Association of BMI, Diet, Physical Activity, and Oral Hygiene Practices with DMFT Index of Male Dental Students at King Faisal University, Al-Ahsa
Abstract
1. Introduction
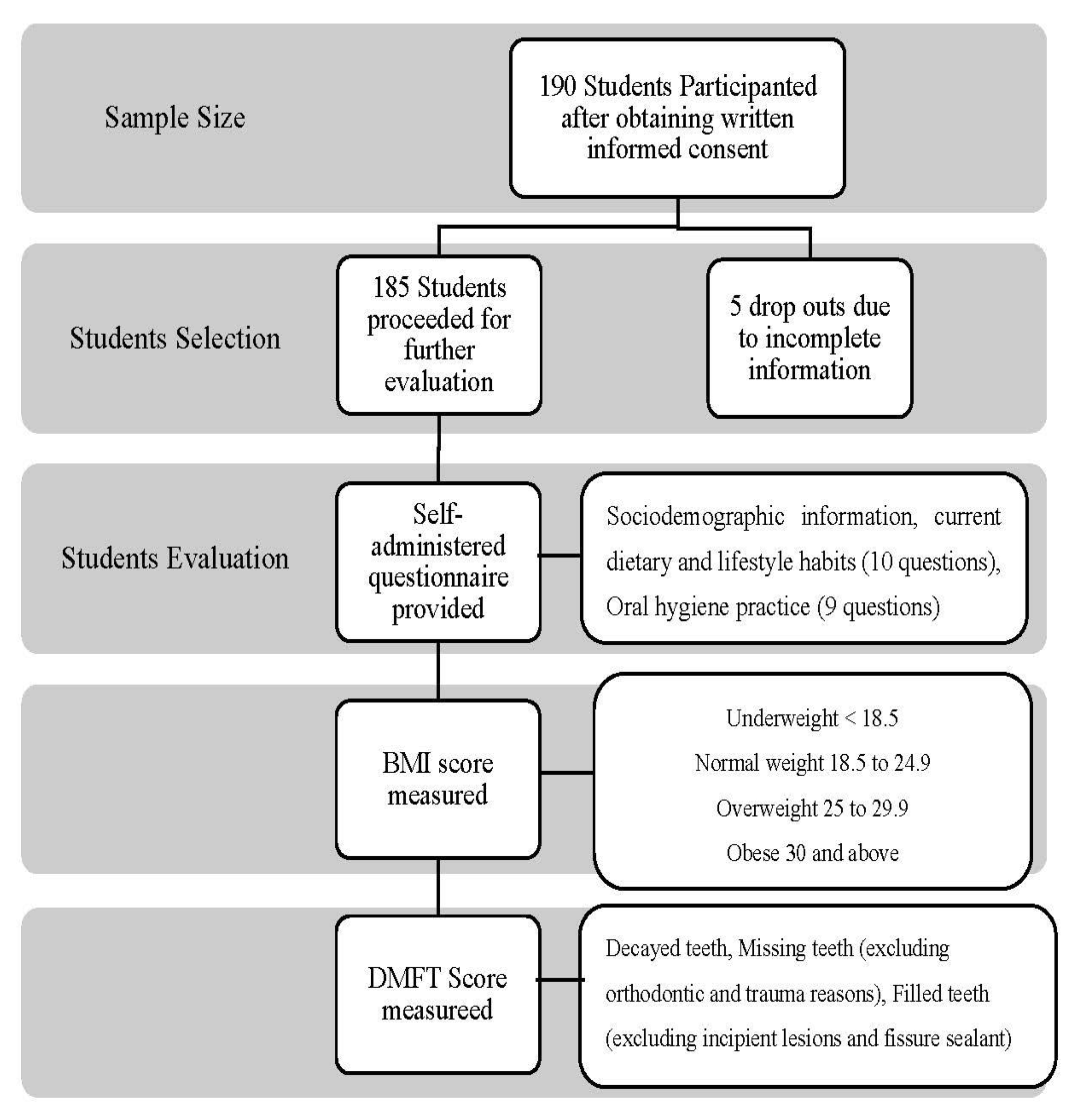
2. Materials and Methods
Statistical Analysis
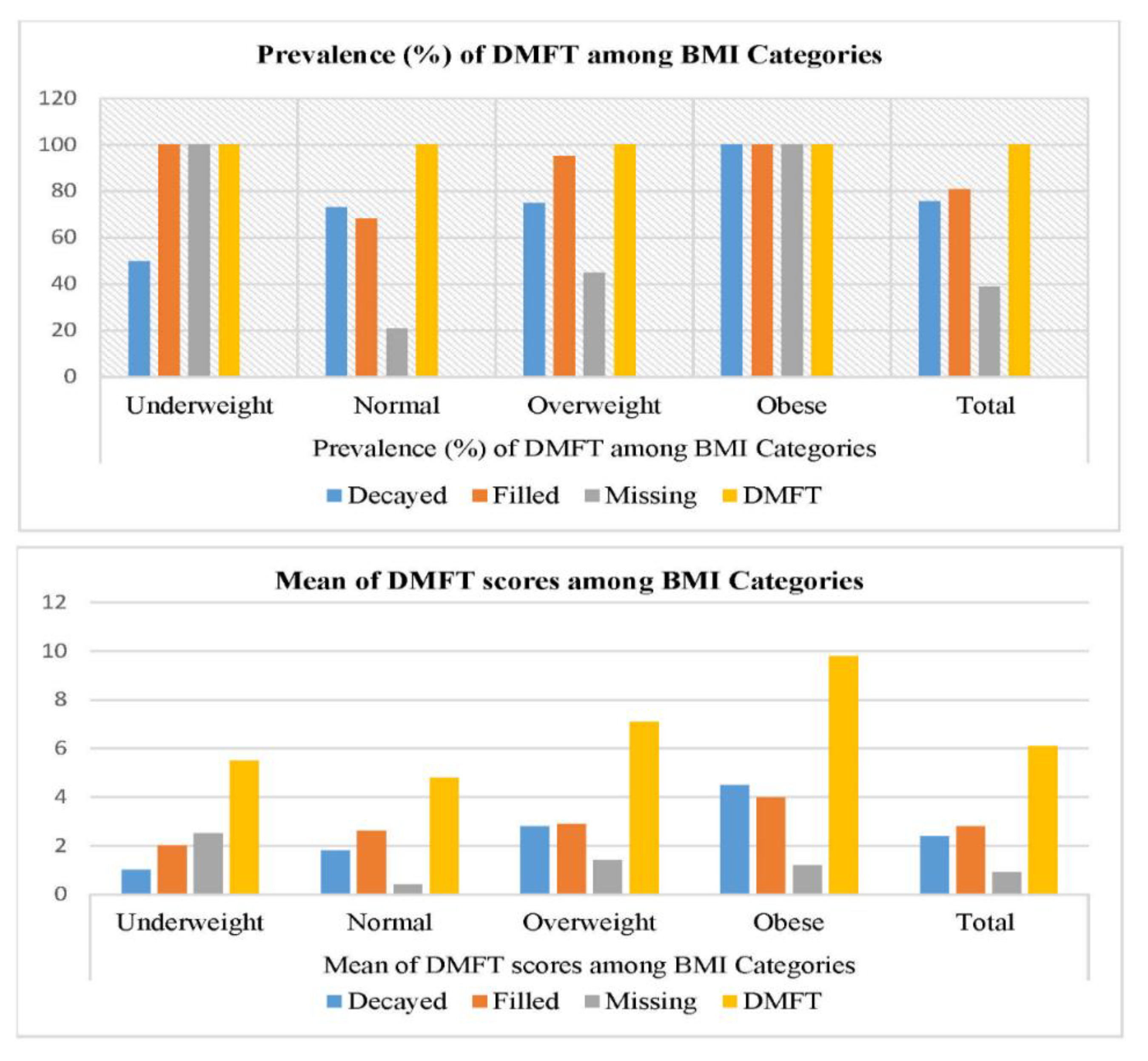
3. Results
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Al-Shehri, H.M.; Al-Qahtani, A.M.; Shaikh, I.A.; Hassan, M.A.; Al-Qahtani, N.S.; Al-Qahtani, A.M.; Alabas, M.A. Assessment of lifestyle and eating habits among undergraduate students in Najran University, Najran, Saudi Arabia. Int. J. Med. Sci. Pub. Health 2017, 6, 638–647. [Google Scholar]
- World Health Organization. Available online: www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 1 April 2020).
- Bhayat, A.; Ahmad, M.; Fadel, H. Association between body mass index, diet and dental caries in Grade 6 boys in Medina, Saudi Arabia. East. Mediterr. Health J. 2016, 22, 687–693. [Google Scholar] [CrossRef] [PubMed]
- Idrees, M.; Hammad, M.; Faden, A.; Kujan, O. Influence of body mass index on severity of dental caries: Cross-sectional study in healthy adults. Ann. Saudi Med. 2017, 37, 444–448. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Health Risks: Mortality and Burden of Disease Attributable to Selected Major Risks; World Health Organization: Geneva, Switzerland, 2009. [Google Scholar]
- Sangachin, M.G.; Cavuoto, L.A.; Wang, Y. Use of various obesity measurement and classification methods in occupational safety and health research: A systematic review of the literature. BMC Obes. 2018, 5, 28. [Google Scholar]
