Online Behavioral Screener with Tailored Obesity Prevention Messages: Application to a Pediatric Clinical Setting
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedures
2.3. Intervention—Behavioral Screening and Tailored Message Program
2.4. Measures
2.5. Data Analysis
3. Results
3.1. Descriptive Results
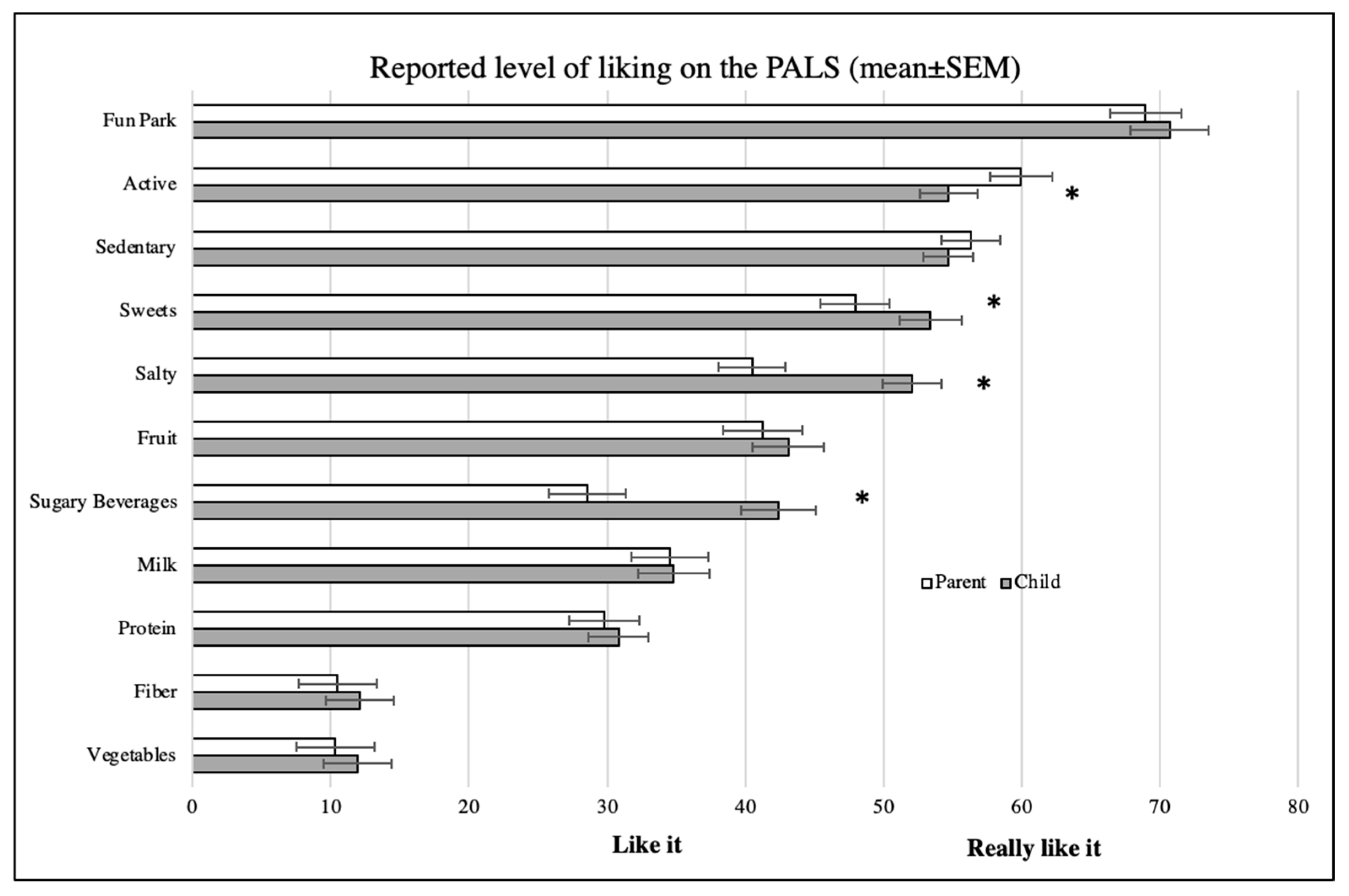
3.2. Description of PALS Responses
3.3. Tailored Health Messages
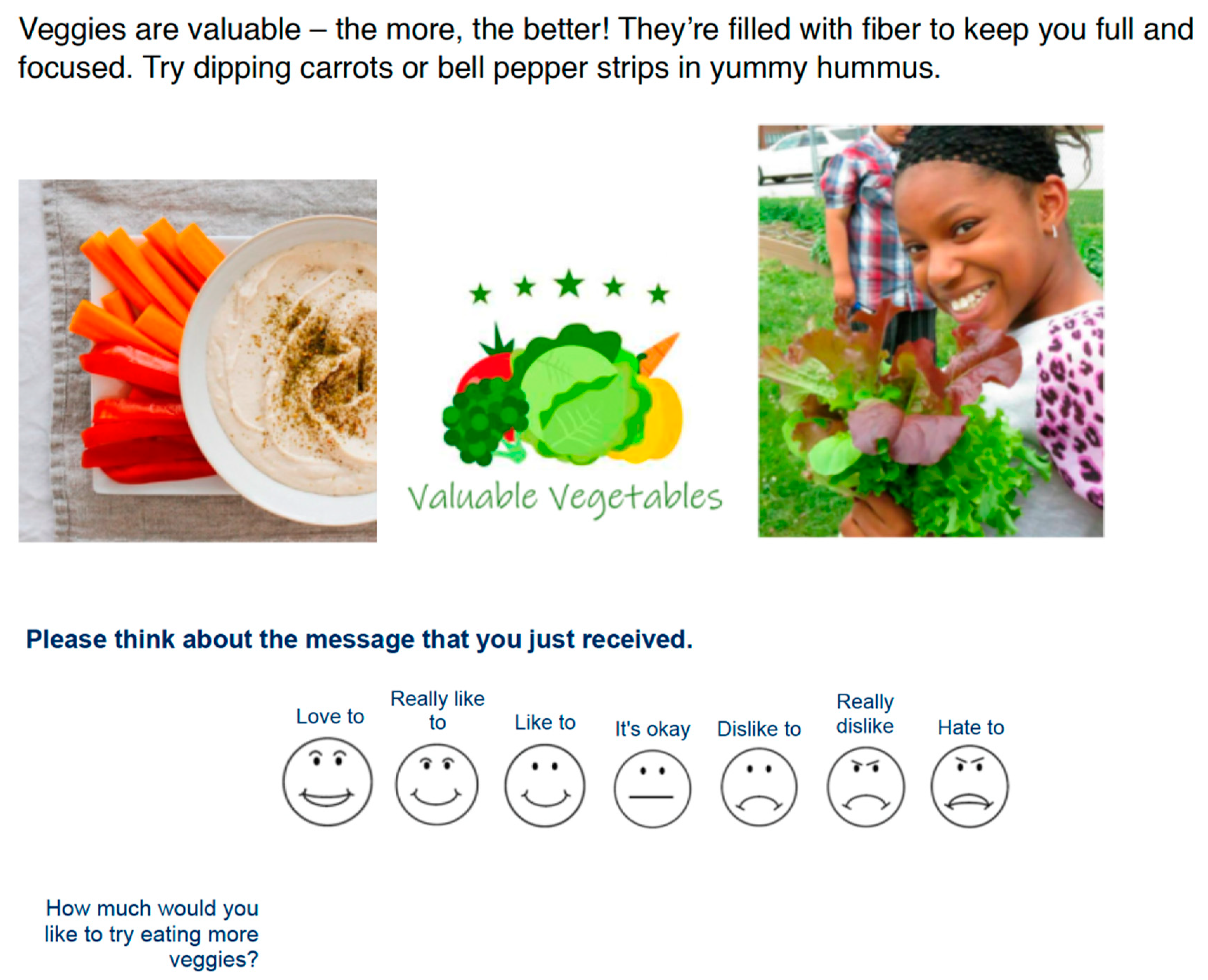
3.4. Relevance and Acceptance of Tailored Messages
3.5. Willingness to Change to or Maintain Healthy Behaviors
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- United Nations Children’s Fund (UNICEF); WHO; International Bank for Reconstruction and Development/The World Bank. Levels and Trends in Child Malnutrition: Key Findings of the 2020 Edition of the Joint Child. Malnutrition Estimates; WHO: Geneva, Switzerland, 2020. [Google Scholar]
- Hales, C.M.; Carroll, M.D.; Fryar, C.D.; Ogden, C.L. Prevalence of Obesity among Adults and Youth: United States, 2015–2016; National Center for Health Statistics: Hyattsville, MD, USA, 2017.
