Cooking Frequency and Perception of Diet among US Adults Are Associated with US Healthy and Healthy Mediterranean-Style Dietary Related Classes: A Latent Class Profile Analysis
Abstract
:1. Introduction
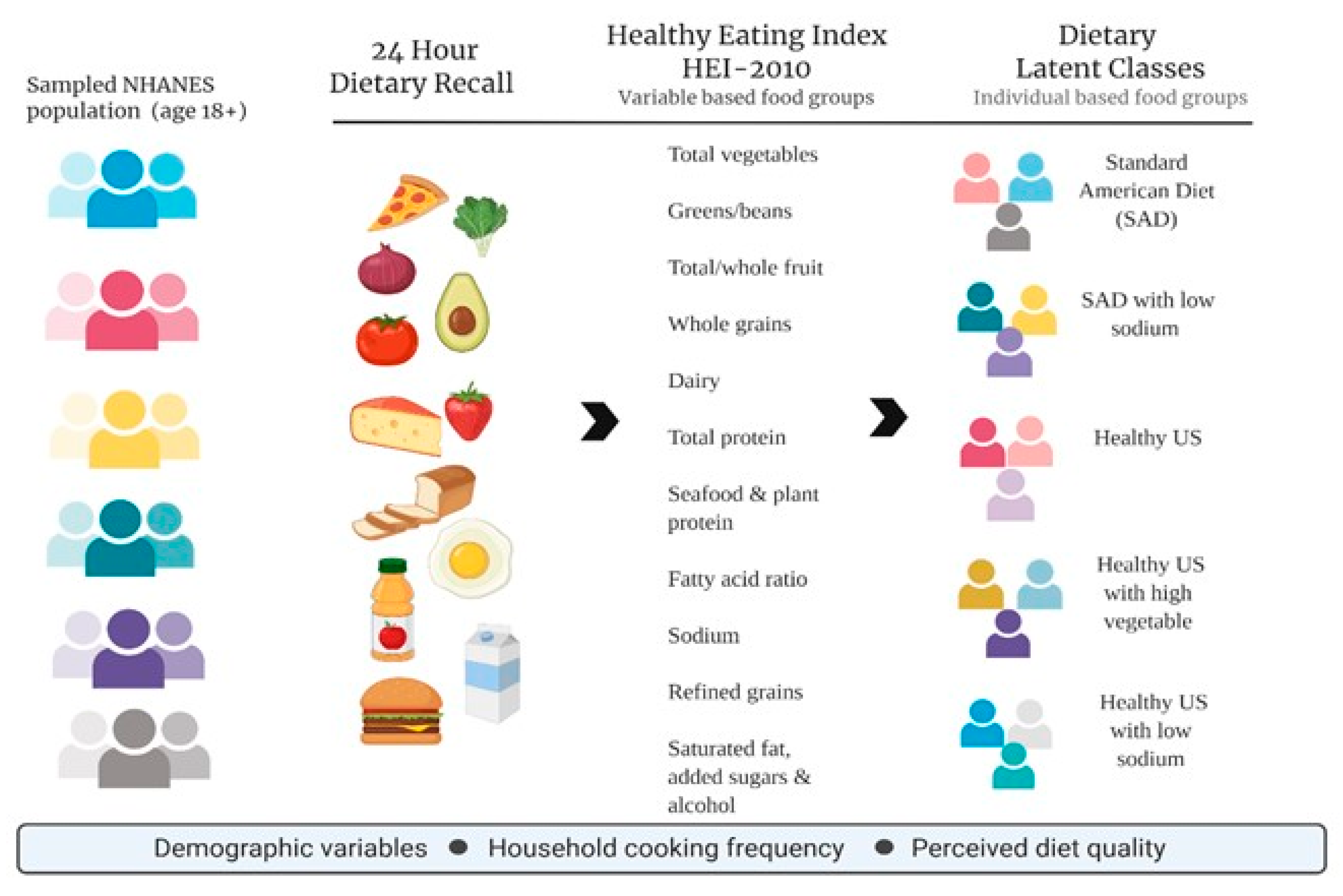
2. Materials and Methods
2.1. Data and Sample
2.2. Measures
2.3. Statistical Analysis
3. Results
3.1. Demographic and Socioeconomic Characteristics and Dietary Habits of Study Population
3.2. Identification, Labeling and Description of Dietary Classes
3.3. Sociodemographic and Meal Preparation Habits Variables and Daily HEI Dietary Classes
3.4. Sociodemographic and Meal Preparation Habits Variables and Dinner HEI Dietary Classes
4. Discussion
4.1. Cooking Frequency and Dietary Classes
4.2. Perceived Diet Quality and Dietary Patterns
4.3. Socioeconomic and Demographic Variables and Dietary Patterns
4.4. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Kant, A.K. Dietary patterns and health outcomes. J. Am. Diet. Assoc. 2004, 104, 615–635. [Google Scholar] [CrossRef] [PubMed]
- Jacques, P.F.; Tucker, K.L. Are dietary patterns useful for understanding the role of diet in chronic disease? Am. J. Clin. Nutr. 2001, 73, 1–2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hu, F.B. Dietary pattern analysis: A new direction in nutritional epidemiology. Curr. Opin. Lipidol. 2002, 13, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, D.R.; Steffen, L.M. Nutrients, foods, and dietary patterns as exposures in research: A framework for food synergy. Am. J. Clin. Nutr. 2003, 78, 508S–513S. [Google Scholar] [CrossRef] [PubMed]
- Liese, A.D.; Krebs-Smith, S.M.; Subar, A.F.; George, S.M.; Harmon, B.E.; Neuhouser, M.L.; Boushey, C.J.; Schap, T.E.; Reedy, J. The Dietary Patterns Methods Project: Synthesis of findings across cohorts and relevance to dietary guidance. J. Nutr. 2015, 145, 393–402. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krebs-Smith, S.M.; Pannucci, T.E.; Subar, A.F.; Kirkpatrick, S.I.; Lerman, J.L.; Tooze, J.A.; Wilson, M.M.; Reedy, J. Update of the Healthy Eating Index: HEI-2015. J. Acad. Nutr. Diet. 2018, 118, 1591–1602. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dubowitz, T.; Zenk, S.N.; Ghosh-Dastidar, B.; Cohen, D.A.; Beckman, R.; Hunter, G.; Steiner, E.D.; Collins, R.L. Healthy food access for urban food desert residents: Examination of the food environment, food purchasing practices, diet and BMI. Public Health Nutr. 2015, 18, 2220–2230. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Raffensperger, S.; Kuczmarski, M.F.; Zonderman, A.B. The effect of race and predictors of socioeconomic status on diet quality in the Healthy Aging in Neighborhoods of Diversity across the Life Span (HANDLS) study sample. J. Natl. Med. Assoc. 2010, 102, 923–930. [Google Scholar] [CrossRef]
- Mata, J.; Frank, R.; Hertwig, R. Higher body mass index, less exercise, but healthier eating in married adults: Nine representative surveys across Europe. Soc. Sci. Med. 2015, 138, 119–127. [Google Scholar] [CrossRef] [Green Version]
- Yannakoulia, M.; Panagiotakos, D.; Pitsavos, C.; Skoumas, Y.; Stafanadis, C. Eating patterns may mediate the association between marital status, body mass index, and blood cholesterol levels in apparently healthy men and women from the ATTICA study. Soc. Sci. Med. 2008, 66, 2230–2239. [Google Scholar] [CrossRef]
- Powell-Wiley, T.M.; E Miller, P.; Agyemang, P.; Agurs-Collins, T.; Reedy, J. Perceived and objective diet quality in US adults: A cross-sectional analysis of the National Health and Nutrition Examination Survey (NHANES). Public Health Nutr. 2014, 17, 2641–2649. [Google Scholar] [CrossRef] [PubMed]
