Mesenchymal Stem/Stromal Cells for Rheumatoid Arthritis Treatment: An Update on Clinical Applications
Abstract
1. Introduction
2. Preclinical Studies
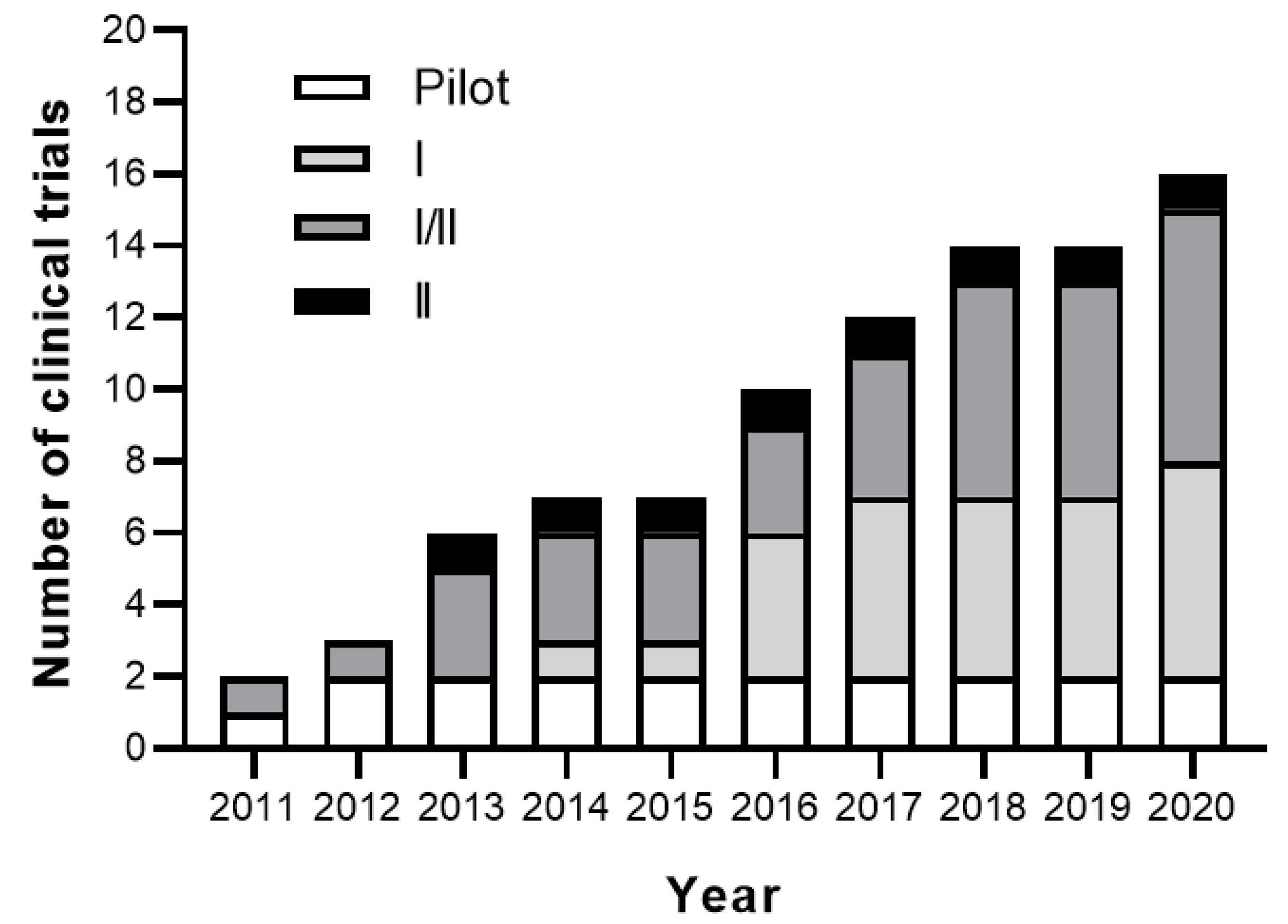
3. Clinical Studies
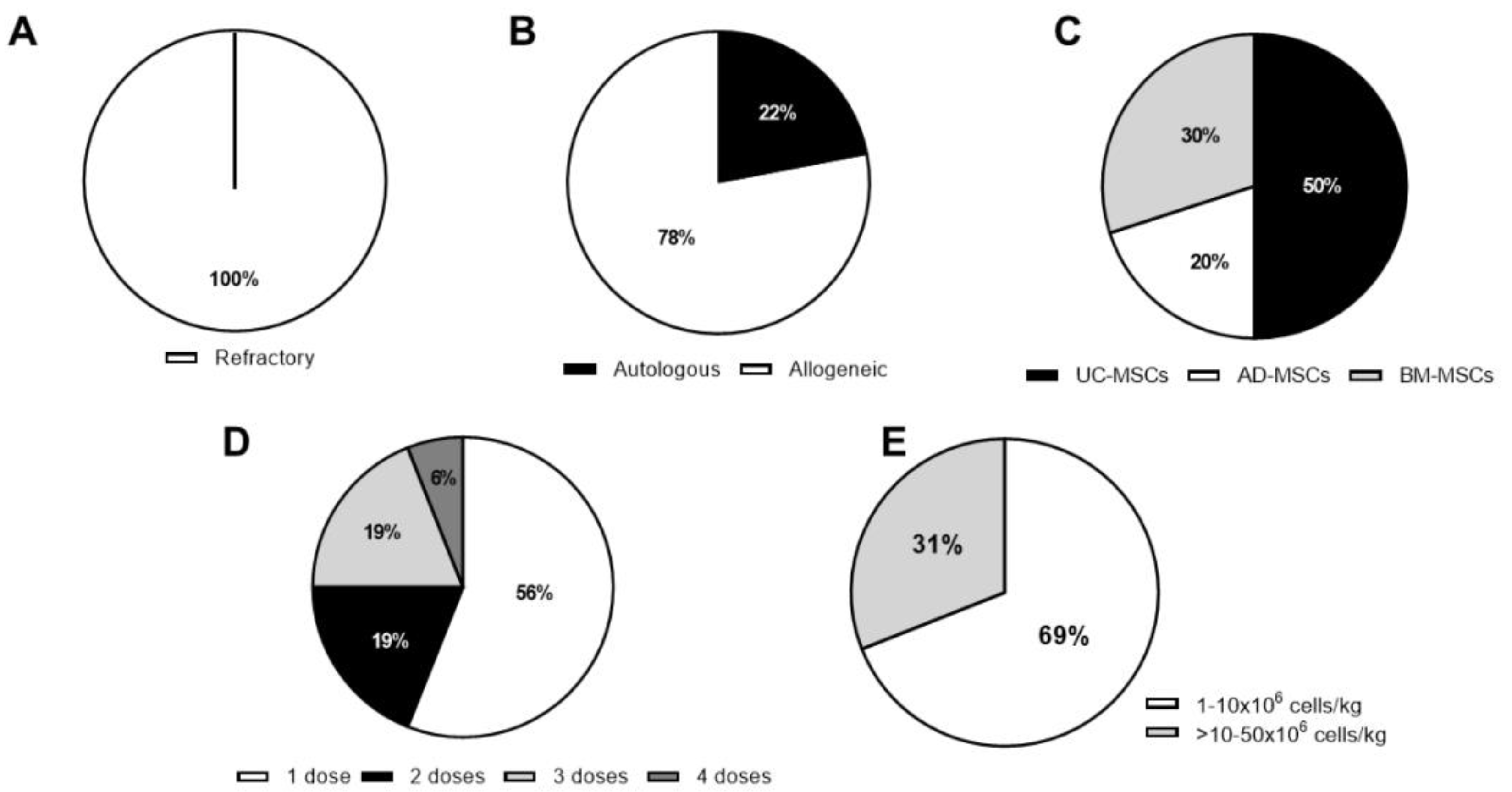
3.1. Completed Studies
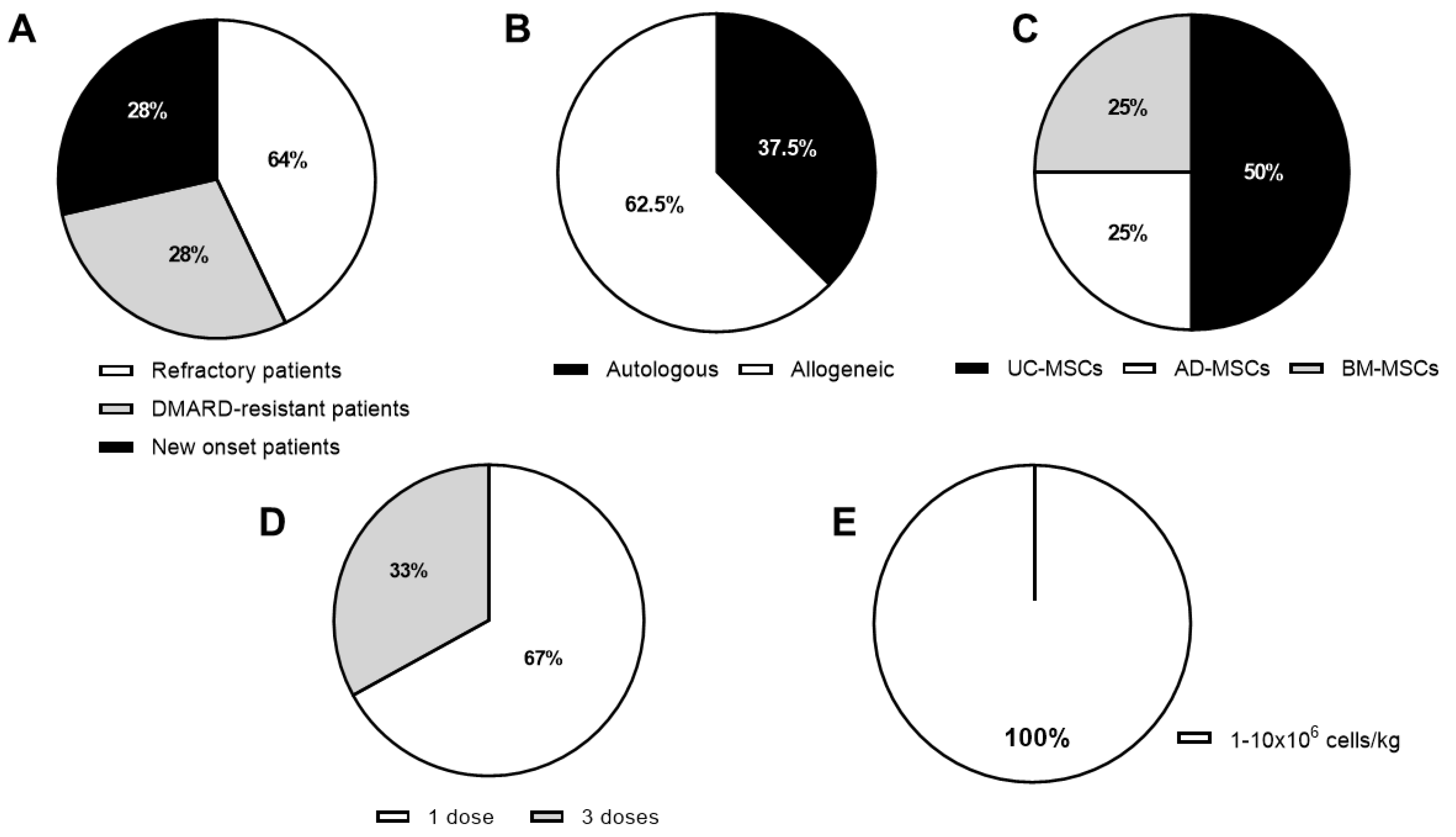
3.2. Active Clinical Trials
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| AD | Adipose tissue |
| ACR | American college of rheumatology improvement criteria |
| APRIL | A proliferation-inducing ligand |
| BAFF | B-cell activating factor |
| BCMA | B-cell maturation antigen |
| BM | Bone marrow |
| BR3 | B cell activation factor receptor 3 |
| CAT | Computer-adaptive testing |
| anti-CCP | antibodies against cyclic citrullinated peptide |
| CDAI | Clinical disease activity index |
| CIA | Collagen-induced arthritis |
| CRP | C reactive protein |
| CXCR3 | Chemokine receptor 3-alternative |
| DAS | Disease activity score |
| DMARDs | Disease-modifying antirheumatic drugs |
| ESR | Erythrocyte sedimentation rate |
| EULAR | European league against rheumatism |
| eASCs | expanded adipose-derived stem cells |
| HAQ | Health assessment questionnaire |
| HLA | Human leukocyte antigen |
| IA | Intra-articular |
| IL | Interleukin |
| IP | Intraperitoneal |
| IP10 | IFN-γ-induced protein 10 |
| IV | Intravenous |
| KHAQ | Korean health assessment questionnaire |
| MCP-1 | Monocyte chemoattractant protein 1 |
| MIP | Macrophage inflammatory protein 1 |
| MHC | Major histocompatibility complex |
| MPCs | Multipotent progenitor cells |
| MSCs | Mesenchymal stromal/stem cells |
| NSAIDs | Non-steroidal anti-inflammatory drugs |
| PGA | Patient global assessment |
| RA | Rheumatoid arthritis |
| RANKL | Receptor activator of nuclear factor kappa-Β ligand |
| RAPID3 | Routine assessment of patient index data 3 |
| RANTES | Regulated on activation, normal T cell expressed and secreted |
| RF | Rheumatoid factor |
| SDAI | Simplex disease activity index |
| TACI | Transmembrane activator and CAML interactor |
| TGF-β 1 | Transforming growth factor β 1 |
| Tregs | Regulatory T cells |
| UC-MSCs | MSCs from umbilical cord |
| VAS | Visual analogue scale |
| WOMAC | Western Ontario and McMaster universities osteoarthritis index |
References
- Firestein, G.S.; McInnes, I. Immunopathogenesis of Rheumatoid Arthritis. Immunity 2017, 46, 183–196. [Google Scholar] [CrossRef] [PubMed]
- Smolen, J.S.; Aletaha, D.; McInnes, I. Rheumatoid arthritis. Lancet 2016, 388, 2023–2038. [Google Scholar] [CrossRef]
- McInnes, I.; Schett, G. The Pathogenesis of Rheumatoid Arthritis. N. Engl. J. Med. 2011, 365, 2205–2219. [Google Scholar] [CrossRef] [PubMed]
- Singh, J.A.; Saag, K.G.; Bridges, S.L.; Akl, E.A.; Bannuru, R.R.; Sullivan, M.; Vaysbrot, E.; McNaughton, C.; Osani, M.; Shmerling, R.H.; et al. 2015 American College of Rheumatology Guideline for the Treatment of Rheumatoid Arthritis. Arthritis Rheumatol. 2015, 68, 1–26. [Google Scholar] [CrossRef] [PubMed]
- Smolen, J.S.; Landewé, R.; Breedveld, F.C.; Dougados, M.; Emery, P.; Gaujoux-Viala, C.; Gorter, S.; Knevel, R.; Nam, J.; Schoels, M.; et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs. Ann. Rheum. Dis. 2010, 69, 964–975. [Google Scholar] [CrossRef] [PubMed]
- Owen, M.; Friedenstein, A.J. Stromal Stem Cells: Marrow-Derived Osteogenic Precursors. Novartis Found. Symp. 2007, 42–60. [Google Scholar] [CrossRef]
- Spaggiari, G.M.; Capobianco, A.; Abdelrazik, H.; Becchetti, F.; Mingari, M.C.; Moretta, L. Mesenchymal stem cells inhibit natural killer–cell proliferation, cytotoxicity, and cytokine production: Role of indoleamine 2,3-dioxygenase and prostaglandin E2. Blood 2008, 111, 1327–1333. [Google Scholar] [CrossRef]
- Nasef, A.; Chapel, A.; Mazurier, C.; Bouchet, S.; Lopez, M.; Mathieu, N.; Sensebé, L.; Zhang, Y.; Gorin, N.-C.; Thierry, D.; et al. Identification of IL-10 and TGF-β Transcripts Involved in the Inhibition of T-Lymphocyte Proliferation During Cell Contact With Human Mesenchymal Stem Cells. Gene Expr. 2006, 13, 217–226. [Google Scholar] [CrossRef]
