The Impact of Time-Restricted Diet on Sleep and Metabolism in Obese Volunteers
Abstract
1. Introduction
2. Methods
2.1. Participants
2.2. Statistical Analysis
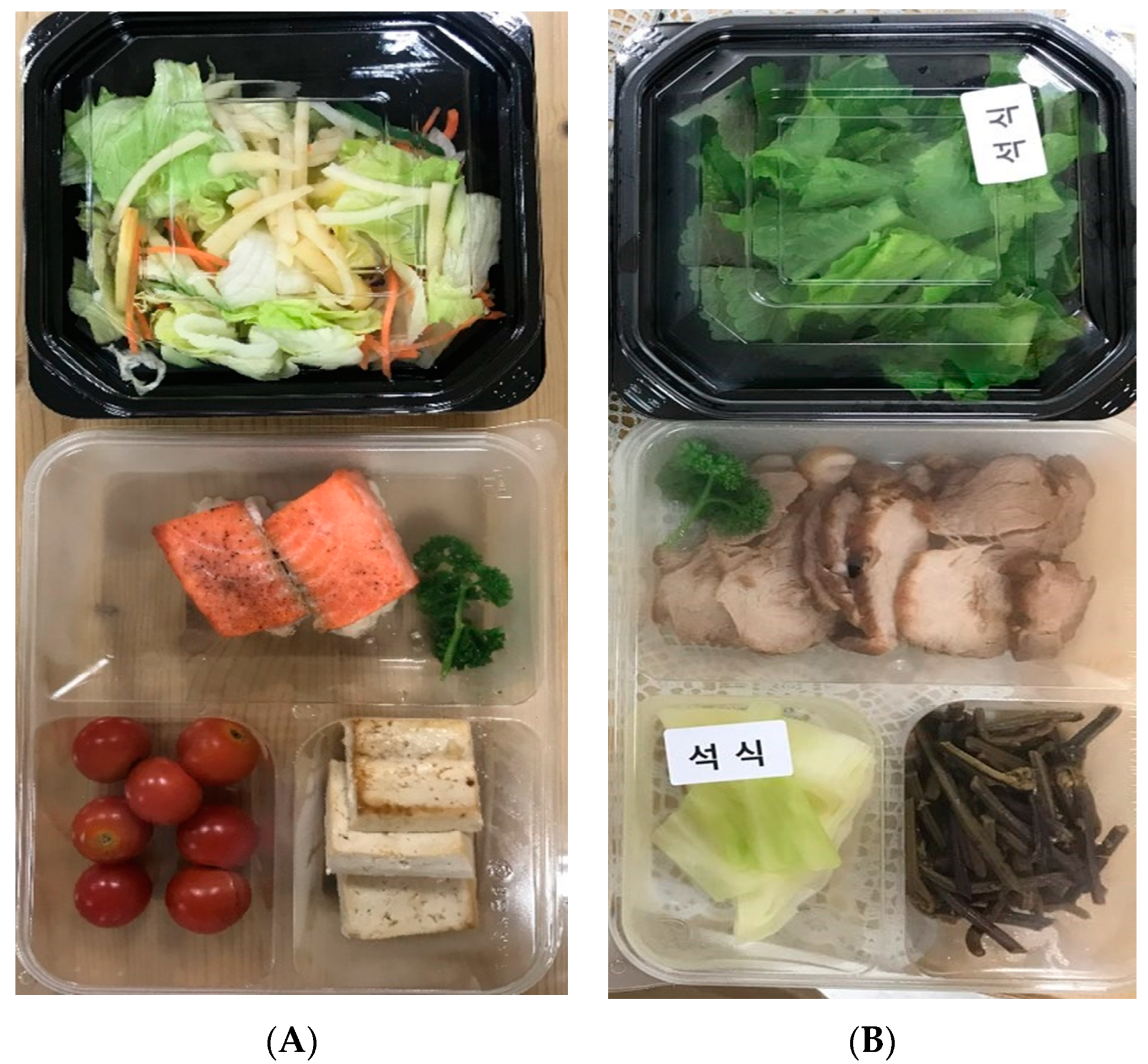
2.3. Diet
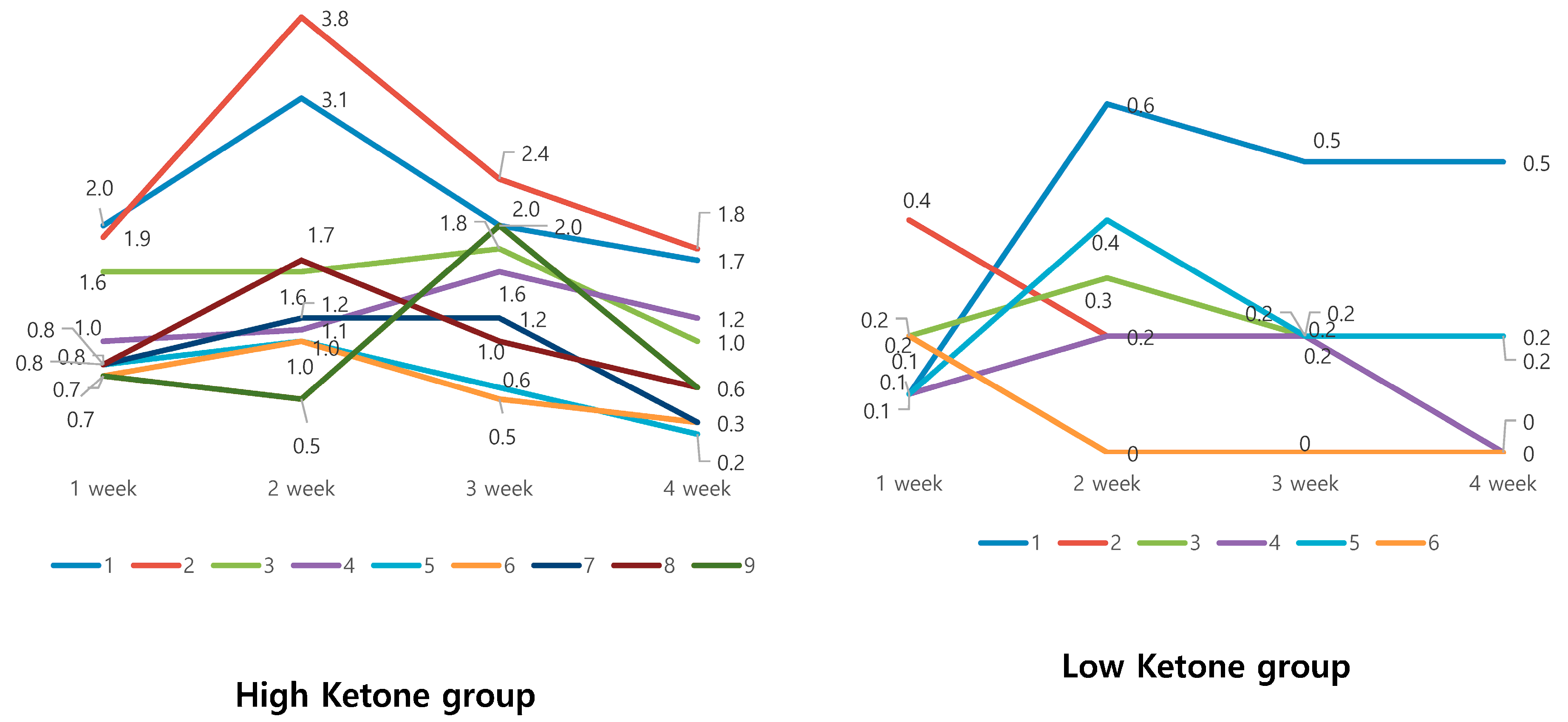
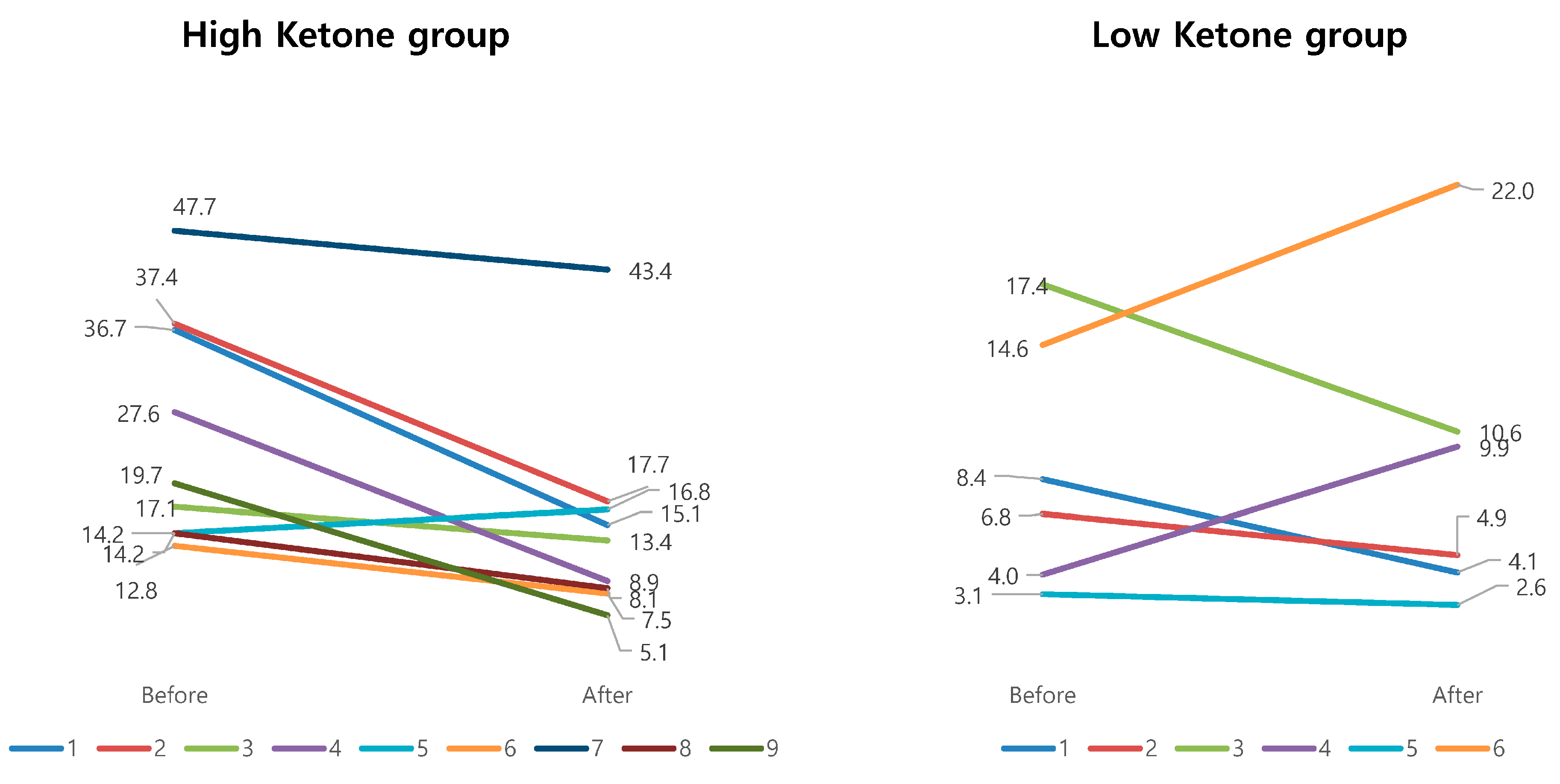
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Harvie, M.; Howell, A. Potential benefits and harms of intermittent energy restriction and intermittent fasting amongst obese, overweight and normal weight subjects—A narrative review of human and animal evidence. Behav. Sci. 2017, 7, 4. [Google Scholar] [CrossRef] [PubMed]
- Martel, J.; Ojcius, D.M.; Chang, C.J.; Lin, C.S.; Lu, C.C.; Ko, Y.F.; Tseng, S.F.; Lai, H.C.; Young, J.D. Anti-obesogenic and antidiabetic effects of plants and mushrooms. Nat. Rev. Endocrinol. 2017, 13, 149–160. [Google Scholar] [CrossRef] [PubMed]
- Ganesan, K.; Xu, B. Anti-obesity effects of medicinal and edible mushrooms. Molecules 2018, 23, 2880. [Google Scholar] [CrossRef] [PubMed]
- Kundakovic, T.; Kolundzic, M. Therapeutic properties of mushrooms in managing adverse effects in the metabolic syndrome. Curr. Topics Med. Chem. 2013, 13, 2734–2744. [Google Scholar] [CrossRef] [PubMed]
- Gill, S.; Panda, S. A smartphone app reveals erratic diurnal eating patterns in humans that can be modulated for health benefits. Cell Metab. 2015, 22, 789–798. [Google Scholar] [CrossRef] [PubMed]