- Falk, P. The Consuming Body; Sage: London, UK, 1994. [Google Scholar]
- Mills, S.; White, M.; Brown, H.; Wrieden, W.; Kwasnicka, D.; Halligan, J.; Robalino, S.; Adams, J. Health and social determinants and outcomes of home cooking: A systematic review of observational studies. Appetite 2017, 111, 116–134. [Google Scholar] [CrossRef] [PubMed]
- Farmer, N.; Wallen, G.R.; Yang, L.; Middleton, K.R.; Kazmi, N.; Powell-Wiley, T.M. Household Cooking Frequency of Dinner Among Non-Hispanic Black Adults is Associated with Income and Employment, Perceived Diet Quality and Varied Objective Diet Quality, HEI (Healthy Eating Index): NHANES Analysis 2007–2010. Nutrients 2019, 11, 2057. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wolfson, J.; Leung, C.; Richardson, C. More frequent cooking at home is associated with higher Healthy Eating Index-2015 score. Public Health Nutr. 2020, 23, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Mills, S.; Brown, H.; Wrieden, W.; White, M.; Adams, J. Frequency of eating home cooked meals and potential benefits for diet and health: Cross-sectional analysis of a population based cohort study. Intl. J. Behav. Nutr. Phys. Act. 2017, 14, 1–11. [Google Scholar] [CrossRef]
- Uzhova, I.; Woolhead, C.; Timon, C.M.; O’Sullivan, A.; Brennan, L.; Peñalvo, J.L.; Gibney, E.R. Generic Meal Patterns Identified by Latent Class Analysis: Insights from NANS (National Adult Nutrition Survey). Nutrients 2018, 10, 310. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fabiani, R. A western dietary pattern increases prostate cancer risk: A systematic review and meta-analysis. Nutrients 2016, 8, 626. [Google Scholar] [CrossRef]
- Fung, T.T.; Rimm, E.B.; Spiegelman, D.; Rifai, N.; Tofler, G.H.; Willett, W.C.; Hu, F.B. Association between dietary patterns and plasma biomarkers of obesity and cardiovascular disease risk. Am. J. Clin. Nutr. 2001, 73, 61–67. [Google Scholar] [CrossRef]
- van Dam, R.M.; Rimm, M.B.; Willett, S.C.; Stampfer, M.J.; Hu, M.B. Dietary patterns and risk for type 2 diabetes mellitus in U.S. men. Ann. Intern. Med. 2002, 136, 201–209. [Google Scholar] [CrossRef] [Green Version]
- Bergman, L.R.; Magnusson, D. A person-oriented approach in research on developmental psychopathology. Dev. Psychopathol. 1997, 9, 291–319. [Google Scholar] [CrossRef]
- Mullie, P.; Clarys, P.; Hulens, M.; Vansant, G. Dietary patterns and socioeconomic position. Eur. J. Clin. Nutr. 2010, 64, 231–238. [Google Scholar] [CrossRef] [PubMed]
- Muthen, B.; Muthen, L.K. Integrating Person-Centered and Variable-Centered Analyses: Growth Mixture Modeling With Latent Trajectory Classes. Alcohol. Clin. Exp. Res. 2000, 24. [Google Scholar] [CrossRef]
- Magidson, J.; Vermunt, J.K. Latent class models for clustering: A comparison with K-means. Can. J. Mark. Res. 2002, 20, 37–44. [Google Scholar]
- Sotres-Alvarez, D.; Herring, A.H.; Siega-Riz, A.M. Latent Class Analysis is useful to classify pregnant women into dietary patterns. J. Nutr. 2010, 40, 2253–2259. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Padmadas, S.S.; Dias, J.G.; Willekens, F.J. Disentangling women’s responses on complex dietary intake patterns from an Indian cross-sectional survey: A latent class analysis. Public Health Nutr. 2006, 9, 204–211. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johnson, C.L.; Dohrmann, S.M.; Burt, V.L.; Mohadjer, L.K. National Health and Nutrition Examination Survey: Sample Design, 2011–2014; Vital and health statistics. Series 2; Data evaluation and methods research; U.S. Department of Health & Human Services: Washington, DC, USA, 2014; pp. 1–33.