- Skinner, A.C.; Ravanbakht, S.N.; Skelton, J.A.; Perrin, E.M.; Armstrong, S.C. Prevalence of Obesity and Severe Obesity in US Children, 1999–2016. Pediatrics 2018, 141. [Google Scholar] [CrossRef]
- Au, L.E.; Zhu, S.M.; Nhan, L.A.; Plank, K.R.; Frongillo, E.A.; Laraia, B.A.; Gurzo, K.; Ritchie, L.D. Household Food Insecurity is Associated with Higher Adiposity among US Schoolchildren Ages 10–15 Years: The Healthy Communities Study. J. Nutr. 2019, 149, 1642–1650. [Google Scholar] [CrossRef]
- Hoelscher, D.M.; Kirk, S.; Ritchie, L.; Cunningham-Sabo, L.; Academy Positions, C. Position of the Academy of Nutrition and Dietetics: Interventions for the prevention and treatment of pediatric overweight and obesity. J. Acad. Nutr. Diet. 2013, 113, 1375–1394. [Google Scholar] [CrossRef] [PubMed]
- Broekhuizen, K.; Kroeze, W.; van Poppel, M.N.; Oenema, A.; Brug, J. A systematic review of randomized controlled trials on the effectiveness of computer-tailored physical activity and dietary behavior promotion programs: An update. Ann. Behav. Med. 2012, 44, 259–286. [Google Scholar] [CrossRef]
- Petty, R.T.; Cacioppo, J.T. Attitudes and Persuasion: Classic and Contemporary Approaches; Westview Press: Boulder, CO, USA, 1996. [Google Scholar]
- Updegraff, J.A.; Sherman, D.K.; Luyster, F.S.; Mann, T.L. The effects of message quality and congruency on perceptions of tailored health communications. J. Exp. Soc. Psychol. 2007, 43, 249–257. [Google Scholar] [CrossRef]
- Gielen, A.C.; McKenzie, L.B.; McDonald, E.M.; Shields, W.C.; Wang, M.C.; Cheng, Y.J.; Weaver, N.L.; Walker, A.R. Using a computer kiosk to promote child safety: Results of a randomized, controlled trial in an urban pediatric emergency department. Pediatrics 2007, 120, 330–339. [Google Scholar] [CrossRef]
- Wright, J.A.; Whiteley, J.A.; Watson, B.L.; Sheinfeld Gorin, S.N.; Hayman, L.L. Tailored communications for obesity prevention in pediatric primary care: A feasibility study. Health Educ. Res. 2017. [Google Scholar] [CrossRef]
- Hawkins, R.P.; Kreuter, M.; Resnicow, K.; Fishbein, M.; Dijkstra, A. Understanding tailoring in communicating about health. Health Educ. Res. 2008, 23, 454–466. [Google Scholar] [CrossRef]
- Prochaska, J.O.; Velicer, W.F. The transtheoretical model of health behavior change. Am. J. Health Promot. 1997, 12, 38–48. [Google Scholar] [CrossRef]
- Lee, J.E.; Lee, D.E.; Kim, K.; Shim, J.E.; Sung, E.; Kang, J.H.; Hwang, J.Y. Development of tailored nutrition information messages based on the transtheoretical model for smartphone application of an obesity prevention and management program for elementary-school students. Nutr. Res. Pract. 2017, 11, 247–256. [Google Scholar] [CrossRef]
- Brown, C.L.; Perrin, E.M. Obesity Prevention and Treatment in Primary Care. Acad. Pediatr. 2018, 18, 736–745. [Google Scholar] [CrossRef] [PubMed]
- Haber, J.J.; Atti, S.; Gerber, L.M.; Waseem, M. Promoting an obesity education program among minority patients in a single urban pediatric Emergency Department (ED). Int. J. Emerg. Med. 2015, 8, 38. [Google Scholar] [CrossRef] [PubMed]
- Kovalerchik, O.; Powers, E.; Holland, M.L.; Sharifi, M.; Langhan, M.L. Differences in Frequency of Visits to Pediatric Primary Care Practices and Emergency Departments by Body Mass Index. Acad. Pediatr. 2020, 20, 532–539. [Google Scholar] [CrossRef]
- Chandler, I.; Rosenthal, L.; Carroll-Scott, A.; Peters, S.M.; McCaslin, C.; Ickovics, J.R. Adolescents Who Visit the Emergency Department Are More Likely to Make Unhealthy Dietary Choices: An Opportunity for Behavioral Intervention. J. Health Care Poor Underserved 2015, 26, 701–711. [Google Scholar] [CrossRef]
