The Efficacy of Digital Cognitive–Behavioral Interventions in Supporting the Psychological Adjustment and Sleep Quality of Pregnant Women with Sub-Clinical Symptoms: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Primary and Secondary Outcomes
2.3. Search Strategy
2.4. Data Extraction
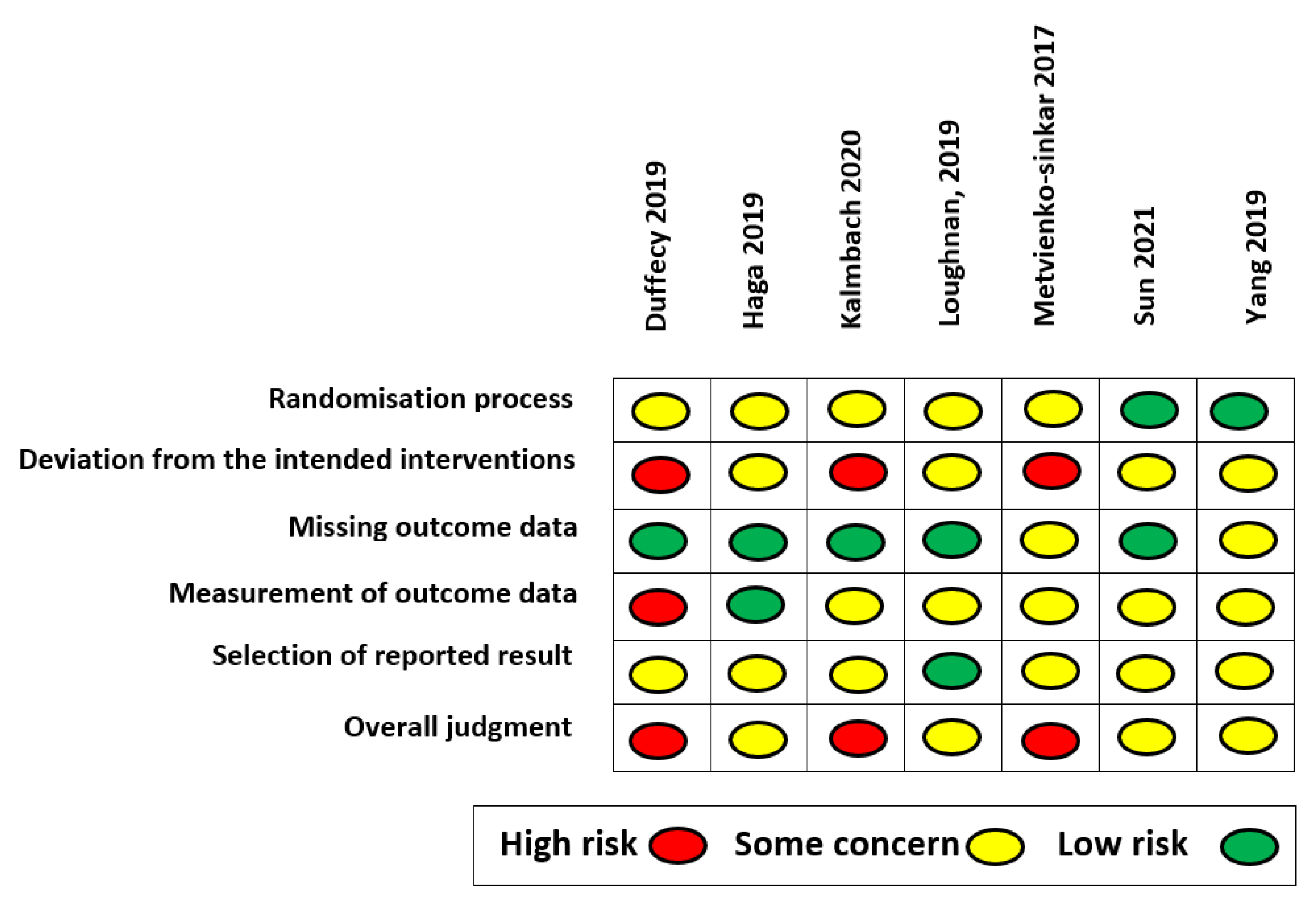
2.5. Quality Assessment
2.6. Data Analysis
3. Results
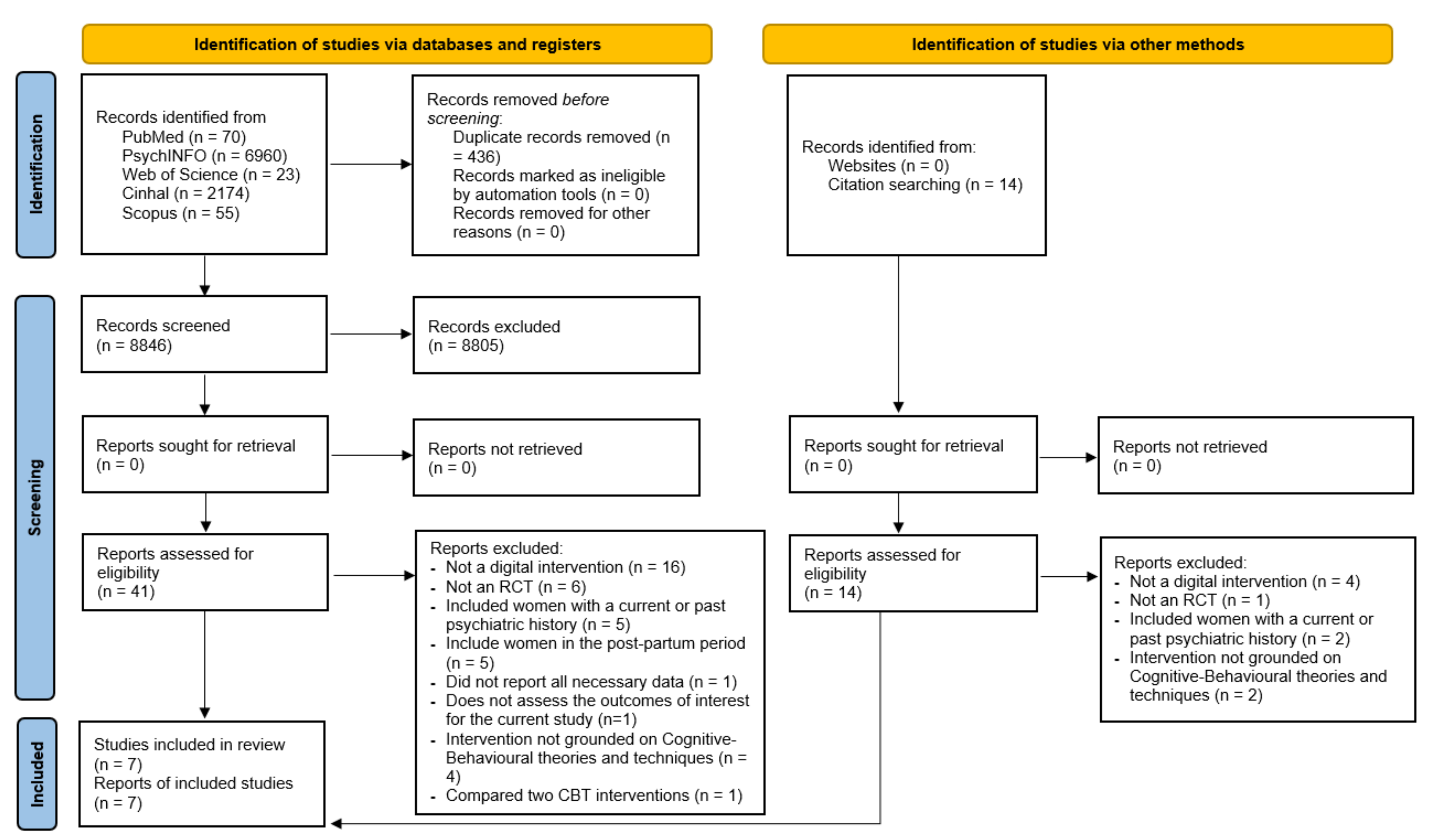
3.1. Search Results
3.2. Studies Characteristics
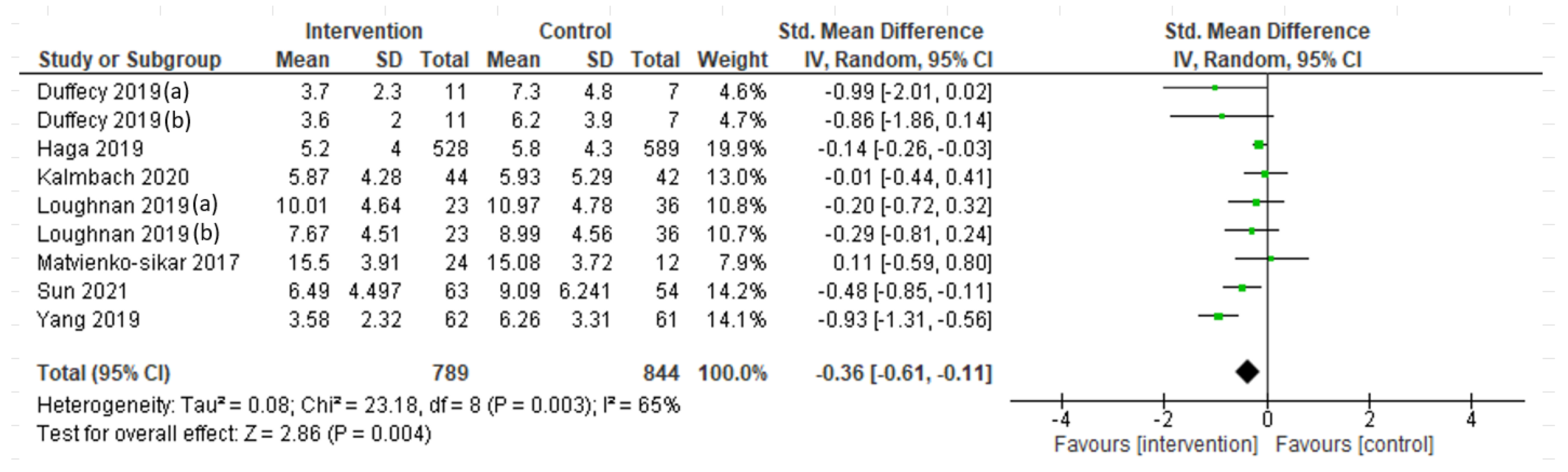
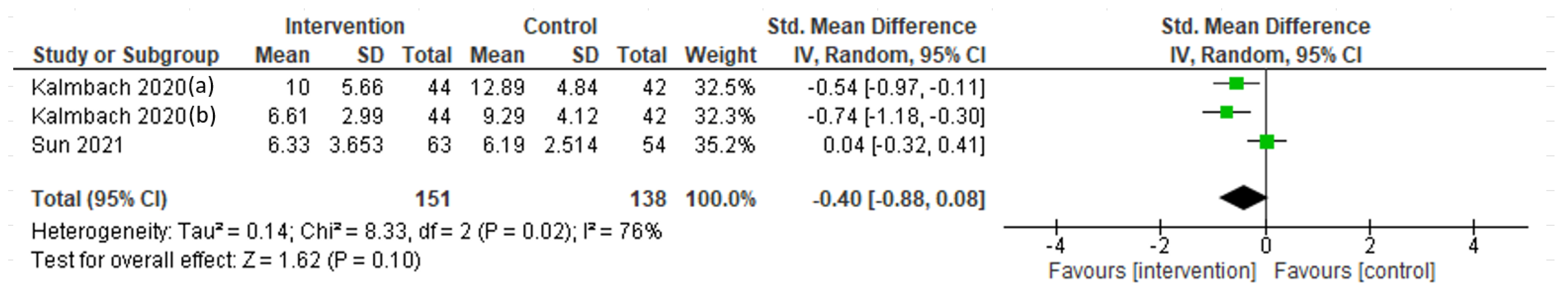
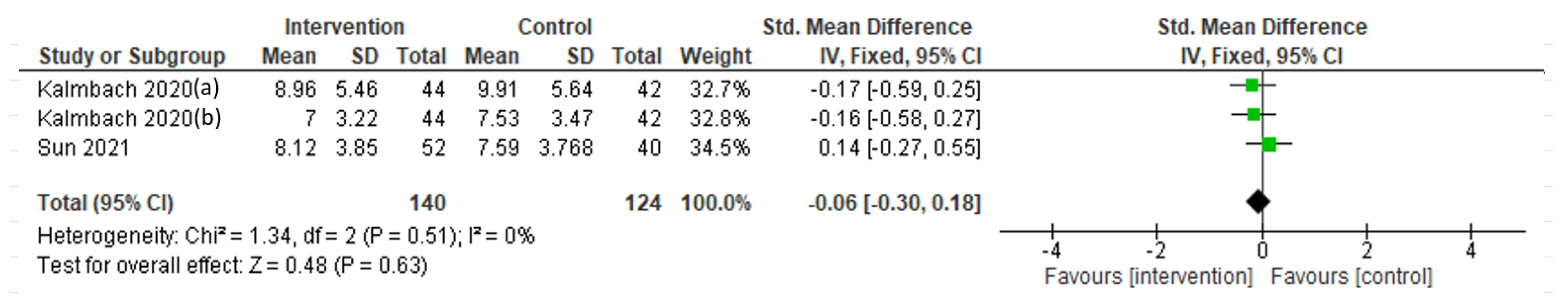
3.3. Intervention Efficacy and Subgroup Analysis
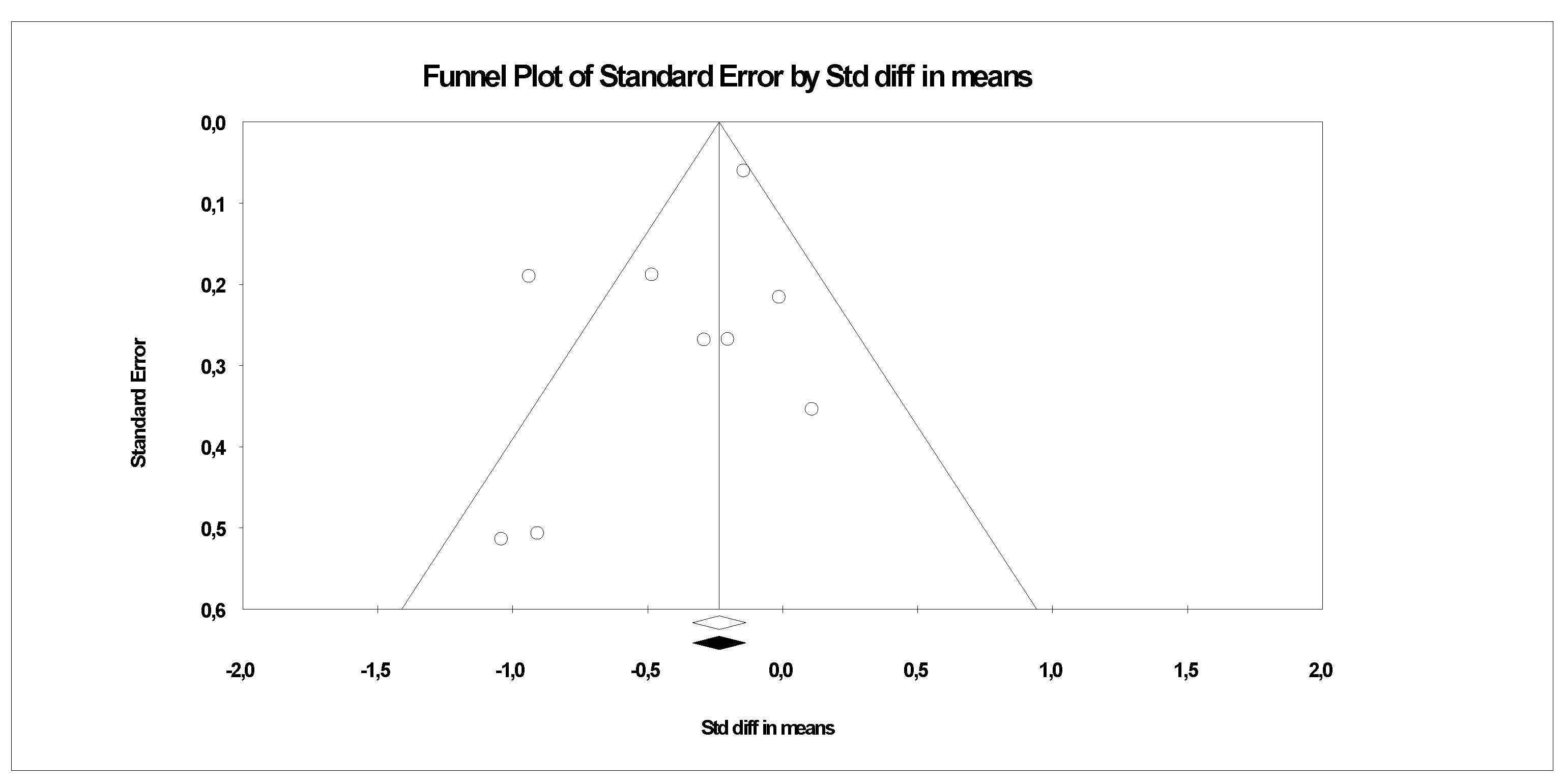
3.4. Publication Bias
3.5. Quality Assessment
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Stern, D.N. The Motherhood Constellation: A Unified View of Parent–Infant Psychotherapy; Routledge: London, UK, 1995. [Google Scholar]
- Sánchez-Polán, M.; Franco, E.; Silva-José, C.; Gil-Ares, J.; Pérez-Tejero, J.; Barakat, R.; Refoyo, I. Exercise During Pregnancy and Prenatal Depression: A Systematic Review and Meta-Analysis. Front. Physiol. 2021, 12, 640024. [Google Scholar] [CrossRef]
- Li, H.; Bowen, A.; Bowen, R.; Muhajarine, N.; Balbuena, L. Mood Instability, Depression, and Anxiety in Pregnancy and Adverse Neonatal Outcomes. BMC Pregnancy Childbirth 2021, 21, 583. [Google Scholar] [CrossRef] [PubMed]
- Cunningham, F.G.; Leveno, K.J.; Bloom, S.L.; Hauth, J.C.; Rouse, D.J.; Spong, C.Y. (Eds.) Parturition. In Williams Obstetrics, 23rd ed.; McGraw-Hill: New York, NY, USA, 2010; p. 143. [Google Scholar]
- Steiner, M. Hormones and Mood: From Menarche to Menopause and Beyond. J. Affect. Disord. 2003, 74, 67–83. [Google Scholar] [CrossRef]
- Lindsay, J.R.; Nieman, L.K. The Hypothalamic-Pituitary-Adrenal Axis in Pregnancy: Challenges in Disease Detection and Treatment. Endocr. Rev. 2005, 26, 775–799. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stetler, C.; Miller, G.E. Depression and Hypothalamic-Pituitary-Adrenal Activation: A Quantitative Summary of Four Decades of Research. Psychosom. Med. 2011, 73, 114–126. [Google Scholar] [CrossRef] [PubMed]
- Eachus, H.; Cunliffe, V.T. Biological Embedding of Psychosocial Stress Over the Life Course. In Epigenetics of Aging and Longevity; Elsevier: Amsterdam, The Netherlands, 2018; pp. 251–270. [Google Scholar]
- Kalin, N.H. The Critical Relationship Between Anxiety and Depression. AJP 2020, 177, 365–367. [Google Scholar] [CrossRef] [PubMed]
