Effectiveness of Lifestyle Health Promotion Interventions for Nurses: A Systematic Review
Abstract
1. Introduction
Aims
2. Materials and Methods
2.1. Eligibility Criteria
2.1.1. Types of Studies
2.1.2. Types of Participants
2.1.3. Context/Setting
2.1.4. Types of Interventions
- Health risk factors: overweight or obesity, diet, PA, smoking habits, problem drinking.
- Clinical health: type 2 diabetes, stroke, chronic heart disease, cancers, hypertension.
- Psychological health: work-related stress, mood, self-efficacy.
2.1.5. Comparator(s)/Control
2.1.6. Types of Outcome Measures
Health Risk Factors:
Clinical Health Outcomes:
Psychological Health Outcomes:
Work-Related or Organisational Outcomes:
2.2. Search Strategy
2.3. Selection Processes
2.4. Data Extraction
2.5. Risk of Bias
2.6. Method of Synthesis
3. Results
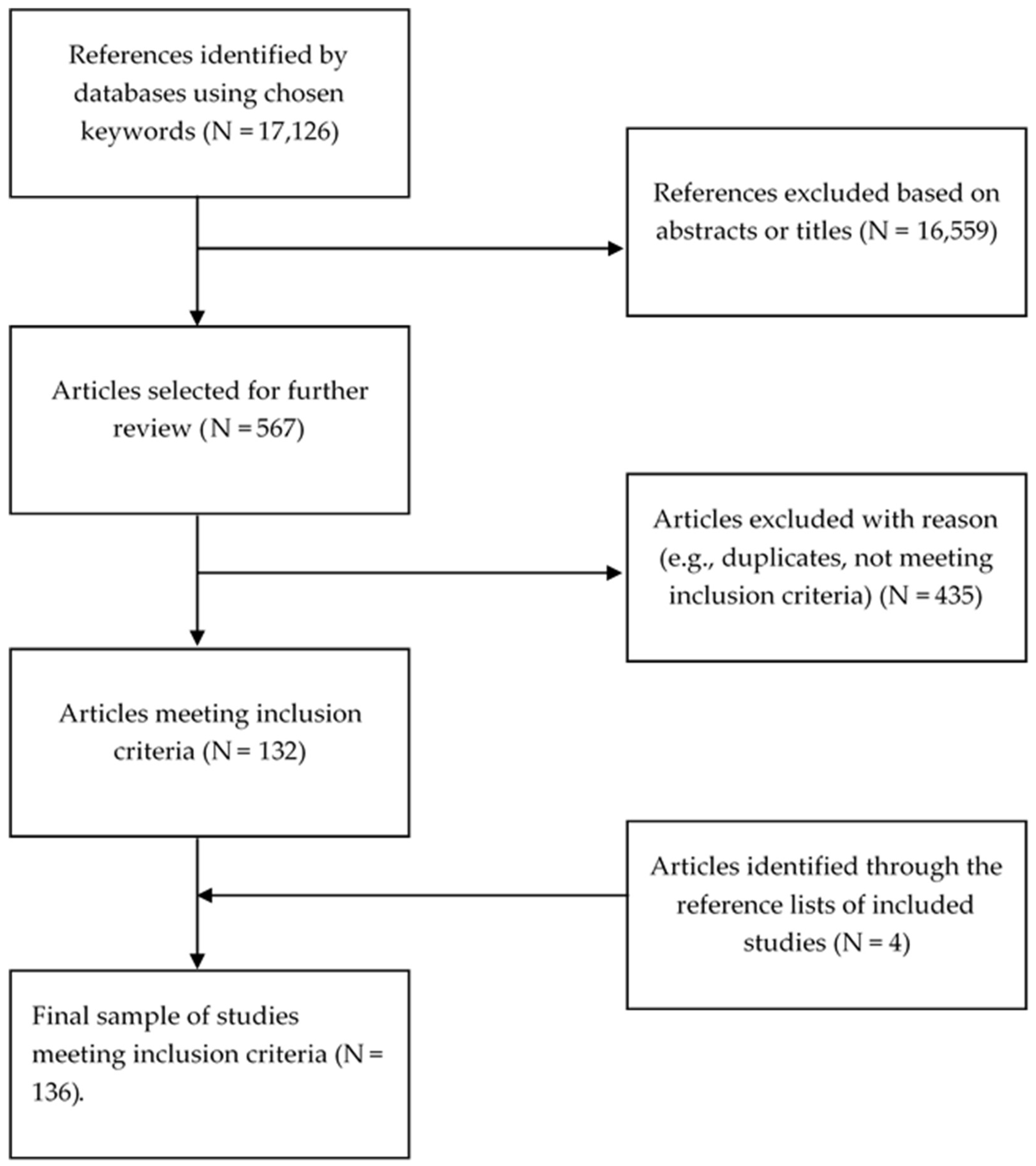
3.1. Included Studies
Designs of the Included Studies
3.2. Characteristics of the Samples
3.3. Characteristics of the Interventions
3.3.1. Educational Interventions
3.3.2. Physical Activity and Dietary Interventions
3.3.3. Smoking Behaviour
3.3.4. Mindfulness and Relaxation
3.3.5. Other Intervention Types
3.3.6. Intervention Duration and Follow-up
3.3.7. Intervention Settings
3.4. Measures Used
3.4.1. Health Risk Factors
3.4.2. Psychological Health Outcomes
3.4.3. Work-Related or Organisational Outcomes
3.5. Overall Effect of the Interventions
3.6. Specific Effects of the Interventions
3.6.1. Health Risk Factors
Clinical Health Outcomes
Body Composition and Functioning
Diet and Nutrition
Physical Activity and Sedentary Behaviour
Smoking
3.6.2. Psychological Health Outcomes
Stress and Coping
Depression and Anxiety
Burnout and Compassion Fatigue
Mindfulness
General Wellbeing and Life Satisfaction
Self-Efficacy
3.6.3. Work-Related or Organisational Outcomes
3.7. Success Rate of the Interventions
3.8. Other Intervention Effects
3.8.1. Unintended Intervention Effects
3.8.2. Interventions with No Significant Positive Effect
3.9. Dropout Rates
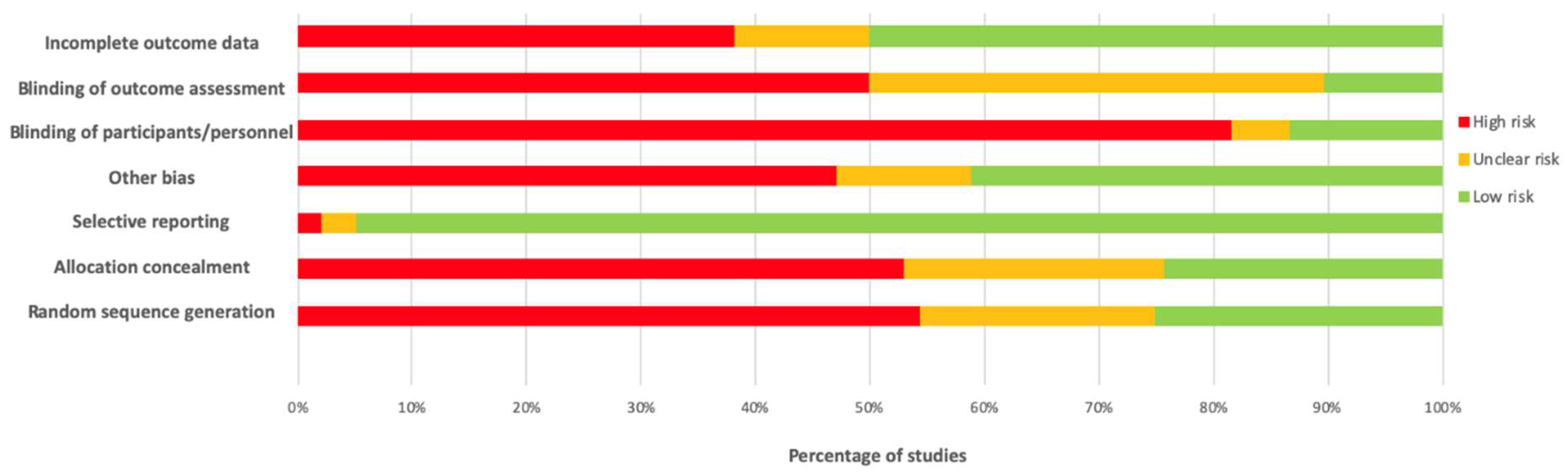
3.10. Results of Included RCTs
3.11. Risk of Bias Results
3.12. Quality Assessment
4. Discussion
4.1. Summary of the Characteristics of the Studies
4.2. Successfulness of Interventions
4.3. Results Specific to RCTs
4.4. Quality Concerns
4.5. Review Limitations
4.6. Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Terada, T.; Mistura, M.; Tulloch, H.; Pipe, A.; Reed, J. Dietary behaviour is associated with cardiometabolic and psychological risk indicators in female hospital nurses—A post-hoc, cross-sectional study. Nutrients 2019, 11, 2054. [Google Scholar] [CrossRef] [PubMed]
- Nilan, K.; McKeever, T.; McNeill, A.; Raw, M.; Murray, R. Prevalence of tobacco use in healthcare workers: A systematic review and meta-analysis. PLoS ONE 2019, 14, e0220168. [Google Scholar] [CrossRef] [PubMed]
- Priano, S.M.; Hong, O.S.; Chen, J.L. Lifestyles and health-related outcomes of US hospital nurses: A systematic review. Nurs. Outlook 2018, 66, 66–76. [Google Scholar] [CrossRef] [PubMed]
- Reed, J.; Prince, S. Women’s heart health: A focus on nurses’ physical activity and sedentary behaviour. Curr. Opin. Cardiol. 2018, 35, 514–520. [Google Scholar]
- Schluter, P.; Turner, C.; Benefer, C. Long working hours and alcohol risk among Australian and New Zealand nurses and midwives: A cross-sectional study. Int. J. Nurs. Stud. 2012, 49, 701–709. [Google Scholar] [CrossRef]
- Blake, H.; Mo, P.; Lee, S.; Batt, M. Health in the NHS: Lifestyle behaviours of hospital employees. Perspect. Public Health 2012, 132, 213–215. [Google Scholar]
- Mo, P.; Blake, H.; Batt, M. Getting healthcare staff more active: The mediating role of self-efficacy. Br. J. Health Psychol. 2011, 16, 690–706. [Google Scholar] [CrossRef]
- Malik, S.; Blake, H.; Batt, M. How healthy are our nurses? New and registered nurses compared. Br. J. Nurs. 2011, 20, 489–496. [Google Scholar] [CrossRef]
- Kyle, R.; Wills, J.; Mahoney, C.; Hoyle, L.; Kelly, M.; Atherton, I. Obesity prevalence among healthcare professionals in England: A cross-sectional study using the Health Survey for England. BMJ Open 2017, 4, 7. [Google Scholar] [CrossRef]
- Kings Fund Time to Think Differently. Available online: https://www.kingsfund.org.uk/projects/time-think-differently/trends-healthy-behaviours-obesity (accessed on 22 November 2019).
