Microleakage and Marginal Integrity of Ormocer/Methacrylate-Based Bulk-Fill Resin Restorations in MOD Cavities: SEM and Stereomicroscopic Evaluation
Abstract
1. Introduction
- (1)
- Different types of matrix structures (ormocer vs. methacrylate) have no effect on the microleakage values of restorations;
- (2)
- Different layer thicknesses (2 mm vs. 4 mm) do not affect the microleakage values of restorations.
2. Materials and Methods
Statistical Analysis
3. Results
3.1. Microleakage Analysis
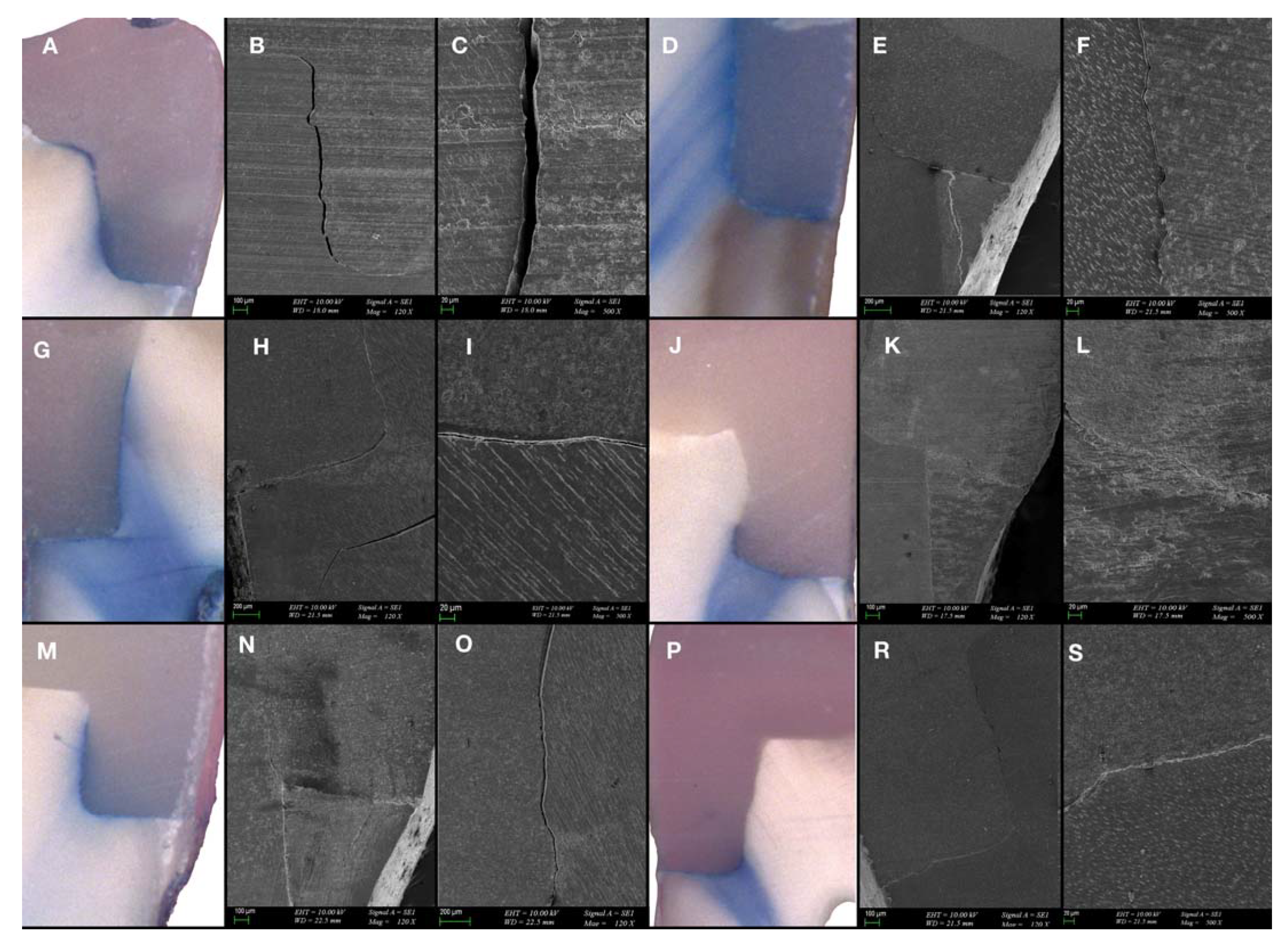
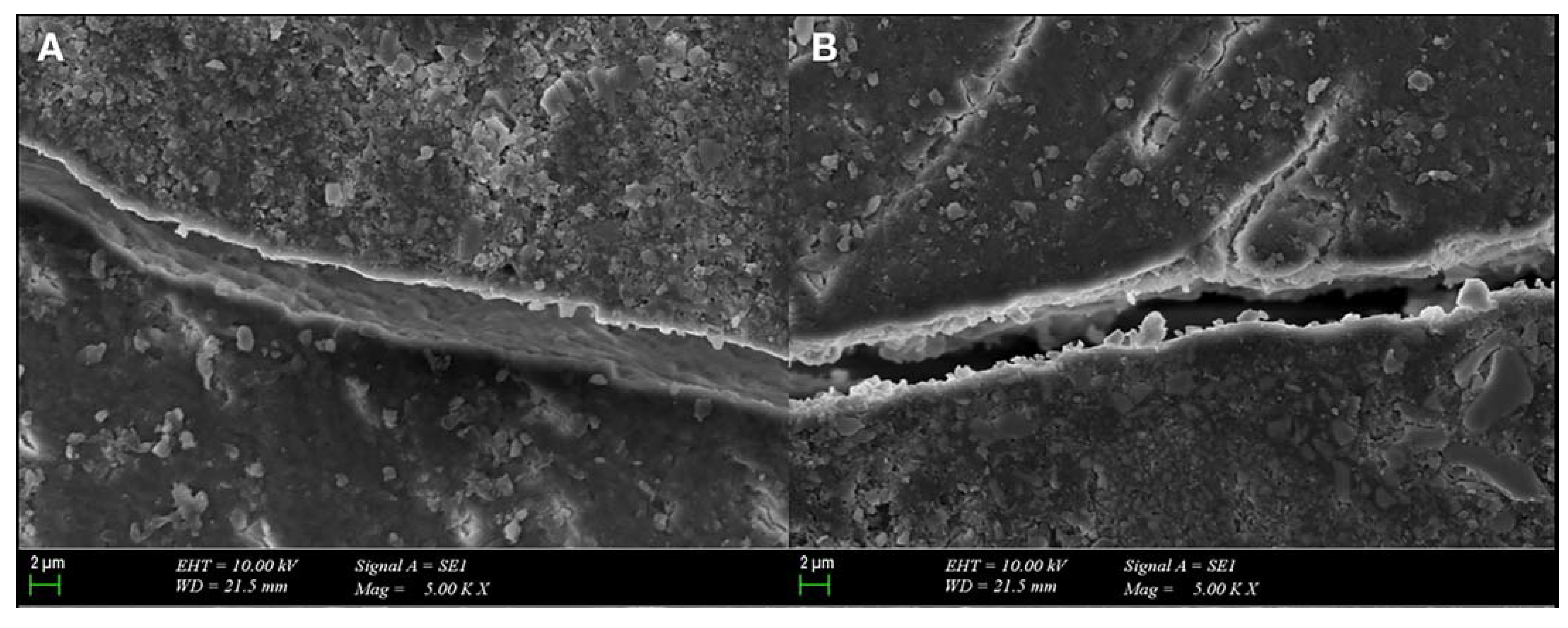
3.2. SEM Evaluation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Miletic, V. Development of Dental Composites. In Dental Composite Materials for Direct Restorations; Miletic, V., Ed.; Springer International Publishing: Cham, Germany, 2018; pp. 3–9. [Google Scholar] [CrossRef]
- Nedeljkovic, I.; Teughels, W.; De Munck, J.; Van Meerbeek, B.; Van Landuyt, K.L. Is secondary caries with composites a material-based problem? Dent. Mater. 2015, 31, e247–e277. [Google Scholar] [CrossRef]
- Braga, R.R.; Ferracane, J.L. Alternatives in polymerization contraction stress management. Crit. Rev. Oral Biol. Med. 2004, 15, 176–184. [Google Scholar] [CrossRef]
- Calheiros, F.C.; Sadek, F.T.; Braga, R.R.; Cardoso, P.E. Polymerization contraction stress of low-shrinkage composites and its correlation with microleakage in class V restorations. J. Dent. 2004, 32, 407–412. [Google Scholar] [CrossRef]
- Randolph, L.D.; Palin, W.M.; Leprince, J.G. Composition of Dental Resin-Based Composites for Direct Restorations. In Dental Composite Materials for Direct Restorations; Miletic, V., Ed.; Springer International Publishing: Cham, Germany, 2018; pp. 11–24. [Google Scholar]
- Park, J.; Chang, J.; Ferracane, J.; Lee, I.B. How should composite be layered to reduce shrinkage stress: Incremental or bulk filling? Dent. Mater. 2008, 24, 1501–1505. [Google Scholar] [CrossRef]
- Alqudaihi, F.S.; Cook, N.B.; Diefenderfer, K.E.; Bottino, M.C.; Platt, J.A. Comparison of Internal Adaptation of Bulk-fill and Increment-fill Resin Composite Materials. Oper. Dent. 2019, 44, E32–E44. [Google Scholar] [CrossRef]
