Blood Flow Dynamics at the Pulmonary Artery Bifurcation
Abstract
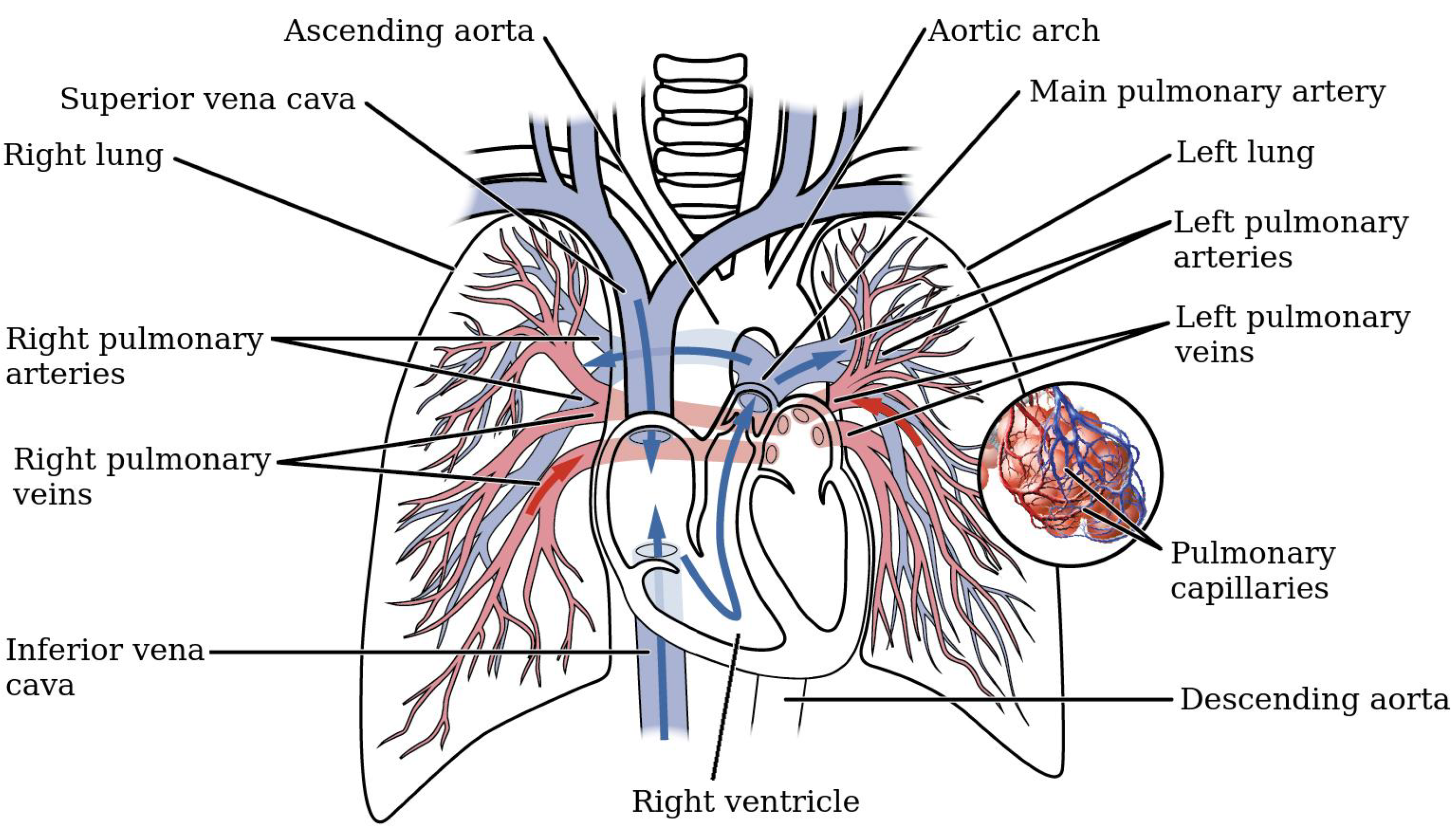
1. Introduction
2. Materials and Methods
2.1. Clinical Data
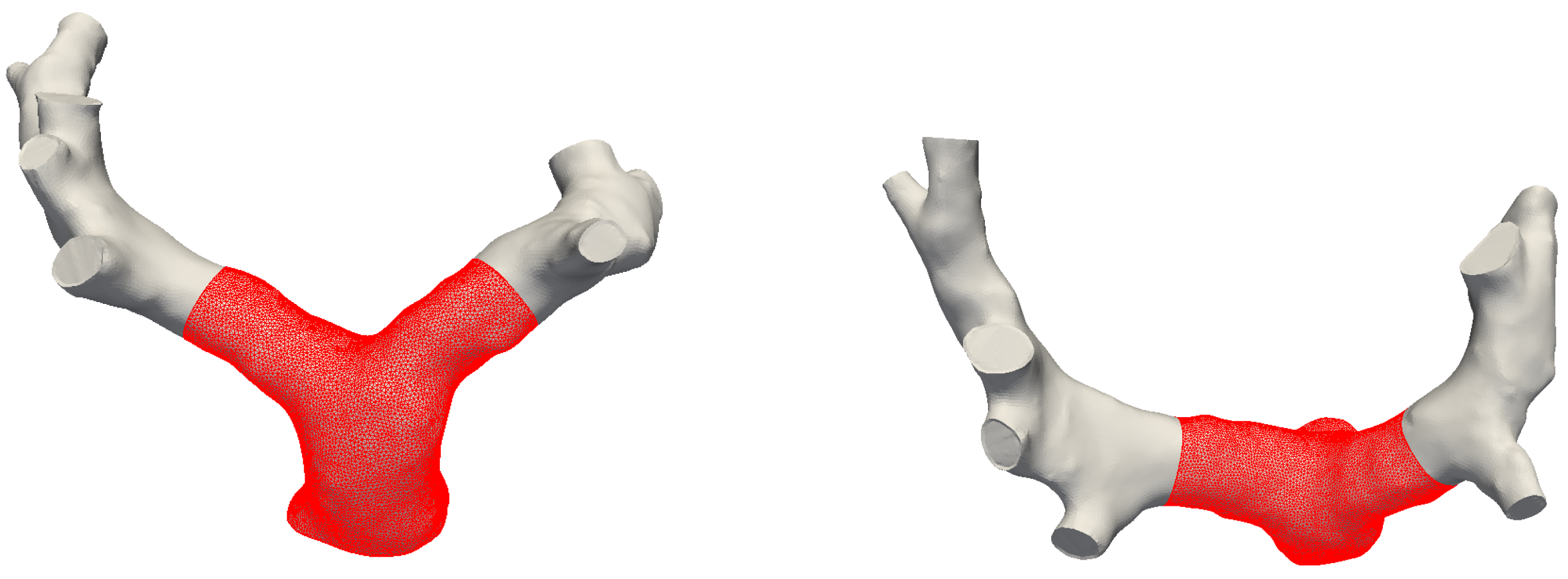
2.2. Model Construction
2.3. Boundary Conditions
2.4. Setup of Numerical Simulations
