Anti-Inflammatory and Anticancer Properties of Bioactive Compounds from Sesamum indicum L.—A Review
Abstract
:1. Introduction
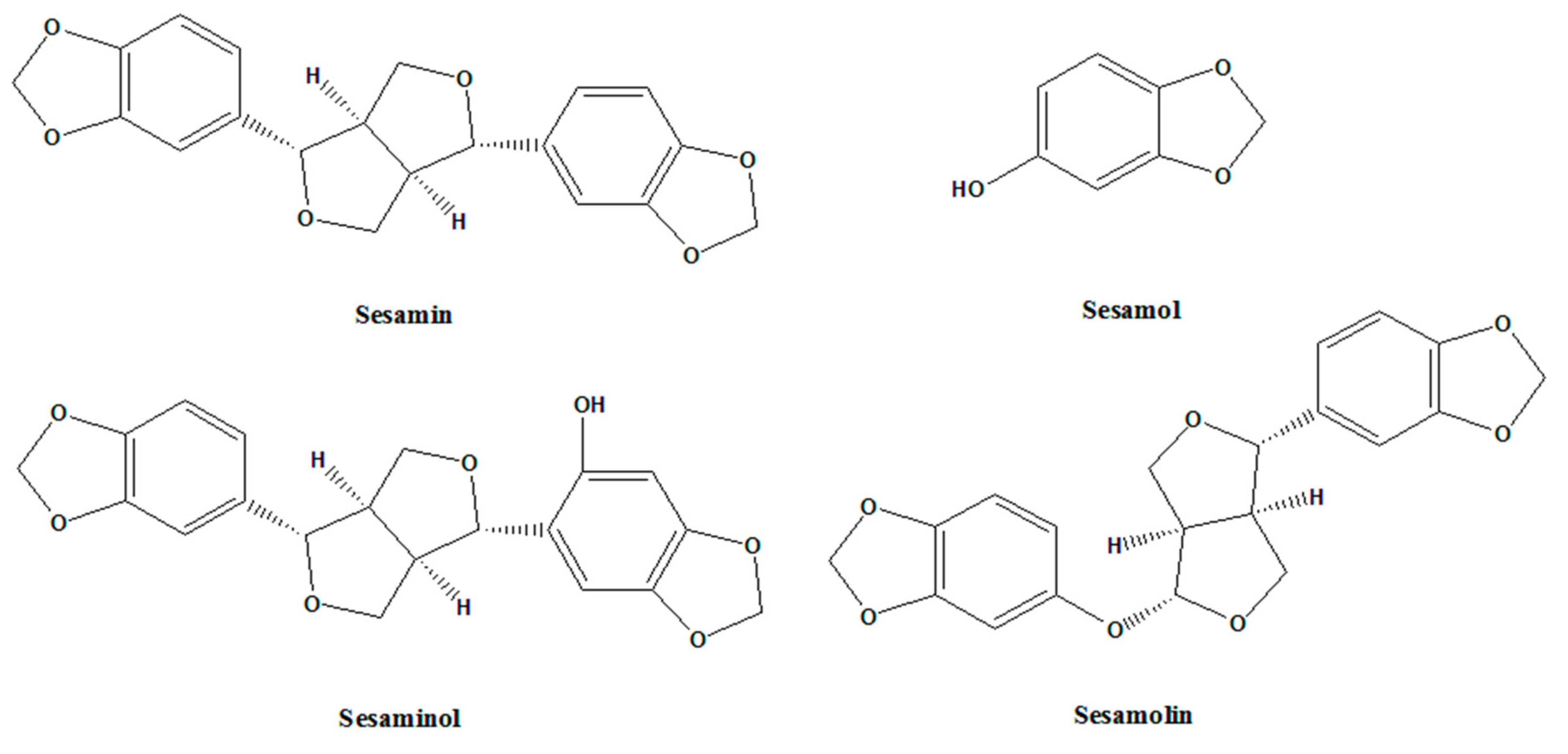
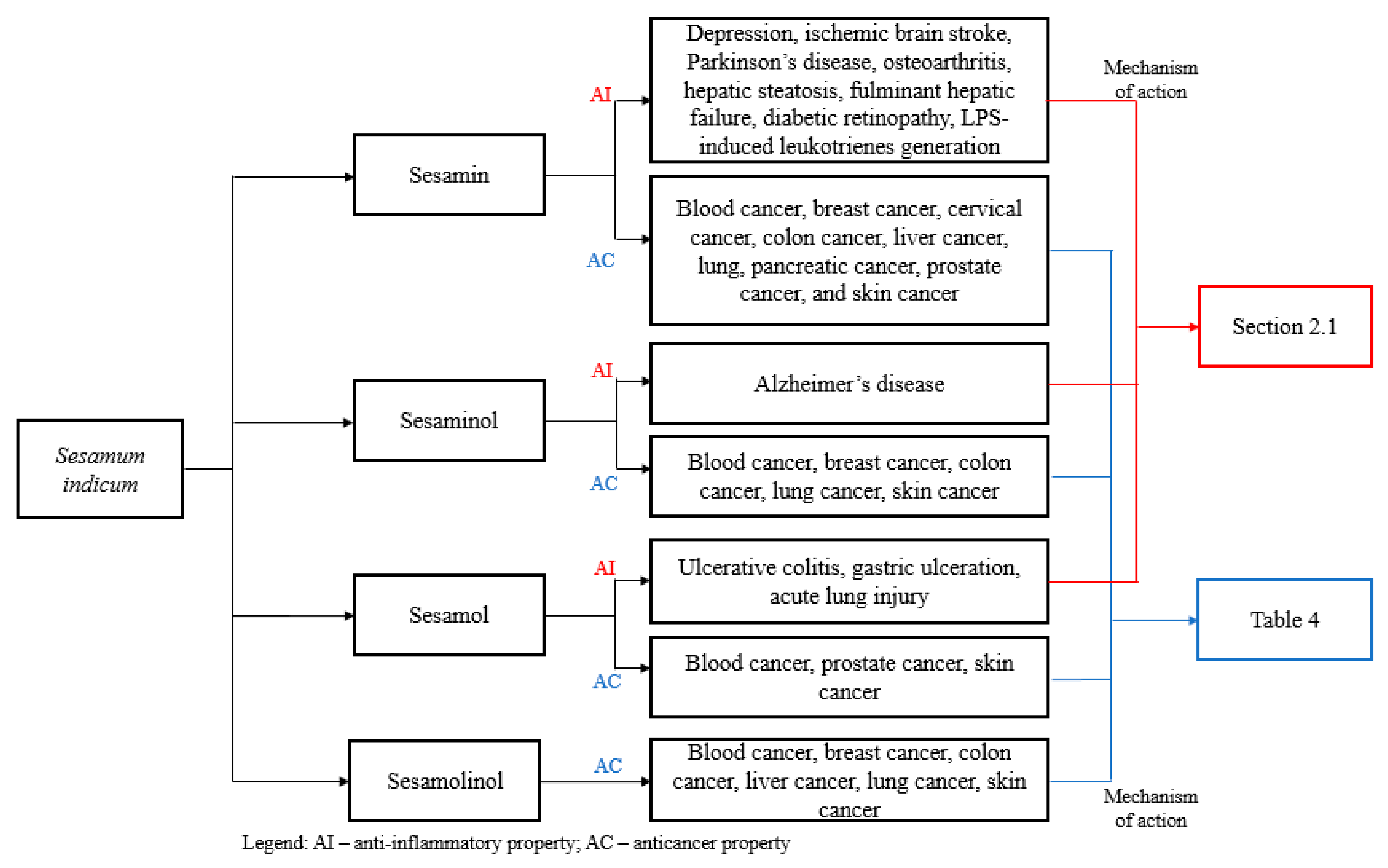
2. Pharmacological Applications of Sesame
2.1. Anti-Inflammatory Activity
2.1.1. Neurodegenerative Disease
2.1.2. Osteoarthritis
2.1.3. Liver Disease
2.1.4. Diabetic Eye Disease
2.1.5. Inflammatory Bowel Disease
2.1.6. Cardiovascular Disease
2.1.7. Lung Disease
| Compound | Inflammatory Disease/Disorder | Rat Model | References |
|---|---|---|---|
| Sesamin | Depression | Chronic unpredictable mild stress (CUMS) rat model | [41] |
| Ischemic brain stroke | Middle cerebral artery occlusion (MCAO) rat model | [42] | |
| Parkinson’s disease | 6-hydroxydopamine (6-OHDA) rat model | [43] | |
| Osteoarthritis | Papain-induced osteoarthritis rat model | [57] | |
| Hepatic steatosis | High-fat diet rat model | [65] | |
| Fulminant hepatic failure | d-galactosamine (d-GalN)-sensitized rat model | [66] | |
| Acute hepatic injury | Lead-induced acute hepatic injury rat model | [69] | |
| Diabetic Retinopathy | Streptozotocin (STZ) induced rat model | [87] | |
| LPS-induced leukotrienes generation | ad libitum semi-synthetic diet rat model | [110] | |
| Sesamol | Ulcerative colitis | Dinitrochlorobenzene (DNCB)—induced rat model | [88] |
| Gastric ulceration | Aspirin-induced gastric mucosal rat model | [92] | |
| Acute lung injury | Endotoxin-induced acute pulmonary inflammation rat model | [108] | |
| Sesaminol | Alzheimer’s disease | senescence-accelerated mouse-prone 8 (SAMP8) model | [50] |
| Sesame Oil | Nonalcoholic steatohepatitis | Methionine-choline deficient (MCD) diet rat model | [76] |
| Hepatic steatosis | High-fat diet-fed rat model | [83] | |
| Cardiac hypertrophy | Deoxycorticosterone/salt (DOCA/salt)-induced hypertension uninephrectomized rat model | [102] |
| Compound | Mechanism of Action | Cell Line | References |
|---|---|---|---|
| Sesamin | Inhibition of LPS-induced TLR4 expression | BV-2 microglial cell | [34] |
| Inhibition of LPS-induced IL-6 mRNA and protein | BV-2 microglial cell | [35] | |
| Inhibition of HO-1 protein ubiquitination | RAW 264.7 murine macrophage cells | [48] | |
| Activation of Nrf2/ARE | PC12 rat pheochromocytoma cells. | [49] | |
| Inhibition of IL-1β-stimulated human osteoarthritis chondrocytes. | Primary chondrocytes | [58] | |
| Inhibition of oxidized low-density lipoprotein (oxLDL)-induced endothelial dysfunction | Human umbilical vein endothelial cells (HUVECs) | [97] | |
| Episesamin and Sesamin metabolites | Activation of Nrf2/ARE | PC12 rat pheochromocytoma cells. | [49] |
| Sesamin Catechol Glucuronides | Inhibition of LPS-induced NO production | J774.1 mouse macrophage-like cells | [75] |
| Sesamol | Inhibition of MMPs expression | SW1353 human chondrosarcoma cells | [59] |
| Inhibition of inflammatory LOX | Soy LOX-1 enzyme model | [113] | |
| Sesaminol Triglucoside | Inhibition of IL-6 and TNF-α | RAW 264.7 murine macrophage cells | [93] |
| Sesamolin | Reduce the activation of p38 MAPK | BV-2 microglial cell | [35] |
2.1.8. Others
| Sesame Component | Mode of Extraction/Solvent | In vitro/In vivo | References |
|---|---|---|---|
| Sesame Oil | Aqueous extract | RAW 264.7 macrophage cell line | [114] |
| Black Sesame Seeds | Ethanol extract | Fructose-induced NAFLD rat model | [115] |
| Black Sesame Seeds | Ethanol extract | Freund’s complete adjuvant (FCA)-induced arthritis rat model | [116] |
| Black Sesame Seeds | CO2 supercritical fluid extraction | Endothelin-1-induced focal ischemia rat model | [117] |
