Anti-Angiogenic Property of Free Human Oligosaccharides
Abstract
:1. Introduction
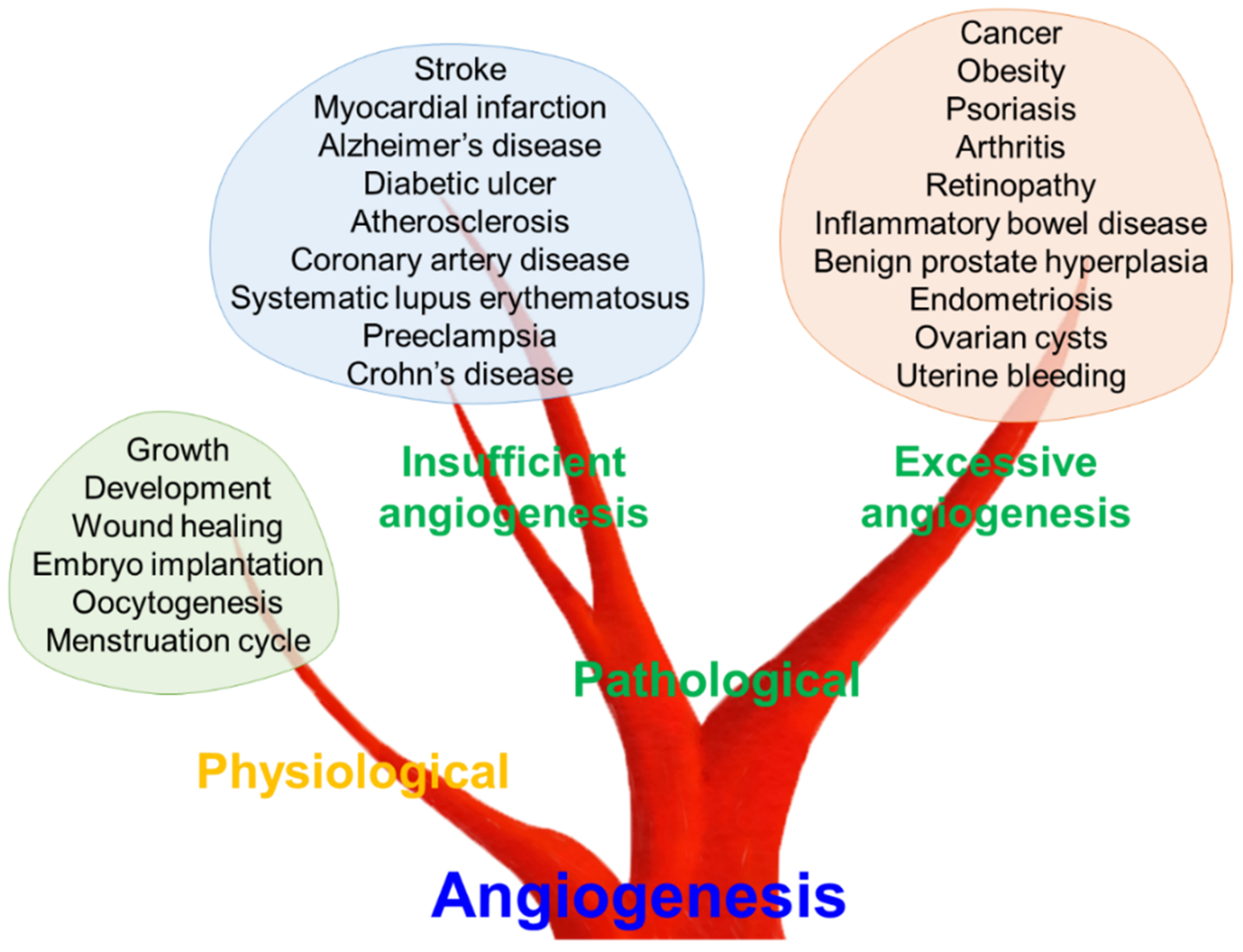
2. Angiogenesis in Human Health and Disease
2.1. Physiological and Pathological Angiogenesis
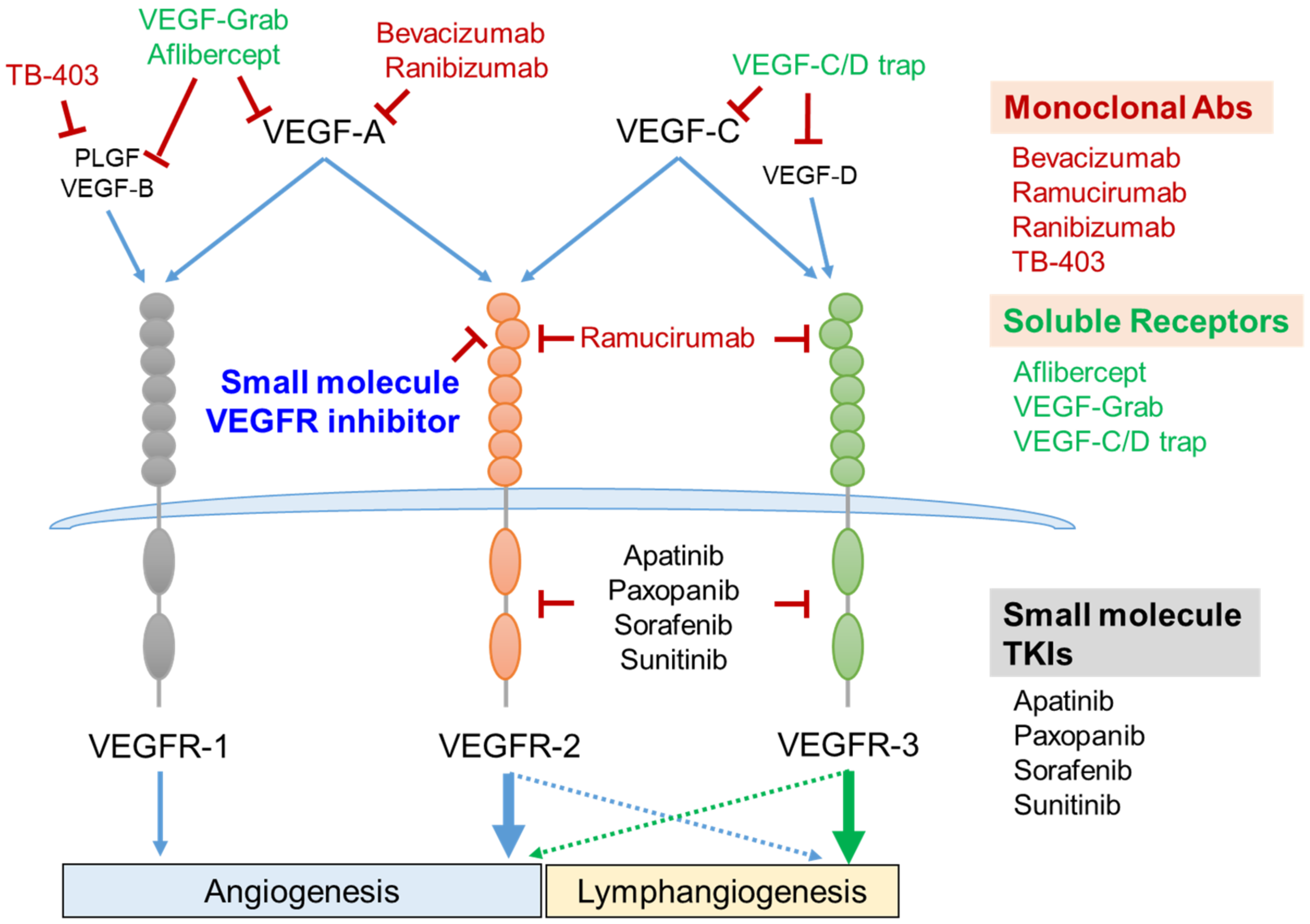
2.2. Vascular Endothelial Cell Growth Factors (VEGFs) and Their Receptors (VEGFRs) as Therapeutic Targets for Pathological Angiogenesis
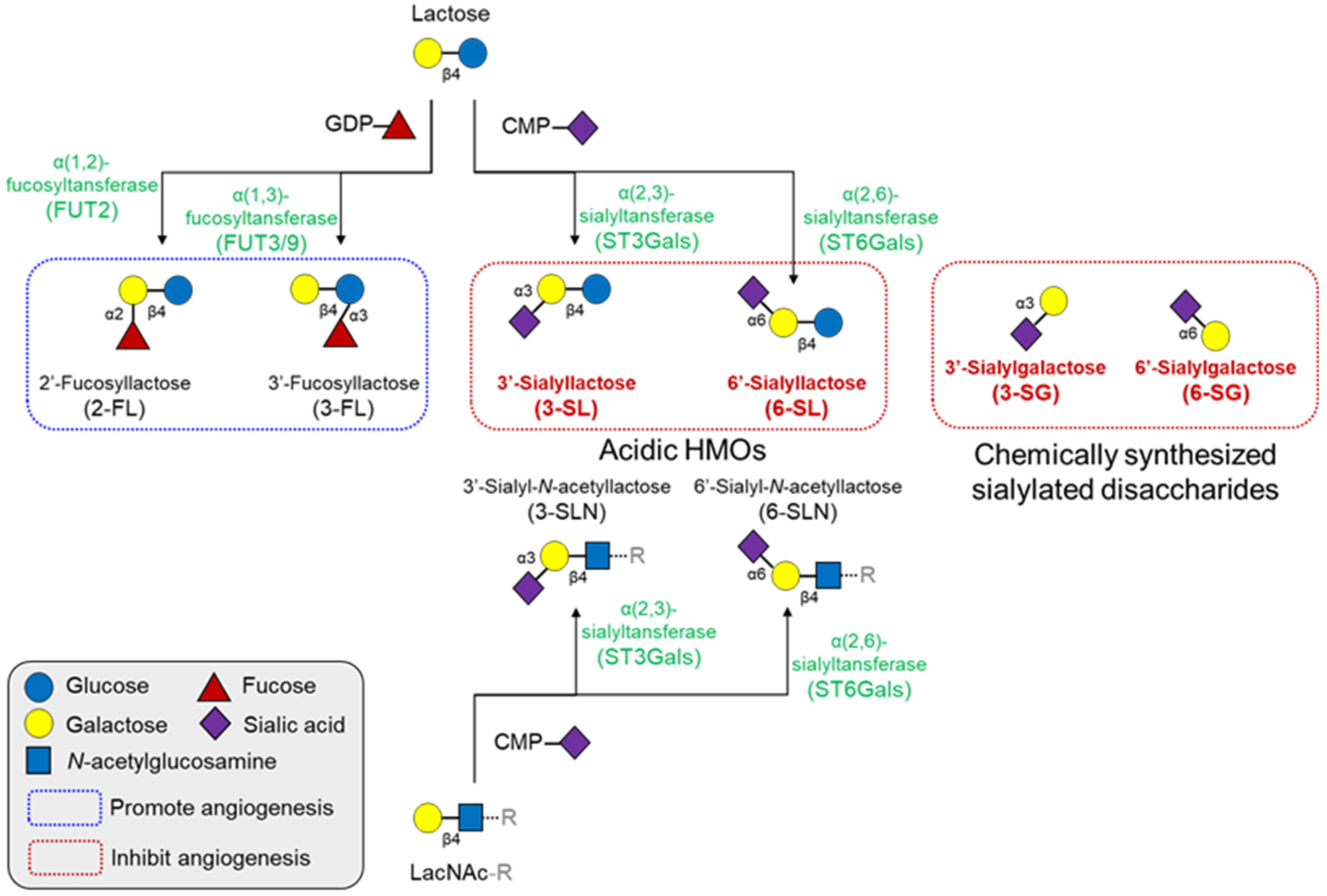
3. Human Milk Oligosaccharides and Angiogenesis
3.1. Oligosaccharides and Angiogenesis
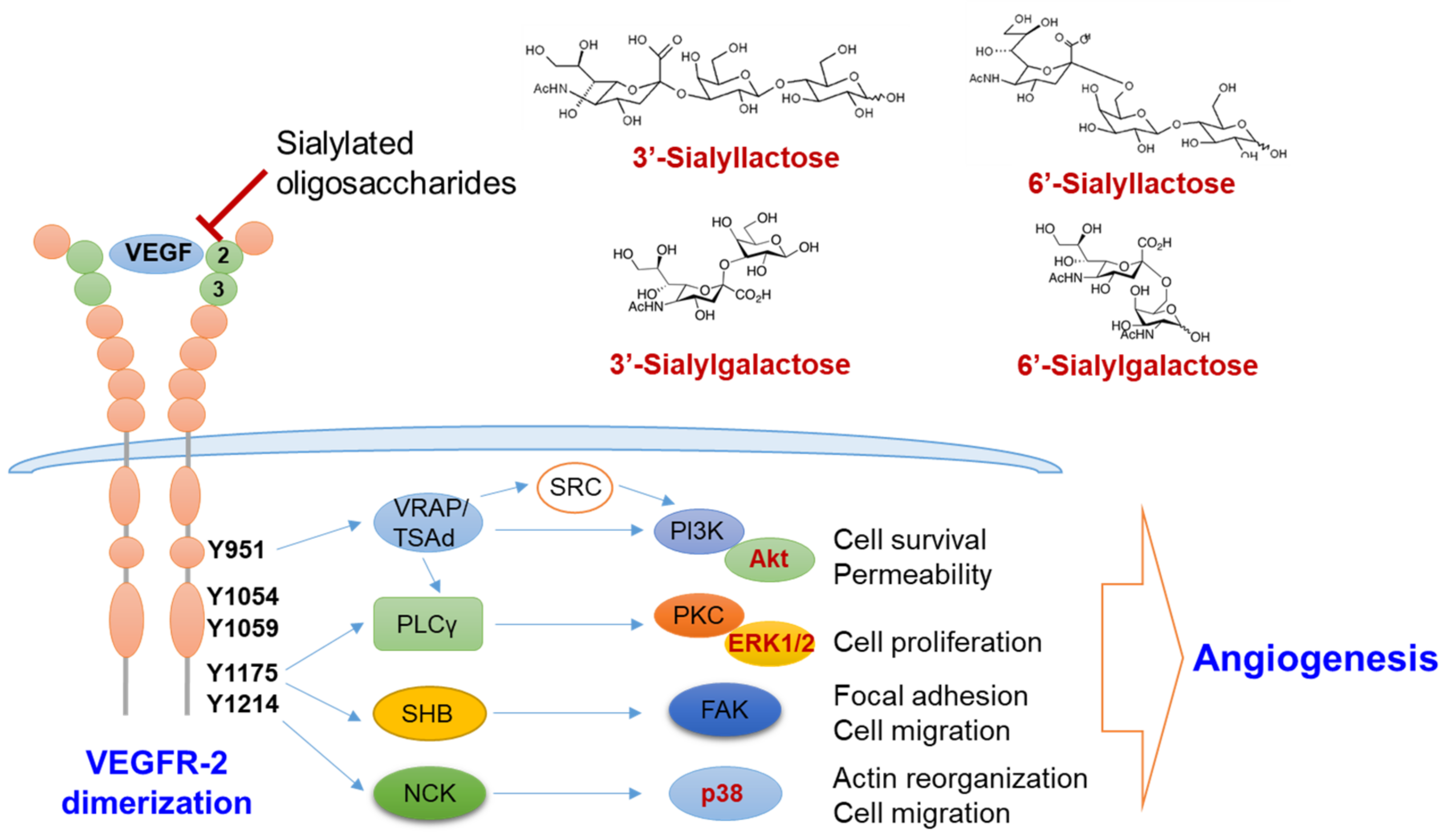
3.2. Roles of Sialylated HMOs in Pathologic Angiogenesis
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hill, D.R.; Newburg, D.S. Clinical applications of bioactive milk components. Nutr. Rev. 2015, 73, 463–476. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ballard, O.; Morrow, A.L. Human milk composition: Nutrients and bioactive factors. Pediatr. Clin. N. Am. 2013, 60, 49–74. [Google Scholar] [CrossRef] [Green Version]
- Andreas, N.J.; Kampmann, B.; Mehring Le-Doare, K. Human breast milk: A review on its composition and bioactivity. Early Hum. Dev. 2015, 91, 629–635. [Google Scholar] [CrossRef] [PubMed]
- Bode, L. Human milk oligosaccharides: Every baby needs a sugar mama. Glycobiology 2012, 22, 1147–1162. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thurl, S.; Munzert, M.; Boehm, G.; Matthews, C.; Stahl, B. Systematic review of the concentrations of oligosaccharides in human milk. Nutr. Rev. 2017, 75, 920–933. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smilowitz, J.T.; Lebrilla, C.B.; Mills, D.A.; German, J.B.; Freeman, S.L. Breast milk oligosaccharides: Structure-function relationships in the neonate. Annu. Rev. Nutr. 2014, 34, 143–169. [Google Scholar] [CrossRef] [Green Version]
- Westerbeek, E.A.; Hensgens, R.L.; Mihatsch, W.A.; Boehm, G.; Lafeber, H.N.; van Elburg, R.M. The effect of neutral and acidic oligosaccharides on stool viscosity, stool frequency and stool ph in preterm infants. Acta Paediatr. 2011, 100, 1426–1431. [Google Scholar] [CrossRef] [PubMed]
- Westerbeek, E.A.; Morch, E.; Lafeber, H.N.; Fetter, W.P.; Twisk, J.W.; Van Elburg, R.M. Effect of neutral and acidic oligosaccharides on fecal il-8 and fecal calprotectin in preterm infants. Pediatr. Res. 2011, 69, 255–258. [Google Scholar] [CrossRef] [Green Version]
- Shimada, I.; Shoji, M.; Futatsuya, R.; Katoh, T.; Kominato, Y.; Sakamoto, T.; Fujikura, T. Elevation of ratio of urinary n-acetylneuraminlactose to free sialic acid in some advanced cancer patients. J. Gastroenterol. 1995, 30, 21–27. [Google Scholar] [CrossRef]
- Ekman, B.; Wahlberg, J.; Landberg, E. Urine oligosaccharide pattern in patients with hyperprolactinaemia. Glycoconj. J. 2015, 32, 635–641. [Google Scholar] [CrossRef]
- Fu, D.; Zopf, D. Analysis of sialyllactoses in blood and urine by high-performance liquid chromatography. Anal. Biochem. 1999, 269, 113–123. [Google Scholar] [CrossRef] [PubMed]
- Bode, L.; Kunz, C.; Muhly-Reinholz, M.; Mayer, K.; Seeger, W.; Rudloff, S. Inhibition of monocyte, lymphocyte, and neutrophil adhesion to endothelial cells by human milk oligosaccharides. Thromb. Haemost. 2004, 92, 1402–1410. [Google Scholar] [CrossRef] [PubMed]
- Idota, T.; Kawakami, H.; Murakami, Y.; Sugawara, M. Inhibition of cholera toxin by human milk fractions and sialyllactose. Biosci. Biotechnol. Biochem. 1995, 59, 417–419. [Google Scholar] [CrossRef] [PubMed]
- Matsubara, T.; Sumi, M.; Kubota, H.; Taki, T.; Okahata, Y.; Sato, T. Inhibition of influenza virus infections by sialylgalactose-binding peptides selected from a phage library. J. Med. Chem. 2009, 52, 4247–4256. [Google Scholar] [CrossRef]
- Wang, B. Sialic acid is an essential nutrient for brain development and cognition. Annu. Rev. Nutr. 2009, 29, 177–222. [Google Scholar] [CrossRef]
