Influence of Aerosolization on Endothelial Cells for Efficient Cell Deposition in Biohybrid and Regenerative Applications
Abstract
1. Introduction
2. Materials and Methods
2.1. Isolation and Culture of Human Umbilical Vein Endothelial Cells
2.2. Spray Setup and Test Parameters
2.3. Cell Spraying with the Vivostat System
2.4. Viability of Sprayed Cells
2.5. Evaluation of Cell Behaviour
2.5.1. Apoptosis Assay
2.5.2. Necrosis Assay
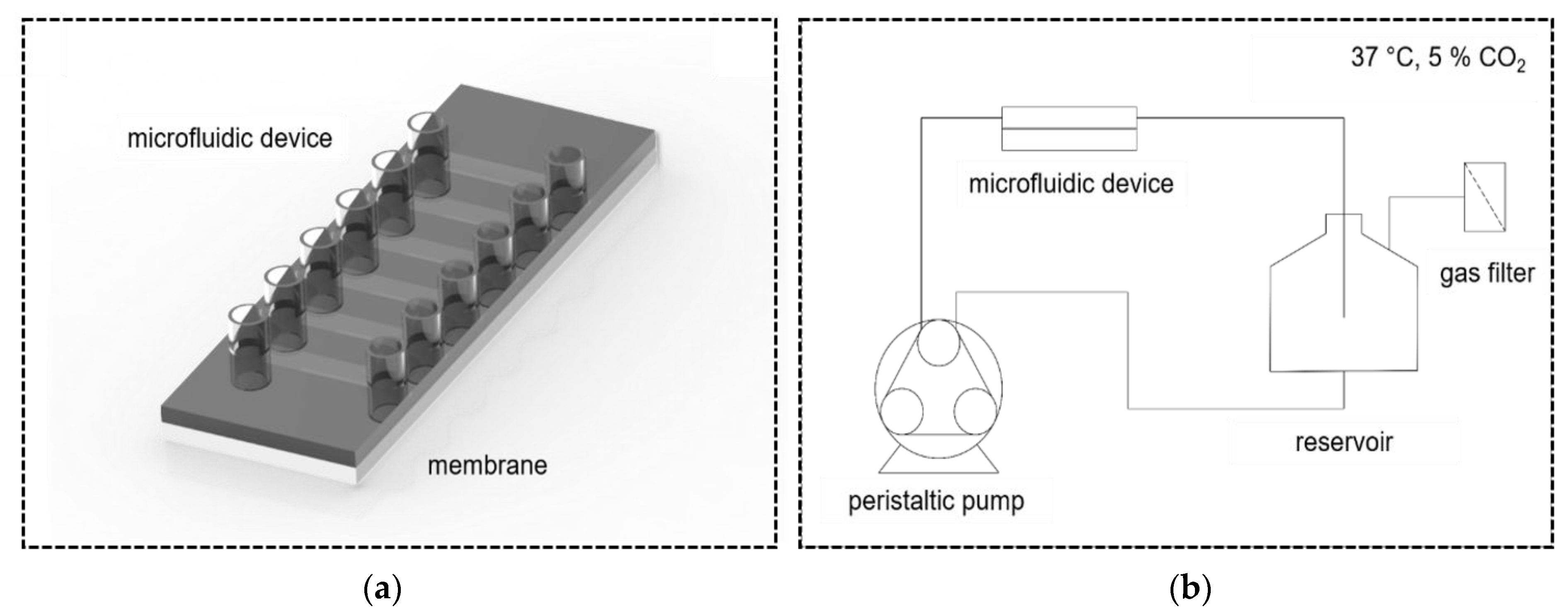
2.6. Static Culture of Endothelial Cells on Gas Exchange Membranes
2.7. Dynamic Culture of Endothelial Cells on Gas Exchange Membranes
2.8. Immunocytochemical Staining
2.9. Quantitative PCR Analysis
2.10. Statistical Analysis
3. Results
3.1. Spray Analysis
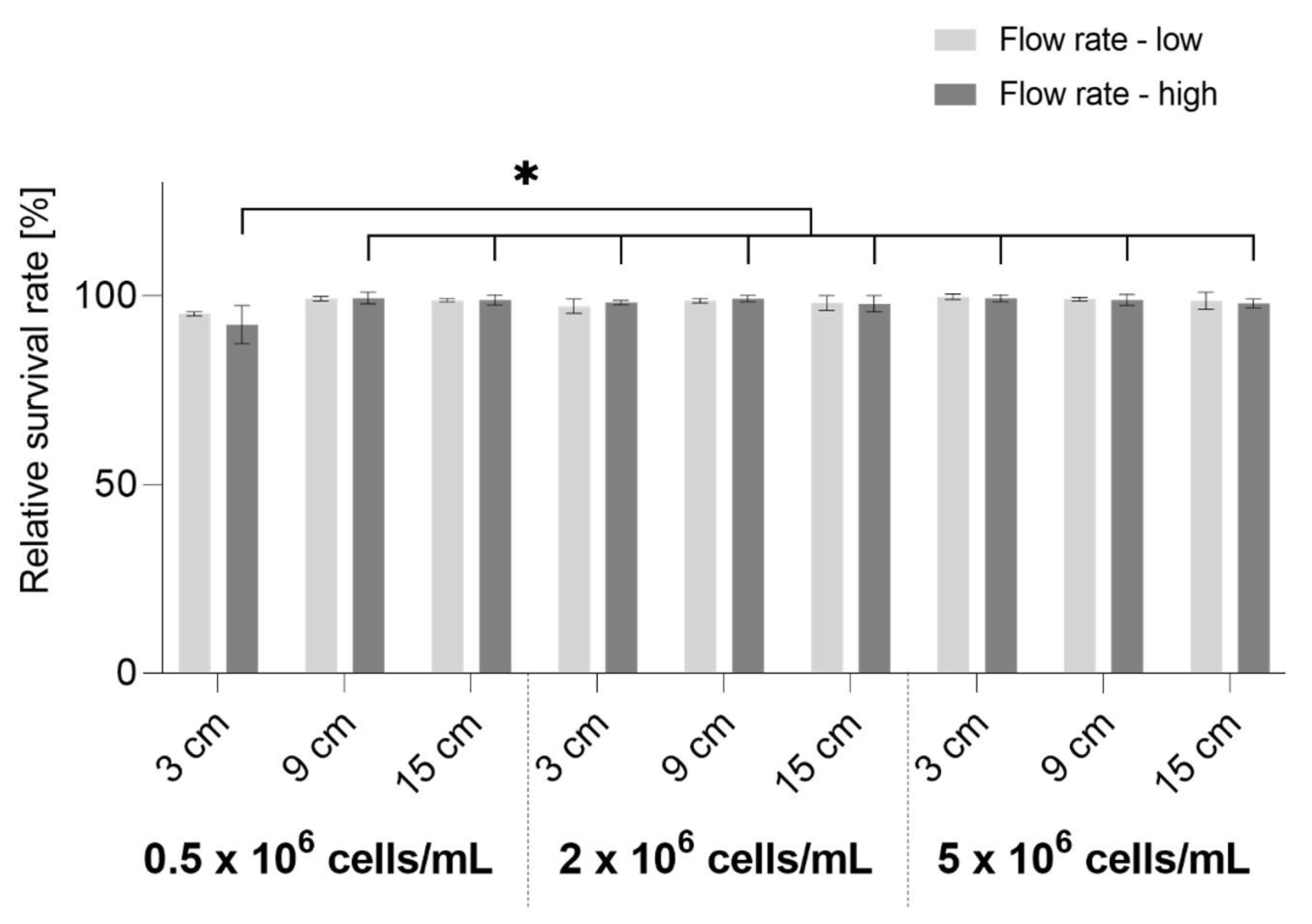
3.2. Cell Survival
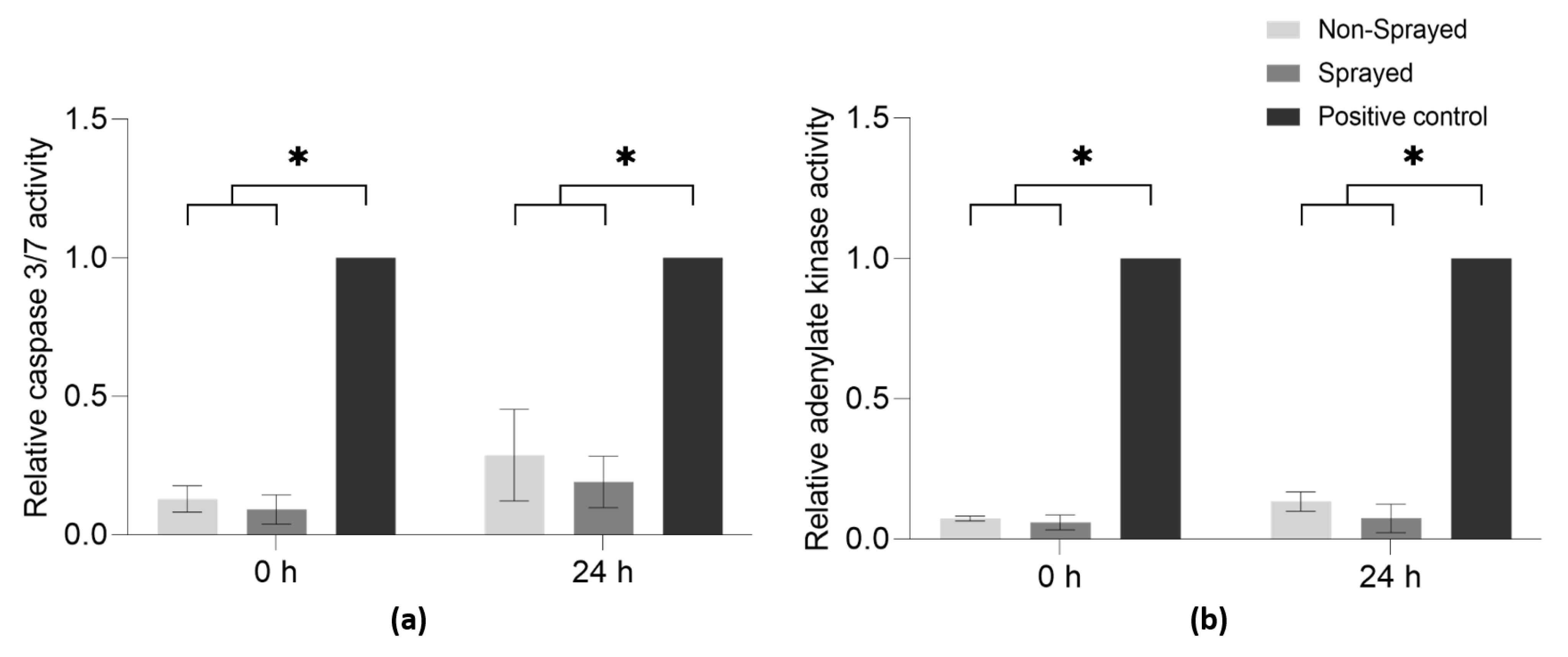
3.3. Cell Behavior
3.4. Static and Dynamic Cultivation of Sprayed Cells
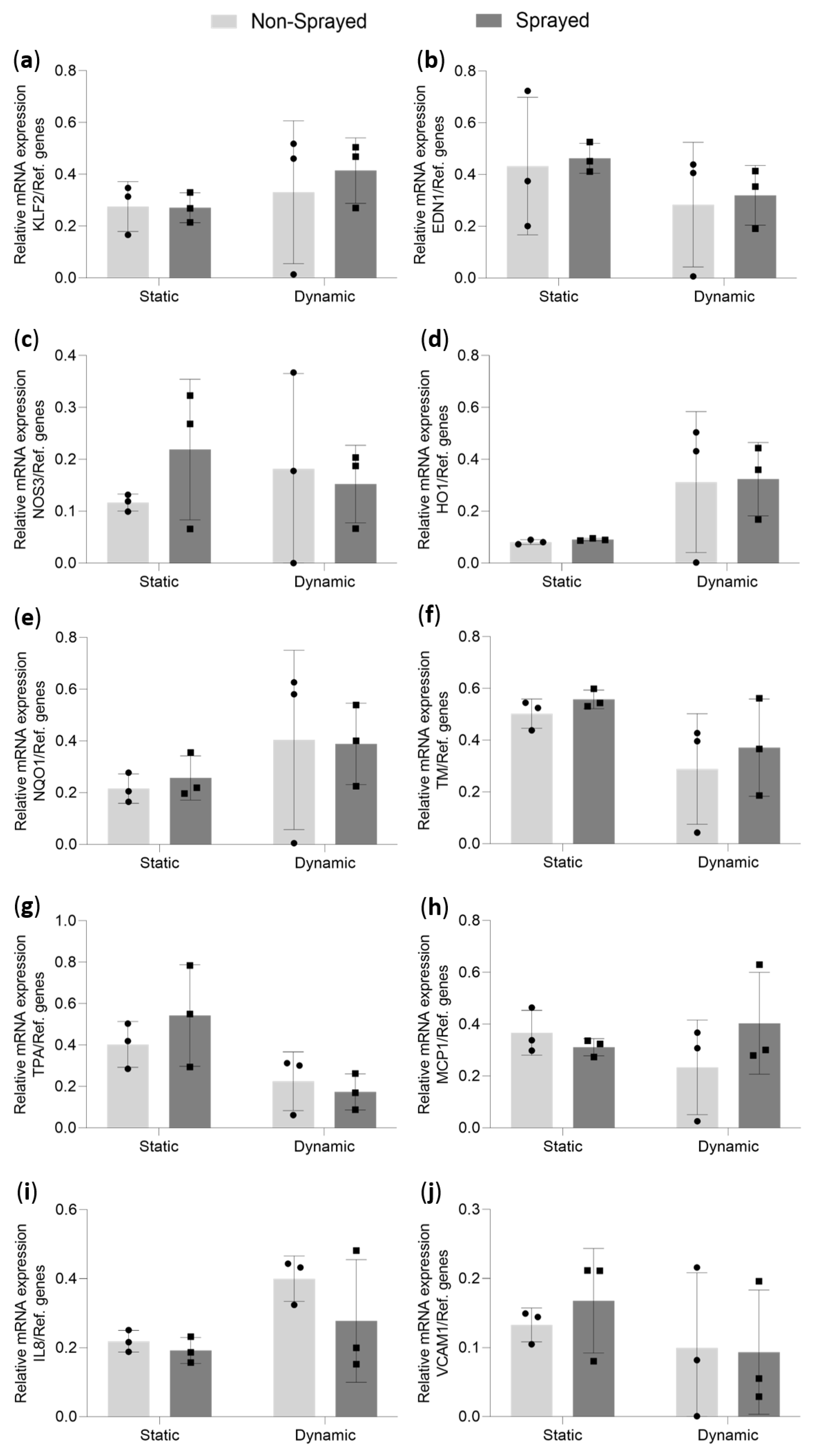
3.5. Quantitative mRNA Analysis of Statically and Dynamically Cultivated Sprayed Cells
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Brodie, D. The Evolution of Extracorporeal Membrane Oxygenation for Adult Respiratory Failure. Ann. Am. Thorac. Soc. 2018, 15 (Suppl. S1), S57–S60. [Google Scholar] [CrossRef] [PubMed]
- Arens, J.; Grottke, O.; Haverich, A.; Maier, L.S.; Schmitz-Rode, T.; Steinseifer, U.; Wendel, H.; Rossaint, R. Toward a Long-Term Artificial Lung. ASAIO J. 2020, 66, 847–854. [Google Scholar] [CrossRef] [PubMed]
- Rajsic, S.; Breitkopf, R.; Jadzic, D.; Popovic Krneta, M.; Tauber, H.; Treml, B. Anticoagulation Strategies during Extracorporeal Membrane Oxygenation: A Narrative Review. J. Clin. Med. 2022, 11, 5147. [Google Scholar] [CrossRef] [PubMed]
- Willers, A.; Arens, J.; Mariani, S.; Pels, H.; Maessen, J.G.; Hackeng, T.M.; Lorusso, R.; Swol, J. New Trends, Advantages and Disadvantages in Anticoagulation and Coating Methods Used in Extracorporeal Life Support Devices. Membranes 2021, 11, 617. [Google Scholar] [CrossRef]
