Experience of Patients with Diabetes and Other Cardiovascular Risk Factors with Health Professionals and Healthcare in Spain
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Study Population
2.2. Assessments
2.3. Statistical Analysis
3. Results
3.1. Patient Location and Characteristics
3.2. Degree of Control of Cardiovascular Risk Factors and Adherence
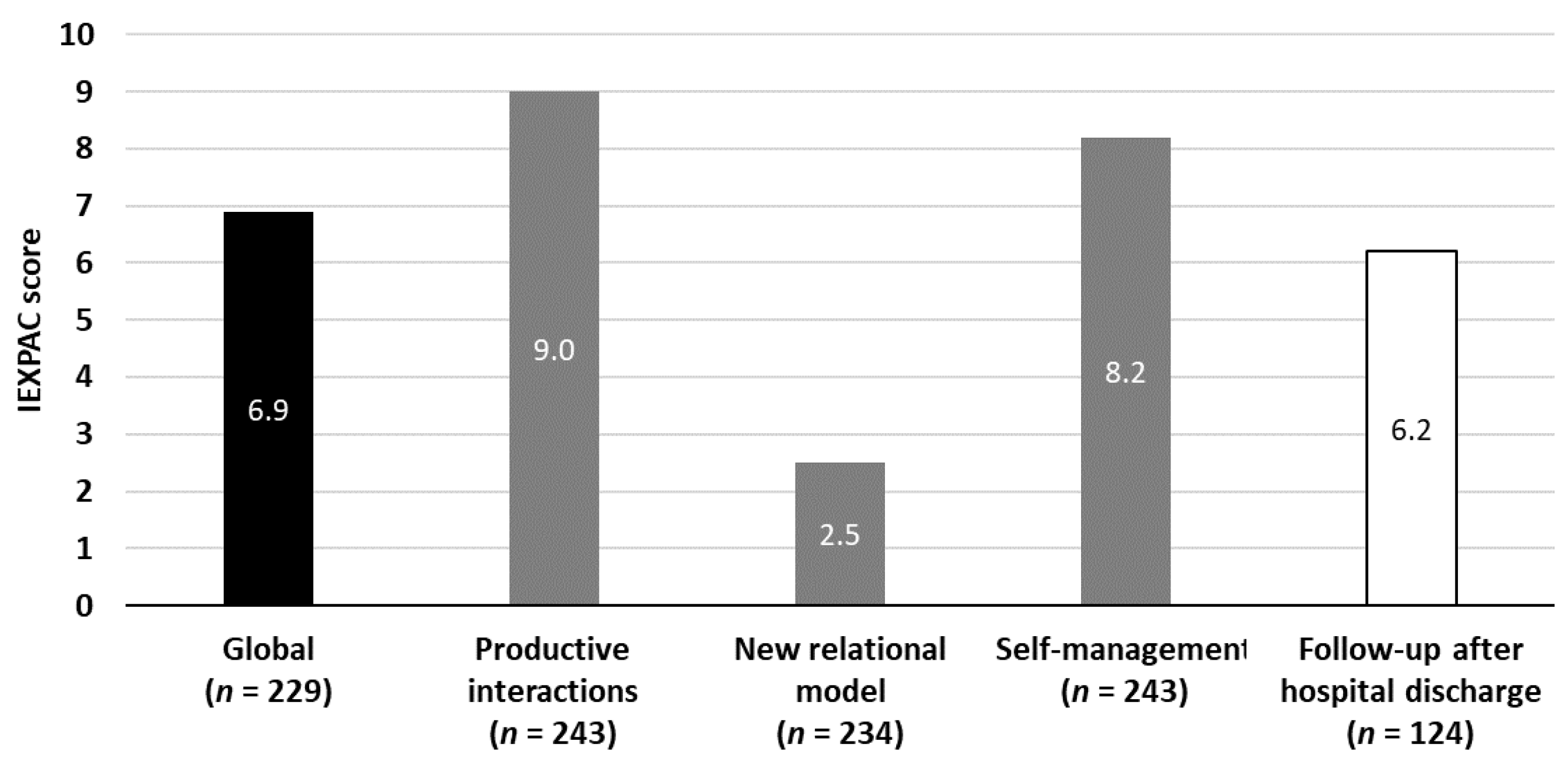
3.3. Patient Experience with Healthcare Professionals and Services
3.4. Relationship between Experience and Comorbidity, Adherence and Degree of Control
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Buttorff, C.; Ruder, T. Multiple Chronic Conditions in the United States; RAND Coorporation: Santa Monica, CA, USA, 2017. [Google Scholar]
- Fortin, M.; Bravo, G.; Hudon, C.; Lapointe, L.; Almirall, J.; Dubois, M.F.; Vanasse, A. Relationship between multimorbidity and health-related quality of life of patients in primary care. Qual. Life Res. 2006, 15, 83–91. [Google Scholar] [CrossRef]
- Fortin, M.; Bravo, G.; Hudon, C.; Lapointe, L.; Dubois, M.F.; Almirall, J. Psychological distress and multimorbidity in primary care. Ann. Fam. Med. 2006, 4, 417–422. [Google Scholar] [CrossRef] [PubMed]
- van der Heide, I.; Snoeijs, S.; Melchiorre, M.G.; Quattrini, S.; Boerma, W.; Schellevis, F.; Rijken, M. Innovating Care for People with Multiple Chronic Conditions in Europe; NIVEL (Netherlands Institute for Health Services Research): Utrecht, The Netherlands, 2015. [Google Scholar]
- Nuno, R.; Coleman, K.; Bengoa, R.; Sauto, R. Integrated care for chronic conditions: The contribution of the ICCC Framework. Health Policy 2012, 105, 55–64. [Google Scholar] [CrossRef] [PubMed]
- Soriguer, F.; Goday, A.; Bosch-Comas, A.; Bordiu, E.; Calle-Pascual, A.; Carmena, R.; Casamitjana, R.; Castano, L.; Castell, C.; Catala, M.; et al. Prevalence of diabetes mellitus and impaired glucose regulation in Spain: The Di@bet.es Study. Diabetologia 2012, 55, 88–93. [Google Scholar] [CrossRef] [PubMed]
- Cinza Sanjurjo, S.; Prieto Díaz, M.Á.; Llisterri Caro, J.L.; Pallarés Carratalá, V.; Barquilla García, A.; Rodríguez Padial, L.; Díaz Rodríguez, Á.; Polo García, J.; Vergara Martín, J.; Vidal Pérez, R.; et al. Características basales y manejo clínico de los primeros 3.000 pacientes incluidos en el estudio IBERICAN (Identificación de la población española de riesgo cardiovascular y renal). Semer. Med. Fam. 2017, 43, 493–500. [Google Scholar] [CrossRef] [PubMed]