- Wang, B. Molecular mechanism underlying sialic acid as an essential nutrient for brain development and cognition. Adv. Nutr. 2012, 3, 465S–472S. [Google Scholar] [CrossRef] [Green Version]
- Potente, M.; Makinen, T. Vascular heterogeneity and specialization in development and disease. Nat. Rev. Mol. Cell Biol. 2017, 18, 477–494. [Google Scholar] [CrossRef]
- Monahan-Earley, R.; Dvorak, A.M.; Aird, W.C. Evolutionary origins of the blood vascular system and endothelium. J. Thromb. Haemost. 2013, 11 (Suppl. 1), 46–66. [Google Scholar] [CrossRef] [Green Version]
- Flamme, I.; Frolich, T.; Risau, W. Molecular mechanisms of vasculogenesis and embryonic angiogenesis. J. Cell Physiol. 1997, 173, 206–210. [Google Scholar] [CrossRef]
- Bikfalvi, A. History and conceptual developments in vascular biology and angiogenesis research: A personal view. Angiogenesis 2017, 20, 463–478. [Google Scholar] [CrossRef]
- Fraser, H.M.; Lunn, S.F. Angiogenesis and its control in the female reproductive system. Br. Med. Bull. 2000, 56, 787–797. [Google Scholar] [CrossRef] [Green Version]
- Potente, M.; Gerhardt, H.; Carmeliet, P. Basic and therapeutic aspects of angiogenesis. Cell 2011, 146, 873–887. [Google Scholar] [CrossRef] [Green Version]
- Ferrara, N.; Kerbel, R.S. Angiogenesis as a therapeutic target. Nature 2005, 438, 967–974. [Google Scholar] [CrossRef]
- Folkman, J. Tumor angiogenesis: Therapeutic implications. N. Engl. J. Med. 1971, 285, 1182–1186. [Google Scholar]
- Chung, A.S.; Ferrara, N. Developmental and pathological angiogenesis. Annu. Rev. Cell Dev. Biol. 2011, 27, 563–584. [Google Scholar] [CrossRef]
- Carmeliet, P. Angiogenesis in life, disease and medicine. Nature 2005, 438, 932–936. [Google Scholar] [CrossRef]
- Polverini, P.J. Angiogenesis in health and disease: Insights into basic mechanisms and therapeutic opportunities. J. Dent. Educ. 2002, 66, 962–975. [Google Scholar] [CrossRef]
- Memis, A.; Ozden, C.; Ozdal, O.L.; Guzel, O.; Han, O.; Seckin, S. Effect of finasteride treatment on suburethral prostatic microvessel density in patients with hematuria related to benign prostate hyperplasia. Urol. Int. 2008, 80, 177–180. [Google Scholar] [CrossRef]
- De Falco, S. Antiangiogenesis therapy: An update after the first decade. Korean J. Intern. Med. 2014, 29, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Betz, C.; Lenard, A.; Belting, H.G.; Affolter, M. Cell behaviors and dynamics during angiogenesis. Development 2016, 143, 2249–2260. [Google Scholar] [CrossRef] [Green Version]
- Sweeney, M.; Foldes, G. It takes two: Endothelial-perivascular cell cross-talk in vascular development and disease. Front. Cardiovasc. Med. 2018, 5, 154. [Google Scholar] [CrossRef] [PubMed]
- Betsholtz, C. Cell-cell signaling in blood vessel development and function. EMBO Mol. Med. 2018, 10, e8610. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eelen, G.; Treps, L.; Li, X.; Carmeliet, P. Basic and therapeutic aspects of angiogenesis updated. Circ. Res. 2020, 127, 310–329. [Google Scholar] [CrossRef] [PubMed]
- Apte, R.S.; Chen, D.S.; Ferrara, N. Vegf in signaling and disease: Beyond discovery and development. Cell 2019, 176, 1248–1264. [Google Scholar] [CrossRef] [Green Version]
- Zirlik, K.; Duyster, J. Anti-angiogenics: Current situation and future perspectives. Oncol. Res. Treat. 2018, 41, 166–171. [Google Scholar] [CrossRef]
- Shaik, F.; Cuthbert, G.A.; Homer-Vanniasinkam, S.; Muench, S.P.; Ponnambalam, S.; Harrison, M.A. Structural basis for vascular endothelial growth factor receptor activation and implications for disease therapy. Biomolecules 2020, 10, 1673. [Google Scholar] [CrossRef]
- Park, S.A.; Jeong, M.S.; Ha, K.T.; Jang, S.B. Structure and function of vascular endothelial growth factor and its receptor system. BMB Rep. 2018, 51, 73–78. [Google Scholar] [CrossRef] [Green Version]
