Micro-CT Marginal and Internal Fit Evaluation of CAD/CAM High-Performance Polymer Onlay Restorations
Abstract
1. Introduction
2. Materials and Methods
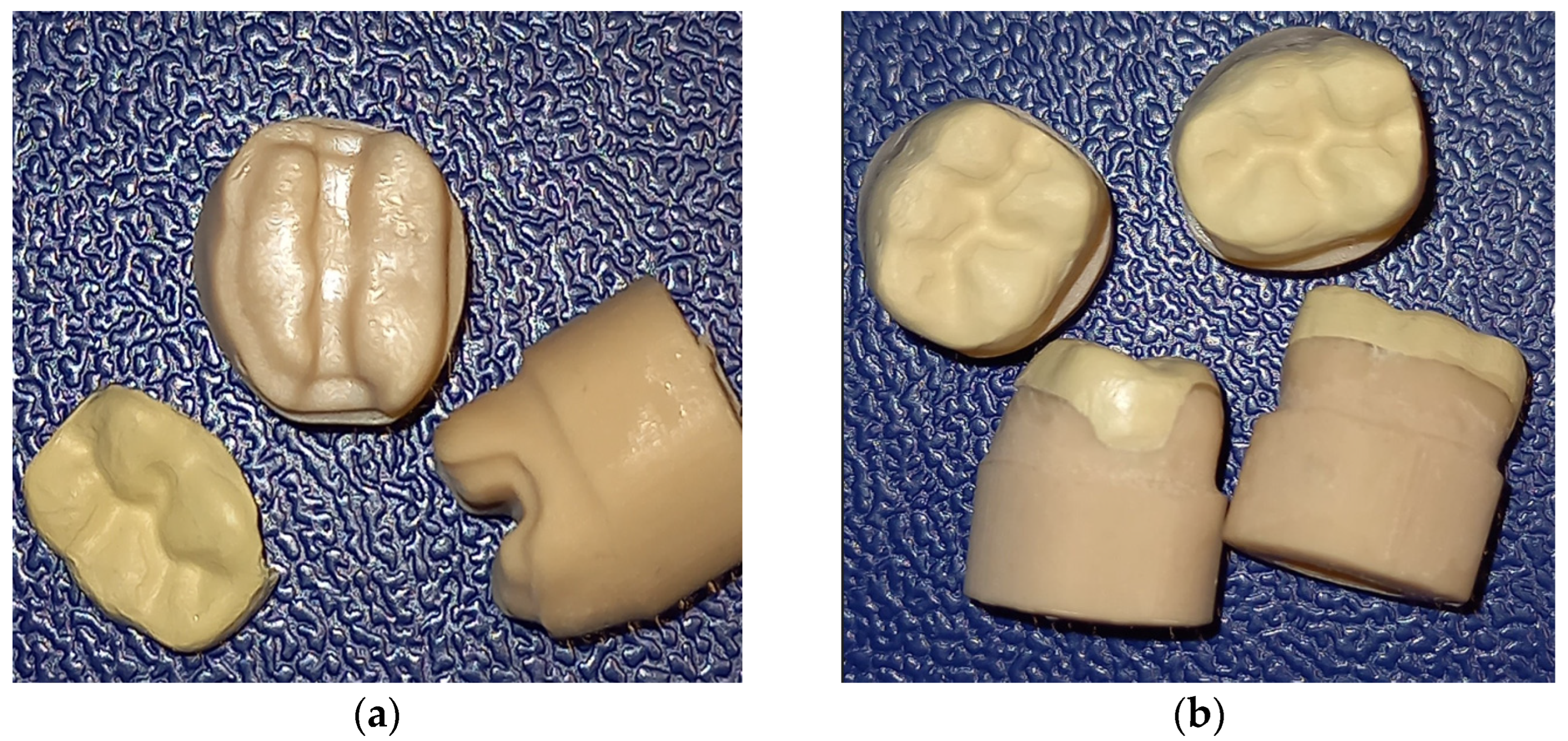
2.1. Onlay Preparation Design
2.2. CAD/CAM
2.3. Cementation Technique
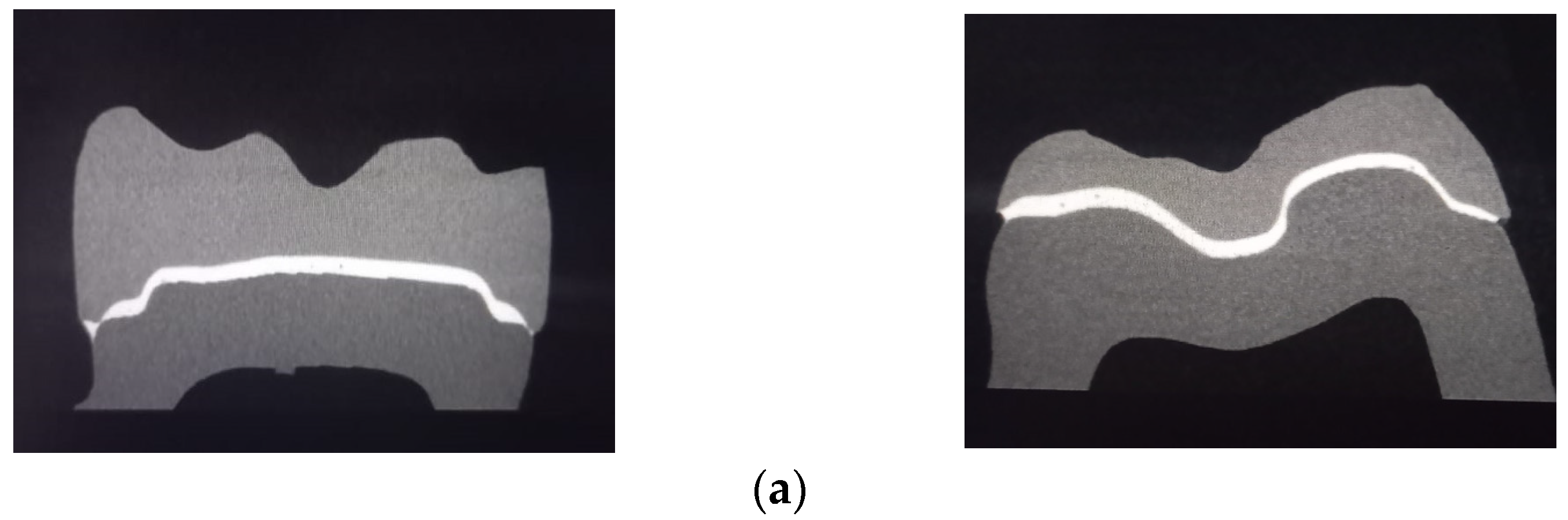
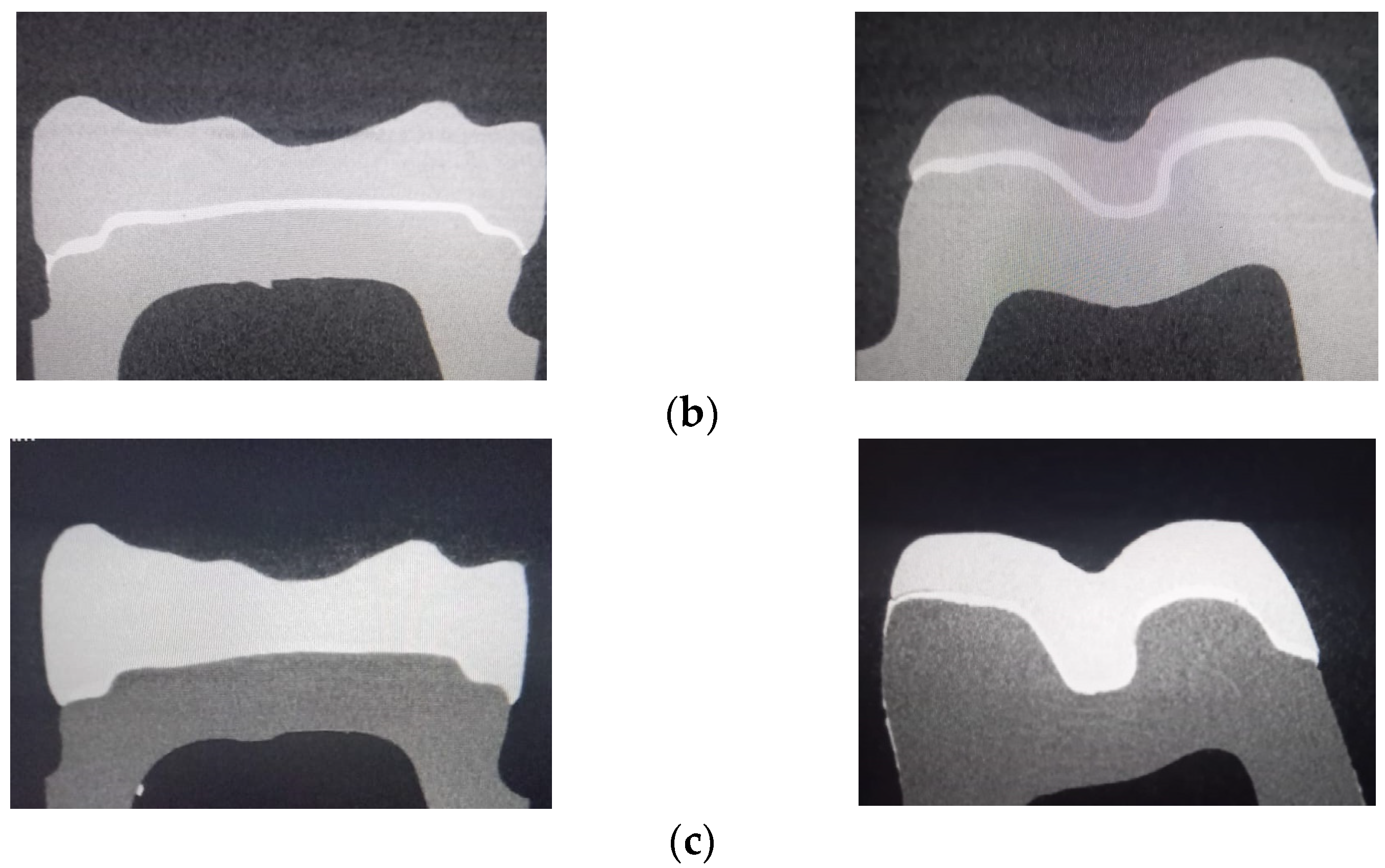
2.4. Micro-CT Analysis
2.5. Statistical Analysis
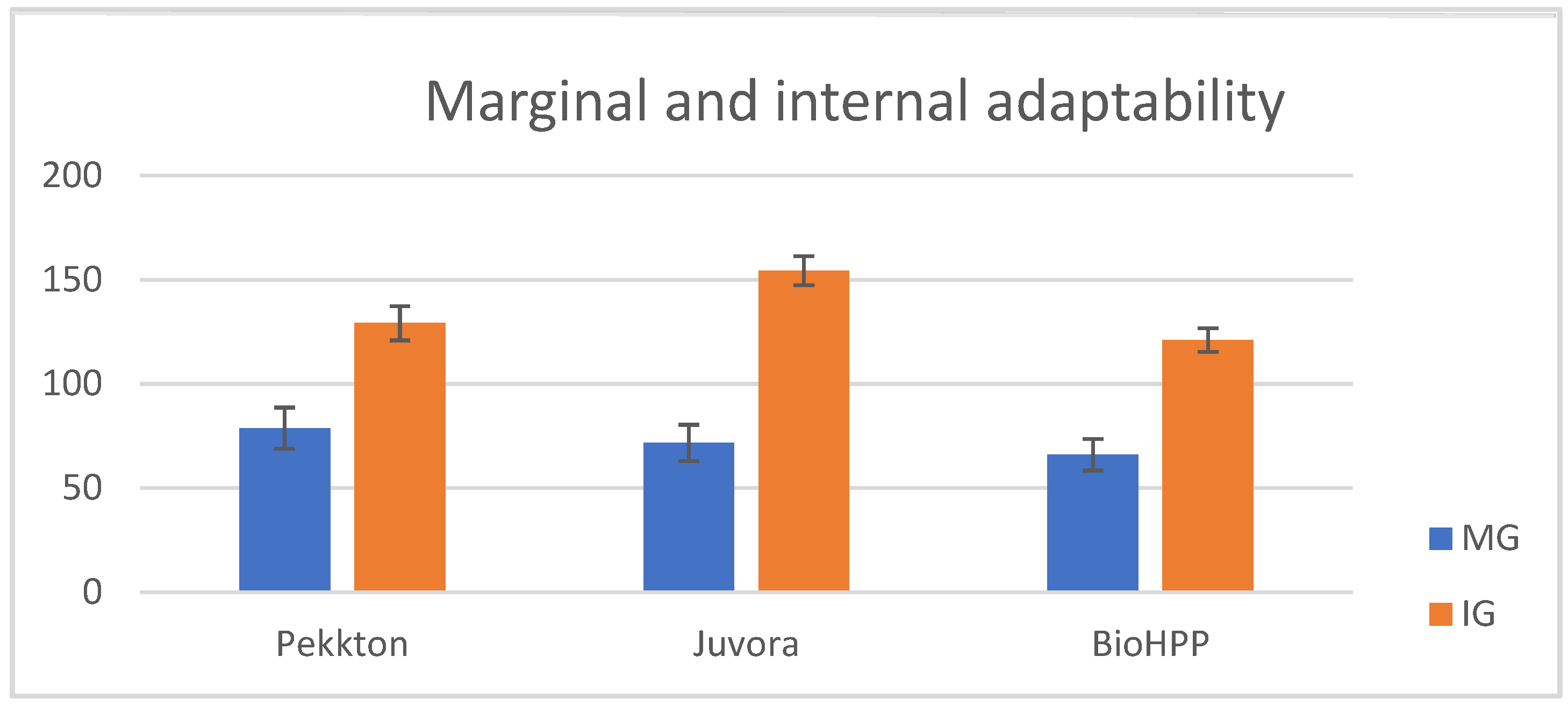
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Donovan, T.E. Factors essential for successful all-ceramic restorations. J. Am. Dent. Assoc. 2008, 139, S14–S18. [Google Scholar] [CrossRef] [PubMed]
- Hamza, T.A.; Ezzat, H.A.; El-Hossary, M.M.; Katamish, H.A.; Shokry, T.E.; Rosenstiel, S.F. Accuracy of ceramic restorations made with two CAD/CAM systems. J. Prosthet. Dent. 2013, 109, 83–87. [Google Scholar] [CrossRef] [PubMed]
- Holmes, J.R.; Bayne, S.C.; Holland, G.A.; Sulik, W.D. Considerations in measurement of marginal fit. J. Prosthet. Dent. 1989, 62, 405–408. [Google Scholar] [CrossRef] [PubMed]
- Mously, H.A.; Finkelman, M. Marginal and internal adaptation of ceramic crown restorations fabricated with CAD/CAM technology and the heat-press technique. J. Prosthet. Dent. 2014, 112, 249–256. [Google Scholar] [CrossRef]
- Bayrak, A.; Akat, B.; Ocak, M.; Kιlιçarslan, M.A.; Özcan, M. Microcomputed tomography analysis of fit of ceramic inlays produced with different CAD software programs. Eur. J. Prosthodont. Restor. Dent. 2021, 29, 29. [Google Scholar]
- Contrepois, M.; Soenen, A.; Bartala, M.; Laviole, O. Marginal adaptation of ceramic crowns: A systematic review. J. Prosthet. Dent. 2013, 110, 447–454. [Google Scholar] [CrossRef] [PubMed]