- Te Morenga, L.; Mallard, S.; Mann, J. Dietary sugars and body weight: Systematic review and meta-analyses of randomised controlled trials and cohort studies. BMJ 2013, 346, e7492. [Google Scholar] [CrossRef]
- Carson, S.J.; Abuhaloob, L.; Richards, D.; Hector, M.P.; Freeman, R. The relationship between childhood body weight and dental caries experience: An umbrella systematic review protocol. Syst. Rev. 2017, 6, 216. [Google Scholar] [CrossRef]
- Chen, D.; Zhi, Q.; Zhou, Y.; Tao, Y.; Wu, L.; Lin, H. Association between dental caries and BMI in children: A systematic review and meta-analysis. Caries Res. 2018, 52, 230–245. [Google Scholar] [CrossRef]
- Pullman, A.W.; Masters, R.C.; Zalot, L.C.; Carde, L.E.; Saraiva, M.M.; Dam, Y.Y.; Randall Simpson, J.A.; Duncan, A.M. Effect of the transition from high school to university on anthropometric and lifestyle variables in males. Appl. Physiol. Nutr. Metab. 2009, 34, 162–171. [Google Scholar] [CrossRef]
- Irwin, J.D. The prevalence of physical activity maintenance in a sample of university students: A longitudinal study. J. Am. Collage Health 2007, 56, 37–42. [Google Scholar] [CrossRef]
- Steptoe, A.; Wardle, J. Health behaviour, risk awareness and emotional well-being in students from Eastern Europe and Western Europe. Soc. Sci Med. 2001, 53, 1621–1630. [Google Scholar] [CrossRef]
- Rivera-Rivera, L.; Allen, B.; Rodríguez-Ortega, G.; Chávez-Ayala, R.; Lazcano-Ponce, E. Dating violence and associations with depression and risk behaviors: Female students in Morelos, Mexico. Salud. Publica Mex. 2006, 48, 288–296. [Google Scholar] [CrossRef][Green Version]
- World Health Organization. Sugars and Dental Caries. Available online: http://www.who.int/news-room/fact-sheets/detail/sugars-and-dental-caries (accessed on 20 September 2017).
