Brain Magnetic Resonance Findings in 117 Children with Autism Spectrum Disorder under 5 Years Old
Abstract
:1. Introduction
2. Materials and Methods
2.1. Sleep-EEG Acquisition
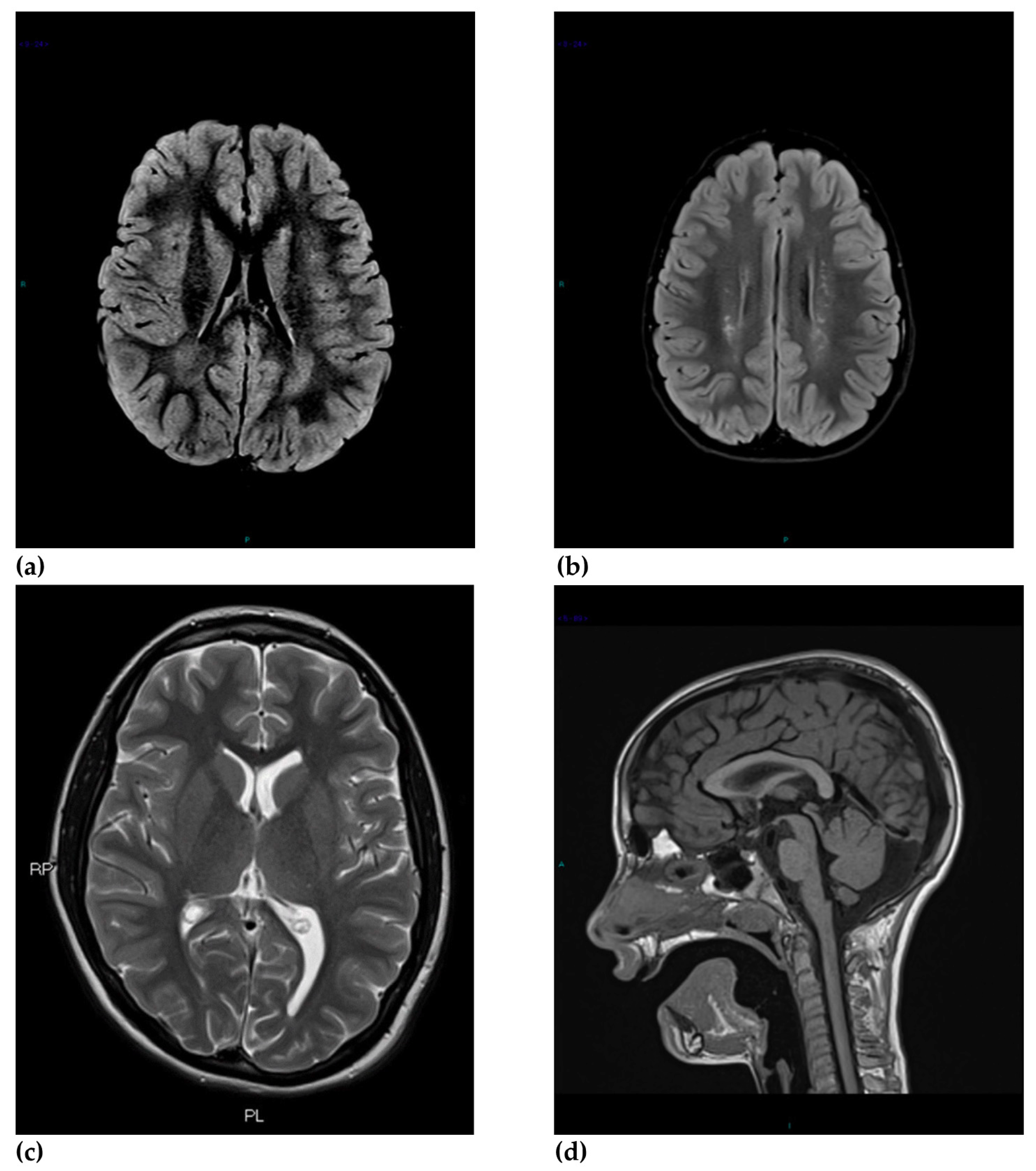
2.2. Magnetic Resonance Imaging Acquisition
2.3. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®); American Psychiatric Pubication; American Psychiatric Association: Arlington County, VA, USA, 2013. [Google Scholar]
- Elsabbagh, M.; Divan, G.; Koh, Y.G.; Kim, Y.S.; Kauchali, S.; Marcín, C.; Montiel-Nava, C.; Patel, V.; Paula, C.S.; Wang, C.; et al. Global Prevalence of Autism and Other Pervasive Developmental Disorders. Autism Res. 2012, 5, 160–179. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maenner, M.J.; Shaw, K.A.; Baio, J.; Washington, A.; Patrick, M.; DiRienzo, M.; Christensen, D.L.; Wiggins, L.D.; Pettygrove, S.; Jennifer, G.A.; et al. Prevalence of Autism Spectrum Disorder Among Children Aged 8 Years—Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2016. MMWR Surveill. Summ. 2020, 69, 1–12. [Google Scholar] [CrossRef]
- Cadman, T.; Eklund, H.; Howley, D.; Hayward, H.; Clarke, H.; Findon, J.; Xenitidis, K.; Murphy, D.; Asherson, P.; Glaser, K. Caregiver burden as people with autism spectrum disorder and attention-deficit/hyperactivity disorder transition into adolescence and adulthood in the United Kingdom. J. Am. Acad. Child. Adolesc. Psychiatry 2012, 51, 879–888. [Google Scholar] [CrossRef]
- Buescher, A.V.; Cidav, Z.; Knapp, M.; Mandell, D.S. Costs of autism spectrum disorders in the United Kingdom and the United States. JAMA Pediatr. 2014, 168, 721–728. [Google Scholar] [CrossRef] [PubMed]
- Vorstman, J.A.S.; Parr, J.R.; Moreno-De-Luca, D.; Anney, R.J.L.; Nurnberger, J.I., Jr.; Hallmayer, J.F. Autism genetics: Opportunities and challenges for clinical translation. Nat. Rev. Genet. 2017, 18, 362–376. [Google Scholar] [CrossRef] [PubMed]
- Ecker, C. The neuroanatomy of autism spectrum disorder: An overview of structural neuroimaging findings and their translatability to the clinical setting. Autism 2017, 21, 18–28. [Google Scholar] [CrossRef] [PubMed]
- Gabard-Durnam, L.J.; Wilkinson, C.; Kapur, K.; Tager-Flusberg, H.; Rand, L.; Nelson, C.A. Longitudinal EEG power in the first postnatal year differentiates autism outcomes. Nat. Commun. 2019, 10, 4188. [Google Scholar] [CrossRef]
- Kagan-Kushnir, T.; Roberts, S.W.; Snead, O.C. Screening Electroencephalograms in Autism Spectrum Disorders: Evidence-Based Guideline. J. Child Neurol. 2005, 20, 197–206. [Google Scholar] [CrossRef]
