Effects and Mechanisms of Tea Regulating Blood Pressure: Evidences and Promises
Abstract
1. Introduction
2. Tea Regulating Blood Pressure in Human Intervention Studies
2.1. Hypotension Effects of Tea in Human Population Studies by Meta-analysis
2.2. Interventional Trials for General Population
2.3. Interventional Trials for Obese and/or Hypertensive Populations
2.4. Interventional Trials for Diabetic Populations
2.5. Intervention Trials for Aging Populations
3. Tea Metabolites Regulating Blood Pressure in Animal Studies
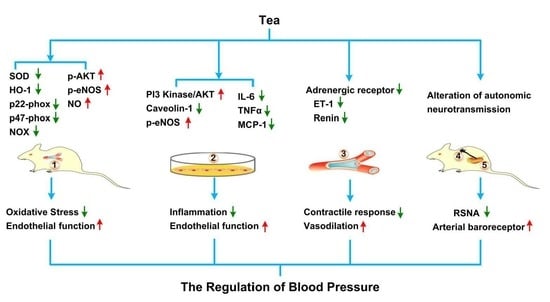
4. Molecular Mechanisms of Tea Regulating Blood Pressure
5. Discussion and Prospective
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Mendis, S.; Puska, P.; Norrving, B. Global Atlas on Cardiovascular Disease Prevention and Control; Geneva World Health Organizationn: Geneva, Switzerland, 2011. [Google Scholar]
- Townsend, N.; Wilson, L.; Bhatnagar, P.; Wickramasinghe, K.; Rayner, M.; Nichols, M. Cardiovascular disease in Europe: Epidemiological update 2016. Eur. Heart J. 2016, 37, 3232–3245. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.S.; Vos, T.; Flaxman, A.D. A comparative risk assessment of burden of disease and injury attributable to 67 risk factor clusters in 21 regions, 1990–2010: A systematic analysis for the global Burden of Disease Study 2010. Lancet 2012, 380, 2224–2260. [Google Scholar] [CrossRef]
- Conti, C.R. Diabetes, hypertension, and cardiovascular disease. Clin. Cardiol. 2001, 24, 1. [Google Scholar] [PubMed]
- Horst-Meyer, H.Z. Report on the World Health Organization Global Observatory for eHealth Strategic Planning Workshop. Meth. Inf. Med. 2008, 47, 381–387. [Google Scholar]
- Law, M.; Wald, N.; Morris, J. Lowering blood pressure to prevent myocardial infarction and stroke: A new preventive strategy. Int. J. Technol. Assess. Health Care 2005, 21, 145. [Google Scholar] [CrossRef]
- Qureshi, A.; Sapkota, B.L. Blood Pressure Reduction in Secondary Stroke Prevention. Continuum 2011, 17, 1233–1241. [Google Scholar] [CrossRef]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey Jr, D.E.; Collins, K.J.; Himmelfarb, C.D.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2017, 19, 213–221. [Google Scholar]
- Mozaffarian, D.; Benjamin, E.J.; Go, A.S.; Arnett, D.K.; Blaha, M.J.; Cushman, M.; Das, S.R.; de Ferranti, S.; Després, J.P.; Fullerton, H.J. Heart Disease and stroke statistics-2016 update a report from the American Heart Association. Circulation 2016, 133, e38–e48. [Google Scholar] [PubMed]
- World Health Organization. A Global Brief on Hypertension: Silent Killer, Global Public Health Crisis; Geneva World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- Macfarlane, A.; Macfarlane, I. The Empire of Tea; Overlook Press: New York, NY, USA, 2004. [Google Scholar]
- Heinrich, U.; Moore, C.E.; De Spirt, S.; Hagen, T.; Wilhelm, S. Green tea polyphenols provide photoprotection, increase microcirculation, and modulate skin properties of women. J. Nutr. 2012, 141, 1202–1208. [Google Scholar] [CrossRef]
- Cabrera, C.; Artacho, R.; Gimenez, R. Beneficial effects of green tea—A review. J. Am. Coll. Nutr. 2006, 25, 79–99. [Google Scholar]