- González-Mesa, E.; Kabukcuoglu, K.; Blasco, M.; Körükcü, O.; Ibrahim, N.; González-Cazorla, A.; Cazorla, O. Comorbid Anxiety and Depression (CAD) at Early Stages of the Pregnancy. A Multicultural Cross-Sectional Study. J. Affect. Disord. 2020, 270, 85–89. [Google Scholar] [CrossRef] [PubMed]
- Cena, L.; Gigantesco, A.; Mirabella, F.; Palumbo, G.; Camoni, L.; Trainini, A.; Stefana, A. Prevalence of Comorbid Anxiety and Depressive Symptomatology in the Third Trimester of Pregnancy: Analysing Its Association with Sociodemographic, Obstetric, and Mental Health Features. J. Affect. Disord. 2021, 295, 1398–1406. [Google Scholar] [CrossRef] [PubMed]
- Cheng, C.-Y.; Chou, Y.-H.; Chang, C.-H.; Liou, S.-R. Trends of Perinatal Stress, Anxiety, and Depression and Their Prediction on Postpartum Depression. Int. J. Environ. Res. Public Health 2021, 18, 9307. [Google Scholar] [CrossRef] [PubMed]
- Giardinelli, L.; Innocenti, A.; Benni, L.; Stefanini, M.C.; Lino, G.; Lunardi, C.; Svelto, V.; Afshar, S.; Bovani, R.; Castellini, G.; et al. Depression and Anxiety in Perinatal Period: Prevalence and Risk Factors in an Italian Sample. Arch. Womens Ment. Health 2012, 15, 21–30. [Google Scholar] [CrossRef]
- Stone, S.L.; Diop, H.; Declercq, E.; Cabral, H.J.; Fox, M.P.; Wise, L.A. Stressful Events During Pregnancy and Postpartum Depressive Symptoms. J. Women’s Health 2015, 24, 384–393. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dadi, A.F.; Miller, E.R.; Bisetegn, T.A.; Mwanri, L. Global Burden of Antenatal Depression and Its Association with Adverse Birth Outcomes: An Umbrella Review. BMC Public Health 2020, 20, 173. [Google Scholar] [CrossRef] [Green Version]
- Dennis, C.-L.; Falah-Hassani, K.; Shiri, R. Prevalence of Antenatal and Postnatal Anxiety: Systematic Review and Meta-Analysis. Br. J. Psychiatry 2017, 210, 315–323. [Google Scholar] [CrossRef] [PubMed]
- Woods, S.M.; Melville, J.L.; Guo, Y.; Fan, M.-Y.; Gavin, A. Psychosocial Stress during Pregnancy. Am. J. Obstet. Gynecol. 2010, 202, 61.e1–61.e7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shorey, S.; Chee, C.Y.I.; Ng, E.D.; Chan, Y.H.; Tam, W.W.S.; Chong, Y.S. Prevalence and Incidence of Postpartum Depression among Healthy Mothers: A Systematic Review and Meta-Analysis. J. Psychiatr. Res. 2018, 104, 235–248. [Google Scholar] [CrossRef]
- Anniverno, R.; Bramante, A.; Mencacci, C.; Durbano, F. New Insights into Anxiety Disorders. In Anxiety Disorders in Pregnancy and the Postpartum Period; INTECH Open Access Publisher: London, UK, 2013; pp. 260–285. [Google Scholar]
- Caparros-Gonzalez, R.A.; Romero-Gonzalez, B.; Strivens-Vilchez, H.; Gonzalez-Perez, R.; Martinez-Augustin, O.; Peralta-Ramirez, M.I. Hair Cortisol Levels, Psychological Stress and Psychopathological Symptoms as Predictors of Postpartum Depression. PLoS ONE 2017, 12, e0182817. [Google Scholar] [CrossRef] [PubMed]