- Escribano Serrano, J.; Mendez-Esteban, M.I.; Garcia-Bonilla, A.; Marquez-Ferrando, M.; Casto-Jarillo, C.; Berruguilla Perez, E.; Calero Ruiz, M.M.; Gonzalez Borrachero, M.L.; Santotoribio, J.D.; Michan-Dona, A. Prevalence of diabetes, use of antidiabetic drugs and degree of glycaemic control in the province of Cadiz (2014–2016): A population-based study. Rev. Clin. Esp. 2019, 219, 177–183. [Google Scholar] [CrossRef]
- Hopman, P.; Heins, M.J.; Korevaar, J.C.; Rijken, M.; Schellevis, F.G. Health care utilization of patients with multiple chronic diseases in the Netherlands: Differences and underlying factors. Eur. J. Intern. Med. 2016, 35, 44–50. [Google Scholar] [CrossRef]
- Mata-Cases, M.; Franch-Nadal, J.; Real, J.; Cedenilla, M.; Mauricio, D. Prevalence and coprevalence of chronic comorbid conditions in patients with type 2 diabetes in Catalonia: A population-based cross-sectional study. BMJ Open 2019, 9, e031281. [Google Scholar] [CrossRef]
- Aguado, A.; Moratalla-Navarro, F.; López-Simarro, F.; Moreno, V. MorbiNet: Multimorbidity networks in adult general population. Analysis of type 2 diabetes mellitus comorbidity. Sci. Rep. 2020, 10, 2416. [Google Scholar] [CrossRef]
- Wagner, E.H.; Austin, B.T.; Von Korff, M. Organizing care for patients with chronic illness. Milbank Q. 1996, 74, 511–544. [Google Scholar] [CrossRef]
- National Academies of Science, Engineering, Medicine. Crossing the Global Quality Chasm: Improving Health Care Worldwide; National Academies of Science, Engineering, Medicine: Washington, DC, USA, 2018; Available online: http://www.nationalacademies.org/hmd/~/media/Files/Report%20Files/2001/Crossing-the-Quality-Chasm/Quality%20Chasm%202001%20%20report%20brief.pdf (accessed on 25 April 2021).
- Doyle, C.; Lennox, L.; Bell, D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open 2013, 3. [Google Scholar] [CrossRef]
- Haugum, M.; Danielsen, K.; Iversen, H.H.; Bjertnaes, O. The use of data from national and other large-scale user experience surveys in local quality work: A systematic review. Int. J. Qual. Health Care 2014, 26, 592–605. [Google Scholar] [CrossRef]
- Bastemeijer, C.M.; Boosman, H.; van Ewijk, H.; Verweij, L.M.; Voogt, L.; Hazelzet, J.A. Patient experiences: A systematic review of quality improvement interventions in a hospital setting. Patient Relat. Outcome Meas. 2019, 10, 157–169. [Google Scholar] [CrossRef]
