Midterm Survivorship of an Uncemented Hydroxyapatite-Coated Titanium Femoral Component and Clinically Meaningful Outcomes in Patients Older Than 75 Years
Abstract
1. Introduction
2. Methods
2.1. Patient Selection
2.2. Psychometric Analysis
2.3. Statistics and Survival Analysis
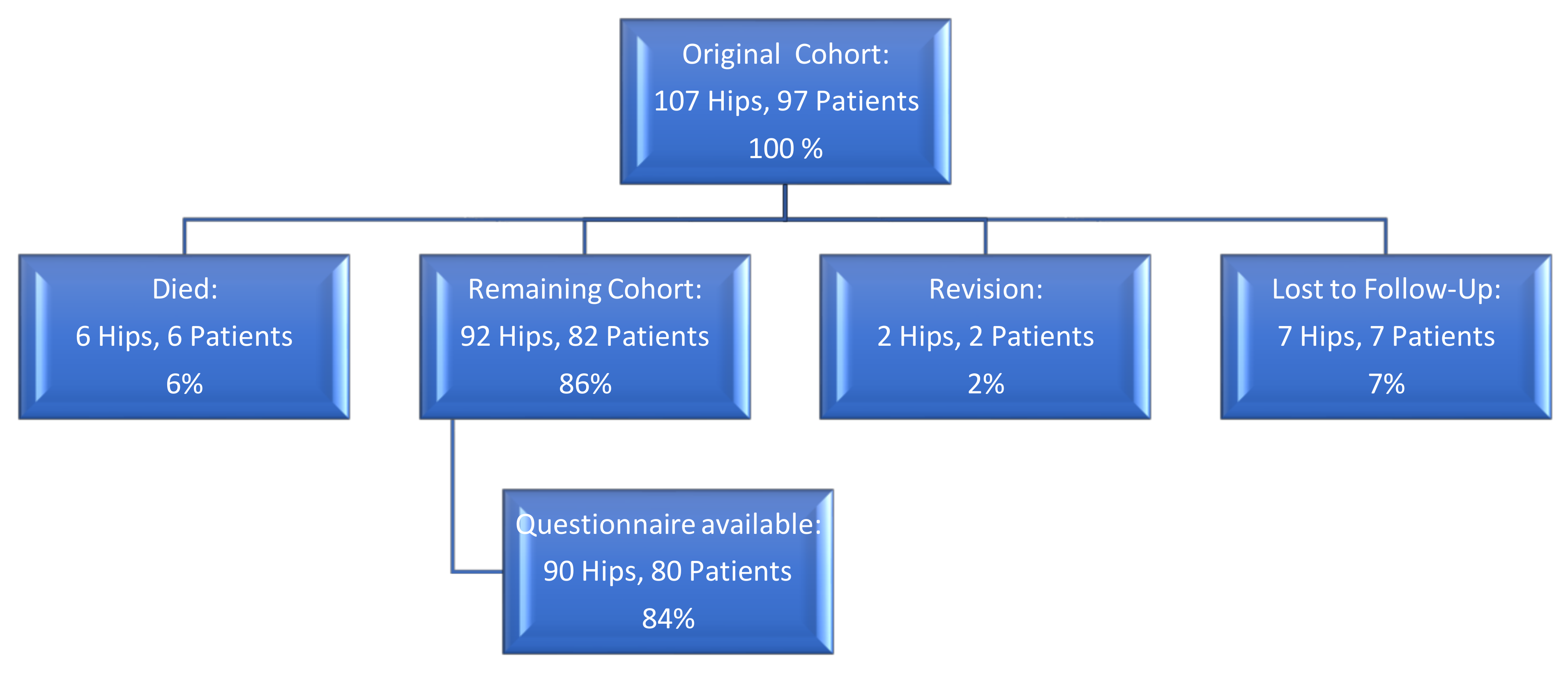
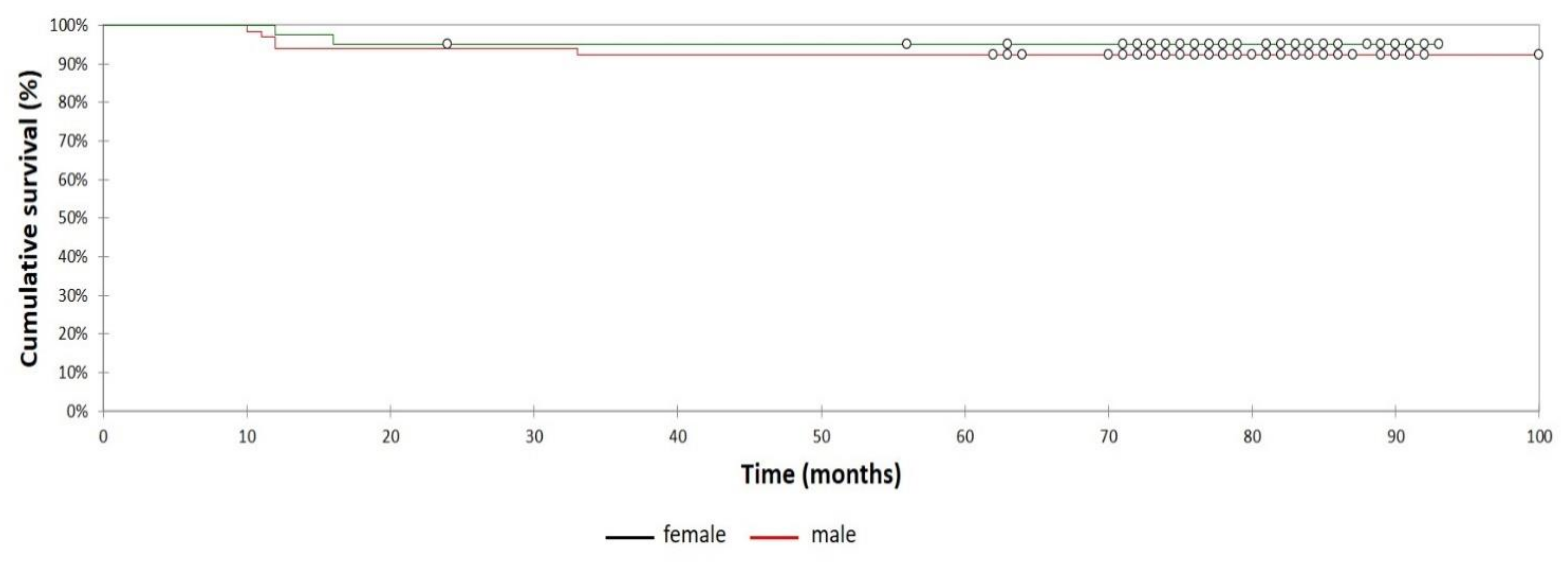
3. Results
3.1. Demographics
3.2. Survival Analysis
3.3. Analysis of Pre- Versus Postoperative Reported Outcome Score Measurements
3.4. Achievement MCID, SCB, and PASS
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Learmonth, I.D.; Young, C.; Rorabeck, C. The operation of the century: Total hip replacement. Lancet 2007, 370, 1508–1519. [Google Scholar] [CrossRef]
- Australian Orthopaedic Association National Joint Replacement Registry. Hip, Knee & Shoulder Arthroplasty Annual Report 2019. Available online: https://aoanjrr.sahmri.com/en/annual-reports-2019 (accessed on 8 August 2020).
- Norwegian National Advisory Uniton Arthroplasty and Hip Fractures. Norwegian Arthroplasty Register Report 2019. Available online: http://nrlweb.ihelse.net (accessed on 8 August 2020).