- Hutchens, B.F.; Kearney, J. Risk Factors for Postpartum Depression: An Umbrella Review. J. Midwifery Women’s Health 2020, 65, 96–108. [Google Scholar] [CrossRef] [PubMed]
- González-Mesa, E.; Cuenca-Marín, C.; Suarez-Arana, M.; Tripiana-Serrano, B.; Ibrahim-Díez, N.; Gonzalez-Cazorla, A.; Blasco-Alonso, M. Poor Sleep Quality Is Associated with Perinatal Depression. A Systematic Review of Last Decade Scientific Literature and Meta-Analysis. J. Perinat. Med. 2019, 47, 689–703. [Google Scholar] [CrossRef]
- Okun, M.L.; Mancuso, R.A.; Hobel, C.J.; Schetter, C.D.; Coussons-Read, M. Poor Sleep Quality Increases Symptoms of Depression and Anxiety in Postpartum Women. J. Behav. Med. 2018, 41, 703–710. [Google Scholar] [CrossRef] [PubMed]
- Slyepchenko, A.; Minuzzi, L.; Reilly, J.P.; Frey, B.N. Longitudinal Changes in Sleep, Biological Rhythms, and Light Exposure From Late Pregnancy to Postpartum and Their Impact on Peripartum Mood and Anxiety. J. Clin. Psychiatry 2022, 83, 39211. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Zhang, Q.; Gao, T.; Kong, Y.; Qin, Z.; Hu, Y.; Cao, R.; Mei, S. Relations between Stress and Quality of Life among Women in Late Pregnancy: The Parallel Mediating Role of Depressive Symptoms and Sleep Quality. Psychiatry Investig. 2019, 16, 363–369. [Google Scholar] [CrossRef] [PubMed]
- Sedov, I.D.; Cameron, E.E.; Madigan, S.; Tomfohr-Madsen, L.M. Sleep Quality during Pregnancy: A Meta-Analysis. Sleep Med. Rev. 2018, 38, 168–176. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Li, W.; Ma, T.-J.; Zhang, L.; Hall, B.J.; Ungvari, G.S.; Xiang, Y.-T. Prevalence of Poor Sleep Quality in Perinatal and Postnatal Women: A Comprehensive Meta-Analysis of Observational Studies. Front. Psychiatry 2020, 11, 161. [Google Scholar] [CrossRef] [PubMed]
- Lagadec, N. Factors Influencing the Quality of Life of Pregnant Women: A Systematic Review. BMC Pregnancy Childbirth 2018, 18, 455. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Betts, K.S.; Williams, G.M.; Najman, J.M.; Alati, R. The Relationship between Maternal Depression, Anxiety and Stress, and Adult Offspring Behavior and Emotional Problems. Depress Anxiety 2015, 32, 82–90. [Google Scholar] [CrossRef] [PubMed]