3. Results and Discussion
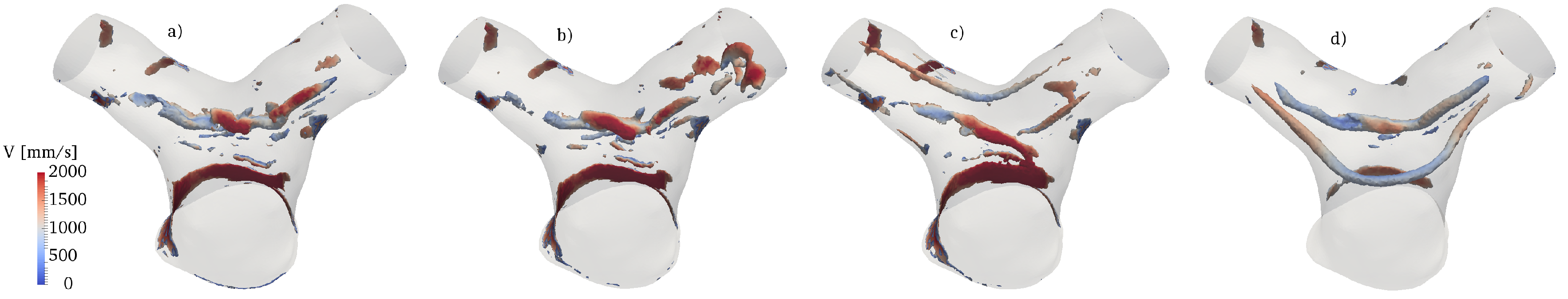
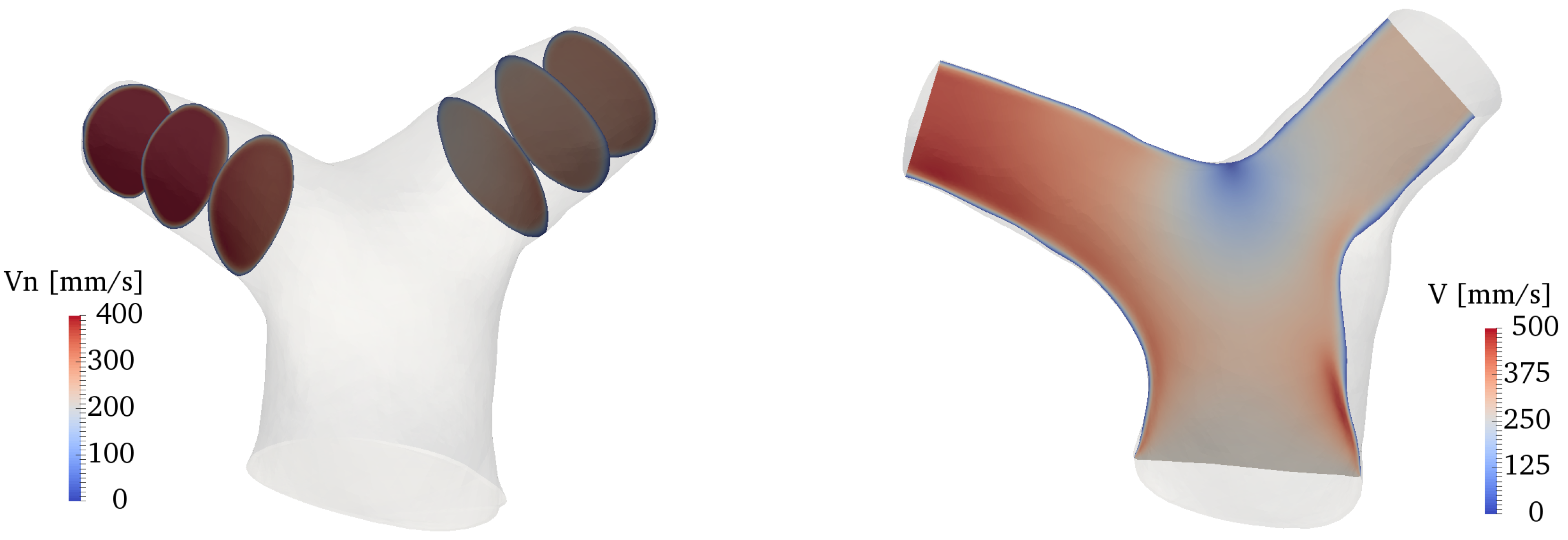
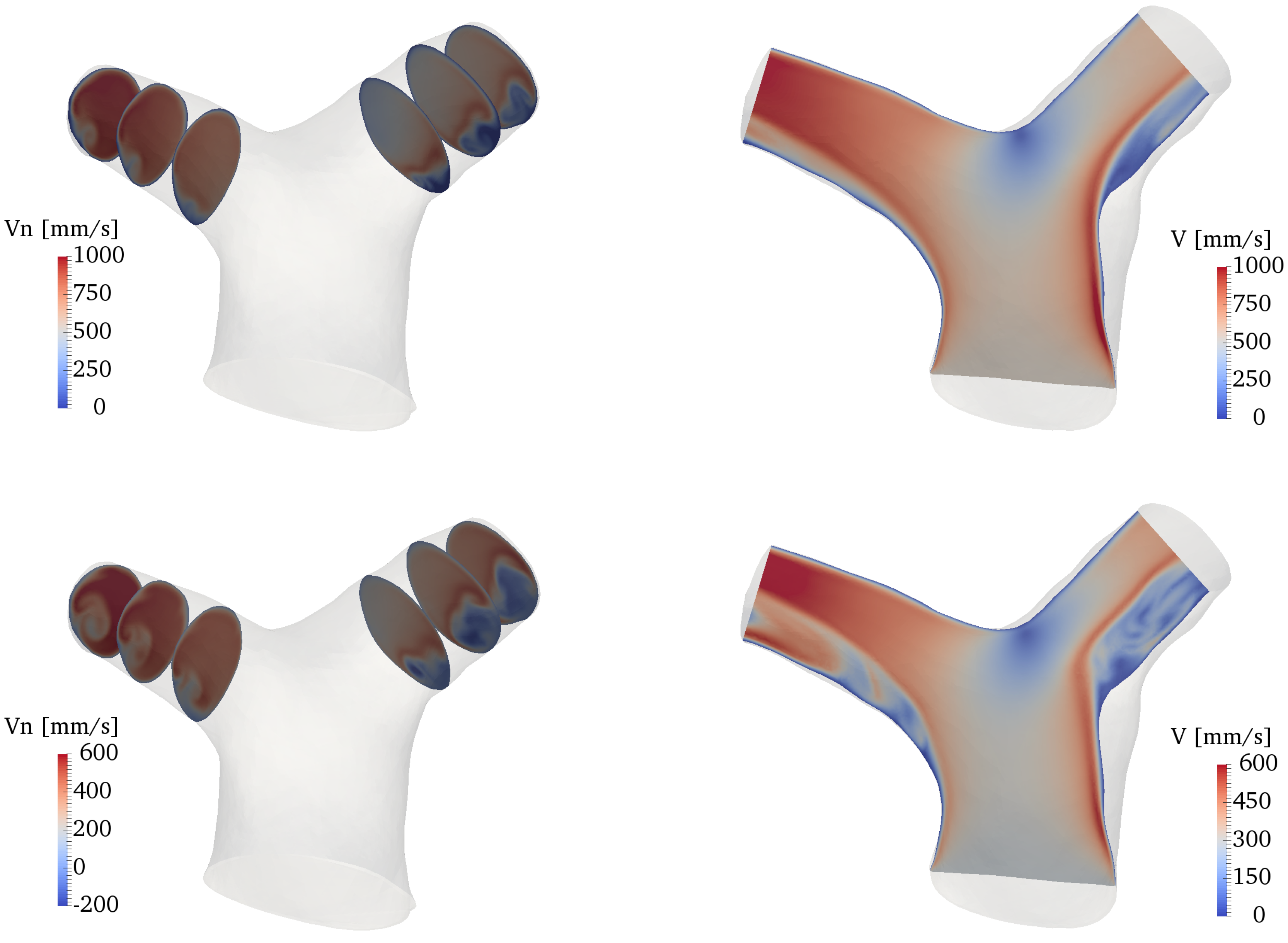
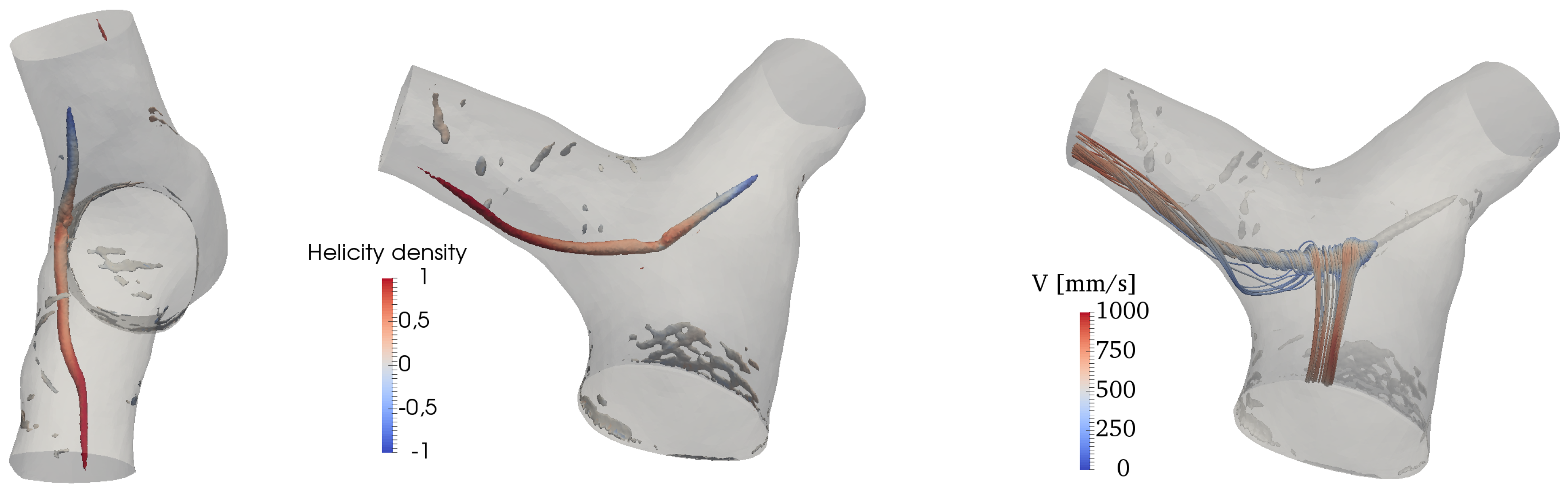
3.1. Global Flow Features
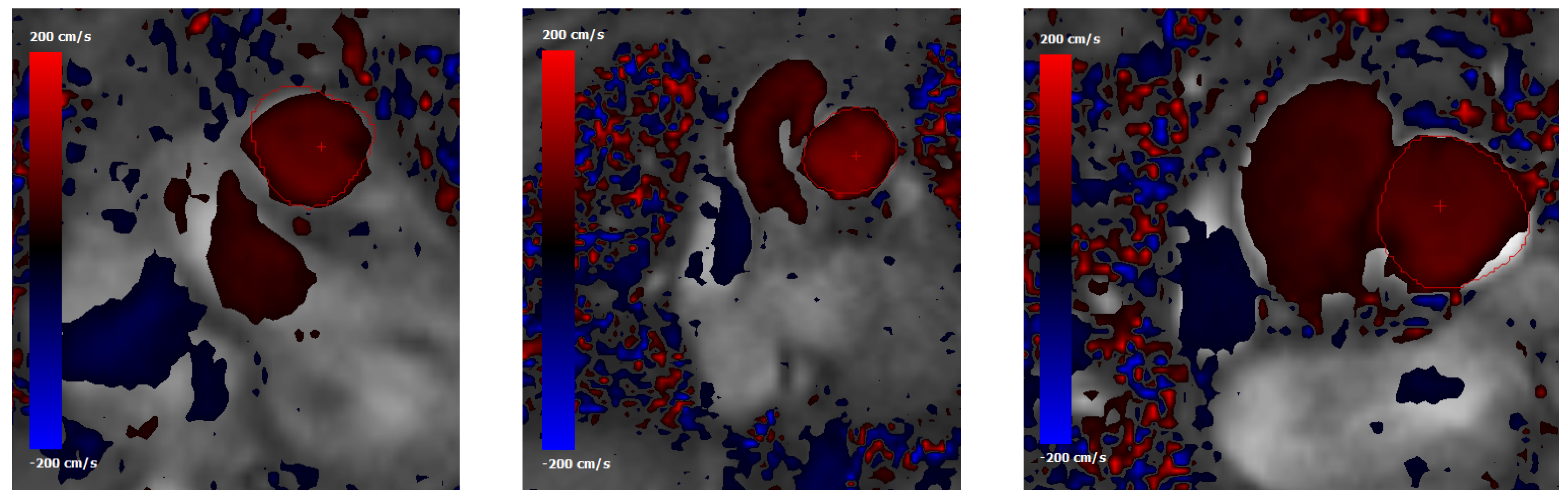
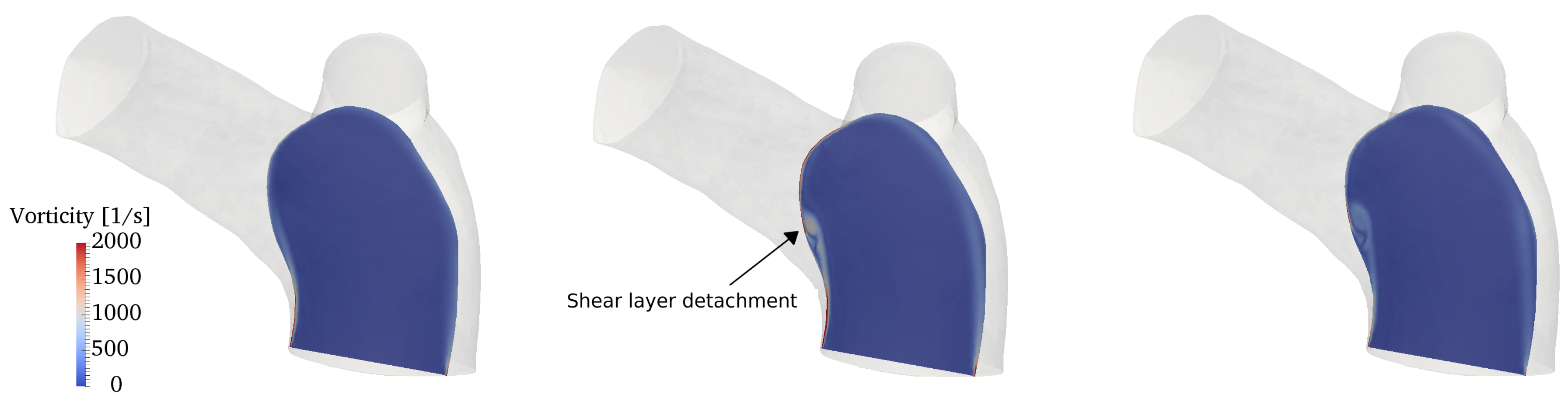
3.2. Phase-Averaged Statistics