- Meftah, M.; John, M.; Lendhey, M.; Khaimov, A.; Ranawat, A.S.; Ranawat, C.S. Safety and efficacy of non-cemented femoral fixation in patients 75 years of age and older. J. Arthroplasty 2013, 28, 1378–1380. [Google Scholar] [CrossRef]
- Troelsen, A.; Malchau, E.; Sillesen, N.; Malchau, H. A Review of Current Fixation Use and Registry Outcomes in Total Hip Arthroplasty: The Uncemented Paradox. Clin. Orthop. Relat. Res. 2013, 471, 2052–2059. [Google Scholar] [CrossRef] [PubMed]
- Klein, G.R.; Levine, B.R.; Hozack, W.J.; Strauss, E.J.; D’Antonio, J.A.; Macaulay, W.; Di Cesare, P.E. Return to athletic activity after total hip arthroplasty. Consensus guidelines based on a survey of the Hip Society and American Association of Hip and Knee Surgeons. J. Arthroplasty 2007, 22, 171–175. [Google Scholar] [CrossRef] [PubMed]
- Demey, G.; Fary, C.; Lustig, S.; Neyret, P.; si Selmi, T.A. Does a collar improve the immediate stability of uncemented femoral hip stems in total hip arthroplasty? A bilateral comparative cadaver study. J. Arthroplasty 2011, 26, 1549–1555. [Google Scholar] [CrossRef] [PubMed]
- World Medical Association. Declaration of Helsinki, Ethical Principles for Medical Research Involving Human Subjects. 2008. Available online: https://www.wma.net/wp-content/uploads/2018/07/DoH-Oct2008.pdf (accessed on 8 August 2020).
- Harris, W.H. Traumatic arthritis of the hip after dislocation and acetabular fractures: Treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J. Bone Joint Surg. Am. 1969, 51, 737–755. [Google Scholar] [CrossRef] [PubMed]
- Byrd, J.W.T. Hip arthroscopy: Patient assessment and indications. Instr. Course Lect. 2003, 52, 711–719. [Google Scholar]
- Paulsen, A.; Roos, E.M.; Pedersen, A.B.; Overgaard, S. Minimal clinically important improvement (MCII) and patient-acceptable symptom state (PASS) in total hip arthroplasty (THA) patients 1 year postoperatively. Acta Orthopaedica 2013, 85, 39–48. [Google Scholar] [CrossRef]
- Glassman, S.D.; Copay, A.G.; Berven, S.H.; Polly, D.W.; Subach, B.R.; Carreon, L.Y. Defining Substantial Clinical Benefit Following Lumbar Spine Arthrodesis. J. Bone Joint Surg. Am. 2008, 90, 1839–1847. [Google Scholar] [CrossRef]
- Nwachukwu, B.U.; Chang, B.; Rotter, B.-Z.; Kelly, B.T.; Ranawat, A.S.; Nawabi, D.H. Minimal Clinically Important Difference and Substantial Clinical Benefit After Revision Hip Arthroscopy. Arthrosc. J. Arthrosc. Relat. Surg. 2018, 34, 1862–1868. [Google Scholar] [CrossRef]
- Chahal, J.; van Thiel, G.S.; Mather, R.C.; Lee, S.; Song, S.H.; Davis, A.M.; Salata, M.; Nho, S.J. The Patient Acceptable Symptomatic State for the Modified Harris Hip Score and Hip Outcome Score Among Patients Undergoing Surgical Treatment for Femoroacetabular Impingement. Am. J. Sports Med. 2015, 43, 1844–1849. [Google Scholar] [CrossRef] [PubMed]
- Berliner, J.L.; Brodke, D.J.; Chan, V.; SooHoo, N.F.; Bozic, K.J. Can Preoperative Patient-reported Outcome Measures Be Used to Predict Meaningful Improvement in Function After TKA? Clin. Orthop. Relat. Res. 2017, 475, 149–157. [Google Scholar] [CrossRef] [PubMed]
- Youden, W.J. Index for rating diagnostic tests. Cancer 1950, 3, 32–35. [Google Scholar] [CrossRef]