- Thundiyil, J.G.; Christiano-Smith, D.; Greenberger, S.; Cramm, K.; Latimer-Pierson, J.; Modica, R.F. Trimming the fat: Identification of risk factors associated with obesity in a pediatric emergency department. Pediatr. Emerg. Care 2010, 26, 709–715. [Google Scholar] [CrossRef]
- Vaughn, L.M.; Nabors, L.; Pelley, T.J.; Hampton, R.R.; Jacquez, F.; Mahabee-Gittens, E.M. Obesity screening in the pediatric emergency department. Pediatr. Emerg. Care 2012, 28, 548–552. [Google Scholar] [CrossRef]
- Lee, M., Jr.; Monuteaux, M.C. Trends in Pediatric Emergency Department Use after the Affordable Care Act. Pediatrics 2019, 143. [Google Scholar] [CrossRef]
- Baumer-Mouradian, S.H.; Kleinschmidt, A.; Servi, A.; Jaworski, B.; Lazarevic, K.; Kopetsky, M.; Nimmer, M.; Hanson, T.; Gray, M.P.; Drendel, A.L. Vaccinating in the Emergency Department, a Novel Approach to Improve Influenza Vaccination Rates via a Quality Improvement Initiative. Pediatr. Qual. Saf. 2020, 5, e322. [Google Scholar] [CrossRef]
- Kumanyika, S.K. A Framework for Increasing Equity Impact in Obesity Prevention. Am. J. Public Health 2019, 109, 1350–1357. [Google Scholar] [CrossRef]
- Woo Baidal, J.A.; Chang, J.; Hulse, E.; Turetsky, R.; Parkinson, K.; Rausch, J.C. Zooming Toward a Telehealth Solution for Vulnerable Children with Obesity During Coronavirus Disease 2019. Obesity (Silver Spring) 2020, 28, 1184–1186. [Google Scholar] [CrossRef]
- Pasquale, E.; Neshteruk, C.D.; Howard, J.; Skinner, A.C.; Story, M.; Frerichs, L.M.; Armstrong, S.C. An Integrated Clinic-Community Model to Treat Childhood Obesity: Revisiting 2 Years Later. Clin. Pediatr. (Phila.) 2020, 9922820930368. [Google Scholar] [CrossRef] [PubMed]
- Barnidge, E.; Krupsky, K.; LaBarge, G.; Arthur, J. Food Insecurity Screening in Pediatric Clinical Settings: A Caregivers’ Perspective. Matern. Child Health J. 2020, 24, 101–109. [Google Scholar] [CrossRef] [PubMed]
- Camp, N.L.; Robert, R.C.; Kelly, K.P. Healthy Habits Questionnaire Feasibility and Utility for High-Risk Children. Clin. Pediatr. (Phila.) 2020, 9922820927030. [Google Scholar] [CrossRef]
- Arheiam, A.; Albadri, S.; Laverty, L.; Harris, R. Reasons for low adherence to diet-diaries issued to pediatric dental patients: A collective case study. Patient Prefer. Adherence 2018, 12, 1401–1411. [Google Scholar] [CrossRef]
- Sharafi, M.; Perrachio, H.; Scarmo, S.; Huedo-Medina, T.B.; Mayne, S.T.; Cartmel, B.; Duffy, V.B. Preschool-Adapted Liking Survey (PALS): A brief and valid method to assess dietary quality of preschoolers. Child. Obes. 2015, 11, 530–540. [Google Scholar] [CrossRef] [PubMed]
- Vosburgh, K.; Smith, S.R.; Oldman, S.; Huedo-Medina, T.; Duffy, V.B. Pediatric-Adapted Liking Survey (PALS): A Diet and Activity Screener in Pediatric Care. Nutrients 2019, 11, 1641. [Google Scholar] [CrossRef]
- Smith, S.; Johnson, S.; Oldman, S.; Duffy, V. Pediatric-adapted liking survey: Feasible and reliable dietary screening in clinical practice. Caries Res. 2018, 53, 153–159. [Google Scholar] [CrossRef]
- Davies, A.; Randall, D. Perceptions of Children’s Participation in Their Healthcare: A Critical Review. Issues Compr. Pediatr. Nurs. 2015, 38, 202–221. [Google Scholar] [CrossRef] [PubMed]
- Gori, D.; Guaraldi, F.; Cinocca, S.; Moser, G.; Rucci, P.; Fantini, M.P. Effectiveness of educational and lifestyle interventions to prevent paediatric obesity: Systematic review and meta-analyses of randomized and non-randomized controlled trials. Obes. Sci. Pract. 2017, 3, 235–248. [Google Scholar] [CrossRef] [PubMed]
- O’Keefe, L. Identifying Food Insecurity: Two-Question Screening Tool Has 97% Sensitivity. Available online: https://www.aappublications.org/news/2015/10/22/FoodSecurity102315 (accessed on 13 January 2021).