- Goujat, A.; Abouelleil, H.; Colon, P.; Jeannin, C.; Pradelle, N.; Seux, D.; Grosgogeat, B. Marginal and internal fit of CAD-CAM inlay/onlay restorations: A systematic review of in vitro studies. J. Prosthet. Dent. 2019, 121, 590–597. [Google Scholar] [CrossRef]
- Cunali, R.S.; Saab, R.C.; Correr, G.M.; Da Cunha, L.F.; Ornaghi, B.P.; Gonzaga, C.C.; Ritter, A.V. Marginal and internal adaptation of zirconia crowns: A comparative study of assessment. Braz. Dent. J. 2017, 28, 467–473. [Google Scholar] [CrossRef]
- Abduo, J.; Lions, K.; Bennamoun, M. Trends in computer-aided manufacturing in prosthodontics: A review of the available streams. Int. J. Dent. 2014, 78, 39–48. [Google Scholar] [CrossRef]
- Chu, J.; Bennani, V.; Aarts, J.; Chandler, N.; Lowe, B. The effect of different geometric shapes and angles on the fracture strength of IPS e.max computer-aided designed ceramic onlays: An in vitro study. J. Conserv. Dent. 2018, 21, 210–215. [Google Scholar]
- Nawafleh, N.A.; Mack, F.; Evans, J.; Hatamleh, M.M. Accuracy andreliability of methods to measure marginal adaptation of crowns and FDPs: A literature review. J. Prosthodont. 2013, 22, 419–428. [Google Scholar] [CrossRef]
- Behr, M.; Hansmann, M.; Rosentritt, M.; Handel, G. Marginal adaptation of three self-adhesive resin cements vs. a well-tried adhesive luting agent. Clin. Oral Investig. 2009, 13, 459–464. [Google Scholar] [CrossRef]
- Lutz, F.; Krejci, I.; Barbakow, F. Quality and durability of marginal adaptation in bonded composite restorations. Dent. Mater. 1991, 7, 107–113. [Google Scholar] [CrossRef]