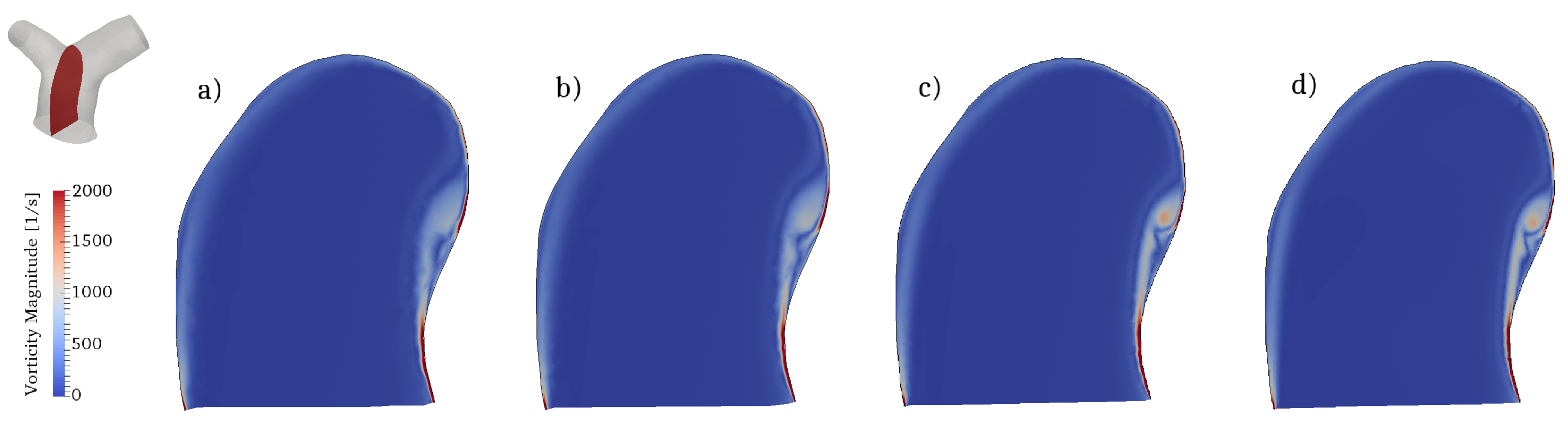
3.3. Vortex Dynamics
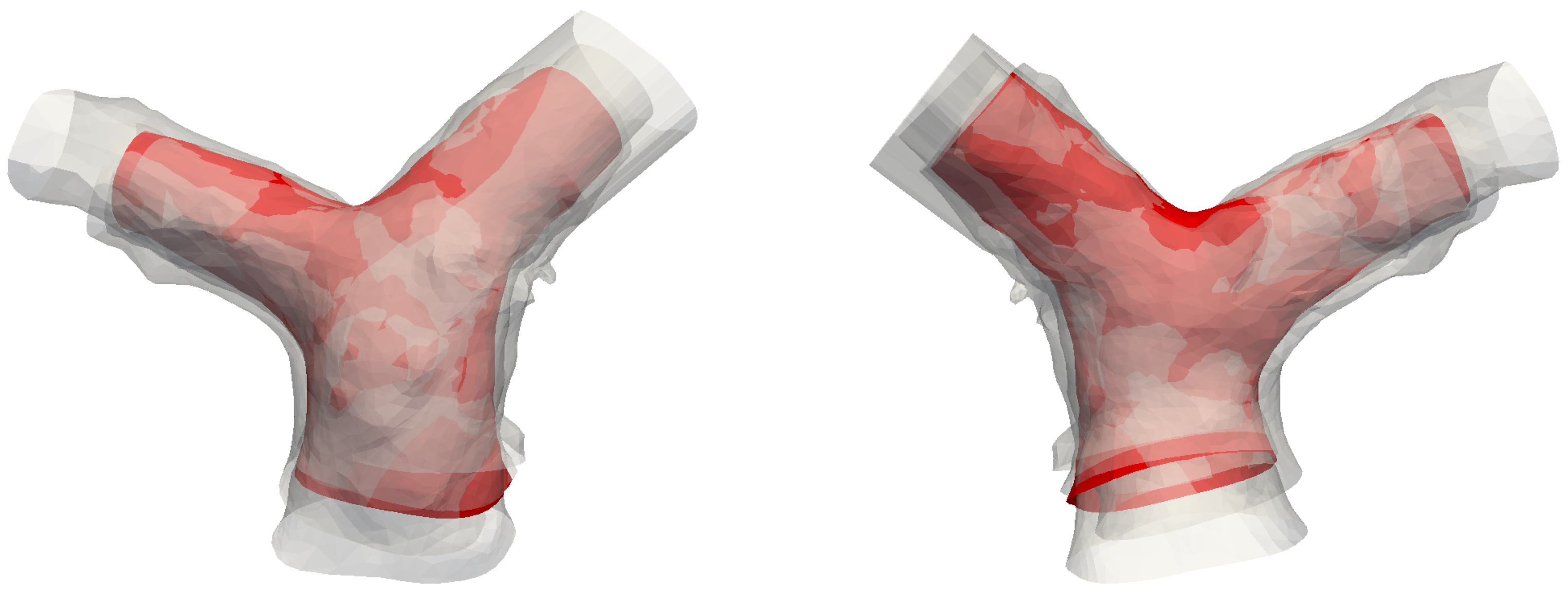
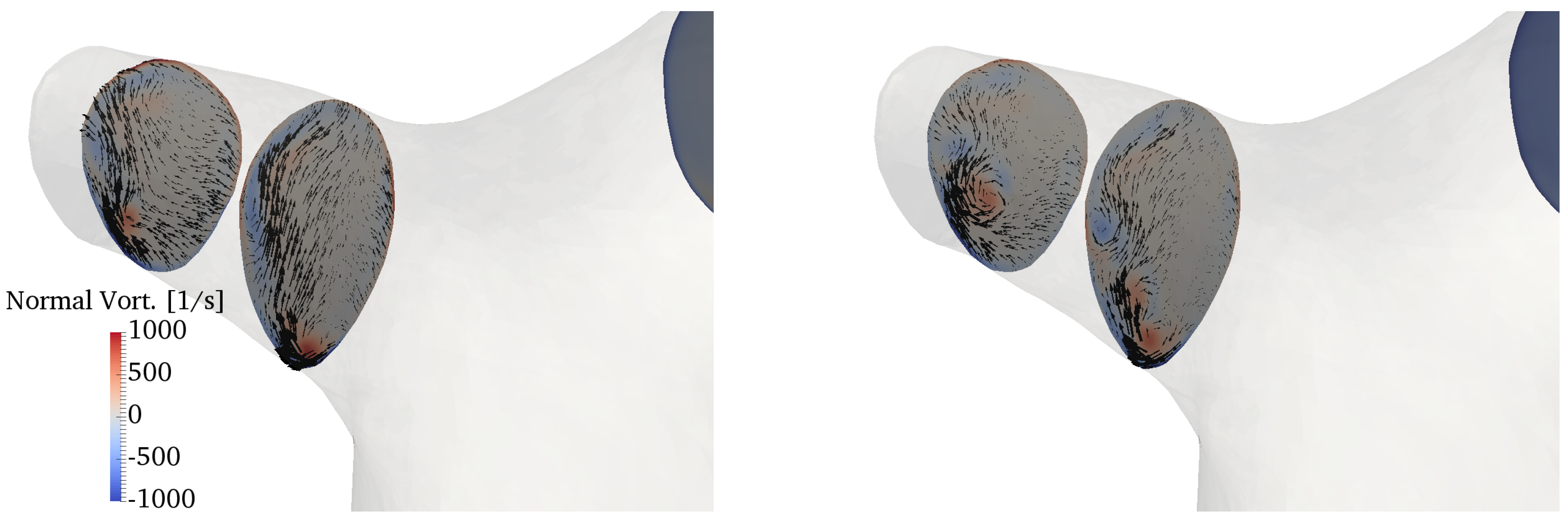
3.4. Secondary Motions
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| CFD | Computational Fluid Dynamics |
| CHD | Congenital Heart Disease |
| LPA | Left Pulmonary Artery |
| MPA | Main Pulmonary Artery |
| PA | Pulmonary Artery |
| RPA | Right Pulmonary Artery |
| RV | Right Ventricle |
| TGA | Transposition of Great Arteries |
| TOF | Tetralogy of Fallot |
| WSS | Wall Shear Stress |
Appendix A. Effects of Domain Size and Inflow Profile
Appendix A.1. Domain Size


Appendix A.2. Inflow Boundary Conditions
- a plug flow profile, based on the in-vivo flow rate waveform;
- a plug profile with superposition of a swirl component of 10%;
- a plug profile with superposition of a swirl component of 30%;
- a parabolic, Poiseuille-like profile.