- Volkmar, F.R.; McPartland, J.C. From Kanner to DSM-5: Autism as an evolving diagnostic concept. Annu. Rev. Clin. Psychol. 2014, 10, 193–212. [Google Scholar] [CrossRef] [Green Version]
- Courchesne, E.; Karns, C.M.; Davis, H.R.; Ziccardi, R.; Carper, R.A.; Tigue, Z.D.; Chisum, H.J.; Moses, P.; Pierce, K.; Lord, C.; et al. Unusual brain growth patterns in early life in patients with autistic disorder: An MRI study. Neurology 2001, 57, 245–254. [Google Scholar] [CrossRef]
- Shen, M.D.; Nordahl, C.W.; Young, G.S.; Wootton-Gorges, S.L.; Lee, A.; Liston, S.E.; Harrington, K.R.; Ozonoff, S.; Amaral, D.G. Early brain enlargement and elevated extra-axial fluid in infants who develop autism spectrum disorder. Brain 2013, 136, 2825–2835. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zielinski, B.A.; Prigge, M.B.D.; Nielsen, J.A.; Froehlich, A.L.; Abildskov, T.J.; Anderson, J.S.; Fletcher, P.T.; Zygmunt, K.M.; Travers, B.G.; Lange, N.; et al. Longitudinal changes in cortical thickness in autism and typical development. Brain 2014, 137, 1799–1812. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shen, M.D.; Nordahl, C.W.; Li, D.D.; Lee, A.; Angkustsiri, K.; Emerson, R.W.; Rogers, S.J.; Ozonoff, S.; Amaral, D.G. Extra-axial cerebrospinal fluid in high-risk and normal-risk children with autism aged 2–4 years: A case-control study. Lancet Psychiatry 2018, 5895–5904. [Google Scholar] [CrossRef]
- Shen, M.D.; Kim, S.H.; McKinstry, R.C.; Gu, H.; Hazlett, H.C.; Nordahl, C.W.; Emerson, R.W.; Shaw, D.; Elison, J.T.; Swanson, M.R.; et al. Increased extra-axial cerebrospinal fluid in high-risk infants who later develop autism. Biol. Psychiatry 2017, 82, 186–193. [Google Scholar] [CrossRef]
- Conti, E.; Mitra, J.; Calderoni, S.; Pannek, K.; Shen, K.K.; Pagnozzi, A.; Rose, S.; Mazzotti, S.; Scelfo, D.; Tosetti, M.; et al. Network over-connectivity differentiates autism spectrum disorder from other developmental disorders in toddlers: A diffusion MRI study. Hum. Brain Mapp. 2017, 38, 2333–2344. [Google Scholar] [CrossRef] [Green Version]
- Monterrey, J.C.; Philips, J.; Cleveland, S.; Tanaka, S.; Barnes, P.; Hallmayer, J.F.; Reiss, A.L.; Lazzeroni, L.C.; Hardan, A.Y. Incidental brain MRI findings in an autism twin study. Autism Res. 2017, 10, 113–120. [Google Scholar] [CrossRef]
- Dangouloff-Ros, V.; Roux, C.J.; Boulouis, G.; Levy, R.; Nicolas, N.; Lozach, C.; Grevent, D.; Brunelle, F.; Boddaert, N.; Naggara, O. Incidental Brain MRI Findings in Children: A Systematic Review and Meta-Analysis. Am. J. Neuroradiol. 2019, 40, 1818–1823. [Google Scholar] [CrossRef]
