Using Photovoice in a Mindfulness-Based Program to Understand the Experiences of Caregivers of Young Adults with Psychosis
Abstract
1. Introduction
Photovoice for Understanding Caregiving and Mindfulness Experiences
2. Materials and Methods
2.1. Study Design
2.2. Photovoice Data Collection
- In MBFPE sessions 2 to 5, exercises on the four photovoice themes (mindfulness of a pleasant moment, mindfulness of an unpleasant moment, mindfulness of a moment of difficult communication with the person in recovery, and the benefits of MBFPE) were given as homework assignments.
- The participants were encouraged to take photographs using their smartphones, according to guidelines offered at the end of these sessions.
- The participants were invited to provide titles and additional reflections on the photographs and share them in subsequent sessions. To facilitate group sharing, the caregivers were asked to send their photographs and reflections to the research team before the session. A PowerPoint slideshow was then prepared in sessions 3 to 6 to enable all of the participants to see the photographs clearly.
- Ten to fifteen minutes were allocated for inquiry into the photographs and the caregivers’ reflections in sessions 3 to 6. With the participants’ consent, the photographs, reflections, and content of the in-session inquiries were used for data analyses.
2.3. Photovoice Data Analysis
3. Results
3.1. Profile of the Caregivers Involved in Photovoice in This Study
3.2. Voices of the Caregivers
3.2.1. Voice 1: I Pay Attention to the Present Moment
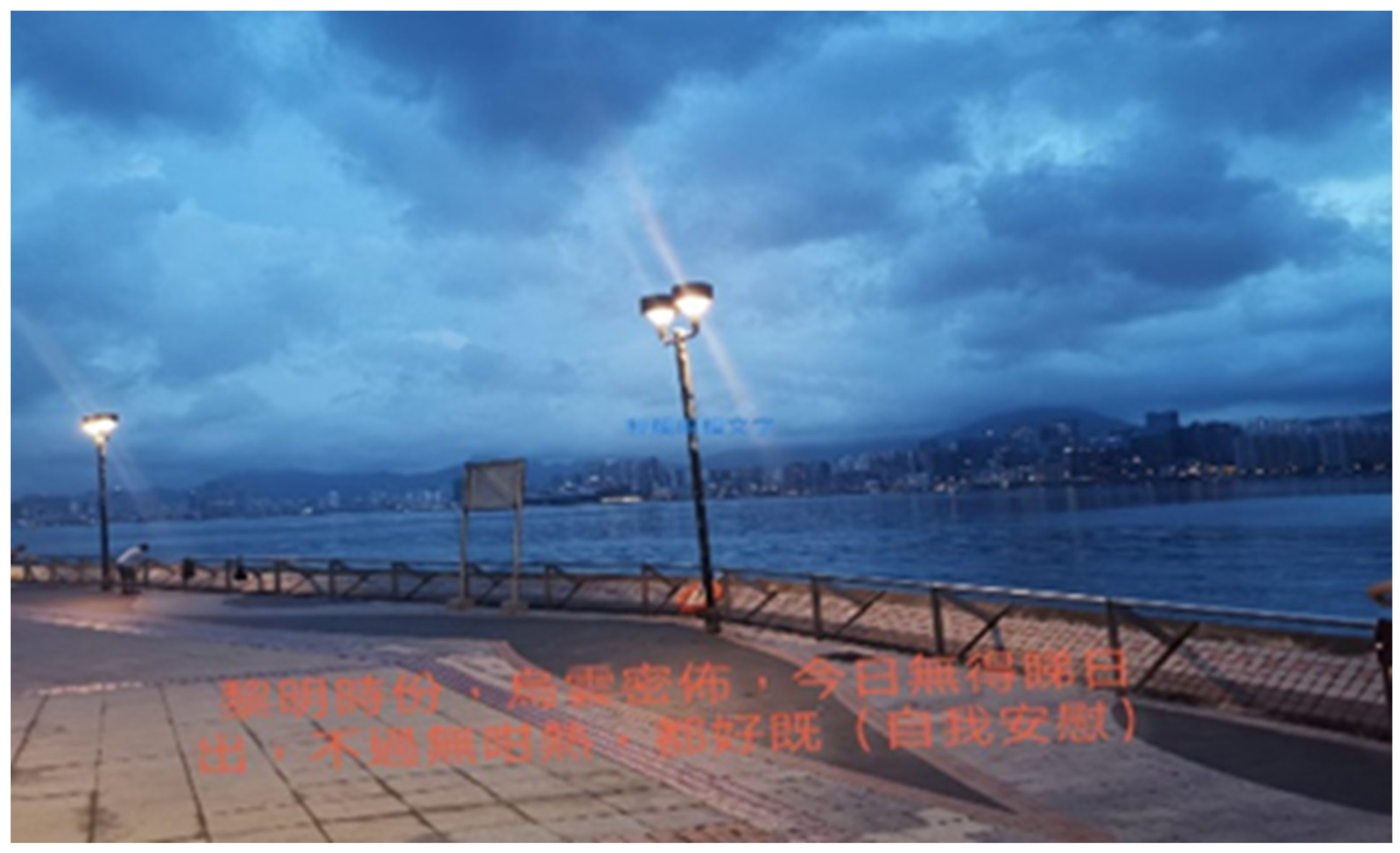
“At dawn, it was cloudy. I couldn’t see the sunrise, but it was not so hot. I comforted myself and thought it was okay.”(Participant A)
“In the past two or three years, I have needed to explore different dishes for him and I felt happy and satisfied when he pigged out on all the dishes.”