- Karaman, S.; Leppanen, V.M.; Alitalo, K. Vascular endothelial growth factor signaling in development and disease. Development 2018, 145, dev151019. [Google Scholar] [CrossRef] [Green Version]
- Hamada, K.; Oike, Y.; Takakura, N.; Ito, Y.; Jussila, L.; Dumont, D.J.; Alitalo, K.; Suda, T. Vegf-c signaling pathways through vegfr-2 and vegfr-3 in vasculoangiogenesis and hematopoiesis. Blood 2000, 96, 3793–3800. [Google Scholar] [CrossRef]
- Hiratsuka, S.; Minowa, O.; Kuno, J.; Noda, T.; Shibuya, M. Flt-1 lacking the tyrosine kinase domain is sufficient for normal development and angiogenesis in mice. Proc. Natl. Acad. Sci. USA 1998, 95, 9349–9354. [Google Scholar] [CrossRef] [Green Version]
- Michaelsen, S.R.; Staberg, M.; Pedersen, H.; Jensen, K.E.; Majewski, W.; Broholm, H.; Nedergaard, M.K.; Meulengracht, C.; Urup, T.; Villingshoj, M.; et al. Vegf-c sustains vegfr2 activation under bevacizumab therapy and promotes glioblastoma maintenance. Neuro Oncol. 2018, 20, 1462–1474. [Google Scholar] [CrossRef] [Green Version]
- Shibuya, M.; Claesson-Welsh, L. Signal transduction by vegf receptors in regulation of angiogenesis and lymphangiogenesis. Exp. Cell Res. 2006, 312, 549–560. [Google Scholar] [CrossRef]
- Goldman, J.; Rutkowski, J.M.; Shields, J.D.; Pasquier, M.C.; Cui, Y.; Schmokel, H.G.; Willey, S.; Hicklin, D.J.; Pytowski, B.; Swartz, M.A. Cooperative and redundant roles of vegfr-2 and vegfr-3 signaling in adult lymphangiogenesis. FASEB J. 2007, 21, 1003–1012. [Google Scholar] [CrossRef]
- Abhinand, C.S.; Raju, R.; Soumya, S.J.; Arya, P.S.; Sudhakaran, P.R. Vegf-a/vegfr2 signaling network in endothelial cells relevant to angiogenesis. J. Cell Commun. Signal. 2016, 10, 347–354. [Google Scholar] [CrossRef] [Green Version]
- Ferrara, N.; Adamis, A.P. Ten years of anti-vascular endothelial growth factor therapy. Nat. Rev. Drug Discov. 2016, 15, 385–403. [Google Scholar] [CrossRef] [Green Version]
- Grothey, A.; Galanis, E. Targeting angiogenesis: Progress with anti-vegf treatment with large molecules. Nat. Rev. Clin. Oncol. 2009, 6, 507–518. [Google Scholar] [CrossRef]
- Hsu, J.Y.; Wakelee, H.A. Monoclonal antibodies targeting vascular endothelial growth factor: Current status and future challenges in cancer therapy. BioDrugs 2009, 23, 289–304. [Google Scholar] [CrossRef]
- Solomon, S.D.; Lindsley, K.; Vedula, S.S.; Krzystolik, M.G.; Hawkins, B.S. Anti-vascular endothelial growth factor for neovascular age-related macular degeneration. Cochrane Database Syst. Rev. 2019, 3, CD005139. [Google Scholar] [CrossRef]
- Gramatzki, D.; Roth, P.; Rushing, E.J.; Weller, J.; Andratschke, N.; Hofer, S.; Korol, D.; Regli, L.; Pangalu, A.; Pless, M.; et al. Bevacizumab may improve quality of life, but not overall survival in glioblastoma: An epidemiological study. Ann. Oncol. 2018, 29, 1431–1436. [Google Scholar] [CrossRef]
- Kurkjian, C.; Kim, E.S. Risks and benefits with bevacizumab: Evidence and clinical implications. Ther. Adv. Drug Saf. 2012, 3, 59–69. [Google Scholar] [CrossRef]
- Ribatti, D.; Annese, T.; Ruggieri, S.; Tamma, R.; Crivellato, E. Limitations of anti-angiogenic treatment of tumors. Transl. Oncol. 2019, 12, 981–986. [Google Scholar] [CrossRef]
- Rampogu, S.; Baek, A.; Park, C.; Son, M.; Parate, S.; Parameswaran, S.; Park, Y.; Shaik, B.; Kim, J.H.; Park, S.J.; et al. Discovery of small molecules that target vascular endothelial growth factor receptor-2 signalling pathway employing molecular modelling studies. Cells 2019, 8, 269. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haibe, Y.; Kreidieh, M.; El Hajj, H.; Khalifeh, I.; Mukherji, D.; Temraz, S.; Shamseddine, A. Resistance mechanisms to anti-angiogenic therapies in cancer. Front. Oncol. 2020, 10, 221. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yu, J.; Rupasinghe, C.; Wilson, J.L.; Taylor, L.; Rahimi, N.; Mierke, D.; Polgar, P. Targeting receptor tyrosine kinases and their downstream signaling with cell-penetrating peptides in human pulmonary artery smooth muscle and endothelial cells. Chem. Biol. Drug Des. 2015, 85, 586–597. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Davis, M.I.; Hunt, J.P.; Herrgard, S.; Ciceri, P.; Wodicka, L.M.; Pallares, G.; Hocker, M.; Treiber, D.K.; Zarrinkar, P.P. Comprehensive analysis of kinase inhibitor selectivity. Nat. Biotechnol. 2011, 29, 1046–1051. [Google Scholar] [CrossRef] [PubMed]