- Ungerer, C.; Quade-Lyssy, P.; Radeke, H.; Henschler, R.; Königs, C.; Koehl, U.; Seifried, E.; Schüttrumpf, J. Galectin-9 Is a Suppressor of T and B Cells and Predicts the Immune Modulatory Potential of Mesenchymal Stromal Cell Preparations. Stem Cells Dev. 2013, 23, 755–766. [Google Scholar] [CrossRef]
- Gieseke, F.; Böhringer, J.; Bussolari, R.; Dominici, M.; Handgretinger, R.; Mueller, I. Human multipotent mesenchymal stromal cells use galectin-1 to inhibit immune effector cells. Blood 2010, 116, 3770–3779. [Google Scholar] [CrossRef]
- Sioud, M.; Mobergslien, A.; Boudabous, A.; Fløisand, Y. Evidence for the Involvement of Galectin-3 in Mesenchymal Stem Cell Suppression of Allogeneic T-Cell Proliferation. Scand. J. Immunol. 2010, 71, 267–274. [Google Scholar] [CrossRef] [PubMed]
- Nasef, A.; Mazurier, C.; Bouchet, S.; François, S.; Chapel, A.; Thierry, D.; Gorin, N.-C.; Fouillard, L.; Chapel, A. Leukemia inhibitory factor: Role in human mesenchymal stem cells mediated immunosuppression. Cell. Immunol. 2008, 253, 16–22. [Google Scholar] [CrossRef] [PubMed]
- Selmani, Z.; Naji, A.; Zidi, I.; Favier, B.; Gaiffe, E.; Obert, L.; Borg, C.; Saas, P.; Tiberghien, P.; Rouas-Freiss, N.; et al. Human Leukocyte Antigen-G5 Secretion by Human Mesenchymal Stem Cells Is Required to Suppress T Lymphocyte and Natural Killer Function and to Induce CD4+CD25highFOXP3+Regulatory T Cells. Stem Cells 2008, 26, 212–222. [Google Scholar] [CrossRef]
- Chabannes, D.; Hill, M.; Merieau, E.; Rossignol, J.; Brion, R.; Soulillou, J.P.; Anegon, I.; Cuturi, M.C. A role for heme oxygenase-1 in the immunosuppressive effect of adult rat and human mesenchymal stem cells. Blood 2007, 110, 3691–3694. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Hematti, P. Mesenchymal stem cell–educated macrophages: A novel type of alternatively activated macrophages. Exp. Hematol. 2009, 37, 1445–1453. [Google Scholar] [CrossRef]
- Melief, S.M.; Schrama, E.; Brugman, M.H.; Tiemessen, M.M.; Hoogduijn, M.J.; Fibbe, W.E.; Roelofs, H. Multipotent stromal cells induce human regulatory T cells through a novel pathway involving skewing of monocytes toward anti-inflammatory macrophages. Stem Cells 2013, 31, 1980–1991. [Google Scholar] [CrossRef]
- López-Santalla, M.; Menta, R.; Mancheño-Corvo, P.; Lopez-Belmonte, J.; Delarosa, O.; Bueren, J.A.; Dalemans, W.; Lombardo, E.; Garín, M. Adipose-derived mesenchymal stromal cells modulate experimental autoimmune arthritis by inducing an early regulatory innate cell signature. Immun. Inflamm. Dis. 2016, 4, 213–224. [Google Scholar] [CrossRef]
- Lopez-Santalla, M.; Hervas-Salcedo, R.; Fernandez-Garcia, M.; Bueren, J.A.; Garín, M. Cell Therapy With Mesenchymal Stem Cells Induces an Innate Immune Memory Response That Attenuates Experimental Colitis in the Long Term. J. Crohns Coliti 2020. [Google Scholar] [CrossRef]
- Zhang, B.; Liu, R.; Shi, D.; Liu, X.; Chen, Y.; Dou, X.; Zhu, X.; Lu, C.; Liang, W.; Liao, L.; et al. Mesenchymal stem cells induce mature dendritic cells into a novel Jagged-2–dependent regulatory dendritic cell population. Blood 2009, 113, 46–57. [Google Scholar] [CrossRef]
- Zhou, C.; Wu, X.-R.; Liu, H.-S.; Liu, X.-H.; Liu, G.-H.; Zheng, X.-B.; Hu, T.; Liang, Z.-X.; He, X.-W.; Wu, X.-J.; et al. Immunomodulatory Effect of Urine-derived Stem Cells on Inflammatory Bowel Diseases via Downregulating Th1/Th17 Immune Responses in a PGE2-dependent Manner. J. Crohns Coliti 2019, 14, 654–668. [Google Scholar] [CrossRef]
- López-Santalla, M.; Mancheño-Corvo, P.; Menta, R.; Lopez-Belmonte, J.; Delarosa, O.; Bueren, J.A.; Dalemans, W.; Lombardo, E.; Garín, M. Human Adipose-Derived Mesenchymal Stem Cells Modulate Experimental Autoimmune Arthritis by Modifying Early Adaptive T Cell Responses. Stem Cells 2015, 33, 3493–3503. [Google Scholar] [CrossRef] [PubMed]
- Kabat, M.; Bobkov, I.; Kumar, S.; Grumet, M. Trends in mesenchymal stem cell clinical trials 2004–2018: Is efficacy optimal in a narrow dose range? Stem Cells Transl. Med. 2019, 9, 17–27. [Google Scholar] [CrossRef] [PubMed]
- Le Blanc, K.; Rasmusson, I.; Sundberg, B.; Götherström, C.; Hassan, M.; Uzunel, M.; Ringdén, O. Treatment of severe acute graft-versus-host disease with third party haploidentical mesenchymal stem cells. Lancet 2004, 363, 1439–1441. [Google Scholar] [CrossRef]
