Appropriate Number of Treatment Sessions in Virtual Reality-Based Individual Cognitive Behavioral Therapy for Social Anxiety Disorder
Abstract
1. Introduction
2. Methods
2.1. Participants
2.2. Procedure
2.3. Measurements
2.4. Statistical Analysis
3. Results
3.1. Participant Characteristics
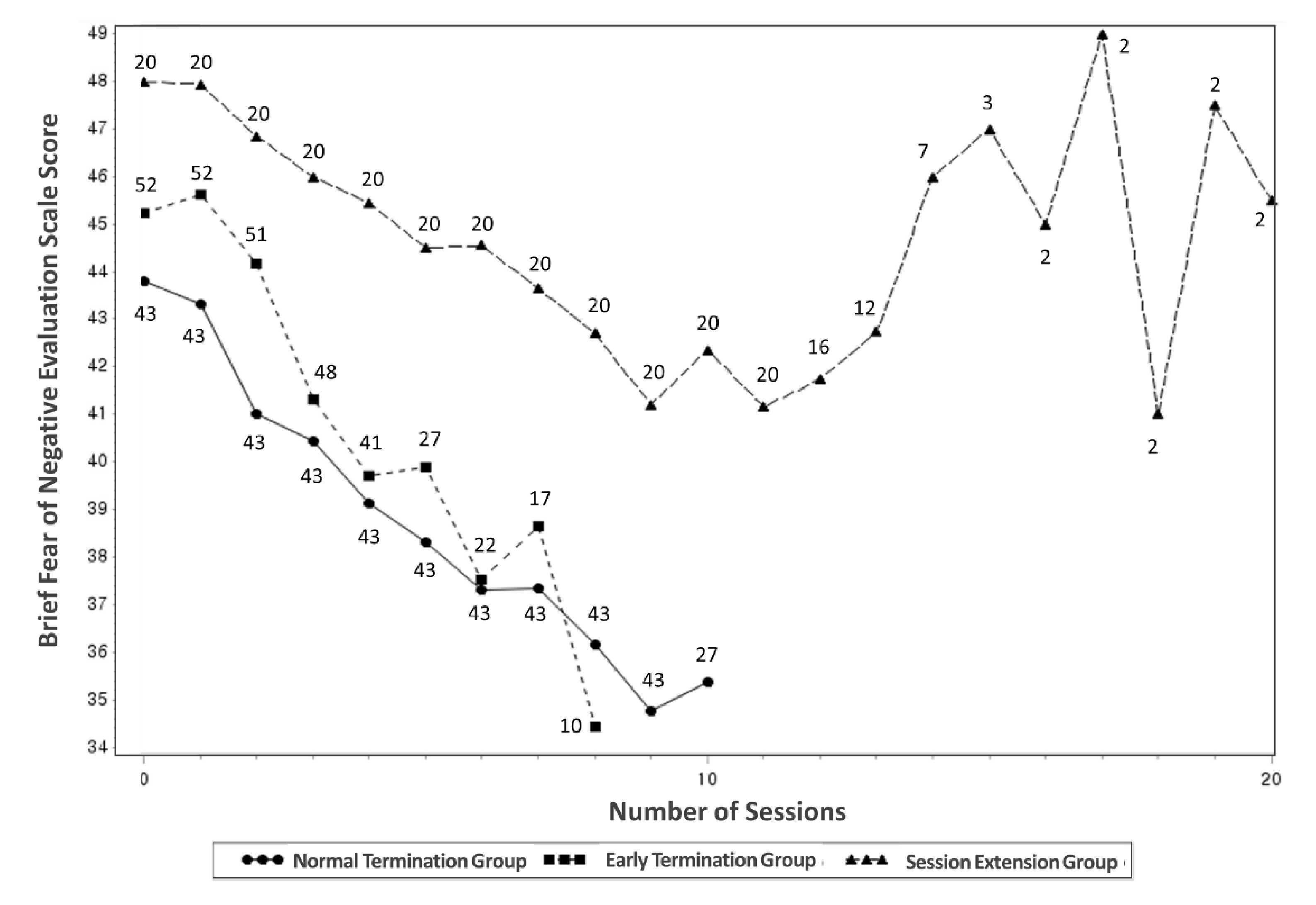
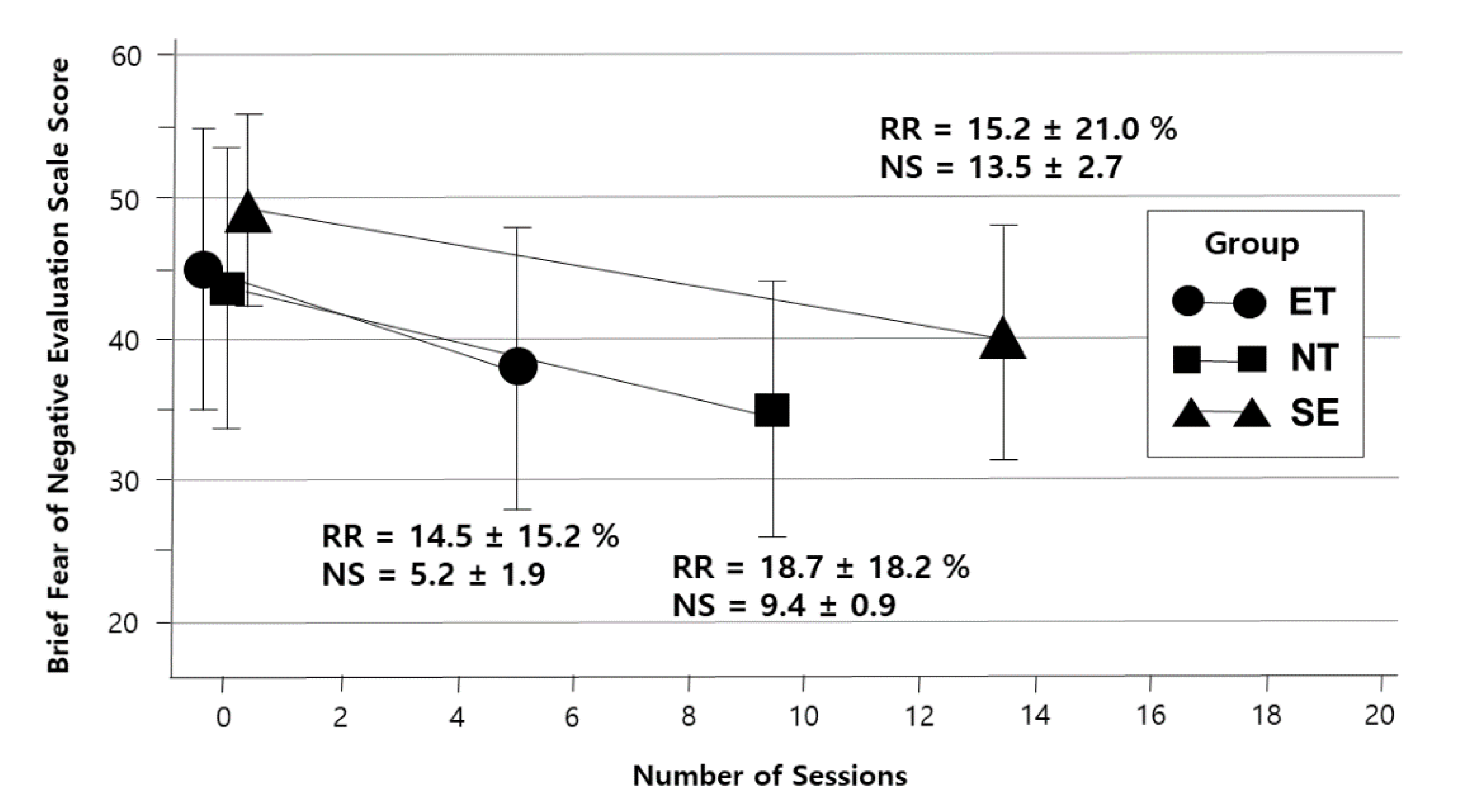
3.2. Changes in the BFNE Scores According to Session Progress
3.3. Changes in Other Psychological Measures before and after VR-Based CBT
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rapee, R.M.; Heimberg, R.G. A cognitive-behavioral model of anxiety in social phobia. Behav. Res. Ther. 1997, 35, 741–756. [Google Scholar] [CrossRef]
- Ruscio, A.M.; Brown, T.A.; Chiu, W.T.; Sareen, J.; Stein, M.B.; Kessler, R.C. Social fears and social phobia in the USA: Results from the national comorbidity survey replication. Psychol. Med. 2008, 38, 15–28. [Google Scholar] [CrossRef]
- Wittchen, H.U.; Fehm, L. Epidemiology and natural course of social fears and social phobia. Acta Psychiatr. Scand. Suppl. 2003, 417, 4–18. [Google Scholar] [CrossRef] [PubMed]
- Heimberg, R.G.; Liebowitz, M.R.; Hope, D.A.; Schneier, F.R.; Holt, C.S.; Welkowitz, L.A.; Juster, H.R.; Campeas, R.; Bruch, M.A.; Cloitre, M.; et al. Cognitive behavioral group therapy vs phenelzine therapy for social phobia: 12-week outcome. Arch. Gen. Psychiatry 1998, 55, 1133–1141. [Google Scholar] [CrossRef]
- Mayo-Wilson, E.; Dias, S.; Mavranezouli, I.; Kew, K.; Clark, D.M.; Ades, A.E.; Pilling, S. Psychological and pharmacological interventions for social anxiety disorder in adults: A systematic review and network meta-analysis. Lancet Psychiatry 2014, 1, 368–376. [Google Scholar] [CrossRef]
- Craske, M.G.; Treanor, M.; Conway, C.C.; Zbozinek, T.; Vervliet, B. Maximizing exposure therapy: An inhibitory learning approach. Behav. Res. Ther. 2014, 58, 10–23. [Google Scholar] [CrossRef]
- Hofmann, S.G.; Smits, J.A. Cognitive-behavioral therapy for adult anxiety disorders: A meta-analysis of randomized place-bo-controlled trials. J. Clin. Psychiatry 2008, 69, 621–632. [Google Scholar] [CrossRef] [PubMed]