- Michaloski, J.S.; Redondo, A.R.; Magalhaes, L.S.; Cambui, C.C.; Giordano, R.J. Discovery of pan-vegf inhibitory peptides directed to the extracellular ligand-binding domains of the vegf receptors. Sci. Adv. 2016, 2, e1600611. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sun, J.Z.; Blaskovich, M.A.; Jain, R.K.; Delarue, F.; Paris, D.; Brem, S.; Wotoczek-Obadia, M.; Lin, Q.; Coppola, D.; Choi, K.H.; et al. Blocking angiogenesis and tumorigenesis with gfa-116, a synthetic molecule that inhibits binding of vascular endothelial growth factor to its receptor. Cancer Res. 2004, 64, 3586–3592. [Google Scholar] [CrossRef] [Green Version]
- Zilberberg, L.; Shinkaruk, S.; Lequin, O.; Rousseau, B.; Hagedorn, M.; Costa, F.; Caronzolo, D.; Balke, M.; Canron, X.; Convert, O.; et al. Structure and inhibitory effects on angiogenesis and tumor development of a new vascular endothelial growth inhibitor. J. Biol. Chem. 2003, 278, 35564–35573. [Google Scholar] [CrossRef] [Green Version]
- Furukawa, J.; Fujitani, N.; Shinohara, Y. Recent advances in cellular glycomic analyses. Biomolecules 2013, 3, 198–225. [Google Scholar] [CrossRef]
- Stowell, S.R.; Ju, T.; Cummings, R.D. Protein glycosylation in cancer. Annu. Rev. Pathol. 2015, 10, 473–510. [Google Scholar] [CrossRef] [Green Version]
- Reily, C.; Stewart, T.J.; Renfrow, M.B.; Novak, J. Glycosylation in health and disease. Nat. Rev. Nephrol. 2019, 15, 346–366. [Google Scholar] [CrossRef]
- Ferreira, I.G.; Pucci, M.; Venturi, G.; Malagolini, N.; Chiricolo, M.; Dall’Olio, F. Glycosylation as a main regulator of growth and death factor receptors signaling. Int. J. Mol. Sci. 2018, 19, 580. [Google Scholar]
- Goth, C.K.; Petaja-Repo, U.E.; Rosenkilde, M.M. G protein-coupled receptors in the sweet spot: Glycosylation and other post-translational modifications. ACS Pharmacol. Transl. Sci. 2020, 3, 237–245. [Google Scholar] [CrossRef] [PubMed]
- Chandler, K.B.; Leon, D.R.; Meyer, R.D.; Rahimi, N.; Costello, C.E. Site-specific n-glycosylation of endothelial cell receptor tyrosine kinase vegfr-2. J. Proteome Res. 2017, 16, 677–688. [Google Scholar] [CrossRef] [Green Version]
- Duchesne, L.; Tissot, B.; Rudd, T.R.; Dell, A.; Fernig, D.G. N-glycosylation of fibroblast growth factor receptor 1 regulates ligand and heparan sulfate co-receptor binding. J. Biol. Chem. 2006, 281, 27178–27189. [Google Scholar] [CrossRef] [Green Version]
- Kaszuba, K.; Grzybek, M.; Simons, K.; Vattulainen, I.; Coskun, U. N-glycosylation as determinant of epidermal growth factor receptor conformation in membranes. Proc. Natl. Acad. Sci. USA 2015, 112, 4334–4339. [Google Scholar] [CrossRef] [Green Version]
- Cui, X.; Xu, H.; Zhou, S.; Zhao, T.; Liu, A.; Guo, X.; Tang, W.; Wang, F. Evaluation of angiogenic activities of hyaluronan oligosaccharides of defined minimum size. Life Sci. 2009, 85, 573–577. [Google Scholar] [CrossRef]
- Gao, F.; Cao, M.; Yang, C.; He, Y.; Liu, Y. Preparation and characterization of hyaluronan oligosaccharides for angiogenesis study. J. Biomed. Mater. Res. B Appl. Biomater. 2006, 78, 385–392. [Google Scholar] [CrossRef]
- Gao, F.; Liu, Y.; He, Y.; Yang, C.; Wang, Y.; Shi, X.; Wei, G. Hyaluronan oligosaccharides promote excisional wound healing through enhanced angiogenesis. Matrix Biol. 2010, 29, 107–116. [Google Scholar] [CrossRef]