- Pflaum, M.; Peredo, A.S.; Dipresa, D.; De, A.; Korossis, S. Membrane bioreactors for (bio-)artificial lung. In Current Trends and Future Developments on (Bio-) Membranes; Elsevier Science: Amsterdam, The Netherlands, 2020; pp. 45–75. [Google Scholar] [CrossRef]
- Klein, S.; Hesselmann, F.; Djeljadini, S.; Berger, T.; Thiebes, A.L.; Schmitz-Rode, T.; Jockenhoevel, S.; Cornelissen, C.G. EndOxy: Dynamic Long-Term Evaluation of Endothelialized Gas Exchange Membranes for a Biohybrid Lung. Ann. BioMed. Eng. 2020, 48, 747–756. [Google Scholar] [CrossRef]
- Menzel, S.; Finocchiaro, N.; Donay, C.; Thiebes, A.L.; Hesselmann, F.; Arens, J.; Djeljadini, S.; Wessling, M.; Schmitz-Rode, T.; Jockenhoevel, S.; et al. Towards a Biohybrid Lung: Endothelial Cells Promote Oxygen Transfer through Gas Permeable Membranes. BioMed. Res. Int. 2017, 2017, 5258196. [Google Scholar] [CrossRef]
- Dietrich, M.; Finocchiaro, N.; Olszweski, S.; Arens, J.; Schmitz-Rode, T.; Sachweh, J.; Jockenhoevel, S.; Cornelissen, C.G. ENDOXY-Development of a Biomimetic Oxygenator-Test-Device. PLoS ONE 2015, 10, e0142961. [Google Scholar] [CrossRef]
- Zwirner, U.; Hoffler, K.; Pflaum, M.; Korossis, S.; Haverich, A.; Wiegmann, B. Identifying an optimal seeding protocol and endothelial cell substrate for biohybrid lung development. J. Tissue Eng. Regen. Med. 2018, 12, 2319–2330. [Google Scholar] [CrossRef]
- Wiegmann, B.; von Seggern, H.; Hoffler, K.; Korossis, S.; Dipresa, D.; Pflaum, M.; Schmeckebier, S.; Seume, J.; Haverich, A. Developing a biohybrid lung-sufficient endothelialization of poly-4-methly-1-pentene gas exchange hollow-fiber membranes. J. Mech. Behav. BioMed. Mater. 2016, 60, 301–311. [Google Scholar] [CrossRef]
- Kolobow, T.; Gattinoni, L.; Tomlinson, T.; White, D.; Pierce, J. The carbon dioxide membrane lung (CDML): A new concept. ASAIO J. 1977, 23, 17–21. [Google Scholar] [CrossRef]