- Guenther, P.M.; Casavale, K.O.; Reedy, J.; Kirkpatrick, S.I.; Hiza, H.A.; Kuczynski, K.J.; Kahle, L.L.; Krebs-Smith, S.M. Update of the Healthy Eating Index: HEI-2010. J. Acad. Nutr. Diet. 2013, 113, 569–580. [Google Scholar] [CrossRef] [Green Version]
- Guenther, P.M.; Kirkpatrick, S.I.; Reedy, J.; Krebs-Smith, S.M.; Buckman, D.W.; Dodd, K.W.; Casavale, K.O.; Carroll, R.J. The Health Eating Index-2010 is a valid and reliable measure of diet quality according to the 2010 Dietary Guidelines for Americans. J. Nutr. 2014, 144, 399–407. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ahluwalia, N.; Dwyer, J.; Terry, A.; Moshfegh, A.; Johnson, C. Update on NHANES Dietary Data: Focus on Collection, Release, Analytical Considerations, and Uses to Inform Public Policy. Adv. Nutr. 2016, 7, 121–134. [Google Scholar] [CrossRef] [Green Version]
- Wolfson, J.; Bleich, S.N. Is cooking at home associated with better diet quality or weight-loss intention? Public Health Nutr. 2015, 18, 1397–1406. [Google Scholar] [CrossRef] [Green Version]
- Chung, H.; Lanza, S.T.; Loken, E. Latent transition analysis: Inference and estimation. Stat. Med. 2008, 27, 1834–1854. [Google Scholar] [CrossRef] [Green Version]
- Vermunt, J.K.; Magidson, J. Latent class cluster analysis. In Applied Latent Class Analysis; Hagenaars, J.A., McCutcheon, A.L., Eds.; Cambridge University Press: Cambridge, UK, 2002; pp. 89–106. [Google Scholar]
- Vermunt, J.K.; Magidson, J. Latent class analysis with sampling weights: A maximum-likelihood approach. Sociol. Methods Res. 2007, 36, 87–111. [Google Scholar] [CrossRef]
- Muthén, B.; Shedden, K. Finite mixture modeling with mixture outcomes using the EM algorithm. Biometrics 1999, 55, 463–469. [Google Scholar] [CrossRef] [PubMed]
- Akaike, H. A new look at the statistical model identification. IEEE Trans. Autom. Control 1974, 19, 716–723. [Google Scholar] [CrossRef]
- Schwartz, G. Estimating the Dimension of a Model. Ann. Stat. 1978, 6, 461–464. [Google Scholar] [CrossRef]
- Celeux, G.; Soromenho, G. An entropy criterion for assessing the number of clusters in a mixture model. J. Classif. 1996, 13, 195–212. [Google Scholar] [CrossRef] [Green Version]
- Nylund, K.L.; Asparouhov, T.; Muthen, B.O. Deciding on the number of classes in latent class analysis and growth mixture modeling a Monte Carlo simulation study. Struct. Equ. Modeling 2007, 14, 535–569. [Google Scholar] [CrossRef]
- Muthén, L.K.; Muthén, B.O. Mplus User’s Guide, 7th ed.; Muthén & Muthén: Los Angeles, CA, USA, 1998–2015.
- Gelman, A. Struggles with survey weighting and regression modeling. Stat. Sci. 2007, 22, 153–164. [Google Scholar] [CrossRef] [Green Version]
- Winship, C.; Radbill, L. Sampling weights and regression analysis. Sociol. Methods Res. 1994, 23, 230–257. [Google Scholar] [CrossRef]
- IBM Corp. IBM SPSS Statistics for Windows; Version 25.0; IBM Corp: Armonk, NY, USA, 2017. [Google Scholar]
- Grotto, D.; Zied, E. The Standard American Diet and Its Relationship to the Health Status of Americans. Nutr. Clin. Pract. 2010, 25, 603–612. [Google Scholar] [CrossRef]
- U.S. Department of Health and Human Services; U.S. Department of Agriculture. 2015–2020 Dietary Guidelines for Americans, 8th ed.; U.S. Department of Health and Human Services and U.S. Department of Agriculture: Washington, DC, USA, 2015.
