Scoping Review of Machine Learning and Patient-Reported Outcomes in Spine Surgery
Abstract
:1. Introduction
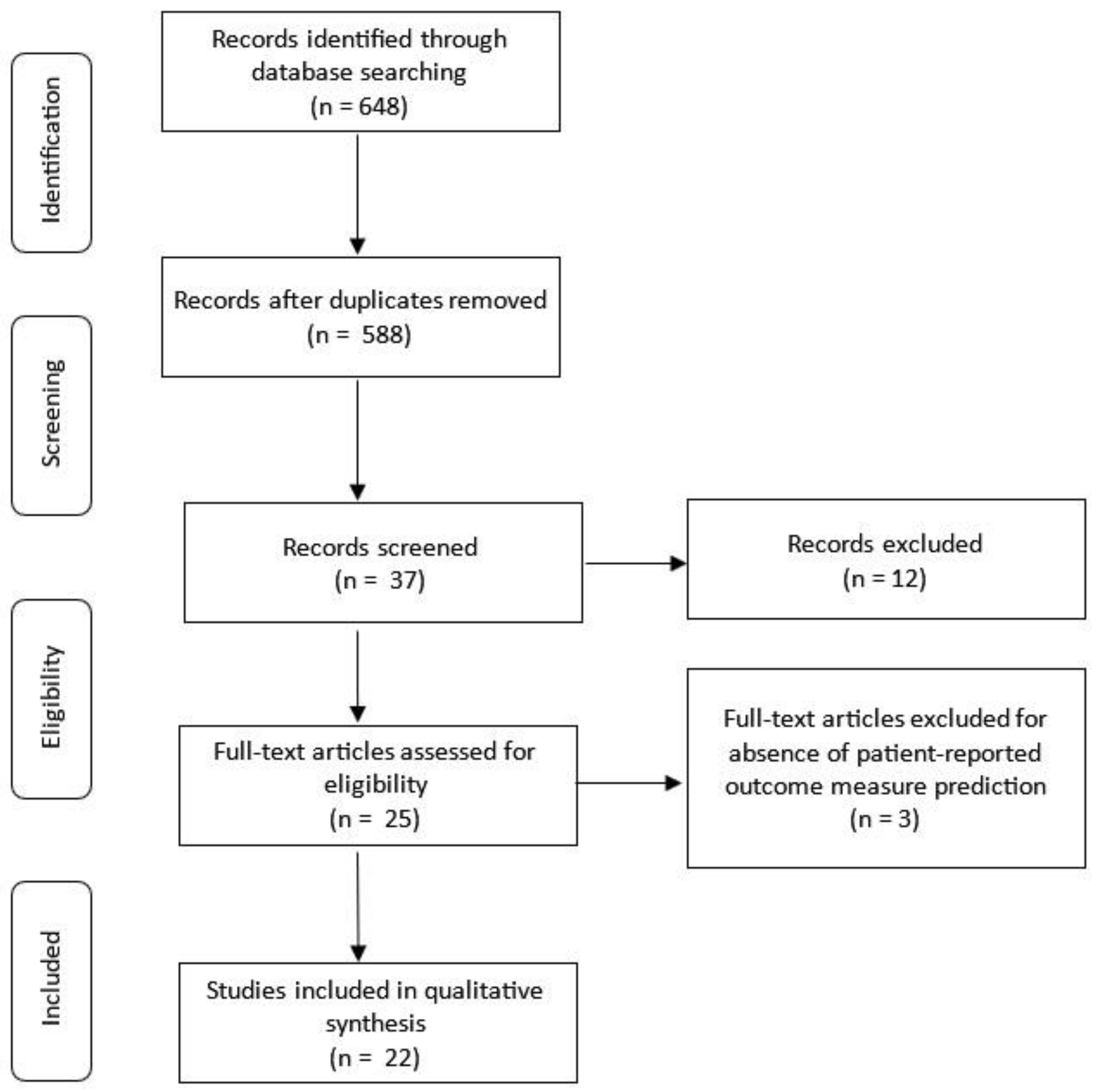
2. Materials and Methods
3. Results
3.1. Search Results
3.2. Study Details
3.3. Key Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tragaris, T.; Benetos, I.S.; Vlamis, J.; Pneumaticos, S.; Tragaris, T.; Benetos, I.S.; Vlamis, J.; Pneumaticos, S.G. Machine Learning Applications in Spine Surgery. Cureus 2023, 15, e48078. [Google Scholar] [CrossRef]
- Vernon, H.; Mior, S. The Neck Disability Index: A Study of Reliability and Validity. J. Manip. Physiol. Ther. 1991, 14, 409–415. [Google Scholar]
- McCormick, J.D.; Werner, B.C.; Shimer, A.L. Patient-Reported Outcome Measures in Spine Surgery. JAAOS J. Am. Acad. Orthop. Surg. 2013, 21, 99. [Google Scholar] [CrossRef] [PubMed]
- Franceschini, M.; Boffa, A.; Pignotti, E.; Andriolo, L.; Zaffagnini, S.; Filardo, G. The Minimal Clinically Important Difference Changes Greatly Based on the Different Calculation Methods. Am. J. Sports Med. 2023, 51, 1067–1073. [Google Scholar] [CrossRef]
- Jaeschke, R.; Singer, J.; Guyatt, G.H. Measurement of Health Status. Ascertaining the Minimal Clinically Important Difference. Control Clin. Trials 1989, 10, 407–415. [Google Scholar] [CrossRef] [PubMed]
- Beighley, A.; Zhang, A.; Huang, B.; Carr, C.; Mathkour, M.; Werner, C.; Scullen, T.; Kilgore, M.D.; Maulucci, C.M.; Dallapiazza, R.F.; et al. Patient-Reported Outcome Measures in Spine Surgery: A Systematic Review. J. Craniovertebral Junction Spine 2022, 13, 378–389. [Google Scholar] [CrossRef]
- Intro to PROMIS. Available online: https://www.healthmeasures.net/explore-measurement-systems/promis/intro-to-promis (accessed on 17 October 2024).
- Young, R.R. Emerging Role of Artificial Intelligence and Big Data in Spine Care. Int. J. Spine Surg. 2023, 17, S3–S10. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Moustafa, I.M.; Ozsahin, D.U.; Mustapha, M.T.; Ahbouch, A.; Oakley, P.A.; Harrison, D.E. Utilizing Machine Learning to Predict Post-Treatment Outcomes in Chronic Non-Specific Neck Pain Patients Undergoing Cervical Extension Traction. Sci. Rep. 2024, 14, 11781. [Google Scholar] [CrossRef] [PubMed]
- Janssen, E.R.; Osong, B.; van Soest, J.; Dekker, A.; van Meeteren, N.L.; Willems, P.C.; Punt, I.M. Exploring Associations of Preoperative Physical Performance With Postoperative Outcomes After Lumbar Spinal Fusion: A Machine Learning Approach. Arch. Phys. Med. Rehabil. 2021, 102, 1324–1330.e3. [Google Scholar] [CrossRef]
- Wondra, J.P.I.; Kelly, M.P.; Greenberg, J.; Yanik, E.L.; Ames, C.P.; Pellise, F.; Vila-Casademunt, A.; Smith, J.S.; Bess, S.; Shaffrey, C.I.; et al. Validation of Adult Spinal Deformity Surgical Outcome Prediction Tools in Adult Symptomatic Lumbar Scoliosis. Spine 2023, 48, 21. [Google Scholar] [CrossRef]