- Haug, T.T.; Blomhoff, S.; Hellstrøm, K.; Holme, I.; Humble, M.; Madsbu, H.P.; Wold, J.E. Exposure therapy and sertraline in social phobia: I-year follow-up of a randomised controlled trial. Br. J. Psychiatry 2003, 182, 312–318. [Google Scholar] [CrossRef]
- Ponniah, K.; Hollon, S.D. Empirically supported psychological interventions for social phobia in adults: A qualitative review of randomized controlled trials. Psychol. Med. 2008, 38, 3–14. [Google Scholar] [CrossRef]
- de Carvalho, M.R.; Freire, R.C.; Nardi, A.E. Virtual reality as a mechanism for exposure therapy. World J. Biol. Psychiatry 2010, 11, 220–230. [Google Scholar] [CrossRef]
- Cieślik, B.; Mazurek, J.; Rutkowski, S.; Kiper, P.; Turolla, A.; Szczepańska-Gieracha, J. Virtual reality in psychiatric disorders: A systematic review of reviews. Complement. Ther. Med. 2020, 52, 102480. [Google Scholar] [CrossRef]
- Wechsler, T.F.; Kümpers, F.; Mühlberger, A. Inferiority or even superiority of virtual reality exposure therapy in phobias?—A systematic review and quantitative meta-analysis on randomized controlled trials specifically comparing the efficacy of virtual reality exposure to gold standard in vivo exposure in agoraphobia, specific phobia, and social phobia. Front. Psychol. 2019, 10, 1758. [Google Scholar]
- Anderson, P.L.; Price, M.; Edwards, S.M.; Obasaju, M.A.; Schmertz, S.K.; Zimand, E.; Calamaras, M.R. Virtual reality exposure therapy for social anxiety disorder: A randomized controlled trial. J. Consult. Clin. Psychol. 2013, 81, 751–760. [Google Scholar] [CrossRef]
- Wallach, H.S.; Safir, M.P.; Bar-Zvi, M. Virtual reality cognitive behavior therapy for public speaking anxiety: A randomized clinical trial. Behav. Modif. 2009, 33, 314–338. [Google Scholar] [CrossRef]
- Kampmann, I.L.; Emmelkamp, P.M.; Hartanto, D.; Brinkman, W.P.; Zijlstra, B.J.; Morina, N. Exposure to virtual social inter-actions in the treatment of social anxiety disorder: A randomized controlled trial. Behav. Res. Ther. 2016, 77, 147–156. [Google Scholar] [CrossRef]