- Schmidlin, P.R.; Huber, T.; Göhring, T.N.; Attin, T.; Bindl, A. Effects of total and selective bonding on marginal adaptation and microleakage of Class I resin composite restorations in vitro. Oper. Dent. 2008, 33, 629–635. [Google Scholar] [CrossRef]
- Mörmann, W.; Wolf, D.; Ender, A.; Bindl, A.; Göhring, T.; Attin, T. Effect of two-self-adhesive cements on marginal adaptation and strength of esthetic ceramic CAD/CAM molar crowns. J. Prosthodont. 2009, 18, 403–410. [Google Scholar] [CrossRef]
- Mörmann, W.H. The evolution of the CEREC system. J. Am. Dent. Assoc. 2006, 137, 7S–13S. [Google Scholar] [CrossRef] [PubMed]
- Magne, P.; Knezevic, A. Simulated fatigue resistance of composite resin versus porcelain CAD/CAM overlay restorations on endodontically treated molars. Quintessence Int. 2009, 40, 125–133. [Google Scholar] [PubMed]
- Fasbinder, D.J.; Dennison, J.B.; Heys, D.R.; Lampe, K. The clinical performance of CAD/CAM-generated composite inlays. J. Am. Dent. Assoc. 2005, 136, 1714–1723. [Google Scholar] [CrossRef] [PubMed]
- Stawarczyk, B.; Ender, A.; Trottmann, A.; Özcan, M.; Fischer, J.; Hämmerle, C.H.F. Load-bearing capacity of CAD/CAM milled poly meric three-unit fixed dental prostheses: Effect of aging regimens. Clin. Oral Investig. 2012, 16, 1669–1677. [Google Scholar] [CrossRef] [PubMed]
- Craig, R.G.; Powers, J.M.; Wataha, J.C. Dental Materials, Properties and Manipulation, 8th ed.; Mosby: St. Louis, MO, USA, 2004; pp. 23–26. [Google Scholar]
- Goncu Basaran, E.; Ayna, E.; Vallittu, P.K.; Lassila, L.V. Load-bearing capacity of handmade and computer-aided design—Computer-aided manufacturing-fabricated three-unit fixed dental prostheses of particulate filler composite. Acta Odontol. Scand. 2011, 69, 144–150. [Google Scholar] [CrossRef]