- Taber, K.H.; Shaw, J.B.; Loveland, K.A.; Pearson, D.A.; Lane, D.M.; Hayman, L.A. Accentuated Virchow-Robin spaces in the centrum semi ovale in children with autistic disorder. J. Comput. Assist. Tomogr. 2014, 28, 263–268. [Google Scholar] [CrossRef]
- Zeegers, M.; Van Der Grond, J.; Durston, S.; Nievelstein, R.J.; Witkamp, T.; Van Daalen, E.; Buitelaar, J.; Engeland, H.V. Radiological findings in autistic and developmentally delayed children. Brain Dev. 2006, 28, 495–499. [Google Scholar] [CrossRef]
- Boddaert, N.; Zilbovicius, M.; Philipe, A.; Robel, L.; Bourgeois, M.; Barthelemy, C.; Seidenwurm, D.; Meressel, I.; Laurierl, L.; Desguerre, I.; et al. MRI findings in 77 children with non-syndromic autistic disorder. PLoS ONE 2009, 4. [Google Scholar] [CrossRef]
- Zeglam, A.M.; Al-Ogab, M.F.; Al-Shaftery, T. MRI or not to MRI! should brain MRI be a routine investigation in children with autistic spectrum disorders? Acta Neurol. Belgica 2015, 115, 351–354. [Google Scholar] [CrossRef] [PubMed]
- Erbetta, A.; Bulgheroni, S.; Contarino, V.E.; Chiapparini, L.; Esposito, S.; Annunziata, S.; Riva, D. Low-Functioning Autism and Nonsyndromic Intellectual Disability: Magnetic Resonance Imaging (MRI) Findings. J. Child. Neurol. 2015, 30, 1658–1663. [Google Scholar] [CrossRef] [PubMed]
- Vasa, R.A.; Ranta, M.; Huisman, T.A.G.M.; Pinto, P.S.; Tillman, R.M.; Mostofsky, S.H. Normal rates of neuroradiological findings in children with high functioning autism. J. Autism Dev. Disord. 2012, 42, 1662–1670. [Google Scholar] [CrossRef] [Green Version]
- Gupta, S.; Kanamalla, U.; Gupta, V. Are incidental findings on brain magnetic resonance images in children merely incidental? J. Child. Neurol. 2010, 25, 1511–1516. [Google Scholar] [CrossRef]
- Carter, M.T.; Scherer, S.W. Autism spectrum disorder in the genetics clinic: A review. Clin. Genet. 2013, 83, 399–407. [Google Scholar] [CrossRef]
- Lord, C.; Rutter, M.; Di Lavore, P.; Risi, S.; Gotham, K.; Bishop, S.L. Autism Diagnostic Observation Schedule (ADOS-2): Manual, 2nd ed.; Western Psychological Services: Torrance, CA, USA, 2012. [Google Scholar]
- Schopler, E.; Van Bourgondien, M.E.; Wellman, G.J.; Love, S.R. Childhood Autism Rating Scale, Second Edition (CARS2); Western Psychological Services: Torrance, CA, USA, 2010. [Google Scholar]
- Heier, L.A.; Bauer, C.J.; Schwartz, L.; Zimmerman, R.D.; Morgello, S.; Deck, M.D. Large Virchow-Robin Spaces: MR-Clinical Correlation. Am. J. Neuroradiol. 1989, 10, 929–936. [Google Scholar]