- Bouchard, S.; Dumoulin, S.; Robillard, G.; Guitard, T.; Klinger, É.; Forget, H.; Loranger, C.; Roucaut, F.X. Virtual reality compared with in vivo exposure in the treatment of social anxiety disorder: A three-arm randomised controlled trial. Br. J. Psychiatry 2017, 210, 276–283. [Google Scholar] [CrossRef] [PubMed]
- Horigome, T.; Kurokawa, S.; Sawada, K.; Kudo, S.; Shiga, K.; Mimura, M.; Kishimoto, T. Virtual reality exposure therapy for social anxiety disorder: A systematic review and meta-analysis. Psychol. Med. 2020, 50, 2487–2497. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.E.; Hong, Y.J.; Kim, M.K.; Jung, Y.H.; Kyeong, S.; Kim, J.J. Effectiveness of self-training using the mobile-based virtual reality program in patients with social anxiety disorder. Comp. Hum. Behav. 2017, 73, 614–619. [Google Scholar] [CrossRef]
- Taube-Schiff, M.; Suvak, M.K.; Antony, M.M.; Bieling, P.J.; McCabe, R.E. Group cohesion in cognitive-behavioral group therapy for social phobia. Behav. Res. Ther. 2007, 45, 687–698. [Google Scholar] [CrossRef]
- Clark, D.M. Cognitive therapy versus exposure and applied relaxation in social phobia: A randomized controlled trial. J. Consult. Clin. Psychol. 2006, 74, 568–1067. [Google Scholar] [CrossRef]
- Mörtberg, E.; Clark, D.M.; Bejerot, S. Intensive group cognitive therapy and individual cognitive therapy for social phobia: Sustained improvement at 5-year follow-up. J. Anxiety Disord. 2011, 25, 994–1000. [Google Scholar] [CrossRef]
- Beidel, D.C.; Alfano, C.A.; Kofler, M.J.; Rao, P.A.; Scharfstein, L.; Wong Sarver, N. The impact of social skills training for social anxiety disorder: A randomized controlled trial. J. Anxiety Disord. 2014, 28, 908–918. [Google Scholar] [CrossRef] [PubMed]
- Jerremalm, A.; Jansson, L.; Öst, L.G. Cognitive and physiological reactivity and the effects of different behavioral methods in the treatment of social phobia. Behav. Res. Ther. 1986, 24, 171–180. [Google Scholar] [CrossRef]