- Magne, P.; Knezevic, A. Thickness of CAD-CAM composite resin overlays influences fatigue resistance of endodontically treated premolars. Dent. Mater. 2009, 25, 1264–1268. [Google Scholar] [CrossRef] [PubMed]
- Anusavice, K.J.; Philips, R. Philips’ Science of Dental Materials, 11th ed.; Elsevier: St. Louis, MO, USA, 2003. [Google Scholar]
- Meyers, M.A.; Chen, P.Y.; Lin, A.Y.M.; Seki, Y. Biological materials: Structure and mechanical properties. Prog. Mater. Sci. 2008, 53, 1–206. [Google Scholar] [CrossRef]
- Frankenberger, R.; Kramer, N.; Appelt, A.; Lohbauer, U.; Naumann, M.; Roggendorf, M.J. Chairside vs. labside ceramic inlays: Effect of temporary restoration and adhesive luting on enamel cracks and marginal integrity. Dent. Mater. 2011, 27, 892–898. [Google Scholar] [CrossRef] [PubMed]
- Keshvad, A.; Hooshmand, T.; Asefzadeh, F.; Khalilinejad, F.; Alihemmati, M.; Van Noort, R. Marginal gap, internal fit, and fracture load of leucite-reinforced ceramic inlays fabricated by CEREC inLab and hot-pressed techniques. J. Prosthodont. 2011, 20, 535–540. [Google Scholar] [CrossRef]
- Alqurashi, H.; Khurshid, Z.; Syed, A.U.Y.; Habib, S.R.; Rokaya, D.; Zafar, M.S. Polyetherketoneketone (PEKK): An emerging biomaterial for oral implants and dental prostheses. J. Adv. Res. 2020, 28, 87–95. [Google Scholar] [CrossRef]
- Benli, M.; EkerGümüş, B. Thermal, structural and morphological characterization of dental polymers for clinical applications. J. Prosthodont. Res. 2021, 65, 176–185. [Google Scholar] [CrossRef]
- esthetic.line Pekkton Ivory. Cendres+Métaux SA-Pekkton® Ivory (cmsa.ch). Available online: https://www.cmsa.ch/index.php?eID=dumpFile&t=f&f=13192&token=02605b17f8e46c6bc1a3f172241de82055b36bd4 (accessed on 2 February 2023).
