Cangrelor Use in Routine Practice: A Two-Center Experience
Abstract
:1. Introduction
2. Materials and Methods
2.1. Source Population and Standard Procedures
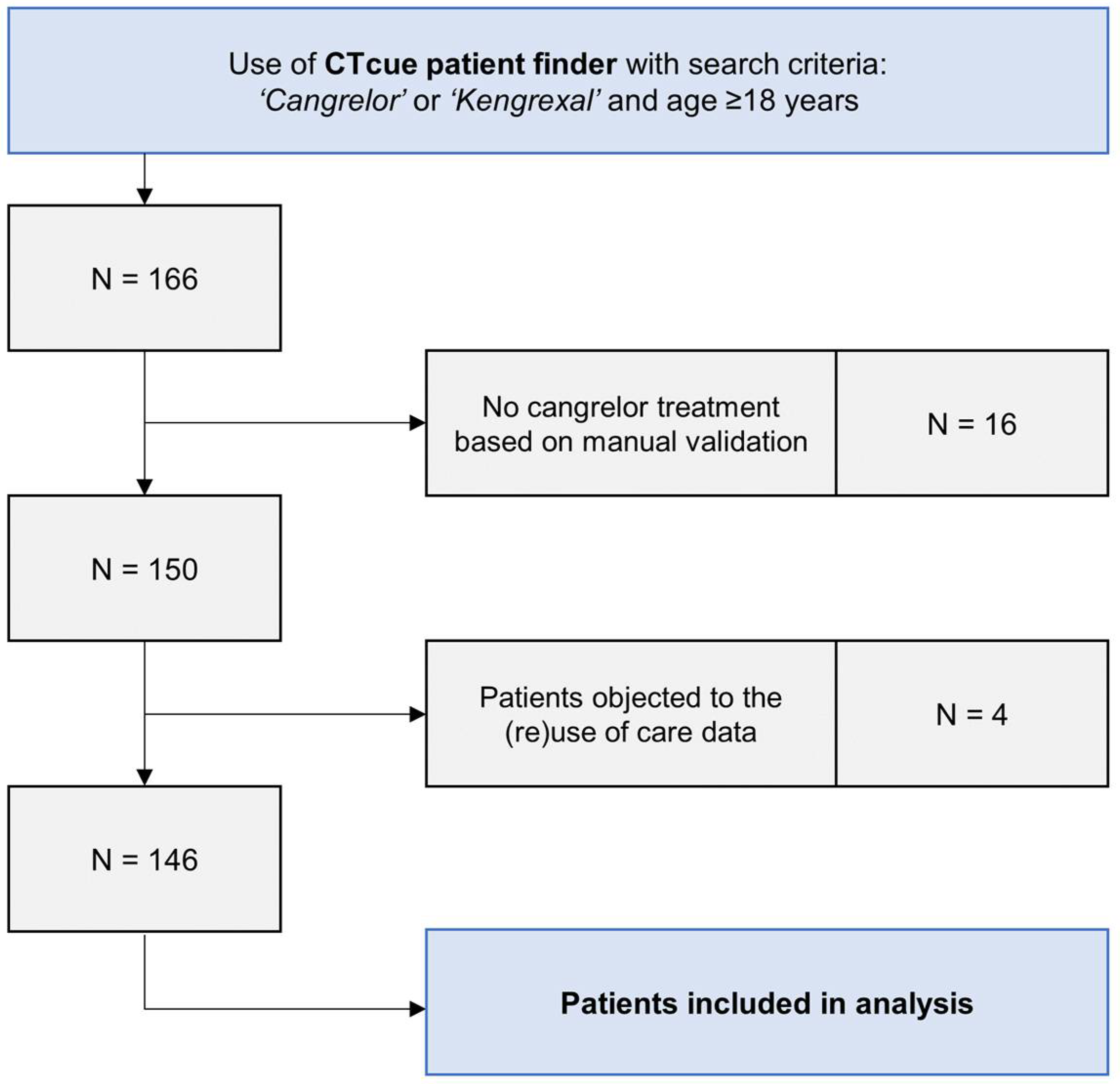
2.2. Patient Identification Method and Data Collection
2.3. Clinical Outcomes
2.4. Statistical Methods
3. Results
3.1. Patient and Procedural Characteristics
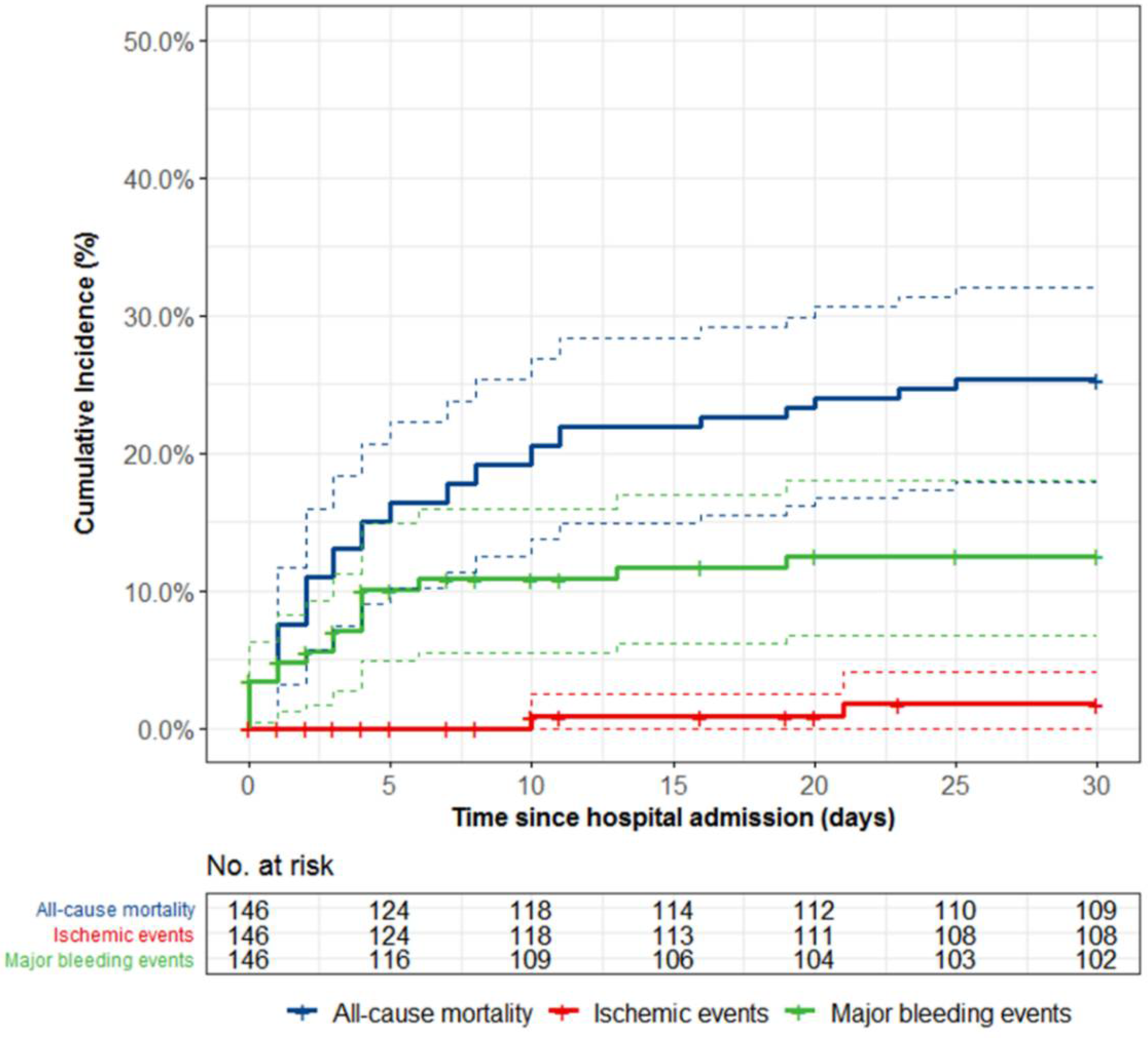
3.2. Clinical Outcomes
4. Discussion
4.1. Ischemic and Bleeding Complications
4.2. Timing and Choice of Oral P2Y12-Inhibititors
4.3. Future Directions
4.4. Limitatioins
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Collet, J.-P.; Thiele, H.; Barbato, E.; Barthélémy, O.; Bauersachs, J.; Bhatt, D.L.; Dendale, P.; Dorobantu, M.; Edvardsen, T.; Folliguet, T.; et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The Task Force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur. Heart J. 2021, 42, 1289–1367. [Google Scholar] [CrossRef]
- Ibanez, B.; James, S.; Agewall, S.; Antunes, M.J.; Bucciarelli-Ducci, C.; Bueno, H.; Caforio, A.L.P.; Crea, F.; Goudevenos, J.A.; Halvorsen, S.; et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur. Hear. J. 2018, 39, 119–177. [Google Scholar] [CrossRef]
- Akers, W.S.; Oh, J.J.; Oestreich, J.H.; Ferraris, S.; Wethington, M.; Steinhubl, S.R. Pharmacokinetics and Pharmacodynamics of a Bolus and Infusion of Cangrelor: A Direct, Parenteral P2Y12 Receptor Antagonist. J. Clin. Pharmacol. 2010, 50, 27–35. [Google Scholar] [CrossRef]
- Harrington, R.A.; Stone, G.W.; McNulty, S.; White, H.D.; Lincoff, A.M.; Gibson, C.M.; Pollack, C.V.; Montalescot, G.; Mahaffey, K.W.; Kleiman, N.S.; et al. Platelet Inhibition with Cangrelor in Patients Undergoing PCI. N. Engl. J. Med. 2009, 361, 2318–2329. [Google Scholar] [CrossRef] [PubMed]
- Bhatt, D.L.; Lincoff, A.M.; Gibson, C.M.; Stone, G.W.; McNulty, S.; Montalescot, G.; Kleiman, N.S.; Goodman, S.G.; White, H.D.; Mahaffey, K.W.; et al. Intravenous Platelet Blockade with Cangrelor during PCI. N. Engl. J. Med. 2009, 361, 2330–2341. [Google Scholar] [CrossRef]
- Bhatt, D.L.; Stone, G.W.; Mahaffey, K.W.; Gibson, C.M.; Steg, P.G.; Hamm, C.W.; Price, M.J.; Leonardi, S.; Gallup, D.; Bramucci, E.; et al. Effect of Platelet Inhibition with Cangrelor during PCI on Ischemic Events. N. Engl. J. Med. 2013, 368, 1303–1313. [Google Scholar] [CrossRef]