- Hodgson, J.M.; Croft, K.D. Tea flavonoids and cardiovascular health. Mol. Asp. Med. 2010, 31, 495–502. [Google Scholar] [CrossRef] [PubMed]
- Chobanian, A.V.; Bakris, G.L.; Black, H.R.; Cushman, W.; Green, L.; Izzo, J.; Jones, D.; Materson, B.; Oparil, S.; Wright, J. Seven report of the joint national committee on prevention, detection, and treatment of high blood pressure. Hypertension 2003, 42, 1206–1252. [Google Scholar] [CrossRef]
- Hooper, L.; Kroon, P.A.; Rimm, E.B.; Cohn, J.S.; Harvey, I.; Kathryn, A.; Cornu, L.; Jonathan, J.R.; Hall, W.L.; Cassidy, A. Flavonoids, flavonoid-rich foods, and cardiovascular risk: A meta-analysis of randomized controlled trials. Am. J. Clin. Nutr. 2008, 88, 38–50. [Google Scholar] [CrossRef]
- Yang, C.S.; Hong, J. Prevention of chronic diseases by tea: Possible mechanisms and human relevance. Annu. Rev. Nutr. 2013, 33, 161–181. [Google Scholar] [CrossRef]
- Sang, S.; Lambert, J.D.; Ho, C.T.; Yang, C.S. The chemistry and biotransformation of tea constituents. Pharmacol. Res. 2011, 64, 87–99. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Zhang, Z.Z.; Zhou, Y.B.; Ling, T.J.; Wan, X.C. Chinese dark teas: Postfermentation, chemistry and biological activities. Food Res. Int. 2013, 53, 600–607. [Google Scholar] [CrossRef]
- Khalesi, S.; Sun, J.; Buys, N.; Jamshidi, A.; Nikbakht-Nasrabadi, E.; Khosravi-Boroujeni, H. Green tea catechins and blood pressure: A systematic review and meta-analysis of randomized controlled trials. Eur. J. Nutr. 2014, 53, 1299–1311. [Google Scholar] [CrossRef] [PubMed]
- Peng, X.; Zhou, R.; Wang, B.; Yu, X.; Yang, X.; Liu, K.; Mi, M. Effect of green tea consumption on blood pressure: A meta-analysis of 13 randomized controlled trials. Sci. Rep. 2014, 4, 6251. [Google Scholar] [CrossRef]
- Greyling, A.; Ras, R.T.; Zock, P.L.; Lorenz, M.; Hopman, M.T.; Thijssen, D.H.; Draijer, R. The effect of black tea on blood pressure: A systematic review with meta-analysis of randomized controlled trials. PLoS ONE 2014, 9, e103247. [Google Scholar] [CrossRef] [PubMed]
- Liu, G.; Mi, X.N.; Zheng, X.X.; Xu, Y.L.; Lu, J.; Huang, X.H. Effects of tea intake on blood pressure: A meta-analysis of randomised controlled trials. Br. J. Nutr. 2014, 112, 1043–1054. [Google Scholar] [CrossRef]
- Yarmolinsky, J.; Gon, G.; Edwards, P. Effect of tea on blood pressure for secondary prevention of cardiovascular disease: A systematic review and meta-analysis of randomized controlled trials. Nutr. Rev. 2015, 73, 236–246. [Google Scholar] [CrossRef] [PubMed]
- Kotsis, V.; Nilsson, P.; Grassi, G.; Mancia, G.; Redon, J.; Luft, F.; Schmieder, R.; Engeli, S.; Stabouli, S.; Antza, C.; et al. New developments in the pathogenesis of obesity-induced hypertension. J. Hypertens. 2015, 33, 1499–1508. [Google Scholar] [CrossRef] [PubMed]
- Hall, J.E.; do Carmo, J.M.; da Silva, A.A.; Wang, Z.; Hall, M.E. Obesity-induced hypertension: Interaction of neurohumoral and renal mechanisms. Circ. Res. 2015, 116, 991–1006. [Google Scholar] [CrossRef]