“In the morning, we had breakfast after testing for COVID-19. We were quite unhappy about the testing, but we enjoyed the nice breakfast and sunshine. After that, we took a walk and went shopping in the new recently launched store near our place.”(Participant C)
“I went to Discovery Bay to shop for food. I felt very happy when I found some attractive items. Like yesterday, there were fruit, bread, tomato soup and a watermelon on the dining table when I got home. All this food made me feel delighted.”(Participant D)
3.2.2. Voice 2: I Care about My Family
“I can only work without disturbance at night. I saw a ship with the word “dream” on the side, and I thought it was meaningful. Sometimes, having some private time is good for self-reflection. I use this ship as a metaphor to describe our lives. The ship is stable when there is no heavy wind; otherwise, the situation will become challenging. There are many conflicts within the family, but it is important to be mindful of every moment. I hope that I will continue believing in my dream: may my family be peaceful.”(Participant E)
“I hoped that my family would become more harmonious, peaceful, caring, and inclusive. This house looked old on the surface, but I thought that the important things were the characteristics I mentioned. Although I am not achieving these things at this moment, I keep learning, including how to accept myself.”(Participant E)
“The memorable reward of this course was that I learned how to live in the present moment. In our life, there are different happy and challenging moments. The important thing is to take care of myself so that I can support my family.”(Participant F)
3.2.3. Voice 3: I Trust My Children
“I observed my son doing a homework assignment for a design course. … I thought the word “hopeful” was meaningful and I wanted to share it because I feel like people do not smile often. I feel hopeful when I know that my son is studying hard and has found something he likes. As a family member, I have learned how to accept my son’s mental problem and to get along with him. Hope is always there.”(Participant F)