- Steg, P.G.; Bhatt, D.L.; Hamm, C.W.; Stone, G.W.; Gibson, C.M.; Mahaffey, K.W.; Leonardi, S.; Liu, T.; Skerjanec, S.; Day, J.; et al. Effect of cangrelor on periprocedural outcomes in percutaneous coronary interventions: A pooled analysis of patient-level data. Lancet 2013, 382, 1981–1992. [Google Scholar] [CrossRef]
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Chaitman, B.R.; Bax, J.J.; Morrow, D.A.; White, H.D. Fourth Universal Definition of Myocardial Infarction (2018). J. Am. Coll. Cardiol. 2018, 72, 2231–2264. [Google Scholar] [CrossRef] [PubMed]
- Cutlip, D.E.; Windecker, S.; Mehran, R.; Boam, A.; Cohen, D.J.; Van Es, G.-A.; Steg, P.G.; Morel, M.-A.; Mauri, L.; Vranckx, P.; et al. Clinical End Points in Coronary Stent Trials. Circulation 2007, 115, 2344–2351. [Google Scholar] [CrossRef] [PubMed]
- Mehran, R.; Rao, S.V.; Bhatt, D.L.; Gibson, C.M.; Caixeta, A.; Eikelboom, J.; Kaul, S.; Wiviott, S.D.; Menon, V.; Nikolsky, E.; et al. Standardized Bleeding Definitions for Cardiovascular Clinical Trials: A consensus report from the bleeding academic research consortium. Circulation 2011, 123, 2736–2747. [Google Scholar] [CrossRef]
- Grimfjärd, P.; Lagerqvist, B.; Erlinge, D.; Varenhorst, C.; James, S. Clinical use of cangrelor: Nationwide experience from the Swedish Coronary Angiography and Angioplasty Registry (SCAAR). Eur. Hear. J. Cardiovasc. Pharmacother. 2019, 5, 151–157. [Google Scholar] [CrossRef] [PubMed]
- Vaduganathan, M.; Qamar, A.; Badreldin, H.A.; Faxon, D.P.; Bhatt, D.L. Cangrelor Use in Cardiogenic Shock: A Single-Center Real-World Experience. JACC: Cardiovasc. Interv. 2017, 10, 1712–1714. [Google Scholar] [CrossRef]
- Iqbal, J.; Sumaya, W.; Tatman, V.; Parviz, Y.; Morton, A.C.; Grech, E.D.; Campbell, S.; Storey, R.F.; Gunn, J. Incidence and predictors of stent thrombosis: A single-centre study of 5,833 consecutive patients undergoing coronary artery stenting. EuroIntervention 2013, 9, 62–69. [Google Scholar] [CrossRef] [PubMed]
