How Effective Are Mindfulness-Based Interventions for Reducing Stress and Weight? A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Screening
2.4. Procedure and Data Extraction
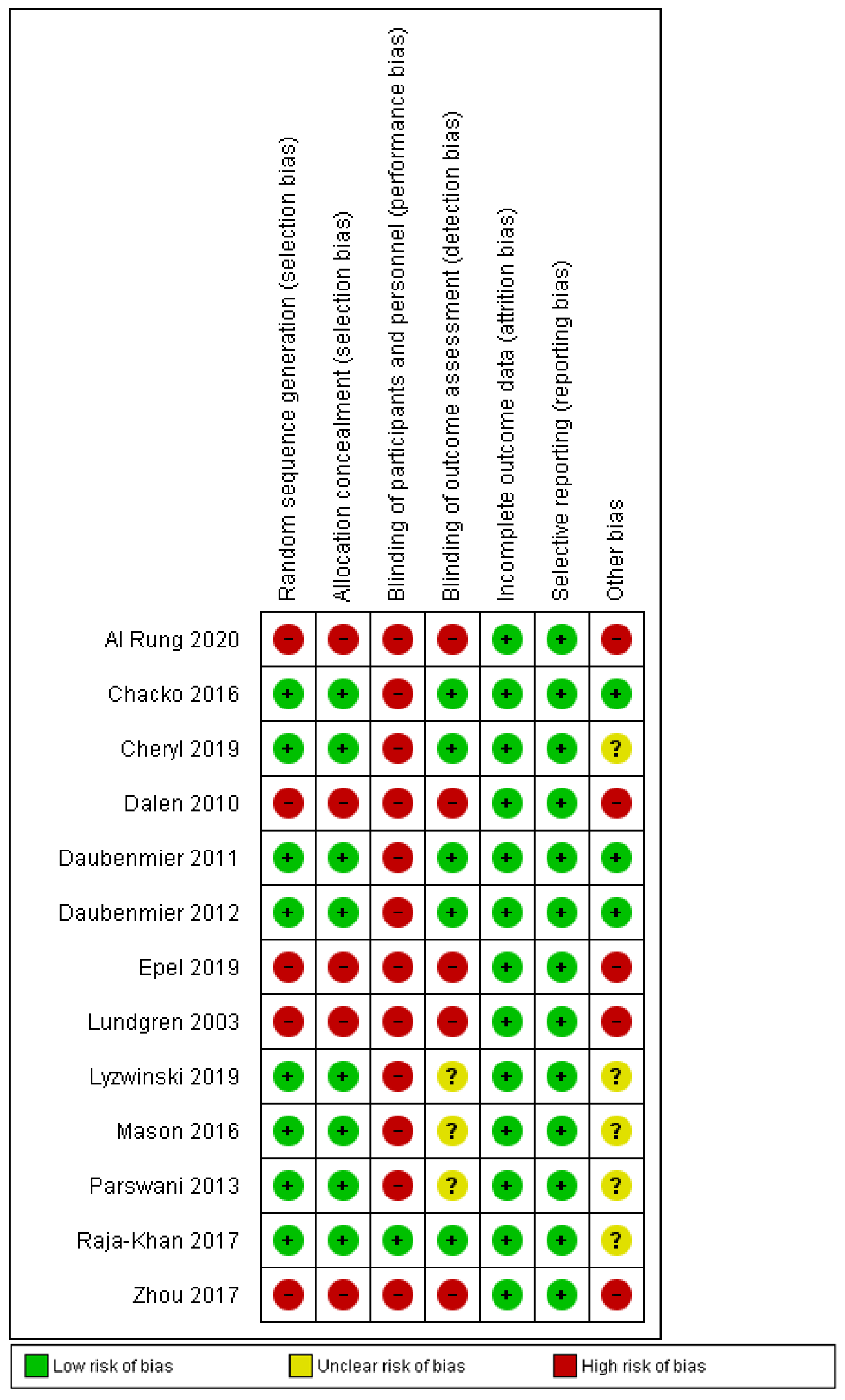
2.5. Risk of Bias Assessment
2.6. Data Analysis
3. Results
3.1. Selection Process
3.2. Characteristics of the Included Studies
3.3. Risk of Bias
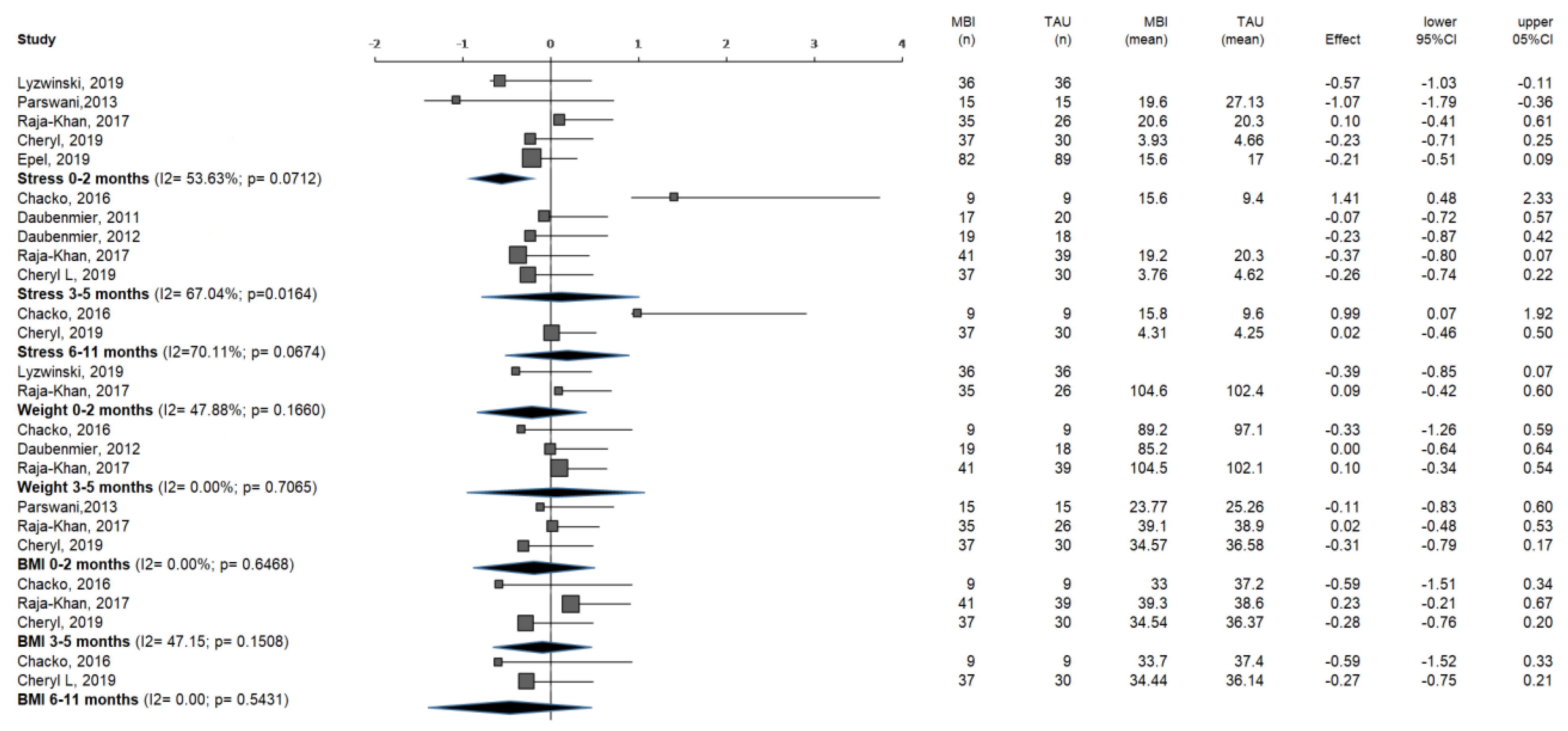
3.4. Meta-Analysis
3.4.1. Outcome Variable: Stress
3.4.2. Outcome Variable: Weight
3.4.3. Outcome Variable: BMI
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Obesity. Available online: https://www.who.int/health-topics/obesity#tab=tab_1 (accessed on 23 March 2020).
- World Health Organization. Obesity and Overweight. Fact Sheet. 2018. Available online: https://www.who.int/en/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 24 March 2020).
