Organizational E-Readiness for the Digital Transformation of Primary Healthcare Providers during the COVID-19 Pandemic in Poland
Abstract
:1. Introduction
2. Literature Review
3. Materials and Methods
3.1. Methodology
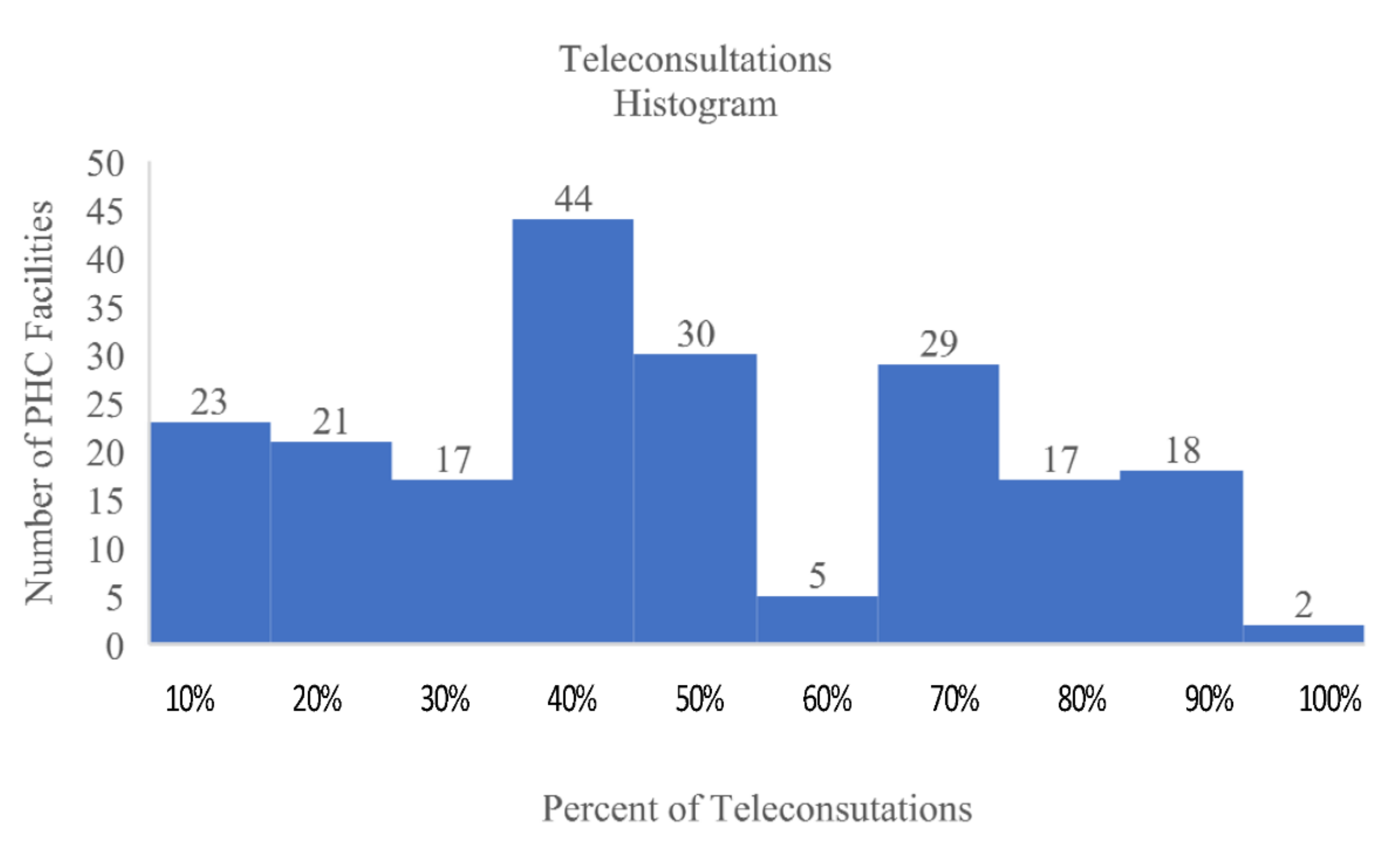
3.2. Population and Data Collection
3.3. Ethics
4. Results
4.1. Data Analysis
4.1.1. Technological Capabilities (TC)
4.1.2. Operational Capabilities
4.2. Factor Analysis
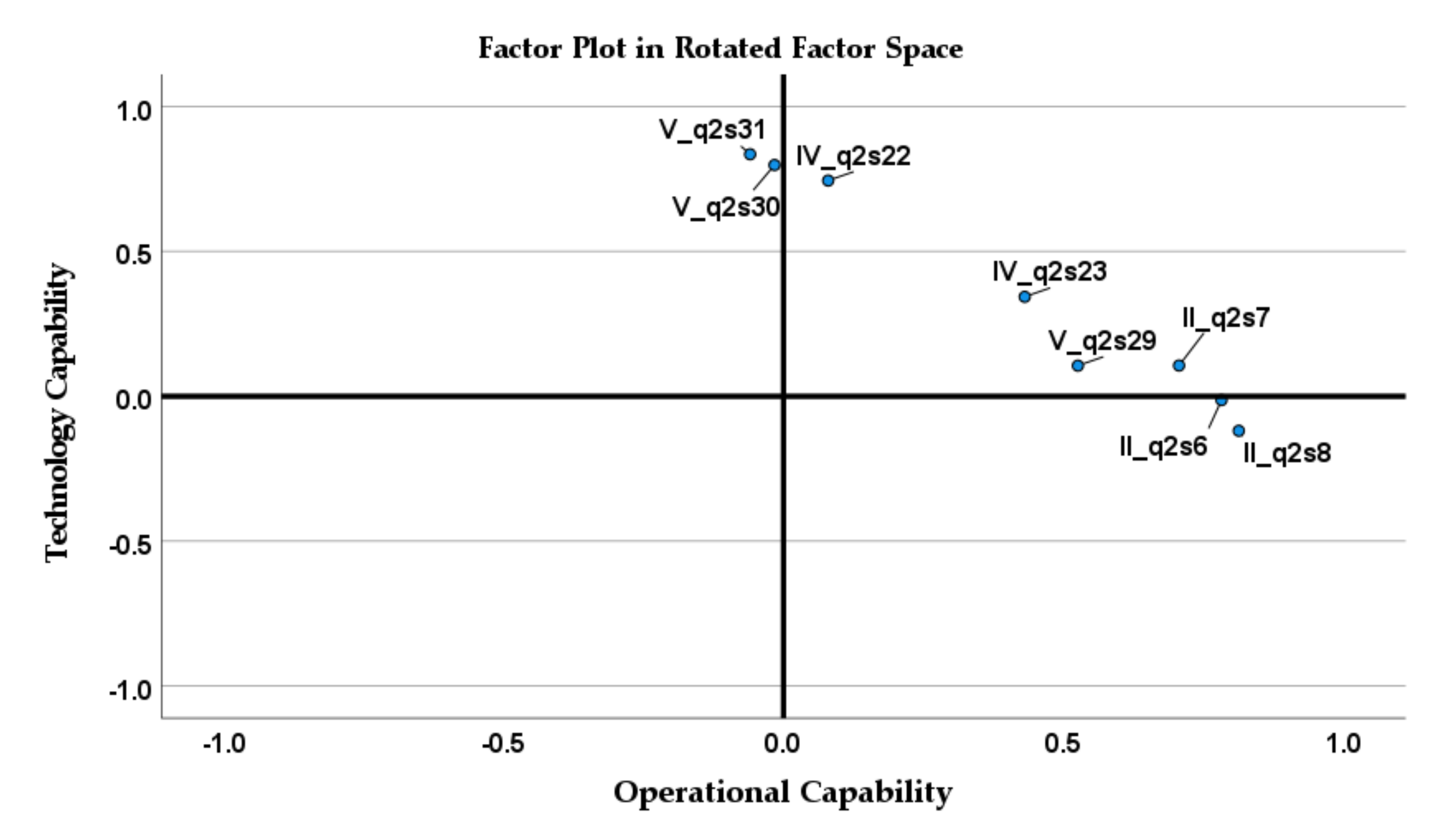
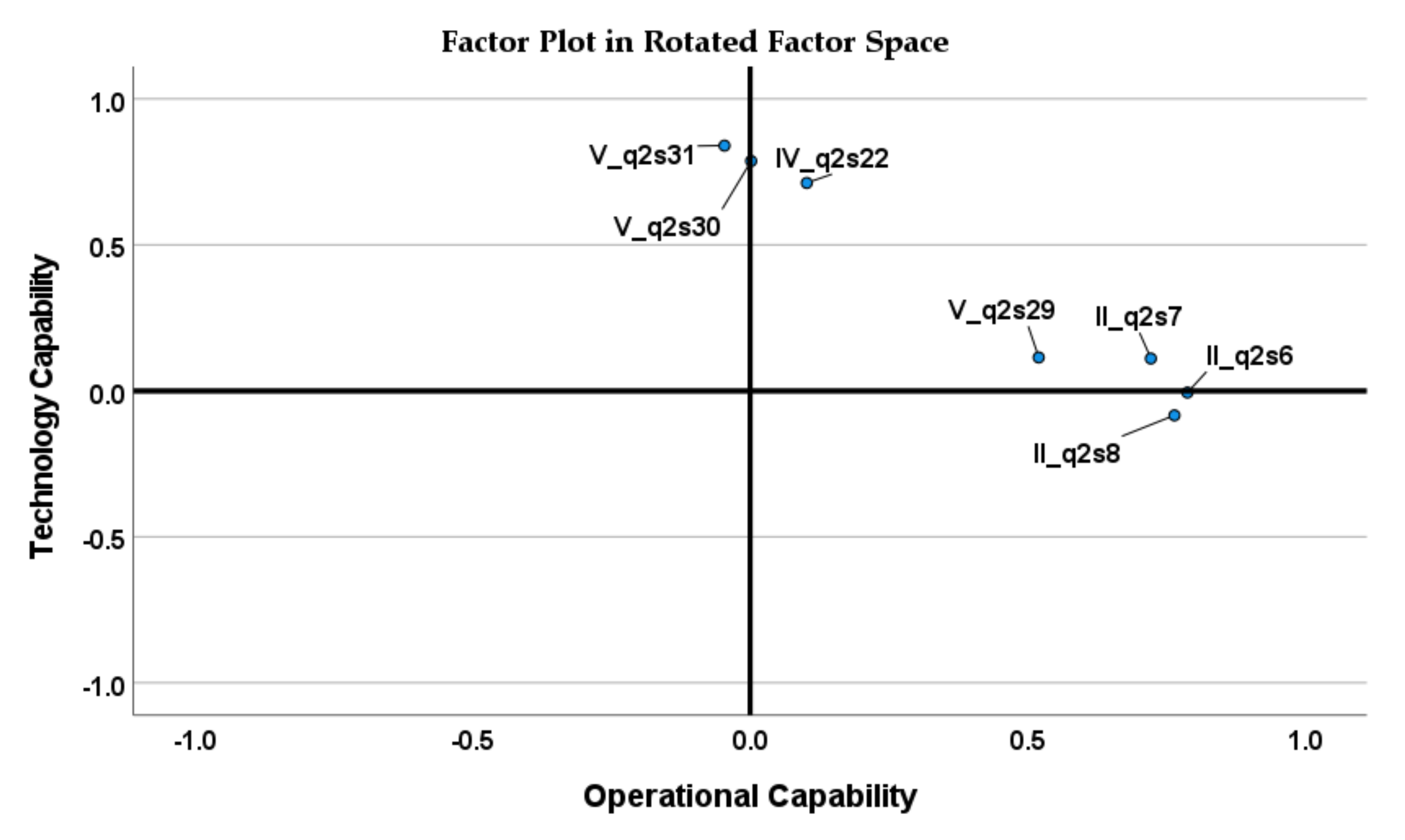
4.2.1. Exploratory Factor Analysis
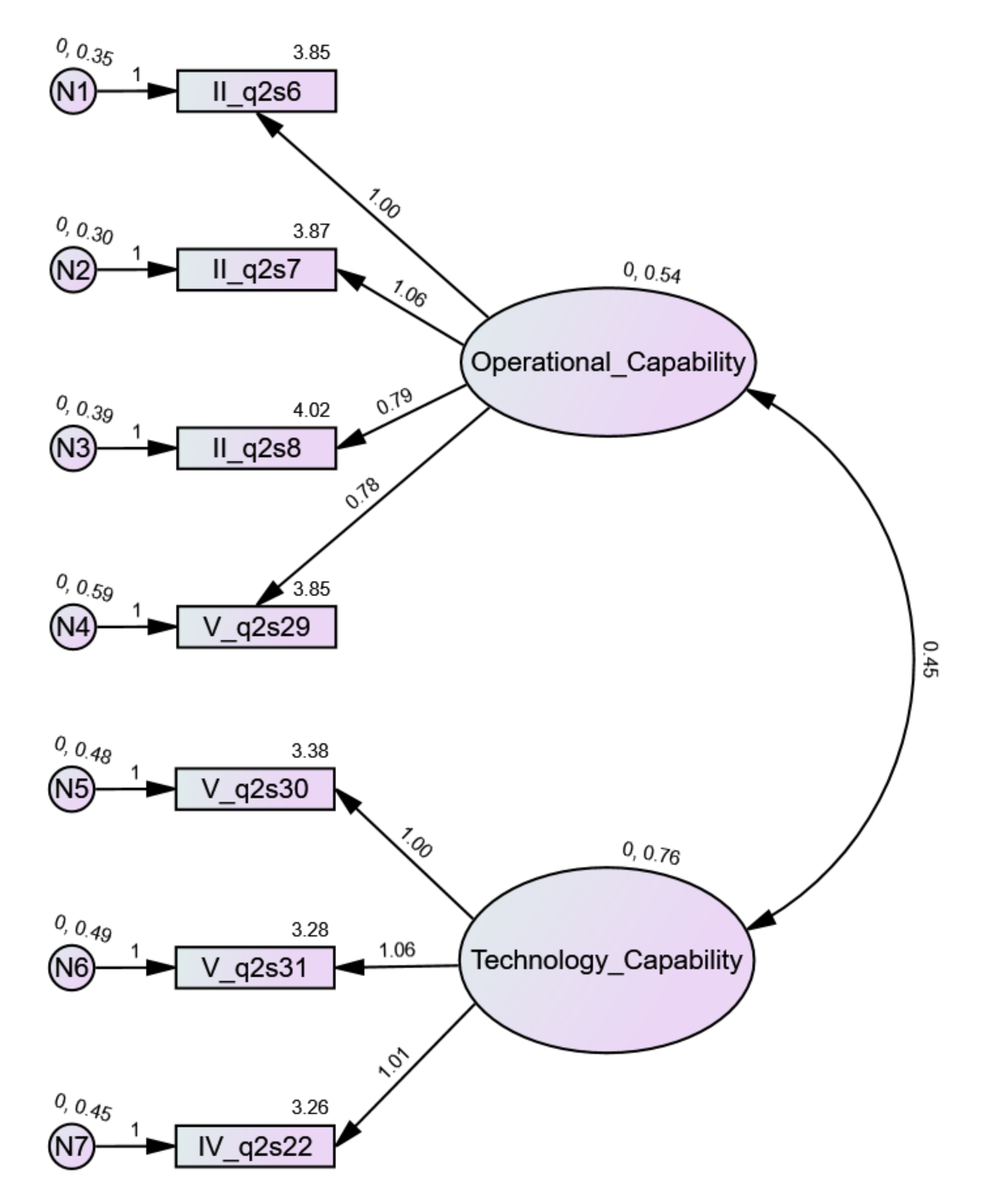
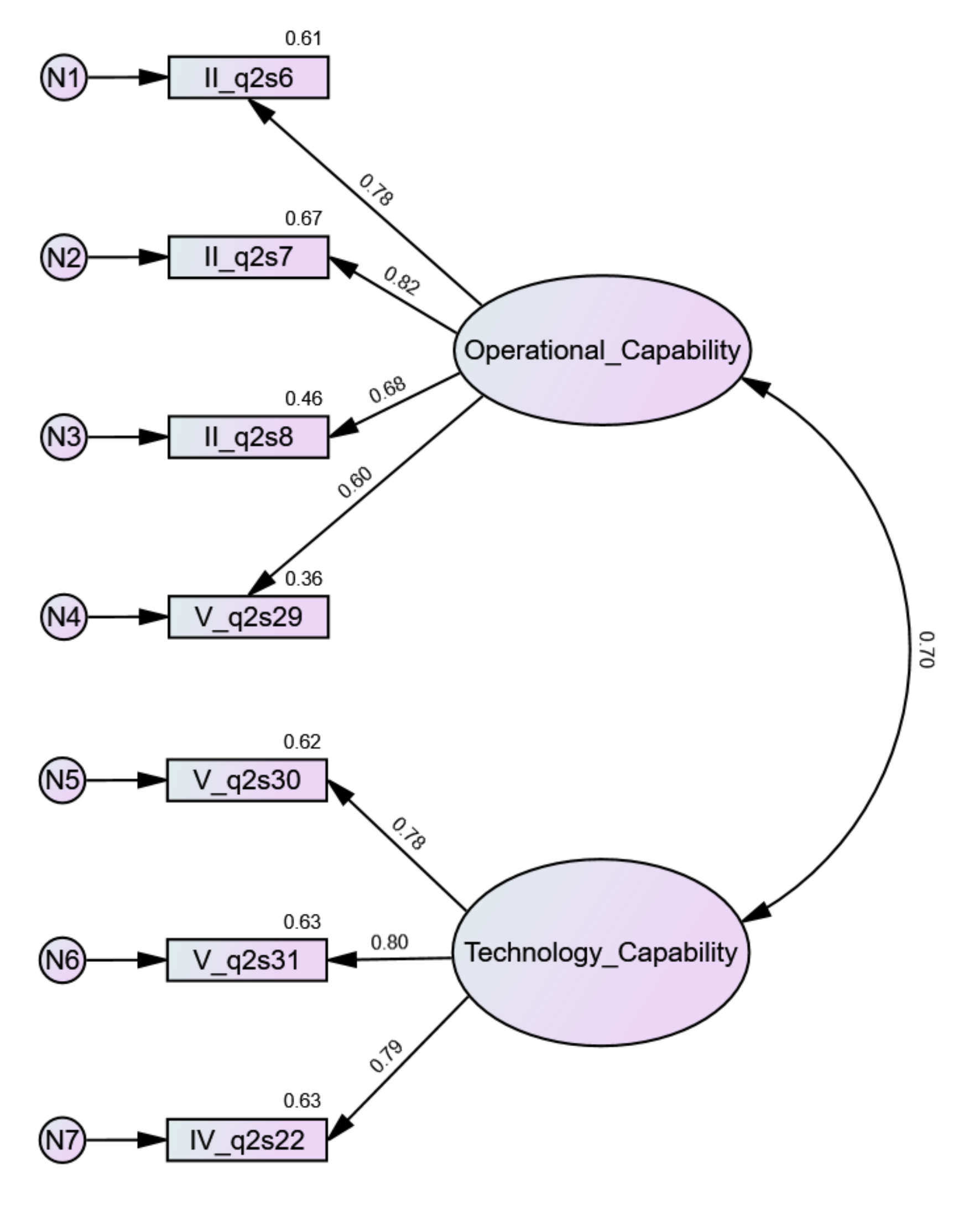
4.2.2. Confirmatory Factor Analysis
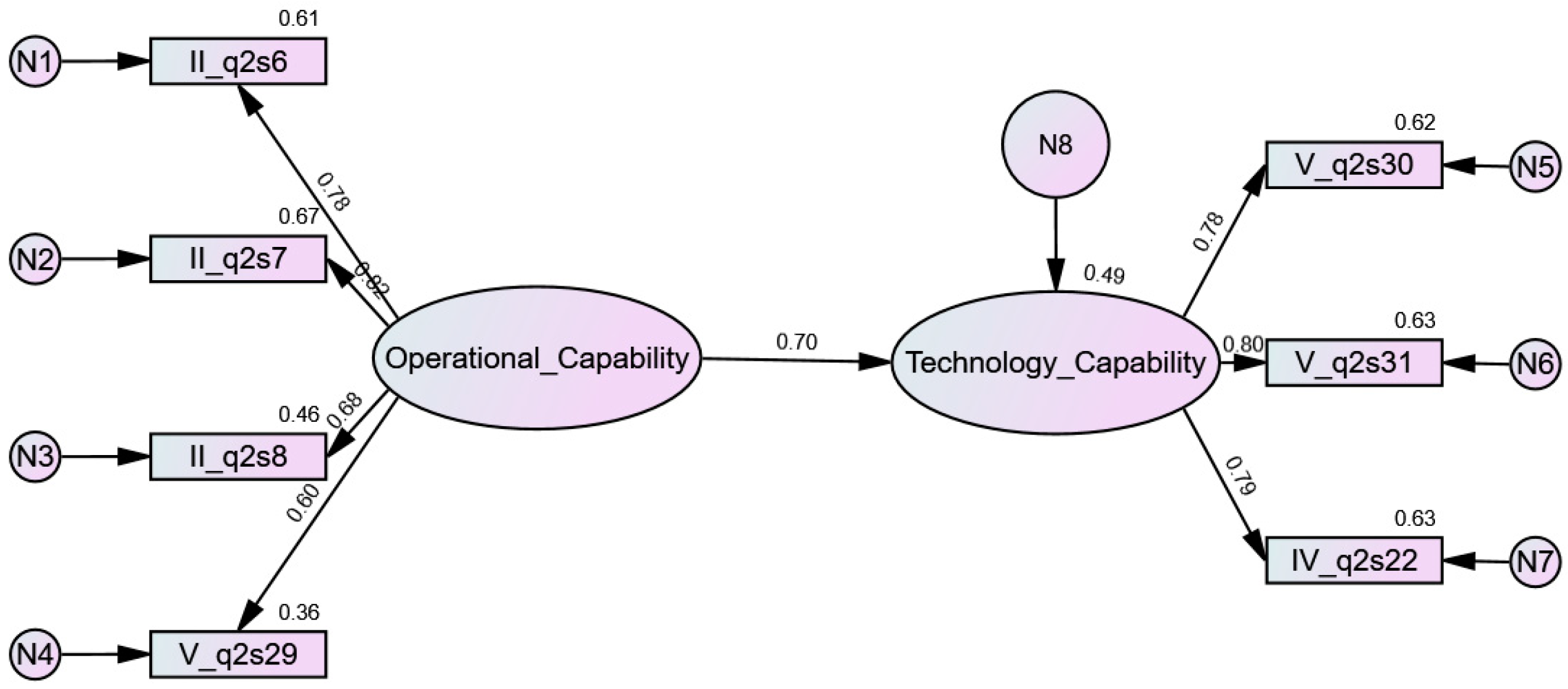
4.2.3. Regression Analysis
5. Discussion
6. Conclusions
- (i)
- We developed a new model of organizational e-readiness for digital transformation, based on organizational and technology capabilities;
- (ii)
- A basic set of variables that can effectively measure the dimensions of OC was confirmed and comprised four variables, namely the degree of agility (variable V_q2s29), level of process integration (variable II_q2s6), quality of resources (variable II_q2s7), and quality of cooperation (variable II_q2s8);
- (iii)
- A basic set of variables that can effectively measure the dimensions of TC was reduced to three, comprising the adoption and usage of technologies (variable V_q2s31), customer interaction (variable IV_q2s22), and process automation (variable IV_q2s30);
- (iv)
- The empirical results showed that OC is on a higher level than TC in Polish PHCs;
- (v)
- We have made one of the first attempts to examine the impact of OC on TC in the healthcare sector. Assessment of the relationship between OC and TC revealed a significant influence of operational capabilities on technological capabilities with a structural coefficient of 0.697.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yang, J.; Xie, H.; Liu, H.; Duan, H. Leveraging informational and relational capabilities for performance: An empirical investigation. Int. J. Logist. Manag. 2018, 29, 985–1000. [Google Scholar] [CrossRef]
- Pham, T.S.H.; Le Monkhouse, L.; Barnes, B.R. The influence of relational capability and marketing capabilities on the export performance of emerging market firms. Int. Mark. Rev. 2017, 34, 606–628. [Google Scholar] [CrossRef]
- Ahmad, N.; Othman, S.N.; Mad Lazim, H. A review of technological capability and performance relationship in manufacturing companies. In Proceedings of the 2014 International Symposium on Technology Management and Emerging Technologies, Bandung, Indonesia, 27–29 May 2014; IEEE: Piscataway, NJ, USA, 2014; pp. 193–198. [Google Scholar] [CrossRef]
- Hollander, J.E.; Carr, B.G. Virtually Perfect? Telemedicine for Covid-19. N. Engl. J. Med. 2020, 382, 1679–1681. [Google Scholar] [CrossRef]
- Favela, J.; Martinez, A.I.; Rodriguez, M.D.; Gonzalez, V.M. Ambient Computing Research for Healthcare: Challenges, Opportunities and Experiences. Comput. Sist. 2008, 12, 109–127. [Google Scholar]
- Rezai-Rad, M.; Vaezi, R.; Nattagh, F. E-Health Readiness Assessment Framework in Iran. Iran. J. Public Health 2012, 41, 43. [Google Scholar] [PubMed]
- Greenhalgh, T.; Wherton, J.; Papoutsi, C.; Lynch, J.; Hughes, G.; A’Court, C.; Hinder, S.; Fahy, N.; Procter, R.; Shaw, S. Beyond adoption: A new framework for theorizing and evaluating nonadoption, abandonment, and challenges to the scale-up, spread, and sustainability of health and care technologies. J. Med. Internet Res. 2017, 19, e367. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weiner, B.J. A theory of organizational readiness for change. Implement. Sci. 2009, 4, 67. [Google Scholar] [CrossRef] [Green Version]