- Introna, M.; Rambaldi, A. Mesenchymal stromal cells for prevention and treatment of graft-versus-host disease. Curr. Opin. Organ Transplant. 2015, 20, 72–78. [Google Scholar] [CrossRef] [PubMed]
- Dothel, G.; Raschi, E.; Rimondini, R.; De Ponti, F. Mesenchymal stromal cell-based therapy: Regulatory and translational aspects in gastroenterology. World J. Gastroenterol. 2016, 22, 9057–9068. [Google Scholar] [CrossRef]
- Zhou, Y.; Zhang, X.; Xue, H.; Liu, L.; Zhu, J.; Jin, T. Autologous Mesenchymal Stem Cell Transplantation in Multiple Sclerosis: A Meta-Analysis. Stem Cells Int. 2019, 2019, 1–11. [Google Scholar] [CrossRef]
- Wang, D.; Zhang, H.; Liang, J.; Li, X.; Feng, X.; Wang, H.; Hua, B.; Liu, B.; Lu, L.; Gilkeson, G.S.; et al. Allogeneic Mesenchymal Stem Cell Transplantation in Severe and Refractory Systemic Lupus Erythematosus: 4 Years of Experience. Cell Transplant. 2013, 22, 2267–2277. [Google Scholar] [CrossRef]
- Liang, J.; Zhang, H.; Hua, B.; Wang, H.; Lu, L.; Shi, S.; Hou, Y.; Zeng, X.; Gilkeson, G.S.; Sun, L. Allogenic mesenchymal stem cells transplantation in refractory systemic lupus erythematosus: A pilot clinical study. Ann. Rheum. Dis. 2010, 69, 1423–1429. [Google Scholar] [CrossRef]
- Cai, J.; Wu, Z.; Xu, X.; Liao, L.; Chen, J.; Huang, L.; Wu, W.; Luo, F.; Wu, C.; Pugliese, A.; et al. Umbilical Cord Mesenchymal Stromal Cell With Autologous Bone Marrow Cell Transplantation in Established Type 1 Diabetes: A Pilot Randomized Controlled Open-Label Clinical Study to Assess Safety and Impact on Insulin Secretion. Diabetes Care 2015, 39, 149–157. [Google Scholar] [CrossRef]
- Carlsson, P.-O.; Schwarcz, E.; Korsgren, O.; Le Blanc, K. Preserved β-Cell Function in Type 1 Diabetes by Mesenchymal Stromal Cells. Diabetes 2014, 64, 587–592. [Google Scholar] [CrossRef]
- Hu, J.; Yu, X.; Wang, Z.; Wang, F.; Wang, L.; Gao, H.; Chen, Y.; Zhao, W.; Jia, Z.; Yan, S.; et al. Long term effects of the implantation of Wharton′s jelly-derived mesenchymal stem cells from the umbilical cord for newly-onset type 1 diabetes mellitus. Endocr. J. 2013, 60, 347–357. [Google Scholar] [CrossRef] [PubMed]
- Sood, V.; Bhansali, A.; Mittal, B.R.; Singh, B.; Marwaha, N.; Jain, A.; Khandelwal, N. Autologous bone marrow derived stem cell therapy in patients with type 2 diabetes mellitus - defining adequate administration methods. World J. Diabetes 2017, 8, 381–389. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Wang, D.; Liu, D.; Fan, Z.; Zhang, H.; Liu, O.; Ding, G.; Gao, R.; Zhang, C.; Ding, Y.; et al. Allogeneic mesenchymal stem cell treatment alleviates experimental and clinical Sjögren syndrome. Blood 2012, 120, 3142–3151. [Google Scholar] [CrossRef] [PubMed]
- Li, A.; Tao, Y.; Kong, D.; Zhang, N.; Wang, Y.; Wang, Z.; Wang, Y.; Wang, J.; Xiao, J.; Jiang, Y.; et al. Infusion of umbilical cord mesenchymal stem cells alleviates symptoms of ankylosing spondylitis. Exp. Ther. Med. 2017, 14, 1538–1546. [Google Scholar] [CrossRef] [PubMed]
- Ra, J.C.; Kang, S.K.; Shin, I.S.; Park, H.G.; Joo, S.A.; Kim, J.G.; Kang, B.-C.; Lee, Y.S.; Nakama, K.; Piao, M.; et al. Stem cell treatment for patients with autoimmune disease by systemic infusion of culture-expanded autologous adipose tissue derived mesenchymal stem cells. J. Transl. Med. 2011, 9, 181. [Google Scholar] [CrossRef]
- Liang, J.; Li, X.; Zhang, H.; Wang, D.; Feng, X.; Wang, H.; Hua, B.; Liu, B.; Sun, L. Allogeneic mesenchymal stem cells transplantation in patients with refractory RA. Clin. Rheumatol. 2011, 31, 157–161. [Google Scholar] [CrossRef]
- Wang, L.; Wang, L.; Cong, X.; Liu, G.; Zhou, J.; Bai, B.; Li, Y.; Bai, W.; Li, M.; Ji, H.; et al. Human Umbilical Cord Mesenchymal Stem Cell Therapy for Patients with Active Rheumatoid Arthritis: Safety and Efficacy. Stem Cells Dev. 2013, 22, 3192–3202. [Google Scholar] [CrossRef]
- Kafaja, S.; Segal, K.; Skerrett, D.; Itescu, S.; Furst, D. FRI0220 Allogeneic mesenchymal precursor cells (MPCS): A novel approach to treating biologic refractory rheumatoid arthritis. Ann. Rheum. Dis. 2017, 76, 566–567. [Google Scholar] [CrossRef]