- Orozco-Beltran, D.; de Toro, J.; Galindo, M.J.; Marin-Jimenez, I.; Casellas, F.; Fuster-RuizdeApodaca, M.J.; Garcia-Vivar, M.L.; Hormigo-Pozo, A.; Guilabert, M.; Sanchez-Vega, N.; et al. Healthcare Experience and their Relationship with Demographic, Disease and Healthcare-Related Variables: A Cross-Sectional Survey of Patients with Chronic Diseases Using the IEXPAC Scale. Patient 2019, 12, 307–317. [Google Scholar] [CrossRef] [PubMed]
- Mira, J.J.; Nuno-Solinis, R.; Guilabert-Mora, M.; Solas-Gaspar, O.; Fernandez-Cano, P.; Gonzalez-Mestre, M.A.; Contel, J.C.; Del Rio-Camara, M. Development and Validation of an Instrument for Assessing Patient Experience of Chronic Illness Care. Int. J. Integr. Care 2016, 16, 13. [Google Scholar] [CrossRef] [PubMed]
- Hickman, R.L.; Clochesy, J.M.; Alaamri, M. Effects of an eHealth Intervention on Patient-Provider Interaction and Functional Health Literacy in Adults With Hypertension. SAGE Open Nurs. 2021, 7, 23779608211005863. [Google Scholar] [CrossRef]
- Robert, C.; Erdt, M.; Lee, J.; Cao, Y.; Naharudin, N.B.; Theng, Y.L. Effectiveness of eHealth Nutritional Interventions for Middle-Aged and Older Adults: Systematic Review and Meta-analysis. J. Med. Internet Res. 2021, 23, e15649. [Google Scholar] [CrossRef] [PubMed]
- Orozco-Beltran, D.; Sánchez-Molla, M.; Sanchez, J.J.; Mira, J.J. Telemedicine in Primary Care for Patients With Chronic Conditions: The ValCrònic Quasi-Experimental Study. J. Med. Internet Res. 2017, 19, e400. [Google Scholar] [CrossRef]
- Gómez-García, A.; Ferreira de Campos, K.; Orozco-Beltrán, D.; Artola-Menéndez, S.; Grahit-Vidosa, V.; Fierro-Alario, M.J.; Alonso-Jerez, J.L.; Villabrille-Arias, M.C.; Zuazagoitia-Nubla, J.F.; Ledesma-Rodríguez, R.; et al. Impacto de los Centros Avanzados de Diabetes en la experiencia de los pacientes con diabetes tipo 2 con la atención sanitaria mediante la herramienta IEXPAC. Endocrinol. Diabetes Nutr. 2020. [Google Scholar] [CrossRef]
- Berwick, D.M.; Nolan, T.W.; Whittington, J. The triple aim: Care, health, and cost. Health Aff. (Millwood) 2008, 27, 759–769. [Google Scholar] [CrossRef]
- Linetzky, B.; Jiang, D.; Funnell, M.M.; Curtis, B.H.; Polonsky, W.H. Exploring the role of the patient-physician relationship on insulin adherence and clinical outcomes in type 2 diabetes: Insights from the MOSAIc study. J. Diabetes 2017, 9, 596–605. [Google Scholar] [CrossRef] [PubMed]
- Chiou, S.J.; Liao, K.; Huang, Y.T.; Lin, W.; Hsieh, C.J. Synergy between the pay-for-performance scheme and better physician-patient relationship might reduce the risk of retinopathy in patients with type 2 diabetes. J. Diabetes Investig. 2021, 12, 819–827. [Google Scholar] [CrossRef]