- Garaulet, M.; Canteras, M.; Morales, E.; López-Guimera, G.; Sánchez-Carracedo, D.; Corbalán-Tutau, M.D. Validation of a questionnaire on emotional eating for use in cases of obesity; the Emotional Eater Questionnaire (EEQ). Nutr. Hosp. 2012, 27, 645–651. [Google Scholar] [PubMed]
- Bongers, P.; Jansen, A. Emotional Eating Is Not What You Think It Is and Emotional Eating Scales Do Not Measure What You Think They Measure. Front. Psychol. 2016, 7, 160–189. [Google Scholar] [CrossRef] [Green Version]
- Van Der Valk, E.S.; Savas, M.; Van Rossum, E.F.C. Stress and Obesity Are There More Susceptible Individuals? Curr. Obes. Rep. 2018, 7, 193–203. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lyzwinski, L.N.; Caffery, L.; Bambling, M.; Edirippulige, S. Relationship between Mindfulness, Weight, and Weight-Related Behaviors in College Students: A Systematic Review. Alt. Comp. Ther. 2018, 24, 202–214. [Google Scholar] [CrossRef]
- Solé, S.; Carrança, B.; Serpa, S.; Palmi, J. Concepto Mindfulness. Rev. Psicol. Deporte. 2014, 23, 501–508. [Google Scholar]
- Aherne, D.; Farrant, K.; Hickey, L.; Hickey, E.; McGrath, L.; McGrath, D. Mindfulness-based stress reduction for medical students: Optimising student satisfaction and engagement. BMC Med. Educ. 2016, 16, 193–196. [Google Scholar] [CrossRef] [Green Version]
- Daubenmier, J.; Epel, E.S.; Moran, P.J.; Thompson, J.; Mason, A.E.; Acree, M.; Goldman, V.; Kristeller, J.; Hecht, F.M.; Mendes, W.B. A Randomized Controlled Trial of a Mindfulness-Based Weight Loss Intervention on Cardiovascular Reactivity to Social-Evaluative Threat Among Adults with Obesity. Mindfulness 2019, 10, 2583–2595. [Google Scholar] [CrossRef] [PubMed]
- Daubenmier, J.; Kristeller, J.; Hecht, F.M.; Maninger, N.; Kuwata, M.; Jhaveri, K.; Lustig, R.H.; Kemeny, M.; Karan, L.; Epel, E. Mindfulness Intervention for Stress Eating to Reduce Cortisol and Abdominal Fat among Overweight and Obese Women: An Exploratory Randomized Controlled Study. J. Obes. 2011, 37, 893–911. [Google Scholar] [CrossRef]
- Shomaker, L.B.; Pivarunas, B.; Annameier, S.K.; Gulley, L.; Quaglia, J.; Brown, K.W.; Broderick, P.; Bell, C. One-year follow-up of a randomized controlled trial piloting a mindfulness-based group intervention for adolescent insulin resistance. Front. Psychol. 2019, 10, 103–203. [Google Scholar] [CrossRef]
- Fulwiler, C.; Siegel, J.A.; Allison, J.; Rosal, M.C.; Brewer, J.; King, J.A. Keeping Weight Off: Study protocol of an RCT to investigate brain changes associated with mindfulness-based stress reduction. BMJ Open 2016, 6, 2583–2587. [Google Scholar] [CrossRef] [Green Version]
- Daubenmier, J.; Lin, J.; Blackburn, E.; Hecht, F.M.; Kristeller, J.; Maninger, N.; Kuwata, M.; Bacchetti, P.; Havel, P.J.; Epel, E. Changes in stress, eating, and metabolic factors are related to changes in telomerase activity in a randomized mindfulness intervention pilot study. Psychoneuroendocrinology 2012, 37, 917–928. [Google Scholar] [CrossRef] [PubMed]
- Schnepper, R.; Richard, A.; Wilhelm, F.H.; Blechert, J. A Combined Mindfulness’Prolonged Chewing Intervention Reduces Body Weight, Food Craving, and Emotional Eating. J. Consult. Clin. Psychol. 2019, 87, 106–111. [Google Scholar] [CrossRef] [PubMed]
- Radin, R.M.; Epel, E.S.; Daubenmier, J.; Moran, P.; Schleicher, S.; Kristeller, J.; Hecht, F.M.; Mason, A.E. Do Stress Eating or Compulsive Eating Influence Metabolic Health in a Mindfulness-Based Weight Loss Intervention? Health Psychol. 2020, 39, 147–158. [Google Scholar] [CrossRef] [PubMed]
- Lattimore, P. Mindfulness-based emotional eating awareness training: Taking the emotional out of eating. Eat. Weight. Disord. 2020, 25, 649–657. [Google Scholar] [CrossRef] [Green Version]
- Lazaridou, A.; Philbrook, P.; Tzika, A.A. Yoga and mindfulness as therapeutic interventions for stroke rehabilitation: A systematic review. Evid. Based Complement. Altern. Med. 2013, 11, 253–295. [Google Scholar] [CrossRef] [PubMed]