- Durand, W.M.; Lafage, R.; Hamilton, D.K.; Passias, P.G.; Kim, H.J.; Protopsaltis, T.; Lafage, V.; Smith, J.S.; Shaffrey, C.; Gupta, M.; et al. Artificial Intelligence Clustering of Adult Spinal Deformity Sagittal Plane Morphology Predicts Surgical Characteristics, Alignment, and Outcomes. Eur. Spine J. 2021, 30, 2157–2166. [Google Scholar] [CrossRef]
- Park, C.; Mummaneni, P.V.; Gottfried, O.N.; Shaffrey, C.I.; Tang, A.J.; Bisson, E.F.; Asher, A.L.; Coric, D.; Potts, E.A.; Foley, K.T.; et al. Which Supervised Machine Learning Algorithm Can Best Predict Achievement of Minimum Clinically Important Difference in Neck Pain after Surgery in Patients with Cervical Myelopathy? A QOD Study. Neurosurg. Focus 2023, 54, E5. [Google Scholar] [CrossRef]
- Merali, Z.G.; Witiw, C.D.; Badhiwala, J.H.; Wilson, J.R.; Fehlings, M.G. Using a Machine Learning Approach to Predict Outcome after Surgery for Degenerative Cervical Myelopathy. PLoS ONE 2019, 14, e0215133. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.K.; Jayasekera, D.; Javeed, S.; Greenberg, J.K.; Blum, J.; Dibble, C.F.; Sun, P.; Song, S.-K.; Ray, W.Z. Diffusion Basis Spectrum Imaging Predicts Long-Term Clinical Outcomes Following Surgery in Cervical Spondylotic Myelopathy. Spine J. 2023, 23, 504–512. [Google Scholar] [CrossRef]
- Khan, O.; Badhiwala, J.H.; Witiw, C.D.; Wilson, J.R.; Fehlings, M.G. Machine Learning Algorithms for Prediction of Health-Related Quality-of-Life after Surgery for Mild Degenerative Cervical Myelopathy. Spine J. 2021, 21, 1659–1669. [Google Scholar] [CrossRef] [PubMed]
- Liew, B.X.W.; Peolsson, A.; Rugamer, D.; Wibault, J.; Löfgren, H.; Dedering, A.; Zsigmond, P.; Falla, D. Clinical Predictive Modelling of Post-Surgical Recovery in Individuals with Cervical Radiculopathy: A Machine Learning Approach. Sci. Rep. 2020, 10, 16782. [Google Scholar] [CrossRef]
- Khan, O.; Badhiwala, J.H.; Akbar, M.A.; Fehlings, M.G. Prediction of Worse Functional Status After Surgery for Degenerative Cervical Myelopathy: A Machine Learning Approach. Neurosurgery 2021, 88, 584. [Google Scholar] [CrossRef]
- Hoffman, H.; Lee, S.I.; Garst, J.H.; Lu, D.S.; Li, C.H.; Nagasawa, D.T.; Ghalehsari, N.; Jahanforouz, N.; Razaghy, M.; Espinal, M.; et al. Use of Multivariate Linear Regression and Support Vector Regression to Predict Functional Outcome after Surgery for Cervical Spondylotic Myelopathy. J. Clin. Neurosci. 2015, 22, 1444–1449. [Google Scholar] [CrossRef]
- Grob, A.; Rohr, J.; Stumpo, V.; Vieli, M.; Ciobanu-Caraus, O.; Ricciardi, L.; Maldaner, N.; Raco, A.; Miscusi, M.; Perna, A.; et al. Multicenter External Validation of Prediction Models for Clinical Outcomes after Spinal Fusion for Lumbar Degenerative Disease. Eur. Spine J. 2024, 33, 3534–3544. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.; Oh, I.Y.; Kim, S.; Marks, M.C.; Payne, P.R.O.; Ames, C.P.; Pellise, F.; Pahys, J.M.; Fletcher, N.D.; Newton, P.O.; et al. Machine Learning for Benchmarking Adolescent Idiopathic Scoliosis Surgery Outcomes. Spine 2023, 48, 1138. [Google Scholar] [CrossRef]