- Orozco-Beltrán, D.; Artola-Menéndez, S.; Hormigo-Pozo, A.; Cararach-Salami, D.; Alonso-Jerez, J.L.; Álvaro-Grande, E.; Villabrille-Arias, C.; de Toro-Santos, F.J.; Galindo-Puerto, M.J.; Marín-Jiménez, I.; et al. Healthcare experience among patients with type 2 diabetes: A cross-sectional survey using the IEXPAC tool. Endocrinol. Diabetes Metab. 2021, 4, e00220. [Google Scholar] [CrossRef]
- Lu, C.; Hu, Y.; Xie, J.; Fu, Q.; Leigh, I.; Governor, S.; Wang, G. The Use of Mobile Health Applications to Improve Patient Experience: Cross-Sectional Study in Chinese Public Hospitals. JMIR Mhealth Uhealth 2018, 6, e126. [Google Scholar] [CrossRef] [PubMed]
- Al-Tannir, M.; AlGahtani, F.; Abu-Shaheen, A.; Al-Tannir, S.; AlFayyad, I. Patient experiences of engagement with care plans and healthcare professionals’ perceptions of that engagement. BMC Health Serv. Res. 2017, 17, 853. [Google Scholar] [CrossRef]
- Caballero, A.E.; Ceriello, A.; Misra, A.; Aschner, P.; McDonnell, M.E.; Hassanein, M.; Ji, L.; Mbanya, J.C.; Fonseca, V.A. COVID-19 in people living with diabetes: An international consensus. J. Diabetes Complicat. 2020, 34, 107671. [Google Scholar] [CrossRef]
- Iyengar, K.; Mabrouk, A.; Jain, V.K.; Venkatesan, A.; Vaishya, R. Learning opportunities from COVID-19 and future effects on health care system. Diabetes Metab. Syndr. 2020, 14, 943–946. [Google Scholar] [CrossRef]
- Medina-Mirapeix, F.; Oliveira-Sousa, S.L.; Escolar-Reina, P.; Sobral-Ferreira, M.; Lillo-Navarro, M.C.; Collins, S.M. Continuity of care in hospital rehabilitation services: A qualitative insight from inpatients’ experience. Braz. J. Phys. Ther. 2017, 21, 85–91. [Google Scholar] [CrossRef]
- Rapport, F.; Hibbert, P.; Baysari, M.; Long, J.C.; Seah, R.; Zheng, W.Y.; Jones, C.; Preece, K.; Braithwaite, J. What do patients really want? An in-depth examination of patient experience in four Australian hospitals. BMC Health Serv. Res. 2019, 19, 38. [Google Scholar] [CrossRef]
- Soler, R.S.; Juvinya Canal, D.; Noguer, C.B.; Poch, C.G.; Brugada Motge, N.; Del Mar Garcia Gil, M. Continuity of care and monitoring pain after discharge: Patient perspective. J. Adv. Nurs. 2010, 66, 40–48. [Google Scholar] [CrossRef] [PubMed]
- Reiner, Z.; Sonicki, Z.; Tedeschi-Reiner, E. Physicians’ perception, knowledge and awareness of cardiovascular risk factors and adherence to prevention guidelines: The PERCRO-DOC survey. Atherosclerosis 2010, 213, 598–603. [Google Scholar] [CrossRef]