- de Veras, B.M.; Guimarães, R.P.; Alves, L.C.; Padilha, R.J.; Fernandes, L.O.; Aguiar, C.M. Evaluation of marginal sealing quality of restorations with low shrinkage composite resins. J. Clin. Exp. Dent. 2020, 12, e1100–e1108. [Google Scholar] [CrossRef]
- Szalewski, L.; Szalewska, M.; Jarosz, P.; Woś, M.; Szymańska, J. Temperature Changes in Composite Materials during Photopolymerization. Appl. Sci. 2021, 11, 474. [Google Scholar]
- Van Ende, A.; De Munck, J.; Lise, D.P.; Van Meerbeek, B. Bulk-Fill Composites: A Review of the Current Literature. J. Adhes. Dent. 2017, 19, 95–109. [Google Scholar] [CrossRef]
- Par, M.; Gamulin, O.; Marovic, D.; Klaric, E.; Tarle, Z. Raman spectroscopic assessment of degree of conversion of bulk-fill resin composites--changes at 24 hours post cure. Oper. Dent. 2015, 40, E92–E101. [Google Scholar] [CrossRef]
- Gauthier, M.A.; Stangel, I.; Ellis, T.H.; Zhu, X.X. Oxygen inhibition in dental resins. J. Dent. Res. 2005, 84, 725–729. [Google Scholar] [CrossRef]
- Kaisarly, D.; El Gezawi, M.; Keßler, A.; Rösch, P.; Kunzelmann, K.H. Shrinkage vectors in flowable bulk-fill and conventional composites: Bulk versus incremental application. Clin. Oral Investig. 2021, 25, 1127–1139. [Google Scholar] [CrossRef]
- Garcia, D.; Yaman, P.; Dennison, J.; Neiva, G. Polymerization shrinkage and depth of cure of bulk fill flowable composite resins. Oper. Dent. 2014, 39, 441–448. [Google Scholar] [CrossRef]
- Yap, A.U.; Pandya, M.; Toh, W.S. Depth of cure of contemporary bulk-fill resin-based composites. Dent. Mater. J. 2016, 35, 503–510. [Google Scholar] [CrossRef]
- Par, M.; Repusic, I.; Skenderovic, H.; Sever, E.K.; Marovic, D.; Tarle, Z. Real-time Light Transmittance Monitoring for Determining Polymerization Completeness of Conventional and Bulk Fill Dental Composites. Oper. Dent. 2018, 43, E19–E31. [Google Scholar] [CrossRef]
- Grubbs, T.D.; Vargas, M.; Kolker, J.; Teixeira, E.C. Efficacy of Direct Restorative Materials in Proximal Box Elevation on the Margin Quality and Fracture Resistance of Molars Restored With CAD/CAM Onlays. Oper. Dent. 2020, 45, 52–61. [Google Scholar] [CrossRef]
- Zhang, H. Fracture Resistance of Endodontically Treated Premolar with Deep Class II: In Vitro Evaluation of Different Restorative Procedures. Investig. Clin. 2019, 60, 154–161. [Google Scholar]