- Yuasa, T.; Maezawa, K.; Nozawa, M.; Kaneko, K. Cementless total hip arthroplasty in patients aged ≥80 years. J. Orthop. 2016, 13, 29–32. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Riley, S.A.; Spears, J.R.; Smith, L.S.; Mont, M.A.; Elmallah, R.K.; Cherian, J.J.; Malkani, A.L. Cementless Tapered Femoral Stems for Total Hip Arthroplasty in Octogenarians. J. Arthroplasty 2016, 31, 2810–2813. [Google Scholar] [CrossRef]
- Stihsen, C.; Springer, B.; Nemecek, E.; Olischar, B.; Kaider, A.; Windhager, R.; Kubista, B. Cementless Total Hip Arthroplasty in Octogenarians. J. Arthroplasty 2017, 32, 1923–1929. [Google Scholar] [CrossRef]
- Ahmad, A.; Mirza, Y.; Evans, A.R.; Teoh, K.H. A Comparative Study Between Uncemented and Hybrid Total Hip Arthroplasty in Octogenarians. J. Arthroplasty 2018, 33, 3719–3723. [Google Scholar] [CrossRef]
- Gkagkalis, G.; Goetti, P.; Mai, S.; Meinecke, I.; Helmy, N.; Bosson, D.; Kutzner, K.P. Cementless short-stem total hip arthroplasty in the elderly patient - is it a safe option?: A prospective multicentre observational study. BMC Geriatr. 2019, 19, 112. [Google Scholar] [CrossRef]
- Thien, T.M.; Chatziagorou, G.; Garellick, G.; Furnes, O.; Havelin, L.I.; Mäkelä, K.; Overgaard, S.; Pedersen, A.; Eskelinen, A.; Pulkkinen, P.; et al. Periprosthetic femoral fracture within two years after total hip replacement: Analysis of 437,629 operations in the nordic arthroplasty register association database. J. Bone Joint Surg. Am. 2014, 96, e167. [Google Scholar] [CrossRef]
- Cook, R.E.; Jenkins, P.J.; Walmsley, P.J.; Patton, J.T.; Robinson, C.M. Risk factors for periprosthetic fractures of the hip: A survivorship analysis. Clin. Orthop. Relat. Res. 2008, 466, 1652–1656. [Google Scholar] [CrossRef]
- Sidler-Maier, C.C.; Waddell, J.P. Incidence and predisposing factors of periprosthetic proximal femoral fractures: A literature review. Int. Orthop. 2015, 39, 1673–1682. [Google Scholar] [CrossRef]
- Lehil, M.S.; Bozic, K.J. Trends in total hip arthroplasty implant utilization in the United States. J. Arthroplasty 2014, 29, 1915–1918. [Google Scholar] [CrossRef] [PubMed]
- Jämsen, E.; Eskelinen, A.; Peltola, M.; Mäkelä, K. High early failure rate after cementless hip replacement in the octogenarian. Clin. Orthop. Relat. Res. 2014, 472, 2779–2789. [Google Scholar] [CrossRef]
- Ng Man Sun, S.; Gillott, E.; Bhamra, J.; Briggs, T. Implant use for primary hip and knee arthroplasty: Are we getting it right first time? J. Arthroplasty 2013, 28, 908–912. [Google Scholar] [CrossRef]
- Ogino, D.; Kawaji, H.; Konttinen, L.; Lehto, M.; Rantanen, P.; Malmivaara, A.; Konttinen, Y.T.; Salo, J. Total hip replacement in patients eighty years of age and older. J. Bone Joint Surg. Am. 2008, 90, 1884–1890. [Google Scholar] [CrossRef]
- Olsen, F.; Kotyra, M.; Houltz, E.; Ricksten, S.-E. Bone cement implantation syndrome in cemented hemiarthroplasty for femoral neck fracture: Incidence, risk factors, and effect on outcome. Br. J. Anaesth. 2014, 113, 800–806. [Google Scholar] [CrossRef] [PubMed]
- Tsai, M.-C.; Ng, Y.-Y.; Chen, W.-M.; Tsai, S.-W.; Wu, S.-C. The effects of cement fixation on survival in elderly patients with hip hemiarthroplasty: A nationwide cohort study. BMC Musculoskelet Disord. 2019, 20, 1–8. [Google Scholar] [CrossRef]