- Hidalgo, J.A.; Tork, C.A.; Varacallo, M. Arnold Chiari Malformation; StatPearls Publishing: Treasure Island, FL, USA, 2020. [Google Scholar]
- Raybaud, C.; Jallo, G.I. Chiari 1 deformity in children: Etiopathogenesis and radiologic diagnosis. Handb. Clin. Neurol. 2018, 155, 25–48. [Google Scholar] [CrossRef] [PubMed]
- Langridge, B.; Phillips, E.; Choi, D. Chiari Malformation Type 1: A Systematic Review of Natural History and Conservative Management. World Neurosurg. 2017, 104, 213–219. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dinçer, A.; Özek, M.M. Radiologic Evaluation of Pediatric Hydrocephalus. Child’s Nerv. Syst. 2011, 27, 1543–1562. [Google Scholar] [CrossRef]
- Gokce, E.; Beyhan, M. Evaluation of Pineal Cysts with Magnetic Resonance Imaging. World J. Radiol. 2018, 10, 65–77. [Google Scholar] [CrossRef]
- Boseman, T.; Orman, G.; Boltshauser, E.; Tekes, A.; Huisman, T.A.G.M.; Poretti, A. Congenital Abnormalities of the Posterior Fossa. Radiographics 2015, 35, 200–220. [Google Scholar] [CrossRef] [PubMed]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gupta, S.N.; Gupta, V.S.; White, A.C. Spectrum of intracranial incidental findings on pediatric brain magnetic resonance imaging: What clinician should know? World J. Clin. Pediatr. 2016, 5, 262–272. [Google Scholar] [CrossRef] [PubMed]
- Ismail, M.M.; Keynton, R.S.; Mostapha, M.M.; ElTanboly, A.H.; Casanova, M.F.; Gimel’farb, G.L.; El-Baz, A. Studying autism spectrum disorder with structural and diffusion magnetic resonance imaging: A survey. Front. Hum. Neurosci. 2016, 10, 211. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Palmen, S.J.M.C.; Hulshoff Pol, H.E.; Kemner, C.; Schnack, H.G.; Janssen, J.; Kahn, R.S.; van Engeland, H. Larger brains in medication naive high-functioning subjects with pervasive developmental disorder. J. Autism Dev. Disord. 2004, 34, 603–613. [Google Scholar] [CrossRef] [PubMed]
- Turner, A.H.; Greenspan, K.S.; van Erp, T.G.M. Pallidum and lateral ventricle volume enlargement in autism spectrum disorder. Psychiatry Res. 2016, 252, 40–45. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Conley, A. Ventricular enlargement. In Encyclopedia of Clinical Neuropsychology; Kreutzer, J.S., DeLuca, J., Caplan, B., Eds.; Springer: Berlin/Heidelberg, Germany, 2011; pp. 2600–2601. ISBN 978-0-387-79948-3. [Google Scholar]
- Stanfield, A.C.; McIntosh, A.M.; Spencer, M.D.; Philip, R.; Gaur, S.; Lawrie, S.M. Towards a neuroanatomy of autism: A systematic review and meta-analysis of structural magnetic resonance imaging studies. Eur. Psychiatry 2008, 23, 289–299. [Google Scholar] [CrossRef] [PubMed]