References
- Caro, C.G.; Pedley, T.; Schroter, R.; Seed, W. The Mechanics of the Circulation; Cambridge University Press: Cambridge, UK, 2012. [Google Scholar]
- Hanna, B.D. Blood flow in normal and diseased pulmonary arteries. In Ventricular Function and Blood Flow in Congenital Heart Disease; Wiley-Blackwell: Hoboken, NJ, USA, 2005; pp. 275–285. [Google Scholar]
- Hoffman, J.I.; Kaplan, S. The incidence of congenital heart disease. J. Am. Coll. Cardiol. 2002, 39, 1890–1900. [Google Scholar] [CrossRef]
- Marsden, A.L. Simulation based planning of surgical interventions in pediatric cardiology. Phys. Fluids 2013, 25, 101303. [Google Scholar] [CrossRef] [PubMed]
- Ntsinjana, H.N.; Capelli, C.; Biglino, G.; Cook, A.C.; Tann, O.; Derrick, G.; Taylor, A.M.; Schievano, S. 3D morphometric analysis of the arterial switch operation using in vivo MRI data. Clin. Anat. 2014, 27, 1212–1222. [Google Scholar] [CrossRef] [PubMed]
- Capuano, F.; Loke, Y.H.; Cronin, I.; Olivieri, L.J.; Balaras, E. Computational Study of Pulmonary Flow Patterns after Repair of Transposition of Great Arteries. J. Biomech. Eng. 2019, 141, 051008. [Google Scholar] [CrossRef] [PubMed]
- Loke, Y.H.; Capuano, F.; Mandell, J.; Cross, R.R.; Cronin, I.; Mass, P.; Balaras, E.; Olivieri, L.J. Abnormal Pulmonary Artery Bending Correlates With Increased Right Ventricular Afterload Following the Arterial Switch Operation. World J. Pediatr. Congenit. Heart Surg. 2019, 10, 572–581. [Google Scholar] [CrossRef] [PubMed]
- Sanz, J.; Sánchez-Quintana, D.; Bossone, E.; Bogaard, H.J.; Naeije, R. Anatomy, function, and dysfunction of the right ventricle: JACC state-of-the-art review. J. Am. Coll. Cardiol. 2019, 73, 1463–1482. [Google Scholar] [CrossRef]
- Dohlen, G.; Chaturvedi, R.R.; Benson, L.N.; Ozawa, A.; Van Arsdell, G.S.; Fruitman, D.S.; Lee, K.J. Stenting of the right ventricular outflow tract in the symptomatic infant with tetralogy of Fallot. Heart 2009, 95, 142–147. [Google Scholar] [CrossRef]
- Nakata, S.; Imai, Y.; Takanashi, Y.; Kurosawa, H.; Tezuka, K.; Nakazawa, M.; Ando, M.; Takao, A. A new method for the quantitative standardization of cross-sectional areas of the pulmonary arteries in congenital heart diseases with decreased pulmonary blood flow. J. Thorac. Cardiovasc. Surg. 1984, 88, 610–619. [Google Scholar]
- Morgan, V.L.; Roselli, R.J.; Lorenz, C.H. Normal three-dimensional pulmonary artery flow determined by phase contrast magnetic resonance imaging. Ann. Biomed. Eng. 1998, 26, 557–566. [Google Scholar] [CrossRef]
- Sloth, E.; Houlind, K.C.; Oyre, S.; Kim, W.Y.; Pedersen, E.M.; Jørgensen, H.S.; Hasenkam, J.M. Three-dimensional visualization of velocity profiles in the human main pulmonary artery with magnetic resonance phase-velocity mapping. Am. Heart J. 1994, 128, 1130–1138. [Google Scholar] [CrossRef]
- Reiter, G.; Reiter, U.; Kovacs, G.; Kainz, B.; Schmidt, K.; Maier, R.; Olschewski, H.; Rienmueller, R. Magnetic resonance-derived 3-dimensional blood flow patterns in the main pulmonary artery as a marker of pulmonary hypertension and a measure of elevated mean pulmonary arterial pressure. Circ. Cardiovasc. Imaging 2008, 1, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Tang, B.T.; Fonte, T.A.; Chan, F.P.; Tsao, P.S.; Feinstein, J.A.; Taylor, C.A. Three-dimensional hemodynamics in the human pulmonary arteries under resting and exercise conditions. Ann. Biomed. Eng. 2011, 39, 347–358. [Google Scholar] [CrossRef] [PubMed]
- Bächler, P.; Pinochet, N.; Sotelo, J.; Crelier, G.; Irarrazaval, P.; Tejos, C.; Uribe, S. Assessment of normal flow patterns in the pulmonary circulation by using 4D magnetic resonance velocity mapping. Magn. Reson. Imaging 2013, 31, 178–188. [Google Scholar] [CrossRef]
- Tang, T.; Chiu, S.; Chen, H.C.; Cheng, K.Y.; Chen, S.J. Comparison of pulmonary arterial flow phenomena in spiral and Lecompte models by computational fluid dynamics. J. Thorac. Cardiovasc. Surg. 2001, 122, 529–534. [Google Scholar] [CrossRef] [PubMed]
- Geiger, J.; Hirtler, D.; Bürk, J.; Stiller, B.; Arnold, R.; Jung, B.; Langer, M.; Markl, M. Postoperative pulmonary and aortic 3D haemodynamics in patients after repair of transposition of the great arteries. Eur. Radiol. 2014, 24, 200–208. [Google Scholar] [CrossRef] [PubMed]
- Riesenkampff, E.; Nordmeyer, S.; Al-Wakeel, N.; Kropf, S.; Kutty, S.; Berger, F.; Kuehne, T. Flow-sensitive four-dimensional velocity-encoded magnetic resonance imaging reveals abnormal blood flow patterns in the aorta and pulmonary trunk of patients with transposition. Cardiol. Young 2014, 24, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Rickers, C.; Kheradvar, A.; Sievers, H.H.; Falahatpisheh, A.; Wegner, P.; Gabbert, D.; Jerosch-Herold, M.; Hart, C.; Voges, I.; Putman, L.M.; et al. Is the Lecompte technique the last word on transposition of the great arteries repair for all patients? A magnetic resonance imaging study including a spiral technique two decades postoperatively. Interact. Cardiovasc. Thorac. Surg. 2016, 22, 817–825. [Google Scholar] [CrossRef]
- Geiger, J.; Markl, M.; Jung, B.; Grohmann, J.; Stiller, B.; Langer, M.; Arnold, R. 4D-MR flow analysis in patients after repair for tetralogy of Fallot. Eur. Radiol. 2011, 21, 1651–1657. [Google Scholar] [CrossRef]
- Zhang, W.; Liu, J.; Yan, Q.; Liu, J.; Hong, H.; Mao, L. Computational haemodynamic analysis of left pulmonary artery angulation effects on pulmonary blood flow. Interact. Cardiovasc. Thorac. Surg. 2016, 23, 519–525. [Google Scholar] [CrossRef]