| Sesame Coat | Ethanol extract | RAW 264.7 macrophage cell line | [118] |
2.2. Anti-Cancer Activity
2.2.1. Lung Cancer
2.2.2. Breast Cancer
2.2.3. Prostate Cancer
2.2.4. Colon Cancer
2.2.5. Liver Cancer
2.2.6. Cervical Cancer
2.2.7. Blood Cancer
2.2.8. Skin Cancer
2.2.9. Others
3. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Grougnet, R.; Magiatis, P.; Laborie, H.; Lazarou, D.; Papadopoulos, A.; Skaltsounis, A.-L. Sesamolinol Glucoside, Disaminyl Ether, and Other Lignans from Sesame Seeds. J. Agric. Food Chem. 2012, 60, 108–111. [Google Scholar] [CrossRef] [PubMed]
- Nagendra Prasad, M.N.; Sanjay, K.R.; Prasad, D.S.; Vijay, N.; Kothari, R.; Nanjunda Swamy, S. A Review on Nutritional and Nutraceutical Properties of Sesame. J. Nutr. Food Sci. 2012, 2, 1–6. [Google Scholar]
- Anilakumar, K.R.; Pal, A.; Khanum, F.; Bawa, A.S. Nutritional, Medicinal and Industrial Uses of Sesame (Sesame indicum L.) Seeds - A Overview. Agric. Conspec. Sci. 2010, 75, 159–168. [Google Scholar]
- Muta, N.; M, P.N. A review on sesame—An ethno medicinally significant oil crop. Int. J. Life Sci. Pharm. Res. 2017, 7, 58–63. [Google Scholar]
- Bedigian, D. History and lore of sesame in Southwest Asia. Econ. Bot. 2004, 58, 329–353. [Google Scholar] [CrossRef]
- Bedigian, D.; Harlan, J.R. Evidence for cultivation of sesame in the ancient world. Econ. Bot. 1986, 40, 137–154. [Google Scholar] [CrossRef]
- Khan, M.S.; Raj, S.K.; Snehi, S.K. First report of ‘Candidatus phytoplasma asteris’ affecting sesame cultivation in India. J. Plant Pathol. 2007, 89, 301–305. [Google Scholar]
- Saydut, A.; Duz, M.Z.; Kaya, C.; Kafadar, A.B.; Hamamci, C. Transesterified sesame (Sesamum indicum L.) seed oil as a biodiesel fuel. Bioresour. Technol. 2008, 99, 6656–6660. [Google Scholar] [CrossRef]
- Moazzami, A. Sesame seed lignas: diversity, human metabolism and bioactivities. Doctoral Thesis, Swedish University of Agricultural Sciences, Uppsala, Sweden, 2006. [Google Scholar]
- Pathak, N.; Rai, A.K.; Kumari, R.; Bhat, K.V. Value addition in sesame: A perspective on bioactive components for enhancing utility and profitability. Pharmacogn. Rev. 2014, 8, 147–155. [Google Scholar]
- Unnikrishnan, M.K.; Kumar, M.S.; Satyamoorthy, K.; Joshi, R. Free radical reactions and antioxidant activities of sesamol: Pulse radiolytic and biochemical studies. J. Agric. Food Chem. 2005, 53, 2696–2703. [Google Scholar]
- Juan, S.; Chen, S.; Qiuhui, H. Antioxidant activity of brown pigment and extracts from black sesame seed (Sesamum indicum L.). Food Chem. 2005, 91, 79–83. [Google Scholar]
- Osawa, T. Protective role of dietary polyphenols in oxidative stress. Mech. Age. Develop. 1999, 111, 133–139. [Google Scholar] [CrossRef]
- Yamashita, K.; Nohara, Y.; Katayama, K.; Namiki, M. Sesame Seed Lignans and γ-Tocopherol Act Synergistically to Produce Vitamin E Activity in Rats. J. Nutr. 1992, 122, 2440–2446. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morris, J.B. Food, industrial, nutraceutical, and pharmaceutical uses of sesame genetic resources. In Trends in New Crops And New Uses; ASHS Press: Alexandria, VA, USA, 2002; pp. 153–156. [Google Scholar]
- Simon, J.E.; Chadwick, A.F.; Craker, L.E. Herbs: An Indexed Bibliography, 1971–1980. The Scientific Literature on Selected Herbs, and Aromatic and Medicinal Plants of the Temperate Zone; Archon Books: Hamden, CT, USA, 1984. [Google Scholar]
- Beckstrom-Sternberg, S.M.; Duke, J.A.; Wain, K.K. The Ethnobotany Database. 1994. Available online: http://arsgenome.cornell.edu/cgibin/WebAce/webace?db=ethnobotdb.