- Saint, O.; Krueger, P.M. Health Lifestyle behaviors among U.S. adults. SSM Popul. Health 2017, 3, 89–98. [Google Scholar] [CrossRef]
- Hanson, A.J.; Kattelmann, K.K.; McCormack, L.A.; Zhou, W.; Brown, O.N.; Horacek, T.M.; Shelnutt, K.P.; Kidd, T.; Opoku-Acheampong, A.; Franzen-Castle, L.D.; et al. Cooking and Meal Planning as Predictors of Fruit and Vegetable Intake and BMI in First-Year College Students. Int. J. Environ. Res. Public Health 2019, 16, 2462. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ducrot, P.; Mejean, C.; Aroumougame, V.; Ibanez, G.; Allès, B.; Kesse-Guyot, E.; Hercberg, S.; Péneau, S. Meal planning is associated with food variety, diet quality and body weight status in a large sample of French adults. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 12. [Google Scholar] [CrossRef] [PubMed]
- Ludwig, D.S.; Ebbeling, C.B. The Carbohydrate-Insulin Model of Obesity: Beyond “Calories In, Calories Out”. JAMA Intern. Med. 2018, 178, 1098–1103. [Google Scholar] [CrossRef] [PubMed]
- Shan, Z.; Guo, Y.; Hu, F.B.; Liu, L.; Qi, Q. Association of Low-Carbohydrate and Low-Fat Diets With Mortality among US Adults. JAMA Intern. Med. 2020, 180, 513–523. [Google Scholar] [CrossRef] [PubMed]
- Anderson, C.A.; Cobb, L.K.; Miller, E.R.; Woodward, M.; Hottenstein, A.; Chang, A.R.; Mongraw-Chaffin, M.; White, K.; Charleston, J.; Tanaka, T.; et al. Effects of a behavioral intervention that emphasizes spices and herbs on adherence to recommended sodium intake: Results of the SPICE randomized clinical trial. Am. J. Clin. Nutr. 2015, 102, 671–679. [Google Scholar] [CrossRef] [Green Version]
- Taillie, L.S. Who’s cooking? Trends in US home food preparation by gender, education, and race/ethnicity from 2003 to 2016. Nutr. J. 2018, 17, 41. [Google Scholar] [CrossRef] [Green Version]
- Gregory, C.A.; Smith, T.A.; Wendt, M. How Americans rate their diet quality: An increasingly realistic perspective. Econ. Res. Serv. USDA 2011. [Google Scholar] [CrossRef]
- Willet, W. Food frequency methods. In Nutritional Epidemiology; Oxford University Press: Oxford, UK, 1998; pp. 69–91. [Google Scholar]
- Darmon, N.; Dresnowskui, A. Does social class predict diet quality? Am. J. Clin. Nutr. 2008, 87, 1107–1117. [Google Scholar] [CrossRef] [Green Version]
- Loughrey, K.; Basiotis, P.; Zizza, C. Profiles of selected target audiences: Promoting the Dietary Guidelines for Americans. Fam. Econ. Nutr. Rev. 2001, 13, 3–14. [Google Scholar]
- Hiza, H.A.; Casavale, K.O.; Guenther, P.M.; Davis, C.A. Diet Quality of Americans Differs by Age Sex Race/ethnicity Income and education level. J. Acad. Nutr. Diet. 2012, 113, 297–306. [Google Scholar] [CrossRef]
- Yu, D.; Sonderman, J.; Buchowski, M.S.; McLaughlin, J.K.; Shu, X.-O.; Steinwandel, M.; Signorello, L.B.; Zhang, X.; Hargreaves, M.K.; Blot, W.J.; et al. Healthy Eating and Risks of Total and Cause-Specific Death among Low-Income Populations of African-Americans and Other Adults in the Southeastern United States: A Prospective Cohort Study. PLoS Med. 2015, 12, e1001830. [Google Scholar] [CrossRef]
- Micha, R.; Penalvo, J.L.; Cudhea, F.; Imamura, F.; Rehm, C.D.; Mozaffarian, D. Association Between Dietary Factors and Mortality from Heart Disease, Stroke, and Type 2 Diabetes in the United States. JAMA 2017, 317, 912–924. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bruce, M.A.; Beech, B.M.; Thorpe, R.J.; Griffith, D.M. Racial disparities in Sugar-Sweetened beverage consumption change efficacy among male first year college students. Am. J. Mens Health 2017, 10, NP168–NP175. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kell, K.P.; Judd, S.E.; Pearson, K.E.; Shikany, J.M.; Fernández, J.R. Associations between socio-economic status and dietary patterns in US black and white adults. Br. J. Nutr. 2015, 113, 1792–1799. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kuczmarski, M.F.; Bodt, B.A.; Stave, S.E.; Zonderman, A.B.; Evans, M.K. Dietary Patterns Associated with Lower 10-Year Atherosclerotic Cardiovascular Disease Risk among Urban African-American and White Adults Consuming Western Diets. Nutrients 2018, 10, 158. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- James, D.C.S. Cluster Analysis Defines Distinct Dietary Patterns for African-American Men and Women. J. Am. Diet. Assoc. 2009, 109, 255–262. [Google Scholar] [CrossRef] [PubMed]