“I hope my son can become a ‘warrior’ like other people who have recovered, and I think positively. My son liked this picture on Facebook; I thought it was a good sign that he appreciates others’ recovery stories. I think that the person in recovery in this picture is the embodiment of courage because they have overcome many difficulties. In terms of recovery, I know that my son will not become ‘normal’ again but I hope that he will at least maintain a stable condition.”(Participant G)
“I wanted to capture this cloudy day. My son has had ADHD and autism since he was a kid; his ADHD meds and the traumatic experience in adolescence caused his schizophrenia, which was validated by medical evidence. However, I believe that the worst experiences can be our best opportunities for growth. …. He knows how to cook now, and I am thankful that he has undergone personal growth and is willing to take his medicine. He no longer feels tired after taking his medicine. I am worried about the upcoming 2022 public exam, but I believe my son will achieve good academic results.”(Participant H)
3.2.4. Voice 4: I Appreciate the Connection with and Support from Nature and the Universe
“I am used to waking up at 5 a.m. and then I will take a walk. I am grateful and thankful to nature and my son who showed me the importance of being flexible and resilient.”(Participant 1)
“After my son suffered from some health problems, I started developing religious beliefs. Subsequently, my sister and my mother developed religious beliefs, too. It helped her to overcome many difficulties in life.”(Participant F)
3.2.5. Voice 5: I Observe My Worries and Guilt and Learn Not to Be Reactive
“I wanted to talk with him more and to understand him. … I was uncertain whether he was in class or doing homework. He looked happy but it is not good to spend a long time on the phone.”(Participant J)
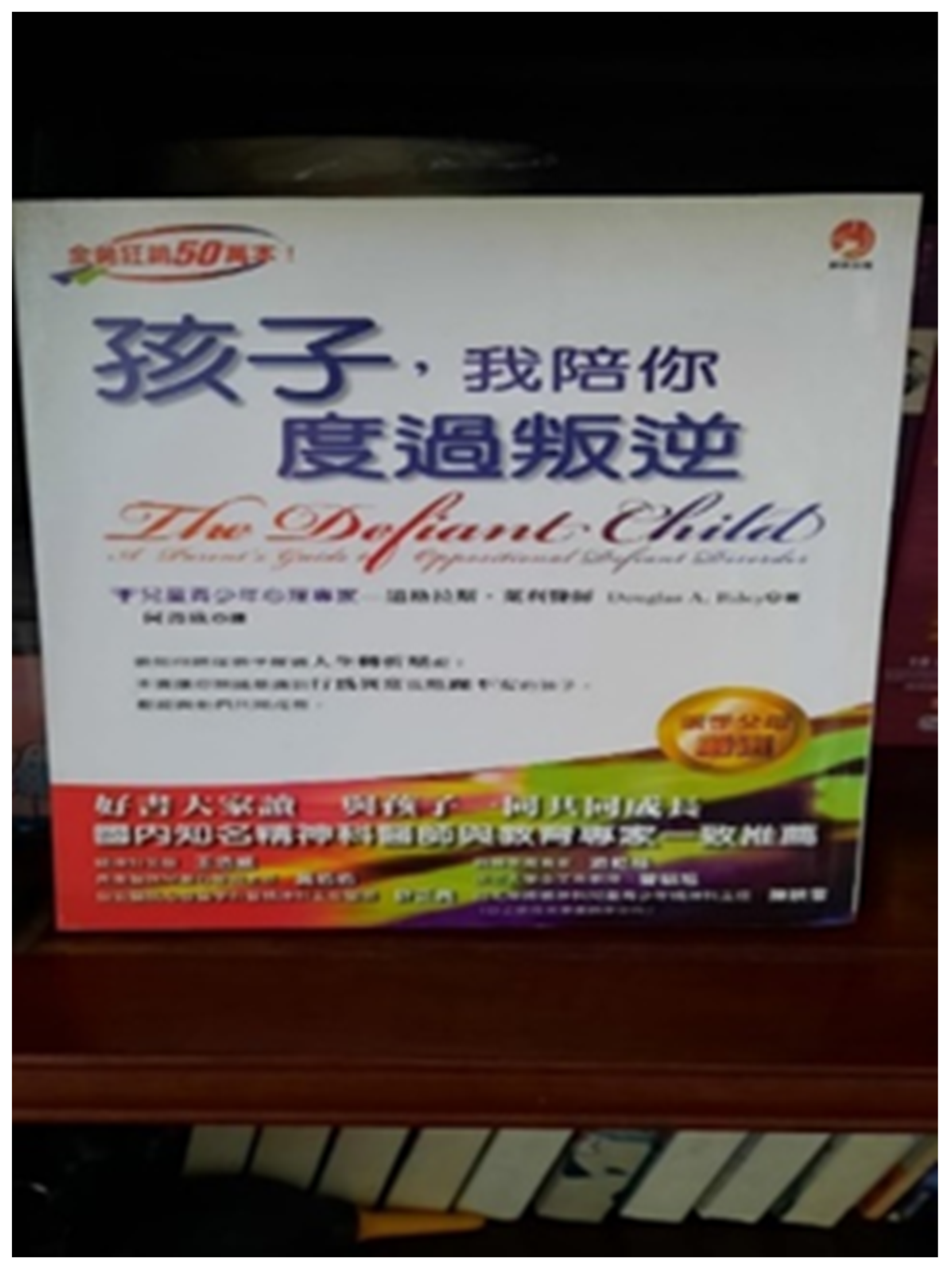