- Nayar, N.M.; Mehra, K.L. Sesame: Its uses, botany, cytogenetics, and origin. Econ. Bot. 2002, 24, 20–31. [Google Scholar] [CrossRef]
- Shahidi, F.; Amarowi, R.; Abou-Gharbia, H.A.; Shehata, A.A.Y. Endogenous antioxidants and stability of sesame oil as affected by processing and storage. J. Am. Oil Chem. Soc. 1997, 74, 143–148. [Google Scholar] [CrossRef]
- Jamieson, G.S.; Baughman, W.F. The chemical composition of sesame oil. J. Am. Chem. Soc. 1924, 46, 775–778. [Google Scholar] [CrossRef]
- Ballakur, V. Inflammation in ayurveda and modern medicine. Int. Ayurvedic Med. J. 2013, 1, 1–7. [Google Scholar]
- Scott, A.; Khan, K.M.; Cook, J.L.; Duronio, V. What is “inflammation”? Are we ready to move beyond Celsus? Br. J. Sports Med. 2004, 38, 248–249. [Google Scholar] [CrossRef] [Green Version]
- Janeway, C.; Travers, P.; Walport, M.; Shlomchik, M. Inflammation. In Immunobiology; Garland Science: New York, NY, USA, 2001; pp. 41–43. [Google Scholar]
- Hsu, D.-Z.; Chu, P.-Y.; Liu, M.-Y. Sesame Seed (Sesamum indicum L.) Extracts and Their Anti-Inflammatory Effect. Emerg. Trends Diet. Compon. Prev. Combat. Dis. 2012, 1093, 335–341. [Google Scholar]
- Fullerton, J.N.; Gilroy, D.W. Resolution of inflammation: a new therapeutic frontier. Nat. Rev. Drug Dis. 2016, 15, 551. [Google Scholar] [CrossRef]
- Kumar, V.; Ahmad, A. Role of MAIT cells in the immunopathogenesis of inflammatory diseases: new players in old game. Int. Rev. Immunol. 2017, 37, 1–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kumar, V. Innate lymphoid cells: new paradigm in immunology of inflammation. Immunol. Lett. 2014, 157, 23–37. [Google Scholar] [CrossRef] [PubMed]
- Kumar, V.; Sharma, A. Neutrophils: Cinderella of innate immune system. Int. Immunopharmacol. 2010, 10, 1325–1334. [Google Scholar] [CrossRef] [PubMed]
- Kumar, V.; Sharma, A. Mast cells: emerging sentinel innate immune cells with diverse role in immunity. Mol. Immunol. 2010, 48, 14–25. [Google Scholar] [CrossRef]
- Kempuraj, D.; Thangavel, R.; Natteru, P.; Selvakumar, G.; Saeed, D.; Zahoor, H.; Zaheer, A. Neuroinflammation Induces Neurodegeneration. J. Neurol. Neurosurg. Spine 2017, 1, 1003. [Google Scholar]
- Chen, W.-W.; Zhang, X.; Huang, W.-J. Role of neuroinflammation in neurodegenerative diseases (Review). Mol. Med. Rep. 2016, 13, 3391–3396. [Google Scholar] [CrossRef] [Green Version]
- Akira, S.; Takeuchi, O. Pattern recognition receptors and inflammation. Cell 2010, 140, 805–820. [Google Scholar]
- Kacimi, R.; Giffard, R.; Yenari, M. Endotoxin-activated microglia injure brain derived endothelial cells via NF-kB, JAK-STAT and JNK stress kinase pathways. J. Inflamm. 2011, 8, 1–15. [Google Scholar] [CrossRef] [Green Version]
- Udomruk, S.; Kaewmool, C.; Pothacharoen, P.; Phitak, T.; Kongtawelert, P. Sesamin suppresses LPS-induced microglial activation via regulation of TLR4 expression. J. Funct. Foods 2018, 49, 32–43. [Google Scholar] [CrossRef]
- Jeng, K.-G.; Hou, R.C.W.; Wang, J.; Ping, L.-I. Sesamin inhibits lipopolysaccharide-induced cytokine production by suppression of p38 mitogen-activated protein kinase and nuclear factor-kB. Immunol. Lett. 2005, 97, 101–106. [Google Scholar] [CrossRef]
- Hamon, M.; Blier, P. Monoamine neurocircuitry in depression and strategies for new treatments. Prog. Neuropsychopharmacol. Biol. Psychiatry 2013, 45, 54–63. [Google Scholar] [CrossRef] [PubMed]
- Root, D.H.; Hoffman, A.F. Norepinephrine activates dopamine D4 receptors in the rat lateral habenula. J. Neurosci. 2015, 35, 3460–3469. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yan, T.; He, B.; Wan, S.; Xu, M.; Yang, H.; Xiao, F.; Bi, K.; Jia, Y. Antidepressant-like effects and cognitive enhancement of Schisandra chinensis in chronic unpredictable mild stress mice and its related mechanism. Sci. Rep. 2017, 7, 6903. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ohsawa, K.; Imai, Y.; Sasaki, Y.; Kohsaka, S. Microglia/macrophage-specific protein Iba1 binds to fimbrin and enhances its actin-bundling activity. J. Neurochem. 2004, 88, 844–856. [Google Scholar] [CrossRef] [PubMed]
- Farooq, R.K.; Isingrini, E.; Tanti, A.; Le Guisquet, A.M.; Arlicot, N.; Minier, F.; Leman, S.; Chalon, S.; Belzung, C.; Camus, V. Is unpredictable chronic mild stress (UCMS) a reliable model to study depression induced neuroinflammation? Behav. Brain Res. 2012, 231, 130–137. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Wang, Q.; Jia, M.; Fu, S.; Pan, J.; Chu, C.; Liu, X.; Liu, X.; Liu, Z. (+)-Sesamin attenuates chronic unpredictable mild stress-induced depressive-like behaviors and memory deficits via suppression of neuroinflammation. J. Nutr. Biochem. 2019, 64, 61–71. [Google Scholar] [CrossRef]
- Ahmad, S.; Elsherbiny, N.M.; Haque, R.; Khan, M.B.; Ishrat, T.; Shah, Z.A.; Khan, M.M.; Ali, M.; Jamal, A.; Katare, D.P.; et al. Sesamin attenuates neurotoxicity in mouse model of ischemic brain stroke. NeuroToxicology 2014, 45, 100–110. [Google Scholar] [CrossRef]
- Baluchnejadmojarad, T.; Mansouri, M.; Ghalami, J.; Mokhtari, Z.; Roghani, M. Sesamin imparts neuroprotection against intrastriatal 6-hydroxydopamine toxicity by inhibition of astroglial activation, apoptosis, and oxidative stress. Biomed. Pharmacol. 2017, 88, 754–761. [Google Scholar] [CrossRef]
- Hsieh, P.F.; Hou, C.-W.; Yao, P.-W.; Wu, S.-P.; Peng, Y.-F.; Shen, M.-L.; Lin, C.-H.; Chao, Y.-Y.; Chang, M.-H.; Jeng, K.-C. Sesamin ameliorates oxidative stress and mortality in kainic acid-induced status epilepticus by inhibition of MAPK and COX-2 activation. J. Neuroinflammation 2011, 8, 57. [Google Scholar] [CrossRef] [Green Version]
- Maines, M.D. The heme oxygenase system: a regulator of second messenger gases. Annu. Rev. Pharmacol. Toxicol. 1997, 37, 517–554. [Google Scholar] [CrossRef]
- Tenhunen, R.; Marver, H.S.; Schmid, R. The enzymatic conversion of heme to bilirubin by microsomal heme oxygenase. Proc. Natl. Acad. Sci. USA 1968, 61, 748–755. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kirkby, K.A.; Adin, C.A. Products of heme oxygenase and their potential therapeutic applications. Am. J. Physiol. Renal. Physiol. 2006, 290, F563–F571. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fukunaga, M.; Ohnishi, M.; Shiratsuchi, A.; Kawakami, T.; Takahashi, M.; Motomura, M.; Egusa, K.; Urasaki, T.; Inoue, A. Sesamin increases heme oxygenase-1 protein in RAW 264.7 macrophages through inhibiting its ubiquitination process. Euro. J. Pharmacol. 2014, 741, 214–221. [Google Scholar] [CrossRef] [PubMed]
- Hamada, N.; Tanaka, A.; Fujita, Y.; Itoh, T.; Ono, Y.; Kitagawa, Y.; Tomimori, N.; Kiso, Y.; Akao, Y.; Nozawa, Y.; et al. Involvement of heme oxygenase-1 induction via Nrf2/ARE activation in protection against H2O2-induced PC12 cell death by a metabolite of sesamin contained in sesame seeds. Bioorg. Med. Chem. 2011, 19, 1959–1965. [Google Scholar] [CrossRef] [PubMed]