- Li, G.W.; Zhang, Y.; Thabane, L.; Liu, A.; Levine, M.A.; Holbrook, A. Effect of green tea supplementation on blood pressure among overweight and obese adults: A systematic review and meta-analysis. J. Hypertens. 2015, 33, 243–254. [Google Scholar] [CrossRef]
- Tong, X.; Taylor, A.; Giles, L.; Wittert, G.A.; Shi, Z. Tea consumption is inversely related to 5-year blood pressure change among adults in Jiangsu, China: A cross-sectional study. Nutr. J. 2014, 13, 98. [Google Scholar] [CrossRef][Green Version]
- Yang, Y.C.; Lu, F.H.; Wu, J.S.; Chang, C.J. The protective effect of habitual tea consumption on hypertension. Arch. Intern. Med. 2004, 164, 1534–1540. [Google Scholar] [CrossRef] [PubMed]
- Nantz, M.P.; Rowe, C.A.; Bukowski, J.F.; Percival, S.S. Standardized capsule of Camellia sinensis lowers cardiovascular risk factors in a randomized, double-blind, placebo-controlled study. Nutrition 2009, 25, 147–154. [Google Scholar] [CrossRef] [PubMed]
- Stensvold, I.; Tverdal, A.; Solvoll, K.; Foss, O.P. Tea consumption, relationship to cholesterol, blood pressure and coronary and total mortality. Prev. Med. 1992, 21, 546–553. [Google Scholar] [CrossRef]
- Hodgson, J.M.; Puddey, I.B.; Woodman, R.J.; Mulder, T.P.; Fuchs, D.; Scott, K.; Croft, K.D. Effects of black tea on blood pressure: A randomized controlled trial. Arch. Intern. Med. 2012, 172, 186–188. [Google Scholar] [CrossRef] [PubMed]
- Pinto, E. Blood pressure and aging. Postgrad. Med. J. 2007, 83, 109–114. [Google Scholar] [CrossRef]
- Hodgson, J.M.; Devine, A.; Puddey, I.B.; Chan, S.Y.; Beilin, L.J.; Prince, R.L. Tea intake is inversely related to blood pressure in older women. J. Nutr. 2003, 133, 2883–2886. [Google Scholar] [CrossRef]
- Yin, J.Y.; Duan, S.Y.; Liu, F.C.; Yao, Q.K.; Tu, S.; Xu, Y.; Pan, C.W. Blood Pressure Is Associated with Tea Consumption: A Cross-sectional Study in a Rural, Elderly Population of Jiangsu China. J. Nutr. Health Aging 2017, 21, 1151–1159. [Google Scholar] [CrossRef] [PubMed]
- Liao, D.; Arnett, D.; Tyroler, H.; Riley, W.A.; Chambless, L.E.; Szklo, M.; Heiss, G. Arterial Stiffness and the Development of Hypertension The ARIC Study. Hypertension 1999, 34, 201–206. [Google Scholar] [CrossRef]
- Lin, Q.F.; Qiu, C.S.; Wang, S.L.; Huang, L.F.; Chen, Z.Y.; Chen, Y.; Chen, G. A Cross-sectional Study of the Relationship Between Habitual Tea Consumption and Arterial Stiffness. J. Am. Coll. Nutr. 2016, 35, 354–361. [Google Scholar] [CrossRef] [PubMed]
- Nagao, T.; Hase, T.; Tokimitsu, I. A green tea extract high in catechins reduces body fat and cardiovascular risks in humans. Obesity (Silver Spring) 2007, 15, 1473–1483. [Google Scholar] [CrossRef] [PubMed]
- Brown, A.L.; Lane, J.; Coverly, J.; Stocks, J.; Jackson, S.; Stephen, A.; Bluck, L.; Coward, A.; Hendrickx, H. Effects of dietary supplementation with the green tea polyphenol epigallocatechin-3-gallate on insulin resistance and associated metabolic risk factors: Randomized controlled trial. Br. J. Nutr. 2009, 101, 886–894. [Google Scholar] [CrossRef] [PubMed]