- Goldin, P.R.; Gross, J.J. Effects of mindfulness-based stress reduction (MBSR) on emotion regulation in social anxiety disorder. Emotion 2010, 10, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Fedoroff, I.C.; Taylor, S. Psychological and pharmacological treatments of social phobia: A meta-analysis. J. Clin. Psycho-pharmacol. 2001, 21, 311–324. [Google Scholar] [CrossRef]
- Powers, M.B.; Sigmarsson, S.R.; Emmelkamp, P.M.G. A meta-analytic review of psychological treatments for social anxiety disorder. Intern. J. Cogn. Ther. 2008, 1, 94–113. [Google Scholar] [CrossRef]
- Stangier, U.; Heidenreich, T.; Peitz, M.; Lauterbach, W.; Clark, D.M. Cognitive therapy for social phobia: Individual versus group treatment. Behav. Res. Ther. 2003, 41, 991–1007. [Google Scholar] [CrossRef]
- Yoshinaga, N.; Matsuki, S.; Niitsu, T.; Sato, Y.; Tanaka, M.; Ibuki, H.; Takanashi, R.; Ohshiro, K.; Ohshima, F.; Asano, K.; et al. Cognitive behavioral therapy for patients with social anxiety disorder who remain symptomatic following antidepressant treatment: A randomized, assessor-blinded, controlled trial. Psychother. Psychosom. 2016, 85, 208–217. [Google Scholar] [CrossRef]
- Sheehan, D.V.; Lecrubier, Y.; Sheehan, K.H.; Amorim, P.; Janavs, J.; Weiller, E.; Hergueta, T.; Baker, R.; Dunbar, G.C. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J. Clin. Psychiatry 1998, 59 (Suppl. 20), 22–57. [Google Scholar] [PubMed]
- Taylor, S.; Woody, S.; Koch, W.J.; McLean, P.; Paterson, R.J.; Anderson, K.W. Cognitive restructuring in the treatment of social phobia. Efficacy and mode of action. Behav. Modif. 1997, 21, 487–511. [Google Scholar] [CrossRef] [PubMed]
- Payne, R.A.; Donaghy, M. Payne’s Handbook of Relaxation Techniques: A Practical Guide for the Health Care Professional; Churchill Livingstone Elsevier: Amsterdam, The Netherlands, 2010. [Google Scholar]
- Leary, M.R. A brief version of the Fear of Negative Evaluation Scale. Pers. Soc. Psychol. Bull. 1983, 9, 371–375. [Google Scholar] [CrossRef]