- Weiner, B.J.; Amick, H.; Lee, S.Y.D. Review: Conceptualization and measurement of organizational readiness for change. A review of the literature in health services research and other fields. Med. Care Res. Rev. 2008, 65, 379–436. [Google Scholar] [CrossRef] [PubMed]
- Rossmann, A.; Reutlingen, H. Digital Maturity: Conceptualization and Measurement Model Social media View project Startups in cooperation with incumbent firms View project Digital Maturity: Conceptualization and Measurement Model. In Proceedings of the Twenty-Sixth European Conference on Information Systems (ECIS 2018), Portsmouth, UK, 23–28 June 2018; University of Portsmouth: Portsmouth, UK, 2018. [Google Scholar]
- Snyder-Halpern, R. Indicators of organizational readiness for clinical information technology/systems innovation: A Delphi study. Int. J. Med. Inform. 2001, 63, 179–204. [Google Scholar] [CrossRef]
- Jennett, P.; Yeo, M.; Pauls, M.; Graham, J. Organizational readiness for telemedicine: Implications for success and failure. J. Telemed. Telecare 2003, 9 (Suppl. 2), 27–30. [Google Scholar] [CrossRef] [PubMed]
- Coombs, J.E.; Bierly, P.E. Measuring technological capability and performance. R D Manag. 2006, 36, 421–438. [Google Scholar] [CrossRef]
- Christensen, C.M.; Overdorf, M. Meeting the challenge of disruptive change. Harv. Bus. Rev. 2000, 78, 66–77. [Google Scholar]
- Guan, J.; Ma, N. Innovative capability and export performance of Chinese firms. Technovation 2003, 23, 737–747. [Google Scholar] [CrossRef]
- Lu, Y.; Ramamurthy, K. Understanding the link between information technology capability and organizational agility: An empirical examination. MIS Q. Manag. Inf. Syst. 2011, 35, 931–954. [Google Scholar] [CrossRef] [Green Version]
- Yeniyurt, S.; Wu, F.; Kim, D.; Cavusgil, S.T. Information technology resources, innovativeness, and supply chain capabilities as drivers of business performance: A retrospective and future research directions. Ind. Mark. Manag. 2019, 79, 46–52. [Google Scholar] [CrossRef]
- Panda, H.; Ramanathan, K. Technological capability assessment of a firm in the electricity sector. Technovation 1996, 16, 561–588. [Google Scholar] [CrossRef]
- Fortuin, F.T.J.M.; Omta, S.W.F. Innovation drivers and barriers in food processing. Br. Food J. 2009, 111, 839–851. [Google Scholar] [CrossRef]
- Ali, Z.; Zwetsloot, I.M.; Nada, N. An empirical study to explore the interplay of Managerial and Operational capabilities to infuse organizational innovation in SMEs. Procedia Comput. Sci. 2019, 158, 260–269. [Google Scholar] [CrossRef]
- Jonker, M.; Romijn, H.; Szirmai, A. Technological effort, technological capabilities and economic performance: A case study of the paper manufacturing sector in West Java. Technovation 2006, 26, 121–134. [Google Scholar] [CrossRef]
- Mohamad, A.A.; Ramayah, T.; Lo, M.C. Knowledge management in MSC Malaysia: The role of information technology capability. Int. J. Bus. Soc. 2017, 18, 651–660. [Google Scholar]
- Tremblay, P.J. Technological Capability and Productivity Growth: An Industrialized/Industrializing Country Comparison; CIRANO: Montréal, QC, Canada, 1998. [Google Scholar]
- Ziggers, G.W.; Henseler, J. Inter-firm network capability: How it affects buyer-supplier performance. Br. Food J. 2009, 111, 794–810. [Google Scholar] [CrossRef]
- Li, T.; Chan, Y.E. Dynamic information technology capability: Concept definition and framework development. J. Strateg. Inf. Syst. 2019, 28, 101575. [Google Scholar] [CrossRef]