- Ames, C.P.; Smith, J.S.; Pellisé, F.; Kelly, M.; Gum, J.L.; Alanay, A.; Acaroğlu, E.; Pérez-Grueso, F.J.S.; Kleinstück, F.S.; Obeid, I.; et al. Development of Predictive Models for All Individual Questions of SRS-22R after Adult Spinal Deformity Surgery: A Step toward Individualized Medicine. Eur. Spine J. 2019, 28, 1998–2011. [Google Scholar] [CrossRef] [PubMed]
- Staartjes, V.E.; de Wispelaere, M.P.; Vandertop, W.P.; Schröder, M.L. Deep Learning-Based Preoperative Predictive Analytics for Patient-Reported Outcomes Following Lumbar Discectomy: Feasibility of Center-Specific Modeling. Spine J. Off. J. N. Am. Spine Soc. 2019, 19, 853–861. [Google Scholar] [CrossRef] [PubMed]
- Khor, S.; Lavallee, D.; Cizik, A.M.; Bellabarba, C.; Chapman, J.R.; Howe, C.R.; Lu, D.; Mohit, A.A.; Oskouian, R.J.; Roh, J.R.; et al. Development and Validation of a Prediction Model for Pain and Functional Outcomes After Lumbar Spine Surgery. JAMA Surg. 2018, 153, 634–642. [Google Scholar] [CrossRef]
- Pedersen, C.F.; Andersen, M.Ø.; Carreon, L.Y.; Eiskjær, S. Applied Machine Learning for Spine Surgeons: Predicting Outcome for Patients Undergoing Treatment for Lumbar Disc Herniation Using PRO Data. Glob. Spine J. 2022, 12, 866–876. [Google Scholar] [CrossRef] [PubMed]
- Berjano, P.; Langella, F.; Ventriglia, L.; Compagnone, D.; Barletta, P.; Huber, D.; Mangili, F.; Licandro, G.; Galbusera, F.; Cina, A.; et al. The Influence of Baseline Clinical Status and Surgical Strategy on Early Good to Excellent Result in Spinal Lumbar Arthrodesis: A Machine Learning Approach. J. Pers. Med. 2021, 11, 1377. [Google Scholar] [CrossRef] [PubMed]
- Halicka, M.; Wilby, M.; Duarte, R.; Brown, C. Predicting Patient-Reported Outcomes Following Lumbar Spine Surgery: Development and External Validation of Multivariable Prediction Models. BMC Musculoskelet. Disord. 2023, 24, 333. [Google Scholar] [CrossRef] [PubMed]
- Karhade, A.; Fogel, H.A.; Cha, T.D.; Hershman, S.H.; Doorly, T.P.; Kang, J.D.; Bono, C.M.; Harris, M.B.; Schwab, J.H.; Tobert, D.G. Development of Prediction Models for Clinically Meaningful Improvement in PROMIS Scores after Lumbar Decompression. Spine J. 2021, 21, 397–404. [Google Scholar] [CrossRef] [PubMed]
- Yagi, M.; Michikawa, T.; Yamamoto, T.; Iga, T.; Ogura, Y.; Tachibana, A.; Miyamoto, A.; Suzuki, S.; Nori, S.; Takahashi, Y.; et al. Development and Validation of Machine Learning-Based Predictive Model for Clinical Outcome of Decompression Surgery for Lumbar Spinal Canal Stenosis. Spine J. 2022, 22, 1768–1777. [Google Scholar] [CrossRef] [PubMed]