- Jeong, D.; Anagnostopoulos, P.V.; Roldan-Alzate, A.; Srinivasan, S.; Schiebler, M.L.; Wieben, O.; Francois, C.J. Ventricular kinetic energy may provide a novel noninvasive way to assess ventricular performance in patients with repaired tetralogy of Fallot. J. Thorac. Cardiovasc. Surg. 2015, 149, 1339–1347. [Google Scholar] [CrossRef]
- Boumpouli, M.; Danton, M.; Gourlay, T.; Kazakidi, A. Hemodynamics in the pulmonary bifurcation in relation to adults with congenital heart disease: Effect of branching angle and origin. In Proceedings of the 6th European Conference on Computational Mechanics and 7th European Conference on Computational Fluid Dynamics 2018, Glasgow, UK, 11–15 June 2018; pp. 1–12. [Google Scholar]
- Dean, W. The stream-line motion of fluid in a curved pipe. Lond. Edinb. Dublin Philos. Mag. J. Sci. 1928, 5, 673–695. [Google Scholar] [CrossRef]
- Lyne, W. Unsteady viscous flow in a curved pipe. J. Fluid Mech. 1971, 45, 13–31. [Google Scholar] [CrossRef]
- Berger, S.; Talbot, L.; Yao, L. Flow in curved pipes. Annu. Rev. Fluid Mech. 1983, 15, 461–512. [Google Scholar] [CrossRef]
- Plesniak, M.W.; Bulusu, K.V. Morphology of Secondary Flows in a Curved Pipe With Pulsatile Inflow. J. Fluids Eng. 2016, 138, 101203. [Google Scholar] [CrossRef]
- Canton, J.; Örlü, R.; Schlatter, P. Characterisation of the steady, laminar incompressible flow in toroidal pipes covering the entire curvature range. Int. J. Heat Fluid Flow 2017, 66, 95–107. [Google Scholar] [CrossRef]
- Najjari, M.R.; Plesniak, M.W. Secondary flow vortical structures in a 180° elastic curved vessel with torsion under steady and pulsatile inflow conditions. Phys. Rev. Fluids 2018, 3, 013101. [Google Scholar] [CrossRef]
- Fernandez, R.C.; De Witt, K.; Botwin, M. Pulsatile flow through a bifurcation with applications to arterial disease. J. Biomech. 1976, 9, 575–580. [Google Scholar] [CrossRef]
- Patil, M.K.; Subbaraj, K. Finite element analysis of two dimensional steady flow in model arterial bifurcation. J. Biomech. 1988, 21, 219–233. [Google Scholar] [CrossRef]
- Ku, D.N. Blood flow in arteries. Annu. Rev. Fluid Mech. 1997, 29, 399–434. [Google Scholar] [CrossRef]
- Durrleman, S.; Prastawa, M.; Charon, N.; Korenberg, J.R.; Joshi, S.; Gerig, G.; Trouvé, A. Morphometry of anatomical shape complexes with dense deformations and sparse parameters. NeuroImage 2014, 101, 35–49. [Google Scholar] [CrossRef]
- Durrleman, S. Deformetrica 4: An Open-Source Software for Statistical Shape Analysis. In Proceedings of the Shape in Medical Imaging: International Workshop, ShapeMI 2018, Held in Conjunction with MICCAI 2018, Granada, Spain, 20 September 2018; Springer: Berlin/Heidelberg, Germany, 2018; Volume 11167, p. 3. [Google Scholar]
- Bruse, J.L.; Khushnood, A.; McLeod, K.; Biglino, G.; Sermesant, M.; Pennec, X.; Taylor, A.M.; Hsia, T.Y.; Schievano, S.; Khambadkone, S.; et al. How successful is successful? Aortic arch shape after successful aortic coarctation repair correlates with left ventricular function. J. Thorac. Cardiovasc. Surg. 2017, 153, 418–427. [Google Scholar] [CrossRef] [PubMed]
- Guibert, R.; Mcleod, K.; Caiazzo, A.; Mansi, T.; Fernández, M.A.; Sermesant, M.; Pennec, X.; Vignon-Clementel, I.E.; Boudjemline, Y.; Gerbeau, J.F. Group-wise construction of reduced models for understanding and characterization of pulmonary blood flows from medical images. Med. Image Anal. 2014, 18, 63–82. [Google Scholar] [CrossRef] [PubMed]
- Knobel, Z.; Kellenberger, C.J.; Kaiser, T.; Albisetti, M.; Bergsträsser, E.; Buechel, E.R.V. Geometry and dimensions of the pulmonary artery bifurcation in children and adolescents: Assessment in vivo by contrast-enhanced MR-angiography. Int. J. Cardiovasc. Imaging 2011, 27, 385–396. [Google Scholar] [CrossRef] [PubMed]
- Gori, P.; Colliot, O.; Marrakchi-Kacem, L.; Worbe, Y.; Poupon, C.; Hartmann, A.; Ayache, N.; Durrleman, S. A Bayesian framework for joint morphometry of surface and curve meshes in multi-object complexes. Med. Image Anal. 2017, 35, 458–474. [Google Scholar] [CrossRef]
- Antiga, L.; Piccinelli, M.; Botti, L.; Ene-Iordache, B.; Remuzzi, A.; Steinman, D.A. An image-based modeling framework for patient-specific computational hemodynamics. Med. Biol. Eng. Comput. 2008, 46, 1097. [Google Scholar] [CrossRef]
- Piccinelli, M.; Veneziani, A.; Steinman, D.A.; Remuzzi, A.; Antiga, L. A framework for geometric analysis of vascular structures: application to cerebral aneurysms. IEEE Trans. Med. Imaging 2009, 28, 1141–1155. [Google Scholar] [CrossRef]
- Caro, C.G.; Doorly, D.J.; Tarnawski, M.; Scott, K.T.; Long, Q.; Dumoulin, C.L. Non-planar curvature and branching of arteries and non-planar-type flow. Proc. R. Soc. Lond. Ser. A Math. Phys. Eng. Sci. 1996, 452, 185–197. [Google Scholar]
- Kheyfets, V.; O’Dell, W.; Smith, T.; Reilly, J.; Finol, E. Considerations for numerical modeling of the pulmonary circulation—a review with a focus on pulmonary hypertension. J. Biomech. Eng. 2013, 135, 061011. [Google Scholar] [CrossRef]
- Grinberg, L.; Karniadakis, G.E. Outflow boundary conditions for arterial networks with multiple outlets. Ann. Biomed. Eng. 2008, 36, 1496–1514. [Google Scholar] [CrossRef]
- Vignon-Clementel, I.E.; Figueroa, C.A.; Jansen, K.E.; Taylor, C.A. Outflow boundary conditions for three-dimensional finite element modeling of blood flow and pressure in arteries. Comput. Methods Appl. Mech. Eng. 2006, 195, 3776–3796. [Google Scholar] [CrossRef]