- Mueller, X.M.; Tevaearai, H.T.; Jegger, D.; Boone, Y.; Augstburger, M.; von Segesser, L.K. Impact of hollow-fiber membrane surface area on oxygenator performance: Dideco D903 Avant versus a prototype with larger surface area. J. Extra Corpor. Technol. 2000, 32, 152–157. [Google Scholar] [PubMed]
- Alabdullh, H.A.; Pflaum, M.; Mälzer, M.; Kipp, M.; Naghilouy-Hidaji, H.; Adam, D.; Kühn, C.; Natanov, R.; Niehaus, A.; Haverich, A.; et al. Biohybrid Lung Development: Towards Complete Endothelialization of an Assembled Extracorporeal Membrane Oxygenator. Bioengineering 2023, 10, 72. [Google Scholar] [CrossRef] [PubMed]
- Thiebes, A.L.; Uhl, F.E.; Hauser, M.; Cornelissen, C.G.; Jockenhoevel, S.; Weiss, D.J. Endoscopic atomization of mesenchymal stromal cells: In vitro study for local cell therapy of the lungs. Cytotherapy 2021, 23, 293–300. [Google Scholar] [CrossRef] [PubMed]
- Thiebes, A.L.; Albers, S.; Klopsch, C.; Jockenhoevel, S.; Cornelissen, C.G. Spraying Respiratory Epithelial Cells to Coat Tissue-Engineered Constructs. BioRes. Open Access 2015, 4, 278–287. [Google Scholar] [CrossRef] [PubMed]
- Andreone, A.; den Hollander, D. A Retrospective Study on the Use of Dermis Micrografts in Platelet-Rich Fibrin for the Resurfacing of Massive and Chronic Full-Thickness Burns. Stem Cells Int. 2019, 2019, 8636079. [Google Scholar] [CrossRef] [PubMed]
- Johnstone, P.; Kwei, J.S.; Filobbos, G.; Lewis, D.; Jeffery, S. Successful application of keratinocyte suspension using autologous fibrin spray. Burns 2017, 43, e27–e30. [Google Scholar] [CrossRef]
- Klopsch, C.; Gabel, R.; Kaminski, A.; Mark, P.; Wang, W.; Toelk, A.; Delyagina, E.; Kleiner, G.; Koch, L.; Chichkov, B.; et al. Spray- and laser-assisted biomaterial processing for fast and efficient autologous cell-plus-matrix tissue engineering. J. Tissue Eng. Regen. Med. 2015, 9, E177–E190. [Google Scholar] [CrossRef]
- Roberts, A.; Wyslouzil, B.E.; Bonassar, L. Aerosol delivery of mammalian cells for tissue engineering. BioTechnol. BioEng. 2005, 91, 801–807. [Google Scholar] [CrossRef]