- Nogueira, L.P.; Nogueira Neto, J.F.; Klein, M.R.; Sanjuliani, A.F. Short-term Effects of Green Tea on Blood Pressure, Endothelial Function, and Metabolic Profile in Obese Prehypertensive Women: A Crossover Randomized Clinical Trial. J. Am. Coll. Nutr. 2017, 36, 108–115. [Google Scholar] [CrossRef]
- Bogdanski, P.; Suliburska, J.; Szulinska, M.; Stepien, M.; Pupek-Musialik, D.; Jablecka, A. Green tea extract reduces blood pressure, inflammatory biomarkers, and oxidative stress and improves parameters associated with insulin resistance in obese, hypertensive patients. Nutr. Res. 2012, 32, 421–427. [Google Scholar] [CrossRef]
- Grassi, D.; Draijer, R.; Desideri, G.; Mulder, T.; Ferri, C. Black tea lowers blood pressure and wave reflections in fasted and postprandial conditions in hypertensive patients: A randomized study. Nutrients 2015, 7, 1037–1051. [Google Scholar] [CrossRef]
- Ferrannini, E.; Cushman, W.C. Diabetes and hypertension: The bad companions. Lancet 2012, 380, 601–610. [Google Scholar] [CrossRef]
- Mozaffari-Khosravi, H.; Ahadi, Z.; Barzegar, K. The effect of green tea and sour tea on blood pressure of patients with type 2 diabetes: A randomized clinical trial. J. Diet. Suppl. 2013, 10, 105–115. [Google Scholar] [CrossRef] [PubMed]
- Fukino, Y.; Ikeda, A.; Maruyama, K.; Aoki, N.; Okubo, T.; Iso, H. Randomized controlled trial for an effect of green tea-extract powder supplementation on glucose abnormalities. Eur. J. Clin. Nutr. 2008, 62, 953–960. [Google Scholar] [CrossRef] [PubMed]
- Henry, J.P.; Stephenes-Larson, P. Reduction of chronic psychosocial hypertension in mice by decaffeinated tea. Hypertension 1984, 6, 437–444. [Google Scholar] [CrossRef]
- Negishi, H.; Xu, J.W.; Ikeda, K.; Njelekela, M.; Nara, Y.; Yamori, Y. Black and Green Tea Polyphenols Attenuate Blood Pressure Increases in Stroke-Prone Spontaneously Hypertensive Rats. J. Nutr. 2004, 134, 38–42. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.S.; Chen, L.; Lee, M.J.; Balentine, D.; Kuo, M.C.; Schantz, S.P. Blood and urine levels of tea catechins after ingestion of different amounts of green tea by human volunteers. Cancer Epidemiol. Biomark. Prev. 1998, 7, 351–354. [Google Scholar]
- Potenza, M.A.; Marasciulo, F.L.; Tarquinio, M.; Tiravanti, E.; Colantuono, G.; Federici, A.; Kim, J.A.; Quon, M.J.; Montagnani, M. EGCG, a green tea polyphenol, improves endothelial function and insulin sensitivity, reduces blood pressure, and protects against myocardial I/R injury in SHR. Am. J. Physiol. Endocrinol. Metab. 2007, 292, E1378–E1387. [Google Scholar] [CrossRef] [PubMed]
- Igarashi, K.; Honma, K.; Yoshinari, O.; Nanjo, F.; Hara, Y. Effects of dietary catechins on glucose tolerance, blood pressure and oxidative status in Goto-Kakizaki rats. J. Nutr. Sci. Vitaminol. (Tokyo) 2007, 53, 496–500. [Google Scholar] [CrossRef] [PubMed]
- Yasuhiko, A.; Satoshi, U.; Koh-Ichi, S.; Hirawa, N.; Kato, Y.; Yokoyama, N.; Yokoyama, T.; Iwai, J.; Ishii, M. Effect of green tea rich in γ-aminobutyric acid on blood pressure of Dahl salt-sensitive rats. Am. J. Hypertens. 1995, 8, 74–79. [Google Scholar]
- Yokogoshi, H.; Kobayashi, M. Hypotensive effect of γ-glutamylmethylamide glutamic acid in spontaneously hypertensive rats. Life Sci. 1998, 62, 1065–1068. [Google Scholar] [CrossRef]