- Wilkinson, M.J.; Manoogian, E.N.; Zadourian, A.; Lo, H.; Fakhouri, S.; Shoghi, A.; Wang, X.; Fleischer, J.G.; Navlakha, S.; Panda, S.; et al. Ten-hour time-restricted eating reduces weight, blood pressure, and atherogenic lipids in patients with metabolic syndrome. Cell Metab. 2020, 31, 92–104. [Google Scholar] [CrossRef] [PubMed]
- Williams, K.V.; Mullen, M.L.; Kelley, D.E.; Wing, R.R. The effect of short periods of caloric restriction on weight loss and glycemic control in type 2 diabetes. Diabetes Care 1998, 21, 2–8. [Google Scholar] [CrossRef] [PubMed]
- Almeneessier, A.S.; Pandi-Perumal, S.R.; BaHammam, A.S. Intermittent fasting, insufficient sleep, and circadian rhythm: Interaction and effects on the cardiometabolic system. Curr. Sleep Med. Rep. 2018, 4, 179–195. [Google Scholar] [CrossRef]
- Hatori, M.; Vollmers, C.; Zarrinpar, A.; DiTacchio, L.; Bushong, E.A.; Gill, S.; Leblanc, M.; Chaix, A.; Joens, M.; Fitzpatrick, J.A.; et al. Time-restricted feeding without reducing caloric intake prevents metabolic diseases in mice fed a high-fat diet. Cell Metab. 2012, 15, 848–860. [Google Scholar] [CrossRef] [PubMed]
- Chaix, A.; Zarrinpar, A.; Miu, P.; Panda, S. Time-restricted feeding is a preventative and therapeutic intervention against diverse nutritional challenges. Cell Metab. 2014, 20, 991–1005. [Google Scholar] [CrossRef] [PubMed]
- Gill, S.; Le, H.D.; Melkani, G.C.; Panda, S. Time-restricted feeding attenuates age-related cardiac decline in Drosophila. Science 2015, 347, 1265–1269. [Google Scholar] [CrossRef] [PubMed]