- Teece, D.J. Explicating dynamic capabilities: The nature and microfoundations of (sustainable) enterprise performance. Strateg. Manag. J. 2007, 28, 1319–1350. [Google Scholar] [CrossRef] [Green Version]
- Avital, M.; Te’Eni, D. From generative fit to generative capacity: Exploring an emerging dimension of information systems design and task performance. Inf. Syst. J. 2009, 19, 345–367. [Google Scholar] [CrossRef]
- Doherty, N.F.; Terry, M. The role of IS capabilities in delivering sustainable improvements to competitive positioning. J. Strateg. Inf. Syst. 2009, 18, 100–116. [Google Scholar] [CrossRef] [Green Version]
- De Carolis, A.; Macchi, M.; Negri, E.; Terzi, S. A.; Macchi, M.; Negri, E.; Terzi, S. A maturity model for assessing the digital readiness of manufacturing companies. In IFIP Advances in Information and Communication Technology; Springer: Cham, Switzerland, 2017; Volume 513, pp. 13–20. [Google Scholar]
- Yusif, S.; Hafeez-Baig, A.; Soar, J. e-Health readiness assessment factors and measuring tools: A systematic review. Int. J. Med. Inform. 2017, 107, 56–64. [Google Scholar] [CrossRef]
- Lehman, W.E.K.; Greener, J.M.; Simpson, D.D. Assessing organizational readiness for change. J. Subst. Abuse Treat. 2002, 22, 197–209. [Google Scholar] [CrossRef]
- Molla, A.; Licker, P.S. Perceived e-readiness factors in e-commerce adoption: An empirical investigation in a developing country. Int. J. Electron. Commer. 2005, 10, 83–110. [Google Scholar] [CrossRef]
- Kwahk, K.-Y.; Lee, J.-N. The role of readiness for change in ERP implementation: Theoretical bases and empirical validation. Inf. Manag. 2008, 45, 474–481. [Google Scholar] [CrossRef]
- Shea, C.M.; Jacobs, S.R.; Esserman, D.A.; Bruce, K.; Weiner, B.J. Organizational readiness for implementing change: A psychometric assessment of a new measure. Implement. Sci. 2014, 9, 7. [Google Scholar] [CrossRef] [Green Version]
- Wiesboeck, F. Thinking outside of the IT capability box. In Proceedings of the Americas Conference on Information Systems 2018: Digital Disruption, AMCIS 2018, New Orleans, LA, USA, 16–18 August 2018. [Google Scholar]
- Sinha, A.; Kumar, P.; Rana, N.P.; Islam, R.; Dwivedi, Y.K. Impact of internet of things (IoT) in disaster management: A task-technology fit perspective. Ann. Oper. Res. 2019, 283, 759–794. [Google Scholar] [CrossRef] [Green Version]
- Datta, P.; Nwankpa, J.K. Digital transformation and the COVID-19 crisis continuity planning. J. Inf. Technol. Teach. Cases 2021, 11, 81–89. [Google Scholar] [CrossRef]
- De Mori, C.; Batalha, M.O.; Alfranca, O. A model for measuring technology capability in the agrifood industry companies. Br. Food J. 2016, 118, 1422–1461. [Google Scholar] [CrossRef]
- Wang, N.; Liang, H.; Zhong, W.; Xue, Y.; Xiao, J. Resource Structuring or Capability Building? An Empirical Study of the Business Value of Information Technology. J. Manag. Inf. Syst. 2014, 29, 325–367. [Google Scholar] [CrossRef]
- Wang, Y.; Lo, H.; Zhang, Q.; Xue, Y. How technological capability influences business performance: An integrated framework based on the contingency approach. J. Technol. Manag. China 2006, 1, 27–52. [Google Scholar] [CrossRef]
- Zawislak, P.A.; Alves, A.C.; Tello-Gamarra, J.; Barbieux, D.; Reichert, F.M. Innovation Capability: From Technology Development to Transaction Capability. J. Technol. Manag. Innov. 2012, 7, 14–27. [Google Scholar] [CrossRef] [Green Version]
- Zawislak, P.; Alves, A.; Tello-Gamarra, J.; Barbieux, D.; Reichert, F. Influences of the internal capabilities of firms on their innovation performance: A case study investigation in Brazil. Int. J. Manag. 2013, 30, 329. [Google Scholar]
