Effect of an Aquatic Balance-Training Program in Patients with Chronic Stroke: A Single-Group Experimental Pilot Study
Abstract
:1. Introduction
2. Materials and Methods
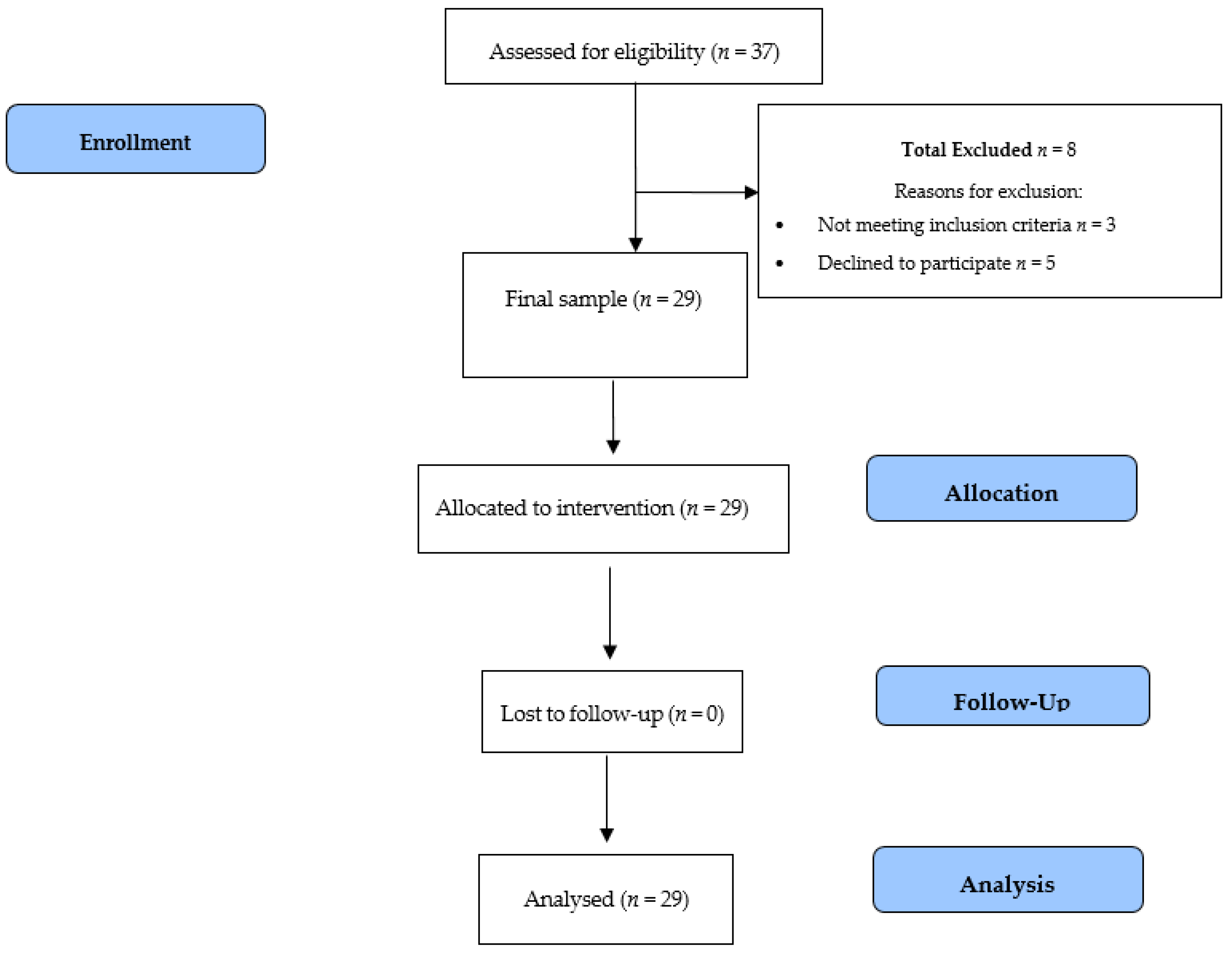
2.1. Study Design and Sample
2.2. Stabilometric Assessment
2.3. Intervention/Aquatic Therapy
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Díez-Tejedor, E. Acuerdo Para el uso del Término ICTUS, Guía Para el Diagnóstco y Tratamiento del Ictus. Guías Oficiales de la Sociedad Española de Neurología; Prous Science: Barcelona, Spain, 2006. [Google Scholar]
- Alvarez Sabín, J.; de Alonso Leciñana, M.; Gallego, J.; Gil-Peralta, A.; Casado, I.; Castillo, J.; Rubio, F. Plan de atención sanitaria al ictus. Neurología 2006, 21, 717–726. [Google Scholar]
- DíazGuzmán, J.; Egido, J.A.; GabrielSánchez, R.; BarberáComes, G.; FuentesGimeno, B.; FernándezPérez, C. IBERICTUS Study Investigators of the Stroke Project of the Spanish Cerebrovascular Diseases Study Group. Stroke and transient ischemic attack incidence rate in Spain: The IBERICTUS study. Cereb. Dis. 2012, 34, 272–281. [Google Scholar]
- Duarte, E.; Alonso, B.; Fernández, M.J.; Fernández, J.M.; Flores, M.; GarcíaMontes, I.; Gentil, J.; Hernández, L.; Juan, F.J.; Palomino, B.; et al. Rehabilitación del ictus: Modelo asistencial. Recomendaciones de la sociedad española de rehabilitación y medicina física. Rehabilitación 2010, 44, 60–68. [Google Scholar] [CrossRef]
- Alonso, M. Principios básicos y fundamentos de la terapia acuática. In Terapia Acuática. Abordajes Desde la Fisioterapia y la Terapia Ocupacional; Gueita, J., Alonso, M., Fernández, C., Eds.; Elsevier: Barcelona, Spain, 2015; pp. 3–15. [Google Scholar]
- Becker, B.E. Aquatic therapy: Scientific foundations and clinical rehabilitation applications. Am. J. Phys. Med. Rehabil. 2009, 1, 859–872. [Google Scholar] [CrossRef]
- Marinho-Buzelli, A.R.; Bonnyman, A.M.; Verrier, M.C. The effects of aquatic therapy on mobility of individuals with neurological diseases: A systematic review. Clin. Rehabil. 2015, 29, 741–751. [Google Scholar] [CrossRef]
- Weber-Nowakowska, K.; Zyzniewska-Banaszk, E.; Gebska, M. New methods in physiotherapy. The Halliwick concept as a form of rehabilitation in water. Ann. Acad. Med. Stetin. 2011, 57, 43–45. [Google Scholar]
- Severin, A.C.; Burkett, B.J.; McKean, M.R.; Wiegand, A.N.; Sayers, M.G. Effects of water immersion on squat and split-squat kinematics in older aged adults. J. Aging Phys. Act. 2018, 9, 1–22. [Google Scholar]