- Parodi, G.; Valenti, R.; Bellandi, B.; Migliorini, A.; Marcucci, R.; Comito, V.; Carrabba, N.; Santini, A.; Gensini, G.F.; Abbate, R.; et al. Comparison of Prasugrel and Ticagrelor Loading Doses in ST-Segment Elevation Myocardial Infarction Patients. J. Am. Coll. Cardiol. 2013, 61, 1601–1606. [Google Scholar] [CrossRef] [PubMed]
- Alexopoulos, D.; Xanthopoulou, I.; Gkizas, V.; Kassimis, G.; Theodoropoulos, K.C.; Makris, G.; Koutsogiannis, N.; Damelou, A.; Tsigkas, G.; Davlouros, P.; et al. Randomized Assessment of Ticagrelor Versus Prasugrel Antiplatelet Effects in Patients with ST-Segment–Elevation Myocardial Infarction. Circ. Cardiovasc. Interv. 2012, 5, 797–804. [Google Scholar] [CrossRef] [PubMed]
- Součková, L.; Opatřilová, R.; Suk, P.; Čundrle, I.; Pavlík, M.; Zvoníček, V.; Hlinomaz, O.; Šrámek, V. Impaired bioavailability and antiplatelet effect of high-dose clopidogrel in patients after cardiopulmonary resuscitation (CPR). Eur. J. Clin. Pharmacol. 2012, 69, 309–317. [Google Scholar] [CrossRef] [PubMed]
- Ratcovich, H.; Sadjadieh, G.; Andersson, H.; Frydland, M.; Wiberg, S.; Dridi, N.; Kjaergaard, J.; Holmvang, L. The effect of TIcagrelor administered through a nasogastric tube to COMAtose patients undergoing acute percutaneous coronary intervention: The TICOMA study. EuroIntervention 2017, 12, 1782–1788. [Google Scholar] [CrossRef]
- Weeks, P.A.; Sieg, A.; Paruthi, C.; Rajapreyar, I. Antiplatelet Therapy Considerations in Ischemic Cardiogenic Shock. J. Cardiovasc. Pharmacol. Ther. 2015, 20, 370–377. [Google Scholar] [CrossRef]
- Steblovnik, K.; Blinc, A.; Mijovski, M.B.; Kranjec, I.; Melkič, E.; Noc, M. Platelet reactivity in comatose survivors of cardiac arrest undergoing percutaneous coronary intervention and hypothermia. EuroIntervention 2015, 10, 1418–1424. [Google Scholar] [CrossRef]
- Ibrahim, K.; Christoph, M.; Schmeinck, S.; Schmieder, K.; Steiding, K.; Schoener, L.; Pfluecke, C.; Quick, S.; Mues, C.; Jellinghaus, S.; et al. High rates of prasugrel and ticagrelor non-responder in patients treated with therapeutic hypothermia after cardiac arrest. Resuscitation 2014, 85, 649–656. [Google Scholar] [CrossRef]