- Ali, O.; Shrestha, A.; Soar, J.; Wamba, S.F. Cloud computing-enabled healthcare opportunities, issues, and applications: A systematic review. Int. J. Inf. Manag. 2018, 43, 146–158. [Google Scholar] [CrossRef]
- Lu, I.Y.; Chen, C.B.; Wang, C.H. Fuzzy multiattribute analysis for evaluating firm technological innovation capability. Int. J. Technol. Manag. 2007, 40, 114–130. [Google Scholar] [CrossRef]
- Wu, S.J.; Melnyk, S.A.; Flynn, B.B. Operational Capabilities: The Secret Ingredient. Decis. Sci. 2010, 41, 721–754. [Google Scholar] [CrossRef]
- Benitez, J.; Chen, Y.; Teo, T.S.H.; Ajamieh, A. Evolution of the impact of e-business technology on operational competence and firm profitability: A panel data investigation. Inf. Manag. 2018, 55, 120–130. [Google Scholar] [CrossRef]
- Ahmed, M.U.; Kristal, M.M.; Pagell, M. Impact of operational and marketing capabilities on firm performance: Evidence from economic growth and downturns. Int. J. Prod. Econ. 2014, 154, 59–71. [Google Scholar] [CrossRef]
- Braojos, J.; Benitez, J.; Llorens, J.; Ruiz, L. Impact of IT integration on the firm’s knowledge absorption and desorption. Inf. Manag. 2020, 57, 103290. [Google Scholar] [CrossRef]
- Raphael, A.; Schoemaker, P.J. Strategic assets and organizational rent. Strateg. Manag. J. 1986, 14, 33. [Google Scholar]
- Helfat, C.E.; Peteraf, M.A. The dynamic resource-based view: Capability lifecycles. Strateg. Manag. J. 2003, 24, 997–1010. [Google Scholar] [CrossRef]
- Benitez, J.; Llorens, J.; Braojos, J. How information technology influences opportunity exploration and exploitation firm’s capabilities. Inf. Manag. 2018, 55, 508–523. [Google Scholar] [CrossRef]
- Bustinza, O.F.; Molina, L.M.; Arias-Ar, D. Organizational learning and performance: Relationship between the dynamic and the operational capabilities of the firm. Afr. J. Bus. Manag. 2010, 4, 4067–4078. [Google Scholar] [CrossRef]
- Kumar, P.; Singh, A.P. Flexibility in service operations: Review, synthesis and research agenda. Benchmarking 2020, 27, 2108–2129. [Google Scholar] [CrossRef]
- Ruiz-Jiménez, J.M.; del Fuentes-Fuentes, M.M. Management capabilities, innovation, and gender diversity in the top management team: An empirical analysis in technology-based SMEs. BRQ Bus. Res. Q. 2016, 19, 107–121. [Google Scholar] [CrossRef] [Green Version]
- Ukko, J.; Nasiri, M.; Saunila, M.; Rantala, T. Sustainability strategy as a moderator in the relationship between digital business strategy and financial performance. J. Clean. Prod. 2019, 236, 117626. [Google Scholar] [CrossRef]
- Hair, J.F.J.; Black, W.C.; Babin, B.J.; Anderson, R.E. Multivariate Data Analysis; Pearson Education, Limited: London, UK, 2013. [Google Scholar]
- GUS. Główny Urząd Statystyczny, Apteki i Punkty Apteczne w 2020 r; GUS: Cracov, Poland, 2020. [Google Scholar]
- Krejcie, R.V.; Morgan, D.W. Determining sample Size for Research Activities. Educational and Psychological Measurement. Int. J. Employ. Stud. 1996, 18, 89–123. [Google Scholar]
- Tabachnick, B.; Fidell, L. Using Multivariate Statistics; Pearson Education: Upper Saddle River, NJ, USA, 2018; ISBN 9780134792859. [Google Scholar]
- Horn, J.L. Factors in Factor Analysis. Psychometrika 1965, 30, 179–185. [Google Scholar] [CrossRef] [PubMed]
- Bergek, A.; Tell, F.; Berggren, C.; Watson, J. Technological capabilities and late shakeouts: Industrial dynamics in the advanced gas turbine industry, 1987–2002. Ind. Corp. Chang. 2008, 17, 335–392. [Google Scholar] [CrossRef] [Green Version]