- Ferrari, M.; Koken, S.; Grandini, S.; Ferrari Cagidiaco, E.; Joda, T.; Discepoli, N. Influence of cervical margin relocation (CMR) on periodontal health: 12-month results of a controlled trial. J. Dent. 2018, 69, 70–76. [Google Scholar] [CrossRef]
- Scotti, N.; Baldi, A.; Vergano, E.A.; Tempesta, R.M.; Alovisi, M.; Pasqualini, D.; Carpegna, G.C.; Comba, A. Tridimensional Evaluation of the Interfacial Gap in Deep Cervical Margin Restorations: A Micro-CT Study. Oper. Dent. 2020, 45, E227–E236. [Google Scholar] [CrossRef]
- Manhart, J.; Kunzelmann, K.H.; Chen, H.Y.; Hickel, R. Mechanical properties and wear behavior of light-cured packable composite resins. Dent. Mater. 2000, 16, 33–40. [Google Scholar] [CrossRef]
- Moszner, N.; Hirt, T. New polymer-chemical developments in clinical dental polymer materials: Enamel–dentin adhesives and restorative composites. J. Polym. Sci. Part A Polym. Chem. 2012, 50, 4369–4402. [Google Scholar] [CrossRef]
- Yılmaz Atalı, P.; Doğu Kaya, B.; Manav Özen, A.; Tarçın, B.; Şenol, A.A.; Tüter Bayraktar, E.; Korkut, B.; Bilgin Göçmen, G.; Tağtekin, D.; Türkmen, C. Assessment of Micro-Hardness, Degree of Conversion, and Flexural Strength for Single-Shade Universal Resin Composites. Polymers 2022, 14, 4987. [Google Scholar] [CrossRef]
- Yarmohamadi, E.; Jahromi, P.R.; Akbarzadeh, M. Comparison of Cuspal Deflection and Microleakage of Premolar Teeth restored with Three Restorative Materials. J. Contemp. Dent. Pract. 2018, 19, 684–689. [Google Scholar]
- Contreras, S.C.M.; Jurema, A.L.B.; Claudino, E.S.; Bresciani, E.; Caneppele, T.M.F. Monowave and polywave light-curing of bulk-fill resin composites: Degree of conversion and marginal adaptation following thermomechanical aging. Biomater. Investig. Dent. 2021, 8, 72–78. [Google Scholar] [CrossRef]
- Ibrahim, H.A.; Shalaby, M.E.; Abdalla, A.I. Marginal fit of class II cavities restored with bulk-fill composites. Tanta Dent. J. 2018, 15, 1–6. [Google Scholar]
- Paganini, A.; Attin, T.; Tauböck, T.T. Margin Integrity of Bulk-Fill Composite Restorations in Primary Teeth. Materials 2020, 13, 3802. [Google Scholar] [CrossRef]
- Politi, I.; McHugh, L.E.J.; Al-Fodeh, R.S.; Fleming, G.J.P. Modification of the restoration protocol for resin-based composite (RBC) restoratives (conventional and bulk fill) on cuspal movement and microleakage score in molar teeth. Dent. Mater. 2018, 34, 1271–1277. [Google Scholar] [CrossRef]