- Porojan, L.; Toma, F.R.; Vasiliu, R.D.; Topala, F.-I.; Porojan, S.D.; Matichescu, A. Optical Properties and Color Stability of Dental PEEK Related to Artificial Aging and Staining. Polymers 2021, 13, 4102. [Google Scholar] [CrossRef]
- Alexakou, E.; Damanaki, M.; Zoidis, P.; Bakiri, E.; Mouzis, N.; Smidt, G.; Kourtis, S. PEEK High Performance Polymers: A Review of Properties and Clinical Applications in Prosthodontics and Restorative Dentistry. Eur. J. Prosthodont. Restor. Dent. 2019, 27, 113–121. [Google Scholar]
- Papathanasiou, I.; Kamposiora, P.; Papavasiliou, G.; Ferrari, M. The use of PEEK in digital prosthodontics: A narrative review. BMC Oral Health 2020, 20, 217. [Google Scholar] [CrossRef]
- Qin, L.; Yao, S. Review on Development and Dental Applications of Polyetheretherketone-Based Biomaterials and Restorations. Materials 2021, 14, 408. [Google Scholar] [CrossRef]
- Porto, T.S.; Roperto, R.C.; Akkus, A.; Akkus, O.; Teich, S.; Faddoul, F.; Porto-Neto, S.T.; Campos, E.A. Effect of storage and aging conditions on the flexural strength and flexural modulus of CAD/CAM materials. Dent. Mater. J. 2019, 31, 264–270. [Google Scholar] [CrossRef] [PubMed]
- Porojan, L.; Toma, F.R.; Vasiliu, R.D.; Uțu, I.D.; Matichescu, A. Surface Characteristics and Color Stability of Dental PEEK Related to Water Saturation and Thermal Cycling. Polymers 2022, 14, 2144. [Google Scholar] [CrossRef] [PubMed]
- Stawarczyk, B.; Eichberger, M.; Uhrenbacher, J.; Wimmer, T.; Edelhoff, D.; Schmidlin, P.R. Three-unit reinforced polyetheretherketone composite FDPs: Influence of fabrication method on load-bearing capacity and failure types. Dent. Mater. J. 2015, 34, 7–12. [Google Scholar] [CrossRef]
- Skal’s’kyi, V.R.; Makeev, V.F. Alternation of the types of fracture for dentalpolymers in different stages of crack propagation. Mater. Sci. 2015, 50, 836–843. [Google Scholar] [CrossRef]
- Alghazzawi, T.F. Advancements in CAD/CAM technology: Options for practical implementation. J. Prosthodont. Res. 2016, 116, 253–259. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Jeong, J.H.; Lee, J.H.; Cho, H.W. Fit of lithium disilicate crowns fabricated from conventional and digital impressions assesed with micro-CT. J. Prosthet. Dent. 2016, 116, 551–557. [Google Scholar] [CrossRef]
- Lee, J.J.; Jeong, I.D.; Park, J.K.; Jeong, J.H.; Kim, J.H.; Kim, W.C. Accuracy of single-abutment digital cast obtained using intraoral and cast scanners. J. Prosthet. Dent. 2017, 117, 253–259. [Google Scholar] [CrossRef]
- Mehl, A.; Ender, A.; Mormann, W.; Attin, T. Accuracy testing of a new intra-oral 3D camera. Int. J. Comput. Dent. 2009, 12, 11–28. [Google Scholar]
- Shim, J.S.; Lee, J.S.; Lee, J.Y.; Choi, Y.J.; Shin, S.W.; Ryu, J.J. Effect of software version and parameter settings on the marginal and internal adaptation of crowns fabricated with the CAD/CAM system. J. Appl. Oral Sci. 2015, 23, 515–522. [Google Scholar] [CrossRef]
- Beuer, F.; Schweiger, J.; Edelhoff, D. Digital dentistry: An overview of recent developments for CAD/CAM generated restorations. Br. Dent. J. 2008, 204, 505–511. [Google Scholar] [CrossRef] [PubMed]
- Laurent, M.; Scheer, P.; Dejou, J.; Laborde, G. Clinical evaluation of the marginal fit of cast crowns–validation of the silicone replica method. J. Oral Rehabil. 2008, 35, 116–122. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Xie, H.; Sadr, A.; Chung, K.H. Evaluation of internal fit and marginal adaptation of provisional crowns fabricated with three different techniques. Sensors 2021, 21, 740. [Google Scholar] [CrossRef] [PubMed]
- Goujat, A.; Abouelleil, H.; Colon, P.; Jeannin, C.; Pradelle, N.; Seux, D.; Grosgogeat, B. Mechanical properties and internal fit of 4 CAD-CAM block materials. J. Prosthet. Dent. 2018, 119, 384–389. [Google Scholar] [CrossRef]
- Svanborg, P. A systematic review on the accuracy of zirconia crowns and fixed dental prostheses. Biomater. Investig. Dent. 2020, 7, 9–15. [Google Scholar] [CrossRef]
- What Is Micro-CT? An Introduction. Available online: https://www.microphotonics.com/ (accessed on 8 February 2023).