- Haar, S.; Berman, S.; Behrmann, M.; Dinstein, I. Anatomical Abnormalities in Autism? Cerebral. Cortex 2016, 26, 1440–1452. [Google Scholar] [CrossRef] [Green Version]
- Levman, J.; Vasung, L.; MacDonald, P.; Rowley, S.; Stewart, N.; Lim, A.; Ewenson, B.; Galaburda, A.; Takahashi, E. Regional volumetric abnormalities in pediatric autism revealed by structural magnetic resonance imaging. Int. J. Dev. Neurosci. 2018, 71, 34–45. [Google Scholar] [CrossRef]
- Hendren, R.L.; De Backer, I.; Pandina, G.J. Review of neuroimaging studies of child and adolescent psychiatric disorders from the past 10 years. J. Am. Acad. Child Adolesc. Psychiatry 2000, 39, 815–828. [Google Scholar] [CrossRef]
- McKechnie, L.; Vasudevan, C.; Levene, M. Neonatal outcome of congenital ventriculomegaly. Semin. Fetal. Neonatal. Med. 2012, 17, 301–307. [Google Scholar] [CrossRef]
- Blackmon, K.; Ben-Avi, E.; Wang, X.; Pardoe, H.R.; Di Martino, A.; Halgren, E.; Devinsky, O.; Thesen, T.; Kuzniecky, R. Periventricular white matter abnormalities and restricted repetitive behavior in autism spectrum disorder. Neuroimage Clin. 2015, 10, 36–45. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barkovich, A.J. Concepts of Myelin and Myelination in Neuroradiology. Am. J. Neuroradiol. 2000, 6, 1099–1109. [Google Scholar] [PubMed]
- Akbari, S.H.; Limbrick, D.D., Jr.; McKinstry, R.C.; Altaye, M.; Ragan, D.K.; Yuan, W.; Mangano, F.T.; Holland, S.K.; Shimony, J.S. Periventricular hyperintensity in children with hydrocephalus. Pediatr. Radiol. 2015, 45, 1189–1197. [Google Scholar] [CrossRef] [Green Version]
- Back, S.A. Perinatal white matter injury: The changing spectrum of pathology and emerging insights into pathogenetic mechanisms. Ment. Retard. Dev. Disabil. Res. Rev. 2006, 12, 129–140. [Google Scholar] [CrossRef]
- Bano, S.; Chaudhary, V.; Garga, U.C. Neonatal hypoxic-ischemic encephalopathy: A radiological review. J. Pediatr. Neurosci. 2017, 12, 1–6. [Google Scholar] [CrossRef]
- Varghese, B.; Xavier, R.; Manoj, V.C.; Aneesh, M.K.; Priya, P.S.; Kumar, A.; Sreenivasan, V.K. Magnetic resonance imaging spectrum of perinatal hypoxic–ischemic brain injury. Neuroimaging 2016, 26, 316–327. [Google Scholar] [CrossRef] [PubMed]
- Glasson, E.J.; Bower, C.; Petterson, B.; de Klerk, N.; Chaney, G.; Hallmayer, J.F. Perinatal factors and the development of autism: A population study. Arch. Gen. Psychiatry 2004, 61, 618–627. [Google Scholar] [CrossRef] [Green Version]
- Bax, M.; Tydeman, C.; Flodmark, O. Clinical and MRI correlates of cerebral palsy: The European Cerebral Palsy Study. JAMA 2006, 296, 1602–1608. [Google Scholar] [CrossRef] [Green Version]