- Gao, F.; Yang, C.X.; Mo, W.; Liu, Y.W.; He, Y.Q. Hyaluronan oligosaccharides are potential stimulators to angiogenesis via rhamm mediated signal pathway in wound healing. Clin. Investig. Med. 2008, 31, E106–E116. [Google Scholar] [CrossRef] [Green Version]
- Lees, V.C.; Fan, T.P.; West, D.C. Angiogenesis in a delayed revascularization model is accelerated by angiogenic oligosaccharides of hyaluronan. Lab. Investig. 1995, 73, 259–266. [Google Scholar] [PubMed]
- Lv, M.; Wang, M.; Cai, W.; Hao, W.; Yuan, P.; Kang, Z. Characterisation of separated end hyaluronan oligosaccharides from leech hyaluronidase and evaluation of angiogenesis. Carbohydr. Polym. 2016, 142, 309–316. [Google Scholar] [CrossRef]
- Matou-Nasri, S.; Gaffney, J.; Kumar, S.; Slevin, M. Oligosaccharides of hyaluronan induce angiogenesis through distinct cd44 and rhamm-mediated signalling pathways involving cdc2 and gamma-adducin. Int. J. Oncol. 2009, 35, 761–773. [Google Scholar]
- Sattar, A.; Kumar, S.; West, D.C. Does hyaluronan have a role in endothelial cell proliferation of the synovium? Semin. Arthritis Rheum. 1992, 22, 37–43. [Google Scholar] [CrossRef]
- Slevin, M.; Kumar, S.; Gaffney, J. Angiogenic oligosaccharides of hyaluronan induce multiple signaling pathways affecting vascular endothelial cell mitogenic and wound healing responses. J. Biol. Chem. 2002, 277, 41046–41059. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Trochon, V.; Mabilat, C.; Bertrand, P.; Legrand, Y.; Smadja-Joffe, F.; Soria, C.; Delpech, B.; Lu, H. Evidence of involvement of cd44 in endothelial cell proliferation, migration and angiogenesis in vitro. Int. J. Cancer 1996, 66, 664–668. [Google Scholar] [CrossRef]
- Wang, N.; Liu, C.; Wang, X.; He, T.; Li, L.; Liang, X.; Wang, L.; Song, L.; Wei, Y.; Wu, Q.; et al. Hyaluronic acid oligosaccharides improve myocardial function reconstruction and angiogenesis against myocardial infarction by regulation of macrophages. Theranostics 2019, 9, 1980–1992. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Han, G.; Guo, B.; Huang, J. Hyaluronan oligosaccharides promote diabetic wound healing by increasing angiogenesis. Pharmacol. Rep. 2016, 68, 1126–1132. [Google Scholar] [CrossRef]
- West, D.C.; Hampson, I.N.; Arnold, F.; Kumar, S. Angiogenesis induced by degradation products of hyaluronic acid. Science 1985, 228, 1324–1326. [Google Scholar] [CrossRef]
- West, D.C.; Kumar, S. The effect of hyaluronate and its oligosaccharides on endothelial cell proliferation and monolayer integrity. Exp. Cell Res. 1989, 183, 179–196. [Google Scholar] [CrossRef]
- Waterstrat, R.M. New alloys show extraordinary resistance to fracture and wear. J. Am. Dent. Assoc. 1992, 123, 32–36. [Google Scholar] [CrossRef]
- Sasisekharan, R.; Ernst, S.; Venkataraman, G. On the regulation of fibroblast growth factor activity by heparin-like glycosaminoglycans. Angiogenesis 1997, 1, 45–54. [Google Scholar] [CrossRef]
- Soker, S.; Svahn, C.M.; Neufeld, G. Vascular endothelial growth factor is inactivated by binding to alpha 2-macroglobulin and the binding is inhibited by heparin. J. Biol. Chem. 1993, 268, 7685–7691. [Google Scholar] [CrossRef]
- Maller, S.M.; Cagnoni, A.J.; Bannoud, N.; Sigaut, L.; Perez Saez, J.M.; Pietrasanta, L.I.; Yang, R.Y.; Liu, F.T.; Croci, D.O.; Di Lella, S.; et al. An adipose tissue galectin controls endothelial cell function via preferential recognition of 3-fucosylated glycans. FASEB J. 2020, 34, 735–753. [Google Scholar] [CrossRef] [Green Version]
- Tapon-Bretaudiere, J.; Chabut, D.; Zierer, M.; Matou, S.; Helley, D.; Bros, A.; Mourao, P.A.; Fischer, A.M. A fucosylated chondroitin sulfate from echinoderm modulates in vitro fibroblast growth factor 2-dependent angiogenesis. Mol. Cancer Res. 2002, 1, 96–102. [Google Scholar]
- Zhu, K.; Amin, M.A.; Zha, Y.; Harlow, L.A.; Koch, A.E. Mechanism by which h-2g, a glucose analog of blood group h antigen, mediates angiogenesis. Blood 2005, 105, 2343–2349. [Google Scholar] [CrossRef] [Green Version]