- Centers for Disease Control. BMI Percentile Calculator for Child and Teen. Available online: https://www.cdc.gov/healthyweight/bmi/calculator.html (accessed on 2 January 2021).
- Oldman, S.; Smith, S.R.; Duffy, V.B. Tailored mHealth messages: Application to a Pediatric Emergency Department (PED) to support obesity prevention. Ann. Behav. Med. 2019, 53 (Suppl. 1), 186. [Google Scholar]
- Kids CTteam. International Children’s Advisory Network. Available online: www.icanresearch.com (accessed on 2 January 2021).
- Carfora, V.; Caso, D.; Conner, M. Randomized controlled trial of a messaging intervention to increase fruit and vegetable intake in adolescents: Affective versus instrumental messages. Br. J. Health Psychol. 2016, 21, 937–955. [Google Scholar] [CrossRef] [PubMed]
- Gillison, F.B.; Lorenc, A.B.; Sleddens, E.F.; Williams, S.L.; Atkinson, L. Can it be harmful for parents to talk to their child about their weight? A meta-analysis. Prev. Med. 2016, 93, 135–146. [Google Scholar] [CrossRef] [PubMed]
- Chau, S.; Oldman, S.; Smith, S.R.; Duffy, V.B. Tailored mHealth messages for obesity prevention: Application to a Pediatric Emergency Department (PED). J. Acad. Nutr. Diet. 2019, 119 (Suppl. 1), A75. [Google Scholar] [CrossRef]
- Wright, J.A.; Whiteley, J.A.; Laforge, R.G.; Adams, W.G.; Berry, D.; Friedman, R.H. Validation of 5 stage-of-change measures for parental support of healthy eating and activity. J. Nutr. Educ. Behav. 2015, 47, 134–142.e131. [Google Scholar] [CrossRef] [PubMed]
- Armitage, C.J. Is there utility in the transtheoretical model? Br. J. Health Psychol. 2009, 14, 195–210. [Google Scholar] [CrossRef] [PubMed]
- Di Noia, J.; Mauriello, L.; Byrd-Bredbenner, C.; Thompson, D. Validity and reliability of a dietary stages of change measure among economically disadvantaged African-American adolescents. Am. J. Health Promot. 2012, 26, 381–389. [Google Scholar] [CrossRef]
- Cloutier, M.M.; Lucuara-Revelo, P.; Wakefield, D.B.; Gorin, A.A. My Weight Ruler: A simple and effective tool to enhance parental understanding of child weight status. Prev. Med. 2013, 57, 550–554. [Google Scholar] [CrossRef]
- Lund, A.M. Measuring Usability with the USE Questionnaire. Usability Interface 2001, 8, 3–6. [Google Scholar]
- Costa-Santos, C.; Bernardes, J.; Ayres-de-Campos, D.; Costa, A.; Amorim-Costa, C. The limits of agreement and the intraclass correlation coefficient may be inconsistent in the interpretation of agreement. J. Clin. Epidemiol. 2011, 64, 264–269. [Google Scholar] [CrossRef]
- USDA. Current Population Survey Food Security Supplement. 2018. Available online: https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/key-statistics-graphics.aspx#map (accessed on 2 January 2021).