- Aoki, Y.; Yoncheva, Y.N.; Chen, B.; Nath, T.; Sharp, D.; Lazar, M.; Velasco, P.; Milham, M.P.; Di Martino, A. Association of White Matter Structure With Autism Spectrum Disorder and Attention-Deficit/Hyperactivity Disorder. JAMA Psychiatry 2017, 74, 1120–1128. [Google Scholar] [CrossRef]
- Hong, S.J.; Hyung, B.; Paquola, C.; Bernhardt, B.C. The Superficial White Matter in Autism and Its Role in Connectivity Anomalies and Symptom Severity. Cereb. Cortex 2019, 29, 4415–4425. [Google Scholar] [CrossRef]
- Wolff, J.J.; Gu, H.; Gerig, G.; Elison, J.T.; Styner, M.; Gouttard, S.; Botteron, K.N.; Dager, S.R.; Dawson, G.; Estes, A.M.; et al. Differences in white matter fiber tract development present from 6 to 24 months in infants with autism. Am. J. Psychiatry 2012, 169, 589–600. [Google Scholar] [CrossRef]
- Solso, S.; Xu, R.; Proudfoot, J.; Hagled, D.J., Jr.; Campbell, K.; Venkatraman, V.; Barnes, C.C.; Ahrens-Barbeau, C.; Pierce, K.; Dale, A.; et al. Diffusion tensor imaging provides evidence of possible axonal overconnectivity in frontal lobes in autism spectrum disorder toddlers. Biol. Psychiatry 2016, 79, 676–684. [Google Scholar] [CrossRef] [Green Version]
- Lewis, J.D.; Evans, A.C.; Pruett, J.R.; Botteron, K.N.; McKinstry, R.C.; Zwaigenbaum, L.; Estes, A.M.; Collins, D.L.; Kostopoulos, P.; Gerig, G.; et al. The emergence of network inefficiencies in infants with autism spectrum disorder. Biol. Psychiatry 2017, 82, 176–185. [Google Scholar] [CrossRef] [PubMed]
- Conti, E.; Calderoni, S.; Marchi, V.; Muratori, F.; Cioni, G.; Guzzetta, A. The first 1000 days of the autistic brain: A systematic review of diffusion imaging studies. Front. Hum. Neurosci. 2015, 9. [Google Scholar] [CrossRef]
- Bolduc, M.E.; Limperopoulos, C. Neurodevelopmental outcomes in children with cerebellar malformations: A systematic review. Dev. Med. Child Neurol. 2009, 51, 256–267. [Google Scholar] [CrossRef]
- Zimmer, E.Z.; Lowenstein, L.; Bronshtein, M.; Goldsher, D.; Aharon-Peretz, J. Clinical significance of isolated mega cisterna magna. Arch. Gynecol. Obstet. 2007, 276, 487. [Google Scholar] [CrossRef]
- Courchesne, E.; Yeung-Courchesne, R.; Press, G.A.; Hesselink, J.R.; Jernigan, T.L. Hypoplasia of cerebellar vermal lobules VI and VII in autism. N. Engl. J. Med. 1988, 318, 1349–1354. [Google Scholar] [CrossRef] [Green Version]
- Scott, J.A.; Schumann, C.M.; Goodlin-Jones, B.L.; Amaral, D.G. A comprehensive volumetric analysis of the cerebellum in children and adolescents with autism spectrum disorder. Autism Res. 2009, 2, 246–257. [Google Scholar] [CrossRef]