- Moberly, T. Sickness absence rates across the nhs. BMJ 2018, 361, 2017–2018. [Google Scholar] [CrossRef][Green Version]
- Soroush, A.; Shamsi, M.; Izadi, N.; Heydarpour, B.; Samadzadeh, S.; Shahmohammadi, A. Musculoskeletal disorders as common problems among Iranian nurses: A systematic review and meta-analysis study. Int. J. Prev. Med. 2018, 9, 27. [Google Scholar] [PubMed]
- Yao, Y.; Zhao, S.; An, Z.; Wang, S.; Li, H.; Lu, L.; Yao, S. the Associations of Work Style and Physical Exercise With the Risk of Work-Related Musculoskeletal Disorders in Nurses. Int. J. Occup. Med. Environ. Health 2019, 32, 15–24. [Google Scholar] [CrossRef] [PubMed]
- Mynarski, W.; Niestrój-jaworska, M. Physical recreational activity and musculoskeletal disorders in nurses. Med. Pr. 2014, 65, 181–188. [Google Scholar] [PubMed]
- Schneider, A.; Bak, M.; Mahoney, C.; Hoyle, L.; Kelly, M.; Atherton, I.; Kyle, R. Health-related behaviours of nurses and other healthcare professionals: A cross-sectional study using the Scottish Health Survey. J. Adv. Nurs. 2019, 75, 1239–1251. [Google Scholar] [CrossRef]
- Chappel, S.; Verswijveren, S.; Aisbett, B.; Considine, J.; Ridgers, N. Nurses’ occupational physical activity levels: A systematic review. Int. J. Nurs. Stud. 2017, 73, 52–62. [Google Scholar] [CrossRef]
- Al-Tannier, M.; Kobrosly, S.; Elbakri, N. Prevalence and predictors of physical exercise among nurses: A cross-sectional study. Saudi Med. J. 2017, 38, 209–212. [Google Scholar] [CrossRef]
- Nicholls, R.; Perry, L.; Duffield, C.; Gallagher, R.; Pierce, H. Barriers and facilitators to healthy eating for nurses in the workplace: An integrative review. J. Adv. Nurs. 2017, 73, 1051–1065. [Google Scholar] [CrossRef]
- Maharaj, S.; Lees, T.; Lal, S. Prevalence and risk factors of depression, anxiety, and stress in a cohort of Australian nurses. Int. J. Environ. Res. Public Health 2019, 16, 61. [Google Scholar] [CrossRef]
- Haplin, Y.; Terry, L.; Curzio, J. A longitudinal, mixed methods investigation of newly qualified nurses’ workplace stressors and stress experiences during transition. J. Adv. Nurs. 2017, 73, 2577–2586. [Google Scholar]
- Adriaenssens, J.; De Gucht, V.; Maes, S. Determinants and prevalence of burnout in emergency nurses: A systematic review of 25 years of research. Int. J. Nurs. Stud. 2015, 52, 649–661. [Google Scholar] [CrossRef]
- Stephenson, J. Specialist Nursing Care ‘Improves Life Expectancy of Cancer Patients’. Available online: https://www.nursingtimes.net/news/research-and-innovation/specialist-nursing-care-improves-life-expectancy-of-cancer-patients-04-07-2018/ (accessed on 15 November 2019).
- De La Fuente-Solana, E.; Suleiman-Martos, N.; Pradas-Hernandez, L.; Gomez-Urquiza, J.; Canadas-De La Fuente, G.; Albendin-Garcia, L. Prevalence, related factors, and levels of burnout syndrome among nurses working in gynecology and obstetrics services: A systematic review and meta-analysis. Int. J. Environ. Res. Public Health 2019, 16, 2585. [Google Scholar] [CrossRef] [PubMed]
- Gomez-Urquiza, J.; Aneas-Lopez, A.; Fuente-Solana, E.; Albendin-Garcia, L.; Diaz-Rodriguez, L.; Fuente, G. Prevalence, risk factors, and levels of burnout among oncology nurses: A systematic review. Oncol. Nurs. Forum 2016, 43, E104–E120. [Google Scholar] [CrossRef] [PubMed]
- Shahri, S.S.S.; Ghashghaee, A.; Behzadifar, M.; Bragazzi, N.L.; Behzadifar, M.; Mousavinejad, N.; Ghaemmohamadi, M.S.; Ebadi, F.; Seyedin, H. Depression among Iranian nurses: A systematic review and meta-analysis. Med. J. Islam. Repub. Iran 2017, 31, 860–868. [Google Scholar] [CrossRef] [PubMed]
- NHS England Simon Stevens Announces Major Drive to Improve Health in NHS Workplace 2015. Available online: https://www.england.nhs.uk/2015/09/02/nhs-workplace/ (accessed on 21 November 2019).
- West, M.A.; Dawson, J.F. Employee Engagement and NHS Performance—Employee-Engagement-NHS-Performance-West-Dawson-Leadership-Review2012-Paper, King’s Fund; NHS South West Leadership Academy: Taunton, MA, USA, 2012; pp. 1–23. [Google Scholar]
- Personnel Today. NHS Sickness Absence: HR Must First Address Culture of “Presenteeism” 2009. Available online: https://www.personneltoday.com/hr/nhs-sickness-absence-hr-must-first-address-culture-of-presenteeism/ (accessed on 22 November 2019).
- Lui, J.; Johnston, J. Working while sick: Validation of the multidimensional presenteeism exposures and productivity survey for nurses (MPEPS-N). Health Serv. Res. 2019, 19, 542. [Google Scholar] [CrossRef]
- Personnel Today. “Presenteeism Costs Twice as Much as Sickness Absence” 2015. Available online: https://www.personneltoday.com/hr/presenteeism-costs-twice-much-sickness-absence/ (accessed on 12 November 2019).