- Fletcher, S.; Wright, C.; Jones, A.; Parkinson, K.; Adamson, A. Tracking of toddler fruit and vegetable preferences to intake and adiposity later in childhood. Matern. Child. Nutr. 2017, 13. [Google Scholar] [CrossRef]
- Duffy, V.B.; Lanier, S.A.; Hutchins, H.L.; Pescatello, L.S.; Johnson, M.K.; Bartoshuk, L.M. Food preference questionnaire as a screening tool for assessing dietary risk of cardiovascular disease within health risk appraisals. J. Am. Diet. Assoc. 2007, 107, 237–245. [Google Scholar] [CrossRef] [PubMed]
- Tuorila, H.; Huotilainen, A.; Lähteenmäki, L.; Ollila, S.; Tuomi-Nurmi, S.; Urala, N. Comparison of affective rating scales and their relationship to variables reflecting food consumption. Food Qual. Pref. 2008, 19, 51–61. [Google Scholar] [CrossRef]
- Ramsay, S.A.; Rudley, M.; Tonnemaker, L.E.; Price, W.J. A Comparison of College Students’ Reported Fruit and Vegetable Liking and Intake from Childhood to Adulthood. J. Am. Coll. Nutr. 2017, 36, 28–37. [Google Scholar] [CrossRef] [PubMed]
- Sharafi, M.; Rawal, S.; Fernandez, M.L.; Huedo-Medina, T.B.; Duffy, V.B. Taste phenotype associates with cardiovascular disease risk factors via diet quality in multivariate modeling. Physiol. Behav. 2018, 194, 103–112. [Google Scholar] [CrossRef]
- Park, H.; Shin, Y.; Kwon, O.; Kim, Y. Association of Sensory Liking for Fat with Dietary Intake and Metabolic Syndrome in Korean Adults. Nutrients 2018, 10, 877. [Google Scholar] [CrossRef]
- Charlot, K.; Malgoyre, A.; Bourrilhon, C. Proposition for a shortened version of the Leeds Food Preference Questionnaire (LFPQ). Physiol. Behav. 2019, 199, 244–251. [Google Scholar] [CrossRef]
- Ledikwe, J.H.; Ello-Martin, J.; Pelkman, C.L.; Birch, L.L.; Mannino, M.L.; Rolls, B.J. A reliable, valid questionnaire indicates that preference for dietary fat declines when following a reduced-fat diet. Appetite 2007, 49, 74–83. [Google Scholar] [CrossRef]
- Sharafi, M.; Duffy, V.B.; Miller, R.J.; Winchester, S.B.; Sullivan, M.C. Dietary Behaviors of Adults Born Prematurely May Explain Future Risk for Cardiovascular Disease. Appetite 2016, 99, 157–167. [Google Scholar] [CrossRef]
- Pallister, T.; Sharafi, M.; Lachance, G.; Pirastu, N.; Mohney, R.P.; MacGregor, A.; Feskens, E.J.; Duffy, V.; Spector, T.D.; Menni, C. Food Preference Patterns in a UK Twin Cohort. Twin Res. Hum. Genet. 2015, 18, 793–805. [Google Scholar] [CrossRef]
- Xu, R.; Blanchard, B.E.; McCaffrey, J.M.; Woolley, S.; Corso, L.M.L.; Duffy, V.B. Food Liking-Based Diet Quality Indexes (DQI) Generated by Conceptual and Machine Learning Explained Variability in Cardiometabolic Risk Factors in Young Adults. Nutrients 2020, 12, 882. [Google Scholar] [CrossRef]
- Bartoshuk, L.M.; Duffy, V.B.; Hayes, J.E.; Moskowitz, H.R.; Snyder, D.J. Psychophysics of sweet and fat perception in obesity: Problems, solutions and new perspectives. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2006, 361, 1137–1148. [Google Scholar] [CrossRef] [PubMed]
- van de Gaar, V.M.; Jansen, W.; van der Kleij, M.J.; Raat, H. Do children report differently from their parents and from observed data? Cross-sectional data on fruit, water, sugar-sweetened beverages and break-time foods. BMC Public Health 2016, 16, 341. [Google Scholar] [CrossRef] [PubMed]
- Bornhorst, C.; Huybrechts, I.; Ahrens, W.; Eiben, G.; Michels, N.; Pala, V.; Molnar, D.; Russo, P.; Barba, G.; Bel-Serrat, S.; et al. Prevalence and determinants of misreporting among European children in proxy-reported 24 h dietary recalls. Br. J. Nutr. 2013, 109, 1257–1265. [Google Scholar] [CrossRef]
