Fractures of the Humeral Shaft with Primary Radial Nerve Palsy: Do Injury Mechanism, Fracture Type, or Treatment Influence Nerve Recovery?
Abstract
:1. Introduction
2. Material and Methods
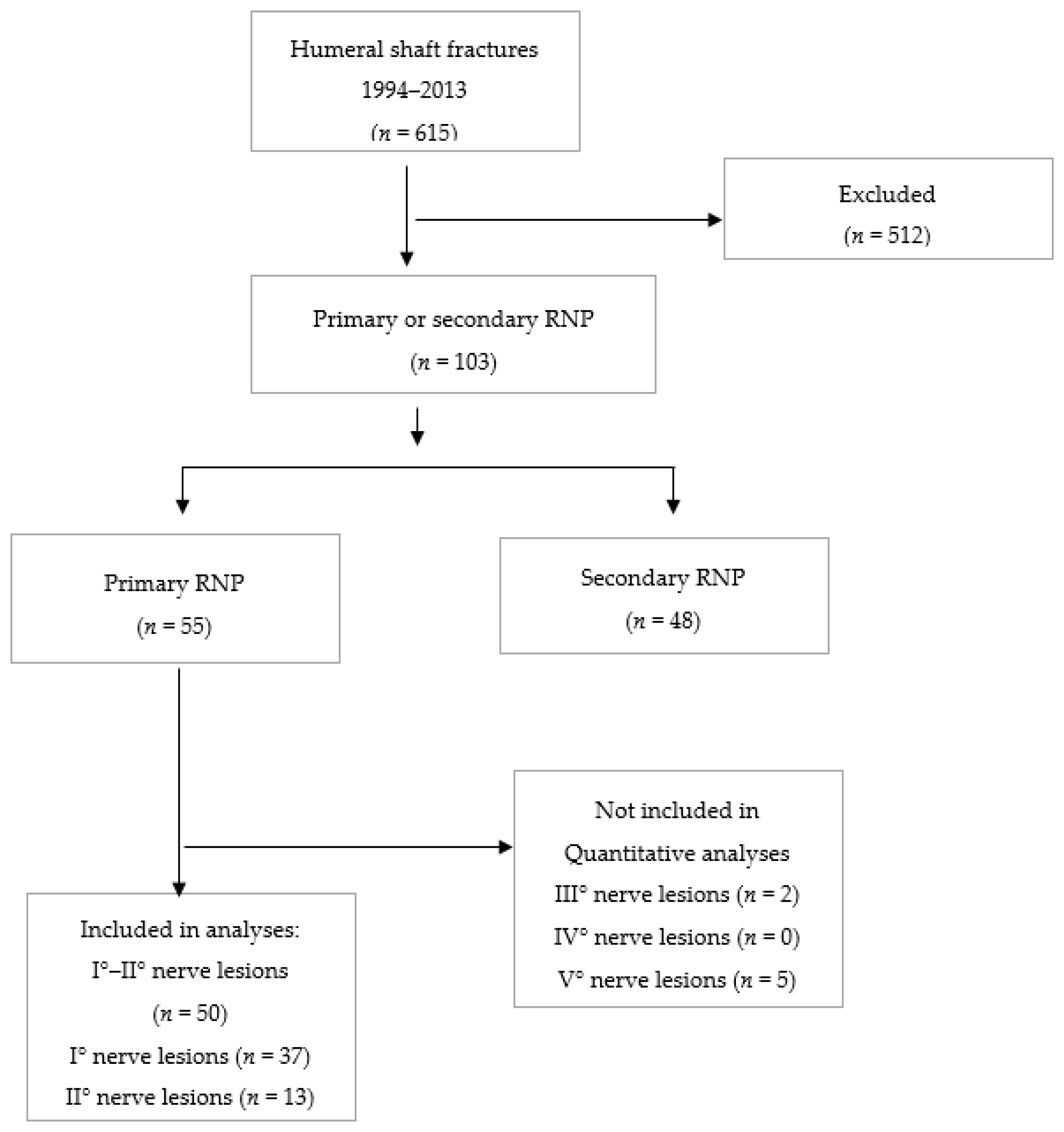
2.1. Study Design and Patient Recruitment
2.2. Diagnosis and Surgical Treatment
2.3. Outcome Assessment
2.4. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Zhao, J.G.; Wang, J.; Wang, C.; Kan, S.L. Intramedullary Nail Versus Plate Fixation for Humeral Shaft Fractures: A Systematic Review of Overlapping Meta-analyses. Medicine 2015, 94, e599. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Ning, G.; Wu, Q.; Feng, S. Review of literature of radial nerve injuries associated with humeral fractures-an integrated management strategy. PLoS ONE 2013, 8, e78576. [Google Scholar] [CrossRef] [PubMed]
- DeFranco, M.J.; Lawton, J.N. Radial nerve injuries associated with humeral fractures. J. Hand Surg. 2006, 31, 655–663. [Google Scholar] [CrossRef] [PubMed]
- Kurup, H.; Hossain, M.; Andrew, J.G. Dynamic compression plating versus locked intramedullary nailing for humeral shaft fractures in adults. Cochrane Database Syst. Rev. 2011. [Google Scholar] [CrossRef] [PubMed]
- Ma, J.; Xing, D.; Ma, X.; Gao, F.; Wei, Q.; Jia, H.; Feng, R.; Yu, J.; Wang, J. Intramedullary nail versus dynamic compression plate fixation in treating humeral shaft fractures: Grading the evidence through a meta-analysis. PLoS ONE 2013, 8, e82075. [Google Scholar] [CrossRef]
- McCormack, R.G.; Brien, D.; Buckley, R.E.; McKee, M.D.; Powell, J.; Schemitsch, E.H. Fixation of fractures of the shaft of the humerus by dynamic compression plate or intramedullary nail. A prospective, randomised trial. J. Bone Jt. Surg. Br. 2000, 82, 336–339. [Google Scholar] [CrossRef]
- Grass, G.; Kabir, K.; Ohse, J.; Rangger, C.; Besch, L.; Mathiak, G. Primary Exploration of Radial Nerve is Not. Required for Radial Nerve Palsy while Treating Humerus Shaft Fractures with Unreamed Humerus Nails (UHN). Open Orthop. J. 2011, 5, 319–323. [Google Scholar] [CrossRef]
- Pailhe, R.; Mesquida, V.; Rubens-Duval, B.; Saragaglia, D. Plate osteosynthesis of humeral diaphyseal fractures associated with radial palsy: Twenty cases. Int. Orthop. 2015. [Google Scholar] [CrossRef]
- Prodromo, J.; Goitz, R.J. Management of radial nerve palsy associated with humerus fracture. J. Hand Surg. 2013, 38, 995–998. [Google Scholar] [CrossRef]
- S3-Leitlinie: Versorgung peripherer Nervenverletzungen. 2013, Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften (AWMF)- Ständige Kommission Leitlinien. Available online: http://www.awmf.org/leitlinien/awmf-regelwerk.html (accessed on 30 June 2013).
- Shao, Y.C.; Harwood, P.; Grotz, M.R.; Limb, D.; Giannoudis, P.V. Radial nerve palsy associated with fractures of the shaft of the humerus: A systematic review. J. Bone Jt. Surg. Br. 2005, 87, 1647–1652. [Google Scholar] [CrossRef]