- Fresco, D.; Coles, M.; Heimberg, R.G.; Liebowitz, M.R.; Hami, S.; Stein, M.B.; Goetz, D. The Liebowitz Social Anxiety Scale: A comparison of the psychometric properties of self-report and clinician-administered formats. Psychol. Med. 2001, 31, 1025–1035. [Google Scholar] [CrossRef]
- Mattick, R.P.; Clarke, J.C. Development and validation of measures of social phobia scrutiny fear and social interaction anxiety. Behav. Res. Ther. 1998, 36, 455–470. [Google Scholar] [CrossRef]
- Collins, K.A.; Westra, H.A.; Dozois, D.J.A.; Stewart, S.H. The validity of the brief version of the Fear of Negative Evaluation Scale. J. Anxiety Disord. 2005, 19, 345–359. [Google Scholar] [CrossRef]
- Carl, E.; Stein, A.T.; Levihn-Coon, A.; Pogue, J.R.; Rothbaum, B.; Emmelkamp, P.; Asmundson, G.J.G.; Carlbring, P.; Powers, M.B. Virtual reality exposure therapy for anxiety and related disorders: A meta-analysis of randomized controlled trials. J. Anxiety Disord. 2019, 61, 27–36. [Google Scholar] [CrossRef] [PubMed]
- Wiederhold, B.K.; Bouchard, S. Social anxiety disorder: Efficacy and virtual humans. In Advances in Virtual Reality and Anxiety Disorders; Springer: Boston, MA, USA, 2014; pp. 187–209. [Google Scholar]
- Leucht, S.; Davis, J.M.; Engel, R.R.; Kane, J.M.; Wagenpfeil, S. Defining ‘response’ in antipsychotic drug trials: Recommendations for the use of scale-derived cutoffs. Neuropsychopharmacology 2007, 32, 1903–1910. [Google Scholar] [CrossRef] [PubMed]
- Lindhiem, O.; Kolko, D.J.; Cheng, Y. Predicting psychotherapy benefit: A probabilistic and individualized approach. Behav. Ther. 2012, 43, 381–392. [Google Scholar] [CrossRef] [PubMed]
- Hedman, E.; Andersson, E.; Ljótsson, B.; Andersson, G.; Andersson, E.; Schalling, M.; Lindefors, N.; Rück, C. Clinical and genetic outcome determinants of internet-and group-based cognitive behavior therapy for social anxiety disorder. Acta Psychiatr. Scand. 2012, 126, 126–136. [Google Scholar] [CrossRef] [PubMed]
- Robillard, G.; Bouchard, S.; Dumoulin, S.; Guitard, T.; Klinger, E. Using virtual humans to alleviate social anxiety: Preliminary report from a comparative outcome study. Stud. Health Technol. Inform. 2010, 154, 57–60. [Google Scholar]