- Kludacz-Alessandri, M.; Walczak, R.; Hawrysz, L.; Korneta, P. The Quality of Medical Care in the Conditions of the COVID-19 Pandemic, with Particular Emphasis on the Access to Primary Healthcare and the Effectiveness of Treatment in Poland. J. Clin. Med. 2021, 10, 3502. [Google Scholar] [CrossRef]
- Mcdermott, A.M.; Conway, E.; Rousseau, D.M.; Flood, P.C. Promoting Effective Psychological Contracts Through Leadership: The Missing Link Between HR Strategy and Performance. Hum. Resour. Manag. 2013, 52, 289–310. [Google Scholar] [CrossRef]
- Andrews, R.; Beynon, M.J.; McDermott, A.M. Organizational Capability in the Public Sector: A Configurational Approach. J. Public Adm. Res. Theory 2016, 26, 239–258. [Google Scholar] [CrossRef]
- Spaulding, A.; Kash, B.A.; Johnson, C.E.; Gamm, L. Organizational capacity for change in health care: Development and validation of a scale. Health Care Manag. Rev. 2017, 42, 151–161. [Google Scholar] [CrossRef] [PubMed]
- Otto, L.; Harst, L. Investigating barriers for the implementation of telemedicine initiatives: A systematic review of reviews. In Proceedings of the Twenty-fifth Americas Conference on Information Systems, Cancun, Mexico, 15–17 August 2019. [Google Scholar]
- Hage, E.; Roo, J.P.; Van Offenbeek, M.A.G.; Boonstra, A. Implementation factors and their effect on e-Health service adoption in rural communities: A systematic literature review. BMC Health Serv. Res. 2013, 13, 19. [Google Scholar] [CrossRef] [Green Version]
- Jang-Jaccard, J.; Nepal, S.; Alem, L.; Li, J. Barriers for Delivering Telehealth in Rural Australia: A Review Based on Australian Trials and Studies. Telemed. e-Health 2014, 20, 496–504. [Google Scholar] [CrossRef]
- Saliba, V.; Legido-Quigley, H.; Hallik, R.; Aaviksoo, A.; Car, J.; McKee, M. Telemedicine across borders: A systematic review of factors that hinder or support implementation. Int. J. Med. Inform. 2012, 81, 793–809. [Google Scholar] [CrossRef]
- Hötker, E.D.V.; Ring, M.M.; Steinhäuser, J. Determinants of the Implementation of Telemedicine in the German Navy—A Mixed Methods Study. Mil. Med. 2021, 2021, usab080. [Google Scholar] [CrossRef] [PubMed]
- Govender, S.M.; Mars, M. The use of telehealth services to facilitate audiological management for children: A scoping review and content analysis. J. Telemed. Telecare 2017, 23, 392–401. [Google Scholar] [CrossRef] [PubMed]
- Gros, D.F.; Morland, L.A.; Greene, C.J.; Acierno, R.; Strachan, M.; Egede, L.E.; Tuerk, P.W.; Myrick, H.; Frueh, B.C. Delivery of Evidence-Based Psychotherapy via Video Telehealth. J. Psychopathol. Behav. Assess. 2013, 35, 506–521. [Google Scholar] [CrossRef]
- Kruse, C.S.; Bouffard, S.; Dougherty, M.; Parro, J.S. Telemedicine Use in Rural Native American Communities in the Era of the ACA: A Systematic Literature Review. J. Med. Syst. 2016, 40, 145. [Google Scholar] [CrossRef] [Green Version]
- Xu, R.; Song, X.; Liu, G. The role of organizational capability on technological innovation. In Proceedings of the 2008 ISECS International Colloquium on Computing, Communication, Control, and Management, Guangzhou, China, 3–4 August 2008; Volume 3, pp. 339–343. [Google Scholar] [CrossRef]
- Mamonov, S.; Peterson, R. The Role of IT in Innovation at the Organizational Level—A Literature Review. In Proceedings of the 53rd Hawaii International Conference on System Sciences, Maui, HI, USA, 7–10 January 2020; Volume 2020. [Google Scholar]
- Zhang, C.; Dhaliwal, J. An investigation of resource-based and institutional theoretic factors in technology adoption for operations and supply chain management. Int. J. Prod. Econ. 2009, 120, 252–269. [Google Scholar] [CrossRef]