- Thiebes, A.L.; Kelly, N.; Sweeney, C.A.; McGrath, D.J.; Clauser, J.; Kurtenbach, K.; Gesche, V.N.; Chen, W.; Kok, R.J.; Steinseifer, U.; et al. PulmoStent: In Vitro to In Vivo Evaluation of a Tissue Engineered Endobronchial Stent. Ann. BioMed. Eng. 2017, 45, 873–883. [Google Scholar] [CrossRef]
- Thiebes, A.L.; Klein, S.; Zingsheim, J.; Moller, G.H.; Gurzing, S.; Reddemann, M.A.; Behbahani, M.; Jockenhoevel, S.; Cornelissen, C.G. Effervescent Atomizer as Novel Cell Spray Technology to Decrease the Gas-to-Liquid Ratio. Pharmaceutics 2022, 14, 2421. [Google Scholar] [CrossRef]
- Kaminski, A.; Klopsch, C.; Mark, P.; Yerebakan, C.; Donndorf, P.; Gabel, R.; Eisert, F.; Hasken, S.; Kreitz, S.; Glass, A.; et al. Autologous valve replacement-CD133+ stem cell-plus-fibrin composite-based sprayed cell seeding for intraoperative heart valve tissue engineering. Tissue Eng. Part C Methods 2011, 17, 299–309. [Google Scholar] [CrossRef] [PubMed]
- Nahmias, Y.; Arneja, A.; Tower, T.; Renn, M.; Odde, D. Cell Patterning on Biological Gels via Cell Spraying trhough a Mask. Tissue Eng. 2005, 11, 701–708. [Google Scholar] [CrossRef] [PubMed]
- Dodd, R.; Cornwell, R.; Holm, N.; Garbarsch, A.; Hollingsbee, D. The Vivostat® application system: A comparison with conventional fibrin sealant application systems. Technol. Health Care 2002, 10, 401–411. [Google Scholar] [CrossRef] [PubMed]
- Stirling, D.R.; Swain-Bowden, M.J.; Lucas, A.M.; Carpenter, A.E.; Cimini, B.A.; Goodman, A. CellProfiler 4: Improvements in speed, utility and usability. BMC Bioinform. 2021, 22, 433. [Google Scholar] [CrossRef]
- Li, B.; Chen, J.; Wang, J.H. RGD peptide-conjugated poly(dimethylsiloxane) promotes adhesion, proliferation, and collagen secretion of human fibroblasts. J. BioMed. Mater. Res. A 2006, 79, 989–998. [Google Scholar] [CrossRef]