“This was the book that my wife had left, reminding me that I had not taken enough responsibility of taking care of my son. It was hard for me to compensate for what I had missed, and I found it difficult to communicate with my son. I wanted to encourage my son to do something, but it was always in vain. Despite the failures, I kept trying; for example, I encouraged him to do more exercises with a friendly tone as I believed that doing these exercises would be beneficial for him. Conversations with my son always became a conflict and we ended up silent. Therefore, I needed to prepare myself before talking to him as I had an inner struggle. I had to control myself. When he lost his temper, I chose to keep quiet, avoiding intense quarrels if possible. I hope that what I taught him has planted a seed and that he will eventually understand.”(Participant K)
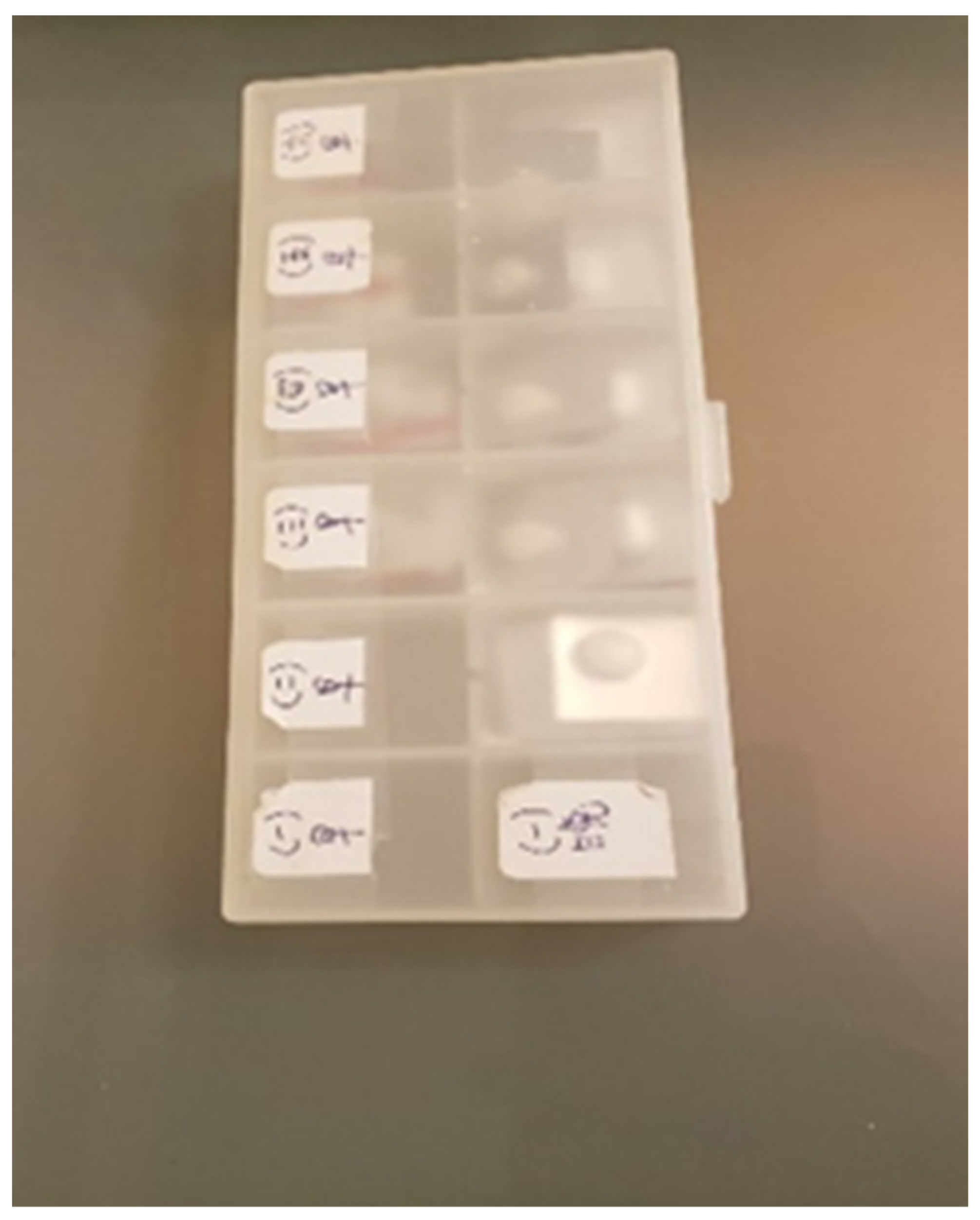
“My daughter moved to a dorm last week. I was worried about whether she would take her medicine on time. If she forgets, it will increase the chance of relapse. I contact her every day to find out how she is. One morning, I called her and she said that she had taken the medicine. However, that night, I noticed that she had not taken it. I was worried and I told her to take the medicine immediately. Then I reminded her to take her medicine next time and talked about the negative consequences of not taking her medicine on time. I was a bit annoyed because she did not tell me the facts. Luckily, the medicine was kept in a box so I could monitor it. I felt anxious about whether she could take care of herself and about the possibility of relapse. I have learned not to overreact in front of my daughter, even while feeling worried.”(Participant L)
3.2.6. Voice 6: I Find Space in Offering Care and Exercising Self-Care
“When I came home, I saw that the pot was open, and I asked my daughter why. My daughter got angry and complained that I did not understand her. … As he [my son] was sick, my daughter thought I cared for him only, and this sometimes made her angry. … I felt that I paid more attention to my son. This made my daughter think I was biased. … We all maybe need to understand and tolerate each other more. I am not biased at all. This scenario may happen time and time again.” (Participant E). (Authors note: in Chinese, an exploded pot has often been used as a metaphor to describe a heated quarrel or fight.)