- Griffiths, R.; White, S.M.; Moppett, I.K.; Parker, M.J.; Chesser, T.J.S.; Costa, M.L.; Johansen, A.; Wilson, H.; Timperley, A.J. Safety guideline: Reducing the risk from cemented hemiarthroplasty for hip fracture 2015: Association of Anaesthetists of Great Britain and Ireland British Orthopaedic Association British Geriatric Society. Anaesthesia 2015, 70, 623–626. [Google Scholar] [CrossRef]
- McMinn, D.J.W.; Snell, K.I.E.; Daniel, J.; Treacy, R.B.C.; Pynsent, P.B.; Riley, R.D. Mortality and implant revision rates of hip arthroplasty in patients with osteoarthritis: Registry based cohort study. BMJ 2012, 344, e3319. [Google Scholar] [CrossRef]
- Donaldson, A.J.; Thomson, H.E.; Harper, N.J.; Kenny, N.W. Bone cement implantation syndrome. Br. J. Anaesth. 2009, 102, 12–22. [Google Scholar] [CrossRef]
- Kennedy, J.W.; Johnston, L.; Cochrane, L.; Boscainos, P.J. Outcomes of total hip arthroplasty in the octogenarian population. Surgeon 2013, 11, 199–204. [Google Scholar] [CrossRef] [PubMed]
- Lamb, J.N.; Baetz, J.; Messer-Hannemann, P.; Adekanmbi, I.; van Duren, B.H.; Redmond, A.; West, R.M.; Morlock, M.M.; Pandit, H.G. A calcar collar is protective against early periprosthetic femoral fracture around cementless femoral components in primary total hip arthroplasty: A registry study with biomechanical validation. Bone Joint J. 2019, 101-B, 779–786. [Google Scholar] [CrossRef]
- Gromov, K.; Bersang, A.; Nielsen, C.S.; Kallemose, T.; Husted, H.; Troelsen, A. Risk factors for post-operative periprosthetic fractures following primary total hip arthroplasty with a proximally coated double-tapered cementless femoral component. Bone Joint J. 2017, 99-B, 451–457. [Google Scholar] [CrossRef] [PubMed]
- Carli, A.V.; Negus, J.J.; Haddad, F.S. Periprosthetic femoral fractures and trying to avoid them: What is the contribution of femoral component design to the increased risk of periprosthetic femoral fracture? Bone Joint J. 2017, 99-B, 50–59. [Google Scholar] [CrossRef] [PubMed]
- Reuling, E.M.B.P.; Sierevelt, I.N.; van den Bekerom, M.P.J.; Hilverdink, E.F.; Schnater, J.M.; van Dijk, C.N.; Goslings, J.C.; Raaymakers, E.L.F.B. Predictors of functional outcome following femoral neck fractures treated with an arthroplasty: Limitations of the Harris hip score. Arch. Orthop. Trauma Surg. 2012, 132, 249–256. [Google Scholar] [CrossRef]
- Jo, S.; Lee, S.H.; Yoon, S.-J. Clinical Outcomes of Total Hip Arthroplasty for Displaced Femoral Neck Fractures in Patients 80 Years of Age and Older Selected by Clinical Frailty Score. Hip Pelvis 2020, 32, 148–155. [Google Scholar] [CrossRef]
- Wolfson, T.S.; Ryan, M.K.; Begly, J.P.; Youm, T. Outcome Trends After Hip Arthroscopy for Femoroacetabular Impingement: When Do Patients Improve? Arthrosc. J. Arthrosc. Relat. Surg. 2019, 35, 3261–3270. [Google Scholar] [CrossRef]
- Nho, S.J.; Beck, E.C.; Nwachukwu, B.U.; Cvetanovich, G.L.; Neal, W.H.; Harris, J.D.; Weber, A.E.; Mather, R.C. Survivorship and Outcome of Hip Arthroscopy for Femoroacetabular Impingement Syndrome Performed With Modern Surgical Techniques. Am. J. Sports Med. 2019, 47, 1662–1669. [Google Scholar] [CrossRef]
- Lyman, S.; Lee, Y.-Y.; McLawhorn, A.S.; Islam, W.; MacLean, C.H. What Are the Minimal and Substantial Improvements in the HOOS and KOOS and JR Versions After Total Joint Replacement? Clin. Orthop. Relat. Res. 2018, 476, 2432–2441. [Google Scholar] [CrossRef]