- Shaghaghian, S.; Abolvardi, M.; Akhlaghian, M. Factors affecting dental caries of preschool children in Shiraz, 2014. J. Dent. (Shiraz) 2018, 19, 100. [Google Scholar]
- Ghani, B.; Jouhar, R.; Ahmed, N. Relationship of Facial Skin Complexion with Gingiva and Tooth Shade on Smile Attractiveness. J. Interdiscipl. Med. Dent. Sci. 2016, 4, 2. [Google Scholar] [CrossRef]
- Jamil, S.; Jouhar, R.; Gandhi, D.; Tahira, T.; Shaikh, J. Comparison between the mean postoperative pain score with two different file systems in patients with irreversible pulpitis-a clinical study in Altamash Institute of Dental Medicine. Prof. Med. J. 2019, 26, 1359–1364. [Google Scholar] [CrossRef]
- Ahmed, J.; Ali, S.A.; Jouhar, R.; Shah, H. Clinical Assessment Of Bonding Agent v/s Fluoride Varnish in Dentinal Hypersensitivity. J. Bahria Uni. Med. Dent. Collage 2019, 7, 53. [Google Scholar]
- Moradi, G.; Bolbanabad, A.M.; Moinafshar, A.; Adabi, H.; Sharafi, M.; Zareie, B. Evaluation of Oral Health Status Based on the Decayed, Missing and Filled Teeth (DMFT) Index. Iran. J. Public Health 2019, 48, 2050. [Google Scholar] [PubMed]
- Wahid, U.; Amin, M.; Choudhry, Z.; Ahmed, M.A. Dental anxiety level of patients presenting to operative dentistry department. Pak. Oral Dent. J. 2015, 35, 675–680. [Google Scholar]
- Wang, P.; Lin, H.C.; Chen, J.H.; Liang, H.Y. The prevalence of dental erosion and associated risk factors in 12-13-year-old school children in Southern China. BMC Public Health 2010, 10, 478. [Google Scholar] [CrossRef] [PubMed]
- Kitasako, Y.; Sasaki, Y.; Takagaki, T.; Sadr, A.; Tagami, J. Age-specific prevalence of erosive tooth wear by acidic diet and gastroesophageal reflux in Japan. J. Dent. 2015, 43, 418–423. [Google Scholar] [CrossRef] [PubMed]
- Wilder, R.S.; O’Donnell, J.A.; Barry, J.M.; Galli, D.M.; Hakim, F.F.; Holyfield, L.J.; Robbins, M.R. Is dentistry at risk? A case for interprofessional education. J. Dent. Educ. 2008, 72, 1231–1237. [Google Scholar] [CrossRef]
- Yoshida, T.; Milgrom, P.; Coldwell, S. How do US and Canadian dental schools teach interpersonal communication skills? J. Dent. Educ. 2002, 66, 1281–1288. [Google Scholar] [CrossRef] [PubMed]
- Kassebaum, D.K.; Hendricson, W.D.; Taft, T.; Haden, N.K. The dental curriculum at North American dental institutions in 2002–03: A survey of current structure, recent innovations, and planned changes. J. Dent. Educ. 2004, 68, 914–931. [Google Scholar] [CrossRef] [PubMed]
- Al-Madi, E.M.; AlJamie, M.; Al-Dukhail, S.; Mohammed, Z.; Abubakr, N.H. Dietary Habits and Oral Hygiene Practice amongst Dental Students at the College of Dentistry, Princess Nourah University. Open J. Stomato. 2016, 6, 28–35. [Google Scholar] [CrossRef][Green Version]
- Ashour, N.A.; Ashour, A.A.; Basha, S. Association between body mass index and dental caries among special care female children in Makkah City. Ann. Saudi Med. 2018, 38, 28–35. [Google Scholar] [CrossRef] [PubMed]
- Word Bank. Taxes on Sugar-Sweetened Beverages: Summary of International Evidence and Experiences; World Bank: Washington, DC, USA, 2020. [Google Scholar] [CrossRef]
- Moynihan, P. Sugars and dental caries: Evidence for setting a recommended threshold for intake. Adv. Nutr. 2016, 7, 149–156. [Google Scholar] [CrossRef] [PubMed]
- Silva, A.E.R.; Menezes, A.M.B.; Demarco, F.F.; Vargas-Ferreira, F.; Peres, M.A. Obesity and dental caries: Systematic review. Rev. Saude Publica 2013, 47, 799–812. [Google Scholar] [CrossRef]