- Yeh, M.; Ickes, S.B.; Lowenstein, L.M.; Shuval, K.; Ammerman, A.S.; Farris, R.; Katz, D.L. Understanding barriers and facilitators of fruit and vegetable consumption among a diverse multi-ethnic population in the USA. Health Promot. Int. 2008, 23, 42–51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fish, C.A.; Brown, J.R.; Quandt, S.A. African American and Latino Low Income Families’ Food Shopping Behaviors: Promoting Fruit and Vegetable Consumption and Use of Alternative Healthy Food Options. J. Immigr. Minor. Health 2015, 17, 498–505. [Google Scholar] [CrossRef] [PubMed]
- Saksena, M.J.; Okrent, A.M.; Hamrick, K.S. America’s Eating Habits: Food Away From Home. USDA Econ. Res. Serv. 2018. [Google Scholar] [CrossRef]
- Archer, E.; Pavela, G.; Lavie, C.J. The Inadmissibility of “What We Eat In America (WWEIA) and NHANES dietary data in nutrition and obesity research and the scientific formulation of National Dietary Guidelines. Mayo Clin. Proc. 2015, 7, 911–926. [Google Scholar] [CrossRef] [Green Version]
- Davy, B.M.; Estabrooks, P.A. The validity of self-reported dietary intake: Focus on the “What We Eat In America” component of the National Health and Nutrition Examination Survey Initiative. Mayo Clin. Proc. 2015, 7, 845–847. [Google Scholar] [CrossRef] [PubMed]
- Mirel, L.B.; Mohadjer, L.K.; Dohrman, S.M.; Clark, J.; Burt, V.L.; Johnson, C.L.; Curtin, L.R. National Health and Nutrition Examination Survey: Estimation procedures, 2007–2010. Vital Health Stat 2013, 2, 1–17. [Google Scholar]
- Thompson, F.E.; Subar, A. Dietary Assessment Methodology. In Nutrition in the Prevention and Treatment of Disease, 4th ed.; Academic Press: San Diego, CA, USA, 2017; pp. 5–48. [Google Scholar]

| Component | Clarifying Description (Type of Component) | Range | |
|---|---|---|---|
| 1 | Total vegetable | Total vegetable, not dark green, but including legumes (adequacy) | 0–5 |
| 2 | Greens/beans | Dark-green vegetables, beans, or peas (adequacy) | 0–5 |
| 3 | Total fruit | Includes all fruit and 100% fruit juice (adequacy) | 0–5 |
| 4 | Whole grains | Grain products that are 100% whole grains (adequacy) | 0–10 |
| 5 | Dairy | Includes all milk products, such as fluid milk, yogurt, and cheese, and fortified soy beverages (adequacy) | 0–10 |
| 6 | Total protein foods | Includes legumes not counted in Total veg or Greens/beans (adequacy) | 0–5 |
| 7 | Seafood and plant proteins | Includes legumes, seafood, nuts, seeds, and soy products (adequacy) | 0–5 |
| 8 | Fatty acid ratio | Ratio of poly-monounsaturated fatty acids to saturated fatty acids (adequacy) | 0–10 |
| 9 | Sodium | (moderation) | 0–10 |
| 10 | Refined grains | (moderation) | 0–10 |
| 11 | SoFAAS | Calories from solid fats, alcohol and added sugars, threshold for counting alcohol is > 13 g/1000 kcal (moderation) | 0–20 |
| Variables | Category | Sample | Unweighted Sample | |||
|---|---|---|---|---|---|---|
| % US Population or Mean | SE | n (%) or Mean | SD | Range | ||
| Demographic and Socioeconomic Characteristics | ||||||
| Age (years) | 46.32 | 0.01 | 49.20 | 18.27 | 19–80 | |
| Gender | Female Male | 52.2 47.8 | 0.00 | 5058 (51.0) 5623 (49.0) | ||
| Race/ethnicity | Mexican American/Other Hispanic Non-Hispanic/Black Non-Hispanic/White Other—Including Multiracial | 13.6 11.5 69.1 5.8 | 0.00 | 3288 (28.6) 2242 (19.5) 5419 (47.2) 532 (4.6) | ||
| Marital status | Married/cohabitating Previously or never married | 62.5 37.5 | 0.00 | 6680 (59.8) 4496 (40.0) | ||
| Education level | ≤ high school graduate or equivalent Some college College, graduate and above | 43.6 30.3 26.1 | 0.00 | 5956 (53.3) 3022 (27.1) 2187 (19.6) | ||