- Boitelle, P.; Mawussi, B.; Tapie, L.; Fromentin, O. A systematic rewiew of CAD/CAM fit restoration evaluations. J. Oral Rehabil. 2014, 41, 853–874. [Google Scholar] [CrossRef] [PubMed]
- Groten, M.; Axmann, D.; Probster, L.; Weber, H. Determination of the minimum number of marginal gap measurements required for practical in vitro testing. J. Prosthet. Dent. 2000, 83, 40–49. [Google Scholar] [CrossRef]
- Ender, A.; Zimmermann, M.; Attin, T.; Mehl, A. In vivo precision of conventional and digital methods obtaining quadrant dental impressions. Clin. Oral Investig. 2015, 17, 63–71. [Google Scholar] [CrossRef]
- Ting-Shu, S.; Jian, S. Intraoral digital impression technique: A review. J. Prosthodont. 2014, 24, 313–321. [Google Scholar] [CrossRef]
- Kirsch, C.; Ender, A.; Attin, T.; Mehl, A. trueness of four different milling procedures used in dental CAD/CAM systems. Clin. Oral Investig. 2017, 28, 551–558. [Google Scholar] [CrossRef]
- Luthardt, R.; Weber, A.; Rudolph, H.; Schone, C.; Quaas, S.; Walter, M. Design and production of dental prosthetic restorations: Basic research on dental CAD/CAM technology. J. Int. Comput. Dent. 2002, 5, 165–176. [Google Scholar]
- Vasiliu, R.D.; Porojan, S.D.; Porojan, L. In vitro study of comparative evaluation of marginal and internal fit between heat-pressed and CAD/CAM monolithic glass-ceramic restorations after thermal aging. Materials 2020, 13, 4239. [Google Scholar] [CrossRef] [PubMed]
- Pagano, S.; Moretti, M.; Marsili, R.; Ricci, A.; Barraco, G.; Cianetti, S. Evaluation of the Accuracy of Four Digital Methods by Linear and Volumetric Analysis of Dental Impressions. Materials 2019, 12, 1958. [Google Scholar] [CrossRef] [PubMed]
- Yildiz, C.; Vanlioglu, B.A.; Evren, B.; Uludamar, A.; Ozkan, Y.K. Marginal-internal adaptation and fracture resistance of CAD/CAM crown restorations. Dent. Mater. J. 2013, 32, 42–47. [Google Scholar] [CrossRef] [PubMed]
- Ekici, Z.; Bilecenoglu, B.; Ocak, M. Microcomputed tomography evaluation of the marginal and internal fit of crown and inlay restorations fabricated via different digital scanners belonging to the same CAD/CAM system. Digit. Dent. Technol. 2021, 34, 381–387. [Google Scholar] [CrossRef]
- Prudente, M.S.; Davi, L.R.; Nabbout, K.O.; Prado, C.J.; Pereira, L.M.; Zancopé, K.; Neves, F.D. Influence of scanner, powder applications, and adjustments on CAD/CAM crown misfit. J. Prosthet. Dent. 2018, 119, 377–383. [Google Scholar] [CrossRef] [PubMed]
- Al Hamad, K.Q.; Al-Rashdan, R.B.; Al-Rashdan, B.A.; Baba, N.Z. Effect of milling protocols on trueness and precision of ceramic crowns. J. Prosthodont. 2021, 30, 171–176. [Google Scholar] [CrossRef] [PubMed]