- Willershausen, B.; Moschos, D.; Azrak, B.; Blettner, M. Correlation between oral health and body mass index (BMI) in 2071 primary school pupils. Eur. J. Med. Res. 2007, 12, 295. [Google Scholar]
- Thippeswamy, H.; Kumar, N.; Acharya, S.; Pentapati, K. Relationship between body mass index and dental caries among adolescent children in South India. West Indian Med. J. 2011, 60, 91–97. [Google Scholar]
- Sede, M.; Ehizele, A. Relationship between obesity and oral diseases. Niger. J. Clin. Pract. 2014, 17, 683–690. [Google Scholar]
- Macek, M.D.; Mitola, D.J. Exploring the association between overweight and dental caries among US children. Pediatr Dent. 2006, 28, 375–380. [Google Scholar]
- Almerich-Torres, T.; Bellot-Arcís, C.; Almerich-Silla, J.M. Relationship between caries, body mass index and social class in Spanish children. GAC Sanit. 2017, 31, 499–504. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Al Othaimeen, A.; Al Nozha, M.; Osman, A. Obesity: An emerging problem in Saudi Arabia. Analysis of data from the National Nutrition Survey. East. Mediterr. Health J. 2007, 13, 441–448. [Google Scholar] [PubMed]
- Al-Agha, A.; Bo, T.; Aiash, D.; Mandourah, L.; Abukhalil, N. The effect of socioeconomic status, number of siblings and parental of education on children’body mass index at Jeddah, Saudi Arabia: Cross sectional study. Fam. Med. Med. Sci. Res. 2015, 4, 5. [Google Scholar] [CrossRef]
- Al-Agha, A.E.; Alzahrani, H.K.; Rajab, F.S.; Taher, A.; Mesawa, A.H.A.; Almarri, A.K.; Kutbi, R.E.; Almutiri, A.A.; Alahdali, H.A.; Bashlawi, S.A. Parental socioeconomic status and occupation in relation to childhood obesity. Int. J. Mod. Res. Dev. 2020, 4, 576–585. [Google Scholar]
- Sallis, J.F.; Nader, P.R. Family determinants of health behaviors. In Health Behavior; Springer: New York, NY, USA, 1988; pp. 107–124. [Google Scholar]
- Kim, T.J.; von dem Knesebeck, O. Income and obesity: What is the direction of the relationship? A systematic review and meta-analysis. BMJ Open 2018, 8, e019862. [Google Scholar]
- Asiseh, F.; Yao, J. Family income and body mass index–what have we learned from China. Health Econ. Rev. 2016, 6, 52. [Google Scholar] [CrossRef][Green Version]
- Jackson, C.L.; Hu, F.B. Long-term associations of nut consumption with body weight and obesity. Am. J. Clin. Nutr. 2014, 100, 408S–411S. [Google Scholar] [CrossRef]
- Bartlett, D.; Fares, J.; Shirodaria, S.; Chiu, K.; Ahmad, N.; Sherriff, M. The association of tooth wear, diet and dietary habits in adults aged 18–30 years old. J. Dent. 2011, 39, 811–816. [Google Scholar] [CrossRef]
- Lupi, S.; Bagordo, F.; Stefanati, A.; Grassi, T.; Piccinni, L.; Bergamini, M.; Donno, A.D. Assessment of lifestyle and eating habits among undergraduate students in northern Italy. Ann. Ist. Super. Sanita 2015, 51, 154–161. [Google Scholar]
- Ahmed, H.S.; Khalid, M.E.; Osman, O.M.; Ballal, M.A.; Al-Hashem, F.H. The association between physical activity and overweight and obesity in a population of children at high and low altitudes in Southwestern Saudi Arabia. J. Fam. Community Med. 2016, 23, 82. [Google Scholar]
- Ferrazzano, G.F.; Sangianantoni, G.; Cantile, T.; Ingenito, A. Relationship Between Social and Behavioural Factors and Caries Experience in Schoolchildren in Italy. Oral Health Prev. Dent. 2016, 1, 55–61. [Google Scholar]
- Paisi, M.; Kay, E.; Bennett, C.; Kaimi, I.; Witton, R.; Nelder, R.; Lapthorne, D. Body mass index and dental caries in young people: A systematic review. BMC Pediatr. 2019, 19, 122. [Google Scholar] [CrossRef] [PubMed]