- McHugh, L.E.J.; Politi, I.; Al-Fodeh, R.S.; Fleming, G.J.P. Implications of resin-based composite (RBC) restoration on cuspal deflection and microleakage score in molar teeth: Placement protocol and restorative material. Dent. Mater. 2017, 33, e329–e335. [Google Scholar] [CrossRef]
- Nawafleh, N.; Hatamleh, M.; Elshiyab, S.; Mack, F. Lithium Disilicate Restorations Fatigue Testing Parameters: A Systematic Review. J. Prosthodont. 2016, 25, 116–126. [Google Scholar] [CrossRef]
- Radhika, M.; Sajjan, G.S.; Kumaraswamy, B.N.; Mittal, N. Effect of different placement techniques on marginal microleakage of deep class-II cavities restored with two composite resin formulations. J. Conserv. Dent. 2010, 13, 9–15. [Google Scholar] [CrossRef]
- Ferracane, J.L.; Hilton, T.J. Polymerization stress—Is it clinically meaningful? Dent. Mater. 2016, 32, 1–10. [Google Scholar] [CrossRef]
- Kleverlaan, C.J.; Feilzer, A.J. Polymerization shrinkage and contraction stress of dental resin composites. Dent. Mater. 2005, 21, 1150–1157. [Google Scholar] [CrossRef]
- Klauer, E.; Belli, R.; Petschelt, A.; Lohbauer, U. Mechanical and hydrolytic degradation of an Ormocer®-based Bis-GMA-free resin composite. Clin. Oral Investig. 2019, 23, 2113–2121. [Google Scholar] [CrossRef]
- Juloski, J.; KÖken, S.; Ferrari, M. No correlation between two methodological approaches applied to evaluate cervical margin relocation. Dent. Mater. J. 2020, 39, 624–632. [Google Scholar] [CrossRef]
- Moon, W.; Chung, S.H.; Chang, J. Effect of Deep Margin Elevation on Interfacial Gap Development of CAD/CAM Inlays after Thermomechanical Cycling. Oper. Dent. 2021, 46, 529–536. [Google Scholar] [CrossRef]
- Samartzi, T.K.; Papalexopoulos, D.; Ntovas, P.; Rahiotis, C.; Blatz, M.B. Deep Margin Elevation: A Literature Review. Dent. J. 2022, 10, 48. [Google Scholar] [CrossRef]
- Lassila, L.V.; Nagas, E.; Vallittu, P.K.; Garoushi, S. Translucency of flowable bulk-filling composites of various thicknesses. Chin. J. Dent. Res. 2012, 15, 31–35. [Google Scholar]
- Leprince, J.G.; Palin, W.M.; Vanacker, J.; Sabbagh, J.; Devaux, J.; Leloup, G. Physico-mechanical characteristics of commercially available bulk-fill composites. J. Dent. 2014, 42, 993–1000. [Google Scholar] [CrossRef]