- Zhou, L.; Yin, R.; Gao, N.; Sun, H.; Chen, D.; Cai, Y.; Ren, L.; Yang, L.; Zuo, Z.; Zhang, H.; et al. Oligosaccharides from fucosylated glycosaminoglycan prevent breast cancer metastasis in mice by inhibiting heparanase activity and angiogenesis. Pharmacol. Res. 2021, 166, 105527. [Google Scholar] [CrossRef]
- Bandara, M.D.; Stine, K.J.; Demchenko, A.V. The chemical synthesis of human milk oligosaccharides: Lacto-n-tetraose (galbeta1 → 3glcnacbeta1 → 3galbeta1 → 4glc). Carbohydr. Res. 2019, 486, 107824. [Google Scholar] [CrossRef]
- Ozcan, E.; Sela, D.A. Inefficient metabolism of the human milk oligosaccharides lacto-n-tetraose and lacto-n-neotetraose shifts bifidobacterium longum subsp. Infantis physiology. Front. Nutr. 2018, 5, 46. [Google Scholar] [CrossRef]
- Marcobal, A.; Barboza, M.; Sonnenburg, E.D.; Pudlo, N.; Martens, E.C.; Desai, P.; Lebrilla, C.B.; Weimer, B.C.; Mills, D.A.; German, J.B.; et al. Bacteroides in the infant gut consume milk oligosaccharides via mucus-utilization pathways. Cell Host Microbe 2011, 10, 507–514. [Google Scholar] [CrossRef] [Green Version]
- Terrazas, L.I.; Walsh, K.L.; Piskorska, D.; McGuire, E.; Harn, D.A. The schistosome oligosaccharide lacto-n-neotetraose expands gr1(+) cells that secrete anti-inflammatory cytokines and inhibit proliferation of naive cd4(+) cells: A potential mechanism for immune polarization in helminth infections. J. Immunol. 2001, 167, 5294–5303. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Farhadihosseinabadi, B.; Gholipourmalekabadi, M.; Salimi, M.; Abdollahifar, M.A.; Bagheri, M.; Samadikuchaksaraei, A.; Ghanbarian, H.; Mozafari, M.; Kazemi, B.; Niknejad, H. The in vivo effect of lacto-n-neotetraose (lnnt) on the expression of type 2 immune response involved genes in the wound healing process. Sci. Rep. 2020, 10, 997. [Google Scholar] [CrossRef] [PubMed]
- Farhadihosseinabadi, B.; Salimi, M.; Kazemi, B.; Samadikuchaksaraei, A.; Ghanbarian, H.; Mozafari, M.; Niknejad, H. Inducing type 2 immune response, induction of angiogenesis, and anti-bacterial and anti-inflammatory properties make lacto-n-neotetraose (lnnt) a therapeutic choice to accelerate the wound healing process. Med. Hypotheses 2020, 134, 109389. [Google Scholar] [CrossRef] [PubMed]
- Morrow, A.L.; Ruiz-Palacios, G.M.; Altaye, M.; Jiang, X.; Guerrero, M.L.; Meinzen-Derr, J.K.; Farkas, T.; Chaturvedi, P.; Pickering, L.K.; Newburg, D.S. Human milk oligosaccharides are associated with protection against diarrhea in breast-fed infants. J. Pediatr. 2004, 145, 297–303. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Bai, Y.; Zhou, J.; Huang, W.; Yan, J.; Tao, J.; Fan, Q.; Liu, Y.; Mei, D.; Yan, Q.; et al. Core fucosylation of maternal milk n-glycan evokes b cell activation by selectively promoting the l-fucose metabolism of gut Bifidobacterium spp. and Lactobacillus spp. mBio 2019, 10. [Google Scholar] [CrossRef] [Green Version]
- Tsou, P.S.; Ruth, J.H.; Campbell, P.L.; Isozaki, T.; Lee, S.; Marotte, H.; Domino, S.E.; Koch, A.E.; Amin, M.A. A novel role for inducible fut2 in angiogenesis. Angiogenesis 2013, 16, 195–205. [Google Scholar] [CrossRef] [Green Version]
- Isozaki, T.; Ruth, J.H.; Amin, M.A.; Campbell, P.L.; Tsou, P.S.; Ha, C.M.; Haines, G.K.; Edhayan, G.; Koch, A.E. Fucosyltransferase 1 mediates angiogenesis, cell adhesion and rheumatoid arthritis synovial tissue fibroblast proliferation. Arthritis Res. Ther. 2014, 16, R28. [Google Scholar] [CrossRef] [Green Version]
- Sun, S.; Liu, Z.; Zhou, H.; Li, G.; Liu, M.; Yao, J.; Zhou, T.; An, G.; Wu, Q.; Dong, N. The role of fucosylation in the promotion of endothelial progenitor cells in neovascularization and bone repair. Biomaterials 2014, 35, 3777–3785. [Google Scholar] [CrossRef]