- Webb, S.; Sparks, B.F.; Friedman, S.D.; Shaw, D.; Giedd, J.; Dawson, G.; Dager, S.R. Cerebellar vermal volumes and behavioral correlates in children with autism spectrum disorder. Psychiatry Res. 2009, 172, 61–67. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rollins, N.K.; Deline, C.; Morriss, M.C. Prevalence and clinical significance of dilated Virchow-Robin spaces in childhood. Radiology 1993, 189, 53–57. [Google Scholar] [CrossRef] [PubMed]
- Linee Guida Nazionali. Sistema Nazionale per le Linee Guida dell’Istituto Superiore di Sanità: Il Trattamento dei Disturbi dello Spettro Autistico nei Bambini e Negli Adolescenti. October 2011, Volume 21. Available online: http://old.iss.it/auti/index.php?lang=1&tipo=5 (accessed on 15 October 2020).
- Filipek, P.A.; Accardo, P.J.; Ashwal, S.; Baranek, G.T., Jr.; Cook, E.H.; Dawson, G.; Gordon, B.; Gravel, J.S.; Johnson, C.P.; Kallen, R.J.; et al. Practice parameter: Screening and diagnosis of autism. Report of the quality standards subcommittee of the American Academy of Neurology AND the Child Neurology Society. Neurology 2000, 55, 468–479. [Google Scholar] [CrossRef] [PubMed]
- Cooper, A.S.; Friedlaender, E.; Levy, S.E.; Shekdar, K.V.; Bradford, A.B.; Wells, K.E.; Mollen, C. The Implications of Brain MRI in Autism Spectrum Disorder. J. Child Neurol. 2016, 31, 1611–1616. [Google Scholar] [CrossRef] [PubMed]
- Anagnostou, E.; Taylor, M.J. Review of neuroimaging in autism spectrum disorders: What have we learned and where we go from here. Mol. Autism. 2011, 2, 4. [Google Scholar] [CrossRef] [Green Version]
| Children with ASD (n = 117) | High-Functioning ASD (n = 41) | Developmental Delay-ASD (n = 76) | Typically Developing Children (n = 39) | Statistics | p | |
|---|---|---|---|---|---|---|
| Age (y), mean (SD), range | 3.4 (0.87), 1.1–4.11 | 3.2 (0.85), 1.1–4.10 | 3.5 (0.86), 1.2–4.11 | 3.2(1.48), 1.1–5.7 | F (2, 151) = 1509 | 0.224 |
| Sex | 90 M; 27 F | 30 M; 11 F | 60 M; 16 F | 21 M; 18 F | Fisher exact test | 0.008 * |
| ADOS-2 comparison score, mean (SD), range | 7.16 (2), 3–10 | 6.51 (2), 3–10 | 7.64 (2), 4–10 | NA | F (1, 116) = 11,561 | 0.001 * |
| Mild ASD | 13 | 9 | 4 | NA | Fisher exact test | 0.01 * |
| Moderate ASD | 46 | 17 | 29 | NA | Fisher exact test | 0.843 |
| Severe ASD | 58 | 15 | 43 | NA | Fisher exact test | 0.402 |
| IQ/GD, mean (SD), range | 67 (27) 25–129 | 94 (19) 71–129 | 48 (12) 25–70 | NA |
| MRI Findings | ASD Children (n = 117) | HF-ASD (n = 41) | DD-ASD (n = 76) | Typically Developing Children (n = 39) | p |