- Hoseinifar, R.; Mofidi, M.; Malekhosseini, N. The Effect of Occlusal Loading on Gingival Microleakage of Bulk Fill Composites Compared with a Conventional Composite. J. Dent. 2020, 21, 87–94. [Google Scholar] [CrossRef]
- Bucuta, S.; Ilie, N. Light transmittance and micro-mechanical properties of bulk fill vs. conventional resin based composites. Clin. Oral Investig. 2014, 18, 1991–2000. [Google Scholar] [CrossRef]
- Jung, J.H.; Park, S.H. Comparison of Polymerization Shrinkage, Physical Properties, and Marginal Adaptation of Flowable and Restorative Bulk Fill Resin-Based Composites. Oper. Dent. 2017, 42, 375–386. [Google Scholar] [CrossRef]
- Moszner, N.; Fischer, U.K.; Ganster, B.; Liska, R.; Rheinberger, V. Benzoyl germanium derivatives as novel visible light photoinitiators for dental materials. Dent. Mater. 2008, 24, 901–907. [Google Scholar] [CrossRef]
- El-Damanhoury, H.; Platt, J. Polymerization shrinkage stress kinetics and related properties of bulk-fill resin composites. Oper. Dent. 2014, 39, 374–382. [Google Scholar] [CrossRef]
- Ferracane, J.L. Developing a more complete understanding of stresses produced in dental composites during polymerization. Dent. Mater. 2005, 21, 36–42. [Google Scholar] [CrossRef]
- Kinomoto, Y.; Torii, M.; Takeshige, F.; Ebisu, S. Comparison of polymerization contraction stresses between self- and light-curing composites. J. Dent. 1999, 27, 383–389. [Google Scholar] [CrossRef]
- Xu, T.; Li, X.; Wang, H.; Zheng, G.; Yu, G.; Wang, H.; Zhu, S. Polymerization shrinkage kinetics and degree of conversion of resin composites. J. Oral Sci. 2020, 62, 275–280. [Google Scholar] [CrossRef]
- Durner, J.; Schrickel, K.; Watts, D.C.; Ilie, N. Determination of homologous distributions of bisEMA dimethacrylates in bulk-fill resin-composites by GC-MS. Dent. Mater. 2015, 31, 473–480. [Google Scholar] [CrossRef]
- Atai, M.; Watts, D.C.; Atai, Z. Shrinkage strain-rates of dental resin-monomer and composite systems. Biomaterials 2005, 26, 5015–5020. [Google Scholar] [CrossRef]
- Szalewski, L.; Wójcik, D.; Sofińska-Chmiel, W.; Kuśmierz, M.; Różyło-Kalinowska, I. How the Duration and Mode of Photopolymerization Affect the Mechanical Properties of a Dental Composite Resin. Materials 2023, 16, 113. [Google Scholar]