- Levy, D.M.; Kuhns, B.D.; Chahal, J.; Philippon, M.J.; Kelly, B.T.; Nho, S.J. Hip Arthroscopy Outcomes With Respect to Patient Acceptable Symptomatic State and Minimal Clinically Important Difference. Arthrosc. J. Arthrosc. Relat. Surg. 2016, 32, 1877–1886. [Google Scholar] [CrossRef]
- Cvetanovich, G.L.; Weber, A.E.; Kuhns, B.D.; Alter, J.; Harris, J.D.; Mather, R.C.; Nho, S.J. Hip Arthroscopic Surgery for Femoroacetabular Impingement With Capsular Management: Factors Associated With Achieving Clinically Significant Outcomes. Am. J. Sports Med. 2017, 46, 288–296. [Google Scholar] [CrossRef] [PubMed]
- Galea, V.P.; Florissi, I.; Rojanasopondist, P.; Connelly, J.W.; Ingelsrud, L.H.; Bragdon, C.; Malchau, H.; Troelsen, A. The Patient Acceptable Symptom State for the Harris Hip Score Following Total Hip Arthroplasty: Validated Thresholds at 3-Month, 1-, 3-, 5-, and 7-Year Follow-Up. J. Arthroplasty 2020, 35, 145–152.e2. [Google Scholar] [CrossRef] [PubMed]

| Male | Female | Total | |
|---|---|---|---|
| Age years, mean (range) | 78 (75 to 87) | 78 (75 to 84) | 78 (75 to 87) |
| Hips, no. (%) | 41 (38) | 66 (42) | 107 |
| Body mass index kg/m2, mean (range) | 26.7 (21.3 to 33.6) | 26.6 (20.2 to 41.8) | 26.6 (20.2 to 41.8) |
| Right:Left | 19:22 | 37:29 | 56:51 |
| Authors | Year of Publication | Sample Size | Mean Follow-Up | Stem(s) Used | Stem Survival overall % | Level of Evidence |
|---|---|---|---|---|---|---|
| Yuasa et al. [17] | 2016 | 30 | 5.6 years | - Natural Hip (Zimmer, Warsaw, Indiana, USA) - Synergy (Smith&Nephew, London, UK) | 100% | 4 |
| Riley et al. [18] | 2016 | 78 | Minimum 2 years | - Accolade I or Accolade II (Stryker, Mahwah, NJ, USA) | 98.7% | 3 |
| Stihsen et al. [19] | 2017 | 162 | 10.7 years | - Zweymüller SL, SLL or SLO (Zimmer, Warsaw, Indiana, USA) | 100% | 3 |
| Ahmad et al. [20] | 2018 | 76 | Minimum 5 years | - Polar (Smith&Nephew, London, UK) | 97.4% | 3 |
| Gkagkalis et al. [21] | 2019 | 121 | 4.1 years | - Optimys (Mathys Ltd., Bettlach, Switzerland) | 100% | 3 |
| Current study | 107 | 6.4 years | - Corail (DePuy Orthopaedics, Warsaw, Indiana, USA) | 98% | 3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zimmerer, A.; Navas, L.; Kinkel, S.; Weiss, S.; Hauschild, M.; Streit, M. Midterm Survivorship of an Uncemented Hydroxyapatite-Coated Titanium Femoral Component and Clinically Meaningful Outcomes in Patients Older Than 75 Years. J. Clin. Med. 2021, 10, 1019. https://doi.org/10.3390/jcm10051019
Zimmerer A, Navas L, Kinkel S, Weiss S, Hauschild M, Streit M. Midterm Survivorship of an Uncemented Hydroxyapatite-Coated Titanium Femoral Component and Clinically Meaningful Outcomes in Patients Older Than 75 Years. Journal of Clinical Medicine. 2021; 10(5):1019. https://doi.org/10.3390/jcm10051019
Chicago/Turabian StyleZimmerer, Alexander, Luis Navas, Stefan Kinkel, Stefan Weiss, Matthias Hauschild, and Marcus Streit. 2021. "Midterm Survivorship of an Uncemented Hydroxyapatite-Coated Titanium Femoral Component and Clinically Meaningful Outcomes in Patients Older Than 75 Years" Journal of Clinical Medicine 10, no. 5: 1019. https://doi.org/10.3390/jcm10051019
APA StyleZimmerer, A., Navas, L., Kinkel, S., Weiss, S., Hauschild, M., & Streit, M. (2021). Midterm Survivorship of an Uncemented Hydroxyapatite-Coated Titanium Femoral Component and Clinically Meaningful Outcomes in Patients Older Than 75 Years. Journal of Clinical Medicine, 10(5), 1019. https://doi.org/10.3390/jcm10051019