- Finkelstein, J.A.; Stark, R.B.; Lee, J.; Schwartz, C.E. Patient Factors That Matter in Predicting Spine Surgery Outcomes: A Machine Learning Approach. J. Neurosurg. Spine 2021, 35, 127–136. [Google Scholar] [CrossRef]
- Siccoli, A.; de Wispelaere, M.P.; Schröder, M.L.; Staartjes, V.E. Machine Learning–Based Preoperative Predictive Analytics for Lumbar Spinal Stenosis. Neurosurg. Focus 2019, 46, E5. [Google Scholar] [CrossRef] [PubMed]
- Staartjes, V.E.; Stumpo, V.; Ricciardi, L.; Maldaner, N.; Eversdijk, H.A.J.; Vieli, M.; Ciobanu-Caraus, O.; Raco, A.; Miscusi, M.; Perna, A.; et al. FUSE-ML: Development and External Validation of a Clinical Prediction Model for Mid-Term Outcomes after Lumbar Spinal Fusion for Degenerative Disease. Eur. Spine J. 2022, 31, 2629–2638. [Google Scholar] [CrossRef] [PubMed]
- Müller, D.; Haschtmann, D.; Fekete, T.F.; Kleinstück, F.; Reitmeir, R.; Loibl, M.; O’Riordan, D.; Porchet, F.; Jeszenszky, D.; Mannion, A.F. Development of a Machine-Learning Based Model for Predicting Multidimensional Outcome after Surgery for Degenerative Disorders of the Spine. Eur. Spine J. 2022, 31, 2125–2136. [Google Scholar] [CrossRef] [PubMed]
- Rigoard, P.; Ounajim, A.; Goudman, L.; Louis, P.-Y.; Slaoui, Y.; Roulaud, M.; Naiditch, N.; Bouche, B.; Page, P.; Lorgeoux, B.; et al. A Novel Multi-Dimensional Clinical Response Index Dedicated to Improving Global Assessment of Pain in Patients with Persistent Spinal Pain Syndrome after Spinal Surgery, Based on a Real-Life Prospective Multicentric Study (PREDIBACK) and Machine Learning Techniques. J. Clin. Med. 2021, 10, 4910. [Google Scholar] [CrossRef] [PubMed]
- Cooper, M.E.; Torre-Healy, L.A.; Alentado, V.J.; Cho, S.; Steinmetz, M.P.; Benzel, E.C.; Mroz, T.E. Heterogeneity of Reporting Outcomes in the Spine Surgery Literature. Clin. Spine Surg. 2018, 31, E221–E229. [Google Scholar] [CrossRef]
- Collins, G.S.; Moons, K.G.M.; Dhiman, P.; Riley, R.D.; Beam, A.L.; Calster, B.V.; Ghassemi, M.; Liu, X.; Reitsma, J.B.; van Smeden, M.; et al. TRIPOD+AI Statement: Updated Guidance for Reporting Clinical Prediction Models That Use Regression or Machine Learning Methods. BMJ 2024, 385, e078378. [Google Scholar] [CrossRef]
- Bielewicz, J.; Daniluk, B.; Kamieniak, P. VAS and NRS, Same or Different? Are Visual Analog Scale Values and Numerical Rating Scale Equally Viable Tools for Assessing Patients after Microdiscectomy? Pain Res. Manag. 2022, 2022, 5337483. [Google Scholar] [CrossRef]
- Archer, K.R.; Devin, C.J.; Vanston, S.W.; Koyama, T.; Phillips, S.E.; Mathis, S.L.; George, S.Z.; McGirt, M.J.; Spengler, D.M.; Aaronson, O.S.; et al. Cognitive-Behavioral-Based Physical Therapy for Patients With Chronic Pain Undergoing Lumbar Spine Surgery: A Randomized Controlled Trial. J. Pain 2016, 17, 76–89. [Google Scholar] [CrossRef]