- Parodi, G.; Bellandi, B.; Xanthopoulou, I.; Capranzano, P.; Capodanno, D.; Valenti, R.; Stavrou, K.; Migliorini, A.; Antoniucci, D.; Tamburino, C.; et al. Morphine Is Associated with a Delayed Activity of Oral Antiplatelet Agents in Patients With ST-Elevation Acute Myocardial Infarction Undergoing Primary Percutaneous Coronary Intervention. Circ. Cardiovasc. Interv. 2015, 8. [Google Scholar] [CrossRef] [PubMed]
- Kubica, J.; Adamski, P.; Ostrowska, M.; Sikora, J.; Kubica, J.M.; Sroka, W.D.; Stankowska, K.; Buszko, K.; Navarese, E.; Jilma, B.; et al. Morphine delays and attenuates ticagrelor exposure and action in patients with myocardial infarction: The randomized, double-blind, placebo-controlled IMPRESSION trial. Eur. Hear. J. 2016, 37, 245–252. [Google Scholar] [CrossRef] [PubMed]
- Vaduganathan, M.; Harrington, R.A.; Stone, G.W.; Deliargyris, E.N.; Steg, P.G.; Gibson, C.M.; Hamm, C.W.; Price, M.J.; Menozzi, A.; Prats, J.; et al. Cangrelor With and Without Glycoprotein IIb/IIIa Inhibitors in Patients Undergoing Percutaneous Coronary Intervention. J. Am. Coll. Cardiol. 2017, 69, 176–185. [Google Scholar] [CrossRef] [PubMed]
- Vaduganathan, M.; Harrington, R.A.; Stone, G.W.; Deliargyris, E.N.; Steg, P.G.; Gibson, C.M.; Hamm, C.W.; Price, M.J.; Menozzi, A.; Prats, J.; et al. Evaluation of Ischemic and Bleeding Risks Associated with 2 Parenteral Antiplatelet Strategies Comparing Cangrelor with Glycoprotein IIb/IIIa Inhibitors. JAMA Cardiol. 2017, 2, 127–135. [Google Scholar] [CrossRef]
- Valgimigli, M.; Bueno, H.; Byrne, R.; Collet, J.-P.; Costa, F.; Jeppsson, A.; Jüni, P.; Kastrati, A.; Kolh, P.; Mauri, L.; et al. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS. Eur. J. Cardio Thora. Surg. 2018, 53, 34–78. [Google Scholar] [CrossRef] [PubMed]
- Franchi, F.; Rollini, F.; Rivas, A.; Wali, M.; Briceno, M.; Agarwal, M.; Shaikh, Z.; Nawaz, A.; Silva, G.; Been, L.; et al. Platelet Inhibition With Cangrelor and Crushed Ticagrelor in Patients With ST-Segment–Elevation Myocardial Infarction Undergoing Primary Percutaneous Coronary Intervention. Circulation 2019, 139, 1661–1670. [Google Scholar] [CrossRef] [PubMed]
- Mohammad, M.A.; Andell, P.; Koul, S.; James, S.; Scherstén, F.; Götberg, M.; Erlinge, D. Cangrelor in combination with ticagrelor provides consistent and potent P2Y12-inhibition during and after primary percutaneous coronary intervention in real-world patients with ST-segment-elevation myocardial infarction. Platelets 2017, 28, 414–416. [Google Scholar] [CrossRef]