- Kantovitz, K.R.; Pascon, F.M.; Rontani, R.M.P.; Gaviao, M.B.D.; Pascon, F.M. Obesity and dental caries--A systematic review. Oral Health Prev. Dent. 2006, 4, 137–144. [Google Scholar] [PubMed]
- Hooley, M.; Skouteris, H.; Boganin, C.; Satur, J.; Kilpatrick, N. Body mass index and dental caries in children and adolescents: A systematic review of literature published 2004 to 2011. Syst. Rev. 2012, 1, 57. [Google Scholar] [CrossRef]
- Alghamdi, A.A.; Almahdy, A. Association Between Dental Caries and Body Mass Index in Schoolchildren Aged Between 14 and 16 Years in Riyadh, Saudi Arabia. J. Clin. Med. Res. 2017, 12, 981–986. [Google Scholar] [CrossRef]
- Sakeenabi, B.; Swamy, H.S.; Mohammed, R.N. Association between obesity, dental caries and socioeconomic status in 6-and 13-year-old school children. Oral Health Prev. Dent. 2012, 10, 231–241. [Google Scholar]
- Honne, T.; Pentapati, K.; Kumar, N.; Acharya, S. Relationship between obesity/overweight status, sugar consumption and dental caries among adolescents in South India. Int. J. Dent. Hyg. 2012, 10, 240–244. [Google Scholar] [CrossRef]
| Variables | BMI Categories (Kg/m2) | |||||
| Underweight | Normal | Overweight | Obese | Total | p-Value | |
| 6 (3.2) | 101 (54.6) | 60 (32.4) | 18 (9.7) | 185 (100) | ||
| 17.83 ± 0.41 | 22.73 ± 1.31 | 27.38 ± 0.98 | 31.61 ± 1.11 | 24.94 ± 3.36 | <0.001 | |
| Age (Years) | 22.33 ± 2.58 | 22.28 ± 2.03 | 22.38 ± 2.28 | 22.29 ± 2.13 | 22.29 ± 2.13 | 0.931 |
| Age group 1 (19–22 years) | 3 (50) | 50 (49.5) | 27 (45) | 11 (61) | 91 (49.2) | 0.694 |
| Age group 2 (23–26 years) | 3 (50) | 51 (50.5) | 33 (55) | 7 (38.9) | 94 (50.8) | |
| BDS Year of Education | ||||||
| Year 1 | 1 (16.7) | 15 (14.9) | 10 (16.7) | 4 (22.2) | 30 (16.2) | 0.827 |
| Year 2 | 1 (16.7) | 14 (13.9) | 9 (15.0) | 1 (5.6) | 25 (13.5) | |
| Year 3 | 0 | 15 (14.9) | 6 (10.0) | 5 (27.8) | 26 (14.1) | |
| Year 4 | 2 (33.3) | 15 (14.9) | 6 (10.0) | 1 (5.6) | 24 (13.0) | |
| Year 5 | 1 (16.7) | 30 (29.7) | 20 (33.3) | 5 (27.8) | 56 (30.3) | |
| Internees | 1 (16.7) | 12 (11.9) | 9 (15.0) | 2 (11.1) | 24 (13) | |
| Sibling | ||||||
| 5/1 | 4 (66.7) | 60 (59.4) | 34 (56.7) | 8 (44.4) | 106 (57.3) | 0.216 |
| 10/6 | 1 (16.7) | 39 (38.6) | 22 (36.7) | 10 (55.6) | 72 (38.9) | |
| >10 | 1 (16.7) | 2 (2.0) | 4 (6.7) | 0 | 7 (3.8) | |
| Father Education | ||||||
| No Education | 3 (50) | 27 (26.7) | 3 (5.0) | 0 | 33 (17.8) | <0.001 |
| School level | 0 | 9 (8.9) | 15 (25) | 9 (50) | 33 (17.8) | |
| College level | 0 | 17 (16.8) | 15 (25) | 6 (33.3) | 38 (20.5) | |
| University level | 3 (50) | 48 (47.5) | 27 (45) | 3 (16.7) | 81 (43.8) | |
| Mother Education | ||||||
| No Education | 3 (50) | 36 (35.6) | 21 (35) | 0 | 60 (32.4) | <0.001 |
| School level | 3 (50) | 21 (20.8) | 21 (35) | 15 (83.3) | 60 (32.4) | |
| College level | 0 | 9 (8.9) | 0 | 0 | 9 (4.9) | |
| University level | 0 | 35 (34.7) | 18 (30) | 3 (16.7) | 56 (30.3) | |
| Father Occupation | ||||||
| Government Service | 6 (100) | 62 (61.4) | 36 (60) | 15 (83.3) | 119 (64.3) | 0.013 |
| Private Service | 0 | 15 (25.0) | 15 (25) | 0 | 30 (16.2) | |
| Business | 0 | 15 (14.9) | 9 (15) | 0 | 24 (13.0) | |
| Others | 0 | 9 (8.9) | 0 | 3 (16.7) | 12 (6.5) | |
| Mother Occupation | ||||||
| Government Service | 0 | 29 (28.7) | 12 (20) | 0 | 41 (22.2) | 0.077 |
| Private Service | 0 | 3 (3) | 3 (5) | 0 | 6 (3.2) | |