| Material and Manufacturer | Monomer and Filler Composition | |
|---|---|---|
| X-tra fil VOCO, Cuxhaven, Germany | Bis-GMA, TEGDMA, UDMA, barium aluminum silicate, fumed silica, and pigments Filler Content (wt%): 86 | |
| X-tra base VOCO, Cuxhaven, Germany | Bis-EMA, aluminum, and barium silicate Filler Content (wt%): 75 | |
| Tetric N-Ceram Bulk Fill Ivoclar Vivadent, Schaan, Liechtenstein | Bis-GMA, UDMA, barium glass, prepolymer, ytterbium trifluoride, and mixed oxide Filler Content (wt%): 75–77 | |
| Tetric N-Flow Bulk Fill Ivoclar Vivadent, Schaan, Liechtenstein | Bis-GMA, UDMA, TEGDMA, barium glass, ytterbium trifluoride, and copolymers Filler Content (wt%): 68.2 | |
| Admira Fusion x-tra VOCO, Cuxhaven, Germany | Ormocer matrix, silicon dioxide, and glass ceramics Filler Content (wt%): 84 | |
| Admira Fusion x-base VOCO, Cuxhaven, Germany | Ormocer matrix, silicon dioxide, and glass ceramics Filler Content (wt%): 72 | |
| Futurabond U Universal VOCO, Cuxhaven, Germany | HEMA, Bis-GMA, HEDMA, acidic adhesive monomer, UDMA, catalyst, silica nanoparticle, and ethanol | |
| Tetric N-Bond Universal Ivoclar Vivadent, Schaan, Liechtenstein | Phosphoric acid acrylate, HEMA, Bis-GMA, UDMA, MDP, MCAP, D3MA, and ethanol | |
| Light device | Wavelength | Light intensity |
| Valo Cordless (Ultradent, ABD) 3rd Generation | 395–480 nm | Standard mode: 1000 mW/cm2 |
| Coronal Microleakage | |||||||||
| Groups | Score | BFC-4 mm + fBFC-2 mm N(%) | BFC-2 mm + fBFC-4 mm N(%) | p | |||||
| XF + XB (G2-G1) | 0 | 7(70) | 5(55.56) | 0.288 | |||||
| 1 | 3(30) | 2(22.22) | |||||||
| 2 | 0(0) | 2(22.22) | |||||||
| AFX + AFB (G6-G5) | 0 | 9(90) | 8(80) | 0.531 | |||||
| 1 | 1(10) | 2(20) | |||||||
| TNB + TFB * (G4-G3) | 0 | 6(75) | 3(33.33) | 0.086 | |||||
| 1 | 2(25) | 6(66.67) | |||||||
| Gingival microleakage | |||||||||
| Gingival–Enamel microleakage | Gingival–Cementum microleakage | ||||||||
| Groups | Score | BFC-4 mm + fBFC-2 mmN(%) | BFC-2 mm + fBFC-4 mm N(%) | p | Groups | Score | BFC-4 mm + fBFC-2 mm N(%) | BFC-2 mm + fBFC-4 mm N(%) | p |
| XF + XB (G2-G1) | 0 | 7(70) | 4(44.44) | 0.428 | XF + XB (G2-G1) | 0 | 5(50) | 3(33.33) | 0.604 |
| 1 | 1(10) | 1(11.11) | 1 | 1(10) | 0(0) | ||||