- Hochholzer, W.; Kleiner, P.; Younas, I.; Valina, C.M.; Löffelhardt, N.; Amann, M.; Bömicke, T.; Ferenc, M.; Hauschke, D.; Trenk, D.; et al. Randomized Comparison of Oral P2Y12-Receptor Inhibitor Loading Strategies for Transitioning from Cangrelor: The ExcelsiorLOAD2 Trial. JACC Cardiovasc. Interv. 2017, 10, 121–129. [Google Scholar] [CrossRef] [PubMed]
- Schneider, D.J.; Agarwal, Z.; Seecheran, N.; Gogo, P. Pharmacodynamic Effects When Clopidogrel Is Given before Cangrelor Discontinuation. J. Interv. Cardiol. 2015, 28, 415–419. [Google Scholar] [CrossRef]
- Judge, H.M.; Buckland, R.; Jakubowski, J.A.; Storey, R. Cangrelor inhibits the binding of the active metabolites of clopidogrel and prasugrel to P2Y12receptorsin vitro. Platelets 2015, 27, 191–195. [Google Scholar] [CrossRef]
- Dovlatova, N.L.; Jakubowski, J.A.; Sugidachi, A.; Heptinstall, S. The reversible P2Y12antagonist cangrelor influences the ability of the active metabolites of clopidogrel and prasugrel to produce irreversible inhibition of platelet function. J. Thromb. Haemost. 2008, 6, 1153–1159. [Google Scholar] [CrossRef] [PubMed]
| Cangrelor-Treated Patients (n = 146) | |
|---|---|
| Demographic Characteristics | |
| Age (years) | 63.7 ± 11.7 |
| Male, no./total no. (%) | 110/146 (75.3%) |
| Body mass index (kg/m2) * | 26.8 ± 3.7 |
| Hypertension, no./total no. (%) | 50/140 (35.7%) |
| Dyslipidemia, no./total no. (%) | 35/104 (33.7%) |
| Current smokers, no./total no. (%) | 46/118 (39.0%) |
| Diabetes mellitus, no./total no. (%) Insulin-dependent diabetes, no./total no. (%) | 23/141 (16.3%) 7/141 (5.0%) |
| Positive family history, no./total no. (%) † | 35/87 (40.2%) |
| Chronic kidney disease, no/total no. (%) ‡ | 6/143 (4.2%) |
| Prior myocardial infarction, no./total no. (%) | 18/143 (12.6%) |
| Prior PCI, no./total no. (%) | 19/143 (13.3%) |
| Prior CABG, no./total no. (%) | 6/143 (4.2%) |
| Prior stroke or TIA, no./total no. (%) | 9/143 (6.3%) |
| Clinical presentation | |
| Diagnosis at presentation, no./total no. (%) STEMI NSTEMI Unstable angina Chronic coronary syndrome Other diagnosis | 123/146 (84.2%) 10/146 (6.8%) 2/146 (1.4%) 4/146 (2.7%) 7/146 (4.8%) |