- Letvak, S.; Ruhm, C.; Lane, S. The impact of nurses’ health on productivity and quality of care. J. Nurs. Adm. 2011, 41, 162–167. [Google Scholar] [CrossRef]
- Sarafis, P.; Rousaki, E.; Tsounis, A.; Malliarou, M.; Lahana, L.; Bamidis, P.; Niakas, D.; Papastavrou, E. The impact of occupational stress on nurses’ caring behaviors and their health related quality of life. BMC Nurs. 2016, 15, 1–9. [Google Scholar] [CrossRef]
- Davey, M.; Cummings, G.; Newburn-Cook, C. Predictors of nurse absenteeism in hospitals: A systematic review. J. Nurs. Manag. 2009, 17, 312–330. [Google Scholar] [CrossRef]
- Letvak, S.; Ruhm, C.; Gupta, S. Nurses’ presenteeism and its effects on self-reported quality of care and costs. Am. J. Nurs. 2012, 112, 30–38. [Google Scholar] [CrossRef]
- Guillaumie, L.; Boiral, O.; Champagne, J. A mixed-methods systematic review of the effects of mindfulness on nurses. J. Adv. Nurs. 2017, 73, 1017–1034. [Google Scholar] [CrossRef]
- Garcia, C.; Abreu, L.; Ramos, J.; Castro, C. Influence of burnout on patient safety: Systematic review and meta-analysis. Medicina 2019, 55, 553. [Google Scholar] [CrossRef]
- Jordan, T.; Khubchandani, J.; Wiblishauser, M. The impact of perceived stress and coping adequacy on the health of nurses: A pilot investigation. Nurs. Res. Pract. 2016, 2016, 5843256. [Google Scholar] [CrossRef]
- Khamisa, N.; Oldenburg, B.; Peltzer, K. Work related stress, burnout, job satisfaction and general health of nurses. Int. J. Environ. Res. Public Health 2015, 12, 652–666. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Fuentes, M.; Molero Jurado, M.; Barragán Martín, A.; Simón Márquez, M.; Martos Martínez, Á.; Gázquez Linares, J. The Mediating Role of Perceived Stress in the Relationship of Self-Efficacy and Work Engagement in Nurses. J. Clin. Med. 2018, 8, 10. [Google Scholar] [CrossRef]
- Jaradat, Y.; Nielsen, M.; Kristensen, P. Shift work, mental distress and job satisfaction among Palestinian nurses. Occup. Med. (Chic. Ill) 2017, 67, 71–74. [Google Scholar] [CrossRef] [PubMed]
- Phiri, L.P.; Draper, C.E.; Lambert, E.V.; Kolbe-Alexander, T.L. Nurses’ lifestyle behaviours, health priorities and barriers to living a healthy lifestyle: A qualitative descriptive study. BMC Nurs. 2014, 13, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Blake, H.; Patterson, J. Paediatric nurses’ attitudes towards the promotion of healthy eating. Br. Nurs. J. 2015, 24, 108–112. [Google Scholar] [CrossRef]
- Kelly, M.; Wills, J. Systematic review: What works to address obesity in nurses? Occup. Med. (Chic. Ill) 2018, 68, 228–238. [Google Scholar] [CrossRef]
- Duaso, M.; Bakhshi, S.; Muhika, A. Nurses’ smoking habits and their professional smoking cessation practices. A systematic review and meta-analysis. Int. J. Nurs. Stud. 2017, 67, 3–11. [Google Scholar] [CrossRef]
- Chan, C.W.; Perry, L. Lifestyle health promotion interventions for the nursing workforce: A systematic review. J. Clin. Nurs. 2012, 21, 2247–2261. [Google Scholar] [CrossRef]
- Häggman-Laitila, A.; Romppanen, J. Outcomes of interventions for nurse leaders’ well-being at work: A quantitative systematic review. J. Adv. Nurs. 2018, 74, 34–44. [Google Scholar] [CrossRef]
- Halter, M.; Pelone, F.; Boiko, O.; Beighton, C.; Harris, R.; Gale, J.; Gourlay, S.; Drennan, V. Interventions to Reduce Adult Nursing Turnover: A Systematic Review of Systematic Reviews. Open Nurs. J. 2017, 11, 108–123. [Google Scholar] [CrossRef] [PubMed]
- Duhoux, A.; Menear, M.; Charron, M.; Lavoie-Tremblay, M.; Alderson, M. Interventions to promote or improve the mental health of primary care nurses: A systematic review. J. Nurs. Manag. 2017, 25, 597–607. [Google Scholar] [CrossRef] [PubMed]
- Torquati, L.; Pavey, T.; Kolbe-Alexander, T.; Leveritt, M. Promoting diet and physical activity in nurses: A systematic review. Am. J. Health Promot. 2017, 31, 19–27. [Google Scholar] [CrossRef] [PubMed]
- Blake, H.; Narayanasamy, M.; Batt, M.E.; Khunti, K. Effectiveness of lifestyle health promotion interventions for nurses: Protocol for a systematic review. J. Nurs. Pract. 2019, 3, 81–85. [Google Scholar]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef]
- Schulz, K.F.; Altman, D.C.; Moher, D.; The CONSORT Group. CONSORT 2010 Statement: Updated guidelines for reporting parallel group randomised trials. Trials 2010, 11, 325–332. [Google Scholar] [CrossRef]
- Moher, D.; Hopewell, S.; Schulz, K.; Montori, V.; Gøtzsche, P.; Devereaux, P.; Elbourne, D.; Egger, M.; Altman, D.G. ConSoRT 2010 explanation and elaboration: Updated guidelines for reporting parallel group randomised trials. BMJ 2010, 340, c869. [Google Scholar] [CrossRef]
- Higgins, J. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef]
- Hersch, R.K.; Cook, R.F.; Deitz, D.K.; Kaplan, S.; Hughes, D.; Friesen, M.A.; Vezina, M. Reducing nurses’ stress: A randomized controlled trial of a web-based stress management program for nurses. Appl. Nurs. Res. 2016, 32, 18–25. [Google Scholar] [CrossRef]
- Wei, R.; Ji, H.; Li, J.; Zhang, L. Active intervention can decrease burnout In ed nurses. J. Emerg. Nurs. 2017, 43, 145–149. [Google Scholar] [CrossRef]
- Müller, A.; Heiden, B.; Herbig, B.; Poppe, F.; Angerer, P. Improving well-being at work: A randomized controlled intervention based on selection, optimization, and compensation. J. Occup. Health Psychol. 2016, 21, 169–181. [Google Scholar] [CrossRef] [PubMed]
- Moazzami, Z.; Dehdari, T.; Taghdisi, M.H.; Soltanian, A. Effect of an ergonomics-based educational intervention based on transtheoretical model in adopting correct body posture among operating room nurses. Glob. J. Health Sci. 2015, 8, 26–34. [Google Scholar] [CrossRef] [PubMed]
- Menzel, N.N.; Robinson, M.E. Back pain in direct patient care providers: Early intervention with cognitive behavioral therapy. Pain Manag. Nurs. 2006, 7, 53–63. [Google Scholar] [CrossRef] [PubMed]
- Mealer, B.M.; Conrad, D.; Evans, J.; Jooste, K.; Solyntjes, J.; Rothbaum, B.; Moss, M. Feasibility and acceptability of a resilience training program for intensive care unit nurses. Chall. Crit. Care Work 2014, 23, 97–106. [Google Scholar] [CrossRef]
- McElligott, D.; Capitulo, K.L.; Morris, D.L.; Click, E.R. The effect of a holistic program on health-promoting behaviors in hospital registered nurses. J. Holist. Nurs. 2010, 28, 175–183. [Google Scholar] [CrossRef]
- Maatouk, I.; Müller, A.; Angerer, P.; Schmook, R.; Nikendei, C.; Herbst, K.; Gantner, M.; Herzog, W.; Gündel, H. Healthy ageing at work—Efficacy of group interventions on the mental health of nurses aged 45 and older: Results of a randomised, controlled trial. PLoS ONE 2018, 13, 1–19. [Google Scholar] [CrossRef]
- Kravits, K.; McAllister-Black, R.; Grant, M.; Kirk, C. Self-care strategies for nurses: A psycho-educational intervention for stress reduction and the prevention of burnout. Appl. Nurs. Res. 2010, 23, 130–138. [Google Scholar] [CrossRef]
- Hartvigsen, J.; Lauritzen, S.; Lings, S.; Lauritzen, T. Intensive education combined with low tech ergonomic intervention does not prevent low back pain in nurses. Occup. Environ. Med. 2005, 62, 13–17. [Google Scholar] [CrossRef]
- Ewers, P.; Bradshaw, T.; McGovern, J.; Ewers, B. Does training in psychosocial interventions reduce burnout rates in forensic nurses? J. Adv. Nurs. 2002, 37, 470–476. [Google Scholar] [CrossRef]
- Craigie, M.; Slatyer, S.; Hegney, D.; Osseiran-Moisson, R.; Gentry, E.; Davis, S.; Dolan, T.; Rees, C. A pilot evaluation of a mindful self-care and resiliency (MSCR) intervention for nurses. Mindfulness (N. Y.) 2016, 7, 764–774. [Google Scholar] [CrossRef]
- Tsai, Y.C.; Liu, C.H. An eHealth education intervention to promote healthy lifestyles among nurses. Nurs. Outlook 2015, 63, 245–254. [Google Scholar] [CrossRef] [PubMed]
- Karahan, A.; Bayraktar, N. Effectiveness of an education program to prevent nurses’ low back pain: An interventional study in Turkey. Workplace Health Saf. 2013, 61, 73–78. [Google Scholar] [CrossRef] [PubMed]