- Cheng, C.P.; Taur, A.S.; Lee, G.S.; Goris, M.L.; Feinstein, J.A. Relative lung perfusion distribution in normal lung scans: observations and clinical implications. Congenit. Heart Dis. 2006, 1, 210–216. [Google Scholar] [CrossRef] [PubMed]
- Zambrano, B.A.; McLean, N.A.; Zhao, X.; Tan, J.L.; Zhong, L.; Figueroa, C.A.; Lee, L.C.; Baek, S. Image-based computational assessment of vascular wall mechanics and hemodynamics in pulmonary arterial hypertension patients. J. Biomech. 2018, 68, 84–92. [Google Scholar] [CrossRef] [PubMed]
- Jin, S.; Oshinski, J.; Giddens, D.P. Effects of wall motion and compliance on flow patterns in the ascending aorta. J. Biomech. Eng. 2003, 125, 347–354. [Google Scholar] [CrossRef] [PubMed]
- Perktold, K.; Rappitsch, G. Computer simulation of local blood flow and vessel mechanics in a compliant carotid artery bifurcation model. J. Biomech. 1995, 28, 845–856. [Google Scholar] [CrossRef]
- Updegrove, A.; Wilson, N.M.; Merkow, J.; Lan, H.; Marsden, A.L.; Shadden, S.C. Simvascular: An open source pipeline for cardiovascular simulation. Ann. Biomed. Eng. 2017, 45, 525–541. [Google Scholar] [CrossRef]
- Whiting, C.H.; Jansen, K.E. A stabilized finite element method for the incompressible Navier–Stokes equations using a hierarchical basis. Int. J. Numer. Methods Fluids 2001, 35, 93–116. [Google Scholar] [CrossRef]
- Kung, E.O.; Les, A.S.; Figueroa, C.A.; Medina, F.; Arcaute, K.; Wicker, R.B.; McConnell, M.V.; Taylor, C.A. In vitro validation of finite element analysis of blood flow in deformable models. Ann. Biomed. Eng. 2011, 39, 1947–1960. [Google Scholar] [CrossRef]
- Kung, E.; Kahn, A.M.; Burns, J.C.; Marsden, A. In vitro validation of patient-specific hemodynamic simulations in coronary aneurysms caused by Kawasaki disease. Cardiovasc. Eng. Technol. 2014, 5, 189–201. [Google Scholar] [CrossRef]
- Berger, S.; Jou, L.D. Flows in stenotic vessels. Annu. Rev. Fluid Mech. 2000, 32, 347–382. [Google Scholar] [CrossRef]
- Du, Z.; Roguin, N.; Barak, M.; Hershkowitz, S.; Milgram, E.; Brezins, M. Doppler echocardiographic study of the pulmonary artery and its branches in 114 normal neonates. Pediatr. Cardiol. 1997, 18, 38–42. [Google Scholar] [CrossRef]
- Giddens, D.P.; Tang, T.D.; Loth, F. Fluid mechanics of arterial bifurcations. In Biological Flows; Springer: Berlin/Heidelberg, Germany, 1995; pp. 51–68. [Google Scholar]
- Marsden, A.L.; Vignon-Clementel, I.E.; Chan, F.P.; Feinstein, J.A.; Taylor, C.A. Effects of exercise and respiration on hemodynamic efficiency in CFD simulations of the total cavopulmonary connection. Ann. Biomed. Eng. 2007, 35, 250–263. [Google Scholar] [CrossRef] [PubMed]
- Sievers, H.H.; Rickers, C. Nature is the best. J. Thorac. Cardiovasc. Surg. 2017, 154, 788–789. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hunt, J.; Wray, A.; Moin, P. Eddies, Streams, and Convergence Zones in Turbulent Flows; Technical Report CTR-S88; Center for Turbulence Research: Stanford, CA, USA, 1988. [Google Scholar]
- Anderson, R.H.; Mori, S.; Spicer, D.E.; Brown, N.A.; Mohun, T.J. Development and morphology of the ventricular outflow tracts. World J. Pediatr. Congenit. Heart Surg. 2016, 7, 561–577. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Sun, A.; Fan, Y.; Deng, X. Physiological significance of helical flow in the arterial system and its potential clinical applications. Ann. Biomed. Eng. 2015, 43, 3–15. [Google Scholar] [CrossRef]
- Markl, M.; Kilner, P.J.; Ebbers, T. Comprehensive 4D velocity mapping of the heart and great vessels by cardiovascular magnetic resonance. J. Cardiovasc. Magn. Reson. 2011, 13, 7. [Google Scholar] [CrossRef]
- Bulusu, K.V.; Hussain, S.; Plesniak, M.W. Determination of secondary flow morphologies by wavelet analysis in a curved artery model with physiological inflow. Exp. Fluids 2014, 55, 1832. [Google Scholar] [CrossRef]
- Evegren, P.; Fuchs, L.; Revstedt, J. On the secondary flow through bifurcating pipes. Phys. Fluids 2010, 22, 103601. [Google Scholar] [CrossRef]
- Pedrizzetti, G.; Domenichini, F. Nature optimizes the swirling flow in the human left ventricle. Phys. Rev. Lett. 2005, 95, 108101. [Google Scholar] [CrossRef]
- Mangual, J.; Domenichini, F.; Pedrizzetti, G. Describing the highly three dimensional right ventricle flow. Ann. Biomed. Eng. 2012, 40, 1790–1801. [Google Scholar] [CrossRef]






| Subject | Age | Gender | BSA | ||||
|---|---|---|---|---|---|---|---|
| #1 | 4 | M | 0.65 | 161 | 67 | 69 | 2.5 |
| #2 | 5 | F | 0.83 | 206 | 118 | 107 | 4.4 |
| #3 | 11 | F | 1.33 | 184 | 98 | 132 | 3.3 |
| #4 | 15 | F | 1.57 | 295 | 116 | 129 | 4.1 |
| #5 | 18 | F | 1.74 | 448 | 168 | 127 | 5.3 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Capuano, F.; Loke, Y.-H.; Balaras, E. Blood Flow Dynamics at the Pulmonary Artery Bifurcation. Fluids 2019, 4, 190. https://doi.org/10.3390/fluids4040190
Capuano F, Loke Y-H, Balaras E. Blood Flow Dynamics at the Pulmonary Artery Bifurcation. Fluids. 2019; 4(4):190. https://doi.org/10.3390/fluids4040190
Chicago/Turabian StyleCapuano, Francesco, Yue-Hin Loke, and Elias Balaras. 2019. "Blood Flow Dynamics at the Pulmonary Artery Bifurcation" Fluids 4, no. 4: 190. https://doi.org/10.3390/fluids4040190
APA StyleCapuano, F., Loke, Y.-H., & Balaras, E. (2019). Blood Flow Dynamics at the Pulmonary Artery Bifurcation. Fluids, 4(4), 190. https://doi.org/10.3390/fluids4040190