- Pérez-de la Cruz, S. Mental health in Parkinson’s disease after receiving aquatic therapy: A clinical trial. Acta Neurol. Belg. 2018, 119, 193–200. [Google Scholar] [CrossRef]
- Ellapen, T.J.; Hammill, H.V.; Swanepoel, M.; Strydom, G.L. The benefits of hydrotherapy to patients with spinal cord injuries. Afr. J. Disabil. 2018, 7, 450. [Google Scholar] [CrossRef] [Green Version]
- Arzzola, M.C.D.P. Oensino do Método Halliwick e Cursos Lato Sensu e Interfaces com a Educação Especial. Ph.D. Thesis, Universidade Federal de São Carlos, São Carlos, SP, USA, 2007. [Google Scholar]
- Douris, P.; Southard, V.; Varga, C.; Schauss, W.; Gennaro, C. The effect of land and aquatic exercise on balance scores in older adults. J. Geriatr. Phys. Ther. 2003, 26, 3–6. [Google Scholar] [CrossRef] [Green Version]
- Zotz, T.G.G.; Souza, E.A.; Israel, V.L.; Loureiro, A.P.C. Aquatic physycal therapy for parkinson’s desease. Adv. Parkinson’s Dis. 2013, 2, 102–107. [Google Scholar] [CrossRef] [Green Version]
- Iliescu, A.M.; McIntyre, A.; Wiener, J.; Iruthayarajah, J.; Lee, A.; Caughlin, S.; Teasell, R. Evaluating the effectiveness of aquatic therapy on mobility, balance, and level of functional independence in stroke rehabilitation: A systematic review and meta-analysis. Clin. Rehabil. 2020, 34, 56–68. [Google Scholar] [CrossRef]
- Giuriati, S.; Servadio, A.; Temperoni, G.; Curcio, A.; Valente, D.; Galeoto, G. The effect of aquatic physical therapy in patients with stroke: A systematic review and meta-analysis. Top. Stroke Rehabil. 2020, 27, 1–14. [Google Scholar] [CrossRef]
- Tripp, F.; Krakow, K. Effects of an aquatic therapy approach (Halliwick-Therapy) on functional mobility in subacute stroke patients: A randomized controlled trial. Clin. Rehabil. 2014, 28, 432–439. [Google Scholar] [CrossRef]
- Chen, H.; Liu, Y.; Huang, G.; Zhu, J.; Feng, W.; He, J. Association between vitamin D status and cognitive impairment in acute ischemic stroke patients: A prospective cohort study. Clin. Interv. Aging 2018, 13, 2503–2509. [Google Scholar] [CrossRef] [Green Version]
- Quinn, T.J.; Dawson, J.; Walters, M.R.; Lees, K.R. Reliability of the modified Rankin Scale: A systematic review. Stroke 2009, 40, 3393–3395. [Google Scholar] [CrossRef] [Green Version]
- Aydog, E. Evaluation of dynamic postural balance using the Biodex Stability system in rheumatoid arthritis patients. Clin. Rheumatol. 2005, 25, 1–6. [Google Scholar]
- Clark, S. Generalizability of the limits of stability test in the evaluation of Dynamic balance among older adults. Arch. Phys. Med. Rehabil. 1997, 78, 1078–1084. [Google Scholar] [CrossRef]