- Isaksson Rø, K.E.; Gude, T.; Tyssen, R.; Aasland, O.G. A self-referral preventive intervention for burnout among Norwegian nurses: One-year follow-up study. Patient Educ. Couns. 2010, 78, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Flarity, K.; Nash, K.; Jones, W.; Steinbruner, D. Intervening to improve compassion fatigue resiliency in forensic nurses. Adv. Emerg. Nurs. J. 2016, 38, 147–156. [Google Scholar] [CrossRef] [PubMed]
- Flarity, K.; Gentry, J.E.; Mesnikoff, N. The effectiveness of an educational program on preventing and treating compassion fatigue in emergency nurses. Adv. Emerg. Nurs. J. 2013, 35, 247–258. [Google Scholar] [CrossRef] [PubMed]
- Edmonds, C.; Lockwood, G.M.; Bezjak, A.; Nyhof-Young, J. Alleviating emotional exhaustion in oncology nurses: An evaluation of wellspring’s “care for the professional caregiver program”. J. Cancer Educ. 2012, 27, 27–36. [Google Scholar] [CrossRef] [PubMed]
- Codier, E.; Kamikawa, C.; Kooker, B.M. The impact of emotional intelligence development on nurse managers. Nurs. Adm. Q. 2011, 35, 270–276. [Google Scholar] [CrossRef]
- Buruck, G.; Dörfel, D.; Kugler, J.; Brom, S.S. Enhancing well-being at work: The role of emotion regulation skills as personal resources. J. Occup. Health Psychol. 2016, 21, 480–493. [Google Scholar] [CrossRef]
- Brox, J.I.; Froøystein, O. Health-related quality of life and sickness absence in community nursing home employees: Randomized controlled trial of physical exercise. Occup. Med. (Chic. Ill) 2005, 55, 558–563. [Google Scholar] [CrossRef]
- Becker, A.; Angerer, P.; Müller, A. The prevention of musculoskeletal complaints: A randomized controlled trial on additional effects of a work-related psychosocial coaching intervention compared to physiotherapy alone. Int. Arch. Occup. Environ. Health 2017, 90, 357–371. [Google Scholar] [CrossRef]
- Bay, P.S.; Ivy, S.S.; Terry, C.L. The effect of spiritual retreat on nurses’ spirituality. Holist. Nurs. Pr. 2010, 24, 125–133. [Google Scholar] [CrossRef] [PubMed]
- Szeto, G.; Wong, T.; Law, R.; Lee, E.; Lau, T.; So, B.; Law, S. The impact of a multifaceted ergonomic intervention program on promoting occupational health in community nurses. Appl. Ergon. 2013, 44, 414–422. [Google Scholar] [CrossRef] [PubMed]
- Appel, L.; Labhart, L.; Balczo, P.; McCleary, N.; Raley, M.; Winsett, R. A comparative study of a happiness intervention in medical-surgical nurses. Medsurg Nurs. 2013, 22, 319–324. [Google Scholar] [PubMed]
- Flarity, K.; Rhodes, W.J.; Reckard, P. Intervening to improve compassion fatigue resiliency in nurse residents. J. Nurs. Educ. Pract. 2016, 6, 99–104. [Google Scholar] [CrossRef]
- Flarity, K.; Moorer, A.; Rhodes Jones, W. Longitudinal study of a compassion fatigue resiliency intervention in nurse residents. J. Nurs. Educ. Pract. 2018, 8, 61–67. [Google Scholar] [CrossRef]
- Potter, P.; Deshields, T.; Berger, J.A.; Clarke, M.; Olsen, S.; Chen, L. Evaluation of a compassion fatigue resiliency program for oncology nurses. Oncol. Nurs. Forum 2013, 40, 180–187. [Google Scholar] [CrossRef]
- Lavoie-Tremblay, M.; Sounan, C.; Trudel, J.G.; Lavigne, G.L.; Martin, K.; Lowensteyn, I. Impact of a pedometer program on nurses working in a health-promoting hospital. Health Care Manag. (Frederick) 2014, 33, 172–180. [Google Scholar] [CrossRef]
- Le Blanc, P.M.; Hox, J.J.; Schaufeli, W.B.; Taris, T.W.; Peeters, M.C.W. Take care! The evaluation of a team-based burnout intervention program for oncology care providers. J. Appl. Psychol. 2007, 92, 213–227. [Google Scholar] [CrossRef]
- Brunero, S.; Cowan, D.; Fairbrother, G. Reducing emotional distress in nurses using cognitive behavioral therapy: A preliminary program evaluation. Jpn. J. Nurs. Sci. 2008, 5, 109–115. [Google Scholar] [CrossRef]
- Moeini, B.; Hazavehei, S.M.M.; Hosseini, Z.; Aghamolaei, T.; Moghimbeigi, A. The impact of cognitive-behavioral stress management training program on job stress in hospital nurses: Applying PRECEDE model. J. Res. Health Sci. 2011, 11, 114–120. [Google Scholar]
- Wasner, M.; Longaker, C.; Fegg, M.J.; Borasio, G.D. Effects of spiritual care training for palliative care professionals. Palliat. Med. 2005, 19, 99–104. [Google Scholar] [CrossRef] [PubMed]
- Hasson, R.; Stark, A.; Constantini, N.; Polak, R.; Verbov, G.; Edelstein, N.; Lachmi, M.; Cohen, R.; Maoz, S.; Daoud, N.; et al. “Practice what you teach” Public health nurses promoting healthy lifestyles (PHeeL-PHiNe): Program evaluation. J. Ambul. Care Manag. 2018, 41, 171–180. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, T.; Mizoue, T.; Kubota, S.; Mishima, N.; Nagata, S. Relationship between burnout and communication skill training among Japanese hospital nurses: A pilot study. J. Occup. Health 2003, 45, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Sands, S.; Stanley, P.; Charon, R. Pediatric narrative oncology: Interprofessional training to promote empathy, build teams, and prevent burnout. J. Support. Oncol. 2008, 6, 307–312. [Google Scholar] [PubMed]
- Chesak, S.S.; Bhagra, A.; Schroeder, D.R.; Foy, D.A.; Cutshall, S.M.; Sood, A. Enhancing resilience among new nurses: Feasibility and efficacy of a pilot intervention. Ochsner J. 2015, 15, 38–44. [Google Scholar]
- Gollwitzer, P.M.; Mayer, D.; Frick, C.; Oettingen, G. Promoting the self-regulation of stress in health care providers: An internet-based intervention. Front. Psychol. 2018, 9, 1–11. [Google Scholar] [CrossRef]
- Slatyer, S.; Craigie, M.; Heritage, B.; Davis, S.; Rees, C. Evaluating the effectiveness of a brief mindful self-care and resiliency (MSCR) intervention for nurses: A controlled trial. Mindfulness (N. Y.) 2018, 9, 534–546. [Google Scholar] [CrossRef]
- Günüşen, N.P.; Üstün, B. An RCT of coping and support groups to reduce burnout among nurses. Int. Nurs. Rev. 2010, 57, 485–492. [Google Scholar] [CrossRef]
- Pipe, T.B.; Buchda, V.L.; Launder, S.; Hudak, B.; Hulvey, L.; Karns, K.E.; Pendergast, D. Building personal and professional resources of resilience and agility in the healthcare workplace. Stress Health 2012, 28, 11–22. [Google Scholar] [CrossRef]
- Tucker, S.J.; Lanningham-Foster, L.M.; Murphy, J.N.; Thompson, W.G.; Weymiller, A.J.; Lohse, C.; Levine, J.A. Effects of a worksite physical activity intervention for hospital nurses who are working mothers. AAOHN J. 2011, 59, 377–386. [Google Scholar] [CrossRef]
- Hrabe, D.P.; Melnyk, B.M.; Buck, J.; Sinnott, L.T. Effects of the nurse athlete program on the healthy lifestyle behaviors, physical health, and mental well-being of new graduate nurses. Nurs. Adm. Q. 2017, 41, 353–359. [Google Scholar] [CrossRef] [PubMed]
- Kozak, A.; Freitag, S.; Nienhaus, A. Evaluation of a training program to reduce stressful trunk postures in the nursing professions: A pilot study. Ann. Work Expo. Health 2017, 61, 22–32. [Google Scholar] [CrossRef] [PubMed]
- Saedpanah, D.; Salehi, S.; Moghaddam, L.F. The effect of emotion regulation training on occupational stress of critical care nurses. J. Clin. Diagn. Res. 2016, 10, VC01–VC04. [Google Scholar] [CrossRef] [PubMed]
- Sharif, F.; Rezaie, S.; Keshavarzi, S.; Mansoori, P.; Ghadakpoor, S. Teaching emotional intelligence to intensive care unit nurses and their general health: A randomized clinical trial. Int. J. Occup. Environ. Med. 2013, 4, 141–148. [Google Scholar]
- Sabzianpoor, B.; Ghazanfari Amrai, M.; Jalali Farahani, M.; Soheila, R.; Mahdavi, A.; Rahmani, S. The impact of teaching psychological welfare on marital satisfaction and self-efficacy in nurses. J. Med. Life 2015, 8, 307–312. [Google Scholar]
- Pahlevani, M.; Ebrahimi, M.; Radmehr, S.; Amini, F.; Bahraminasab, M.; Yazdani, M. Effectiveness of stress management training on the psychological well-being of the nurses. J. Med. Life 2015, 8, 313–318. [Google Scholar]
- Motamed-Jahromi, M.; Fereidouni, Z.; Dehghan, A. Effectiveness of positive thinking training program on nurses’ quality of work life through smartphone applications. Int. Sch. Res. Not. 2017, 2017, 4965816. [Google Scholar] [CrossRef]
- Ketelaar, S.M.; Nieuwenhuijsen, K.; Bolier, L.; Smeets, O.; Sluiter, J.K. Improving work functioning and mental health of health care employees using an e-mental health approach to workers’ health surveillance: Pretest-posttest study. Saf. Health Work 2014, 5, 216–221. [Google Scholar] [CrossRef]