| Killip classification, no./total no. (%) Class I Class II Class III Class IV | 62/146 (42.5%) 14/146 (9.6%) 4/146 (2.7%) 66/146 (45.2%) |
| Cardiac arrest at presentation, no./total no. (%) | 80/146 (54.8%) |
| Mechanical ventilation, no./total no. (%) | 71/146 (48.6%) |
| Mechanical circulatory support, no./total no. (%) § | 18/146 (12.3%) |
| Cangrelor-Treated Patients (n = 146) | |
|---|---|
| Procedural Characteristics | |
| Procedural length (min) | 44 (34–62) |
| Access route, no./total no. (%) Radial access Femoral access | 80/146 (54.8%) 66/146 (45.2%) |
| PCI, no./total no. (%) Drug-eluting stent Balloon angioplasty | 140/146 (95.9%) 132/140 (94.3%) 8/140 (5.7%) |
| Target vessel, no./total no. (%) * Left main Left anterior descending Left circumflex artery Ramus intermedius Right coronary artery Saphenous vein graft | 18/140 (12.9%) 76/140 (54.3%) 25/140 (17.9%) 10/140 (7.1%) 45/140 (32.1%) 1/140 (0.7%) |
| Multi-vessel PCI, no./total no. (%) | 26/140 (18.6%) |
| Aspiration thrombectomy, no./total no. (%) | 28/140 (20.0%) |
| Unsuccessful or no PCI, no./total no. (%) | 6/146 (4.1%) |
| Procedural medication | |
| Aspirin loading dose, no./total no. (%) | 138/146 (94.5%) |
| P2Y12-inhibitor loading dose, no./total no. (%) | 139/146 (95.2%) |
| Type of oral P2Y12-inhibitor, no./total no. (%) Clopidogrel Prasugrel Ticagrelor | 15/139 (10.8%) 0/139 (0.0%) 124/139 (89.2%) |
| Timing of P2Y12-inhibitor loading dose, no./total no. (%) Pre-PCI During PCI Post-PCI | 37/139 (26.6%) 4/139 (2.9%) 98/139 (70.5%) |
| P2Y12-inhibitor reloading, no./total no. (%) † | 5/139 (3.6%) |
| Oral anticoagulants use, no./total no. (%) Vitamin K antagonist Direct oral anticoagulant | 5/146 (3.4%) 6/146 (4.1%) |
| Peri-procedural anticoagulants, no./total no. (%) Unfractionated heparin Glycoprotein IIb/IIIa inhibitors | 143/146 (97.9%) 1/146 (0.7%) |
| Cangrelor-Treated Patients (n = 146) | ||
|---|---|---|
| 48 h | 30 Days | |
| All-cause mortality, no. of patients (%) | 16 (11.0%) | 37 (25.3%) |
| Myocardial infarction, no. of patients (%) | 0 (0.0%) | 2 (1.7%) |
| Definite stent thrombosis, no. of patients (%) | 0 (0.0%) | 2 (1.7%) |