- Wallmann, H.W.; Player, K.R.; Bugnet, M. Acute effects of static stretching on balance in young versus elderly adults. Phys. Occup. Ther. Geriatr. 2012, 30, 301–315. [Google Scholar] [CrossRef]
- Lambeck, J.F.; Gamper, U.N. The Halliwick Concept. In Comprehensive Aquatic Therapy, 3rd ed.; Becker, B.E., Cole, A.J., Eds.; Washington State University Publishing: Pullman, France, 2010; pp. 77–107. [Google Scholar]
- Park, B.S.; Noh, J.W.; Kim, M.Y.; Lee, L.K.; Yang, S.M.; Lee, W.D.; Shin, Y.S.; Kim, J.H.; Lee, J.U.; Kwak, T.Y.; et al. The effects of aquatic trunk exercise on gait and muscle activity in stroke patients: A randomized controlled pilot study. J. Phys. Ther. Sci. 2015, 27, 3549–3553. [Google Scholar] [CrossRef] [Green Version]
- Chan, K.; Phadke, C.P.; Stremler, D.; Suter, L.; Pauley, T.; Ismail, F.; Boulias, C. The effect of wáter based exercises on balance in persons post-stroke: A randomized controlled trial. Top. Stroke Rehabil. 2017, 24, 228–235. [Google Scholar] [CrossRef] [PubMed]
- Santos, S.M.; da Silva, R.A.; Terra, M.B.; Almeida, I.A.; De Melo, L.B.; Ferraz, H.B. Balance versus resistance training on postural control in patients with Parkinson’s disease: A randomized controlled trial. Eur. J. Phys. Rehabil. Med. 2017, 53, 173–183. [Google Scholar] [PubMed]
- Marinho-Buzelli, A.R.; Rouhani, H.; Masani, K.; Verrier, M.C.; Popovic, M.R. The influence of the aquatic environment on the control of postural sway. Gait. Posture 2017, 51, 70–76. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Noh, D.K.; Lim, J.Y.; Shin, H.I.; Paik, N.J. The effect of aquatic therapy on postural balance and muscle strength in stroke survivors: A randomized controlled pilot trial. Clin. Rehabil. 2008, 22, 9669–9676. [Google Scholar]
- Eyvaz, N.; Dundar, U.; Yesil, H. Effects of water-based and land-based exercises on walking and balance functions of patients with hemiplegia. NeuroRehabilitation 2018, 43, 237–246. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.; Lee, D.K.; Kim, E.K. Effect of aquatic dual-task training on balance and gait in stroke patients. J. Phys. Sci. 2016, 28, 2044–2047. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morer, C.; Boestad, C.; Zuluaga, P.; Alvarez-Badillo, A.; Maraver, F. Effects of an intensive thalassotherapy and aquatic therapy program in stroke patients. A pilot study. Rev. Neurol. 2017, 65, 249–256. [Google Scholar] [PubMed]