- Khan, A.S.R.; Mattei, T.A.; Mercier, P.J.; Cloney, M.; Dahdaleh, N.S.; Koski, T.R.; El Tecle, N.E. Outcome Reporting in Spine Surgery: A Review of Historical and Emerging Trends. World Neurosurg. 2023, 179, 88–98. [Google Scholar] [CrossRef]
- Christodoulou, E.; Ma, J.; Collins, G.S.; Steyerberg, E.W.; Verbakel, J.Y.; Van Calster, B. A Systematic Review Shows No Performance Benefit of Machine Learning over Logistic Regression for Clinical Prediction Models. J. Clin. Epidemiol. 2019, 110, 12–22. [Google Scholar] [CrossRef] [PubMed]
| Article | Pathology | # of Pts | Predicted PROMs | ML Models | Input Features | PPT (Months) | Results (AUC) * |
|---|---|---|---|---|---|---|---|
| Liew et al. [17] | Cervical | 193 | NDI, EQ5D, NP | Stepwise regression, LASSO, boosting, MARS | Demographics, PE, PROMs | 12 | Not reported |
| Park et al. [13] | CSM | 535 | VAS-NP | LR, SVM, DT, RF, extra trees, Gaussian naïve Bayes, KNN, multilayer perceptron, EGBT | Demographics, Sx chars, PROMs, spinal pathology, PE | 3; 24 | VAS-NP 0.773–0.762 |
| Zhang et al. [15] | CSM | 50 | SF-36, PCS | SVM | Demographics, PE, PROs, imaging chars | 6 | SF-36 PCS 86.4, MCS 89.8 |
| Merali et al. [14] | DCM | 757 | SF-6D, mJOA | RF, SVM, LR, DT, ANN models | Demographics, spinal pathology, Sx chars, comorbidities, PROMs, PE | 3–24 | SF-6D and mJOA0.83–0.87 |
| Khan et al. [16] | DCM | 173 | SF-36 MCS, SF-36 PCS | Classification trees, SVM, partial least squares, generalized boosted models, generalized additive models, MARS, RF, LR | Demographics, PE, comorbidities, Sx Hx, spinal pathology, mJOA | 12 | MCS 0.77, PCS 0.78 |
| Hoffman et al. [19] | DCM | 20 | ODI | MLR, SVR | Demographics, spinal pathology, Sx chars, comorbidities, PROs, PE, fine motor function | 6, 12, and 24 | MAA of 0.0283 with SVR |
| Khan et al. [18] | DCM | 702 | mJOA | Boosted LR, SVM, naïve Bayes, generalized boosted machines, partial least squares, LR | Demographics, Sx chars, spinal pathology, PE | 12 | mJOA 0.834 |
| Grob et al. [20] | Thoraco- lumbar | 1115 | ODI, BP (NRS), LP (NRS) | FUSE-ML, EN regularization | MRI, PROMs, demographics, ASA, PMHx, Sx Hx | 12 | ODI 0.70, BP 0.72, LP 0.70 |
| Gupta et al. [21] | AIS | 6076 | SRS-Pain, SRS-Self-Image | LR, gradient boosting, EGBT | PROMs, demographics, spinal pathology, Sx chars | 6; 12; 24 | MAE 0.47–0.55 |
| Pedersen et al. [25] | LDH | 1968 | ODI, VAS | DL, DT, RF, BT, SVM, LR, MARS | Demographics, PROs, employment details, comorbidities, self-reported expectations to return to work | 24 | EQ-5D 0.82, ODI 0.75, VAS LP 0.73, VAS BP 0.81, return to work 0.84 |
| Ve et al. [23] | LDH | 422 | LP (NRS), BP (NRS), ODI | DL, LR | Demographics, ASA, PROMs, Sx chars, Sx Hx, spinal pathology, social Hx | 12 | BP 0.90, LP 0.87, ODI 0.84 |