- Field, T.; Diego, M.; Hernandez-Reif, M.; Figueiredo, B.; Deeds, O.; Ascencio, A.; Schanberg, S.; Kuhn, C. Comorbid Depression and Anxiety Effects on Pregnancy and Neonatal Outcome. Infant Behav. Dev. 2010, 33, 23–29. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koutra, K.; Chatzi, L.; Bagkeris, M.; Vassilaki, M.; Bitsios, P.; Kogevinas, M. Antenatal and Postnatal Maternal Mental Health as Determinants of Infant Neurodevelopment at 18 Months of Age in a Mother–Child Cohort (Rhea Study) in Crete, Greece. Soc Psychiatry Psychiatr. Epidemiol. 2013, 48, 1335–1345. [Google Scholar] [CrossRef] [PubMed]
- Talge, N.M.; Neal, C.; Glover, V. Antenatal Maternal Stress and Long-Term Effects on Child Neurodevelopment: How and Why? J. Child Psychol. Psychiat. 2007, 48, 245–261. [Google Scholar] [CrossRef] [PubMed]
- Tuovinen, S.; Lahti-Pulkkinen, M.; Girchenko, P.; Lipsanen, J.; Lahti, J.; Heinonen, K.; Reynolds, R.M.; Hämäläinen, E.; Kajantie, E.; Laivuori, H.; et al. Maternal Depressive Symptoms during and after Pregnancy and Child Developmental Milestones. Depress. Anxiety 2018, 35, 732–741. [Google Scholar] [CrossRef] [Green Version]
- Sieverson, C.; Olhaberry, M.; Duarte, J.; Morán-Kneer, J.; Costa, S.; León, M.J.; Valenzuela, S.; Leyton, F.; Honorato, C.; Muzard, A. Beyond the Outcomes: Generic Change Indicators in a Video-Feedback Intervention with a Depressed Mother and Her Baby: A Single Case Study. Res. Psychother.-Psych. 2022, 25, 11–21. [Google Scholar] [CrossRef] [PubMed]
- Fairburn, C.G.; Patel, V. The Impact of Digital Technology on Psychological Treatments and Their Dissemination. Behav. Res. Ther. 2017, 88, 19–25. [Google Scholar] [CrossRef]
- Wang, Q.; Su, M.; Zhang, M.; Li, R. Integrating Digital Technologies and Public Health to Fight Covid-19 Pandemic: Key Technologies, Applications, Challenges and Outlook of Digital Healthcare. Int. J. Environ. Res. Public Health 2021, 18, 6053. [Google Scholar] [CrossRef] [PubMed]
- Feliu-Soler, A.; Cebolla, A.; McCracken, L.M.; D’Amico, F.; Knapp, M.; López-Montoyo, A.; García-Campayo, J.; Soler, J.; Baños, R.M.; Pérez-Aranda, A.; et al. Economic Impact of Third-Wave Cognitive Behavioral Therapies: A Systematic Review and Quality Assessment of Economic Evaluations in Randomized Controlled Trials. Behav. Ther. 2018, 49, 124–147. [Google Scholar] [CrossRef] [PubMed]
- Hayes, S.C.; Hofmann, S.G. The Third Wave of Cognitive Behavioral Therapy and the Rise of Process-Based Care. World Psychiatry 2017, 16, 245–246. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, X.; Laplante, D.P.; Paquin, V.; Lafortune, S.; Elgbeili, G.; King, S. Effectiveness of Cognitive Behavioral Therapy for Perinatal Maternal Depression, Anxiety and Stress: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Clin. Psychol. Rev. 2022, 92, 102129. [Google Scholar] [CrossRef] [PubMed]
