) | 0.08 | 84.2 (59.5, 96.7) | 71.2 (52.5, 85) | ||
| Week 4 | 85.2 (59, 96.5) | 0.04 * | 87.7 (62.8, 95.5) | 0.04 * | 73.2 (42.5, 95) | 0.07 |
| Total QoL (P) | ||||||
| Week 0 | 78.9 (57.3, 98.4) | 0.14 | 82.8 (60.5, 98.4) | 70.5 (57.3, 83.4) | ||
| Week 4 | 81.2 (58.9, 91.9) | 0.09 | 85 (45, 100) | 0.12 | 71.2 (60.3, 85.4) | 0.07 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yeves-Lite, A.; Zuil-Escobar, J.C.; Martínez-Cepa, C.; Romay-Barrero, H.; Ferri-Morales, A.; Palomo-Carrión, R. Conventional and Virtual Reality Mirror Therapies in Upper Obstetric Brachial Palsy: A Randomized Pilot Study. J. Clin. Med. 2020, 9, 3021. https://doi.org/10.3390/jcm9093021
Yeves-Lite A, Zuil-Escobar JC, Martínez-Cepa C, Romay-Barrero H, Ferri-Morales A, Palomo-Carrión R. Conventional and Virtual Reality Mirror Therapies in Upper Obstetric Brachial Palsy: A Randomized Pilot Study. Journal of Clinical Medicine. 2020; 9(9):3021. https://doi.org/10.3390/jcm9093021
Chicago/Turabian StyleYeves-Lite, Alba, Juan Carlos Zuil-Escobar, Carmen Martínez-Cepa, Helena Romay-Barrero, Asunción Ferri-Morales, and Rocío Palomo-Carrión. 2020. "Conventional and Virtual Reality Mirror Therapies in Upper Obstetric Brachial Palsy: A Randomized Pilot Study" Journal of Clinical Medicine 9, no. 9: 3021. https://doi.org/10.3390/jcm9093021
APA StyleYeves-Lite, A., Zuil-Escobar, J. C., Martínez-Cepa, C., Romay-Barrero, H., Ferri-Morales, A., & Palomo-Carrión, R. (2020). Conventional and Virtual Reality Mirror Therapies in Upper Obstetric Brachial Palsy: A Randomized Pilot Study. Journal of Clinical Medicine, 9(9), 3021. https://doi.org/10.3390/jcm9093021