- Álvaro-Gracia, J.M.; Jover, J.A.; Garcia-Vicuna, R.; Carreño, L.; Alonso, A.; Marsal, S.; Blanco, F.; Martínez-Taboada, V.M.; Taylor, P.; Martín-Martín, C.; et al. Intravenous administration of expanded allogeneic adipose-derived mesenchymal stem cells in refractory rheumatoid arthritis (Cx611): Results of a multicentre, dose escalation, randomised, single-blind, placebo-controlled phase Ib/IIa clinical trial. Ann. Rheum. Dis. 2016, 76, 196–202. [Google Scholar] [CrossRef]
- Yang, Y.; He, X.; Zhao, R.-S.; Guo, W.; Zhu, M.; Xing, W.; Jiang, D.; Liu, C.-Y.; Xu, X. Serum IFN-γ levels predict the therapeutic effect of mesenchymal stem cell transplantation in active rheumatoid arthritis. J. Transl. Med. 2018, 16, 165. [Google Scholar] [CrossRef]
- Park, E.H.; Lim, H.-S.; Lee, S.; Roh, K.; Seo, K.-W.; Kang, K.-S.; Shin, K. Intravenous Infusion of Umbilical Cord Blood-Derived Mesenchymal Stem Cells in Rheumatoid Arthritis: A Phase Ia Clinical Trial. Stem Cells Transl. Med. 2018, 7, 636–642. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Huang, S.; Li, S.; Li, M.; Shi, J.; Bai, W.; Wang, Q.; Zheng, L.; Liu, Y. Efficacy and Safety of Umbilical Cord Mesenchymal Stem Cell Therapy for Rheumatoid Arthritis Patients: A Prospective Phase I/II Study. Drug Des. Dev. Ther. 2019, 13, 4331–4340. [Google Scholar] [CrossRef] [PubMed]
- Ghoryani, M.; Shariati-Sarabi, Z.; Tavakkol-Afshari, J.; Ghasemi, A.; Poursamimi, J.; Mohammadi, M. Amelioration of clinical symptoms of patients with refractory rheumatoid arthritis following treatment with autologous bone marrow-derived mesenchymal stem cells: A successful clinical trial in Iran. Biomed. Pharmacother. 2019, 109, 1834–1840. [Google Scholar] [CrossRef] [PubMed]
- Fang, B.; Song, Y.; Li, N.; Li, J.; Han, Q.; Zhao, R. Resolution of Refractory Chronic Autoimmune Thrombocytopenic Purpura Following Mesenchymal Stem Cell Transplantation: A Case Report. Transplant. Proc. 2009, 41, 1827–1830. [Google Scholar] [CrossRef]
- Lechanteur, C.; Briquet, A.; Giet, O.; Delloye, O.; Baudoux, E.; Beguin, Y. Clinical-scale expansion of mesenchymal stromal cells: A large banking experience. J. Transl. Med. 2016, 14, 145. [Google Scholar] [CrossRef]
- Hynes, K.; Bright, R.; Proudman, S.; Haynes, D.; Gronthos, S.; Bartold, M.; Bartold, P.M. Immunomodulatory properties of mesenchymal stem cell in experimental arthritis in rat and mouse models: A systematic review. Semin. Arthritis Rheum. 2016, 46, 1–19. [Google Scholar] [CrossRef]
- Liu, L.; Wong, C.W.; Han, M.; Farhoodi, H.P.; Liu, G.; Liu, Y.; Liao, W.; Zhao, W. Meta-analysis of preclinical studies of mesenchymal stromal cells to treat rheumatoid arthritis. EBioMedicine 2019, 47, 563–577. [Google Scholar] [CrossRef]
- Mennan, C.; Brown, S.J.; McCarthy, H.S.; Mavrogonatou, E.; Kletsas, D.; Garcia, J.; Balain, B.; Richardson, J.; Roberts, S. Mesenchymal stromal cells derived from whole human umbilical cord exhibit similar properties to those derived from Wharton’s jelly and bone marrow. FEBS Open Bio. 2016, 6, 1054–1066. [Google Scholar] [CrossRef]
- Valencia, J.; Blanco, B.; Yañez, R.M.; Vázquez, M.; Sánchez, C.H.; Garcia, M.N.V.; Serrano, C.R.; Pescador, D.; Blanco, J.F.; Hernando-Rodriguez, M.; et al. Comparative analysis of the immunomodulatory capacities of human bone marrow– and adipose tissue–derived mesenchymal stromal cells from the same donor. Cytotherapy 2016, 18, 1297–1311. [Google Scholar] [CrossRef]
- Mattar, P.; Bieback, K. Comparing the Immunomodulatory Properties of Bone Marrow, Adipose Tissue, and Birth-Associated Tissue Mesenchymal Stromal Cells. Front. Immunol. 2015, 6, 1418. [Google Scholar] [CrossRef]
- Zhang, Q.; Li, Q.; Zhu, J.; Guo, H.; Zhai, Q.; Li, B.; Jin, Y.; He, X.; Jin, F. Comparison of therapeutic effects of different mesenchymal stem cells on rheumatoid arthritis in mice. PeerJ 2019, 7, e7023. [Google Scholar] [CrossRef] [PubMed]