- Maguire, P.N.; Clark, G.I.; Wootton, B.M. The Efficacy of Cognitive Behavior Therapy for the Treatment of Perinatal Anxiety Symptoms: A Preliminary Meta-Analysis. J. Anxiety Disord. 2018, 60, 26–34. [Google Scholar] [CrossRef] [PubMed]
- Lau, Y.; Yen, K.Y.; Wong, S.H.; Cheng, J.Y.; Cheng, L.J. Effect of Digital Cognitive Behavioral Therapy on Psychological Symptoms among Perinatal Women in High Income-Countries: A Systematic Review and Meta-Regression. J. Psychiatr. Res. 2022, 146, 234–248. [Google Scholar] [CrossRef]
- Wan Mohd Yunus, W.M.A.; Matinolli, H.-M.; Waris, O.; Upadhyaya, S.; Vuori, M.; Korpilahti-Leino, T.; Ristkari, T.; Koffert, T.; Sourander, A. Digitalized Cognitive Behavioral Interventions for Depressive Symptoms During Pregnancy: Systematic Review. J. Med. Internet. Res. 2022, 24, e33337. [Google Scholar] [CrossRef] [PubMed]
- Hasan, F.; Tu, Y.-K.; Yang, C.-M.; James Gordon, C.; Wu, D.; Lee, H.-C.; Yuliana, L.T.; Herawati, L.; Chen, T.-J.; Chiu, H.-Y. Comparative Efficacy of Digital Cognitive Behavioral Therapy for Insomnia: A Systematic Review and Network Meta-Analysis. Sleep Med. Rev. 2022, 61, 101567. [Google Scholar] [CrossRef]
- Dhillon, A.; Sparkes, E.; Duarte, R.V. Mindfulness-Based Interventions During Pregnancy: A Systematic Review and Meta-Analysis. Mindfulness 2017, 8, 1421–1437. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yan, H.; Wu, Y.; Li, H. Effect of Mindfulness-Based Interventions on Mental Health of Perinatal Women with or without Current Mental Health Issues: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Affect. Disord. 2022, 305, 102–114. [Google Scholar] [CrossRef] [PubMed]
- Corbally, L.; Wilkinson, M. The Effect of Mindfulness-Based Interventions on Stress, Depression and Anxiety During the Perinatal Period in Women Without Pre-Existing Stress, Depressive or Anxiety Disorders: A Systematic Review and Meta-Analysis of Controlled Trials. Mindfulness 2021, 12, 2357–2370. [Google Scholar] [CrossRef]
- Forsell, E.; Bendix, M.; Holländare, F.; Szymanska von Schultz, B.; Nasiell, J.; Blomdahl-Wetterholm, M.; Eriksson, C.; Kvarned, S.; Lindau van der Linden, J.; Söderberg, E.; et al. Internet Delivered Cognitive Behavior Therapy for Antenatal Depression: A Randomised Controlled Trial. J. Affect. Disord. 2017, 221, 56–64. [Google Scholar] [CrossRef]
- O’Mahen, H.A.; Woodford, J.; McGinley, J.; Warren, F.C.; Richards, D.A.; Lynch, T.R.; Taylor, R.S. Internet-Based Behavioral Activation—Treatment for Postnatal Depression (Netmums): A Randomized Controlled Trial. J. Affect. Disord. 2013, 150, 814–822. [Google Scholar] [CrossRef] [PubMed]