| Employment status | Working Not working a | 41.2 58.8 | 0.00 | 5954 (51.9) 5526 (48.1) | ||
| Poverty income ratio | Low (≤130%) Middle (131–185%) High (>185%) | 22.2 11.4 66.3 | 3397 (32.6) 1475 (12.8) 5558 (48.4) | |||
| Total number of people in household | 3.03 | 0.00 | 3.21 | 1.70 | 1–7 | |
| Diet Perception and Meal Habits | ||||||
| Energy (kcal/day) | 2128.61 | 0.05 | 2128.61 | 987.44 | 70–13509 | |
| PDQ | Low Medium High | 25.9 42.3 31.8 | 3322 (28.9) 4753 (41.4) 3403 (29.6) | |||
| The number of times cooked dinner at home (a week) | Low (0–2) Sometimes (3–5) High (6–7) | 13.0 38.3 48.1 | 1521 (13.4) 3765 (33.2) 6049 (53.4) | |||
| Class | N. of Parameters | AIC | BIC | Entropy | VLMR a | BLRT a |
|---|---|---|---|---|---|---|
| Daily dietary patterns | ||||||
| 2 | 34 | 591,109.562 | 591,359.409 | 0.993 | p < 0.001 | p < 0.001 |
| 3 | 46 | 580,090.445 | 580,428.473 | 0.996 | p < 0.001 | p < 0.001 |
| 4 | 58 | 575,221.906 | 575,648.116 | 0.873 | p < 0.001 | p < 0.001 |
| 5 b | 70 | 571,428.053 | 571,942.444 | 0.867 | p < 0.001 | p < 0.001 |
| 6 | 82 | 569,268.543 | 569,871.116 | 0.886 | p = 0.8711 | p < 0.001 |
| Dinner dietary patterns | ||||||
| 2 | 34 | 540,270.913 | 540,517.904 | 0.999 | p < 0.001 | p < 0.001 |
| 3 | 46 | 528,976.751 | 529,310.916 | 0.982 | p < 0.001 | p < 0.001 |
| 4 | 58 | 513,747.784 | 514,169.122 | 0.999 | p < 0.001 | p < 0.001 |
| 5 | 70 | 512,479.929 | 512,988.440 | 0.983 | p = 0.0107 | p < 0.001 |
| 6 c | 82 | 501,781.884 | 502,377.569 | 0.976 | p < 0.001 | p < 0.001 |
| 7 | 94 | 498,611.403 | 499,294.262 | 0.971 | p = 0.5023 | p < 0.001 |
| Daily | Dinner | |
|---|---|---|
| Class 1 | SAD | SAD dinner |
| Class 2 | SAD with low sodium | SAD dinner with high sodium |
| Class 3 | Healthy US | SAD dinner with high seafood |
| Class 4 | Healthy US with high vegetable | Healthy US dinner with high vegetable |
| Class 5 | Healthy US with low sodium | Healthy Mediterranean-style dinner |
| Class 6 | Healthy US dinner with low sodium |
| Variables | 5-Class Solution | p Value | ||||
|---|---|---|---|---|---|---|
| Class 1 (n = 2908, 25%) | Class 2 (n = 1568, 14%) | Class 3 (n = 3798, 33%) | Class 4 (n = 2502, 22%) | Class 5 (n = 705, 6%) | ||
| SAD | SAD with Low Sodium | Healthy US | Healthy US with High Vegetable | Healthy US with Low Sodium | ||
| Mean (SD) | ||||||
| Total vegetable | 1.87 (1.42) | 2.23 (1.73) | 3.33 (1.60) | 4.09 (1.14) | 3.10 (1.40) | <0.001 |
| Green/beans | 0.04 (0.18) | 0.02 (0.12) | 0.04 (0.19) | 4.91 (0.28) | 2.52 (0.67) | <0.001 |
| Total fruit | 1.19 (1.72) | 2.32 (2.17) | 2.76 (2.14) | 2.52 (2.13) | 2.31 (2.04) | <0.001 |
| Whole grains | 1.12 (2.10) | 2.51 (3.31) | 2.78 (3.37) | 2.48 (3.24) | 2.13 (3.01) | <0.001 |
| Dairy | 5.00 (3.36) | 6.72 (3.35) | 4.43 (3.37) | 4.66 (3.38) | 4.99 (3.25) | <0.001 |
| Total protein foods | 4.56 (0.66) | 1.68 (0.92) | 4.69 (0.61) | 4.65 (0.92) | 4.55 (1.01) | <0.001 |
| Seafood | 1.39 (1.99) | 0.83 (1.50) | 2.27 (2.29) | 2.47 (2.25) | 2.66 (2.20) | <0.001 |
| Fatty acid ratio | 3.25 (3.08) | 3.37 (3.50) | 6.46 (3.33) | 5.90 (3.50) | 5.29 (3.45) | <0.001 |
| Sodium * | 5.54 (3.46) | 6.17 (3.40) | 3.57 (3.41) | 3.99 (3.50) | 4.26 (3.60) | <0.001 |
| Refined grains * | 6.42 (3.50) | 4.93 (3.95) | 5.73 (3.73) | 6.12 (3.73) | 5.62 (3.64) | <0.001 |
| SoFAAS * | 6.31 (4.35) | 9.31 (6.43) | 16.27 (3.64) | 14.61 (5.50) | 12.56 (5.85) | <0.001 |
| Energy (kcal/day) | 2323.93 (1132.29) | 2037.81 (1057.91) | 1908.47 (865.31) | 1995.99 (895.34) | 2404.42 (1103.41) | <0.001 |
| Variables | 6-Class Solution | p Value | |||||
|---|---|---|---|---|---|---|---|
| Class 1 (n = 1431, 14%) | Class 2 (n = 5028, 48%) | Class 3 (n = 1380, 13%) | Class 4 (n = 1396, 13%) | Class 5 (n = 737, 7%) | Class 6 (n = 584, 6%) | ||
| SAD Dinner | SAD Dinner with High Sodium | SAD Dinner with High Seafood | Healthy US Dinner with High Vegetable | Healthy Mediterranean-Style Dinner | Healthy US Dinner with Low Sodium | ||