- Baark, E.; Antonio, K.; Lo, W. Sharif Innovation sources, capabilities and competitiveness: Evidence from Hong Kong firms. In Proceedings of the DIME Final Conference, Maastricht, The Netherlands, 6–8 April 2011. [Google Scholar]
- Benitez-Amado, J.; Walczuch, R.M. Information technology, the organizational capability of proactive corporate environmental strategy and firm performance: A resource-based analysis. Eur. J. Inf. Syst. 2012, 21, 664–679. [Google Scholar] [CrossRef]
- Liu, H.; Ke, W.; Wei, K.K.; Hua, Z. The impact of IT capabilities on firm performance: The mediating roles of absorptive capacity and supply chain agility. Decis. Support. Syst. 2013, 54, 1452–1462. [Google Scholar] [CrossRef]
- Kang, T.; Chen, H.-C.; Sun, J. Does Organizational Structure Influence IT Investment and its Effects on Operational Capability? J. Res. Bus. Econ. Manag. 2016, 7, 1013–1019. [Google Scholar]
- Song, M.; Nason, R.W.; Di Benedetto, C.A. Distinctive Marketing and Information Technology Capabilities and Strategic Types: A Cross-National Investigation. J. Int. Mark. 2008, 16, 4–38. [Google Scholar] [CrossRef]
- Kahli, R.; Grover, V. Business Value of IT: An Essay on Expanding Research Directions to Keep up with the Times. J. Assoc. Inf. Syst. 2008, 9, 1. [Google Scholar] [CrossRef]
- Schryen, G. Revisiting IS business value research: What we already know, what we still need to know, and how we can get there. Eur. J. Inf. Syst. 2012, 22, 139–169. [Google Scholar] [CrossRef]
- Nevo, S.; Wade, M. Firm-level benefits of IT-enabled resources: A conceptual extension and an empirical assessment. J. Strateg. Inf. Syst. 2011, 20, 403–418. [Google Scholar] [CrossRef]
- Salas-Vallina, A.; López-Cabrales, Á.; Alegre, J.; Fernández, R. On the road to happiness at work (HAW): Transformational leadership and organizational learning capability as drivers of HAW in a healthcare context. Pers. Rev. 2017, 46, 314–338. [Google Scholar] [CrossRef]
- Floyd, S.W.; Wooldridge, B. Path Analysis of the Relationship between Competitive Strategy, Information Technology, and Financial Performance. J. Manag. Inf. Syst. 2015, 7, 47–64. [Google Scholar] [CrossRef]


| Statements | Supporting Literature | Essence |
|---|---|---|
| We regularly use emerging technologies (e.g., voice interfaces, augmented reality, artificial intelligence, blockchain, etc.) to improve the patient care process. | Fortuin and Omta (2009) [19] | Strategic capabilities (coordination and information accessibility) |
| Ali et al. (2018) [43] | ||
| We use patient experience tools and methods, such as persona and journey maps, to design and modify digital solutions. | Lu et al. (2007) [44] | Indicators of innovation effort process |
| Yeniyurt et al. (2019) [17] | ||
| We use digital tools to promote innovation, collaboration, and mobility for doctors, medical staff, and administration. | Jonker et al. (2006) [21] | Learning mechanisms |
| Mohamad et al. (2017) [22] | ||
| We use modern architectures (APIs, cloud storage, etc.) to promote speed and flexibility in implementing digital solutions. | Ziggers and Henseler (2009) [24] | Technology upgrade for motivation and commitment to change |
| Ali et al. (2018) [43] | ||
| Li and Chan (2019) [25] |
| Statement | Supporting Literature | Essence |
|---|---|---|
| We have defined, well-described, and repeatable processes for implementing digital solutions. | Christensen and Overdorf (2000) [14] | Processes and routine |
| Wu et al. (2010) [45] | ||