|---|---|---|---|---|---|
| Abnormal MRI | 64 * | 27 * | 37 | 14 * | <0.05 *,1 |
| Isolated IF | 37 * | 15 * | 22 * | 13 * | All Ps < 0.05 * |
| 2 IFs | 22 | 10 | 12 | 1 | NS |
| 3 IFs | 5 | 2 | 3 | 0 | NS |
| Major abnormal findings | |||||
| Abnormal signal intensities | 26 | 10 | 16 | 4 | NS |
| Retrotrigonal WM intensities | 18 | 4 | 14 | 3 | NS |
| Gliosis | 7 | 6 * | 1 * | 2 | 0.007 * |
| Myelination delay | 3 | 2 | 1 | 0 | NS |
| Abnormal cortical development and/or organization | 2 | 1 | 1 | 1 | NS |
| Atrophy | 1 | 1 | 0 | 0 | NS |
| Corpus callosum anomalies | 5 | 1 | 4 | 0 | NS |
| Ventricular anomalies | 11 | 7 * | 4 * | 3 | 0.049 * |
| Ventricular enlargement and asymmetries | 9 | 6 * | 3 | 0 * | 0.026 * |
| Other ventricular anomalies | 2 | 1 | 1 | 3 | NS |
| Chiari I malformation | 3 | 2 | 1 | 1 | NS |
| Cerebellar anomalies | 4 | 2 | 2 | 0 | NS |
| Minor abnormal findings | |||||
| Dilated Virchow-Robin spaces | 15 | 5 | 10 | 1 | NS |
| Mega cisterna magna | 12 * | 5 | 7 | 0 * | 0.038 * |
| Pineal cyst | 13 | 4 | 9 | 2 | NS |
| Choroid plexus cyst | 2 | 2 | 0 | 1 | NS |
| Arachnoid cyst | 2 | 1 | 1 | 2 | NS |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rochat, M.J.; Distefano, G.; Maffei, M.; Toni, F.; Posar, A.; Scaduto, M.C.; Resca, F.; Cameli, C.; Bacchelli, E.; Maestrini, E.; et al. Brain Magnetic Resonance Findings in 117 Children with Autism Spectrum Disorder under 5 Years Old. Brain Sci. 2020, 10, 741. https://doi.org/10.3390/brainsci10100741
Rochat MJ, Distefano G, Maffei M, Toni F, Posar A, Scaduto MC, Resca F, Cameli C, Bacchelli E, Maestrini E, et al. Brain Magnetic Resonance Findings in 117 Children with Autism Spectrum Disorder under 5 Years Old. Brain Sciences. 2020; 10(10):741. https://doi.org/10.3390/brainsci10100741
Chicago/Turabian StyleRochat, Magali Jane, Giacomo Distefano, Monica Maffei, Francesco Toni, Annio Posar, Maria Cristina Scaduto, Federica Resca, Cinzia Cameli, Elena Bacchelli, Elena Maestrini, and et al. 2020. "Brain Magnetic Resonance Findings in 117 Children with Autism Spectrum Disorder under 5 Years Old" Brain Sciences 10, no. 10: 741. https://doi.org/10.3390/brainsci10100741
APA StyleRochat, M. J., Distefano, G., Maffei, M., Toni, F., Posar, A., Scaduto, M. C., Resca, F., Cameli, C., Bacchelli, E., Maestrini, E., & Visconti, P. (2020). Brain Magnetic Resonance Findings in 117 Children with Autism Spectrum Disorder under 5 Years Old. Brain Sciences, 10(10), 741. https://doi.org/10.3390/brainsci10100741