| Mean (SD) | |||||||
| Total vegetable | 1.24 (1.65) | 3.17 (1.97) | 2.82 (2.03) | 4.59 (0.88) | 4.48 (0.99) | 2.82 (2.33) | < 0.001 |
| Green/beans | 0.01 (0.15) | 0.03 (0.20) | 0.09 (0.38) | 4.92 (0.34) | 4.89 (0.42) | 0.02 (0.20) | < 0.001 |
| Total fruit | 0.62 (1.53) | 0.69 (1.59) | 0.88 (1.71) | 0.79 (1.68) | 0.80 (1.63) | 1.63 (2.26) | < 0.001 |
| Whole grains | 0.85 (2.60) | 0.65 (2.16) | 1.07 (2.81) | 0.66 (2.22) | 0.92 (2.64) | 1.80 (3.68) | < 0.001 |
| Dairy | 7.16 (4.05) | 3.00 (3.71) | 2.67 (3.67) | 2.93 (6.64) | 2.67 (3.54) | 1.81 (3.14) | < 0.001 |
| Total protein foods | 0.65 (0.88) | 4.76 (0.58) | 4.59 (0.93) | 4.44 (1.40) | 4.88 (0.53) | 0.36 (0.66) | < 0.001 |
| Seafood | 0.04 (0.27) | 0.04 (0.26) | 4.83 (0.51) | 0.13 (0.44) | 4.81 (0.55) | 0.04 (0.25) | < 0.001 |
| Fatty acid ratio | 1.14 (2.31) | 5.00 (3.88) | 7.19 (3.79) | 5.71 (3.91) | 7.13 (3.75) | 8.98 (2.36) | < 0.001 |
| Sodium * | 4.99 (4.23) | 3.30 (3.70) | 3.55 (3.91) | 2.68 (3.55) | 3.23 (3.73) | 5.37 (4.30) | < 0.001 |
| Refined grains * | 3.94 (4.42) | 5.84 (4.10) | 5.77 (4.16) | 6.36 (4.04) | 5.79 (4.19) | 5.95 (4.51) | < 0.001 |
| SoFAAS * | 7.55 (7.02) | 13.41 (6.60) | 14.61 (6.46) | 15.21 (5.85) | 15.89 (5.68) | 15.70 (6.73) | < 0.001 |
| Energy (kcal/day) | 706.48 (626.33) | 850.03 (522.18) | 851.57 (563.57) | 844.54 (478.80) | 914.50 (605.21) | 525.48 (474.47) | < 0.001 |
| Predictors | B (SE) | OR (95% CI) | |
|---|---|---|---|
| Class 2 (SAD with low sodium) vs. Class 1 (SAD) | |||
| Race/ethnicity | Mexican American/Other Hispanic | 0.24 (0.10) | 1.27 (1.04, 1.54) * |
| Non-Hispanic/Black | −0.48 (0.11) | 0.62 (0.50, 0.78) *** | |
| Other | 0.47 (0.23) | 1.60 (1.01, 2.51) * | |
| Non-Hispanic/White a | |||
| Class 3 (Healthy US) vs. Class 1 | |||
| Race/ethnicity | Mexican American/Other Hispanic | 0.70 (0.08) | 2.01 (1.71, 2.36) *** |
| Non-Hispanic/Black | 0.13 (0.08) | 1.14 (0.97, 1.35) | |
| Other | 1.08 (0.18) | 2.95 (2.06, 4.20) *** | |
| Non-Hispanic/White a | |||
| Educational level | College, graduate or above | 0.56 (0.09) | 1.75 (1.46, 2.10) *** |
| Some college | 0.21 (0.07) | 1.23 (1.07, 1.42) ** | |
| ≤ high school graduate/equivalent a | |||
| Income | High | 0.18 (0.08) | 1.20 (1.02, 1.39) * |
| Middle | 0.13 (0.10) | 1.13 (0.94, 1.37) | |
| Low a | |||
| PDQ | High | 0.65 (0.09) | 1.92 (1.62, 2.27) *** |
| Middle | 0.36 (0.07) | 1.43 (1.24, 1.67) *** | |
| Low a | |||
| Class 4 (Healthy US with high vegetable) vs. Class 1 | |||
| Race/ethnicity | Mexican American/Other Hispanic | 1.04 (0.09) | 2.82 (2.37, 3.36) *** |
| Non-Hispanic/Black | 0.15 (0.10) | 1.16 (0.95, 1.40) | |
| Other | 1.35 (0.19) | 3.87 (2.66, 5.63) *** | |
| Non-Hispanic/White a | |||
| Educational level | College, graduate or above | 0.58 (0.10) | 1.79 (1.47, 2.18) *** |
| Some college | 0.13 (0.08) | 1.13 (0.96, 1.34) | |
| ≤ high school graduate/equivalent a | |||
| Frequency of cooked dinner at home (a week) | High (6–7) | 0.39 (0.15) | 1.47 (1.09, 1.98) * |
| Moderate (3–5) | 0.28 (0.15) | 1.33 (0.98, 1.79) | |
| Low (0–2) a | |||
| PDQ | High | 0.86 (0.10) | 2.36 (1.96, 2.85) *** |
| Middle | 0.36 (0.09) | 1.44 (1.22, 1.70) *** | |
| Low a | |||
| Class 5 (Healthy US with low sodium) vs. Class 1 | |||
| Race/ethnicity | Mexican American/Other Hispanic | 0.88 (0.13) | 0.41 (1.87, 3.10) *** |
| Non-Hispanic/Black | −0.21 (0.16) | 0.81 (0.60, 1.11) | |
| Others | 1.32 (0.24) | 3.74 (2.32, 6.25) *** | |
| Non-Hispanic/White a | |||
| Educational level | College, graduate or above | 0.83 (0.14) | 2.29 (1.73, 3.02) *** |
| Some college | 0.29 (0.13) | 1.34 (1.05, 1.71) * | |
| ≤ high school graduate/equivalent a | |||
| Predictors | B (SE) | OR (95% CI) | |
|---|---|---|---|
| Class 2 (SAD dinner with high sodium) vs. Class 1 (SAD dinner) | |||
| Race/ethnicity | Mexican American/Other Hispanic | −0.35 (0.81) | 0.70 (0.60, 0.82) *** |
| Non-Hispanic/Black | 0.53 (0.10) | 1.70 (1.40, 2.06) *** | |
| Other | 0.01 (0.19) | 1.00 (0.70, 1.45) | |