- Gu, Y.; Shi, S. Transplantation of gingiva-derived mesenchymal stem cells ameliorates collagen-induced arthritis. Arthritis Res. 2016, 18, 1–9. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Chen, M.; Su, W.-R.; Lin, X.; Guo, Z.; Wang, J.; Zhang, Q.; Brand, D.D.; Ryffel, B.; Huang, J.; Liu, Z.; et al. Adoptive Transfer of Human Gingiva-Derived Mesenchymal Stem Cells Ameliorates Collagen-Induced Arthritis via Suppression of Th1 and Th17 Cells and Enhancement of Regulatory T Cell Differentiation. Arthritis Rheum. 2013, 65, 1181–1193. [Google Scholar] [CrossRef] [PubMed]
- Shu, J.; Pan, L.; Huang, X.; Wang, P.; Li, H.; He, X.; Cai, Z. Transplantation of human amnion mesenchymal cells attenuates the disease development in rats with collagen-induced arthritis. Clin. Exp. Rheumatol. 2015, 33. [Google Scholar]
- Parolini, O.; Souza-Moreira, L.; O’Valle, F.; Magatti, M.; Hernandez-Cortes, P.; Gonzalez-Rey, E.; Delgado, M. Therapeutic Effect of Human Amniotic Membrane-Derived Cells on Experimental Arthritis and Other Inflammatory Disorders. Arthritis Rheumatol. 2014, 66, 327–339. [Google Scholar] [CrossRef]
- Cargnoni, A.; Gibelli, L.; Tosini, A.; Signoroni, P.B.; Nassuato, C.; Arienti, D.; Lombardi, G.; Albertini, A.; Wengler, G.S.; Parolini, O. Transplantation of Allogeneic and Xenogeneic Placenta-Derived Cells Reduces Bleomycin-Induced Lung Fibrosis. Cell Transplant. 2009, 18, 405–422. [Google Scholar] [CrossRef]
- Lee, W.J.; Hah, Y.-S.; Ock, S.-A.; Lee, J.-H.; Jeon, R.-H.; Park, J.-S.; Lee, S.-I.; Rho, N.-Y.; Rho, G.-J.; Lee, S.-L. Cell source-dependent in vivo immunosuppressive properties of mesenchymal stem cells derived from the bone marrow and synovial fluid of minipigs. Exp. Cell Res. 2015, 333, 273–288. [Google Scholar] [CrossRef]
- Rui, K.; Zhang, Z.; Tian, J.; Lin, X.; Wang, X.; Ma, J.; Tang, X.; Xu, H.; Lu, L.; Wang, S. Olfactory ecto-mesenchymal stem cells possess immunoregulatory function and suppress autoimmune arthritis. Cell. Mol. Immunol. 2015, 13, 401–408. [Google Scholar] [CrossRef]
- Tian, J.; Rui, K.; Tang, X.; Wang, W.; Ma, J.; Tian, X.; Wang, Y.; Xu, H.; Lu, L.; Wang, S. IL-17 down-regulates the immunosuppressive capacity of olfactory ecto-mesenchymal stem cells in murine collagen-induced arthritis. Oncotarget 2016, 7, 42953–42962. [Google Scholar] [CrossRef]
- Dominici, M.; Le Blanc, K.; Mueller, I.; Slaper-Cortenbach, I.; Marini, F.; Krause, D.; Deans, R.; Keating, A.; Prockop, D.; Horwitz, E. Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy 2006, 8, 315–317. [Google Scholar] [CrossRef]
- Mancheño-Corvo, P.; López-Santalla, M.; Menta, R.; Delarosa, O.; Mulero, F.; Del Rio, B.; Ramirez, C.; Büscher, D.; Bueren, J.A.; Lopez-Belmonte, J.; et al. Intralymphatic Administration of Adipose Mesenchymal Stem Cells Reduces the Severity of Collagen-Induced Experimental Arthritis. Front. Immunol. 2017, 8. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, M.A.; Gonzalez-Rey, E.; Rico, L.; Büscher, D.; Delgado, M. Treatment of experimental arthritis by inducing immune tolerance with human adipose-derived mesenchymal stem cells. Arthritis Rheum. 2009, 60, 1006–1019. [Google Scholar] [CrossRef] [PubMed]
- Greish, S.; Abogresha, N.; Abdel-Hady, Z.; Zakaria, E.; Ghaly, M.; Hefny, M. Human umbilical cord mesenchymal stem cells as treatment of adjuvant rheumatoid arthritis in a rat model. World J. Stem Cells 2012, 4, 101–109. [Google Scholar] [CrossRef] [PubMed]
- Kehoe, O.; Cartwright, A.; Askari, A.; El Haj, A.; Middleton, J. Intra-articular injection of mesenchymal stem cells leads to reduced inflammation and cartilage damage in murine antigen-induced arthritis. J. Transl. Med. 2014, 12, 157. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Ding, J.; Li, C.; Wang, C.; Wang, Y.; Wang, J.; Chang, F. Hydrogel is Superior to Fibrin Gel as Matrix of Stem Cells in Alleviating Antigen-Induced Arthritis. Polymers 2016, 8, 182. [Google Scholar] [CrossRef]
- Kay, A.G.; Long, G.; Tyler, G.; Stefan, A.; Broadfoot, S.J.; Piccinini, A.M.; Middleton, J.; Kehoe, O. Mesenchymal Stem Cell-Conditioned Medium Reduces Disease Severity and Immune Responses in Inflammatory Arthritis. Sci. Rep. 2017, 7, 18019. [Google Scholar] [CrossRef]
- Zhang, X.; Yamaoka, K.; Sonomoto, K.; Kaneko, H.; Satake, M.; Yamamoto, Y.; Kondo, M.; Zhao, J.; Miyagawa, I.; Yamagata, K.; et al. Local Delivery of Mesenchymal Stem Cells with Poly-Lactic-Co-Glycolic Acid Nano-Fiber Scaffold Suppress Arthritis in Rats. PLoS ONE 2014, 9, e114621. [Google Scholar] [CrossRef][Green Version]