- Kudo, T.; Akiyama, M.; Kuriyama, K.; Sudo, M.; Moriya, T.; Shibata, S. Night-time restricted feeding normalises clock genes and Pai-1 gene expression in the db/db mouse liver. Diabetologia 2004, 47, 1425–1436. [Google Scholar] [CrossRef] [PubMed]
- Manoogian, E.N.; Panda, S. Circadian rhythms, time-restricted feeding, and healthy aging. Ageing Res. Rev. 2017, 39, 59–67. [Google Scholar] [CrossRef] [PubMed]
- Melkani, G.C.; Panda, S. Time-restricted feeding for prevention and treatment of cardiometabolic disorders. J. Physiol. 2017, 595, 3691–3700. [Google Scholar] [CrossRef] [PubMed]
- Roky, R.; Chapotot, F.; Hakkou, F.; Benchekroun, M.T.; Buguet, A. Sleep during Ramadan intermittent fasting. J. Sleep Res. 2001, 10, 319–327. [Google Scholar] [CrossRef] [PubMed]
- Aalling, N.N.; Nedergaard, M.; DiNuzzo, M. Cerebral metabolic changes during sleep. Curr. Neurol. Neurosci. Rep. 2018, 189, 57. [Google Scholar] [CrossRef] [PubMed]
- Sachiko, C.; Noriyuki, S.; Tetsuya, S.; Hiroyoshi, S. Ketone body metabolism and sleep homeostasis in mice. Neuropharmacology 2014, 79, 399–404. [Google Scholar]
| Nutrition Composition (g) | % kcal | |||||
|---|---|---|---|---|---|---|
| Carbohydrate | Protein | Fat | Carbohydrate | Protein | Fat | |
| 1, 2 weeks | 26.8 | 88.5 | 90.1 | 8 | 28 | 64 |
| 3 weeks | 32.5 | 90.6 | 97.6 | 9 | 26 | 65 |
| 4 weeks | 65.4 | 85.2 | 90.0 | 18 | 24 | 58 |
| Before Program | After Program | p | |
|---|---|---|---|
| Body weight (kg) | 82.0 ± 15.6 | 78.2 ± 14.1 | 0.539 |
| Body Mass Index (kg/m2) | 29.3 ± 4.6 | 27.9 ± 3.8 | 0.233 |
| Body fat mass (kg) | 29.5 ± 8.7 | 26.1 ± 7.6 | 0.285 |