| Major bleeding, no. of patients (%) Access site bleeding | 8 (5.6%) 2 (25.0%) * | 17 (12.5%) 3 (17.6%) * |
| Major or minor bleeding, no. of patients (%) Access site bleeding | 20 (13.8%) 4 (20.0%) * | 31 (22.0%) 5 (16.1%) * |
| Univariate Analysis | Multivariable Analysis | |||
|---|---|---|---|---|
| HR (95%-CI) | p-Value | HR (95%-CI) | p-Value | |
| Age per year * | 1.00 (0.97–1.02) | 0.74 | 1.01 (0.98–1.04) | 0.71 |
| Male sex | 1.41 (0.62–3.21) | 0.41 | 0.92 (0.40–2.14) | 0.85 |
| Hypertension | 1.56 (0.80–3.04) | 0.19 | ||
| Diabetes mellitus | 0.80 (0.31–2.05) | 0.64 | ||
| Current smoker | 0.82 (0.37–1.84) | 0.63 | ||
| Pervious MI | 0.61 (0.19–2.00) | 0.61 | ||
| Previous revascularization † | 0.93 (0.39–2.24) | 0.87 | ||
| STEMI at presentation | 1.63 (0.58–4.59) | 0.36 | ||
| Cardiac arrest at presentation | 5.00 (2.08–12.0) | <0.01 | 5.20 (2.10–12.9) | <0.01 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
van der Sangen, N.M.R.; Cheung, H.Y.; Verouden, N.J.W.; Appelman, Y.; Beijk, M.A.M.; Claessen, B.E.P.M.; Delewi, R.; Knaapen, P.; Lemkes, J.S.; Nap, A.; et al. Cangrelor Use in Routine Practice: A Two-Center Experience. J. Clin. Med. 2021, 10, 2829. https://doi.org/10.3390/jcm10132829
van der Sangen NMR, Cheung HY, Verouden NJW, Appelman Y, Beijk MAM, Claessen BEPM, Delewi R, Knaapen P, Lemkes JS, Nap A, et al. Cangrelor Use in Routine Practice: A Two-Center Experience. Journal of Clinical Medicine. 2021; 10(13):2829. https://doi.org/10.3390/jcm10132829
Chicago/Turabian Stylevan der Sangen, Niels M. R., Ho Yee Cheung, Niels J. W. Verouden, Yolande Appelman, Marcel A. M. Beijk, Bimmer E. P. M. Claessen, Ronak Delewi, Paul Knaapen, Jorrit S. Lemkes, Alexander Nap, and et al. 2021. "Cangrelor Use in Routine Practice: A Two-Center Experience" Journal of Clinical Medicine 10, no. 13: 2829. https://doi.org/10.3390/jcm10132829
APA Stylevan der Sangen, N. M. R., Cheung, H. Y., Verouden, N. J. W., Appelman, Y., Beijk, M. A. M., Claessen, B. E. P. M., Delewi, R., Knaapen, P., Lemkes, J. S., Nap, A., Vis, M. M., Kikkert, W. J., & Henriques, J. P. S. (2021). Cangrelor Use in Routine Practice: A Two-Center Experience. Journal of Clinical Medicine, 10(13), 2829. https://doi.org/10.3390/jcm10132829