| Business | 0 | 0 | 0 | 0 | 0 | |
| Others (house wife) | 6 (100) | 69 (68.3) | 45 (75) | 18 (100) | 138 (74.6) | |
| Family Income | ||||||
| <10,000 | 3 (50) | 27 (26.7) | 12 (20) | 0 | 42 (22.7) | |
| 10,001–20,000 | 3 (50) | 42 (41.6) | 33 (55) | 18 (100) | 96 (51.9) | 0.001 |
| 20,000–30,000 | 0 | 26 (25.7) | 9 (15) | 0 | 35 (18.9) | |
| >30,000 | 0 | 6 (5.9) | 6 (10) | 0 | 12 (6.5) | |
| BMI Categories (Kg/m2) | |||||
| Variables | Underweight | Normal | Overweight | Obese | p-Value |
| 6 (3.2) | 101 (54.6) | 60 (32.4) | 18 (9.7) | ||
| Frequency of main meals | |||||
| 1 meal /day | 0 | 12 (11.9) | 3 (5) | 0 | 0.034 |
| 2 meals/day | 0 | 41 (40.6) | 18 (30) | 6 (33.3) | |
| 3 meals / day | 6 (100) | 48 (47.5) | 36 (60) | 12 (66.7) | |
| >3 meals/day | 0 | 0 | 3 (5) | 0 | |
| Use of Snacks in between meals | 6 (100) | 98 (97) | 60 (100) | 15(83.3) | 0.006 |
| Raw vegetables | 3 (50) | 63 (62.4) | 27 (45) | 6(33.3) | 0.048 |
| Fruits | 6 (100) | 77 (76.2) | 48 (80) | 12 (66.7) | 0.347 |
| Nuts | 0 | 56 (55.4) | 36 (60) | 15 (83.3) | 0.004 |
| Eggs | 3 (50) | 48 (47.5) | 36 (36.4) | 12 (66.7) | 0.289 |
| Yogurt plain | 3 (50) | 51 (50.5) | 42 (70) | 15 (83.3) | 0.014 |
| Yogurt fruit | 6 (100) | 24 (23.8) | 9 (15) | 0 | 0.047 |
| Chocolate | 3 (50) | 83 (82.2) | 48 (80) | 18 (100) | 0.04 |
| Smoothies | 0 | 42 (41.6) | 15 (25) | 9 (50) | 0.024 |
| Cheese | 3 (50) | 48 (47.5) | 42 (70) | 12 (66.7) | 0.035 |
| Ice cream | 3 (50) | 57 (56.4) | 36 (60) | 18 (100) | 0.005 |
| Popcorn | 0 | 36 (35.6) | 21 (35) | 3 (16.7) | 0.134 |
| Candy | 0 | 30 (29.7) | 42 (70) | 18 (100) | 0 |
| Soft drink | 0 | 50 (49.5) | 48 (80) | 18 (100) | 0 |
| Juice | 6 (100) | 65 (64.4) | 42 (70) | 15 (83.3) | 0.139 |
| Chips | 3 (50) | 50 (49.5) | 33 (55) | 18 (100) | 0.001 |
| Use of Drinks | |||||
| Lemon Juice | 3 (50) | 42 (41.6) | 33 (55) | 3 (16.7) | 0.033 |
| Orange Juice | 0 | 9 (8.9) | 6 (10) | 3 (16.7) | 0.634 |
| Green tea with sugar | 0 | 9 (8.9) | 9 (15) | 3 (16.7) | 0.446 |
| Green tea without sugar | 0 | 29 (28.7) | 12 (20) | 3 (16.7) | 0.24 |
| Black Coffee with sugar | 0 | 3 (3) | 15(25) | 3 (16.7) | 0 |
| Black Coffee without sugar | 3 (50) | 62 (61.4) | 24 (40) | 12 (66.7) | 0.043 |
| Arabic tea non-sugary | 0 | 59 (58.4) | 30 (50) | 9 (50) | 0.041 |
| Soft drinks | 0 | 47 (46.5) | 51 (85) | 15 (83.3) | 0 |
| Hold drink in mouth (yes) | 6 (100) | 53 (52.3) | 21 (35) | 18 (100) | 0 |
| Hold for <1 min | 3 (50) | 53 (52.3) | 21 (35) | 3 (16.7) | 0.015 |
| Hold for >1 min | 3 (50) | 48 (47.5) | 39 (65) | 15 (83.3) | |
| Frequency of Sweets | |||||
| Chocolate bar | 3 (50) | 77 (76.2) | 54 (90) | 18 (100) | 0.004 |
| Candy | 3 (50) | 36 (35.6) | 42 (70) | 18 (100) | 0 |
| Dates | 6 (100) | 77 (76.5) | 51 (85) | 18 (100) | 0.047 |
| Other sweets | 0 | 3 (3) | 6 (10) | 3 (16.7) | 0.08 |
| Physical Activity on week days | |||||
| None | 3 (50) | 6 (5.9) | 18 (30) | 12 (66.7) | 0 |
| <30 min | 0 | 24 (23.8) | 18 (30) | 6 (30.3) | |
| >30 min | 3 (50) | 71 (70.3) | 24 (40) | 0 | |
| Physical Activity on week end | |||||
| None | 0 | 3 (3) | 18 (30) | 3 (16.7) | 0 |
| <30 min | 3 (50) | 18 (17.8) | 12 (20) | 9 (50) | |
| >30 min | 3 (50) | 80 (79.2) | 30 (50) | 6 (33.3) | |
| Watch TV, Play Video games on week days | |||||
| None | 0 | 23 (22.8) | 6 (10) | 3 (16.7) | 0.025 |
| <30 min | 3 (50) | 24 (23.8) | 12 (20) | 15 (83.3) | |
| >30 min | 3 (50) | 54 (53.5) | 42 (70) | 0 | |