“It was a bowl of congee. I received some pumpkins from my relatives in mainland China. I felt grateful that they were healthy. Actually, I cooked this for my daughter. However, she did not like it and she even complained about it in the interview with the clinical psychologist. I was fine and I realized that there were different expectations between my daughter and myself.”(Participant B)
3.3. Feedback and Comments from MBFPE Program Instructors
3.4. Feedback and Comments from Other Mindfulness-Based Program Instructors
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Leng, A.; Xu, C.; Nicholas, S.; Nicholas, J.; Wang, J. Quality of life in caregivers of a family member with serious mental illness: Evidence from China. Arch. Psychiatr. Nurs. 2019, 33, 23–29. [Google Scholar] [CrossRef]
- Saunders, J.C. Families living with severe mental illness: A literature review. Issues Ment. Health Nurs. 2003, 24, 175–198. [Google Scholar] [CrossRef] [PubMed]
- Koutra, K.; Vgontzas, A.N.; Lionis, C.; Triliva, S. Family functioning in first-episode psychosis: A systematic review of the literature. Soc. Psychiatry Psychiatr. Epidemiol. 2014, 49, 1023–1036. [Google Scholar] [CrossRef] [PubMed]
- Lally, J.; Ajnakina, O.; Stubbs, B.; Cullinane, M.; Murphy, K.C.; Gaughran, F.; Murray, R.M. Remission and recovery from first-episode psychosis in adults: Systematic review and meta-analysis of long-term outcome studies. Br. J. Psychiatry 2017, 211, 350–358. [Google Scholar] [CrossRef]
- Jansen, J.E.; Gleeson, J.; Cotton, S. Towards a better understanding of caregiver distress in early psychosis: A systematic review of the psychological factors involved. Clin. Psychol. Rev. 2015, 35, 56–66. [Google Scholar] [CrossRef] [PubMed]
- McCann, T.V.; Lubman, D.I.; Clark, E. First-time primary caregivers’ experience of caring for young adults with first-episode psychosis. Schizophr. Bull. 2011, 37, 381–388. [Google Scholar] [CrossRef]
- Chang, W.C.; Chan, S.S.I.; Hui, C.L.M.; Chan, S.K.W.; Lee, E.H.M.; Chen, E.Y.H. Prevalence and risk factors for violent behavior in young people presenting with first-episode psychosis in Hong Kong: A 3-year follow-up study. Aust. N. Z. J. Psychiatry 2015, 49, 914–922. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Amminger, G.P.; Aguilar-Gaxiola, S.; Alonso, J.; Lee, S.; Ustun, T.B. Age of onset of mental disorders: A review of recent literature. Curr. Opin. Psychiatry 2007, 20, 359–364. [Google Scholar] [CrossRef] [PubMed]
- Link, B.G.; Phelan, J.C. Conceptualizing stigma. Annu. Rev. Sociol. 2001, 27, 363–385. [Google Scholar] [CrossRef]
- Mak, W.W.; Cheung, R.Y. Psychological distress and subjective burden of caregivers of people with mental illness: The role of affiliate stigma and face concern. Community Ment. Health J. 2012, 48, 270–274. [Google Scholar] [CrossRef] [PubMed]
- Hwang, K.K. Guanxi and mientze: Conflict resolution in Chinese society. Intercult. Commun. Stud. 1998, 7, 17–42. [Google Scholar]
- Kung, W.W. Consideration of cultural factors in working with Chinese American families with a mentally ill patient. Fam. Soc. 2001, 82, 97–107. [Google Scholar] [CrossRef]
- Sue, S.; Sue, D. Cultural factors in the clinical assessment of Asian Americans. J. Consult. Clin. Psychol. 1987, 55, 479–487. [Google Scholar] [CrossRef] [PubMed]
- Chen, E.S.; Chang, W.C.; Hui, C.L.; Chan, S.K.; Lee, E.H.M.; Chen, E.Y. Self-stigma and affiliate stigma in first-episode psychosis patients and their caregivers. Soc. Psychiatry Psychiatr. Epidemiol. 2016, 51, 1225–1231. [Google Scholar] [CrossRef]