- Carroll, E.A.; Harwood, P.; Grotz, M.R.; Limb, D.; Giannoudis, P.V. Management of humeral shaft fractures. J. Am. Acad. Orthop. Surg. 2012, 20, 423–433. [Google Scholar] [CrossRef] [PubMed]
- Siebenrock, K.A.; Gerber, C. Classification of fractures and problems in proximal humeral fractures. Orthopade 1992, 21, 98–105. [Google Scholar] [PubMed]
- Horn, B.D.; Rettig, M.E. Interobserver reliability in the Gustilo and Anderson classification of open fractures. J. Orthop. Trauma 1993, 7, 357–360. [Google Scholar] [CrossRef] [PubMed]
- Sunderland, S. A classification of peripheral nerve injuries producing loss of function. Brain 1951, 74, 491–516. [Google Scholar] [CrossRef] [PubMed]
- Hislop, H.J.; Montgomery, J.; Connolly, B.H.; Daniels, L. Daniels and Worthingham’s Muscle Testing: Techniques of Manual Examination, 6th ed.; W.B. Saunders: Philadelphia, PA, USA, 1995; Volume 17, p. 437. [Google Scholar]
- Chapman, J.R.; Henley, M.B.; Agel, J.; Benca, P.J. Randomized prospective study of humeral shaft fracture fixation: Intramedullary nails versus plates. J. Orthop. Trauma 2000, 14, 162–166. [Google Scholar] [CrossRef]
- Korompilias, A.V.; Lykissas, M.G.; Kostas-Agnantis, I.P.; Vekris, M.D.; Soucacos, P.N.; Beris, A.E. Approach to radial nerve palsy caused by humerus shaft fracture: Is primary exploration necessary? Injury 2013, 44, 323–326. [Google Scholar] [CrossRef]
- Ekholm, R.; Ponzer, S.; Tornkvist, H.; Adami, J.; Tidermark, J. Primary radial nerve palsy in patients with acute humeral shaft fractures. J. Orthop. Trauma 2008, 22, 408–414. [Google Scholar] [CrossRef]
- Venouziou, A.I.; Dailiana, Z.H.; Varitimidis, S.E.; Hantes, M.E.; Gougoulias, N.E.; Malizos, K.N. Radial nerve palsy associated with humeral shaft fracture. Is the energy of trauma a prognostic factor? Injury 2011, 42, 1289–1293. [Google Scholar] [CrossRef]
- Elton, S.G.; Rizzo, M. Management of radial nerve injury associated with humeral shaft fractures: An evidence-based approach. J. Reconstr. Microsurg. 2008, 24, 569–573. [Google Scholar] [CrossRef]
- Ljungquist, K.L.; Martineau, P.; Allan, C. Radial nerve injuries. J. Hand Surg. 2015, 40, 166–172. [Google Scholar] [CrossRef] [PubMed]
- Larsen, L.B.; Barfred, T. Radial nerve palsy after simple fracture of the humerus. Scand. J. Plast. Reconstr. Surg. Hand Surg. 2000, 34, 363–366. [Google Scholar] [PubMed]
| Patients | n = 50 |
|---|---|
| Age | 43.5 ± 21.3 years |
| Sex | |
| Female | 18 (36%) |
| Male | 32 (64%) |
| Trauma mechanism | |
| High-energy | 29 (58%) |
| Low-energy | 21 (42%) |
| Fracture type | |
| A1 | n = 17 (34%) |
| A2 | n = 5 (10%) |
| A3 | n = 7 (14%) |
| B1 | n = 14 (28%) |
| B2 | n = 2 (4%) |
| B3 | n = 3 (6%) |
| C1 | n = 2 (4%) |