- Aidar, F.J.; de Jacó Oliveira, R.; Gama de Matos, D.; Chilibeck, P.D.; de Souza, R.F.; Carneiro, A.L.; Machado Reis, V. A randomized trial of the effects of an aquatic exercise program on depression, anxiety levels, and functional capacity of people who suffered an ischemic stroke. J. Sports Med. Phys. Fit. 2018, 58, 117–177. [Google Scholar]
- Zhang, Y.; Wang, Y.Z.; Huang, L.P.; Bai, B.; Zhou, S.; Yin, M.M.; Zhao, H.; Zhou, X.N.; Wang, H.T. Aquatic Therapy Improves Outcomes for Subacute Stroke Patients by Enhancing Muscular Strength of Paretic Lower Limbs Without Increasing Spasticity: A Randomized Controlled Trial. Am. J. Phys. Med. Rehabil. 2016, 95, 840–849. [Google Scholar] [CrossRef]
- Lee, S.Y.; Im, S.H.; Kim, B.R.; Han, E.Y. The Effects of a Motorized Aquatic Treadmill Exercise Program on Muscle Strength, Cardiorespiratory Fitness, and Clinical Function in Subacute Stroke Patients: A Randomized Controlled Pilot Trial. Am. J. Phys. Med. Rehabil. 2018, 97, 533–540. [Google Scholar] [CrossRef]
- Cronin, N.J.; Valtonen, A.M.; Waller, B.; Pöyhönen, T.; Avela, J. Effects of short term water immersion on peripheral reflex excitability in hemiplegic and healthy individuals: A preliminary study. J. Musculoskelet Neuronal. Interact. 2016, 16, 58–62. [Google Scholar] [PubMed]
- Zhu, Z.; Cui, L.; Yin, M.; Yu, Y.; Zhou, X.; Wang, H.; Yan, H. Hydrotherapy vs. conventional land-based exercise for improving walking and balance after stroke: A randomized controlled trial. Clin. Rehabil. 2016, 30, 587–593. [Google Scholar] [CrossRef] [PubMed]
| Session Parts | Progression | Duration |
|---|---|---|
| Warm-Up |
| 10 min |
| Halliwick Therapy |
| 25 min |
| Cool-Down |
| 10 min |
| Total duration of the session | 45 min |
| Participants | IQ 95% | |||
|---|---|---|---|---|
| Male (n = 20) | Female (n = 9) | Total (n = 29) | ||
| Age (years) | 48.1 (2.86) | 45.8 (2.65) | 47.2 (7.07) | (42–55) |
| Weight | 73.63 (9.02) | 68.04 (6.89) | 71.9 (14.55) | (59.44–82.76) |
| Height (cm) | 177 (0.22) | 172.71 (0.08) | 176.01 (8.12) | (166–188) |
| BMI | 23.69 (2.38) | 21.54 (2.88) | 22.71 (3.14) | (19.25–27.39) |
| Mean time since diagnosis (years) | 4.20 (2.50) | 5.56 (3.01) | 4.93 (3.68) | (3.22–7.98) |
| Measurement, Mean (SD) | ANOVA MR | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | 1 Month | F (2.22) | p-Value | eta2 | ||||
| Overall Stability Index | 1.10 (0.70) | a | 0.68 (0.29) | b | 0.59 (0.28) | b | 8.951 | 0.001 | 0.449 |
| Anterior/Posterior Instability Index | 0.88 (0.41) | a | 0.52 (0.22) | b | 0.43 (0.11) | b | 12.269 | <0.001 | 0.527 |
| Medial/Lateral Index | 0.65 (0.42) | a | 0.38 (0.18) | b | 0.41 (0.28) | b | 9.599 | 0.001 | 0.466 |