- Liu, Y.C.; Yen, H.Y.; Chen, C.Y.; Chen, C.H.; Cheng, P.F.; Juan, Y.H.; Chen, C.H.; Khoo, K.H.; Yu, C.J.; Yang, P.C.; et al. Sialylation and fucosylation of epidermal growth factor receptor suppress its dimerization and activation in lung cancer cells. Proc. Natl. Acad. Sci. USA 2011, 108, 11332–11337. [Google Scholar] [CrossRef] [Green Version]
- Yoon, S.J.; Nakayama, K.; Hikita, T.; Handa, K.; Hakomori, S.I. Epidermal growth factor receptor tyrosine kinase is modulated by gm3 interaction with n-linked glcnac termini of the receptor. Proc. Natl. Acad. Sci. USA 2006, 103, 18987–18991. [Google Scholar] [CrossRef] [Green Version]
- Hirakawa, M.; Takimoto, R.; Tamura, F.; Yoshida, M.; Ono, M.; Murase, K.; Sato, Y.; Osuga, T.; Sato, T.; Iyama, S.; et al. Fucosylated tgf-beta receptors transduces a signal for epithelial-mesenchymal transition in colorectal cancer cells. Br. J. Cancer 2014, 110, 156–163. [Google Scholar] [CrossRef] [Green Version]
- Chandler, K.B.; Leon, D.R.; Kuang, J.; Meyer, R.D.; Rahimi, N.; Costello, C.E. N-glycosylation regulates ligand-dependent activation and signaling of vascular endothelial growth factor receptor 2 (vegfr2). J. Biol. Chem. 2019, 294, 13117–13130. [Google Scholar] [CrossRef]
- Chung, T.W.; Kim, S.J.; Choi, H.J.; Kim, K.J.; Kim, M.J.; Kim, S.H.; Lee, H.J.; Ko, J.H.; Lee, Y.C.; Suzuki, A.; et al. Ganglioside gm3 inhibits vegf/vegfr-2-mediated angiogenesis: Direct interaction of gm3 with vegfr-2. Glycobiology 2009, 19, 229–239. [Google Scholar] [CrossRef] [Green Version]
- Mukherjee, P.; Faber, A.C.; Shelton, L.M.; Baek, R.C.; Chiles, T.C.; Seyfried, T.N. Thematic review series: Sphingolipids. Ganglioside gm3 suppresses the proangiogenic effects of vascular endothelial growth factor and ganglioside gd1a. J. Lipid Res. 2008, 49, 929–938. [Google Scholar] [CrossRef] [Green Version]
- Bousseau, S.; Vergori, L.; Soleti, R.; Lenaers, G.; Martinez, M.C.; Andriantsitohaina, R. Glycosylation as new pharmacological strategies for diseases associated with excessive angiogenesis. Pharmacol. Ther. 2018, 191, 92–122. [Google Scholar] [CrossRef]
- Chiodelli, P.; Urbinati, C.; Paiardi, G.; Monti, E.; Rusnati, M. Sialic acid as a target for the development of novel antiangiogenic strategies. Future Med. Chem. 2018, 10, 2835–2854. [Google Scholar] [CrossRef]
- Rudloff, S.; Schneider, D.; Kunz, C.; Bretzel, R.G.; Linn, T. Human milk as a natural source of anti-angiogenic compounds. Pediatr. Res. 2004, 56, 503. [Google Scholar] [CrossRef] [Green Version]
- Chung, T.W.; Kim, E.Y.; Kim, S.J.; Choi, H.J.; Jang, S.B.; Kim, K.J.; Ha, S.H.; Abekura, F.; Kwak, C.H.; Kim, C.H.; et al. Sialyllactose suppresses angiogenesis by inhibiting vegfr-2 activation, and tumor progression. Oncotarget 2017, 8, 58152–58162. [Google Scholar] [CrossRef] [Green Version]
- Kim, E.Y.; Jin, B.R.; Chung, T.W.; Bae, S.J.; Park, H.; Ryu, D.; Jin, L.; An, H.J.; Ha, K.T. 6-sialyllactose ameliorates dihydrotestosterone-induced benign prostatic hyperplasia through suppressing vegf-mediated angiogenesis. BMB Rep. 2019, 52, 560–565. [Google Scholar] [CrossRef]
- Chung, T.W.; Kim, E.Y.; Choi, H.J.; Han, C.W.; Jang, S.B.; Kim, K.J.; Jin, L.; Koh, Y.J.; Ha, K.T. 6′-sialylgalactose inhibits vascular endothelial growth factor receptor 2-mediated angiogenesis. Exp. Mol. Med. 2019, 51, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Teran, M.; Nugent, M.A. Characterization of receptor binding kinetics for vascular endothelial growth factor-a using spr. Anal. Biochem. 2019, 564–565, 21–31. [Google Scholar] [CrossRef] [PubMed]
- Prueksaritanont, T.; Tang, C. Adme of biologics-what have we learned from small molecules? AAPS J. 2012, 14, 410–419. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Phipps, K.R.; Baldwin, N.J.; Lynch, B.; Stannard, D.R.; Soltesova, A.; Gilby, B.; Miks, M.H.; Rohrig, C.H. Toxicological safety evaluation of the human-identical milk oligosaccharide 6′-sialyllactose sodium salt. J. Appl. Toxicol. 2019, 39, 1444–1461. [Google Scholar] [CrossRef]