| Ames et al. [22] | ASD | 561 | Individual SRS-22R questions | EN, gradient boosting machines, EGBT, extreme gradient boosting linear, RF, EN regularized generalized linear models | Demographics, comorbidities, Sx chars, imaging chars, hospital chars, surgeon chars | 12 | SRS-22R questions 0.869 with EGBT |
| Karhade et al. [28] | LS | 906 | PROMIS-PF | Stochastic gradient boosting, RF, SVM, NN, EN penalized LR | Demographics, ASA, spinal pathology, Sx chars, PROMs, Rx opioids, geographic information | 12 | PROMIS-PF 0.75 |
| Yagi et al. [29] | LS | 848 | VAS BP, VAS LP, JOABPEQ | Generalized LR, generalized linear mixed, LR, SVM, single-layer ANN, random trees, linear-AS, tree-AS, EGBT, chi-squared automatic interaction detection classification, regression tree | Demographics, Sx chars, PROMs | 10 | MAE 9.3−16.5 |
| Siccoli et al. [31] | LS | 635 | BP (NRS), LP (NRS), ODI | RF, EGBT, BGLM, BT, KNN, simple BGLM, ANN with a single hidden layer | Clinical data, imaging chars, PROMs, demographics, ASA, Sx Hx, spinal pathology | 6 weeks; 12 months | NRS-BP 0.79, 0.92 |
| Khor et al. [24] | LS | 1965 | BP (NRS), LP (NRS), ODI | Binary LR | Demographics, clinical chars, ASA, Sx Hx, PROMs, comorbidities, Sx chars, Rx opioids, hospital chars | 12 | ODI 0.66, BP 0.79, and LP 0.69 |
| Berjano et al. [26] | Lumbar | 1243 | ODI, SF-36, PCS, COMI Back | RF | Demographics, comorbidities, spinal pathology, PROMs, past Sx Hx | 6 | ODI 0.808 |
| Finkelstein et al. [30] | Lumbar | 122 | NRS | LASSO regression | Clinical and demographic variables, PROMs, patient expectations and cognitive appraisal processes | 10 | NRS of 0.12 MBR2 |
| Staartjes et al. [32] | Lumbar | 1115 | ODI, COMI, NRS | EN regularization | Demographics, Rx opioids, Sx Hx, Sx chars, PROMs | 12 | ODI and COMI 0.67 |
| Halicka et al. [27] | Lumbar | 4307 | COMI-BP, COMI-LP | RF, LR | Demographics, Sx chars, hospitalization chars | 3–24 | COMI 0.63, BP 0.72, LP 0.68 |
| Rigoard et al. [33] | Lumbar | 200 | PGIC | DRFA, PCA | ODI, EQ-5D, HADS, NRS | 12 | PGIC 0.853 |
| Muller et al. [34] | Cervical and lumbar | 10,002 | COMI | LASSO, ridge regression | Demographics, Sx chars, surgeon chars, PROMs, psychological assessment | 12 | MAE back patients 2.1, neck patients 1.8 |
| Domain | PROM | Description |
|---|---|---|
| Multiple Outcomes | MCRI | Modified Clinical Response Index (MCRI) evaluates pain, functional capacity, quality of life, and outcomes in spinal surgery patients with Persistent Spinal Pain syndrome |
| NASS | North American Spine Society (NASS) assesses outcomes and pain related to lumbar spine disease | |
| EQ-5D | EuroQol-5 Dimensions (EQ-5D) measures health status across five dimensions: mobility, self-care, usual activities, pain/discomfort, anxiety/depression | |
| COMI | Core Outcome Measures Index (COMI) measures the impact of back and leg pain, assessing pain, function, and quality of life | |
| SRS | Scoliosis Research Society (SRS) assesses function, pain, self-image, mental health, and satisfaction | |