- Reiner, Z.; Sonicki, Z.; Tedeschi-Reiner, E. Public perceptions of cardiovascular risk factors in Croatia: The PERCRO survey. Prev. Med. 2010, 51, 494–496. [Google Scholar] [CrossRef]
- Mosca, L.; Linfante, A.H.; Benjamin, E.J.; Berra, K.; Hayes, S.N.; Walsh, B.W.; Fabunmi, R.P.; Kwan, J.; Mills, T.; Simpson, S.L. National study of physician awareness and adherence to cardiovascular disease prevention guidelines. Circulation 2005, 111, 499–510. [Google Scholar] [CrossRef]
- Dallongeville, J.; Banegas, J.R.; Tubach, F.; Guallar, E.; Borghi, C.; De Backer, G.; Halcox, J.P.; Massó-González, E.L.; Perk, J.; Sazova, O.; et al. Survey of physicians’ practices in the control of cardiovascular risk factors: The EURIKA study. Eur. J. Prev. Cardiol. 2012, 19, 541–550. [Google Scholar] [CrossRef] [PubMed]
- Doroodchi, H.; Abdolrasulnia, M.; Foster, J.A.; Foster, E.; Turakhia, M.P.; Skelding, K.A.; Sagar, K.; Casebeer, L.L. Knowledge and attitudes of primary care physicians in the management of patients at risk for cardiovascular events. BMC Fam. Pract. 2008, 9. [Google Scholar] [CrossRef] [PubMed]
- Pepió Vilaubí, J.M.; Orozco-Beltrán, D.; Gonçalves, A.Q.; Rodriguez Cumplido, D.; Aguilar Martin, C.; Lopez-Pineda, A.; Gil-Guillen, V.F.; Quesada, J.A.; Carratala-Munuera, C. Adherence to European Clinical Practice Guidelines for Secondary Prevention of Cardiovascular Disease: A Cohort Study. Int. J. Environ. Res. Public Health 2018, 15, 1233. [Google Scholar] [CrossRef] [PubMed]
- Ortiz Tobarra, M.T.; Orozco Beltrán, D.; Gil Guillén, V.; Terol Moltó, C. [Frequency of attendance and degree of control of type-2 diabetic patients]. Aten. Primaria 2008, 40, 139–144. [Google Scholar] [CrossRef][Green Version]
| Variable | IEXPAC Population (n = 248) | IEXPAC 11 Items (n = 229) | IEXPAC Item No. 12 (n = 124) |
|---|---|---|---|
| Age (years), mean (SD) | 70.9 (9.17) | 70.7 (9.29) | 70.3 (9.33) |
| Woman, n (%) | 119 (48.0) | 111 (48.5) | 52 (41.9) |
| Caucasian, n (%) | 247 (99.6) | 228 (99.6%) | 123 (99.2) |
| Weight (kg), mean (SD) | 81.4 (14.1) | ||
| BMI (kg/m2), mean (SD) | 31.3 (4.9) | ||
| Patient living with others, n (%) | 221 (89.1) | 204 (89.9) | 113 (92.6) |
| Risk factors, mean (SD) | |||
| HbA1c (%) | 6.73 (0.98) | 6.74 (0.99) | 6.87 (1.05) |
| LDLc | 85.95 (27.67) | 85.93 (28.1) | 86.59 (28.38) |
| SBP (mm/Hg) | 133.01 (13.65) | 132.51 (13.81) | 133.93 (14.01) |
| DBP (mm/Hg) | 75.63 (8.96) | 75.42 (8.98) | 75.98 (9.07) |
| Mean no. of risk factors according to therapeutic guidelines (SD) | 2.00 (0.83) | ||
| Mean No. of controlled risk factors based on clinical opinion (SD) | 2.43 (0.70) | ||