- Alharbi, N.; Alharbi, S.; Cuijpers, V.M.J.I.; Osman, R.B.; Wismeijer, D. Three-dimensional evaluation of marginal and internal fit of 3D-printed interim restorations fabricated on different finish line designs. J. Prosthodont. Res. 2018, 62, 218–226. [Google Scholar] [CrossRef]
- Alajaji, N.K.; Bardwell, D.; Finkelman, M.; Ali, A. Micro-CT evaluation of ceramic inlay: Comparison of the marginal and internal fit of five and three axis CAM system with a heat press technique. J. Esthet. Restor. Dent. 2017, 29, 49–58. [Google Scholar] [CrossRef]
- Bousnaki, M.; Chatziparaskeva, M.; Bakopoulou, A.; Pissiotis, A.; Koidis, P. Variables affecting the fit of zirconia fixed partial dentures: A systematic review. J. Prosthet. Dent. 2020, 123, 686–692.e8. [Google Scholar] [CrossRef]
- Spitznagel, F.A.; Boldt, J.; Gierthmuehlen, P.C. CAD/CAM ceramic restorative materials for natural teeth. J. Dent. Res. 2018, 97, 108. [Google Scholar] [CrossRef]
- Tedlapu, S.; Hima, B. Evaluation of marginal adaptation and microleakage of all-ceramic crown systems by using two commercially available luting agents-an an in vitro evaluation. Int. J. Curr. Res. 2018, 10, 72760–72765. [Google Scholar]
- Papadiochou, S.; Pissiotis, A.L. Marginal adaptation and CAD-CAM technology: A systematic review of restorative material and fabrication techniques. J. Prosthet. Dent. 2018, 119, 545–551. [Google Scholar] [CrossRef] [PubMed]
- Dahl, B.E.; Dahl, J.E.; Ronold, H.J. Digital evaluation of marginal and internal fit of single-crown fixed dental prostheses. Eur. J. Oral Sci. 2018, 126, 512–517. [Google Scholar] [CrossRef]
- Liang, S.; Yuan, K.S.; Luo, X.; Yu, Z.; Tang, Z. Digital evaluation of absolute marginal discrepancy. A comparison of ceramic crowns fabricated with conventional and digital techniques. J. Prosthet. Dent. 2018, 120, 525–529. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.Y.; Lee, H.N.; Kim, J.H.; Kim, W.C. Evaluation of marginal discrepancy of pressable ceramic veneer fabricated using CAD/CAM system: Additive and subtractive manufacturing. J. Adv. Prosthodont. 2018, 10, 347–353. [Google Scholar] [CrossRef]
- Uzgur, R.; Ercan, E.; Uzgur, Z.; Colak, H.; Yalcin, M.; Ozcan, M. Cement thickness of inlay restoration made of lithium disilicate, polymer-infiltrated ceramic and nano-ceramic CAD/CAM materials evaluated using 3D x-ray micro-computed tomography. J. Prosthodont. 2018, 27, 456–460. [Google Scholar] [CrossRef]



| Material | Manufacturer | Composition |
|---|---|---|
| Pekkton ivory (P) | Cendrez + Metaux, Biel/Bienne, Switzerland | polyetherketoneketone (PEKK) |
| Juvora Natural Dental (J) | Juvora Ltd. Global Technology Center, Lancashire, UK | 100% polyetheretherketone (PEEK) |
| BioHPP shade 2 (B) | Bredent group GmbH & Co.KG, Senden, Germany | 20% ceramic reinforced (0.3–0.5 µm grain size) partially crystalline polyetheretherketone (PEEK) |
| Pekkton (P) | Juvora (J) | BioHPP (B) | ||||