- Katayama, S.; Sugiyama, H.; Kushimoto, S.; Uchiyama, Y.; Hirano, M.; Nakamura, S. Effects of Sesaminol Feeding on Brain Aβ Accumulation in a Senescence-Accelerated Mouse-Prone 8. J. Agric. Food Chem. 2016, 64, 4908–4913. [Google Scholar] [CrossRef]
- Hayami, T.; Pickarski, M.; Zhuo, Y.; Wesolowski, G.A.; Rodan, G.A.; Duong, L.T. Characterization of articular cartilage and subchondral bone changes in the rat anterior cruciate ligament transection and meniscectomized models of osteoarthritis. Bone 2006, 38, 234–243. [Google Scholar] [CrossRef]
- Pearle, A.D.; Warren, R.F.; Rodeo, S.A. Basic science of articular cartilage and osteoarthritis. Clin. Sports Med. 2005, 24, 1–12. [Google Scholar] [CrossRef]
- Goldring, M.B. Osteoarthritis and cartilage: the role of cytokines. Curr. Rheumatol. Rep. 2000, 2, 459–465. [Google Scholar] [CrossRef]
- Daheshia, M.; Yao, J.Q. The interleukin-1β pathway in the pathogenesis of osteoarthritis. J. Rheumatol. 2008, 35, 2306–2312. [Google Scholar] [CrossRef]
- Struglics, A.; Larsson, S.; Pratta, M.A.; Kumar, S.; Lark, M.W.; Lohmander, L.S. Human osteoarthritis synovial fluid and joint cartilage contain both aggrecanase- and matrix metalloproteinase-generated aggrecan fragments. Osteoarthr. Cartil. 2006, 14, 101–113. [Google Scholar] [CrossRef] [Green Version]
- Mitchell, P.G.; Magna, H.A.; Reeves, L.M.; Lopresti-Morrow, L.L.; Yocum, S.A.; Rosner, P.J.; Geoghegan, K.F.; Hambor, J.E. Cloning, expression, and type II collagenolytic activity of matrix metalloproteinase-13 from human osteoarthritic cartilage. J. Clin. Invest. 1996, 97, 761–768. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Phitak, T.; Pothacharoen, P.; Settakorn, J.; Poompimol, W.; Caterson, B.; Kongtawelert, P. Chondroprotective and anti-inflammatory effects of sesamin. Phytochemistry 2012, 80, 77–88. [Google Scholar] [CrossRef] [PubMed]
- Kong, P.; Chen, G.; Jiang, A.; Wang, Y.; Song, C.; Zhuang, J.; Xi, C.; Wang, G.; Ji, Y.; Yan, J. Sesamin inhibits IL-1β-stimulated inflammatory response in human osteoarthritis chondrocytes by activating Nrf2 signalling pathway. Oncotarget 2016, 7, 83720–83726. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lu, Y.-C.; Jayakumar, T.; Duann, Y.-F.; Chou, Y.-C.; Hsieh, C.-Y.; Yu, S.-Y.; Sheu, J.-R.; Hsiao, G. Chondroprotective Role of Sesamol by Inhibiting MMPs Expression via Retaining NF-κB Signalling in Activated SW1353 Cells. J. Agric. Food Chem. 2011, 59, 4969–4978. [Google Scholar] [CrossRef] [PubMed]
- Yashaswini, P.S.; Kurrey, N.K.; Singh, S.A. Encapsulation of sesamol in phosphatidyl choline micelles: Enhanced bioavailability and anti-inflammatory activity. Food Chem. 2017, 228, 330–337. [Google Scholar] [CrossRef] [PubMed]
- Askari, A.; Ravansalar, S.A.; Naghizadeh, M.M.; Mosavat, S.Y.; Khodadoost, M.; Jazani, A.M.; Hashempur, M.H. The efficacy of topical sesame oil in patients with knee osteoarthritis: A randomized double-blinded active-controlled non-inferiority clinical trial. Complement. Ther. Med. 2019, 47, 102183. [Google Scholar] [CrossRef] [PubMed]
- Clark, J.M.; Diehl, A.M. Defining nonalcoholic fatty liver disease: implications for epidemiologic studies. Gastroenterology 2003, 124, 248–250. [Google Scholar] [CrossRef]
- Miller, A.M.; Wang, H.; Bertola, A.; Park, O.; Horiguchi, N.; Ki, S.H.; Yin, S.; Lafdil, F.; Gao, B. Inflammation-associated interleukin-6/signal transducer and activator of transcription 3 activation ameliorates alcoholic and nonalcoholic fatty liver diseases in interleukin-10-deficient mice. Hepatology 2011, 54, 846–856. [Google Scholar] [CrossRef] [Green Version]
- Yoshikawa, T.; Ide, T.; Shimano, H.; Yahagi, N.; Amemiya-Kudo, M.; Matsuzaka, T.; Yatoh, S.; Kitamine, T.; Okazaki, H.; Tamura, Y.; et al. Cross-Talk between Peroxisome Proliferator-Activated Receptor (PPAR) α and Liver X Receptor (LXR) in Nutritional Regulation of Fatty Acid Metabolism. I. PPARs Suppress Sterol Regulatory Element Binding Protein-1c Promoter through Inhibition of LXR Signalling. Mol. Endocrinol. 2003, 17, 1240–1254. [Google Scholar]
- Zhang, R.; Yu, Y.; Hu, S.; Zhang, J.; Yang, H.; Han, B.; Cheng, Y.; Luo, X. Sesamin ameliorates hepatic steatosis and inflammation in rats on a high-fat diet via LXRα and PPARα. Nutr. Res. 2016, 36, 1022–1030. [Google Scholar] [CrossRef]
- Bernal, W.; Auzinger, G.; Dhawan, A.; Wendon, J. Acute liver failure. Lancet 2010, 376, 190–201. [Google Scholar] [CrossRef]
- Felipo, V. Hepatic encephalopathy: effects of liver failure on brain function. Nat. Rev. Neurosci. 2013, 14, 851–858. [Google Scholar] [CrossRef] [PubMed]
- Ma, L.; Gong, X.; Kuang, G.; Jiang, R.; Chen, R.; Wan, J. Sesamin ameliorates lipopolysaccharide/d-galactosamine-induced fulminant hepatic failure by suppression of Toll-like receptor 4 signalling in mice. Biochem. Biophys. Res. Commun. 2015, 461, 230–236. [Google Scholar] [CrossRef] [PubMed]
- Chiang, H.-M.; Chang, H.; Yao, P.-W.; Chen, Y.-S.; Jeng, K.-C.; Wang, J.-S.; Hou, C.-W. Sesamin reduces acute hepatic injury induced by lead coupled with lipopolysaccharide. J. Chin. Med. Assoc. 2014, 77, 227–233. [Google Scholar] [CrossRef] [Green Version]
- Nakai, M.; Harada, M.; Nakahara, K.; Akimoto, K.; Shibata, H.; Miki, W.; Kiso, Y. Novel antioxidative metabolites in rat liver with ingested sesamin. J. Agric. Food Chem. 2003, 51, 1666–1670. [Google Scholar] [CrossRef]
- Yasuda, K.; Ikushiro, S.; Kamakura, M.; Ohta, M.; Sakaki, T. Metabolism of sesamin by cytochrome P450 in human liver microsomes. Drug Metab. Dispos. 2010, 38, 2117–2123. [Google Scholar] [CrossRef] [Green Version]
- Yasuda, K.; Ikushiro, S.; Kamakura, M.; Munetsuna, E.; Ohta, M.; Sakaki, T. Sequential metabolism of sesamin by cytochrome P450 and UDP-glucuronosyltransferase in human liver. Drug Metab. Dispos. 2011, 39, 1538–1545. [Google Scholar] [CrossRef] [Green Version]
- Tomimori, N.; Tanaka, Y.; Kitagawa, Y.; Fujii, W.; Sakakibara, Y.; Shibata, H. Pharmacokinetics and safety of the sesame lignans, sesamin and episesamin, in healthy subjects. Biopharm. Drug Dispos. 2013, 34, 462–473. [Google Scholar] [CrossRef]
- Tomimori, N.; Rogi, T.; Shibata, H. Absorption, distribution, metabolism, and excretion of [14C] sesamin in rats. Mol. Nutr. Food Res. 2017, 61, 1600844. [Google Scholar] [CrossRef]
- Abe-Kanoh, N.; Lee, Y.; Takemoto, D.; Ono, Y.; Shibata, H.; Ohnishi, K.; Kawai, Y. Sesamin catechol glucuronides exert anti-inflammatory effects by suppressing IFN-β and iNOS expression through the deconjugation in macrophage-like J774.1 cells. J. Agric. Food Chem. 2019, 67, 7640–7649. [Google Scholar] [CrossRef]