| Treatments, mean (SD) | |||
| No. daily OAD | 2.62 (1.79) | 2.67 (1.84) | 2.63 (1.92) |
| No. daily AHT | 1.77 (0.96) | 1.77 (0.98) | 1.79 (1.06) |
| No. daily LLD | 1.16 (0.46) | 1.17 (0.47) | 1.15 (0.46) |
| No. daily OAD, AHT and LLD | 5.55 (2.26) | 5.60 (2.31) | 5.58 (2.50) |
| Mean No. of concomitant tablets (other than OAD, AHT and LLD) (SD) | 4.19 (3.74) | 4.23 (3.78) | 4.51 (4.02) |
| Mean No. of concomitant tablets (OAD, AHT, LLD + concomitant drugs) (SD) | 9.74 (4.40) | 9.83 (4.44) | 10.09 (4.70) |
| Diabetes-related complications, n (%) | |||
| Retinopathy | 15 (6.3) | 15 (6.8) | 11 (9.1) |
| Nephropathy | 38 (15.6) | 35 (15.6) | 28 (22.8) |
| Neuropathy | 6 (2.5) | 5 (2.2) | 3 (2.4) |
| Diabetic foot | 1 (0.4) | 1 (0.4) | 0 |
| Comorbidities, n (%) | |||
| Coronary heart disease | 50 (20.2) | 47 (20.5) | 28 (22.5) |
| Heart failure | 16 (6.5) | 15 (6.6) | 10 (8.1) |
| Occlusive peripheral artery disease | 13 (5.2) | 12 (5.3) | 5 (4.1) |
| Cerebrovascular disease | 21 (8.5) | 21 (9.2) | 10 (8.1) |
| Depression | 40 (16.2) | 38 (16.7) | 18 (14.6) |
| Arthrosis | 107 (43.7) | 99 (43.8) | 55 (45.1) |
| Chronic obstructive pulmonary disease | 20 (8.1) | 17 (7.5) | 11 (9.0) |
| Dimension | Item | Mean Score (From 1—Never to 5—Always) | % “Always” or “Almost Always” | |
|---|---|---|---|---|
| Dimension 1 Productive interactions | 1 | They respect my lifestyle | 4.6 | 91.9 |
| 2 | They are coordinated in offering me good care | 4.5 | 87.0 | |
| 5 | They ask me about and help me follow my treatment plan | 4.7 | 94.3 | |
| 9 | They are concerned about my wellbeing | 4.6 | 94.3 | |
| Dimension 2 New relational model | 3 | They help me become informed via the internet | 2.0 | 15.4 |
| 7 | I use the internet and my mobile phone to consult my clinical record | 1.5 | 8.1 | |
| 11 | They encourage me to talk with other patients | 2.6 | 27.4 | |
| Dimension 3 Patient’s self-care | 4 | Now I know how to look after myself better | 4.3 | 82.4 |
| 6 | We agree on objectives to have a healthy life and to control my health problems better | 4.6 | 89.5 | |
| 8 | They ensure I take my medication correctly | 4.6 | 91.5 | |
| 10 | They inform me about health and social resources that can help me | 3.6 | 59.4 | |
| Mean score (from 0—never to 10—always) | % “always” or “almost always” | |||
| Item 12 Continued care after hospital discharge | 12 | They care about me upon my arrival home after being in hospital | 6.2 | 57.3 |