| Benitez et al. (2018) [51] | ||
| Helfat and Peteraf (2003) [50] | ||
| We dedicate appropriate resources to the work of digitization. | Coombs and Bierly (2006) [13] | Resources |
| Ahmed, Kristal, Pagell (2014) [47] | ||
| Raphael and Schoemaker (1986) [49] | ||
| Our organizational model encourages collaboration between doctors, medical staff, and administrative staff and IT specialists. | Guan and Ma (2003) [15] | Learning mechanisms |
| Bustinza, Molina, and Arias-Ar (2010) [52] | ||
| We have a flexible, iterative, and collaborative approach to developing digital solutions. | De Mori, Batalha, and Alfranca (2016) [38] | Job coordination and contribution |
| Kumar and Singh 2019 [53] |
| Dimension | Variable Name | Question |
|---|---|---|
| Technological capabilities | V_q2s31 | We regularly use emerging technologies (e.g., voice interfaces, augmented reality, artificial intelligence, blockchain, etc.) to improve the patient care process. |
| IV_q2s22 | We use patient experience tools and methods, such as persona and journey maps, to design and modify digital solutions. | |
| IV_q2s23 | We use digital tools to promote innovation, collaboration, and mobility for doctors, medical staff, and administrative staff. | |
| V_q2s30 | We use modern architectures (APIs, cloud storage, etc.) to promote speed and flexibility in implementing digital solutions. | |
| Operational capabilities | II_q2s6 | We have defined, well-described, and repeatable processes for implementing digital solutions. |
| II_q2s7 | We dedicate appropriate resources to the work of digitization. | |
| II_q2s8 | Our organizational model encourages collaboration between doctors, medical staff, and administrative staff and IT specialists. | |
| V_q2s29 | We have a flexible, iterative, and collaborative approach to developing digital solutions. |
| Variable | Mean | Median | Mode | Std. Deviation | Skewness | Kurtosis | Cronbach’s Alpha |
|---|---|---|---|---|---|---|---|
| IV_q2s22 | 3.26 | 3 | 4 | 1.109 | −0.711 | −0.202 | 0.841 |
| IV_q2s23 | 3.74 | 4 | 4 | 0.976 | −0.835 | 0.652 | |
| V_q2s30 | 3.38 | 4 | 4 | 1.114 | −0.815 | −0.127 | |
| V_q2s31 | 3.28 | 4 | 4 | 1.161 | −0.687 | −0.428 |
| Variable | Mean | Median | Mode | Std. Deviation | Skewness | Kurtosis | Cronbach’s Alpha |
|---|---|---|---|---|---|---|---|
| II_q2s6 | 3.85 | 4 | 4 | 0.947 | −1.162 | 1.522 | 0.809 |
| II_q2s7 | 3.87 | 4 | 4 | 0.958 | −1.054 | 1.051 | |
| II_q2s8 | 4.02 | 4 | 4 | 0.852 | −0.984 | 1.331 | |
| V_q2s29 | 3.85 | 4 | 4 | 0.962 | −0.898 | 0.680 |
| OC Variables | II_q2s6 | II_q2s7 | II_q2s8 | V_q2s29 |
|---|---|---|---|---|
| II_q2s6 | 1 | 0.643 | 0.552 | 0.447 |
| II_q2s7 | 0.643 | 1 | 0.546 | 0.471 |
| II_q2s8 | 0.552 | 0.546 | 1 | 0.442 |
| V_q2s29 | 0.447 | 0.471 | 0.442 | 1 |
| TC variables | IV_q2s22 | IV_q2s23 | V_q2s30 | V_q2s31 |
| IV_q2s22 | 1 | 0.568 | 0.612 | 0.629 |
| IV_q2s23 | 0.568 | 1 | 0.497 | 0.466 |
| V_q2s30 | 0.612 | 0.497 | 1 | 0.64 |
| V_q2s31 | 0.629 | 0.466 | 0.64 | 1 |
| Factor | Initial Eigenvalues | Extraction Sums of Squared Loadings | Rotation Sums of Squared Loadings | ||||
|---|---|---|---|---|---|---|---|
| Total | % of Variance | Cumulative % | Total | % of Variance | Cumulative % | Total | |
| 1 | 4.313 | 53.909 | 53.909 | 3.886 | 48.579 | 48.579 | 3.418 |
| 2 | 1.039 | 12.983 | 66.893 | 0.631 | 7.892 | 56.471 | 3.310 |
| 3 | 0.609 | 7.608 | 74.501 | ||||
| 4 | 0.549 | 6.867 | 81.368 | ||||
| 5 | 0.445 | 5.559 | 86.927 | ||||
| 6 | 0.375 | 4.685 | 91.612 | ||||
| 7 | 0.348 | 4.345 | 95.957 | ||||
| 0.323 | 4.043 | 100.000 | |||||