| Non-Hispanic/White a | |||
| Frequency of cooked dinner at home (a week) | High (6–7) | 0.20 (0.10) | 1.23 (1.00, 1.50) * |
| Moderate (3–5) | 0.17 (0.11) | 1.19 (0.97, 1.46) | |
| Low (0–2) a | |||
| Class 3 (SAD dinner with high seafood) vs. Class 1 | |||
| Race/ethnicity | Mexican American/Other Hispanic | −0.07 (0.10) | 0.93 (0.76, 1.14) |
| Non-Hispanic/Black | 0.48 (0.12) | 1.62 (1.28, 2.06) *** | |
| Other | 0.93 (0.20) | 2.54 (1.71, 3.77) *** | |
| Non-Hispanic/White a | |||
| Educational level | College, graduate or above | 0.28 (0.12) | 1.32 (1.05, 1.65) * |
| Some college | 0.19 (0.10) | 1.10 (0.92, 1.32) | |
| ≤ high school graduate/equivalent a | |||
| Income | High | −0.30 (0.10) | 0.74 (0.61, 0.91) ** |
| Middle | −0.15 (0.10) | 0.87 (0.71, 1.05) | |
| Low a | |||
| Class 4 (Healthy US dinner with high vegetable) vs. Class 1 | |||
| Race/ethnicity | Mexican American/Other Hispanic | −0.06 (0.10) | 0.94 (0.77, 1.16) |
| Non-Hispanic/Black | 0.72 (0.12) | 2.05 (1.62, 2.59) *** | |
| Other | 0.61 (0.21) | 1.84 (1.21, 2.79) ** | |
| Non-Hispanic/White a | |||
| Income | High | −0.31 (0.10) | 0.74 (0.60, 0.90) ** |
| Middle | −0.32 (0.13) | 0.72 (0.56, 0.93) * | |
| Low a | |||
| Frequency of cooked dinner at home (a week) | High (6–7) | 0.29 (0.13) | 1.34 (1.03, 1.74) * |
| Moderate (3–5) | 0.34 (0.14) | 1.41 (1.08, 1.84) * | |
| Low (0–2) a | |||
| PDQ | High | −0.48 (0.11) | 0.62 (0.50, 0.78) *** |
| Middle | −0.18 (0.10) | 0.84 (0.69, 1.02) | |
| Low a | |||
| Class 5 (Healthy Mediterranean-style dinner) vs. Class 1 | |||
| Race/ethnicity | Mexican American/Other Hispanic | 0.18 (0.13) | 1.20 (0.94, 1.53) |
| Non-Hispanic/Black | 0.53 (0.15) | 1.69 (1.26, 2.27) *** | |
| Other | 1.29 (0.22) | 3.63 (2.37, 5.56) *** | |
| Non-Hispanic/White a | |||
| Educational level | College, graduate or above | 0.47 (0.13) | 1.60 (1.23, 2.08) *** |
| Some college | 0.08 (0.13) | 1.08 (0.85, 1.38) | |
| ≤ high school graduate/equivalent a | |||
| Income | High | −0.35 (0.13) | 0.71 (0.55, 0.91) ** |
| Middle | −0.13 (0.15) | 0.88 (0.65, 0.18) | |
| Low a | |||
| Frequency of cooked dinner at home (a week) | High (6–7) | 0.45 (0.17) | 1.57 (1.13, 2.18) ** |
| Moderate (3–5) | 0.30 (0.17) | 1.35 (0.97, 1.90) | |
| Low (0–2) a | |||
| PDQ | High | −0.42 (0.14) | 0.66 (0.51, 0.86) ** |
| Middle | −0.33 (0.12) | 0.72 (0.57, 0.91) ** | |
| Low a | |||
| Class 6 (Healthy US dinner with low sodium) vs. Class 1 | |||
| Race/ethnicity | Mexican American/Other Hispanic | 0.22 (0.13) | 1.25 (0.97, 1.62) |
| Non-Hispanic/Black | 0.37 (0.16) | 1.45(1.05, 1.99) * | |
| Other | 1.08 (0.24) | 2.94(1.84, 4.72) *** | |
| Non-Hispanic/White a | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Farmer, N.; Lee, L.J.; Powell-Wiley, T.M.; Wallen, G.R. Cooking Frequency and Perception of Diet among US Adults Are Associated with US Healthy and Healthy Mediterranean-Style Dietary Related Classes: A Latent Class Profile Analysis. Nutrients 2020, 12, 3268. https://doi.org/10.3390/nu12113268
Farmer N, Lee LJ, Powell-Wiley TM, Wallen GR. Cooking Frequency and Perception of Diet among US Adults Are Associated with US Healthy and Healthy Mediterranean-Style Dietary Related Classes: A Latent Class Profile Analysis. Nutrients. 2020; 12(11):3268. https://doi.org/10.3390/nu12113268
Chicago/Turabian StyleFarmer, Nicole, Lena J. Lee, Tiffany M. Powell-Wiley, and Gwenyth R. Wallen. 2020. "Cooking Frequency and Perception of Diet among US Adults Are Associated with US Healthy and Healthy Mediterranean-Style Dietary Related Classes: A Latent Class Profile Analysis" Nutrients 12, no. 11: 3268. https://doi.org/10.3390/nu12113268
APA StyleFarmer, N., Lee, L. J., Powell-Wiley, T. M., & Wallen, G. R. (2020). Cooking Frequency and Perception of Diet among US Adults Are Associated with US Healthy and Healthy Mediterranean-Style Dietary Related Classes: A Latent Class Profile Analysis. Nutrients, 12(11), 3268. https://doi.org/10.3390/nu12113268