- Coşan, D.T.; Saydam, F.; Özbayer, C.; Doğaner, F.; Soyocak, A.; Güneş, H.V.; Değirmenci, İ.; Kurt, H.; Üstüner, M.C.; Bal, C. Impact of tannic acid on blood pressure, oxidative stress and urinary parameters in L-NNA-induced hypertensive rats. Cytotechnology 2015, 67, 97–105. [Google Scholar] [CrossRef] [PubMed]
- Sagesaka-Mitane, Y.; Sugiura, T.; Miwa, Y.; Yamaguchi, K.; Kyuki, K. Effect of tea-leaf saponin on blood pressure of spontaneously hypertensive rats. Yakugaku Zasshi 1996, 116, 388–395. [Google Scholar] [CrossRef]
- Griendling, K.K.; Alexander, R.W. Oxidative stress and cardiovascular disease. Circulation 1997, 96, 3264–3265. [Google Scholar] [PubMed]
- Rajagopalan, S.; Kurz, S.; Munzel, T.; Tarpey, M.; Freeman, B.A.; Griendling, K.K.; Harrison, D.G. Angiotensin II-mediated hypertension in the rat increases vascular superoxide production via membrane NADH/NADPH oxidase activation: Contribution to alterations of vasomotor tone. J. Clin. Investig. 1996, 97, 1916–1923. [Google Scholar] [CrossRef] [PubMed]
- Pagano, P.J.; Clark, J.K.; Cifuentes-Pagano, M.E.; Clark, S.M.; Callis, G.M.; Quinn, M.T. Localization of a constitutively active, phagocyte-like NADPH oxidase in rabbit aortic adventitia: Enhancement by angiotensin II. Proc. Natl. Acad. Sci. USA 1997, 94, 14483–14488. [Google Scholar] [CrossRef]
- Wu, R.; Millette, E.; Wu, L.; de Champlain, J. Enhanced superoxide anion formation in vascular tissues from spontaneously hypertensive and desoxycorticosterone acetate-salt hypertensive rats. J. Hypertens. 2001, 19, 741–748. [Google Scholar] [CrossRef]
- Beswick, R.A.; Dorrance, A.M.; Leite, R.; Webb, R.C. NADH/NADPH oxidase and enhanced superoxide production in the mineralocorticoid hypertensive rat. Hypertension 2001, 38, 1107–1111. [Google Scholar] [CrossRef]
- Antonello, M.; Montemurro, D.; Bolognesi, M.; Di, P.M.; Piva, A.; Grego, F.; Sticchi, D.; Giuliani, L.; Garbisa, S.; Rossi, G.P. Prevention of hypertension, cardiovascular damage and endothelial dysfunction with green tea extracts. Am. J. Hypertens. 2007, 20, 1321–1328. [Google Scholar] [CrossRef]
- Ihm, S.H.; Jang, S.W.; Kim, O.R.; Chang, K.; Oak, M.H.; Lee, J.O.; Lim, D.Y.; Kim, J.H. Decaffeinated green tea extract improves hypertension and insulin resistance in a rat model of metabolic syndrome. Atherosclerosis 2012, 224, 377–383. [Google Scholar] [CrossRef]
- Gómez-Guzmán, M.; Jiménez, R.; Sánchez, M.; Zarzuelo, M.J.; Galindo, P.; Quintela, A.M.; López-Sepúlveda, R.; Romero, M.; Tamargo, J.; Vargas, F.; et al. Epicatechin lowers blood pressure, restores endothelial function, and decreases oxidative stress and endothelin-1 and NADPH oxidase activity in DOCA-salt hypertension. Free Radic. Biol. Med. 2012, 52, 70–79. [Google Scholar] [CrossRef] [PubMed]
- Galleano, M.; Bernatova, I.; Puzserova, A.; Balis, P.; Sestakova, N.; Pechanova, O.; Fraga, C.G. (-)-Epicatechin reduces blood pressure and improves vasorelaxation in spontaneously hypertensive rats by NO-mediated mechanism. IUBMB Life 2013, 65, 710–715. [Google Scholar] [CrossRef]