- Yılmaz, G.; Üstün, B.; Günüşen, N.P. Effect of a nurse-led intervention programme on professional quality of life and post-traumatic growth in oncology nurses. Int. J. Nurs. Pract. 2018, 24, 1–7. [Google Scholar] [CrossRef]
- Sarid, O.; Berger, R.; Segal-Engelchin, D. The impact of cognitive behavioral interventions on SOC, perceived stress and mood states of nurses. Procedia Soc. Behav. Sci. 2010, 2, 928–932. [Google Scholar] [CrossRef]
- Kooshalshah, S.F.R.; Hidarnia, A.; Tavousi, M.; Shahmohamadi, S.; Aghdamizade, S. Effect of positive thinking intervention on the nurses’ job stress. Acta Med. Mediterr. 2015, 31, 1495–1500. [Google Scholar]
- Fillion, L.; Duval, S.; Dumont, S.; Gagnon, P.; Tremblay, I.; Bairati, I.; Breitbart, W.S. Impact of a meaning-centered intervention on job satisfaction and on quality of life among palliative care nurses. Psychooncology 2009, 18, 1300–1310. [Google Scholar] [CrossRef] [PubMed]
- Sarabia-Cobo, C.M.; Suárez, S.G.; Menéndez Crispín, E.J.; Sarabia Cobo, A.B.; Pérez, V.; de Lorena, P.; Rodríguez Rodríguez, C.; Sanlúcar Gross, L. Emotional intelligence and coping styles: An intervention in geriatric nurses. Appl. Nurs. Res. 2017, 35, 94–98. [Google Scholar] [CrossRef] [PubMed]
- Sarid, O.; Berger, R.; Eckshtein, R.; Segal-Engelchin, D. Are cognitive-behavioral interventions effective in reducing occupational stress among nurses? Appl. Nurs. Res. 2012, 25, 152–157. [Google Scholar]
- Noben, C.; Smit, F.; Nieuwenhuijsen, K.; Ketelaar, S.; Boon, B.; Sluiter, J.; Evers, S. Comparative cost-effectiveness of two interventions to promote work functioning by targeting mental health complaints among nurses: Pragmatic cluster randomised trial. Int. J. Nurs. Stud. 2014, 51, 1321–1331. [Google Scholar] [CrossRef]
- Nahm, E.S.; Warren, J.; Friedmann, E.; Brown, J.; Rouse, D.; Park, B.K.; Quigley, K.W. Implementation of a participant-centered weight management program for older nurses: A feasibility study. Online J. Issues Nurs. 2014, 19. [Google Scholar]
- Torquati, L.; Kolbe-Alexander, T.; Pavey, T.; Leveritt, M. Changing diet and physical activity in nurses: A pilot study and process evaluation highlighting challenges in workplace health promotion. J. Nutr. Educ. Behav. 2018, 50, 1015–1025. [Google Scholar] [CrossRef]
- Yuan, S.C.; Chou, M.C.; Hwu, L.J.; Chang, Y.O.; Hsu, W.H.; Kuo, H.W. An intervention program to promote health-related physical fitness in nurses. J. Clin. Nurs. 2009, 18, 1404–1411. [Google Scholar] [CrossRef]
- Tucker, S.; Farrington, M.; Lanningham-Foster, L.M.; Clark, M.K.; Dawson, C.; Quinn, G.J.; Laffoon, T.; Perkhounkova, Y. Worksite physical activity intervention for ambulatory clinic nursing staff. Work. Health Saf. 2016, 64, 313–325. [Google Scholar] [CrossRef]
- Speroni, K.G.; Earley, C.; Seibert, D.; Kassem, M.; Shorter, G.; Ware, C.C.; Kosak, E.; Atherton, M. Effect of nurses living fitTM exercise and nutrition intervention on body Mass index in nurses. J. Nurs. Adm. 2012, 42, 231–238. [Google Scholar] [CrossRef]
- Oldervoll, L.M.; Rø, M.; Zwart, J.A.; Svebak, S. Comparison of two physical exercise programs for the early intervention of pain in the neck, shoulders and lower back in female hospital staff. J. Rehabil. Med. 2001, 33, 156–161. [Google Scholar] [CrossRef] [PubMed]
- Matsugaki, R.; Kuhara, S.; Saeki, S.; Jiang, Y.; Michishita, R.; Ohta, M.; Yamato, H. Effectiveness of workplace exercise supervised by a physical therapist among nurses conducting shift work: A randomized controlled trial. J. Occup. Health 2017, 62, 477–490. [Google Scholar] [CrossRef] [PubMed]
- Koehne, K. A new threat to the nursing workforce: Take a stand! Creat. Nurs. 2015, 21, 234–241. [Google Scholar] [CrossRef] [PubMed]
- Andersen, L.L.; Brandt, M.; Poulsen, O.M.; Sundstrup, E.; Jay, K.; Clausen, T.; Borg, V.; Jakobsen, M.D.; Persson, R. Effect of physical exercise on workplace social capital: Cluster randomized controlled trial. Scand. J. Public Health 2015, 43, 810–818. [Google Scholar] [CrossRef]
- Freitas, A.R.; Carneseca, E.C.; Paiva, C.E.; Paiva, B.S.R. Impact of a physical activity program on the anxiety, depression, occupational stress and burnout syndrome of nursing professionals. Rev. Lat. Am. Enferm. 2014, 22, 332–336. [Google Scholar] [CrossRef]
- Fang, R.; Li, X. A regular yoga intervention for staff nurse sleep quality and work stress: A randomised controlled trial. J. Clin. Nurs. 2015, 24, 3374–3379. [Google Scholar] [CrossRef]
- Croteau, K.A. Using pedometers to increase the non-workday steps of hospital nursing and support staff: A pilot study. Work. Health Saf. 2016, 65, 452–456. [Google Scholar] [CrossRef]
- Chen, H.M.; Wang, H.H.; Chen, C.H.; Hu, H.M. Effectiveness of a stretching exercise program on low back pain and exercise self-efficacy among nurses in Taiwan: A randomized clinical trial. Pain Manag. Nurs. 2014, 15, 283–291. [Google Scholar] [CrossRef]
- Alexander, G.K.; Rollins, K.; Walker, D.; Wong, L.; Pennings, J. Yoga for self-care and burnout prevention among nurses. Work. Health Saf. 2015, 63, 462–470. [Google Scholar] [CrossRef]
- Ando, M.; Natsume, T.; Kukihara, H.; Shibata, H.; Ito, S. Efficacy of mindfulness-based meditation therapy on the sense of coherence and mental health of nurses. Health (Irvine. Calif) 2011, 3, 118–122. [Google Scholar] [CrossRef]
- Hess, I.; Borg, J.; Rissel, C. Workplace nutrition and physical activity promotion at Liverpool Hospital. Health Promot. J. Aust. 2011, 22, 44–50. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, J.N.; Gurgel, J.L.; da Silva, E.B.; Porto, F. Acute and chronic effect of stretching exercise on posture and flexibility of nurses and licensed practical nurses. Man. Ther. Posturology Rehabil. J. 2017, 15, 478. [Google Scholar] [CrossRef]
- Oka, H.; Nomura, T.; Asada, F.; Takano, K.; Nitta, Y.; Uchima, Y.; Sato, T.; Kawase, M.; Sawada, S.; Sakamoto, K.; et al. The effect of the ‘One Stretch’ exercise on the improvement of low back pain in Japanese nurses: A large-scale, randomised, controlled trial. Mod. Rheumatol. 2019, 29, 861–866. [Google Scholar] [CrossRef] [PubMed]
- Palumbo, M.V.; Wu, G.; Shaner-McRae, H.; Rambur, B.; McIntosh, B. Tai Chi for older nurses: A workplace wellness pilot study. Appl. Nurs. Res. 2012, 25, 54–59. [Google Scholar] [CrossRef] [PubMed]
- Reed, J.L.; Cole, C.A.; Ziss, M.C.; Tulloch, H.E.; Brunet, J.; Sherrard, H.; Reid, R.D.; Pipe, A.L. The impact of web-based feedback on physical activity and cardiovascular health of nurses working in a cardiovascular setting: A randomized trial. Front. Physiol. 2018, 9, 1–10. [Google Scholar] [CrossRef]
- Mehrabi, T.; Azadi, F.; Pahlavanzadeh, S.; Meghdadi, N. The effect of yoga on coping strategies among intensive care unit nurses. Iran. J. Nurs. Midwifery Res. 2012, 17, 421–424. [Google Scholar]
- Bazarko, D.; Cate, R.A.; Azocar, F.; Kreitzer, M.J. The impact of an innovative mindfulness-based stress reduction program on the health and well-being of nurses employed in a corporate setting. J. Workplace Behav. Health 2013, 28, 107–133. [Google Scholar] [CrossRef]
- Freimann, T.; Merisalu, E.; Pääsuke, M. Effects of a home-exercise therapy programme on cervical and lumbar range of motion among nurses with neck and lower back pain: A quasi-experimental study. BMC Sports Sci. Med. Rehabil. 2015, 7, 31–38. [Google Scholar] [CrossRef]
- Steinberg, B.B.A.; Klatt, M.; Duchemin, A.M. Feasibility of a mindfulness-based intervention for surgical intensive care unit personnel. Am. J. Crit. Care 2017, 26, 10–19. [Google Scholar] [CrossRef]
- Flanagan, J.; McCord, A.; Cheney, M.; Lundquist, D. The feasibility, safety, and efficacy of using a wireless pedometer to improve the activity level in a cohort of nurses. J. Holist. Nurs. 2017, 35, 134–141. [Google Scholar] [CrossRef]
- Patel, P.R.; Yadav, A.O. Comparison of static stretching versus eccentric training to increase flexibility of hamstring muscle in healthy hospital nurses. Indian J. Physiother. Occup. Ther. 2013, 7, 11–14. [Google Scholar] [CrossRef]