- Djouad, F.; Fritz, V.; Apparailly, F.; Bony, C.; Sany, J.; Jorgensen, C.; Noel, D.; Louis-Plence, P. Reversal of the immunosuppressive properties of mesenchymal stem cells by tumor necrosis factor α in collagen-induced arthritis. Arthritis Rheum. 2005, 52, 1595–1603. [Google Scholar] [CrossRef]
- Hu, J.; Li, H.; Chi, G.; Yang, Z.; Zhao, Y.; Liu, W.; Zhang, C. IL-1RA gene-transfected bone marrow-derived mesenchymal stem cells in APA microcapsules could alleviate rheumatoid arthritis. Int. J. Clin. Exp. Med. 2015, 8, 706–713. [Google Scholar]
- Swart, J.F.; De Roock, S.; Hofhuis, F.M.; Rozemuller, H.; Broek, T.V.D.; Moerer, P.; Broere, F.; Van Wijk, F.; Kuis, W.; Prakken, B.; et al. Mesenchymal stem cell therapy in proteoglycan induced arthritis. Ann. Rheum. Dis. 2014, 74, 769–777. [Google Scholar] [CrossRef]
- Lopez-Santalla, M.; Mancheño-Corvo, P.; Escolano, A.; Menta, R.; Delarosa, O.; Abad, J.L.; Büscher, D.; Redondo, J.M.; Bueren, J.A.; Dalemans, W.; et al. Biodistribution and Efficacy of Human Adipose-Derived Mesenchymal Stem Cells Following Intranodal Administration in Experimental Colitis. Front. Immunol. 2017, 8. [Google Scholar] [CrossRef] [PubMed]
- López-Santalla, M.; Mancheno-Corvo, P.; Escolano, A.; Menta, R.; Delarosa, O.; Redondo, J.M.; Bueren, J.A.; Dalemans, W.; Lombardo, E.; Garín, M. Comparative Analysis between the In Vivo Biodistribution and Therapeutic Efficacy of Adipose-Derived Mesenchymal Stromal Cells Administered Intraperitoneally in Experimental Colitis. Int. J. Mol. Sci. 2018, 19, 1853. [Google Scholar] [CrossRef] [PubMed]
- Augello, A.; Tasso, R.; Negrini, S.; Cancedda, R.; Pennesi, G. Cell therapy using allogeneic bone marrow mesenchymal stem cells prevents tissue damage in collagen-induced arthritis. Arthritis Rheum. 2007, 56, 1175–1186. [Google Scholar] [CrossRef] [PubMed]
- Papadopoulou, A.; Yiangou, M.; Athanasiou, E.; Zogas, N.; Kaloyannidis, P.; Batsis, I.; Fassas, A.; Anagnostopoulos, A.; Yannaki, E. Mesenchymal stem cells are conditionally therapeutic in preclinical models of rheumatoid arthritis. Ann. Rheum. Dis. 2012, 71, 1733–1740. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.-H.; Lee, Y.T.; Oh, K.; Cho, J.; Lee, D.-S.; Hwang, Y.-I. Paradoxical effects of human adipose tissue-derived mesenchymal stem cells on progression of experimental arthritis in SKG mice. Cell. Immunol. 2014, 292, 94–101. [Google Scholar] [CrossRef] [PubMed]
- Zhou, B.; Yuan, J.; Zhou, Y.; Ghawji, M.; Deng, Y.-P.; Lee, A.J.; Lee, A.J.; Nair, U.; Kang, A.H.; Brand, D.D.; et al. Administering human adipose-derived mesenchymal stem cells to prevent and treat experimental arthritis. Clin. Immunol. 2011, 141, 328–337. [Google Scholar] [CrossRef]
- Mao, F.; Xu, W.; Qian, H.; Zhu, W.; Yan, Y.; Shao, Q.-X.; Xu, H.-X. Immunosuppressive effects of mesenchymal stem cells in collagen-induced mouse arthritis. Inflamm. Res. 2009, 59, 219–225. [Google Scholar] [CrossRef]
- Choi, E.W.; Shin, I.S.; Song, J.W.; Lee, M.; Yun, T.W.; Yang, J.; Choi, K.-S.; Kim, S.-J. Effects of Transplantation of CTLA4Ig-Overexpressing Adipose Tissue-Derived Mesenchymal Stem Cells in Mice with Sustained Severe Rheumatoid Arthritis. Cell Transplant. 2016, 25, 243–259. [Google Scholar] [CrossRef]
- Gao, J.; Zhang, G.; Xu, K.; Ma, D.; Ren, L.; Fan, J.; Hou, J.; Han, J.; Zhang, L. Bone marrow mesenchymal stem cells improve bone erosion in collagen-induced arthritis by inhibiting osteoclasia-related factors and differentiating into chondrocytes. Stem Cell Res. Ther. 2020, 11, 1–14. [Google Scholar] [CrossRef]
- Luz-Crawford, P.; Tejedor, G.; Beaulieu, E.; Jorgensen, C.; Noel, D.; Djouad, F.; Mausset-Bonnefont, A.; Morand, E.F. Glucocorticoid-Induced Leucine Zipper Governs the Therapeutic Potential of Mesenchymal Stem Cells by Inducing a Switch From Pathogenic to Regulatory Th17 Cells in a Mouse Model of Collagen-Induced Arthritis. Arthritis Rheumatol. 2015, 67, 1514–1524. [Google Scholar] [CrossRef]