- Saw, S.N.; Dawn, C.; Biswas, A.; Mattar, C.N.Z.; Yap, C.H. Characterization of the in vivo wall shear stress environment of human fetus umbilical arteries and veins. BioMech. Model Mechanobiol. 2017, 16, 197–211. [Google Scholar] [CrossRef]
- Ruijter, J.; Ramakers, C.; Hoogaars, W.; Karlen, Y.; Bakker, O.; Van den Hoff, M.; Moorman, A. Amplification efficiency: Linking baseline and bias in the analysis of quantitative PCR data. Nucleic Acids Res. 2009, 37, e45. [Google Scholar] [CrossRef]
- Veazey, W.S.; Anusavice, K.J.; Moore, K. Mammalian cell delivery via aerosol deposition. J. BioMed. Mater. Res. B Appl. BioMater. 2005, 72, 334–338. [Google Scholar] [CrossRef]
- Grant, I.; Warwick, K.; Marshall, J.; Green, C.; Martin, R. The co-application of sprayed cultured autologous keratinocytes and autologous fibrin sealant in a porcine wound model. Br. J. Plast Surg. 2002, 55, 219–227. [Google Scholar] [CrossRef]
- Festjens, N.; Vanden Berghe, T.; Vandenabeele, P. Necrosis, a well-orchestrated form of cell demise: Signalling cascades, important mediators and concomitant immune response. Biochim. Biophys. Acta 2006, 1757, 1371–1387. [Google Scholar] [CrossRef]
- Paolone, S. Extracorporeal Membrane Oxygenation (ECMO) for Lung Injury in Severe Acute Respiratory Distress Syndrome (ARDS): Review of the Literature. Clin. Nurs. Res. 2017, 26, 747–762. [Google Scholar] [CrossRef] [PubMed]
- Rogers, C.; Fernandes-Alnemri, T.; Mayes, L.; Alnemri, D.; Cingolani, G.; Alnemri, E.S. Cleavage of DFNA5 by caspase-3 during apoptosis mediates progression to secondary necrotic/pyroptotic cell death. Nat. Commun. 2017, 8, 14128. [Google Scholar] [CrossRef] [PubMed]
- Somer, F.D.; Foubert, L.; Vanackere, M.; Dujardin, D.; Delanghe, J.; Nooten, G.V. Impact of Oxygenator Design on Hemolysis, Shear Stress, and White Blood Cell and Platelet Count. J. Cardlothoracm. Vasc. Anesth. 1996, 10, 884–889. [Google Scholar] [CrossRef] [PubMed]