- Phipps, K.R.; Baldwin, N.J.; Lynch, B.; Stannard, D.R.; Soltesova, A.; Gilby, B.; Miks, M.H.; Rohrig, C.H. Toxicological safety assessment of the human-identical milk oligosaccharide 3′-sialyllactose sodium salt. J. Appl. Toxicol. 2019, 39, 1378–1393. [Google Scholar] [CrossRef] [PubMed]
- Monaco, M.H.; Gurung, R.B.; Donovan, S.M. Safety evaluation of 3′-siallylactose sodium salt supplementation on growth and clinical parameters in neonatal piglets. Regul. Toxicol. Pharmacol. 2019, 101, 57–64. [Google Scholar] [CrossRef]

| Compound | Reference (PMID) | Exam | Molecular Target | Effect on Angiogenesis | Disease Model | |
|---|---|---|---|---|---|---|
| Heparin, heparan sulfate, or their fragments | 7681826 | in vitro | α2-Macroglobulin | Promotion | N.D. (1) | |
| 3746342 | in vitro, in vivo | Growth of cerebral microvessel endothelial cell | Inhibition | N.D. (1) | ||
| 14517393 | in vitro | FGF | Inhibition | N.D. (1) | ||
| Hyaluronan, hyaluronic acid, or their fragments | 2408340 | in vitro | N.D. (1) | Promote | N.D. (1) | |
| 2472284 | in vitro | Endothelial cell proliferation | Promotion or inhibition (2) | N.D. (1) | ||
| 1384133 | in vitro | N.D. (1) | Promotion or inhibition (2) | N.D. (1) | ||
| 8647630 | in vitro | CD44 | Promotion | N.D. (1) | ||
| 7543630 | in vivo | N.D. (1) | Promotion | Skin wound healing | ||
| 18544273 | in vitro | RHAMM (receptor for hyaluronan mediated motility) | Promotion | Skin wound healing | ||
| 12194965 | in vitro | PKCα, -β1, -β2, -ε | Promotion | Skin wound healing | ||
| 19724912 | in vitro | CD44 and RHAMM | Promotion | Wound healing | ||
| 19913615 | in vivo | LYVE-1 (lymphatic vessel endothelial hyaluronan receptor 1) and CD31 | Promotion | Skin wound healing | ||
| 16544303 | in vitro | Endothelial cell proliferation | Promotion | Wound healing | ||
| 27588388 | in vivo | Phosphorylation of Src and ERK TGF-β expression | Promotion | Diabetic wound | ||
| 31037151 | in vivo | macrophage M2 polarization (MAPK, JAK/STAT pathway) | Promotion | Myocardial infarction | ||
| 26917404 | in vitro, in vivo | CD44 | Promotion | N.D. (1) | ||
| 19720068 | in vitro | VEGF (mRNA level) | Promotion | N.D. (1) | ||
| Lacto-N-Neotetraose (3) | 31969618 | in vitro, in vivo | Th2 immune response | Promotion | Skin wound healing | |
| Sialylated oligosaccharides | 6′-sialylgalactose, 3′-sialylgalactose | 31604908 | in vitro, in vivo | VEGF receptor 2 | Inhibition | Cancer and retinopathy |
| 6′-sialyllactose, 3′-sialyllactose (3) | 28938544 | in vitro, in vivo | VEGF receptor 2 | Inhibition | Cancer | |
| 6′-sialyllactose (3) | 31383249 | in vitro, in vivo | VEGF receptor 2 | Inhibition | Benign prostatic hyperplasia | |
| Fucosylated oligosaccharides | Fucosylated glycosaminoglycan | 33667689 | in vitro, in vivo | Heparanase | Inhibition | Cancer |
| Fucosylated chondroitin sulfate | 12496356 | in vitro, in vivo | FGF-2 | Promotion | Ischemia and thrombosis | |
| 3′-fucosylated glycans (3) | 31914594 | in vitro, in vivo | Galectin-12 | Promotion | Adipose metabolic disorder | |
| 2′-fucosyl lactose (H-2g) (3) | 15498849 | in vitro, in vivo | Secretion of bFGF and VEGF | Promotion | N.D. (1) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bae, B.; Kim, H.; Park, H.; Koh, Y.J.; Bae, S.-J.; Ha, K.-T. Anti-Angiogenic Property of Free Human Oligosaccharides. Biomolecules 2021, 11, 775. https://doi.org/10.3390/biom11060775
Bae B, Kim H, Park H, Koh YJ, Bae S-J, Ha K-T. Anti-Angiogenic Property of Free Human Oligosaccharides. Biomolecules. 2021; 11(6):775. https://doi.org/10.3390/biom11060775
Chicago/Turabian StyleBae, Boram, Haeun Kim, Hyerin Park, Young Jun Koh, Sung-Jin Bae, and Ki-Tae Ha. 2021. "Anti-Angiogenic Property of Free Human Oligosaccharides" Biomolecules 11, no. 6: 775. https://doi.org/10.3390/biom11060775