- Bennett, C.A.; de Silva-Sanigorski, A.M.; Nichols, M.; Bell, A.C.; Swinburn, B.A. Assessing the intake of obesity-related foods and beverages in young children: Comparison of a simple population survey with 24 hr-recall. Int. J. Behav. Nutr. Phys. Act. 2009, 6, 71. [Google Scholar] [CrossRef]
- Martins, C.C.; Oliveira, M.J.; Pordeus, I.A.; Paiva, S.M. Comparison between observed children’s tooth brushing habits and those reported by mothers. BMC Oral Health 2011, 11, 22. [Google Scholar] [CrossRef]
- Borrelli, B.; Tooley, E.M.; Scott-Sheldon, L.A. Motivational Interviewing for Parent-child Health Interventions: A Systematic Review and Meta-Analysis. Pediatr. Dent. 2015, 37, 254–265. [Google Scholar] [PubMed]
- Resnicow, K.; McMaster, F.; Bocian, A.; Harris, D.; Zhou, Y.; Snetselaar, L.; Schwartz, R.; Myers, E.; Gotlieb, J.; Foster, J.; et al. Motivational interviewing and dietary counseling for obesity in primary care: An RCT. Pediatrics 2015, 135, 649–657. [Google Scholar] [CrossRef]
- Carcone, A.I.; Naar-King, S.; Brogan, K.E.; Albrecht, T.; Barton, E.; Foster, T.; Martin, T.; Marshall, S. Provider communication behaviors that predict motivation to change in black adolescents with obesity. J. Dev. Behav. Pediatr. 2013, 34, 599–608. [Google Scholar] [CrossRef]
- Faircloth, R.S.; Brooks, D.I.; Vogt, K.S.; Emerick, J.E. Talking About Childhood Obesity: A Survey of What Parents Want. Acad. Pediatr. 2019, 19, 756–763. [Google Scholar] [CrossRef]
- Deci, E.L.; Eghrari, H.; Patrick, B.C.; Leone, D.R. Facilitating internalization: The self-determination theory perspective. J. Pers. 1994, 62, 119–142. [Google Scholar] [CrossRef]
- Yee, A.Z.; Lwin, M.O.; Ho, S.S. The influence of parental practices on child promotive and preventive food consumption behaviors: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 47. [Google Scholar] [CrossRef] [PubMed]
- Bogart, L.M.; Elliott, M.N.; Ober, A.J.; Klein, D.J.; Hawes-Dawson, J.; Cowgill, B.O.; Uyeda, K.; Schuster, M.A. Home Sweet Home: Parent and Home Environmental Factors in Adolescent Consumption of Sugar-Sweetened Beverages. Acad. Pediatr. 2017, 17, 529–536. [Google Scholar] [CrossRef]
- Karner, H.; Oldman, S.; Lin, C.A.; Harris, J.; Plant, D.; Duffy, V.B. Testing the feasibility of a school-based online survey to assess middle schoolers’ food and activity behaviors and provide tailored health messages. J. Acad. Nutr. Diet. 2019, 119 (Suppl. 1), A77. [Google Scholar] [CrossRef]
- Taveras, E.M.; Marshall, R.; Kleinman, K.P.; Gillman, M.W.; Hacker, K.; Horan, C.M.; Smith, R.L.; Price, S.; Sharifi, M.; Rifas-Shiman, S.L.; et al. Comparative effectiveness of childhood obesity interventions in pediatric primary care: A cluster-randomized clinical trial. JAMA Pediatr. 2015, 169, 535–542. [Google Scholar] [CrossRef] [PubMed]
- Bedell, C.E.; Zelinsky, C.; Puglisi, M.; Fenn, L.M.; Harris, J.; Duffy, V.B. Online Toddler Feeding Survey with Tailored Messages for Parents and to Assist Nutrition Counseling: Pilot Testing in a WIC Waiting Room. J. Acad. Nutr. Diet. 2020, 120, A84. [Google Scholar] [CrossRef]
- Hassink, S.G.; Fairbrother, G. Obesity and Hunger Threaten the Foundations of Child Health. Acad. Pediatr. 2020. [Google Scholar] [CrossRef]
| N = 245 | % | |
|---|---|---|
| Age (Average = 10.2 Years) | ||
| 5 to <9 years | 88 | 36 |
| 9 to <13 years | 85 | 35 |
| 13 to 17 years | 72 | 29 |
| Gender | ||