| Body muscle mass (kg) | 29.4 ± 7.1 | 29.0 ± 6.8 | 0.870 |
| Low Ketone Group (n = 6) | High Ketone Group (n = 9) | p | |||
|---|---|---|---|---|---|
| Before | After | Before | After | ||
| Body weight (kg) | 75.23 ± 75.14 | 73.90 ± 14.66 | 86.43 ± 15.03 | 81.13 ± 13.71 | 0.006 |
| Body Mass Index (kg/m2) | 27.33 ± 1.64 | 26.93 ± 1.90 | 30.61 ± 5.56 | 28.62 ± 4.71 | 0.008 |
| Body fat mass (kg) | 28.40 ± 2.42 | 27.22 ± 2.71 | 30.20 ± 11.23 | 25.42 ± 9.69 | 0.007 |
| Body muscle mass (kg) | 25.83 ± 8.70 | 25.65 ± 8.06 | 31.76 ± 4.98 | 31.29 ± 5.03 | 0.522 |
| Low Ketone Group (n = 6) | High Ketone Group (n = 9) | p | |||
|---|---|---|---|---|---|
| Before | After | Before | After | ||
| AST | 20.50 ± 3.45 | 23.00 ± 6.23 | 31.11 ± 16.10 | 31.89 ± 19.19 | 0.600 |
| ALT | 19.83 ± 9.41 | 20.17 ± 7.22 | 62.33 ± 75.22 | 45.33 ± 47.42 | 0.192 |
| BUN | 11.55 ± 3.16 | 12.50 ± 4.61 | 14.74 ± 2.88 | 14.27 ± 2.79 | 0.521 |
| Creatine | 0.56 ± 0.10 | 0.58 ± 0.11 | 0.76 ± 0.15 | 0.83 ± 0.16 | 0.223 |
| γ-GTP | 35.00 ± 13.60 | 24.00 ± 10.77 | 42.67 ± 34.44 | 19.89 ± 13.60 | 0.257 |
| ALP | 69.17 ± 20.17 | 70.17 ± 15.68 | 63.78 ± 15.68 | 66.22 ± 18.55 | 0.803 |
| Total Cholesterol | 173.33 ± 31.94 | 169.17 ± 21.10 | 186.22 ± 33.46 | 180.56 ± 45.36 | 0.910 |
| LDL Cholesterol | 105.00 ± 24.23 | 99.67 ± 16.08 | 116.89 ± 25.30 | 110.44 ± 32.01 | 0.909 |
| TG | 119.50 ± 55.39 | 129.33 ± 73.55 | 153.67 ± 67.54 | 172.89 ± 231.20 | 0.934 |
| Glucose | 95.67 ± 29.04 | 104.33 ± 5.99 | 115.56 ± 45.12 | 96.33 ± 8.03 | 0.175 |