- Litterio, M.C.; Jaggers, G.; Celep, G.S.; Adamo, A.M.; Costa, M.A.; Oteiza, P.I.; Fraga, C.G.; Galleano, M. Blood pressure-lowering effect of dietary (-)-epicatechin administration in L-NAME-treated rats is associated with restored nitric oxide levels. Free Radic. Biol. Med. 2012, 53, 1894–1902. [Google Scholar] [CrossRef]
- Tanida, M.; Tsuruoka, N.; Shen, J.; Kiso, Y.; Nagai, K. Effects of oolong tea on renal sympathetic nerve activity and spontaneous hypertension in rats. Metabolism 2008, 57, 526–534. [Google Scholar] [CrossRef]
- Han, J.Y.; Kim, C.S.; Lim, K.H.; Kim, J.H.; Kim, S.; Yun, Y.P.; Hong, J.T.; Oh, K.W. Increases in blood pressure and heart rate induced by caffeine are inhibited by (-)-epigallocatechin-3-O-gallate: Involvement of catecholamines. J. Cardiovasc. Pharmacol. 2011, 58, 446–449. [Google Scholar] [CrossRef] [PubMed]
- Garcia, M.L.; Pontes, R.B.; Nishi, E.E.; Ibuki, F.K.; Oliveira, V.; Sawaya, A.C.; Carvalho, P.O.; Nogueira, F.N.; Franco, M.D.; Campos, R.R.; et al. The antioxidant effects of green tea reduces blood pressure and sympathoexcitation in an experimental model of hypertension. J. Hypertens. 2017, 35, 348–354. [Google Scholar] [CrossRef] [PubMed]
- Anter, E.; Thomas, S.R.; Schulz, E.; Shapira, O.M.; Vita, J.A.; Keaney, J.F. Activation of endothelial nitric-oxide synthase by the p38 MAPK in response to black tea polyphenols. J. Biol. Chem. 2004, 279, 46637–46643. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Ying, C.; Zuo, X.; Yi, H.; Yi, W.; Meng, Y.; Ikeda, K.; Ye, X.; Yamori, Y.; Sun, X. Green tea polyphenols down-regulate caveolin-1 expression via ERK1/2 and p38MAPK in endothelial cells. J. Nutr. Biochem. 2009, 20, 1021–1027. [Google Scholar] [CrossRef]
- Ramirez-Sanchez, I.; Aguilar, H.; Ceballos, G.; Villarreal, F. (-)-Epicatechin-induced calcium independent eNOS activation: Roles of HSP90 and AKT. Mol. Cell. Biochem. 2012, 370, 141–150. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.A.; Formoso, G.; Li, Y.; Potenza, M.A.; Marasciulo, F.L.; Montagnani, M.; Quon, M.J. Epigallocatechin gallate, a green tea polyphenol, mediates NO-dependent vasodilation using signaling pathways in vascular endothelium requiring reactive oxygen species and Fyn. J. Biol. Chem. 2007, 282, 13736–13745. [Google Scholar] [CrossRef] [PubMed]
- Guo, B.C.; Wei, J.; Su, K.H.; Chiang, A.N.; Zhao, J.F.; Chen, H.Y.; Shyue, S.K.; Lee, T.S. Transient receptor potential vanilloid type 1 is vital for (-)-epigallocatechin-3-gallate mediated activation of endothelial nitric oxide synthase. Mol. Nutr. Food Res. 2015, 59, 646–657. [Google Scholar] [CrossRef]
- Lim, D.Y.; Lee, E.S.; Park, H.G.; Kim, B.C.; Hong, S.P.; Lee, E.B. Comparison of Green Tea Extract and Epigallocatechin Gallate on Blood Pressure and Contractile Responses of Vascular Smooth Muscle of Rats. Arch. Pharm. Res. 2003, 26, 214–223. [Google Scholar] [CrossRef]
- Letizia, C.; Cerci, S.; De Toma, G.; D’Ambrosio, C.; De Ciocchis, A.; Coassin, S.; Scavo, D. High plasma endothelin-1 levels in hypertensive patients with low renin essential hypertension. J. Hum Hypertens. 1997, 11, 447–451. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Ohnishi-Kameyama, M.; Takahashi, Y.; Yamaki, K. Tea polyphenols as novel and potent inhibitory substances against renin activity. J Agric. Food Chem. 2013, 61, 9697–9704. [Google Scholar] [CrossRef]