- Harris, S.R.; Kemmerling, R.L.; North, M.M. Brief virtual reality therapy for public speaking anxiety. Cyberpsychol. Behav. 2002, 5, 543–550. [Google Scholar] [CrossRef]
| Early Termination Group (n = 52) | Normal Termination Group (n = 43) | Session Extension Group (n = 20) | χ2or F | p | |
|---|---|---|---|---|---|
| Gender, male/female | 28/24 | 32/11 | 15/5 | 5.41 | 0.067 |
| Age, years | 34.3 ± 13.3 | 31.2 ± 15.5 | 27.6 ± 10.7 | 1.81 | 0.169 |
| Education level, years * | 14.2 ± 3.2 | 13.0 ± 3.4 | 13.5 ± 3.1 | 1.60 | 0.207 |
| Job status, employed/unemployed | 22/30 | 13/30 | 7/13 | 1.51 | 0.471 |
| Marital status, single/married/divorced | 29/20/3 | 29/12/2 | 15/5/0 | 3.33 | 0.504 |
| Medication, medicated/unmedicated | 28/24 | 23/20 | 15/5 | 3.07 | 0.215 |
| BFNE | 45.2 ± 9.7 | 43.8 ± 10.4 | 48.0 ± 6.4 | 2.07 | 0.264 |
| LSAS, anxiety | 34.1 ± 14.6 | 35.5 ± 13.9 | 46.6 ± 11.4 | 6.19 | 0.003 |
| LSAS, avoidance | 27.7 ± 15.7 | 31.0 ± 14.8 | 34.6 ± 10.8 | 1.70 | 0.187 |
| SPS | 32.2 ± 18.5 | 32.4 ± 18.0 | 49.2 ± 17.6 | 5.35 | 0.007 |
| SIAS | 43.9 ± 21.7 | 46.6 ± 15.9 | 56.1 ± 12.7 | 3.62 | 0.101 |
| Session Number | Early Termination Group (n = 52) | Normal Termination Group (n = 43) | Session Extension Group (n = 20) | p | Post-hoc |
|---|---|---|---|---|---|
| Baseline | 46.0 (1.2) | 43.3 (1.3) | 48.2 (1.9) | 0.089 | |
| 1 | 44.7 (1.2) | 42.4 (1.3) | 47.5 (1.9) | 0.074 | |
| 2 | 43.4 (1.1) | 41.4 (1.3) | 46.8 (1.8) | 0.057 | |
| 3 | 42.1 (1.1) | 40.5 (1.2) | 46.2 (1.8) | 0.041 | ET = NT, ET = SE, NT < SE |
| 4 | 40.8 (1.2) | 39.5 (1.2) | 45.5 (1.8) | 0.028 | ET = NT, ET = SE, NT < SE |
| 5 | 39.4 (1.2) | 38.6 (1.2) | 44.8 (1.8) | 0.019 | ET = NT, ET < SE, NT < SE |
| 6 | 38.1 (1.2) | 37.6 (1.2) | 44.2 (1.8) | 0.012 | ET = NT, ET < SE, NT < SE |
| 7 | 36.8 (1.3) | 36.7 (1.3) | 43.5 (1.8) | 0.008 | ET = NT, ET < SE, NT < SE |
| 8 | 35.5 (1.3) | 35.7 (1.3) | 42.8 (1.8) | 0.005 | ET = NT, ET < SE, NT < SE |
| 9 | 34.2 (1.4) | 34.8 (1.3) | 42.2 (1.9) | 0.004 | ET = NT, ET < SE, NT < SE |