| Insulin | 8.70 ± 1.72 | 8.08 ± 1.31 | 15.37 ± 5.53 | 8.14 ± 5.53 | 0.006 |
| HOMA IR | 2.27 ± 0.58 | 2.09 ± 0.42 | 4.79 ± 3.98 | 2.00 ± 1.49 | 0.052 |
| Low Ketone Group (n = 6) | High Ketone Group (n = 9) | p | |||
|---|---|---|---|---|---|
| Variables | Before | After | Before | After | |
| PSQI-K 1 | 8.00 ± 3.46 | 6.50 ± 1.22 | 7.11 ± 2.37 | 5.11 ± 0.78 | 0.759 |
| STOP BANG | 2.50 ± 1.64 | 2.50 ± 1.64 | 3.00 ± 1.00 | 3.00 ± 1.00 | - |
| SSS 2 | 2.17 ± 0.98 | 2.83 ± 1.17 | 2.56 ± 0.23 | 2.67 ± 0.50 | 0.256 |
| ESS 3 | 9.00 ± 3.46 | 10.00 ± 2.19 | 9.11 ± 4.59 | 8.89 ± 4.91 | 0.465 |
| HADS 4 Anxiety | 4.67 ± 2.34 | 6.33 ± 3.93 | 6.78 ± 2.54 | 6.44 ± 2.55 | 0.225 |
| HADS Depression | 3.33 ± 1.86 | 4.50 ± 1.38 | 4.67 ± 3.32 | 4.11 ± 2.37 | 0.082 |
| ISI 5 | 6.17 ± 3.87 | 5.00 ± 1.41 | 7.75 ± 1.83 | 5.38 ± 2.97 | 0.529 |
| Low Ketone Group (n = 6) | High Ketone Group (n = 9) | p | |||
|---|---|---|---|---|---|
| Before | After | Before | After | ||
| Total Sleep Time (min) | 425.53 ± 37.96 | 415.32 ± 97.12 | 428.39 ± 51.76 | 442.87 ± 42.44 | 0.547 |
| Latency to sleep onset | 11.30 ± 3.91 | 27.02 ± 21.57 | 28.23 ± 34.01 | 27.61 ± 31.93 | 0.295 |
| Latency to REM onset | 90.03 ± 30.02 | 81.82 ± 52.77 | 148.90 ± 129.27 | 69.80 ± 61.56 | 0.220 |
| Sleep Efficiency (%) | 90.40 ± 7.57 | 89.17 ± 6.19 | 89.09 ± 8.99 | 86.50 ± 6.07 | 0.776 |
| Sleep stage N1 (%) | 1.80 ± 0.49 | 1.48 ± 0.33 | 3.49 ± 4.49 | 2.63 ± 1.26 | 0.775 |
| Sleep stage N2 (%) | 54.23 ± 8.97 | 52.83 ± 10.90 | 59.92 ± 13.38 | 55.50 ± 6.49 | 0.683 |