| Measurement, Mean (SD) | ANOVA MR | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | 1 Month | F (2.22) | p-Value | eta2 | ||||
| Time to complete trial (sec) | 79.75 (20.48) | a | 54.25 (16.77) | b | 512.5 (12.19) | b | 24.457 | <0.001 | 0.69 |
| Overall (mm) | 23.50 (14.79) | a | 33.67 (14.90) | b | 29.50 (12.18) | a | 6.731 | 0.005 | 0.38 |
| Forward (mm) | 23.33 (18.57) | 27.08 (16.88) | 24.58 (13.94) | 0.399 | 0.676 | 0.035 | |||
| Backward (mm) | 32.42 (10.60) | 33.83 (15.46) | 31.33 (15.41) | 0.449 | 0.644 | 0.039 | |||
| Right (mm) | 35.08 (19.60) | a | 51.00 (22.55) | b | 45.08 (20.42) | c | 6.196 | 0.007 | 0.36 |
| Left (mm) | 35.75 (20.99) | a | 48.17 (18.59) | b | 41.58 (14.16) | b | 3.464 | 0.049 | 0.239 |
| Forward right (mm) | 33.17 (19.04) | 40.25 (13.03) | 40.00 (13.42) | 1.675 | 0.21 | 0.132 | |||
| Forward left (mm) | 28.83 (16.53) | a | 35.25 (13.87) | b | 34.75 (14.98) | b | 3.56 | 0.046 | 0.229 |
| Backward right (mm) | 28.25 (12.67) | a | 36.25 (16.89) | b | 33.33 (12.94) | b | 6.171 | 0.007 | 0.359 |
| Backward left (mm) | 34.08 (11.33) | a | 44.58 (19.27) | b | 38.75 (14.50) | b | 3.703 | 0.041 | 0.252 |
| Measurement, Mean (SD) | ANOVA MR | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | 1 Month | F (2.22) | p-Value | eta2 | ||||
| Overall Stability Index | 1.65 (0.51) | a | 1.17 (0.60) | ab | 1.04 (0.47) | b | 5.491 | 0.012 | 0.333 |
| Anterior Position Index | 1.15 (0.33) | 0.98 (0.45) | 0.98 (0.48) | 0.614 | 0.55 | 0.053 | |||
| Medial Lateral Index | 1.08 (0.28) | a | 0.71 (0.41) | b | 0.86 (0.41) | b | 3.471 | 0.049 | 0.238 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pérez-de la Cruz, S. Effect of an Aquatic Balance-Training Program in Patients with Chronic Stroke: A Single-Group Experimental Pilot Study. Medicina 2020, 56, 656. https://doi.org/10.3390/medicina56120656
Pérez-de la Cruz S. Effect of an Aquatic Balance-Training Program in Patients with Chronic Stroke: A Single-Group Experimental Pilot Study. Medicina. 2020; 56(12):656. https://doi.org/10.3390/medicina56120656
Chicago/Turabian StylePérez-de la Cruz, Sagrario. 2020. "Effect of an Aquatic Balance-Training Program in Patients with Chronic Stroke: A Single-Group Experimental Pilot Study" Medicina 56, no. 12: 656. https://doi.org/10.3390/medicina56120656
APA StylePérez-de la Cruz, S. (2020). Effect of an Aquatic Balance-Training Program in Patients with Chronic Stroke: A Single-Group Experimental Pilot Study. Medicina, 56(12), 656. https://doi.org/10.3390/medicina56120656