| Watch TV, Play Video games on week end | |||||
| None | 0 | 14 (13.9) | 0 | 0 | 0.02 |
| <30 min | 0 | 21 (20.8) | 12 (20) | 3 (16.7) | |
| >30 min | 6 (100) | 66 (65.3) | 48 (80) | 15 (83.3) | |
| Use Sugar free chew gum | 3 (50) | 44 (43.6) | 36 (60) | 9 (50) | 0.254 |
| BMI Categories (Kg/m2) | |||||
| Variables | Underweight | Normal | Overweight | Obese | p-Value |
| 6 (3.2) | 101 (54.6) | 60 (32.4) | 18 (9.7) | ||
| Tooth Brushing | |||||
| None | 0 | 0 | 3 (5) | 0 | 0 |
| Once daily | 0 | 23 (22.8) | 36 (60) | 15 (83.3) | |
| Twice daily | 3 (50) | 63 (62.4) | 18 (30) | 3 (16.7) | |
| >Twice daily | 3 (50) | 15 (14.9) | 3 (5) | 0 | |
| Miswak | |||||
| None | 6 | 57 (56.4) | 39 (65) | 9 (50) | 0.242 |
| Daily | 0 | 3 (3) | 3 (5) | 0 | |
| Occasionally | 0 | 41 (40.6) | 18 (30) | 9 (50) | |
| Brushing Technique | |||||
| Bass | 0 | 0 | 6 (10) | 0 | 0 |
| Modified Bass | 6 (100) | 95 (94.1) | 36 (60) | 12 (66.7) | |
| Stillman | 0 | 0 | 3 (5) | 0 | |
| Modified Stillman | 0 | 0 | 9 (15) | 0 | |
| Charters | 0 | 3 (3) | 3 (5) | 3 (16.7) | |
| Rolling | 0 | 3 (3) | 3 (3) | 0 | |
| Horizontal | 0 | 0 | 0 | 3 (16.70 | |
| Type of Toothpaste | |||||
| Fluoridated | 6 (100) | 92 (91.1) | 48 (80) | 12 (66.7) | 0.003 |
| Non-fluoridated | 0 | 3 (3) | 0 | 0 | |
| Anti-sensitive | 0 | 3 (3) | 3 (5) | 0 | |
| Others | 0 | 0 | 3 (5) | 0 | |
| Do not know | 0 | 3 (3) | 6 (10) | 6 (33.3) | |
| Type of Tooth brush | |||||
| Extra-soft | 3 (50) | 15 (14.9) | 9 (15) | 0 | 0 |
| Soft | 3 (50) | 45 (44.6) | 39 (65) | 3 (16.7) | |
| Medium | 0 | 35 (34.7) | 12 (20) | 15 (83.3) | |
| Electric | 0 | 6 (5.9) | 0 | 0 | |
| Brush Change time | |||||
| Once in 3 months | 6 (100) | 50 (45) | 27 (45) | 6 (33.3) | 0.001 |
| Once in 6 months | 0 | 45 (44.6) | 30 (50) | 6 (33.3) | |
| Once in year | 0 | 6 (5.9) | 3 (5) | 6 (66.3) | |
| Interdental Cleaning Aid Name | |||||
| Flossing | 3 (50) | 18 (17.8) | 15 (25) | 18 (100) | 0 |
| Wooden toothpick | 0 | 44 (43.6) | 21 (35) | 0 | |
| Plastic toothpick with floss | 0 | 6 (5.9) | 6 (10) | 0 | |
| Water-pick | 0 | 6 (5.9) | 3 (5) | 0 | |
| Interdental brush | 3 (50) | 27 (26.7) | 15 (25) | 0 | |
| Use Mouthwash | |||||
| None | 3 (50) | 42 (41.6) | 24 (40) | 6 (33.3) | 0.415 |
| Once daily | 0 | 15 (14.9) | 6 (10) | 0 | |
| Occasionally | 3 (50) | 44 (43.6) | 30 (50) | 12 (66.7) | |
| Dental Visit | |||||
| Every 3 months | 0 | 12 (11.9) | 3 (5) | 0 | 0 |
| Every 6 months | 6 (100) | 42 (41.6) | 15 (25) | 0 | |
| Every year | 0 | 20 (19.8) | 18 (30) | 3 (16.7) | |
| Only when required | 0 | 24 (23.8) | 24 (40) | 15 (83.3) | |
| Never | 0 | 3 (3) | 0 | 0 | |
| Model | Unstandardized Coefficients | Standardized Coefficients | t | Sig. | 95.0% Confidence Interval for B | ||
|---|---|---|---|---|---|---|---|
| B | Std. Error | Beta | Lower Bound | Upper Bound | |||
| BMI & Decayed teeth | 0.228 | 0.045 | 0.353 | 5.112 | 0.000 | 0.140 | 0.315 |
| BMI & Missing Teeth | 0.049 | 0.032 | 0.112 | 1.523 | 0.676 | 0.014 | 0.112 |
| BMI & Filled Teeth | 0.118 | 0.055 | 0.157 | 2.154 | 0.033 | 0.010 | 0.225 |
| BMI & DMFT | 0.394 | 0.082 | 0.336 | 4.822 | 0.000 | 0.233 | 0.555 |
| Decayed (Yes/No) | Missing (Yes/No) | Filled (Yes/No) | ||||
|---|---|---|---|---|---|---|
| Variables | n | Adjusted OR | n | Adjusted OR | n | Adjusted OR |
| (C.I. 95%) | (C.I. 95%) | (C.I. 95%) | ||||
| BMI | ||||||
| Underweight and Normal weight # | 77/30 | 1.41(0.5–3.50) | 27/80 | 3.99(1.80–8.82) ** | 75/32 | 9.23(2.30–37.03) ** |