| Sleep stage N3 (%) | 19.73 ± 8.35 | 21.42 ± 5.80 | 15.51 ± 3.91 | 19.09 ± 8.67 | 0.699 |
| Sleep stage REM (%) | 24.25 ± 3.69 | 24.27 ± 5.65 | 21.10 ± 10.00 | 22.57 ± 5.41 | 0.745 |
| Wake After Sleep Onset | 45.40 ± 41.60 | 44.92 ± 35.97 | 51.56 ± 42.63 | 69.54 ± 41.63 | 0.472 |
| AHI | 9.05 ± 5.78 | 9.02 ± 7.13 | 25.27 ± 12.67 | 15.11 ± 11.50 | 0.025 |
| PLMSi | 4.78 ± 7.86 | 2.85 ± 5.28 | 30.90 ± 49.32 | 19.57 ± 44.70 | 0.752 |
| Oxygen desaturation index | 4.07 ± 3.02 | 5.87 ± 6.59 | 18.43 ± 12.79 | 10.69 ± 10.69 | 0.004 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, H.; Jang, B.J.; Jung, A.R.; Kim, J.; Ju, H.j.; Kim, Y.I. The Impact of Time-Restricted Diet on Sleep and Metabolism in Obese Volunteers. Medicina 2020, 56, 540. https://doi.org/10.3390/medicina56100540
Kim H, Jang BJ, Jung AR, Kim J, Ju Hj, Kim YI. The Impact of Time-Restricted Diet on Sleep and Metabolism in Obese Volunteers. Medicina. 2020; 56(10):540. https://doi.org/10.3390/medicina56100540
Chicago/Turabian StyleKim, Hyeyun, Bong Jin Jang, A Ram Jung, Jayoung Kim, Hyo jin Ju, and Yeong In Kim. 2020. "The Impact of Time-Restricted Diet on Sleep and Metabolism in Obese Volunteers" Medicina 56, no. 10: 540. https://doi.org/10.3390/medicina56100540
APA StyleKim, H., Jang, B. J., Jung, A. R., Kim, J., Ju, H. j., & Kim, Y. I. (2020). The Impact of Time-Restricted Diet on Sleep and Metabolism in Obese Volunteers. Medicina, 56(10), 540. https://doi.org/10.3390/medicina56100540