| IEXPAC Score | HbA1c | LDLc | Blood Pressure | All Factors | ||||
|---|---|---|---|---|---|---|---|---|
| Control | No Control | Control | No Control | Control | No Control | Control | No Control | |
| Total | 6.8 | 7.1 * | 6.9 | 6.9 | 6.8 | 7.0 | 6.6 | 7.0 * |
| Productive relationships | 8.9 | 9.2 | 9.0 | 8.9 | 8.9 | 9.1 | 8.7 | 9.1 |
| New relational model | 2.4 | 2.8 | 2.4 | 2.7 | 2.6 | 2.3 | 2.0 | 2.7 * |
| Self-management | 8.1 | 8.5 | 8.2 | 8.1 | 8.0 | 8.4 | 7.9 | 8.3 * |
| IEXPAC Score | OAD | AHT | LLD | Total | ||||
|---|---|---|---|---|---|---|---|---|
| Adherent | Non-Adherent | Adherent | Non-Adherent | Adherent | Non-Adherent | Adherent | Non-Adherent | |
| Total | 6.9 | 6.8 | 6.9 | 6.7 | 7.0 * | 6.4 | 7.0 | 6.6 |
| Productive relationships | 9.0 | 9.0 | 9.0 | 8.9 | 9.1 ** | 8.4 | 9.0 | 8.8 |
| New relational model | 2.5 | 2.4 | 2.5 | 2.1 | 2.6 | 2.1 | 2.6 | 2.3 |
| Self-management | 8.2 | 8.0 | 8.2 | 8.1 | 8.2 | 7.7 | 8.3 | 7.9 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Orozco-Beltrán, D.; Cinza-Sanjurjo, S.; Escribano-Serrano, J.; López-Simarro, F.; Fernández, G.; Gómez-García, A.; Cedenilla-Horcajuelo, M.; Ferreira de Campos, K. Experience of Patients with Diabetes and Other Cardiovascular Risk Factors with Health Professionals and Healthcare in Spain. J. Clin. Med. 2021, 10, 2831. https://doi.org/10.3390/jcm10132831
Orozco-Beltrán D, Cinza-Sanjurjo S, Escribano-Serrano J, López-Simarro F, Fernández G, Gómez-García A, Cedenilla-Horcajuelo M, Ferreira de Campos K. Experience of Patients with Diabetes and Other Cardiovascular Risk Factors with Health Professionals and Healthcare in Spain. Journal of Clinical Medicine. 2021; 10(13):2831. https://doi.org/10.3390/jcm10132831
Chicago/Turabian StyleOrozco-Beltrán, Domingo, Sergio Cinza-Sanjurjo, José Escribano-Serrano, Flora López-Simarro, Gonzalo Fernández, Antón Gómez-García, Marta Cedenilla-Horcajuelo, and Karine Ferreira de Campos. 2021. "Experience of Patients with Diabetes and Other Cardiovascular Risk Factors with Health Professionals and Healthcare in Spain" Journal of Clinical Medicine 10, no. 13: 2831. https://doi.org/10.3390/jcm10132831
APA StyleOrozco-Beltrán, D., Cinza-Sanjurjo, S., Escribano-Serrano, J., López-Simarro, F., Fernández, G., Gómez-García, A., Cedenilla-Horcajuelo, M., & Ferreira de Campos, K. (2021). Experience of Patients with Diabetes and Other Cardiovascular Risk Factors with Health Professionals and Healthcare in Spain. Journal of Clinical Medicine, 10(13), 2831. https://doi.org/10.3390/jcm10132831