- Vanderkruik, R.; Raffi, E.; Freeman, M.P.; Wales, R.; Cohen, L. Perinatal Depression Screening Using Smartphone Technology: Exploring Uptake, Engagement and Future Directions for the MGH Perinatal Depression Scale (MGHPDS). PLoS ONE 2021, 16, e0257065. [Google Scholar] [CrossRef]
- Chae, J.; Kim, H.K. Internet-Based Prenatal Interventions for Maternal Health among Pregnant Women: A Systematic Review and Meta-Analysis. Child. Youth Serv. Rev. 2021, 127, 106079. [Google Scholar] [CrossRef]
- Lara-Cinisomo, S.; Ramirez Olarte, A.; Rosales, M.; Barrera, A.Z. A Systematic Review of Technology-Based Prevention and Treatment Interventions for Perinatal Depression and Anxiety in Latina and African American Women. Matern. Child Health J. 2021, 25, 268–281. [Google Scholar] [CrossRef] [PubMed]
- Loughnan, S.A.; Joubert, A.E.; Grierson, A.; Andrews, G.; Newby, J.M. Internet-Delivered Psychological Interventions for Clinical Anxiety and Depression in Perinatal Women: A Systematic Review and Meta-Analysis. Arch. Womens Ment. Health 2019, 22, 737–750. [Google Scholar] [CrossRef] [PubMed]
- Zuccolo, P.F.; Xavier, M.O.; Matijasevich, A.; Polanczyk, G.; Fatori, D. A Smartphone-Assisted Brief Online Cognitive-Behavioral Intervention for Pregnant Women with Depression: A Study Protocol of a Randomized Controlled Trial. Trials 2021, 22, 227. [Google Scholar] [CrossRef]
- Lee, E.W.; Denison, F.C.; Hor, K.; Reynolds, R.M. Web-Based Interventions for Prevention and Treatment of Perinatal Mood Disorders: A Systematic Review. BMC Pregnancy Childbirth 2016, 16, 38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barrera, A.Z.; Wickham, R.E.; Muñoz, R.F. Online Prevention of Postpartum Depression for Spanish- and English-Speaking Pregnant Women: A Pilot Randomized Controlled Trial. Internet Interv. 2015, 2, 257–265. [Google Scholar] [CrossRef] [Green Version]
- Richards, D.A. Stepped Care: A Method to Deliver Increased Access to Psychological Therapies. Can. J. Psychiatry 2012, 57, 210–215. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. Res. Methods Rep. 2021, 10, 89. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Cochrane Collaboration (Eds.) Cochrane Handbook for Systematic Reviews of Interventions, 2nd ed.; Cochrane Book Series; Wiley-Blackwell: Hoboken, NJ, USA, 2020; ISBN 978-1-119-53662-8. [Google Scholar]
- Borenstein, M.; Hedges, L.; Higgins, J.; Rothstein, H. Comprehensive Meta-Analysis, Version 3; Biostat: Englewood, NJ, USA, 2013. [Google Scholar]
- The Cochrane Collaboration Review Manager (RevMan), Version 5.3; The Nordic Cochrane Centre: Copenhagen, Denmark, 2014.