| Male | 132 | 54 |
| Female | 110 | 45 |
| Other | 3 | 1 |
| Race/Ethnicity | ||
| White | 86 | 35 |
| Black | 47 | 19 |
| Hispanic | 102 | 42 |
| Asian | 8 | 3 |
| Other | 2 | 1 |
| Insurance | ||
| Private | 99 | 40 |
| Public | 146 | 60 |
| Food Security † | ||
| Secure | 184 | 75 |
| Insecure | 61 | 25 |
| BMI percentile †† | ||
| Underweight | 15 | 6 |
| Normal | 148 | 60 |
| Overweight | 33 | 14 |
| Obese | 48 | 20 |
| Motivating Tailored Health Message | Willingness to Change Behavior Question | Child % Reporting “Like”–“Love to” |
|---|---|---|
| Sugary Drinks: Tame your thirst with water—fruit juices and sugary drinks will just make you thirstier! | How much would you like to drink more water? | 86 |
| Sweets: Cookies and candy have extra sugar that your body doesn’t like. Instead, try eating your favorite fruits as a sweet treat! | How much would you like to eat fruit as a snack or for dessert? | 80 |
| Screen time: TV and video games are fun to play, but try to limit them to 2 h a day! Instead, dance with friends, play fetch with your pup, or go to the playground with your parents! Aim to be active for 1 h each day. | How much would you like to be moving and playing for 1 h or more each day? | 80 |
| Dairy: Dairy is delightful! Try choosing yogurt, milk, and cheese. These foods deliver calcium to your body to keep your bones strong and your smile bright. | How much would you like to eat more yogurt, milk and cheese? | 75 |
| Salty Snacks: Slow down with salt! Snacks like chips and French fries are oh-so-salty. Eating them will make you thirsty. Try choosing a smart snack, like celery sticks topped with peanut butter and whole grain cereal! | How much would you like eating healthier snacks? | 74 |
| Fruit: Feast on fruit! They pack vitamins that make your skin glow and hair shine. Try topping your cereal or yogurt with a blend of berries! | How much would you like to try eating fruit at most meals and snacks? | 73 |
| Vegetables: Veggies are valuable—the more, the better! They’re filled with fiber to keep you full and focused. Try dipping carrots or bell pepper strips in yummy hummus. | How much would you like to try eating more veggies? | 56 |
| Fiber: Go with the whole grain! Try munching on whole wheat breads for your lunchtime sandwiches and brown rice when building your dinner plate! | How much would you like to eat more whole grains? | 50 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chau, S.; Oldman, S.; Smith, S.R.; Lin, C.A.; Ali, S.; Duffy, V.B. Online Behavioral Screener with Tailored Obesity Prevention Messages: Application to a Pediatric Clinical Setting. Nutrients 2021, 13, 223. https://doi.org/10.3390/nu13010223
Chau S, Oldman S, Smith SR, Lin CA, Ali S, Duffy VB. Online Behavioral Screener with Tailored Obesity Prevention Messages: Application to a Pediatric Clinical Setting. Nutrients. 2021; 13(1):223. https://doi.org/10.3390/nu13010223
Chicago/Turabian StyleChau, Sarah, Samantha Oldman, Sharon R. Smith, Carolyn A. Lin, Saba Ali, and Valerie B. Duffy. 2021. "Online Behavioral Screener with Tailored Obesity Prevention Messages: Application to a Pediatric Clinical Setting" Nutrients 13, no. 1: 223. https://doi.org/10.3390/nu13010223
APA StyleChau, S., Oldman, S., Smith, S. R., Lin, C. A., Ali, S., & Duffy, V. B. (2021). Online Behavioral Screener with Tailored Obesity Prevention Messages: Application to a Pediatric Clinical Setting. Nutrients, 13(1), 223. https://doi.org/10.3390/nu13010223