- Jakobsen, M.D.; Sundstrup, E.; Brandt, M.; Jay, K.; Aagaard, P.; Andersen, L.L. Effect of workplace-versus home-based physical exercise on musculoskeletal pain among healthcare workers: A cluster randomized controlled trial. Scand. J. Work. Environ. Health 2015, 41, 153–163. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, N.; Matsuoka, Y.; Kumachi, M.; Hamazaki, K.; Horikoshi, M.; Furukawa, T.A. Omega-3 fatty acids for a better mental state in working populations—Happy Nurse Project: A 52-week randomized controlled trial. J. Psychiatr. Res. 2018, 102, 72–80. [Google Scholar] [CrossRef] [PubMed]
- Bukowska-Durawa, A.; Haynes, C.; Luszczynska, A. Plans not needed if you have high and stable self-efficacy: Planning intervention and snack intake in the context of self-efficacy trajectories. Pol. Psychol. Bull. 2010, 41, 91–97. [Google Scholar] [CrossRef]
- Glavaš, D.; Rumboldt, M.; Rumboldt, Z. Smoking cessation with nicotine replacement therapy among health care workers: Randomized double-blind study. Croat. Med. J. 2003, 44, 219–224. [Google Scholar]
- Chalmers, K.; Bramadat, I.J.; Cantin, B.; Murnaghan, D.; Shuttleworth, E.; Scott-Findlay, S.; Tataryn, D. A smoking reduction and cessation program with registered nurses: Findings and implications for community health nursing. J. Community Health Nurs. 2001, 18, 115–134. [Google Scholar] [CrossRef]
- Kamiíşlií, S.; Öz, F. Evalution of a smoking cessation psychoeducational program for nurses. J. Addict. Nurs. 2011, 22, 117–123. [Google Scholar] [CrossRef]
- Mackenzie, C.S.; Poulin, P.A.; Seidman-Carlson, R. A brief mindfulness-based stress reduction intervention for nurses and nurse aides. Appl. Nurs. Res. 2006, 19, 105–109. [Google Scholar] [CrossRef]
- Horner, J.K.; Piercy, B.S.; Eure, L.; Woodard, E.K. A pilot study to evaluate mindfulness as a strategy to improve inpatient nurse and patient experiences. Appl. Nurs. Res. 2014, 27, 198–201. [Google Scholar] [CrossRef]
- Foureur, M.; Besley, K.; Burton, G.; Yu, N.; Crisp, J. Enhancing the resilience of nurses and midwives: Pilot of a mindfulnessbased program for increased health, sense of coherence and decreased depression, anxiety and stress. Contemp. Nurse 2013, 45, 114–125. [Google Scholar] [CrossRef]
- Geary, C.; Rosenthal, S.L. Sustained impact of MBSR on stress, well-being, and daily spiritual experiences for 1 year in academic health care employees. J. Altern. Complement. Med. 2011, 17, 939–944. [Google Scholar] [CrossRef] [PubMed]
- Gauthier, T.; Meyer, R.M.L.; Grefe, D.; Gold, J.I. An on-the-job mindfulness-based intervention for pediatric ICU nurses: A pilot. J. Pediatr. Nurs. 2015, 30, 402–409. [Google Scholar] [CrossRef] [PubMed]
- Duarte, J.; Pinto-Gouveia, J. Effectiveness of a mindfulness-based intervention on oncology nurses’ burnout and compassion fatigue symptoms: A non-randomized study. Int. J. Nurs. Stud. 2016, 64, 98–107. [Google Scholar] [CrossRef]
- Pipe, T.B.; Bortz, J.J.; Dueck, A.; Pendergast, D.; Buchda, V.; Summers, J. Nurse leader mindfulness meditation program for stress management: A randomized controlled trial. J. Nurs. Adm. 2009, 39, 130–137. [Google Scholar] [CrossRef] [PubMed]
- Poulin, P.A.; Mackenzie, C.S.; Soloway, G.; Karayolas, E. Mindfulness training as an evidenced-based approach to reducing stress and promoting well-being among human services professionals. Int. J. Heal. Promot. Educ. 2008, 46, 72–80. [Google Scholar] [CrossRef]
- Ceravolo, D.; Raines, D.A. The impact of a mindfulness intervention for nurse managers. J. Holist. Nurs. 2019, 37, 47–55. [Google Scholar] [CrossRef]
- Delaney, M.C. Caring for the caregivers: Evaluation of the effect of an eight-week pilot mindful self-compassion (MSC) training program on nurses’ compassion fatigue and resilience. PLoS ONE 2018, 13, 1–20. [Google Scholar] [CrossRef]
- Mahon, M.A.; Mee, L.; Brett, D.; Dowling, M. Nurses’ perceived stress and compassion following a mindfulness meditation and self compassion training. J. Res. Nurs. 2017, 22, 572–583. [Google Scholar] [CrossRef]
- Moody, K.; Kramer, D.; Santizo, R.O.; Magro, L.; Wyshogrod, D.; Ambrosio, J.; Castillo, C.; Lieberman, R.; Stein, J. Helping the helpers: Mindfulness training for burnout in pediatric oncology-A pilot program. J. Pediatr. Oncol. Nurs. 2013, 30, 275–284. [Google Scholar] [CrossRef]
- Lan, H.K.; Subramanian, P.; Rahmat, N.; Kar, P.C. The effects of mindfulness training program on reducing stress and promoting well-being amongnurses in critical care units. Aust. J. Adv. Nurs. 2014, 31, 22–31. [Google Scholar]
- Yang, J.; Tang, S.; Zhou, W. Effect of mindfulness-based stress reduction therapy on work stress and mental health of psychiatric nurses. Psychiatr. Danub. 2018, 30, 189–196. [Google Scholar] [CrossRef] [PubMed]
- Morrison Wylde, C.; Mahrer, N.E.; Meyer, R.M.L.; Gold, J.I. Mindfulness for novice pediatric nurses: Smartphone application versus traditional intervention. J. Pediatr. Nurs. 2017, 36, 205–212. [Google Scholar] [CrossRef] [PubMed]
- Martín-Asuero, A.; García-Banda, G. The mindfulness-based stress reduction program (MBSR) reduces stress-related psychological distress in healthcare professionals. Span. J. Psychol. 2010, 13, 897–905. [Google Scholar] [CrossRef] [PubMed]
- Sallon, S.; Katz-Eisner, D.; Yaffe, H.; Bdolah-Abram, T. Caring for the caregivers: Results of an extended, five-component stress-reduction intervention for hospital staff. Behav. Med. 2017, 43, 47–60. [Google Scholar] [CrossRef] [PubMed]
- Oman, D.; Hedberg, J.; Thoresen, C.E. Passage meditation reduces perceived stress in health professionals: A randomized, controlled trial. J. Consult. Clin. Psychol. 2006, 74, 714–719. [Google Scholar] [CrossRef] [PubMed]
- Hevezi, J.A. Evaluation of a meditation intervention to reduce the effects of stressors associated with compassion fatigue mmong nurses. J. Holist. Nurs. 2016, 34, 343–350. [Google Scholar] [CrossRef]
- Dyess, S.M.L.; Prestia, A.S.; Marquit, D.E.; Newman, D. Self-care for nurse leaders in acute care environment reduces perceived stress: A mixed-methods pilot study merits further investigation. J. Holist. Nurs. 2018, 36, 79–90. [Google Scholar] [CrossRef]
- Cutshall, S.M.; Wentworth, L.J.; Wahner-Roedler, D.L.; Vincent, A.; Schmidt, J.E.; Loehrer, L.L.; Cha, S.S.; Bauer, B.A. Evaluation of a biofeedback-assisted meditation program as a stress management tool for hospital nurses: A pilot study. Explore 2011, 7, 110–112. [Google Scholar] [CrossRef]
- Lin, L.; He, G.; Yan, J.; Gu, C.; Xie, J. The Effects of a Modified Mindfulness-Based Stress Reduction Program for Nurses: A Randomized Controlled Trial. Work. Health Saf. 2018, 67, 111–122. [Google Scholar] [CrossRef]
- Oman, D.; Thoresen, C.E.; Hedberg, J. Does passage meditation foster compassionate love among health professionals?: A randomised trial. Ment. Health Relig. Cult. 2010, 13, 129–154. [Google Scholar] [CrossRef]
- Lai, H.L.; Li, Y.M. The effect of music on biochemical markers and self-perceived stress among first-line nurses: A randomized controlled crossover trial. J. Adv. Nurs. 2011, 67, 2414–2424. [Google Scholar] [CrossRef] [PubMed]
- Karpavičiūtė, S.; Macijauskienė, J. The impact of arts activity on nursing staff well-being: An intervention in the workplace. Int. J. Environ. Res. Public Health 2016, 13, 435. [Google Scholar] [CrossRef] [PubMed]
- Bost, N.; Wallis, M. The effectiveness of a 15 minute weekly massage in reducing physical and psychological stress in nurses. Aust. J. Adv. Nurs. 2006, 23, 28–33. [Google Scholar] [PubMed]
- Brennan, M.K.; DeBate, R.D. The effect of chair massage on stress perception of hospital bedside nurses. J. Bodyw. Mov. Ther. 2006, 10, 335–342. [Google Scholar] [CrossRef]
- Cooke, M.; Holzhauser, K.; Jones, M.; Davis, C.; Finucane, J. The effect of aromatherapy massage with music on the stress and anxiety levels of emergency nurses: Comparison between summer and winter. J. Clin. Nurs. 2007, 16, 1695–1703. [Google Scholar] [CrossRef]