- Soltani, S.; Chitsazi, M.J.; Salehi-Abargouei, A. The effect of dietary approaches to stop hypertension (DASH) on serum inflammatory markers: A systematic review and meta-analysis of randomized trials. Clin. Nutr. 2018, 37, 542–550. [Google Scholar] [CrossRef]
- Savoia, C.; Schiffrin, E.L. Vascular inflammation in hypertension and diabetes: Molecular mechanisms and therapeutic interventions. Clin. Sci. 2007, 112, 375–384. [Google Scholar] [CrossRef] [PubMed]
- Mahajan, N.; Dhawan, V.; Sharma, G.; Jain, S.; Kaul, D. Induction of inflammatory gene expression by THP-1 macrophages cultured in normocholesterolaemic hypertensive sera and modulatory effects of green tea polyphenols. J. Hum. Hypertens. 2008, 22, 141–143. [Google Scholar] [CrossRef]
- Ahn, H.Y.; Xu, Y.; Davidge, S.T. Epigallocatechin-3-O-gallate inhibits TNFalpha-induced monocyte chemotactic protein-1 production from vascular endothelial cells. Life Sci. 2008, 82, 964–968. [Google Scholar] [CrossRef] [PubMed]
- Elijovich, F.; Laffer, C.L.; Amador, E.; Gavras, H.; Bresnahan, M.R.; Schiffrin, E.L. Regulation of plasma endothelin by salt in salt-sensitive hypertension. Circulation 2001, 103, 263–268. [Google Scholar] [CrossRef]
- Li, L.; Fink, G.D.; Watts, S.W.; Northcott, C.A.; Galligan, J.J.; Pagano, P.J.; Chen, A.F. Endothelin-1 increases vascular superoxide via endothelin(A)–NADPH oxidase pathway in low-renin hypertension. Circulation 2003, 107, 1053–1058. [Google Scholar] [CrossRef] [PubMed]
- Jiménez, R.; López-Sepúlveda, R.; Kadmiri, M.; Romero, M.; Vera, R.; Sánchez, M.; Vargas, F.; O’Valle, F.; Zarzuelo, A.; Dueñas, M.; et al. Polyphenols restore endothelial function in DOCA-salt hypertension: Role of endothelin-1 and NADPH oxidase. Free Radic. Biol. Med. 2007, 43, 462–473. [Google Scholar] [CrossRef]
- Nicholson, S.K.; Tucker, G.A.; Brameld, J.M. Physiological concentrations of dietary polyphenols regulate vascular endothelial cell expression of genes important in cardiovascular health. Br. J. Nutr. 2010, 103, 1398–1403. [Google Scholar] [CrossRef]
- Reiter, C.E.; Kim, J.A.; Quon, M.J. Green tea polyphenol epigallocatechin gallate reduces endothelin-1 expression and secretion in vascular endothelial cells: Roles for AMP-activated protein kinase, Akt, and FOXO1. Endocrinology 2010, 151, 103–114. [Google Scholar] [CrossRef] [PubMed]
- Hodgson, J.M.; Puddey, I.B.; Burke, V.; Beilin, L.J.; Jordan, N. Effects on blood pressure of drinking green and black tea. J Hypertens. 1999, 17, 457–463. [Google Scholar] [CrossRef] [PubMed]
- Rakic, V.; Beilin, L.J.; Burke, V. Effect of coffee and tea drinking on postprandial hypotension in older men and women. Clin. Exp. Pharmacol. Physiol. 1996, 23, 559–563. [Google Scholar] [CrossRef]
- Bingham, S.A.; Vorster, H.; Jerling, J.C.; Magee, E.; Mulligan, A.; Runswick, S.A.; Cummings, J.H. Effect of black tea drinking on blood lipids, blood pressure and aspects of bowel habit. Br. J. Nutr. 1997, 78, 41–55. [Google Scholar] [CrossRef] [PubMed]