| Physical Function | NDI | Neck Disability Index (NDI) evaluates disability related to neck pain and its impact on daily activities |
| JOA | Japanese Orthopaedic Association Score (JOA) assesses neurological function in patients with cervical myelopathy | |
| mJOA | Modified JOA (mJOA) evaluates functional impairment in cervical spine conditions | |
| ODI | Oswestry Disability Index (ODI) assesses disability due to lower back pain | |
| PROMIS- PF | Patient-Reported Outcomes Measurement Information System (PROMIS)-Physical Function (PF) assesses physical function and the ability to perform physical activities | |
| PCS | Physical Component Summary (PCS) is a subscore from SF36 measuring physical health | |
| DASH | Disabilities of the Arm, Shoulder, and Hand (DASH) measures upper-extremity function, pain, and work and social activity participation | |
| Mental Health | MCS | Mental Component Summary (MCS) assesses psychological well-being |
| MDI | Mental Disability Index (MDI) measures mental health-related disability | |
| PGIC | Patient Global Impression of Change (PGIC) measures a patient’s overall perception of improvement or change in condition | |
| Quality of Life | SF-36 | Short Form-36 Health Survey (SF-36) assesses overall health-related quality of life across multiple domains (physical, mental, and social) |
| SF-6D | Short Form-6 Dimensions (SF-6D) is a condensed version of SF36 that measures a single index for health-related quality of life | |
| Pain | VAS | Visual Analog Scale (VAS) measures intensity of pain using a 0–10 visual scale |
| NRS | Numeric rating scale (NRS) quantifies pain on a 0–10 scale | |
| Social | JOABPEQ | Japanese Orthopaedic Association Back Pain Evaluation Questionnaire (JOABPEQ) evaluates the impact of back pain on physical and social functioning |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Quinones, C.; Kumbhare, D.; Guthikonda, B.; Hoang, S. Scoping Review of Machine Learning and Patient-Reported Outcomes in Spine Surgery. Bioengineering 2025, 12, 125. https://doi.org/10.3390/bioengineering12020125
Quinones C, Kumbhare D, Guthikonda B, Hoang S. Scoping Review of Machine Learning and Patient-Reported Outcomes in Spine Surgery. Bioengineering. 2025; 12(2):125. https://doi.org/10.3390/bioengineering12020125
Chicago/Turabian StyleQuinones, Christian, Deepak Kumbhare, Bharat Guthikonda, and Stanley Hoang. 2025. "Scoping Review of Machine Learning and Patient-Reported Outcomes in Spine Surgery" Bioengineering 12, no. 2: 125. https://doi.org/10.3390/bioengineering12020125
APA StyleQuinones, C., Kumbhare, D., Guthikonda, B., & Hoang, S. (2025). Scoping Review of Machine Learning and Patient-Reported Outcomes in Spine Surgery. Bioengineering, 12(2), 125. https://doi.org/10.3390/bioengineering12020125