- Periasamy, S.; Chien, S.-P.; Chang, P.-C.; Hsu, D.-Z.; Liu, M.-Y. Sesame oil mitigates nutritional steatohepatitis via attenuation of oxidative stress and inflammation: a tale of two-hit hypothesis. J. Nutr. Biochem. 2014, 25, 232–240. [Google Scholar] [CrossRef] [PubMed]
- Periasamy, S.; Hsu, D.-Z.; Chang, P.-C.; Liu, M.-Y. Sesame oil attenuates nutritional fibrosing steatohepatitis by modulating matrix metalloproteinases-2, 9 and PPAR-γ. J. Nutr. Biochem. 2014, 25, 337–344. [Google Scholar] [CrossRef] [PubMed]
- Hsu, D.Z.; Chien, S.P.; Li, Y.H.; Liu, M.Y. Sesame oil does not show accumulatively enhanced protection against oxidative-stress-associated hepatic injury in septic rats. J. Parenter. Enter. Nutr. 2008, 32, 276–280. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Xu, J.-P.; Zheng, Y.-C.; Chen, W.; Sun, Y.-W.; Wu, Z.-Y.; Luo, M. Peroxisome proliferator-activated receptor gamma inhibits hepatic fibrosis in rats. Hepatobiliary Pancreat. Dis. Int. 2011, 10, 64–71. [Google Scholar] [CrossRef]
- Abdelmegeed, M.A.; Yoo, S.H.; Henderson, L.E.; Gonzalez, F.J.; Woodcroft, K.J.; Song, B.J. PPAR alpha expression protects male mice from high fat-induced non-alcoholic fatty liver. J. Nutr. 2011, 141, 603–610. [Google Scholar] [CrossRef] [PubMed]
- Zhang, F.; Lu, Y.; Zheng, S. Peroxisome proliferator-activated receptor-γ crossregulation of signalling events implicated in liver fibrogenesis. Cell Sign. 2012, 24, 596–605. [Google Scholar] [CrossRef]
- Periasamy, S.; Yang, S.S.; Chen, S.Y.; Chang, C.C.; Liu, M.Y. Prophylactic sesame oil attenuates sinusoidal obstruction syndrome by inhibiting matrix metalloproteinase- 9 and oxidative stress. J. Parenter. Enter. Nutr. 2013, 37, 529–537. [Google Scholar] [CrossRef]
- Kim, M.; Woo, M.; Noh, J.S.; Choe, E.; Song, Y.O. Sesame oil lignans inhibit hepatic endoplasmic reticulum stress and apoptosis in high-fat diet-fed mice. J. Funct. Foods 2017, 37, 658–665. [Google Scholar] [CrossRef]
- Gologorsky, D.; Thanos, A.; Vavvas, D. Therapeutic interventions against inflammatory and angiogenic mediators in proliferative diabetic retinopathy. Mediat. Inflamm. 2012, 2012, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Saijo, K.; Glass, C.K. Microglial cell origin and phenotypes in health and disease. Nat. Rev. Immunol. 2011, 11, 775–787. [Google Scholar] [CrossRef]
- Elsherbiny, N.M.; Ahmad, S.; Naime, M.; Elsherbini, A.M.; Fulzele, S.; Al-Gayyar, M.M.; Eissa, L.A.; El-Shishtawy, M.M.; Liou, G.I. ABT-702, an adenosine kinase inhibitor, attenuates inflammation in diabetic retinopathy. Life Sci. 2013, 93, 78–88. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, S.; ElSherbiny, N.M.; Jamal, M.S.; Alzahrani, F.A.; Haque, R.; Khan, R.; Zaidi, S.K.; AlQahtani, M.H.; Liou, G.I.; Bhatia, K. Anti-inflammatory role of sesamin in STZ induced mice model of diabetic retinopathy. J. Neuroimmunol. 2016, 295–296, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Kondamudi, P.K.; Kovelamudi, H.; Mathew, G.; Nayak, P.G.; Rao, C.M.; Shenoy, R.R. Modulatory effects of sesamol in dinitrochlorobenzene-induced inflammatory bowel disorder in albino rats. Pharm. Rep. 2013, 65, 658–665. [Google Scholar] [CrossRef]
- Hawkey, C.J. Non-steroidal anti-inflammatory drug gastropathy: Causes and treatment. Scand. J. Gastroenterol. 1996, 220, 124–127. [Google Scholar] [CrossRef]
- Tappel, A.L. Lipid peroxidation damage to cell components. Fed. Proc. 1973, 32, 1870–1874. [Google Scholar]
- Szabo, C.; Cuzzocrea, S.; Zingarelli, B.; O’Connor, M.; Salzman, A.L. Endothelial dysfunction in a rat model of endotoxic shock. Importance of the activation of poly (ADPribose) synthetase by peroxynitrite. J. Clin. Investig. 1997, 100, 723–735. [Google Scholar] [CrossRef] [Green Version]
- Hsu, D.-Z.; Chu, P.-Y.; Chandrasekaran, V.R.M.; Liu, M.-Y. Sesame lignan sesamol protects against aspirin-induced gastric mucosal damage in rats. J. Funct. Foods 2009, 1, 349–355. [Google Scholar] [CrossRef]
- Jan, K.-C.; Ku, K.-L.; Chu, Y.-H.; Hwang, L.S.; Ho, C.-T. Tissue Distribution and Elimination of Estrogenic and Anti-Inflammatory Catechol Metabolites from Sesaminol Triglucoside in Rats. J. Agric. Food Chem. 2010, 58, 7693–7700. [Google Scholar] [CrossRef]
- Lee, S.Y.; Son, D.J.; Lee, Y.K.; Lee, J.W.; Lee, H.J.; Yun, Y.W.; Ha, T.Y.; Hong, J.T. Inhibitory effect of sesaminol glucosides on lipopolysaccharide-induced NF-kappaB activation and target gene expression in cultured rat astrocytes. Neurosci. Res. 2006, 56, 204–212. [Google Scholar] [CrossRef]
- Ji, Z.-L.; Li, J.-S.; Yuan, C.-W.; Chen, W.; Zhang, Y.-N.; Ju, X.-T.; Tang, W.-H. Therapeutic value of sesame oil in the treatment of adhesive small bowel obstruction. Am. J. Surg. 2010, 199, 160–165. [Google Scholar] [CrossRef]
- Yeh, M.; Leitinger, N.; de Martin, R.; Onai, N.; Matsushima, K.; Vora, D.K.; Berliner, J.A.; Reddy, S.T. Increased transcription of IL-8 in endothelial cells is differentially regulated by TNF-R and oxidized phospholipids. Arterioscler. Thromb. Vasc. Biol. 2001, 21, 1585–1591. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, W.-J.; Ou, H.-C.; Wu, C.-M.; Lee, I.; Lin, S.-Y.; Lin, L.-Y.; Tsai, K.-L.; Lee, S.-D.; Sheu, W.H.-H. Sesamin Mitigates Inflammation and Oxidative Stress in Endothelial Cells Exposed to Oxidized Low-Density Lipoprotein. J. Agric. Food Chem. 2009, 57, 11406–11417. [Google Scholar] [CrossRef] [PubMed]
- Shenasa, M.; Shenasa, H.; El-Sherif, N. Left ventricular hypertrophy and arrhythmogenesis. Card. Electrophysiol. Clin. 2015, 7, 207–220. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, A.A.; Prieto, M.C. Renin and the (pro) renin receptor in the renal collecting duct: role in the pathogenesis of hypertension. Clin. Exp. Pharmacol. Physiol. 2015, 42, 14–21. [Google Scholar] [CrossRef] [Green Version]
- Omura, T.; Yoshiyama, M.; Yoshida, K.; Nakamura, Y.; Kim, S.; Iwao, H.; Takeuchi, H.; Yoshikawa, J. Dominant negative mutant of c-Jun inhibits cardiomyocyte hypertrophy induced by endothelin 1 and phenylephrine. Hypertension 2002, 39, 81–86. [Google Scholar] [CrossRef] [Green Version]
- Abdelhamid, G.; El-Kadi, A.O. Buthionine Sulfoximine, an inhibitor of glutathione biosynthesis, induces expression of soluble epoxide hydrolase and markers of cellular hypertrophy in a rat cardiomyoblast cell line: roles of the NF-κB and MAPK signaling pathways. Free Radic. Bio. Med. 2015, 82, 1–12. [Google Scholar] [CrossRef]
- Liu, C.-T.; Liu, M.-Y. Daily sesame oil supplementation attenuates local renin-angiotensin system via inhibiting MAPK activation and oxidative stress in cardiac hypertrophy. J. Nutr. Biochem. 2017, 42, 108–116. [Google Scholar] [CrossRef]
- Bone, R.C. The pathogenesis of sepsis. Ann. Intern. Med. 1991, 115, 457–469. [Google Scholar] [CrossRef]
- Matthay, M.A.; Zimmerman, G.A. Acute lung injury and the acute respiratory distress syndrome: four decades of inquiry into pathogenesis and rational management. Am. J. Respir. Cell Mol. Biol. 2005, 33, 319–327. [Google Scholar] [CrossRef]