- Onishi, K.; Tsujikawa, M.; Inoue, K.; Yoshida, K.; Goto, S. The effect of complementary therapy for hospital nurses with high stress. Asia Pac. J. Oncol. Nurs. 2016, 3, 272–280. [Google Scholar] [CrossRef]
- Chang, Y.Y.; Lin, C.L.; Chang, L.Y. The effects of aromatherapy massage on sleep quality of nurses on monthly rotating night shifts. Evid. Based Complement. Altern. Med. 2017, 2017, 3861273. [Google Scholar] [CrossRef]
- Sajadi, M.; Goudarzi, K.; Khosravi, S.; Farmahini-Farahani, M.; Mohammadbeig, A. Benson’s relaxation effect in comparing to systematic desensitization on anxiety of female nurses: A randomized clinical trial. Indian J. Med. Paediatr. Oncol. 2017, 38, 111–115. [Google Scholar]
- Nazari, F.; Mirzamohamadi, M.; Yousefi, H. The effect of massage therapy on occupational stress of Intensive Care Unit nurses. Iran. J. Nurs. Midwifery Res. 2015, 20, 508–515. [Google Scholar]
- Ploukou, S.; Panagopoulou, E. Playing music improves well-being of oncology nurses. Appl. Nurs. Res. 2018, 39, 77–80. [Google Scholar] [CrossRef]
- Lee, K.A.; Gay, C.L.; Alsten, C.R. Home-based behavioral sleep training for shift workers: A pilot study. Behav. Sleep Med. 2014, 12, 455–468. [Google Scholar] [CrossRef] [PubMed]
- Villani, D.; Grassi, A.; Cognetta, C.; Toniolo, D.; Cipresso, P.; Riva, G. Self-help stress management training through mobile phones: An experience with oncology nurses. Psychol. Serv. 2013, 10, 315–322. [Google Scholar] [CrossRef] [PubMed]
- Hilliard, R.E. The effect of music therapy sessions on compassion fatigue and team building of professional hospice caregivers. Arts Psychother. 2006, 33, 395–401. [Google Scholar] [CrossRef]
- Anderson, L.W.; Gustavson, C.U. The impact of a knitting intervention on compassion fatigue in oncology nurses. Clin. J. Oncol. Nurs. 2016, 20, 102–104. [Google Scholar] [CrossRef] [PubMed]
- Cuneo, C.L.; Curtis Cooper, M.R.; Drew, C.S.; Naoum-Heffernan, C.; Sherman, T.; Walz, K.; Weinberg, J. The effect of Reiki on work-related stress of the registered nurse. J. Holist. Nurs. 2011, 29, 33–43. [Google Scholar] [CrossRef] [PubMed]
- McElligott, D.; Holz, M.B.; Carollo, L.; Somerville, S.; Baggett, M.; Kuzniewski, S.; Shi, Q. A pilot feasibility study of the effects of touch therapy on nurses. J. N. Y. State Nurses Assoc. 2003, 34, 16–24. [Google Scholar]
- Kurebayashi, L.F.S.; Da Silva, M.J.P. Efficacy of Chinese auriculotherapy for stress in nursing staff. Rev. Lat. Am. Enferm. 2014, 22, 371–378. [Google Scholar] [CrossRef]
- Kurebayashi, L.F.S.; Gnatta, J.R.; Borges, T.P.; da Silva, M.J.P. Applicability of auriculotherapy in reducing stress and as a coping strategy in nursing professionals. Rev. Lat. Am. Enferm. 2012, 20, 980–987. [Google Scholar] [CrossRef]
- do Prado, J.M.; Kurebayashi, L.F.S.; da Silva, M.J.P. Experimental and placebo auriculotherapy for stressed nurses: Randomized controlled trial. Rev. Da Esc. Enferm. 2018, 52, 1–8. [Google Scholar]
- Leppämäki, S.; Partonen, T.; Piiroinen, P.; Haukka, J.; Lönnqvist, J. Timed bright-light exposure and complaints related to shift work among women. Scand. J. Work. Environ. Health 2003, 29, 22–26. [Google Scholar] [CrossRef]
- Bormann, J.E.; Becker, S.; Gershwin, M.; Kelly, A.; Pada, L.; Smith, T.L.; Gifford, A.L. Relationship of frequent mantram repetition to emotional and spiritual well-being in healthcare workers. J. Contin. Educ. Nurs. 2006, 37, 218–224. [Google Scholar] [CrossRef] [PubMed]
- HemmatiMaslakpak, M.; Farhadi, M.; Fereidoni, J. The effect of neuro-linguistic programming on occupational stress in critical care nurses. Iran. J. Nurs. Midwifery Res. 2016, 21, 38. [Google Scholar] [CrossRef] [PubMed]
- Murphy, G.T.; Stewart, M.; Ritchie, J.; Viscount, P.W.; Johnson, A. Telephone support for Canadian nurses in HIV/AIDS care. J. Assoc. Nurses AIDS Care 2000, 11, 73–88. [Google Scholar] [CrossRef]
- Gärtner, F.R.; Nieuwenhuijsen, K.; Ketelaar, S.M.; Van Dijk, F.J.H.; Sluiter, J.K. The mental vitality @ Work Study: Effectiveness of a mental module for workers’ health surveillance for nurses and allied health care professionals on their help-seeking behaviour. J. Occup. Environ. Med. 2013, 55, 1219–1229. [Google Scholar] [CrossRef] [PubMed]
- Pett, M. Nonparametric Statistics for Health Care Research: Statistics for Small Samples and Unusual Distributions; Sage Publications, Inc.: London, UK, 1997. [Google Scholar]
- Salkind, N. Statistics For. People Who (Think They) Hate Statistics, 2nd ed.; SAGE Publications, Inc.: London, UK, 2019. [Google Scholar]
- Des Jarlais, D.C.; Lyles, C.; Crepaz, N. Improving the reporting quality of nonrandomized evaluations of behavioral and public health interventions: The TREND statement. Am. J. Public Health 2004, 94, 361–366. [Google Scholar] [CrossRef] [PubMed]
- Mhurchu, C.N.; Aston, L.; Jebb, S.A. Effects of worksite health promotioninterventions on employee diets: A systematic review. BMC Public Health 2010, 10, 62. [Google Scholar] [CrossRef]
- Cherry, M.G.; Brown, J.M.; Bethell, G.S.; Neal, T.; Shaw, N.J. Features of educational interventions that lead to compliance with hand hygiene in healthcare professionals within a hospital care setting. A BEME systematic review: BEME Guide No. 22. Med. Teach. 2012, 34, e406–e420. [Google Scholar] [CrossRef][Green Version]
- Gaither, C.A.; Kahaleh, A.A.; Doucette, W.R.; Mott, D.A.; Pederson, C.A.; Schommer, J.C. A modified model of pharmacists’ job stress: The role of organizational, extra-role, and individual factors on work-related outcomes. Res. Soc. Adm. Pharm. 2008, 4, 231–243. [Google Scholar] [CrossRef]
- Spence Laschinger, H.K.; Grau, A.; Finegan, J.; Wilk, P. Predictors of new graduate nurses’ workplace well-being: Testing the job demands-resources model. Health Care Manage. Rev. 2012, 37, 175–186. [Google Scholar] [CrossRef]
- Davidson, R.J.; Kaszniak, A.W. Conceptual and methodological issues in research on mindfulness and meditation. Am. Psychol. 2015, 70, 581–592. [Google Scholar] [CrossRef]
- Jamieson, S.D.; Tuckey, M.R. Mindfulness interventions in the workplace: A critique of the current state of the literature. J. Occup. Health Psychol. 2017, 22, 180. [Google Scholar] [CrossRef] [PubMed]
- Crane, R.S.; Hecht, F.M. Intervention integrity in mindfulness-based research. Mindfulness (N. Y.) 2018, 9, 1370–1380. [Google Scholar] [CrossRef] [PubMed]
- Slatten, L.A.D.; David Carson, K.; Carson, P.P. Compassion fatigue and burnout: What managers should know. Health Care Manag. (Frederick) 2011, 30, 325–333. [Google Scholar] [CrossRef] [PubMed]
- Awa, W.L.; Plaumann, M.; Walter, U. Burnout prevention: A review of intervention programs. Patient Educ. Couns. 2010, 78, 184–190. [Google Scholar] [CrossRef] [PubMed]
- McLeod, J. The effectiveness of workplace counselling: A systematic review. Couns. Psychother. Res. 2010, 10, 238–248. [Google Scholar] [CrossRef]
- LaMontagne, A.D.; Martin, A.; Page, K.M.; Reavley, N.J.; Noblet, A.J.; Milner, A.J.; Keegel, T.; Smith, P.M. Workplace mental health: Developing an integrated intervention approach. BMC Psychiatry 2014, 14, 1–11. [Google Scholar] [CrossRef]
- Fitzpatrick, R.; Fletcher, A.; Gore, S.; Jones, D.; Spiegelhalter, D.; Cox, D. Quality oflife measures in health care. I: Applications and issues in assessment. BMJ 1992, 305, 1074–1077. [Google Scholar] [CrossRef]
- Su, J.A.; Weng, H.H.; Tsang, H.Y.; Wu, J.L. Mental health and quality of life among doctors, nurses and other hospital staff. Stress Health 2009, 25, 423–430. [Google Scholar] [CrossRef]
- Shao, M.-F.; Chou, Y.C.; Yeh, M.Y.; Tzeng, W.C. Sleep quality and quality of life in female shift-working nurses. J. Adv. Nurs. 2010, 66, 1565–1572. [Google Scholar] [CrossRef]
- Anderson, K.L.; Burckhardt, C.S. Conceptualization and measurement of quality of life as an outcome variable for health care intervention and research. J. Adv. Nurs. 1999, 29, 298–306. [Google Scholar] [CrossRef]
- Bray, J.; Johns, N.; Kilburn, D. An exploratory study into the factors impeding ethical consumption. J. Bus. Ethicd 2011, 98, 597–608. [Google Scholar] [CrossRef]