- Pleman, B.; Park, M.; Han, X.; Price, L.L.; Bannuru, R.R.; Harvey, W.F.; Driban, J.B.; Wang, C. Mindfulness is associated with psychological health and moderates the impact of fibromyalgia. Clin. Rheumatol. 2019, 38, 1737–1745. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Fernández, M.D.; Pérez-García, E.; Ortega-Galán, Á.M. Quality of life in nursing professionals: Burnout, fatigue, and compassion satisfaction. Int. J. Environ. Res. Public Health 2020, 17, 1253. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; LiberatI, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Higgins, J.P.T.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. [updated March 2011]; The Cochrane Collaboration, 2011; Centro Cochrane Iberoamericano: Barcelona, Spain, 2012; pp. 1–138. [Google Scholar]
- Botella-Ausina, J.; Sánchez-Meca, J. Meta Analisis En Ciencias Sociales Y De La Salud; Sintesis: Madrid, Spain, 2015; pp. 154–166. [Google Scholar]
- Kontopantelis, E.; Reeves, D. MetaEasy: A meta-analysis add-in for Microsoft Excel. J. Stat. Softw. 2009, 30, 1–25. [Google Scholar] [CrossRef]
- Chacko, S.A.; Yeh, G.Y.; Davis, R.B.; Wee, C.C. A mindfulness-based intervention to control weight after bariatric surgery: Preliminary results from a randomized controlled pilot trial. Complement. Ther. Med. 2016, 28, 13–21. [Google Scholar] [CrossRef]
- Dalen, J.; Smith, B.W.; Shelley, B.M.; Sloan, A.L.; Leahigh, L.; Begay, D. Pilot study: Mindful Eating and Living (MEAL): Weight, eating behavior, and psychological outcomes associated with a mindfulness-based intervention for people with obesity. Complement. Ther. Med. 2010, 18, 260–280. [Google Scholar] [CrossRef] [PubMed]
- Lyzwinski, L.N.; Caffery, L.; Bambling, M.; Edirippulige, S. The mindfulness app trial for weight, weight-related behaviors, and stress in university students: Randomized controlled trial. JMIR Mhealth Uhealth 2019, 7, 153–189. [Google Scholar] [CrossRef] [PubMed]
- Rung, A.L.; Oral, E.; Berghammer, L.; Peters, E.S. Feasibility and acceptability of a mobile mindfulness meditation intervention among women: An intervention study. JMIR Mhealth Uhealth 2020, 8, 167–168. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.E.; Jackson, C.D.; Oates, V.J.; Davis, G.W.; Davis, C.; Takizala, Z.-M.; Akatue, R.A.; Williams, K.; Liu, J.; Hébert, J.R.; et al. Refining a Church-Based Lifestyle Intervention Targeting African American Adults at Risk for Cardiometabolic Diseases: A Pilot Study. Open J. Epidemiol. 2017, 7, 96–114. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lundgren, J.D. A Mindfulness-Based Behavioral Treatment for Weight Loss. A dissertation. Ph.D. Thesis, University at Albany, State University of New York, Albany, NY, USA, 2003; pp. 13–27. [Google Scholar]
- Mason, A.E.; Epel, E.S.; Aschbacher, K.; Lustig, R.H.; Acree, M.; Kristeller, J.; Cohn, M.; Dallman, M.; Moran, P.J.; Bacchetti, P.; et al. Reduced reward-driven eating accounts for the impact of a mindfulness-based diet and exercise intervention on weight loss: Data from the SHINE randomized controlled trial. Appetite 2016, 100, 86–93. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Parswani, M.; Sharma, M.; Iyengar, S. Mindfulness-based stress reduction program in coronary heart disease: A randomized control trial. Int. J. Yoga. 2013, 6, 111–113. [Google Scholar] [CrossRef]
- Raja-Khan, N.; Agito, K.; Shah, J.; Stetter, C.M.; Gustafson, T.S.; Socolow, H.; Kunselman, A.R.; Reibel, D.K.; Legro, R.S. Mindfulness-Based Stress Reduction in Women with Overweight or Obesity: A Randomized Clinical Trial. Obesity 2017, 25, 1349–1359. [Google Scholar] [CrossRef] [Green Version]
- Woods-Giscombe, C.L.; Gaylord, S.A.; Li, Y.; Brintz, C.E.; Bangdiwala, S.I.; Buse, J.B.; Mann, J.D.; Lynch, C.; Phillips, P.; Smith, S.; et al. A Mixed-Methods, Randomized Clinical Trial to Examine Feasibility of a Mindfulness-Based Stress Management and Diabetes Risk Reduction Intervention for African Americans with Prediabetes. Evid. Based Complement. Altern. Med. 2019, 17, 13–18. [Google Scholar] [CrossRef] [Green Version]