|---|---|---|---|---|---|---|
| Point | Mean ± SD | 95% CI | Mean ± SD | 95% CI | Mean ± SD | 95% CI |
| a | 43.75 ± 5.99 | 31.77–55.73 | 64.38 ± 12.23 | 39.92–88.84 | 61.88 ± 10.73 | 40.42–83.34 |
| b | 195 ± 26.93 | 141.14–248.86 | 197.5 ± 20.16 | 157.18–237.81 | 165 ± 25.73 | 113.54–216.46 |
| c | 197.5 ± 22.78 | 151.95–243.06 | 190 ± 25.74 | 138.52–241.48 | 183.13 ± 26.63 | 129.67–236.39 |
| d | 93.12 ± 19.60 | 53.92–132.32 | 160 ± 20.62 | 118.76–201.24 | 101.25 ± 23.15 | 54.3–147.55 |
| e | 150 ± 28.06 | 93.88–206.12 | 177.5 ± 24.11 | 129.28–225.72 | 145.63 ± 28.50 | 88.63–202.63 |
| f | 195 ± 22.36 | 150.28–239.72 | 196.25 ± 16.54 | 163.17–229.08 | 168.13 ± 26.98 | 114.17–222.09 |
| g | 134.38 ± 24.99 | 84.01–83.98 | 158.75 ± 23.95 | 110–206.65 | 90.63 ± 16 | 58.63–122.63 |
| h | 58.75 ± 12.18 | 34.39–83.11 | 120.63 ± 21.06 | 78.51–162.75 | 89.38 ± 14.78 | 59.82–118.94 |
| i | 73.13 ± 13.56 | 46.01–100.25 | 135 ± 22.64 | 89.72–180.28 | 123.13 ± 25.67 | 71.79–174.47 |
| j | 170 ± 17.68 | 134.64–205.36 | 170 ± 26.09 | 117.82–222.18 | 173.75 ± 28.70 | 116.35–231.15 |
| k | 50 ± 11.18 | 27.64–72.36 | 80 ± 13.23 | 53.54–106.46 | 33.13 ± 8.45 | 16.23–65.59 |
| l | 67.50 ± 10.90 | 45.7–89.3 | 91.25 ± 11.11 | 69.03–113.47 | 30 ± 8.66 | 12.68–47.32 |
| m | 76.25 ± 11.66 | 52.93–59.57 | 63.13 ± 12.10 | 34.93–87.33 | 35 ± 7.91 | 19.18–45.82 |
| n | 116.25 ± 22.88 | 70.49–162.01 | 87.5 ± 16.39 | 54.72–120.28 | 101.25 ± 19 | 63.25–139.25 |
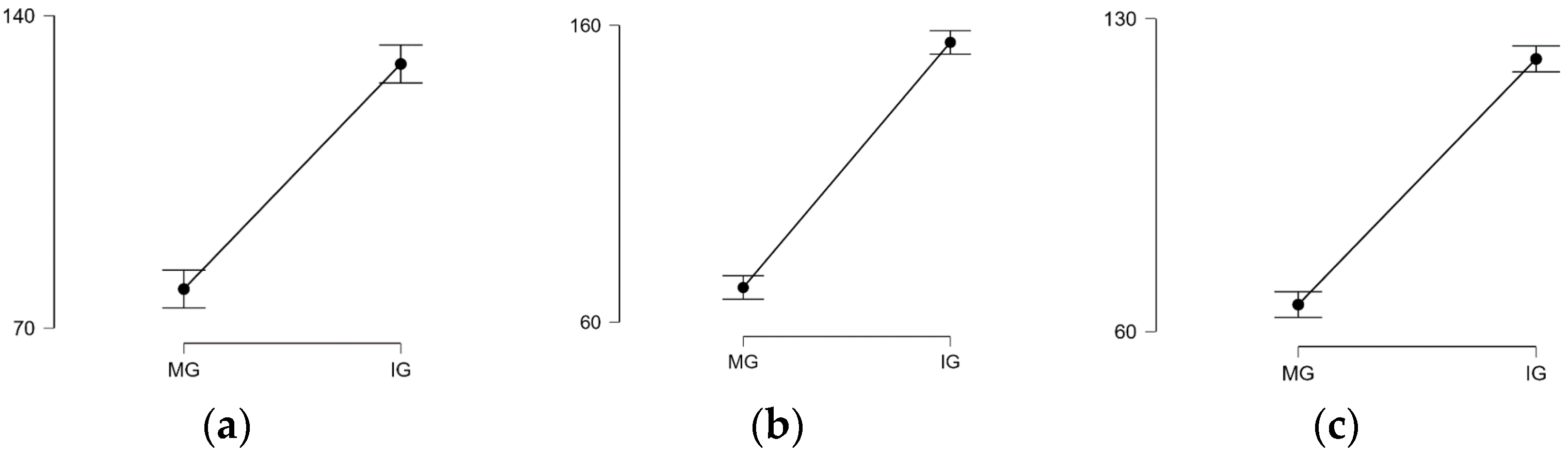
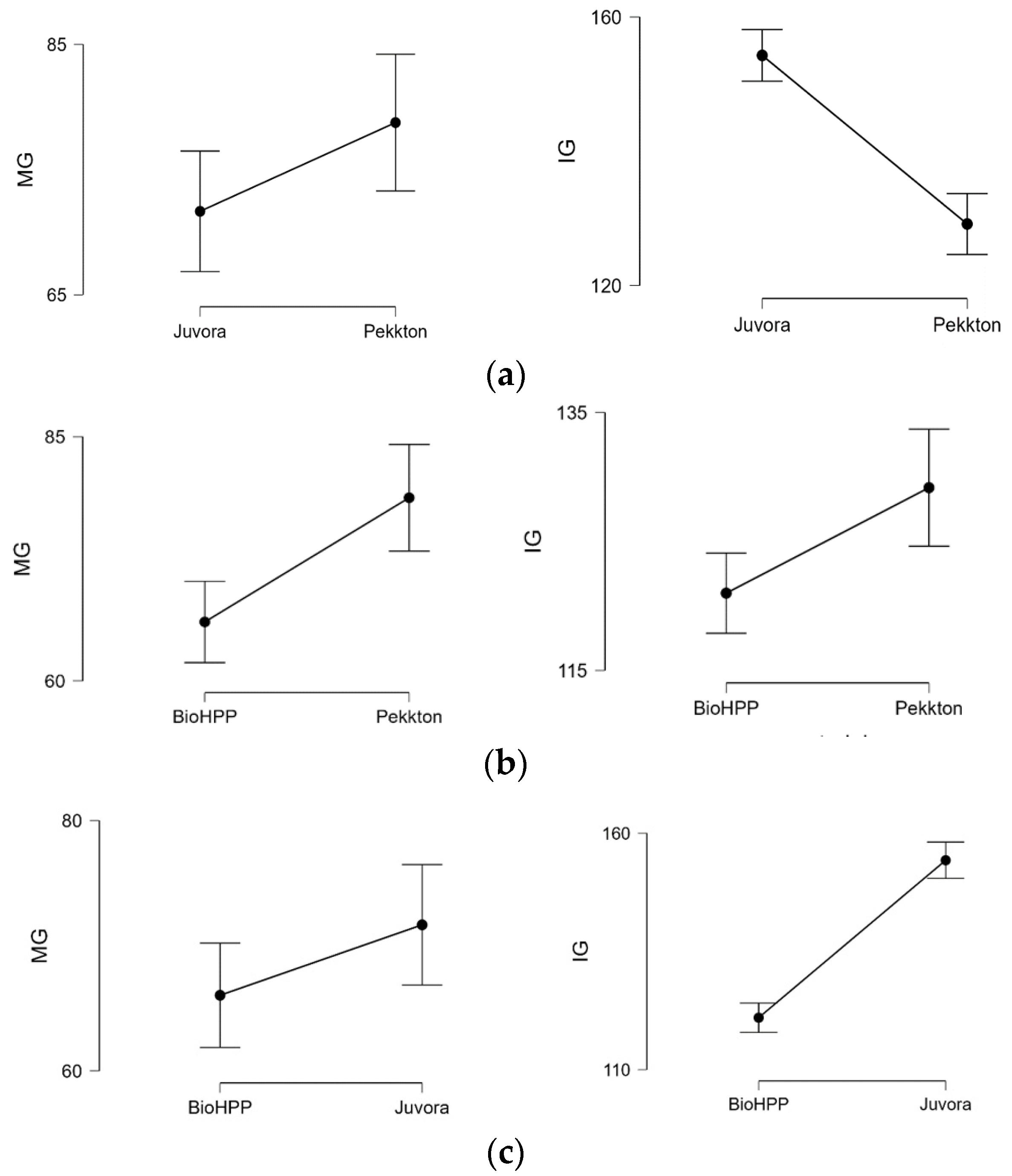
| Mean | Pekkton (P) | Juvora (J) | BioHPP (B) |
|---|---|---|---|
| MG | 78.75 ± 9.92 | 71.67 ± 8.74 | 66.04 ± 7.57 |
| IG | 129.17 ± 8.23 | 154.27 ± 6.98 | 120.99 ± 9.65 |
| MG | IG | |
|---|---|---|
| P-J | p = 0.047 | p < 0.001 |
| P-B | p < 0.001 | p = 0.013 |
| J-B | p = 0.11 | p < 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Toma, F.R.; Moleriu, L.C.; Porojan, L. Micro-CT Marginal and Internal Fit Evaluation of CAD/CAM High-Performance Polymer Onlay Restorations. Polymers 2023, 15, 1715. https://doi.org/10.3390/polym15071715
Toma FR, Moleriu LC, Porojan L. Micro-CT Marginal and Internal Fit Evaluation of CAD/CAM High-Performance Polymer Onlay Restorations. Polymers. 2023; 15(7):1715. https://doi.org/10.3390/polym15071715
Chicago/Turabian StyleToma, Flavia Roxana, Lavinia Cristina Moleriu, and Liliana Porojan. 2023. "Micro-CT Marginal and Internal Fit Evaluation of CAD/CAM High-Performance Polymer Onlay Restorations" Polymers 15, no. 7: 1715. https://doi.org/10.3390/polym15071715
APA StyleToma, F. R., Moleriu, L. C., & Porojan, L. (2023). Micro-CT Marginal and Internal Fit Evaluation of CAD/CAM High-Performance Polymer Onlay Restorations. Polymers, 15(7), 1715. https://doi.org/10.3390/polym15071715