- Pflaum, M.; Jurmann, S.; Katsirntaki, K.; Malzer, M.; Haverich, A.; Wiegmann, B. Towards Biohybrid Lung Development-Fibronectin-Coating Bestows Hemocompatibility of Gas Exchange Hollow Fiber Membranes by Improving Flow-Resistant Endothelialization. Membranes 2021, 12, 35. [Google Scholar] [CrossRef]
- Chen, X.L.; Varner, S.E.; Rao, A.S.; Grey, J.Y.; Thomas, S.; Cook, C.K.; Wasserman, M.A.; Medford, R.M.; Jaiswal, A.K.; Kunsch, C. Laminar flow induction of antioxidant response element-mediated genes in endothelial cells. A novel anti-inflammatory mechanism. J. Biol. Chem. 2003, 278, 703–711. [Google Scholar] [CrossRef]
- Chen, S.; Qin, L.; Wu, X.; Fu, X.; Lin, S.; Chen, D.; Xiao, G.; Shao, Z.; Cao, H. Moderate Fluid Shear Stress Regulates Heme Oxygenase-1 Expression to Promote Autophagy and ECM Homeostasis in the Nucleus Pulposus Cells. Front. Cell Dev. Biol. 2020, 8, 127. [Google Scholar] [CrossRef]
- Dekker, R.J.; van Soest, S.; Fontijn, R.D.; Salamanca, S.; de Groot, P.G.; VanBavel, E.; Pannekoek, H.; Horrevoets, A.J. Prolonged fluid shear stress induces a distinct set of endothelial cell genes, most specifically lung Kruppel-like factor (KLF2). Blood 2002, 100, 1689–1698. [Google Scholar] [CrossRef]
- Babendreyer, A.; Molls, L.; Simons, I.M.; Dreymueller, D.; Biller, K.; Jahr, H.; Denecke, B.; Boon, R.A.; Bette, S.; Schnakenberg, U.; et al. The metalloproteinase ADAM15 is upregulated by shear stress and promotes survival of endothelial cells. J. Mol. Cell Cardiol. 2019, 134, 51–61. [Google Scholar] [CrossRef]
- Fledderus, J.O.; van Thienen, J.V.; Boon, R.A.; Dekker, R.J.; Rohlena, J.; Volger, O.L.; Bijnens, A.P.; Daemen, M.J.; Kuiper, J.; van Berkel, T.J.; et al. Prolonged shear stress and KLF2 suppress constitutive proinflammatory transcription through inhibition of ATF2. Blood 2007, 109, 4249–4257. [Google Scholar] [CrossRef]
- SenBanerjee, S.; Lin, Z.; Atkins, G.B.; Greif, D.M.; Rao, R.M.; Kumar, A.; Feinberg, M.W.; Chen, Z.; Simon, D.I.; Luscinskas, F.W.; et al. KLF2 Is a novel transcriptional regulator of endothelial proinflammatory activation. J. Exp. Med. 2004, 199, 1305–1315. [Google Scholar] [CrossRef]