- Daubenmier, J.; Lustig, R.H.; Hecht, F.M.; Kristeller, J.; Woolley, J.; Adam, T.; Dallman, M.; Epel, E. A new biomarker of hedonic eating? A preliminary investigation of cortisol and nausea responses to the acute opioid blockade. Appetite 2014, 74, 92–100. [Google Scholar] [CrossRef] [Green Version]
- Epel, E.; Laraia, B.; Coleman-Phox, K.; Leung, C.; Vieten, C.; Mellin, L.; Kristeller, J.L.; Thomas, M.; Stotland, N.; Bush, N.; et al. Effects of a Mindfulness-Based Intervention on Distress, Weight Gain, and Glucose Control for Pregnant Low-Income Women: A Quasi-Experimental Trial Using the ORBIT Model. Int. J. Behav. Med. 2019, 26, 461–473. [Google Scholar] [CrossRef] [Green Version]
- Woods-Giscombé, C.L.; Gaylord, S.A. The Cultural Relevance of Mindfulness Meditation as a Health Intervention for African Americans: Implications for Reducing Stress-Related Health Disparities. J. Holist. Nurs. 2014, 32, 147–160. [Google Scholar] [CrossRef] [PubMed]
- Raja-Khan, N.; Agito, K.; Shah, J.; Stetter, C.M.; Gustafson, T.S.; Socolow, H.; Kunselman, A.R.; Reibel, D.K.; Legro, R.S. Mindfulness-based stress reduction for overweight/obese women with and without polycystic ovary syndrome: Design and methods of a pilot randomized controlled trial. Contemp. Clin. Trials 2015, 41, 287–297. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mason, A.E.; Jhaveri, K.; Cohn, M.; Brewer, J.A. Testing a mobile mindful eating intervention targeting craving-related eating: Feasibility and proof of concept. J. Behav. Med. 2018, 41, 160–173. [Google Scholar] [CrossRef]
- Beaulac, J.; Sandre, D.; Mercer, D. Impact on mindfulness, emotion regulation, and emotional overeating of a DBT skills training group: A pilot study. Eat. Weight Disord. 2019, 24, 373–377. [Google Scholar] [CrossRef] [PubMed]
- Duan, W.; Wang, Z. Dispositional mindfulness promotes public health of the obesity population by reducing perceived discrimination and weight stigma concerns. J. Public Health 2019, 27, 195–202. [Google Scholar] [CrossRef]
- Schell, L.K.; Monsef, I.; Wöckel, A.; Skoetz, N. Mindfulness-based stress reduction for women diagnosed with breast cancer. Cochrane Database Syst. Rev. 2019, 3, 123–140. [Google Scholar] [CrossRef]
- Morton, M.L.; Helminen, E.C.; Felver, J.C. A systematic review of mindfulness interventions on psychophysiological responses to acute stress. Mindfulness 2020, 11, 2039–2054. [Google Scholar] [CrossRef]
- Burton, E.T.; Smith, W.A. Mindful eating and active living: Development and implementation of a multidisciplinary pediatric weight management intervention. Nutrients 2020, 12, 1425. [Google Scholar] [CrossRef]


| Authors | Sample | Methods | Location | Aim | Intervention | Control | Duration | Variables | Main outcomes |
|---|---|---|---|---|---|---|---|---|---|
| Lundgren et al., 2003 [29] | N = 19 Mean age = 44.8 | Pre-post | USA | Assess whether IGs decrease general symptomatology | Mindfulness meditation practice + traditional behavioral treatment | No control group | 20 weeks | General symptomatology, stress, quality of life, acceptance of body image, percent weight loss, and binge eating | PSS pre-post (p > 0.05). BMI not significant pre-post measures differences. Several completed homework was positively correlated with the amount of weight lost (r = 0.55, p = 0.0018). Number of meditations and binge eating score (r = 0.46, p = 0.046). |
| Chacko et al., 2016 [24] | N = 18 IG = 9 CG = 9 Mean age = 54 | RCT | USA | Assess a new MBI aimed at weight management after a bariatric medical procedure | Mindfulness with modified versions of traditional behavioral plan | 1 h personalized advice session with a dietitian | 10 weeks | Viability and acceptance of MBI, weight, eating behaviors, and psychological results | No differences in weight, BMI, or circumference. At 12 weeks, higher scores on perceived stress and depression (p < 0.05). |