| Treatment | |
| Intramedullary nailing | n = 20 (40%) |
| ORIF | n = 30 (60%) |
| Injury Mechanism | p | Fracture Type | p * | Treatment | p | Fracture Location | p | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Low-Energy | High-Energy | A1 | A2 | A3 | IN | IN | B3 | C1 | IN | ORIF | Mid-Shaft | Distal-Shaft | |||||
| Time to onset of recovery (weeks) | 10.7 ± 3.1 | 10.3 ± 3.5 | 0.680 | 10.7 ±2.9 | 11.4 ± 4.0 | 11.4 ± 4.0 | 10.7 ± 3.5 | 10.7 ± 3.5 | 12.3 ± 2.9 | 10.5 ± 0.7 | 0.552 | 10.7 ± 3.5 | 10.3 ± 3.3 | 0.774 | 10.7 ± 3.4 | 10.4 ± 3.4 | 0.737 |
| Time to full recovery (weeks) | 28.1 ± 10.1 | 25.8 ± 8.0 | 0.387 | 26.2 ±8.3 | 25.0 ± 4.7 | 30.3 ± 9.0 | 25.4 ± 7.8 | 25.4 ± 7.8 | 26.0 ± 4.4 | 35.5 ± 2.1 | 0.728 | 25.4 ± 7.8 | 27.8 ± 9.6 | 0.353 | 27.0 ± 9.3 | 26.7 ± 8.9 | 0.911 |
| Β * | t ** | p ** | 95% Confidence Interval * | |
|---|---|---|---|---|
| Trauma mechanism | −0.312 | −0.308 | 0.759 | −2.352 to 1.728 |
| Fracture type | −0.139 | −0.464 | 0.645 | −0.742 to 0.464 |
| Treatment | −0.111 | −0.043 | 0.966 | −2.256 to 2.163 |
| Fracture location | −0.248 | −0.228 | 0.821 | −2.436 to 1.941 |
| R2 = 0.011 |
| Β * | t ** | p ** | 95% Confidence Interval * | |
|---|---|---|---|---|
| Trauma mechanism | −2.454 | −0.928 | 0.358 | −7.777 to 2.869 |
| Fracture type | 0.322 | 0.412 | 0.682 | −1.251 to 1.895 |
| Treatment | 2.431 | 0.849 | 0.400 | −3.335 to 8.196 |
| Fracture location | −0.941 | −0.332 | 0.741 | −6.652 to 4.769 |
| R2 = 0.041 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ostermann, R.C.; Lang, N.W.; Joestl, J.; Pauzenberger, L.; Tiefenboeck, T.M.; Platzer, P. Fractures of the Humeral Shaft with Primary Radial Nerve Palsy: Do Injury Mechanism, Fracture Type, or Treatment Influence Nerve Recovery? J. Clin. Med. 2019, 8, 1969. https://doi.org/10.3390/jcm8111969
Ostermann RC, Lang NW, Joestl J, Pauzenberger L, Tiefenboeck TM, Platzer P. Fractures of the Humeral Shaft with Primary Radial Nerve Palsy: Do Injury Mechanism, Fracture Type, or Treatment Influence Nerve Recovery? Journal of Clinical Medicine. 2019; 8(11):1969. https://doi.org/10.3390/jcm8111969
Chicago/Turabian StyleOstermann, Roman C., Nikolaus W. Lang, Julian Joestl, Leo Pauzenberger, Thomas M. Tiefenboeck, and Patrick Platzer. 2019. "Fractures of the Humeral Shaft with Primary Radial Nerve Palsy: Do Injury Mechanism, Fracture Type, or Treatment Influence Nerve Recovery?" Journal of Clinical Medicine 8, no. 11: 1969. https://doi.org/10.3390/jcm8111969
APA StyleOstermann, R. C., Lang, N. W., Joestl, J., Pauzenberger, L., Tiefenboeck, T. M., & Platzer, P. (2019). Fractures of the Humeral Shaft with Primary Radial Nerve Palsy: Do Injury Mechanism, Fracture Type, or Treatment Influence Nerve Recovery? Journal of Clinical Medicine, 8(11), 1969. https://doi.org/10.3390/jcm8111969