- Babendreyer, A.; Molls, L.; Dreymueller, D.; Uhlig, S.; Ludwig, A. Shear Stress Counteracts Endothelial CX3CL1 Induction and Monocytic Cell Adhesion. Mediat. Inflamm. 2017, 2017, 1515389. [Google Scholar] [CrossRef] [PubMed]
- Chakraborty, S.; Njah, K.; Pobbati, A.V.; Lim, Y.B.; Raju, A.; Lakshmanan, M.; Tergaonkar, V.; Lim, C.T.; Hong, W. Agrin as a Mechanotransduction Signal Regulating YAP through the Hippo Pathway. Cell Rep. 2017, 18, 2464–2479. [Google Scholar] [CrossRef]
- Lu, Y.W.; Martino, N.; Gerlach, B.D.; Lamar, J.M.; Vincent, P.A.; Adam, A.P.; Schwarz, J.J. MEF2 (Myocyte Enhancer Factor 2) Is Essential for Endothelial Homeostasis and the Atheroprotective Gene Expression Program. Arter. Thromb. Vasc. Biol. 2021, 41, 1105–1123. [Google Scholar] [CrossRef] [PubMed]
- Vania, V.; Wang, L.; Tjakra, M.; Zhang, T.; Qiu, J.; Tan, Y.; Wang, G. The interplay of signaling pathway in endothelial cells-matrix stiffness dependency with targeted-therapeutic drugs. Biochim. Biophys. Acta Mol. Basis Dis. 2020, 1866, 165645. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.; Liu, L.; Yu, T.; Wang, Q.; Fu, H. VCAM1-targeted RNA interference inhibits the proliferation of human oral squamous carcinoma HN12 cells. Oncol. Lett. 2018, 15, 5650–5654. [Google Scholar] [CrossRef]
- Tanaka, E.; Shimokawa, H.; Kamiuneten, H.; Eto, Y.; Matsumoto, Y.; Morishige, K.; Koike, G.; Yoshinaga, M.; Egashira, K.; Tokunaga, O.; et al. Disparity of MCP-1 mRNA and Protein Expressions Between the Carotid Artery and the Aorta in WHHL Rabbits. Arterioscler. Thromb. Vasc. Biol. 2003, 23, 244–250. [Google Scholar] [CrossRef]
- Hoffmann, E.; Dittrich-Breiholz, O.; Holtmann, H.; Kracht, M. Multiple control of interleukin-8 gene expression. J. Leukoc. Biol. 2002, 72, 847–855. [Google Scholar] [CrossRef]