- Moudatsou, M.; Koukouli, S.; Palioka, E.; Pattakou, G.; Teleme, P.; Fasoi, G.; Kaba, E.; Stavropoulou, A. Caring for patients with psychosis: Mental health professionals’ views on informal caregivers’ needs. Int. J. Environ. Res. Public Health 2021, 18, 2964. [Google Scholar] [CrossRef] [PubMed]
- Wong, Y.L.I.; Kong, D.; Tu, L.; Frasso, R. “My bitterness is deeper than the ocean”: Understanding internalized stigma from the perspectives of persons with schizophrenia and their family caregivers. Int. J. Ment. Health Syst. 2018, 12, 14. [Google Scholar] [CrossRef]
- Okpokoro, U.; Adams, C.E.; Sampson, S. Family intervention (brief) for schizophrenia. Cochrane Database Syst. Rev. 2014, 3, CD009802. [Google Scholar]
- Sadath, A.; Muralidhar, D.; Varambally, S.; Jose, J.P.; Gangadhar, B.N. Family intervention in first-episode psychosis: A qualitative systematic review. Sage Open 2015, 5, 2158244015613108. [Google Scholar] [CrossRef]
- Harvey, C. Family psychoeducation for people living with schizophrenia and their families. BJ. Psych. Adv. 2018, 24, 9–19. [Google Scholar] [CrossRef]
- Brown, G.W.; Birley, J.L.; Wing, J.K. Influence of family life on the course of schizophrenic disorders: A replication. Br. J. Psychiatry 1972, 121, 241–258. [Google Scholar] [CrossRef] [PubMed]
- Hooley, J.M. Expressed emotion and relapse of psychopathology. Annu. Rev. Clin. Psychol. 2007, 3, 329–352. [Google Scholar] [CrossRef]
- Weintraub, M.J.; Hall, D.L.; Carbonella, J.Y.; Weisman de Mamani, A.; Hooley, J.M. Integrity of literature on expressed emotion and relapse in patients with schizophrenia verified by a p-curve analysis. Fam. Process 2007, 56, 436–444. [Google Scholar] [CrossRef] [PubMed]
- Bhugra, D.; McKenzie, K. Expressed emotion across cultures. In Clinical Topics in Cultural Psychiatry; Bhattacharya, R., Cross, S., Bhugra, D., Eds.; The Royal College of Psychiatrists: London, UK, 2010; pp. 52–67. [Google Scholar]
- Hinojosa-Marqués, L.; Domínguez-Martínez, T.; Kwapil, T.R.; Barrantes-Vidal, N. Predictors of criticism and emotional over-involvement in relatives of early psychosis patients. PLoS ONE 2020, 15, e0234325. [Google Scholar] [CrossRef] [PubMed]
- McNab, C.; Linszen, D. Family intervention in early psychosis. In The Recognition and Management of Early Psychosis; Jackson, H.J., McGorry, P.D., Eds.; Cambridge University Press: Cambridge, UK, 2009; pp. 305–330. [Google Scholar]
- Mountain, D.; Shah, P.J. Recovery and the medical model. Adv. Psychiatr. Treat. 2008, 14, 241–244. [Google Scholar] [CrossRef]
- Murray, G.; Leitan, N.D.; Thomas, N.; Michalak, E.E.; Johnson, S.L.; Jones, S.; Periche, T.; Berk, L.; Berk, M. Towards recovery-oriented psychosocial interventions for bipolar disorder: Quality of life outcomes, stage-sensitive treatments, and mindfulness mechanisms. Clin. Psychol. Rev. 2017, 52, 148–163. [Google Scholar] [CrossRef] [PubMed]
- Wciórka, J.; Świtaj, P.; Anczewska, M. The sense of empowerment in the early stage of recovery from psychosis. Psychosis 2015, 7, 249–260. [Google Scholar] [CrossRef]
- Lo, H.H.M.; Ho, W.C.; Lau, E.N.S.; Lo, C.W.; Mak, W.W.S.; Ng, S.M.; Wong, S.Y.-S.; Wong, J.O.Y.; Lui, S.S.Y.; Lo, C.S.L.; et al. A Brief Mindfulness-Based Family Psychoeducation Intervention for Chinese Young Adults with First Episode Psychosis: A Study Protocol. Front. Psychol. 2019, 10, 516. [Google Scholar] [CrossRef] [PubMed]
- Kabat-Zinn, J. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain and Illness, Revised and Updated Version; Bantam Books: New York, NY, USA, 2013; 720p. [Google Scholar]