- Carrington, M.; Neville, B.; Whitewell, G. Why ethical consumers don’t walk their talk: Towards a framework for understanding the gap between ethical purchase intentions and actual buying behaviour of ethically minded consumers. J. Bus. Ethics 2010, 97, 139–158. [Google Scholar] [CrossRef]
- Chatzidakis, A.; Hibbert, S.; Smith, A. Why people don’t take their concerns about fair trade to the supermarket: The role of neutralisation. J. Bus. Ethics 2007, 74, 89–100. [Google Scholar] [CrossRef]
- De Pelsmaker, P.; Driesen, L.; Rayp, G. Do consumers care abour ethics? Willingness to pay for fair-trade coffee. J. Consum. Aff. 2005, 39, 363–385. [Google Scholar] [CrossRef]
- Gardner, B.; Lally, P.; Wardle, J. Making health habitual: The psychology of “habit-formation” and general practice. Br. J. Gen. Pract. 2012, 62, 664–666. [Google Scholar] [CrossRef]
- Lally, P.; Van Jaarsveld, C.H.; Potts, H.W.; Wardle, J. How are habits formed: Modelling habit formation in the real world. Eur. J. Soc. Psychol. 2010, 40, 998–1009. [Google Scholar] [CrossRef]
| Search Term 1–10 | Search Term 11–20 | Search Term 21–30 | Search Term 31–40 | Search Term 41–44 |
|---|---|---|---|---|
| Physical Activity/ | alcohol drinking or alcohol consum*. af | (hypertension or diabetes or coronary or renal failure or kidney failure or liver failure or cancer). af | mental health or mental illness or psychological or psychological wellbeing or stress or anxiety or burnout or depression or self-efficacy or self ADJ efficacy | (nurs$ not in-patient$ not inpatient$ not patient$).af. |
| Exercise/ | 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 | 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 | 23 or 24 or 25 or 26 or 27 or 28 or 29 or 31 | 12 or 22 or 32 or 39 |
| (physical activity or exercise). af | Hypertension/ | Mental Health/ | Absenteeism/ | 40 and 41 and 42 |
| Diet/ | Diabetes Mellitus, Type 2/ | Stress Disorders, Traumatic, Acute/ | Job Satisfaction/ | limit 43 to (human and English language) and yr = “2000-Current” |
| Obesity/ | Acute Coronary Syndrome/ | Anxiety/ | Work Engagement/ | |
| (diet or obesity or weight).af | Acute Kidney Injury/ | Burnout, Professional/ | Work Performance/ | |
| Smoking/ | Liver Failure/ | Compassion Fatigue/ | Patient Safety/ | |
| Smoking Cessation/ | Liver Failure, Acute/ | Depression/ | sicknessabsen* or absen* or job satisfaction or employee engagement or work performance or staff retention or staff turnover or patient safety or quality of care or patient care.af | |
| (smok*or cigarette$ or nicotine or tobacco).af | Peripheral Vascular Diseases/ | Depressive Disorder/ | 33 or 34 or 35 or 36 or 37 or 38 | |
| Alcohol Drinking/ | Cerebrovascular Disorders/ | Self-Efficacy/ | (intervention or lifestyle or behavior* or behavior* change intervention* or behavior* change technique*).af. |
| Outcome | No. of Studies Reporting Improvement | No. of Studies Reporting the Outcome | Success Rate (% Reporting at Least Some Improvement) | No. of RCTs | |
|---|---|---|---|---|---|
| RCT+ | RCT− | ||||
| Diet and nutrition | 8 | 9 | 88.9 | 2 | 0 |
| Body composition | 20 | 24 | 83.3 | 10 | 0 |
| PA | 11 | 14 | 78.6 | 3 | 1 |
| Stress and coping | 49 | 66 | 74.2 | 16 | 6 |
| Smoking cessation | 2 | 3 | 66.7 | 0 | 0 |
| Self-efficacy | 2 | 3 | 66.7 | 2 | 1 |
| Health and physical symptoms | 11 | 17 | 64.7 | 4 | 3 |
| Wellbeing and QoL | 14 | 23 | 60.9 | 5 | 6 |
| Burnout/CF | 21 | 35 | 60.0 | 4 | 4 |
| Depression and Anxiety | 19 | 32 | 59.4 | 10 | 6 |
| Mindfulness | 5 | 9 | 55.6 | 1 | 1 |
| Work-related | 16 | 32 | 50.0 | 8 | 9 |
| Type of Intervention | No. of Studies | Improvements | No Effect | Comments |
|---|---|---|---|---|
| Education | 15 | Physical health [100], Emotional intelligence [100], Self-efficacy [58,101], Correct body posture [58], Stress [55,92], Spirituality [77], Gratitude [79], Work engagement [92], Emotional exhaustion [54,65,94], Depersonalisation [54,65], Personal achievement [65], Mental health knowledge [65], Marital satisfaction [101], Perception of work benefits [108] | Work functioning [111], Work ability [57], Work limitations [55], Mental health [57], Job control [57], Quality of life [108], Mood [59], Happiness [79], Job satisfaction [55,108], Coping [55], Resilience [91], Anxiety [91], Stress [91], Mindfulness [91], Depersonalisation [94], Personal achievement [54,94] | 4 studies with no significant improvements in any result [57,59,91,111]; 1 reported increase in stress [59] |
| PA | 10 | Depressive symptoms [118], Muscle strength [118], Muscle flexibility [128,130], Metabolic indicators [118], Blood pressure [131], Work stress [122], Sleep quality [122], Pain [124,129], Exercise self-efficacy [124], Work social capital [120], Work ability [130], Mindfulness [125], Self-care [125], EE and DP [125], Body fat [131], PA [115], BMI [115] | Aerobic fitness [118], BMI [131], Waist size [131], Personal achievement [125], Physical health (incl. cardiovascular health) [129,130], Pain chronicity [129], Wellbeing [130], Work stress [130], General stress [130]; Work productivity [115] | |
| Relaxation | 8 | Stress [167,170,172,175], Heart rate [167], Blood pressure [167], Cortisol level [167], Anxiety [169,174,176], Depression [176], Mood [172], Psychosomatic symptoms [176], Sleep quality [173] | Blood pressure [169,172], Cortisol level [169] | 6 studies reported only positive changes [167,170,173,174,175,176] |
| Meditation/mindfulness | 6 | Stress [150,157,161,165], Depression [157], Anxiety [157], Affect [165], Resilience [165], Wellbeing [161], Physical symptoms [157], Altruism and Perspective taking [166] | Job satisfaction [161,165], Burnout [155,161], Depression [155], Stress [155], Personal distress [166], Caring efficacy [150], Vitality [161] | 1 study reported no positive changes [155] |
| Diet | 2 | Depressive symptoms [139], Insomnia [139], Presenteeism [139], Snack intake [140] | Anxiety [139], Burnout [139] | |
| Smoking | 1 | Abstinence rate [141] | Short-term only | |
| Alternative | 5 | Stress [183,184,185], Work functioning [190], Mental health [183], Coping [184] | Distress [190], Depressive symptoms [190], Anxiety [190], Need for recovery after work [190] | 1 study [182] reported improvements in anxiety, relaxation, and physiological state; but the same was true for mock intervention |
| Complex | 7 | Depressive symptoms [60], Anxiety [178], Pain [138], Coping skills [178], Muscle strength [138], Musculoskeletal complaints [75], PA [75], Work ability [76], Work wellbeing [76], Work satisfaction [135], Quality of life [62] | Aerobic fitness [75], Quality of life [75], Life satisfaction [135], Health complains [75], Muscle strength [75], Anxiety [62], Depressive symptoms [62], Stress [135], Work ability [62], Job control [62], Work absence [75,135] | 3 studies reported only positive changes [60,138,178] |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stanulewicz, N.; Knox, E.; Narayanasamy, M.; Shivji, N.; Khunti, K.; Blake, H. Effectiveness of Lifestyle Health Promotion Interventions for Nurses: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 17. https://doi.org/10.3390/ijerph17010017
Stanulewicz N, Knox E, Narayanasamy M, Shivji N, Khunti K, Blake H. Effectiveness of Lifestyle Health Promotion Interventions for Nurses: A Systematic Review. International Journal of Environmental Research and Public Health. 2020; 17(1):17. https://doi.org/10.3390/ijerph17010017
Chicago/Turabian StyleStanulewicz, Natalia, Emily Knox, Melanie Narayanasamy, Noureen Shivji, Kamlesh Khunti, and Holly Blake. 2020. "Effectiveness of Lifestyle Health Promotion Interventions for Nurses: A Systematic Review" International Journal of Environmental Research and Public Health 17, no. 1: 17. https://doi.org/10.3390/ijerph17010017
APA StyleStanulewicz, N., Knox, E., Narayanasamy, M., Shivji, N., Khunti, K., & Blake, H. (2020). Effectiveness of Lifestyle Health Promotion Interventions for Nurses: A Systematic Review. International Journal of Environmental Research and Public Health, 17(1), 17. https://doi.org/10.3390/ijerph17010017