- Olmer, R.; Engels, L.; Usman, A.; Menke, S.; Malik, M.N.H.; Pessler, F.; Gohring, G.; Bornhorst, D.; Bolten, S.; Abdelilah-Seyfried, S.; et al. Differentiation of Human Pluripotent Stem Cells into Functional Endothelial Cells in Scalable Suspension Culture. Stem Cell Rep. 2018, 10, 1657–1672. [Google Scholar] [CrossRef]

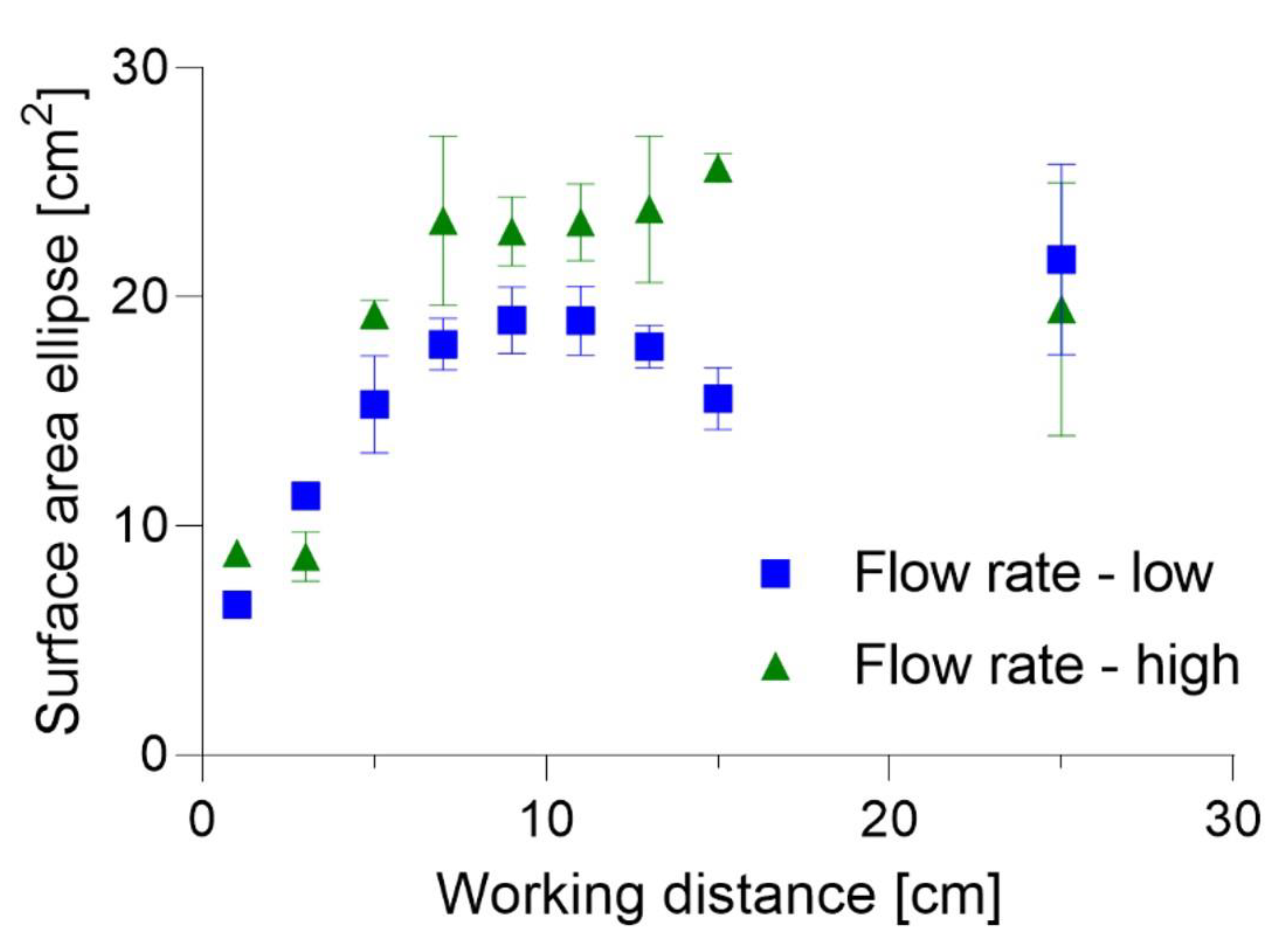

| Parameter | Tested Values | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Flow rate | Low | High | |||||||
| Working distance [cm] | 1 | 3 | 5 | 7 | 9 | 11 | 13 | 15 | 25 |
| Parameter | Tested Values | ||
|---|---|---|---|
| Flow rate | Low | High | |
| Working distance [cm] | 3 | 9 | 15 |
| Cell concentration [cells/mL] | 0.5 × 106 | 2 × 106 | 5 × 106 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cheremkhina, M.; Klein, S.; Babendreyer, A.; Ludwig, A.; Schmitz-Rode, T.; Jockenhoevel, S.; Cornelissen, C.G.; Thiebes, A.L. Influence of Aerosolization on Endothelial Cells for Efficient Cell Deposition in Biohybrid and Regenerative Applications. Micromachines 2023, 14, 575. https://doi.org/10.3390/mi14030575
Cheremkhina M, Klein S, Babendreyer A, Ludwig A, Schmitz-Rode T, Jockenhoevel S, Cornelissen CG, Thiebes AL. Influence of Aerosolization on Endothelial Cells for Efficient Cell Deposition in Biohybrid and Regenerative Applications. Micromachines. 2023; 14(3):575. https://doi.org/10.3390/mi14030575
Chicago/Turabian StyleCheremkhina, Maria, Sarah Klein, Aaron Babendreyer, Andreas Ludwig, Thomas Schmitz-Rode, Stefan Jockenhoevel, Christian G. Cornelissen, and Anja Lena Thiebes. 2023. "Influence of Aerosolization on Endothelial Cells for Efficient Cell Deposition in Biohybrid and Regenerative Applications" Micromachines 14, no. 3: 575. https://doi.org/10.3390/mi14030575
APA StyleCheremkhina, M., Klein, S., Babendreyer, A., Ludwig, A., Schmitz-Rode, T., Jockenhoevel, S., Cornelissen, C. G., & Thiebes, A. L. (2023). Influence of Aerosolization on Endothelial Cells for Efficient Cell Deposition in Biohybrid and Regenerative Applications. Micromachines, 14(3), 575. https://doi.org/10.3390/mi14030575