- Egger, M.; Smith, G.D.; Schneider, M.; Minder, C. Bias in Meta-Analysis Detected by a Simple, Graphical Test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Begg, C.B.; Mazumdar, M. Operating Characteristics of a Rank Correlation Test for Publication Bias. Biometrics 1994, 50, 1088. [Google Scholar] [CrossRef] [PubMed]
- Orwin, R.G. A Fail-Safe N for Effect Size in Meta-Analysis. J. Educ. Stat. 2014, 8, 157–159. [Google Scholar] [CrossRef]
- Duffecy, J.; Grekin, R.; Hinkel, H.; Gallivan, N.; Nelson, G.; O’Hara, M.W. A Group-Based Online Intervention to Prevent Postpartum Depression (Sunnyside): Feasibility Randomized Controlled Trial. JMIR Ment. Health 2019, 6, e10778. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haga, S.M.; Drozd, F.; Lisøy, C.; Wentzel-Larsen, T.; Slinning, K. Mamma Mia-A Randomized Controlled Trial of an Internet-Based Intervention for Perinatal Depression. Psychol. Med. 2019, 49, 1850–1858. [Google Scholar] [CrossRef] [Green Version]
- Kalmbach, D.A.; Cheng, P.; O’Brien, L.M.; Swanson, L.M.; Sangha, R.; Sen, S.; Guille, C.; Cuamatzi-Castelan, A.; Henry, A.L.; Roth, T.; et al. A Randomized Controlled Trial of Digital Cognitive Behavioral Therapy for Insomnia in Pregnant Women. Sleep Med. 2020, 72, 82–92. [Google Scholar] [CrossRef] [PubMed]
- Loughnan, S.A.; Sie, A.; Hobbs, M.J.; Joubert, A.E.; Smith, J.; Haskelberg, H.; Mahoney, A.E.J.; Kladnitski, N.; Holt, C.J.; Milgrom, J.; et al. A Randomized Controlled Trial of “MUMentum Pregnancy”: Internet-Delivered Cognitive Behavioral Therapy Program for Antenatal Anxiety and Depression. J. Affect. Disord. 2019, 243, 381–390. [Google Scholar] [CrossRef] [PubMed]
- Matvienko-Sikar, K.; Dockray, S. Effects of a Novel Positive Psychological Intervention on Prenatal Stress and Well-Being: A Pilot Randomised Controlled Trial. Women Birth 2017, 30, e111–e118. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Li, Y.; Wang, J.; Chen, Q.; Bazzano, A.N.; Cao, F. Effectiveness of Smartphone-Based Mindfulness Training on Maternal Perinatal Depression: Randomized Controlled Trial. J. Med. Internet Res. 2021, 23, e23410. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.; Jia, G.; Sun, S.; Ye, C.; Zhang, R.; Yu, X. Effects of an Online Mindfulness Intervention Focusing on Attention Monitoring and Acceptance in Pregnant Women: A Randomized Controlled Trial. J. Midwifery Women’s Health 2019, 64, 68–77. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feldman, N.; Back, D.; Boland, R.; Torous, J. A Systematic Review of MHealth Application Interventions for Peripartum Mood Disorders: Trends and Evidence in Academia and Industry. Arch. Womens Ment. Health 2021, 24, 881–892. [Google Scholar] [CrossRef] [PubMed]
- Rismawan, W.; Marchira, C.R.; Rahmat, I. Usability, Acceptability, and Adherence Rates of Mobile Application Interventions for Prevention or Treatment of Depression: A Systematic Review. J. Psychosoc. Nurs. Ment. Health Serv. 2021, 59, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Cole-Lewis, H.; Ezeanochie, N.; Turgiss, J. Understanding Health Behavior Technology Engagement: Pathway to Measuring Digital Behavior Change Interventions. JMIR Form. Res. 2019, 3, e14052. [Google Scholar] [CrossRef]
- Martínez-Borba, V.; Suso-Ribera, C.; Osma, J. Usability, Acceptability, and Feasibility of Two Technology-Based Devices for Mental Health Screening in Perinatal Care: A Comparison of Web Versus App. In Pervasive Computing Paradigms for Mental Health; Cipresso, P., Serino, S., Villani, D., Eds.; Springer International Publishing: Cham, Switzerland, 2019; pp. 176–189. ISBN 978-3-030-25872-6. [Google Scholar]
- De Vries, L.P.; Baselmans, B.M.L.; Bartels, M. Smartphone-Based Ecological Momentary Assessment of Well-Being: A Systematic Review and Recommendations for Future Studies. J. Happiness Stud. 2021, 22, 2361–2408. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Marcusson-Clavertz, D.; Yoshiuchi, K.; Smyth, J.M. Potential Benefits of Integrating Ecological Momentary Assessment Data into MHealth Care Systems. BioPsychoSocial Med. 2019, 13, 19. [Google Scholar] [CrossRef] [Green Version]
- Morrison, L.G.; Geraghty, A.W.A.; Lloyd, S.; Goodman, N.; Michaelides, D.T.; Hargood, C.; Weal, M.; Yardley, L. Comparing Usage of a Web and App Stress Management Intervention: An Observational Study. Internet Interv. 2018, 12, 74–82. [Google Scholar] [CrossRef] [PubMed]
- Conejo-Cerón, S.; Lokkerbol, J.; Moreno-Peral, P.; Wijnen, B.; Fernández, A.; Mendive, J.M.; Smit, F.; Bellón, J.Á. Health-Economic Evaluation of Psychological Interventions for Depression Prevention: Systematic Review. Clin. Psychol. Rev. 2021, 88, 102064. [Google Scholar] [CrossRef] [PubMed]


| Author | Country | N | Age M (SD) | Marital Status N; % | Educational Level N; % | Weeks Pregnant M (SD) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| EG | CG | EG | CG | EG | CG | EG | CG | EG | CG | ||
| [64] | USA | 18 | 7 | 30.5 (4.05) |
|
| n/r | n/r | |||
| [65] | Norway | 678 | 664 | 31 (4.6) | 31.1 (4.5) | n/r | n/r |
|
| n/r | n/r |
| [66] | USA | 46 | 45 | 28.91 (4.25) | 29.16 (4.11) | n/r | n/r | n/r | n/r | n/r | n/r |
| [67] | Australia | 36 | 41 | 31.69 (4.44) | 31.54 (3.63) |
|
|
|
| 20.54 (6.01) | 22.63 (5.76) |
| [68] # | Ireland | 32 | 14 | 33.81(2.53) |
| n/r | n/r | 16.15 (2.88) | |||
| [69] | China | 84 | 84 | 30.27 (3.8) | 29.55 (4.21) |
| n/r | n/r | 13.81 * (na) | 14.41 * (na) | |
| [70] | China | 62 | 61 | 31.31 (4.97) | 30.98 (3.91) | n/r | n/r |
|
| 25.52 (1.84) | 26.33 (3.45) |
| Author | Intervention | Control Condition | Theoretical Background | Full-Protocol vs. Techniques | Length (Weeks) | Intervention Description |
|---|---|---|---|---|---|---|