- Cosenza, S.; Toupet, K.; Maumus, M.; Luz-Crawford, P.; Blanc-Brude, O.; Jorgensen, C.; Noël, D. Mesenchymal stem cells-derived exosomes are more immunosuppressive than microparticles in inflammatory arthritis. Theranostics 2018, 8, 1399–1410. [Google Scholar] [CrossRef] [PubMed]
- Varkouhi, A.K.; Monteiro, A.P.T.; Tsoporis, J.N.; Mei, S.H.J.; Stewart, D.J.; Dos Santos, C.C. Genetically Modified Mesenchymal Stromal/Stem Cells: Application in Critical Illness. Stem Cell Rev. Rep. 2020, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Park, N.; Rim, Y.A.; Jung, H.; Kim, J.; Yi, H.; Kim, Y.; Jang, Y.; Jung, S.M.; Lee, J.; Kwok, S.-K.; et al. Etanercept-Synthesising Mesenchymal Stem Cells Efficiently Ameliorate Collagen-Induced Arthritis. Sci. Rep. 2017, 7, 39593. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.N.; Wang, G.; Hendricks, K.; Lee, K.; Bohnlein, E.; Junker, U.; Mosca, J.D. Comparison of Drug and Cell-Based Delivery: Engineered Adult Mesenchymal Stem Cells Expressing Soluble Tumor Necrosis Factor Receptor II Prevent Arthritis in Mouse and Rat Animal Models. Stem Cells Transl. Med. 2013, 2, 362–375. [Google Scholar] [CrossRef] [PubMed]
- Alvaro-Gracia, J.M.; Jover, J.A.; Garcia-Vicuña, R.; Carreño, L.; Alonso, A.; Marsal, S.; Blanco, F.J.; Martínez-Taboada, V.M.; Taylor, P.C.; Díaz-González, F.; et al. Phase IB/IIA study on intravenous administration of expanded allogeneic adipose-derived mesenchymal stem cells in refractory rheumatoid arthritis patients. Proceeding of 2013 ACR/ARHP Annual Meeting, San Diego, CA, USA, 25–30 October 2013. Abstract Number 2644. [Google Scholar]
- He, X.; Yang, Y.; Yao, M.; Yang, L.; Ao, L.; Hu, X.; Li, Z.; Wu, X.; Tan, Y.; Xing, W.; et al. Combination of human umbilical cord mesenchymal stem (stromal) cell transplantation with IFN-γ treatment synergistically improves the clinical outcomes of patients with rheumatoid arthritis. Ann. Rheum. Dis. 2020. [Google Scholar] [CrossRef]
- Ghoryani, M.; Shariati-Sarabi, Z.; Tavakkol-Afshari, J.; Mohammadi, M. The Sufficient Immunoregulatory Effect of Autologous Bone Marrow-Derived Mesenchymal Stem Cell Transplantation on Regulatory T Cells in Patients with Refractory Rheumatoid Arthritis. J. Immunol. Res. 2020, 2020, 1–8. [Google Scholar] [CrossRef]
- Shabgah, A.G.; Shariati-Sarabi, Z.; Tavakkol-Afshari, J.; Ghasemi, A.; Ghoryani, M.; Mohammadi, M. A significant decrease of BAFF, APRIL, and BAFF receptors following mesenchymal stem cell transplantation in patients with refractory rheumatoid arthritis. Gene 2020, 732, 144336. [Google Scholar] [CrossRef]
- Shabgah, A.G.; Shariati-Sarabi, Z.; Tavakkol-Afshari, J.; Ghoryani, M.; Mohammadi, M. Possible anti-inflammatory effects of mesenchymal stem cells transplantation via changes in CXCL8 levels in patients with refractory rheumatoid arthritis. Int. J. Mol. Cell. Med. 2019, 8, 191–199. [Google Scholar] [CrossRef]
- Gronthos, S.; Zannettino, A.C.; Hay, S.J.; Shi, S.; Graves, S.; Kortesidis, A.; Simmons, P.J. Molecular and cellular characterisation of highly purified stromal stem cells derived from human bone marrow. J. Cell Sci. 2003, 116, 1827–1835. [Google Scholar] [CrossRef]
- Panés, J.; Garcia-Olmo, D.; Van Assche, G.; Colombel, J.F.; Reinisch, W.; Baumgart, D.C.; Dignass, A.; Nachury, M.; Ferrante, M.; Kazemi-Shirazi, L.; et al. Long-term Efficacy and Safety of Stem Cell Therapy (Cx601) for Complex Perianal Fistulas in Patients With Crohn’s Disease. Gastroenterology 2018, 154, 1334–1342. [Google Scholar] [CrossRef]
| Immune-Mediated Disorders | Number of Clinical Trials | Year of First Clinical Trial | References |
|---|---|---|---|
| Graft vs. host disease | 49 | 2004 | [24] |
| Inflammatory bowel disease | 23 | 2006 | [25] |
| Multiple sclerosis | 29 | 2006 | [26] |
| Systemic lupus erythematosus | 10 | 2007 | [27,28] |
| Type I diabetes | 26 | 2008 | [29,30,31] |
| Primary Sjögren syndrome | 1 | 2009 | [33] |
| Type II diabetes | 13 | 2010 | [32] |
| Autoimmune hepatitis | 2 | 2011 | NCT01661842 and NCT02997878 |
| Ankylosing spondylitis | 2 | 2011 | [34] |
| Chronic urticaria | 1 | 2017 | NCT02824393 |
| Refractory autoimmune thrombocytopenia | 1 | 2019 | NCT04014166 |