| Dalen et al., 2010 [25] | N = 10 Mean age = 44 | Pilot study: pre-post | Mexico | Mindful eating and living | Training in mindfulness meditation, mindful eating, and group discussion | No control group | 6 weeks | Changes in weight, BMI, eating behaviors, and psychological distress. | All participants significantly lost weight (p < 0.001) Perceived stress (after 12 weeks) (p = 0.02). |
| Daubenmier et al., 2011 [10] | N = 47 IG = 24 CG = 23 Mean age = 32.5 | Randomized waitlist-controlled pilot study | USA | Assess the impact of a mindfulness intervention on stomach adiposity in women who suffer from overweight or obesity | Included nine 2.5 h sessions and one 7 h silent day of coordinated reflection practice following class 6 | Waitlist group | 4 months | Mindfulness, eating behaviors, mental misery, weight, and cortisol arousing reaction stomach fat | No difference was found between groups regarding mean weight. The effect size was medium for self-perceived levels of stress. |
| Daubenmier et al., 2012 [13] | N = 47 IG = 24 CG = 23 Mean age = 32.5 | RCT | USA | Assess MBIs whether decreased psychological distress, eating patterns, and metabolic characteristics | MBSR and MB-EAT | Waitlist group 2 h diet and exercise information | 4 months | Stress eating, telomerase activity, psychological distress, eating behaviors, and metabolic characteristics | Not a significant change after some time in the levels of self-perceived stress; both groups maintained their weight over time. |
| Lyzwinski et al., 2019 [26] | N = 90 IG= 45 CG = 45 Mean age = 20.16 | RCT | Australia | Assess a mindfulness app for weight, weight-related conduct, and stress management | Intervention group was given the mindfulness app with ME and MBSR strategies | Behavioral self-observation; electronic diary for diet and physical exercise | 11 weeks | Weight, stress, mindfulness, mindful eating, physical exercise, and eating behaviors | There were no statistically significant differences in weight between both the mindfulness app intervention and control e-diary groups at follow-up using ANCOVA (p = 0.27). Pairwise comparisons indicate that the control had stress levels that were 3.921 points higher on the PSS than the IG (p < 0.05; 95% CI 0.591–0.592). |
| Mason et al., 2016 [30] | N = 194 IG = 100 CG = 94 Mean age = 47 | RCT | USA | Assess post-intervention reward-driven eating and psychological stress acting as an intermediary of the effect of the intervention arm on weight loss at 12 and 18 months | Nutritional and physical exercise plan with mindfulness training. | Diet and exercise intervention and active control | 5.5 months | Reward-based eating, psychological stress, and weight | The whole sample significantly lost weight and self-perceived stress decreased after 12 months. |
| Parswani et al., 2013 [31] | N = 30 IG = 15 CG = 15 Mean age = 47.27 | RCT | India | Assess the impact of the MBSR program on health symptoms | MBSR | TAU = health education session | MBSR = 8 weeks TAU = 1 session | Anxiety and depressive symptoms, and self-perceived stress | A significant reduction was observed in symptoms of anxiety and depression, perceived stress, BP, and BMI in patients in the MBSR group after the completion of the intervention assessment. At 3-months follow-up, therapeutic gains were maintained in patients of the MBSR group. |
| Raja-Khan et al., 2017 [32] | N = 86 IG = 42 CG = 44 Mean age = 44.5 | RCT | USA | Evaluate MBSR on women who suffer from overweight or obesity | MBSR | Health education and stress management incorporated to minimize bias of subject expectations | 8 weeks | Mindfulness, perceived stress, fasting glucose, and blood pressure | Compared to health education, the MBSR group demonstrated significantly improved mindfulness at 8 weeks (mean change from baseline, 4.5 vs. −1.0; p = 0.03) and significantly decreased perceived stress at 16 weeks (−3.6 vs. −1.3, p = 0.01). In the MBSR group, there were significant reductions in fasting glucose at 8 weeks (−8.9 mg/dL, p = 0.02) and 16 weeks (−9.3 mg/dL, p = 0.02) compared to baseline. |