| [64] | Share Web-based | Active; same as Share without the group activities | CBT | Techniques | 8 | Unguided group intervention that comprised 16 main didactic activities. It provided information on both pregnancy and the postpartum period. The intervention also included 3 postpartum bust sessions (not considered in the current study). The CBT techniques employed were the following: (1) thought restructuring; (2) mood tracking; (3) activity scheduling; (4) monitoring; (5) relaxation; (6) goal setting. Participants could also interact with other women (by posting, leaving comments or likes on their posts, and by sending direct messages) encouraging discussion among them after each lesson. Participants had a personal profile in which they could post information about themselves to increase group bonding. |
| [65] | Mamma Mia * Web-based | TAU | Third generation CBT | Techniques | 16 # | An unguided program that included 11 sessions each, which needed to be concluded to proceed to the following lesson. Provided psychoeducational information on pregnancy in a step-by-step fashion as well as cognitive and behavioral assignments. The intervention was focused on the following: (1) providing information on the specific perinatal period; (2) working on expectancies and attitudes; (3) supporting attachment, emotion regulation, and help-seeking; (4) working on relationship satisfaction and communication skills. |
| [66] | Sleepio Web-based CBTI program | Active; sleep education | CBT | Full protocol | 6 | Digital CBT intervention was specific for insomnia symptoms and included 6 sessions. The sessions were guided by a personal agent or “virtual therapist.” New sessions could be completed only after finishing the preceding one. The interventions included: (1) behavioral components (sleep restriction, stimulus control); (2) cognitive components (e.g., cognitive restructuring, paradoxical intention); (3) progressive muscle relaxation; (4) sleep hygiene. |
| [67] | MUMmentum Web-based | TAU | CBT | Full protocol | 4 | Unguided CBT intervention specific for pregnant women showing generalized anxiety and depression symptoms. It included three lessons during which content was presented through illustrated stories displayed using slides to learn how to self-manage anxiety and depression symptoms. Overall the intervention included: (1) psychoeducation; (2) relaxation techniques; (3) thought challenging; (4) structured problem solving; (5) active planning and monitoring; (6) grade exposure; (7) assertive communication; (8) relapse prevention; (9) sleep hygiene; (10) pleasant activities; (11) self-care plans; (10) understanding intrusive thoughts and images. |
| [68] | Gratitude and Mindfulness Web-based | TAU | Third generation CBT | Techniques | 3 | The unguided intervention focused on two main components: (1) a gratitude diary that was aimed at favoring reflection on the pregnancy experience; (2) mindfulness audio tracks, particularly the body scan practice, during which the focus was placed on breathing and on paying attention to each part of the body. |
| [69] | Spirits Healing Smartphone-based | Active; attention control group | Third generation CBT | Full protocol | 8 | Revised unguided MBCT focused on perinatal depression and negative emotions and on supporting the adaptation to the body changes given by the pregnancy. It included formal mindfulness training deployed through videos, reading material, and audio tracks for guided mindfulness practices. It comprised 8 sessions focused on: (1) providing information on mindfulness; (2) increasing focus on the present; (3) supporting mindfulness of negative emotions; (4) accepting difficulties; (5) understanding that thoughts are only thoughts; (6) supporting the enjoyment of daily happiness; (7) favoring mindfulness during pregnancy and childbirth; (8) continuing mindfulness practice. |
| [70] | Mindfulness intervention Smartphone-based | TAU | Third generation CBT | Techniques | 8 | Unguided mindfulness intervention was created ad hoc by a multidisciplinary team and supported by mindfulness-trained nurses who provided technical help while monitoring for changes in the symptom levels. Four mindfulness sessions were video-recorded by the mindfulness-trained nurses and shared on a smartphone chat platform (Wechat) and supplemented by text, pictures, and audio recordings that women could review. These sessions were focused on different mindfulness practices: (1) body screening; (2) relaxation; (3) meditation. During each session, the participants reviewed what had been done in the previous session and were then introduced to new mindfulness constructs. Between-session homework was foreseen by the intervention. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mancinelli, E.; Bassi, G.; Gabrielli, S.; Salcuni, S. The Efficacy of Digital Cognitive–Behavioral Interventions in Supporting the Psychological Adjustment and Sleep Quality of Pregnant Women with Sub-Clinical Symptoms: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 9549. https://doi.org/10.3390/ijerph19159549
Mancinelli E, Bassi G, Gabrielli S, Salcuni S. The Efficacy of Digital Cognitive–Behavioral Interventions in Supporting the Psychological Adjustment and Sleep Quality of Pregnant Women with Sub-Clinical Symptoms: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2022; 19(15):9549. https://doi.org/10.3390/ijerph19159549
Chicago/Turabian StyleMancinelli, Elisa, Giulia Bassi, Silvia Gabrielli, and Silvia Salcuni. 2022. "The Efficacy of Digital Cognitive–Behavioral Interventions in Supporting the Psychological Adjustment and Sleep Quality of Pregnant Women with Sub-Clinical Symptoms: A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 19, no. 15: 9549. https://doi.org/10.3390/ijerph19159549
APA StyleMancinelli, E., Bassi, G., Gabrielli, S., & Salcuni, S. (2022). The Efficacy of Digital Cognitive–Behavioral Interventions in Supporting the Psychological Adjustment and Sleep Quality of Pregnant Women with Sub-Clinical Symptoms: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 19(15), 9549. https://doi.org/10.3390/ijerph19159549