- Roemer, L.; Williston, S.K.; Rollins, L.G. Mindfulness and emotion regulation. Curr. Opin. Psychol. 2015, 3, 52–57. [Google Scholar] [CrossRef]
- Bögels, S.M.; Hellemans, J.; van Deursen, S.; Römer, M.; van der Meulen, R. Mindful parenting in mental health care: Effects on parental and child psychopathology, parental stress, parenting, coparenting, and marital functioning. Mindfulness 2014, 5, 536–551. [Google Scholar] [CrossRef]
- Burgdorf, V.; Szabó, M.; Abbott, M.J. The effect of mindfulness interventions for parents on parenting stress and youth psychological outcomes: A systematic review and meta-analysis. Front. Psychol. 2019, 10, 1336. [Google Scholar] [CrossRef]
- Wang, C.C. Photovoice: A participatory action research strategy applied to women’s health. J. Womens Health 1999, 8, 185–192. [Google Scholar] [CrossRef]
- Baker, T.A.; Wang, C.C. Photovoice: Use of a participatory action research method to explore the chronic pain experience in older adults. Qual. Health Res. 2006, 16, 1405–1413. [Google Scholar] [CrossRef]
- Wang, C.C.; Pies, C.A. Family, maternal, and child health through photovoice. Matern. Child Health J. 2004, 8, 95–102. [Google Scholar] [CrossRef] [PubMed]
- Ho, W.C.; Rochelle, T.L.; Yuen, W.K. ‘We Are Not Sad at All’ Adolescents Talk about Their ‘City of Sadness’ through Photovoice. J. Adolesc. Res. 2011, 26, 727–765. [Google Scholar] [CrossRef]
- To, P.D.N.; Huynh, J.; Wu, J.T.C.; Vo Dang, T.; Lee, C.; Tanjasiri, S.P. Through Our Eyes, Hear Our Stories: A Virtual Photovoice Project to Document and Archive Asian American and Pacific Islander Community Experiences During COVID-19. Health Promot. Pract. 2022, 23, 289–295. [Google Scholar] [CrossRef] [PubMed]
- Catalani, C.; Minkler, M. Photovoice: A review of the literature in health and public health. Health Educ. Behav. 2020, 37, 424–451. [Google Scholar] [CrossRef] [PubMed]
- Kurtz, J.L. Seeing through new eyes: An experimental investigation of the benefits of photography. J. Basic Appl. Sci. 2015, 11, 354–358. [Google Scholar] [CrossRef]
- Liebenberg, L. Photovoice and Being Intentional About Empowerment. Health Promot. Pract. 2022, 23, 267–273. [Google Scholar] [CrossRef] [PubMed]
- Segal, Z.V.; Teasdale, J.D.; Williams, J.M. Mindfulness-Based Cognitive Therapy for Depression: A New Approach to Preventing Relapse, 2nd ed.; Guilford Press: New York, NY, USA, 2013; 471p. [Google Scholar]
- Wang, C.; Burris, M.A. Empowerment through photo novella: Portraits of participation. Health Educ. Q. 1994, 21, 171–186. [Google Scholar] [CrossRef]
- Petrakis, M.; Bloom, H.; Oxley, J. Family perceptions of benefits and barriers to first episode psychosis carer group participation. Soc. Work Ment. Health 2014, 12, 99–116. [Google Scholar] [CrossRef]
- Wang, C.C.; Cash, J.L.; Powers, L.S. Who knows the streets as well as the homeless? Promoting personal and community action through photovoice. Health Promot. Pract. 2000, 1, 81–89. [Google Scholar] [CrossRef]
- Bryman, A. Integrating quantitative and qualitative research: How is it done? Qual. Res. 2006, 6, 97–113. [Google Scholar] [CrossRef]
- Padgett, D.K. Qualitative Methods in Social Work Research, 2nd ed.; SAGE: Los Angeles, CA, USA, 2008; 304p. [Google Scholar]
- Charmaz, K. Constructing Grounded Theory: A Practical Guide through Qualitative Analysis; SAGE: London, UK, 2006; 208p. [Google Scholar]
- Boeije, H. A purposeful approach to the constant comparative method in the analysis of qualitative interviews. Qual. Quant. 2002, 367, 391–409. [Google Scholar] [CrossRef]
- Scardamalia, M. Collective cognitive responsibility for the advancement of knowledge. Lib. Educ. A Knowl. Soc. 2002, 97, 67–98. [Google Scholar]