- Braude, S.; Nolop, K.B.; Hughes, J.M.B.; Barnes, P.J.; Royston, D. Comparison of lung vascular and epithelial permeability indices in the adult respiratory distress syndrome. Am. Rev. Respir. Dis. 1986, 133, 1002–1005. [Google Scholar]
- Tomashefski, J. Pulmonary pathology of the adult respiratory distress syndrome. Clin. Chest Med. 1990, 11, 593–619. [Google Scholar] [PubMed]
- Sinclair, D.G.; Braude, S.; Haslam, P.L.; Evans, T.W. Pulmonary endothelial permeability in patients with severe lung injury. Clin. Correl. Nat. His. Chest 1994, 106, 535–539. [Google Scholar] [CrossRef] [PubMed]
- Chu, P.-Y.; Chien, S.-P.; Hsu, D.-Z.; & Liu, M.-Y. Protective effect of sesamol on the pulmonary inflammatory response and lung injury in endotoxemic rats. Food Chem. Toxicol. 2010, 48, 1821–1826. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.; Yokomizo, T. The role of leukotrienes in allergic diseases. Allergol. Int. 2015, 64, 17–26. [Google Scholar] [CrossRef] [Green Version]
- Yashaswini, P.S.; Sadashivaiah, B.; Ramaprasad, T.R.; Singh, S.A. In vivo modulation of LPS induced leukotrienes generation and oxidative stress by sesame lignans. J. Nutr. Biochem. 2017, 41, 151–157. [Google Scholar] [CrossRef]
- Andreou, A.; Gobel, C.; Hamberg, M.; Feussner, I. A bisallylic mini-lipoxygenase from cyanobacterium Cyanothece sp. that has an iron as cofactor. J. Biol. Chem. 2010, 285, 14178–14186. [Google Scholar] [CrossRef] [Green Version]
- Mahesha, H.G.; Singh, S.A.; Appu Rao, A.G. Inhibition of lipoxygenase by soy isoflavones: Evidence of isoflavones as redox inhibitors. Arch. Biochem. Biophys. 2007, 461, 176–185. [Google Scholar] [CrossRef]
- Yashaswini, P.S.; Rao, A.G.A.; Singh, S.A. Inhibition of lipoxygenase by sesamol corroborates its potential anti-inflammatory activity. Int. J. Biol. Macromol. 2017, 94, 781–787. [Google Scholar] [CrossRef]
- Deme, P.; Narasimhulu, C.A.; Parthasarathy, S. Identification and evaluation of anti-inflammatory properties of aqueous components extracted from sesame (Sesamum indicum) oil. J. Chromatogr. B 2018, 1087–1088, 61–69. [Google Scholar] [CrossRef]
- Yang, Y.; Wang, J.; Zhang, Y.; Li, J.; Sun, W. Black Sesame Seeds Ethanol Extract Ameliorates Hepatic Lipid Accumulation, Oxidative Stress and Insulin Resistance in Fructose-induced Nonalcoholic Fatty Liver Disease. J. Agric. Food Chem. 2018, 66, 10458–10469. [Google Scholar] [CrossRef]
- Ruckmani, A.; Meti, V.; Vijayashree, R.; Arunkumar, R.; Konda, V.R.; Prabhu, L.; Madhavi, E.; Devi, S. Anti-rheumatoid activity of ethanolic extract of Sesamum indicum seed extract in Freund’s complete adjuvant induced arthritis in Wistar albino rats. J. Tradit. Complement. Med. 2018, 8, 377–386. [Google Scholar] [CrossRef] [PubMed]
- Botelho, J.R.S.; Medeiros, N.G.; Rodrigues, A.M.C.; Araújo, M.E.; Machado, N.T.; Guimarães Santos, A.; Rogerio Santos, I.; Gomes-Leal, W.; Carvalho, R.N. Black sesame (Sesamum indicum L.) seeds extracts by CO2 supercritical fluid extraction: Isotherms of global yield, kinetics data, total fatty acids, phytosterols and neuroprotective effects. J. Supercrit. Fluids 2014, 93, 49–55. [Google Scholar] [CrossRef]
- Wang, B.-S.; Chang, L.-W.; Yen, W.-J.; Duh, P.-D. Antioxidative effect of sesame coat on LDL oxidation and oxidative stress in macrophages. Food Chem. 2007, 102, 351–360. [Google Scholar] [CrossRef]
- Chang, L.W.; Yen, W.J.; Huang, S.C.; Duh, P.D. Antioxidant activity of sesame coat. Food Chem. 2002, 78, 347–354. [Google Scholar] [CrossRef]
- Kay, J.; Thadhani, E.; Samson, L.; Engelward, B. Inflammation-Induced DNA Damage Mutations and Cancer. DNA Repair 2019, 83, 102673. [Google Scholar] [CrossRef]
- Greten, F.R.; Grivennikov, S.I. Inflammation and Cancer: Triggers, Mechanisms, and Consequences. Immunity 2019, 51, 27–41. [Google Scholar] [CrossRef]
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global Cancer Statistics 2018: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [Green Version]
- Cabral, B.P.; Fonseca, M.G.D.; Mota, F.B. The Recent Landscape of Cancer Research Worldwide: A Bibliometric and Network Analysis. Oncotarget 2018, 9, 30474–30484. [Google Scholar] [CrossRef]
- Gutschner, T.; Diederichs, S. The Hallmarks of Cancer: A Long Non-Coding RNA Point of View. RNA Biol. 2012, 9, 703–719. [Google Scholar] [CrossRef] [Green Version]
- Hanahan, D.; Weinberg, R.A. The Hallmarks of Cancer. Cell Press. 2000, 100, 57–70. [Google Scholar] [CrossRef] [Green Version]
- Hanahan, D.; Weinberg, R.A. Hallmarks of Cancer: The Next Generation. Cell 2011, 144, 646–674. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Prakash, K.; Naik, S.N. Bioactive Constituents as a Potential Agent in Sesame for Functional and Nutritional Application. J. Bioresour. Eng. Technol. 2014, 1, 48–66. [Google Scholar]
- Harikumar, K.B.; Sung, B.; Tharakan, S.T.; Pandey, M.K.; Joy, B.; Guha, S.; Krishnan, S.; Aggarwal, B.B. Sesamin Manifests Chemopreventive Effects through the Suppression of NF-κB-Regulated Cell Survival, Proliferation, Invasion, and Angiogenic Gene Products. Mol. Cancer Res. 2010, 8, 751–761. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Watanabe, M.; Iizumi, Y.; Iizuka-Ohashi, M.; Sowa, Y.; Sakai, T. The Pleiotropic Regulation of Cyclin D1 by Newly Identified Sesaminol-Binding Protein ANT2. Oncogenesis 2017, 6, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Majdalawieh, A.F.; Mansour, Z.R. Sesamol, a Major Lignan in Sesame Seeds (Sesamum indicum): Anti-Cancer Properties and Mechanisms of Action. Eur. J. Pharmacol. 2019, 855, 75–89. [Google Scholar] [CrossRef] [PubMed]
- Siriwarin, B.; Weerapreeyakul, N. Sesamol Induced Apoptotic Effect in Lung Adenocarcinoma Cells through Both Intrinsic and Extrinsic Pathways. Chem.-Biol. Interact. 2016, 254, 109–116. [Google Scholar] [CrossRef] [PubMed]
- Siriwarin, B.; Weerapreeyakul, N.; Tanthanuch, W.; Thumanu, K. Biomolecular Changes and DNA Targeting Effect of Sesamol in Human Lung Adenocarcinoma (SK-LU-1) Cells by FTIR Microscopy. Asian Pac. J. Trop. Biomed. 2018, 8, 377–386. [Google Scholar]
- Majdalawieh, A.F.; Massri, M.; Nasrallah, G.K. A Comprehensive Review on the Anti-Cancer Properties and Mechanisms of Action of Sesamin, a Lignan in Sesame Seeds (Sesamum indicum). Eur. J. Pharmacol. 2017, 815, 512–521. [Google Scholar] [CrossRef]
- Liu, C.-M.; Zheng, G.-H.; Ming, Q.-L.; Chao, C.; Sun, J.-M. Sesamin Protects Mouse Liver against Nickel-Induced Oxidative DNA Damage and Apoptosis by the PI3K-Akt Pathway. J. Agric. Food Chem. 2013, 61, 1146–1154. [Google Scholar] [CrossRef]
- Fang, Q.; Zhu, Y.; Wang, Q.; Song, M.; Gao, G.; Zhou, Z. Suppression of Cyclooxygenase-2 Increases Chemosensitivity to Sesamin through the Akt-PI3K Signalling Pathway in Lung Cancer Cells. Int. J. Mol. Med. 2019, 43, 507–516. [Google Scholar]