| Overweight and Obese | 63/15 | 45/33 | 75/3 | |||
| Toothbrush time | ||||||
| 1 time daily # | 65/12 | 0.90(0.3–2.30) | 39/38 | 1.23(0.54–2.81) | 69/8 | 0.75(0.26–2.14) |
| ≥2 times daily | 75/33 | 33/75 | 81/27 | |||
| Toothbrush type | ||||||
| Extra or soft # | 78/39 | 6.05(2.1–16.9) ** | 45/72 | 1.06(0.49–2.26) | 99/18 | 0.48(0.20–1.14) |
| Medium or hard | 62/6 | 27/41 | 51/17 | |||
| Fluoridated toothpaste | ||||||
| Yes # | 119/42 | 0.17(0.02–0.10) | 60/101 | 0.38(0.13–1.13) | 129/32 | 0.42(0.07–2.30) |
| Other | 21/3 | 12/12 | 21/3 | |||
| Interdental cleaning | ||||||
| Dental floss # | 63/3 | 0.14(0.01–0.25) ** | 42/24 | 0.17(0.07–0.37) ** | 60/6 | 0.33(0.10–1.10) |
| Other | 77/42 | 30/89 | 90/29 | |||
| Socioeconomic Status | ||||||
| Father Education (Yes) # | 122/30 | 3.38(1.53–7.79) * | 60/92 | 1.14(0.05–2.49) | 126/26 | 1.81(0.75–4.33) |
| Mother Education (Yes) # | 92/33 | 0.89(0.68–1.16) | 45/80 | 6.68(0.36–1.28) | 99/26 | 0.67(0.29–1.54) |
| Father Occupation (Yes) # | 140/45 | 0.92(0.65–1.31) | 72/113 | 1.18(0.86–1.61) | 150/35 | 0.73(0.51–1.05) |
| Mother Occupation (Yes) # | 32/15 | 0.59(0.28–1.23) | 9/38 | 0.28(0.17–0.62) ** | 33/14 | 0.45(0.19–0.92) ** |
| Family Income (>10,000) # | 116/27 | 3.22(1.53–6.75) * | 54/89 | 0.80(0.40–1.62) | 120/23 | 2.08(0.93–4.68) |
| Frequency of Sweets | ||||||
| Chocolate bar (Yes) # | 116/36 | 1.20(0.51–2.83) | 60/92 | 1.14(0.52–2.49) | 120/32 | 0.37(0.10–1.30) |
| Candy (Yes) # | 78/12 | 3.46(1.65–7.25) ** | 54/36 | 6.14(3.30–12.46) * | 78/12 | 2.07(0.96–4.46) |
| Dates (Yes) # | 125/27 | 5.55(2.49–12.30) ** | 60/92 | 1.10(0.50–2.10) | 132/20 | 5.50(2.39–12.62) |
| Other sweets (Yes) # | 9/3 | 0.96(0.24–3.71) | 6/6 | 1.62(0.50–5.23) | 12/10 | ---- |
| Physical Activity (Moderate Level) | ||||||
| On weekdays (Yes) # | 110/36 | 0.91(0.39–2.10) | 45/101 | 0.19(0.09–0.42) ** | 114/32 | 0.29(0.08–1.02) |
| On weekend (Yes) # | 128/33 | 3.8(1.59–9.41) ** | 63/92 | 1.07(0.44–2.59) | 129/32 | 0.57(0.16–2.05) |
| Watch TV play videogames | ||||||
| On weekdays (Yes) # | 111/42 | 0.27(0.07–0.94) ** | 69/84 | 7.94(2.32–27.80) | 129/24 | 2.81(1.20–6.58) ** |
| On weekend (Yes) # | 126/45 | 0.15(0.05–0.74) | 72/99 | 0.21(0.11–0.38) | 138/33 | 0.69(0.14–3.24) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jouhar, R.; Ahmed, M.A.; Khurshid, Z.; Bokhari, S.A.H. Association of BMI, Diet, Physical Activity, and Oral Hygiene Practices with DMFT Index of Male Dental Students at King Faisal University, Al-Ahsa. Nutrients 2021, 13, 224. https://doi.org/10.3390/nu13010224
Jouhar R, Ahmed MA, Khurshid Z, Bokhari SAH. Association of BMI, Diet, Physical Activity, and Oral Hygiene Practices with DMFT Index of Male Dental Students at King Faisal University, Al-Ahsa. Nutrients. 2021; 13(1):224. https://doi.org/10.3390/nu13010224
Chicago/Turabian StyleJouhar, Rizwan, Muhammad Adeel Ahmed, Zohaib Khurshid, and Syed Akhtar Hussain Bokhari. 2021. "Association of BMI, Diet, Physical Activity, and Oral Hygiene Practices with DMFT Index of Male Dental Students at King Faisal University, Al-Ahsa" Nutrients 13, no. 1: 224. https://doi.org/10.3390/nu13010224
APA StyleJouhar, R., Ahmed, M. A., Khurshid, Z., & Bokhari, S. A. H. (2021). Association of BMI, Diet, Physical Activity, and Oral Hygiene Practices with DMFT Index of Male Dental Students at King Faisal University, Al-Ahsa. Nutrients, 13(1), 224. https://doi.org/10.3390/nu13010224