| Clinical Trial Identifier | Clinical Phase | Source | Registration Year | Country | RA Patients | MHC Context; Route of Administration | Cells/kg of Body Weight; Number of Doses and Route of Administration | Number of RA Patients Enrolled | Follow-Up (Months) | Publication (Year) | Included Control Group |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Unknown | Pilot | AD | 2011 | Korea | Refractory | Autologous; IV and IA | 3 × 108/patient; 2 doses 2 × 108/patient; 4 doses 2 × 108/patient; 1 dose IV + 1 × 108/patient; 1 dose IA 3.5 × 108/patient, 1 dose IV +1.5 × 108/patient; 1 dose IA | 4 out of the 10 patients enrolled | 12 | [35] | No |
| Unknown | Pilot | BM/UC | 2012 | China | Refractory | Allogeneic; IV | 1 × 106 1 dose | 4 | 19 | [36] | No |
| NCT01663116 | Ib/IIa | AD | 2011 | Spain | Refractory | Allogeneic; IV | 1, 2 or 4 × 106; 3 doses, weekly | 53 | 6 | [39] | Yes |
| NCT01547091 | I/II | UC | 2013 | China | Refractory | Allogeneic; IV | 4 × 107/patient; 1 dose | 172 | 36 | [37,42] | Yes |
| ChiCTR-ONC-16008770 | I | UC | 2016 | China | Refractory | Allogeneic; IV | 1 × 106; 1 dose | 53 | 12 | [40] | Yes |
| NCT03333681 | I | BM | 2016 | Iran | Refractory | Autologous; IV | 1 to 2 × 106; 1 dose | 15 | 12 | [43] | No |
| NCT02221258 | I | UC | 2014 | Korea | Refractory | Allogeneic; IV | 2.5, 5 or 10 × 107/patient; 1 dose | 9 | 1 | [41] | No |
| NCT01851070 | II | MPCs | 2013 | USA | Refractory | Allogeneic; IV | 1 or 2 × 106; 1 dose | 48 | 3 | [38] | Yes |
| ChiCTR-INR-17012462 | I/II | UC | 2017 | China | Refractory | Allogeneic; IV | 1 × 106; 1 dose | 63 | 3 | [86] | No |
| Clinical Trial Identifier | Clinical Phase | Source | Registration Year | Country | Status | RA Patients | MHC Context; Route of Administration | Cells/kg of Body Weight; Number of Doses | Estimated Number of RA Patients | Follow-Up (Months) | Included Control Group | Estimated Completion Date |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| NCT01985464 | I/II | UC | 2013 | Panama | Active, not recruiting | DMARD-resistant | Allogeneic; IV | Unknown | 20 | 12 | No | June 2020 |
| NCT03067870 | I | BM | 2016 | Jordan | Active, not recruiting | Unknown | Autologous, IV and IA | Unknown | 100 | 6 | No | February 2022 |
| NCT03798028 | N/A | UC | 2017 | China, | Recruiting | Anemia or pulmonary disease associated | Allogeneic; IV | 1 × 106; 1 dose | 250 | 6 | Yes | June 2020 |
| NCT03186417 | I | MPCs | 2017 | USA | Recruiting | During onset | Allogeneic; IV | 2, 4 or 6 × 106; 1 dose | 20 | 24 | Yes | December 2020 |
| NCT03618784 | I/II | UC | 2018 | Korea | Recruiting | Refractory | Allogeneic; IV | 5.0 or 10 × 107/patient; 3 doses | 33 | 4 | Yes | April 2021 |
| NCT03691909 | I/II | AD | 2018 | USA | Recruiting | Stable treatment | Autologous; IV | Unknown | 15 | 12 | No | June 2020 |
| NCT03828344 | I | UC | 2020 | USA | Active, not recruiting | Refractory | Allogeneic; IV | 0.75 or 1.5 × 106; 1 dose | 16 | 12 | Yes | September 2020 |
| NCT04170426 | I/IIa | AD | 2020 | USA | Active, not recruiting | DMARD-resistant | Autologous; IV | 2.0 or 2.86 × 106; 1 dose or 3 doses, every 3 days | 54 | 12 | Yes | December 2023 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lopez-Santalla, M.; Fernandez-Perez, R.; Garin, M.I. Mesenchymal Stem/Stromal Cells for Rheumatoid Arthritis Treatment: An Update on Clinical Applications. Cells 2020, 9, 1852. https://doi.org/10.3390/cells9081852
Lopez-Santalla M, Fernandez-Perez R, Garin MI. Mesenchymal Stem/Stromal Cells for Rheumatoid Arthritis Treatment: An Update on Clinical Applications. Cells. 2020; 9(8):1852. https://doi.org/10.3390/cells9081852
Chicago/Turabian StyleLopez-Santalla, Mercedes, Raquel Fernandez-Perez, and Marina I. Garin. 2020. "Mesenchymal Stem/Stromal Cells for Rheumatoid Arthritis Treatment: An Update on Clinical Applications" Cells 9, no. 8: 1852. https://doi.org/10.3390/cells9081852
APA StyleLopez-Santalla, M., Fernandez-Perez, R., & Garin, M. I. (2020). Mesenchymal Stem/Stromal Cells for Rheumatoid Arthritis Treatment: An Update on Clinical Applications. Cells, 9(8), 1852. https://doi.org/10.3390/cells9081852