| 10 | 32.9 (1.5) | 33.8 (1.3) | 41.5 (1.9) | 0.003 | ET = NT, ET < SE, NT < SE |
| Scale | Normal Termination Group | Session Extension Group | Reduction Rate | Group × Time Interaction | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Last | pa | Reduction Rate, % | Baseline | Last | pa | Reduction Rate, % | tb | p | Fc | p | |
| LSAS, anxiety | 35.5 ± 13.9 | 27.0 ± 12.8 | 0.000 | 19.5 ± 25.0 | 46.6 ± 11.4 | 33.7 ± 11.4 | 0.002 | 25.1 ± 26.6 | −0.70 | 0.486 | 0.64 | 0.424 |
| LSAS, avoidance | 31.0 ± 14.8 | 23.5 ± 13.7 | 0.001 | 13.1 ± 37.9 | 34.6 ± 10.8 | 26.0 ± 7.7 | 0.009 | 20.7 ± 31.7 | −0.67 | 0.507 | 0.04 | 0.848 |
| SPS | 32.4 ± 18.0 | 22.8 ± 15.6 | 0.001 | 22.9 ± 41.2 | 49.2 ± 17.6 | 25.8 ± 13.9 | 0.000 | 43.4 ± 23.4 | −1.59 | 0.121 | 3.58 | 0.062 |
| SIAS | 46.6 ± 15.9 | 32.9 ± 15.6 | 0.000 | 23.2 ± 26.9 | 56.0 ± 12.7 | 39.6 ± 14.5 | 0.006 | 25.8 ± 28.4 | −0.26 | 0.796 | 0.17 | 0.680 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jeong, H.S.; Lee, J.H.; Kim, H.E.; Kim, J.-J. Appropriate Number of Treatment Sessions in Virtual Reality-Based Individual Cognitive Behavioral Therapy for Social Anxiety Disorder. J. Clin. Med. 2021, 10, 915. https://doi.org/10.3390/jcm10050915
Jeong HS, Lee JH, Kim HE, Kim J-J. Appropriate Number of Treatment Sessions in Virtual Reality-Based Individual Cognitive Behavioral Therapy for Social Anxiety Disorder. Journal of Clinical Medicine. 2021; 10(5):915. https://doi.org/10.3390/jcm10050915
Chicago/Turabian StyleJeong, Hyu Seok, Jee Hyun Lee, Hesun Erin Kim, and Jae-Jin Kim. 2021. "Appropriate Number of Treatment Sessions in Virtual Reality-Based Individual Cognitive Behavioral Therapy for Social Anxiety Disorder" Journal of Clinical Medicine 10, no. 5: 915. https://doi.org/10.3390/jcm10050915
APA StyleJeong, H. S., Lee, J. H., Kim, H. E., & Kim, J.-J. (2021). Appropriate Number of Treatment Sessions in Virtual Reality-Based Individual Cognitive Behavioral Therapy for Social Anxiety Disorder. Journal of Clinical Medicine, 10(5), 915. https://doi.org/10.3390/jcm10050915