- Bilancio, A.; Rinaldi, B.; Oliviero, M.A.; Donniacuo, M.; Monti, M.G.; Boscaino, A.; Marino, I.; Friedman, L.; Rossi, F.; Vanhaesebroeck, B.; et al. Inhibition of p11δ PI3K Prevents Inflammatory Response and Restenosis After Artery Injury. Biosci. Rep. 2017, 37, 1–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yokota, T.; Matsuzaki, Y.; Koyama, M.; Hitomi, T.; Kawanaka, M.; Enoki-Konishi, M.; Okuyama, Y.; Takayasu, J.; Nishino, H.; Nishikawa, A.; et al. Sesamin, a lignan of sesame, down-regulates cyclin D1 protein expression in human tumor cells. Cancer Sci. 2007, 98, 1447–1453. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.-C.; Liu, K.-J.; Wu, Y.-C.; Lin, S.-J.; Chang, C.-C.; Huang, T.-S. Sesamin Inhibits Macrophage-Induced Vascular Endothelial Growth Factor and Matrix Metalloproteinase-9 Expression and Proangiogenic Activity in Breast Cancer Cells. Inflammation 2010, 34, 209–221. [Google Scholar] [CrossRef] [PubMed]
- Akl, M.R.; Ayoub, N.M.; Abuasal, B.S.; Kaddoumi, A.; Sylvester, P.W. Sesamin Synergestically Potentiates the Anticancer Effects of γ-Tocotrienol in Mammary Cancer Cell Lines. Fitoterapia 2013, 84, 347–359. [Google Scholar] [CrossRef] [PubMed]
- Truan, J.S.; Chen, J.-M.; Thompson, L.U. Comparative Effects of Sesame Seed Lignan and Flaxseed Lignan in Reducing the Growth of Human Breast Tumors (MCF-7) at High Levels of Circulating Estrogen in Athymic Mice. Nutr. Cancer 2012, 64, 65–71. [Google Scholar] [CrossRef] [PubMed]
- Jacklin, A.; Ratledge, C.; Welham, K.; Bilko, D.; Newton, C.J. The Sesame Seed Oil Constituent, Sesamol, Induces Growth Arrest and Apoptosis of Cancer and Cardiovascular Cells. Ann. N. Y. Acad. Sci. 2003, 1010, 374–380. [Google Scholar] [CrossRef]
- Galli, F.; Stabile, A.M.; Betti, M.; Conte, C.; Pistilli, A.; Rende, M.; Floridi, A.; Azzi, A. The Effect of α- and γ-Tocopherol and Their Carboxyethyl Hydroxychroman Metabolites on Prostate Cancer Cell Proliferation. Arch. Biochem. Biophys. 2004, 423, 97–102. [Google Scholar] [CrossRef]
- Isha, D.; Milind, P. Eat Til and Protect Dil. Int. Res. J. Pharm. 2012, 3, 54–57. [Google Scholar]
- Cooney, R.V.; Custer, L.J.; Okinaka, L.; Franke, A.A. Effects of Dietary Sesame Seeds on Plasma Tocopherol Levels. Nutr. Cancer 2009, 39, 66–71. [Google Scholar] [CrossRef]
- Yamashita, K.; Iizuka, Y.; Imai, T.; Namiki, M. Sesame Seed and Its Lignans Produce Marked Enhancement of Vitamin E Activity in Rats Fed a Low α-Tocopherol Diet. Lipids 1995, 30, 1019–1028. [Google Scholar] [CrossRef]
- Jeng, K.C.G.; Hou, R.C.W. Sesamin and Sesamolin: Nature’s Therapeutic Lignans. Curr. Enzyme Inhib. 2005, 1, 11–20. [Google Scholar] [CrossRef]
- Shimizu, S.; Fujii, G.; Takahashi, M.; Nakanishi, R.; Komiya, M.; Shimura, M.; Noma, N.; Onuma, W.; Terasaki, M.; Yano, T.; et al. Sesamol Suppresses Cyclooxygenase-2 Transcriptional Activity in Colon Cancer Cells and Modifies Intestinal Polyp Development in ApcMin/+ Mice. J. Clin. Biochem. Nutr. 2014, 54, 95–101. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khamphio, M.; Barusrux, S.; Weerapreeyakul, N. Sesamol Induces Mitochondrial Apoptosis Pathway in HCT116 Human Colon Cancer Cells via Pro-Oxidant Effect. Life Sci. 2016, 158, 46–56. [Google Scholar] [CrossRef] [PubMed]
- Silva-Prado, L.; Azevedo, L.; Oliveira, J.A.C.; Moreire, A.P.M.; Schmiele, M.; Chang, Y.K.; Paula, F.B.A.; Clerici, M.T.P.S. Sesame and Resistance Starch Reduce the Colon Carcinogenesis and Oxidative Stress in 1,2-dimethylhydrazine-induced Cancer in Wistar Rats. Food Res. Int. 2014, 62, 609–617. [Google Scholar] [CrossRef]
- Sheng, H.Q.; Hirose, Y.; Hata, K.; Zheng, Q.; Kuno, T.; Asano, N.; Yamada, Y.; Hara, A.; Osawa, T.; Mori, H. Modifying Effect of Dietary Sesaminol Glucosides on the Formation of Azoxymethane-Induced Premalignant Lesions of Rat Colon. Cancer Lett. 2007, 246, 63–68. [Google Scholar] [CrossRef]
- Deng, P.; Wang, C.; Chen, L.; Wang, C.; Du, Y.; Yan, X.; Chen, M.; Yang, G.; He, G. Sesamin Induces Cell Cycle Arrest and Apoptosis through the Inhibition of Signal Transducer and Activator of Transcription 3 Signalling in Human Hepatocellular Carcinoma Cell Line HepG2. Biol. Pharm. Bull. 2013, 36, 1540–1548. [Google Scholar] [CrossRef] [Green Version]
- Liu, Z.; Xiang, Q.; Du, L.; Song, G.; Wang, Y.; Liu, X. The Interaction of Sesamol with DNA and Cytotoxicity, Apoptosis, and Localization in HepG2 Cells. Food Chem. 2013, 141, 289–296. [Google Scholar] [CrossRef]
- Liu, Z.; Ren, B.; Wang, Y.; Zou, C.; Qiao, Q.; Diao, Z.; Mi, Y.; Zhu, D.; Liu, X. Sesamol Induces Human Hepatocellular Carcinoma Cells Apoptosis by Impairing Mitochondrial Function and Suppression Autophagy. Sci. Rep. 2017, 7, 45728. [Google Scholar] [CrossRef]
- Zhou, L.; Lin, X.; Abbasi, A.M.; Zheng, B. Phytochemical Contents and Antioxidant and Antiproliferative Activities of Selected Black and White Sesame Seeds. Biomed. Res. Int. 2016, 2016, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Dou, H.; Yang, S.; Hu, Y.; Xu, D.; Liu, L.; Li, X. Sesamin Induces ER Stress-Mediated Apoptosis and Activates Autophagy in Cervical Cancer Cells. Life Sci. 2018, 200, 87–93. [Google Scholar] [CrossRef]
- Miyahara, Y.; Hibasami, H.; Katsuzaki, H.; Imai, K.; Komiya, T. Sesamol Induces Apoptosis in Human Lymphoid Leukemia Molt 4B Cells. Food. Sci. Technol. Res. 2000, 6, 201–203. [Google Scholar] [CrossRef]
- Fujimoto, A.; Shingai, Y.; Oyama, T.B.; Kawanai, T.; Hashimoto, E.; Koizumi, K.; Kimura, K.; Masuda, T.; Oyama, Y. Apoptosis-Inducing Action of Two Products from Oxidation of Sesamol, an Antioxidative Constituent of Sesame Oil: A Possible Cytotoxicity of Oxidized Antioxidant. Toxicol. Vitro 2010, 24, 1720–1726. [Google Scholar] [CrossRef] [PubMed]
- Geetha, T.; Kapila, M.; Prakash, O.; Deol, P.K.; Kakkar, V.; Kaur, I.P. Sesamol-Loaded Solid Lipid Nanoparticles for Treatment of Skin Cancer. J. Drug Target. 2015, 23, 159–169. [Google Scholar] [CrossRef] [PubMed]
- Namiki, M. Nutraceutical Functions of Sesame: A Review. Crit. Rev. Food Sci. Nutr. 2007, 47, 651–673. [Google Scholar] [CrossRef] [PubMed]
- Miyahara, Y.; Katsuzaki, H.; Imai, K.; Osawa, T.; Ina, K.; Komiya, T. Sesaminol from Sesame Seed Induces Apoptosis in Human Lymphoid Leukemia Molt 4B Cells. Int. J. Mol. Med. 2001, 7, 485–488. [Google Scholar] [CrossRef]
- Kim, J.H.; Lee, J.K. Sesamolin Enhances NK Cell Lysis Activity by Increasing the Expression of NKG2D Ligands on Burkitt’s Lymphoma Cells. Int. Immunopharmacol. 2015, 28, 977–984. [Google Scholar] [CrossRef] [PubMed]
- Srisayam, M.; Weerapreeyakul, N.; Kanokmedhakul, K. Inhibition of Two Stages of Melanin Synthesis by Sesamol, Sesamin, and Sesamolin. Asian Pac. J. Trop. Biomed. 2017, 7, 886–895. [Google Scholar] [CrossRef]