| 2 | 2(20) | 2(22.22) | 2 | 2(20) | 3(33.33) | ||||
| 3 | 0(0) | 2(22.22) | 3 | 2(20) | 3(33.33) | ||||
| AFX + AFB (G6-G5) | 0 | 8(80) | 5(50) | 0.113 | AFX + AFB (G6-G5) | 0 | 4(40) | 3(30) | 0.481 |
| 1 | 1(10) | 0(0) | 1 | 2(20) | 1(10) | ||||
| 2 | 1(10) | 5(50) | 2 | 4(40) | 4(40) | ||||
| 3 | 0(0) | 0(0) | 3 | 0(0) | 2(20) | ||||
| TNB + TFB (G4-G3) | 0 | 5(62.50) | 2(22.22) | 0.257 | TNB + TFB (G4-G3) | 0 | 3(37.50) | 0(0) | 0.018 |
| Coronal Microleakage | Gingival–Enamel Microleakage | Gingival–Cementum Microleakage | ||||
|---|---|---|---|---|---|---|
| BFC-2 mm + fBFC-4 mm | BFC-4 mm + fBFC-2 mm | BFC-2 mm + fBFC-4 mm | BFC-4 mm + fBFC-2 mm | BFC-2 mm + fBFC-4 mm | BFC-4 mm + fBFC-2 mm | |
| XF + XB/AFX + AFB/TNB + TFB | 0.048 | 0.529 | 0.112 | 0.935 | 0.563 | 0.529 |
| XF + XB/AFX + AFB | 0.266 | 0.582 | 0.225 | 0.818 | 0.731 | 0.374 |
| XF + XB/TNB + TFB | 0.105 | 0.998 | 0.423 | 0.945 | 0.232 | 0.416 |
| AFX + AFB/TNB + TFB | 0.039 | 0.558 | 0.058 | 0.666 | 0.305 | 0.968 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Şenol, A.A.; Karabulut Gençer, B.; Tarçın, B.; Kahramanoğlu, E.; Yılmaz Atalı, P. Microleakage and Marginal Integrity of Ormocer/Methacrylate-Based Bulk-Fill Resin Restorations in MOD Cavities: SEM and Stereomicroscopic Evaluation. Polymers 2023, 15, 1716. https://doi.org/10.3390/polym15071716
Şenol AA, Karabulut Gençer B, Tarçın B, Kahramanoğlu E, Yılmaz Atalı P. Microleakage and Marginal Integrity of Ormocer/Methacrylate-Based Bulk-Fill Resin Restorations in MOD Cavities: SEM and Stereomicroscopic Evaluation. Polymers. 2023; 15(7):1716. https://doi.org/10.3390/polym15071716
Chicago/Turabian StyleŞenol, Aslı A., Büşra Karabulut Gençer, Bilge Tarçın, Erkut Kahramanoğlu, and Pınar Yılmaz Atalı. 2023. "Microleakage and Marginal Integrity of Ormocer/Methacrylate-Based Bulk-Fill Resin Restorations in MOD Cavities: SEM and Stereomicroscopic Evaluation" Polymers 15, no. 7: 1716. https://doi.org/10.3390/polym15071716
APA StyleŞenol, A. A., Karabulut Gençer, B., Tarçın, B., Kahramanoğlu, E., & Yılmaz Atalı, P. (2023). Microleakage and Marginal Integrity of Ormocer/Methacrylate-Based Bulk-Fill Resin Restorations in MOD Cavities: SEM and Stereomicroscopic Evaluation. Polymers, 15(7), 1716. https://doi.org/10.3390/polym15071716