| Rung et al., 2020 [27] | N = 236 Mean age = 46.1 | Pre-post | USA | Evaluate the viability and acceptance of a mobile mindfulness app in real daily-life conditions in a pilot study | Mobile MBSR training program: Headspace | No control group | 30 days | Viability and acceptance of the app and characteristics of app usage, mindfulness, depression, self-perceived stress, sleep quality, physical exercise, BMI, and healthy eating | Compared to health education, the MBSR group showed significantly lower levels of perceived stress at 16 weeks, compared to previous stages. No significant changes were found in weight in the MBSR group. |
| Cheryl et al., 2019 [33] | N = 68 IG = 38 CG = 30 Mean age = 52.57 | Mixed | USA | Assess MPD to reduce the risk of having diabetes via reduced stress levels | MBSR adapted for prediabetes risk reduction | Conventional diabetes risk-reduction treatment | 8 weeks | Diabetes biomarkers, body composition measurements, self-perceived stress, quality of life, and diet and physical exercise measures | Only the MPD group experienced significant reductions in BMI at 3 months. In addition, the MPD group experienced significant reductions in perceived stress at 3 months follow-up, whereas there were no significant changes in perceived stress in the CPD group. |
| Zhou et al., 2017 [28] | N = 34 Mean age = 56.1 | Pre-post | USA | Assess the viability of a multiple-component lifestyle plan | Individual and group advice on nutrition, exercise, and mindfulness | No control group | 12 weeks | Barriers and facilitators of healthy eating, being physically active, and practicing mindfulness. Psychological, dietary, physical exercise and anthropometric data, and clinical data | After 12 weeks, questionnaire-derived PSS scores slightly decreased (from 13.7 ± 1.4 to 12.4 ± 1.5, not significant). After 12 weeks’ intervention, body fat% was reduced among males (33.8 ± 2.6 to 28 ± 2.6, p = 0.043). |
| Epel et al., 2019 [35] | N = 225 IG = 115 CG = 105 Mean age = 28 | Quasi-experimental study Non-randomized control group | USA | Assess MMT on self-perceived stress, eating behaviors, and gestational weight gain | MMT + prenatal medical care | TAU = prenatal medical mindfulness | 8 weeks | Weight gain, self-perceived stress, and depression | The intervention group showed significant decreases from baseline to the post-intervention period in distress (perceived stress (p = 0.04) and depression (p = 0.007)). There were also improvements in the acceptance of negative experiences (0.006). |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sosa-Cordobés, E.; Ramos-Pichardo, J.D.; Sánchez-Ramos, J.L.; García-Padilla, F.M.; Fernández-Martínez, E.; Garrido-Fernández, A. How Effective Are Mindfulness-Based Interventions for Reducing Stress and Weight? A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2023, 20, 446. https://doi.org/10.3390/ijerph20010446
Sosa-Cordobés E, Ramos-Pichardo JD, Sánchez-Ramos JL, García-Padilla FM, Fernández-Martínez E, Garrido-Fernández A. How Effective Are Mindfulness-Based Interventions for Reducing Stress and Weight? A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2023; 20(1):446. https://doi.org/10.3390/ijerph20010446
Chicago/Turabian StyleSosa-Cordobés, Elena, Juan Diego Ramos-Pichardo, José Luis Sánchez-Ramos, Francisca María García-Padilla, Elia Fernández-Martínez, and Almudena Garrido-Fernández. 2023. "How Effective Are Mindfulness-Based Interventions for Reducing Stress and Weight? A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 20, no. 1: 446. https://doi.org/10.3390/ijerph20010446
APA StyleSosa-Cordobés, E., Ramos-Pichardo, J. D., Sánchez-Ramos, J. L., García-Padilla, F. M., Fernández-Martínez, E., & Garrido-Fernández, A. (2023). How Effective Are Mindfulness-Based Interventions for Reducing Stress and Weight? A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 20(1), 446. https://doi.org/10.3390/ijerph20010446