- Smith, D.E.; Salerno, J.W. Selective Growth Inhibition of a Human Malignant Melanoma Cell Line by Sesame Oil In Vitro. Prostaglandins Leukot. Essent. Fat. Acids 1992, 46, 145–150. [Google Scholar] [CrossRef]
- Kumar, C.M.; Sathisha, U.V.; Dharmesh, S.; Rao, A.G.A.; Singh, S.A. Interaction of Sesamol (3,4-methylenedioxyphenol) with Tyrosinase and its Effect on Melanin Synthesis. Biochimie 2011, 93, 562–569. [Google Scholar] [CrossRef]
- Kapadia, G.J.; Azuine, M.A.; Tokuda, H.; Takasaki, M.; Mukainaka, T.; Konoshima, T.; Nishino, H. Chemopreventive Effect of Resveratrol, Sesamol, Sesame Oil and Sunflower Oil in the Epstein-Barr Virus Early Antigen Activation Assay and the Mouse Skin Two-Stage Carcinogenesis. Pharmacol. Res. 2002, 45, 499–505. [Google Scholar] [CrossRef]
- Sugano, M.; Gu, J.-Y.; Yamada, K. Sesamin, a Multifunctional Factor for Prevention of Various Disorders Including Carcinogenesis. Food Fact. Cancer Prev. 1997, 245–248. [Google Scholar]
- Ogawa, T.; Makino, T.; Hirose, N.; Sugano, M. Lack of Influence of Low Blood Cholesterol Levels on Pancreatic Carcinogenesis After Initiation with N-nitrosobis (2-oxopropyl)amine in Syrian golden hamsters. Carcinogensis 1994, 15, 1663–1666. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.-H.; Leu, S.-F.; Jen, C.-Y.; Huang, B.-M. Effects of Sesamol on Apoptosis and Steroidogenesis in MA-10 Mouse Leydig Tumor Cells. J. Agric. Food Chem. 2011, 59, 9885–9891. [Google Scholar] [CrossRef] [PubMed]
| Compound | Cancer Type | Cell Line | Mechanism of Action | Reference |
|---|---|---|---|---|
| Sesame Oil | Skin Cancer | |||
| human malignant melanoma | SK-MEL | - | [163] | |
| two-stage mouse skin carcinogenesis | in vivo | protection against TPA tumor promotion | [165] | |
| Sesame Extract | Liver Cancer | |||
| human hepatocellular carcinoma | HepG2 | - | [154] | |
| Sesamin | Blood Cancer | |||
| chronic myeloid leukemia | K562 KBM-5 | inhibition of TNF-induced NF-κB activation | [128] | |
| myeloma | U266 | inhibition of TNF-induced NF-κB activation | [128] | |
| Breast Cancer | MCF-7 | induction of G1 cell cycle arrest; down-regulation of Cyclin D1 protein | [137] | |
| MCF-7 MDA-MB-231 | inhibition of macrophage-induced VEGF and MMP-9 mRNA expressions | [138] | ||
| MDA-MB-231 | inhibition of TNF-induced NF-κB activation | [128] | ||
| MCF-7 MDA-MB-231 | induction of G1 cell cycle arrest and reduction of protein expression levels | [139] | ||
| MCF-7 | down regulation of growth factor receptors EGFR, HER2, and pMAPK expression | [140] | ||
| Cervical Cancer | HeLa | favored apoptosis through the increase of Bax/Bcl-2 ratio; ER stress-mediated apoptosis by IRE1α/JNK pathway | [155] | |
| Colon Cancer | ||||
| colon carcinoma | HCT116 | inhibition of TNF-induced NF-κB activation | [128] | |
| Liver Cancer | ||||
| human hepatocellular carcinoma | HepG2 | suppression of the STAT3 signaling pathway | [151] | |
| Lung Cancer | ||||
| human lung adenocarcinoma | H1299 | inhibition of TNF-induced NF-κB activation | [128] | |
| Pancreatic cancer | MiaPaCa-2 | inhibition of TNF-induced NF-κB activation | [128] | |
| Prostate Cancer | PC-3 | degradation of γ-tocopherol metabolism | [146] | |
| DU145 | inhibition of TNF-induced NF-κB activation | [128] | ||
| Skin Cancer | ||||
| malignant melanoma | SK-MEL2 | absorption of ultraviolet in the UV range and inhibition of mushroom and cellular tyrosinase | [162] | |
| Sesaminol | Blood Cancer | |||
| lymphoid leukemia | Molt 4B | DNA fragmentation leading to apoptosis | [159,160] | |
| Breast Cancer | MCF-7 MDA-MB-231 | Reduction of cyclin D1 expression by binding to ANT2 protein | [129] | |
| Colon Cancer | ||||
| colon carcinoma | RKO | Reduction of cyclin D1 expression by binding to ANT2 protein | [129] | |
| Lung Cancer | ||||
| lung adenocarcinoma | A549 | Reduction of cyclin D1 expression by binding to ANT2 protein | [129] | |
| Skin Cancer | ||||
| melanoma | SK-MEL-28 | Reduction of cyclin D1 expression by binding to ANT2 protein | [129] | |
| Sesamol | Blood Cancer | |||
| acute myeloid leukemia | HL-60 | DNA fragmentation leading to apoptosis | [158] | |
| chronic myeloid leukemia | K562 | oxidation to tetramer; increased caspases activity leading to DNA damage | [157] | |
| lymphoid leukemia | Molt 4B | DNA fragmentation leading to apoptosis | [156] | |
| Breast Cancer | MCF-7 | growth inhibition and apoptosis in S and G2/M phases | [141] | |
| Colon Cancer | ||||
| colon adenocarcinoma | DLD-1 | suppression of cyclooxygenase-2 transcriptional activity | [147] | |
| colon carcinoma | HCT116 | subG1 phase cell cycle arrest causing cell death | [148] | |
| Liver Cancer | ||||
| human hepatocellular carcinoma | HepG2 | induced apoptosis and necrosis via DNA fragmentation and | [152,153] | |
| induced apoptosis via suppression of autophagy | ||||
| Lung Cancer | ||||
| lung adenocarcinoma | SK-LU-1 | increased activity of caspase 3 leading to DNA damage | [131,132] | |
| Skin Cancer | ||||
| human malignant melanoma | SK-MEL2 | absorption of ultraviolet in the UV range and inhibition of mushroom and cellular tyrosinase | [162] | |
| mouse melanoma | B16F10 | inhibition of monophenolase and diphenolase activities and promotion of apoptosis | [164] | |
| two-stage mouse skin carcinogenesis | in vivo | protection against TPA tumor promotion | [165] | |
| Others | ||||
| Mouse Leydig tumor | MA-10 | increased activity of caspase 3 leading to DNA damage at subG1 phase | [168] | |
| Sesamolin | Blood Cancer | |||
| Burkitt’s lymphoma | Raji | enhancement of NK cell lysis activity via escalated NKG2D ligand expression | [161] | |
| Prostate Cancer | PC-3 | degradation of γ-tocopherol metabolism | [146] | |
| Skin Cancer | ||||
| human malignant melanoma | SK-MEL2 | absorption of ultraviolet in the UV range and inhibition of mushroom and cellular tyrosinase | [162] |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, M.-S.; Aquino, L.B.B.; Barbaza, M.Y.U.; Hsieh, C.-L.; De Castro-Cruz, K.A.; Yang, L.-L.; Tsai, P.-W. Anti-Inflammatory and Anticancer Properties of Bioactive Compounds from Sesamum indicum L.—A Review. Molecules 2019, 24, 4426. https://doi.org/10.3390/molecules24244426
Wu M-S, Aquino LBB, Barbaza MYU, Hsieh C-L, De Castro-Cruz KA, Yang L-L, Tsai P-W. Anti-Inflammatory and Anticancer Properties of Bioactive Compounds from Sesamum indicum L.—A Review. Molecules. 2019; 24(24):4426. https://doi.org/10.3390/molecules24244426
Chicago/Turabian StyleWu, Ming-Shun, Levent Bless B. Aquino, Marjette Ylreb U. Barbaza, Chieh-Lun Hsieh, Kathlia A. De Castro-Cruz, Ling-Ling Yang, and Po-Wei Tsai. 2019. "Anti-Inflammatory and Anticancer Properties of Bioactive Compounds from Sesamum indicum L.—A Review" Molecules 24, no. 24: 4426. https://doi.org/10.3390/molecules24244426