- Balazs, C.L.; Morello-Frosch, R. The three Rs: How community-based participatory research strengthens the rigor, relevance, and reach of science. Environ. Justice 2013, 6, 9–16. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5), 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar] [CrossRef]
- Kabat-Zinn, M.; Kabat-Zinn, J. Everyday Blessings: The Inner Work of Mindful Parenting, Revised and Updated Version; Hachette Book: New York, NY, USA, 2014; 394p. [Google Scholar]
- Kate, N.; Grover, S.; Kulhara, P.; Nehra, R. Scale for positive aspects of caregiving experience: Development, reliability, and factor structure. East Asian Arch. Psychiatry 2012, 22, 62–69. [Google Scholar] [PubMed]
- Hawkes, E.; Heintz, H.; Vahia, I.V. Digitally enhanced art therapy and mindfulness in older adults. Am. J. Geriatr. Psychiatry 2020, 28, 495–496. [Google Scholar] [CrossRef] [PubMed]
- Nettleton, J.A.; Burton, A.E.; Povey, R.C. “No-one realises what we go through as Type 1s”: A qualitative photo-elicitation study on coping with diabetes. Diabetes Res. Clin. Pract. 2022, 187, 109876. [Google Scholar] [CrossRef] [PubMed]
- Yeh, Y.C.; Chang, C.Y.; Ting, Y.S.; Chen, S.Y. Effects of Mindful Learning Using a Smartphone Lens in Everyday Life and Beliefs toward Mobile based Learning on Creativity Enhancement. Educ. Technol. Soc. 2020, 23, 45–58. [Google Scholar]









| Participant | Sex | Age | Relationship to Person in Recovery | Age of Person in Recovery | Diagnosis of Person in Recovery |
|---|---|---|---|---|---|
| A | F | 41 | son | 15 | Schizophrenia |
| B | F | 45 | son | 18 | Schizophrenia |
| C | F | 49 | daughter | 22 | Schizophrenia |
| D | F | 60 | son | 30 | Schizophrenia |
| E | F | 53 | son | 27 | Psychosis |
| F | F | 60 | son | 26 | Psychosis |
| G | M | 57 | son | 27 | Psychosis |
| H | F | 48 | son | 21 | Schizophrenia, ASD, ADHD |
| I | F | 52 | son | 24 | Schizophrenia |
| J | F | 53 | son | 19 | Schizophrenia |
| K | M | 65 | son | 27 | Schizophrenia |
| L | M | 55 | daughter | 21 | Psychosis |
| M | F | 46 | son | 19 | Schizophrenia |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lo, H.H.M.; Liu, K.H.K.; Ho, W.C.; Lau, E.N.S.; Poon, M.F.; Lo, C.S.L.; Tam, H.S.W. Using Photovoice in a Mindfulness-Based Program to Understand the Experiences of Caregivers of Young Adults with Psychosis. Int. J. Environ. Res. Public Health 2022, 19, 15461. https://doi.org/10.3390/ijerph192315461
Lo HHM, Liu KHK, Ho WC, Lau ENS, Poon MF, Lo CSL, Tam HSW. Using Photovoice in a Mindfulness-Based Program to Understand the Experiences of Caregivers of Young Adults with Psychosis. International Journal of Environmental Research and Public Health. 2022; 19(23):15461. https://doi.org/10.3390/ijerph192315461
Chicago/Turabian StyleLo, Herman Hay Ming, Ken Ho Kan Liu, Wing Chung Ho, Elsa Ngar Sze Lau, Man Fai Poon, Cola Siu Lin Lo, and Hillman Shiu Wah Tam. 2022. "Using Photovoice in a Mindfulness-Based Program to Understand the Experiences of Caregivers of Young Adults with Psychosis" International Journal of Environmental Research and Public Health 19, no. 23: 15461. https://doi.org/10.3390/ijerph192315461
APA StyleLo, H. H. M., Liu, K. H. K., Ho, W. C., Lau, E. N. S., Poon, M. F., Lo, C. S. L., & Tam, H. S. W. (2022). Using Photovoice in a Mindfulness-Based Program to Understand the Experiences of Caregivers of Young Adults with Psychosis. International Journal of Environmental Research and Public Health, 19(23), 15461. https://doi.org/10.3390/ijerph192315461