| Variable | Factor IV_q2s23 Included | Factor IV_q2s23 Deleted | ||
|---|---|---|---|---|
| Operational Capabilities | Technological Capabilities | Operational Capabilities | Technological Capabilities | |
| II_q2s6 | 0.782 | 0.788 | ||
| II_q2s7 | 0.706 | 0.722 | ||
| II_q2s8 | 0.813 | 0.765 | ||
| V_q2s29 | 0.526 | 0.520 | ||
| V_q2s30 | 0.798 | 0.787 | ||
| V_q2s31 | 0.835 | 0.840 | ||
| IV_q2s22 | 0.745 | 0.712 | ||
| IV_q2s23 | 0.431 | 0.343 | ||
| Factor | Initial Eigenvalues | Extraction Sums of Squared Loadings | Rotation Sums of Squared Loadings | ||||
|---|---|---|---|---|---|---|---|
| Total | % of Variance | Cumulative % | Total | % of Variance | Cumulative % | Total | |
| 1 | 3.798 | 54.259 | 54.259 | 3.384 | 48.346 | 48.346 | 2.950 |
| 2 | 1.039 | 14.838 | 69.098 | 0.631 | 9.014 | 57.359 | 2.867 |
| 3 | 0.607 | 8.671 | 77.769 | ||||
| 4 | 0.476 | 6.796 | 84.564 | ||||
| 5 | 0.393 | 5.617 | 90.182 | ||||
| 6 | 0.362 | 5.172 | 95.354 | ||||
| 7 | 0.325 | 4.646 | 100.000 | ||||
| Factor | CR | AVE | SQR(AVE) | Correlation between Factors |
|---|---|---|---|---|
| Operational capabilities | 0.813 | 0.525 | 0.725 | 0.697 |
| Technological capabilities | 0.835 | 0.627 | 0.792 |
| Relationship between Variables | Unstandardized Estimate | S.E. | C.R. | p | Standardized Estimate | ||
|---|---|---|---|---|---|---|---|
| Technological_capabilities | <--- | Operational_capabilities | 0.825 | 0.078 | 10.599 | *** | 0.697 |
| II_q2s6 | <--- | Operational_capabilities | 1.000 | 0.779 | |||
| II_q2s7 | <--- | Operational_capabilities | 1.062 | 0.071 | 14.858 | *** | 0.818 |
| II_q2s8 | <--- | Operational_capabilities | 0.786 | 0.062 | 12.570 | *** | 0.681 |
| V_q2s29 | <--- | Operational_capabilities | 0.781 | 0.071 | 10.998 | *** | 0.600 |
| V_q2s30 | <--- | Technological_capabilities | 1.000 | 0.785 | |||
| V_q2s31 | <--- | Technological_capabilities | 1.057 | 0.072 | 14.739 | *** | 0.796 |
| IV_q2s22 | <--- | Technological_capabilities | 1.007 | 0.068 | 14.722 | *** | 0.795 |
| Measure | Estimate | Threshold |
|---|---|---|
| CMIN | 18.806 | |
| DF | 13.000 | |
| CMIN/DF | 1.447 | Between 1 and 3 |
| CFI | 0.995 | >0.95 |
| SRMR | 0.031 | <0.08 |
| RMSEA | 0.035 | <0.06 |
| PClose | 0.750 | >0.05 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kruszyńska-Fischbach, A.; Sysko-Romańczuk, S.; Rafalik, M.; Walczak, R.; Kludacz-Alessandri, M. Organizational E-Readiness for the Digital Transformation of Primary Healthcare Providers during the COVID-19 Pandemic in Poland. J. Clin. Med. 2022, 11, 133. https://doi.org/10.3390/jcm11010133
Kruszyńska-Fischbach A, Sysko-Romańczuk S, Rafalik M, Walczak R, Kludacz-Alessandri M. Organizational E-Readiness for the Digital Transformation of Primary Healthcare Providers during the COVID-19 Pandemic in Poland. Journal of Clinical Medicine. 2022; 11(1):133. https://doi.org/10.3390/jcm11010133
Chicago/Turabian StyleKruszyńska-Fischbach, Agnieszka, Sylwia Sysko-Romańczuk, Mateusz Rafalik, Renata Walczak, and Magdalena Kludacz-Alessandri. 2022. "Organizational E-Readiness for the Digital Transformation of Primary Healthcare Providers during the COVID-19 Pandemic in Poland" Journal of Clinical Medicine 11, no. 1: 133. https://doi.org/10.3390/jcm11010133
APA StyleKruszyńska-Fischbach, A., Sysko-Romańczuk, S., Rafalik, M., Walczak, R., & Kludacz-Alessandri, M. (2022). Organizational E-Readiness for the Digital Transformation of Primary Healthcare Providers during the COVID-19 Pandemic in Poland. Journal of Clinical Medicine, 11(1), 133. https://doi.org/10.3390/jcm11010133