- Hodgson, J.M.; Puddey, I.B.; Burke, V.; Watts, G.F.; Beilin, L.J. Regular ingestion of black tea improves brachial artery vasodilator function. Clin. Sci. (Lond.) 2002, 102, 195–201. [Google Scholar] [CrossRef] [PubMed]
- Quinlan, P.; Lane, J.; Aspinall, L. Effects of hot tea, coffee and water ingestion on physiological responses and mood: The role of caffeine, water and beverage type. Psychopharmacology (Berl.) 1997, 134, 164–173. [Google Scholar] [CrossRef]
- Hodgson, J.M.; Burke, V.; Puddey, I.B. Acute effects of tea on fasting and postprandial vascular function and blood pressure in humans. J. Hypertens. 2005, 23, 47–54. [Google Scholar] [CrossRef]
- Hodgson, J.M.; Woodman, R.J.; Puddey, I.B.; Mulder., T.; Fuchs, D.; Croft, K.D. Short-term effects of polyphenol-rich black tea on blood pressure in men and women. Food Funct. 2013, 4, 111–115. [Google Scholar] [CrossRef]
- Lastra, G.; Syed, S.; Kurukulasuriya, L.R.; Manrique, C.; Sowers, J.R. Type 2 diabetes mellitus and hypertension: An update. Endocrinol. Metab. Clin. N. Am. 2014, 43, 103–122. [Google Scholar] [CrossRef]
- Kondo, Y.; Goto, A.; Noma, H.; Iso, H.; Hayashi, K.; Noda, M. Effects of Coffee and Tea Consumption on Glucose Metabolism: A Systematic Review and Network Meta-Analysis. Nutrients 2018, 11, 48. [Google Scholar] [CrossRef]
- Eng, Q.Y.; Thanikachalam, P.V.; Ramamurthy, S. Molecular understanding of Epigallocatechin gallate (EGCG) in cardiovascular and metabolic diseases. J. Ethnopharmacol. 2018, 210, 296–310. [Google Scholar] [CrossRef] [PubMed]
- Waltner-Law, M.E.; Wang, X.L.; Law, B.K.; Hall, R.K.; Nawano, M.; Granner, D.K. Epigallocatechin gallate, a constituent of green tea, represses hepatic glucose production. J. Biol. Chem. 2002, 277, 34933–34940. [Google Scholar] [CrossRef] [PubMed]
- Teng, Y.; Li, D.; Guruvaiah, P.; Xu, N.; Xie, Z. Dietary Supplement of Large Yellow Tea Ameliorates Metabolic Syndrome and Attenuates Hepatic Steatosis in db/db Mice. Nutrients 2018, 10, 75. [Google Scholar] [CrossRef] [PubMed]
- Ortsater, H.; Grankvist, N.; Wolfram, S.; Kuehn, N.; Sjoholm, A. Diet supplementation with green tea extract epigallocatechin gallate prevents progression to glucose intolerance in db/db mice. Nutr. Metab. 2012, 9, 11. [Google Scholar] [CrossRef] [PubMed]
| No. | Methods of Study | Selected Participants | Tea or Dosage & Duration | Test Site | Primary Outcomes and Comments | Year (Citation) |
|---|---|---|---|---|---|---|
| 1 | Meta-analysis | 13 studies | Green tea | Australia | Significantly reduced SBP by 2.08 mmHg and DBP by 1.71 mmHg. Good methodology analysis and trusted results | 2014 [20] |
| 2 | Meta-analysis | 13 randomized controlled trials across, 1367 subjects | Green tea polyphenols (<582.8 mg/day), ≥12 weeks | Several countries | Significantly reduced SBP level by 1.98 mmHg and DBP by 1.92 mmHg. Good methodology analysis, a large population and trusted results | 2014 [21] |
| 3 | Meta-analysis | 11 randomized controlled trials, 378 subjects | 4–5 cups of black tea | Netherland | The SBP and DBP were decreased by 1.8 mmHg and 1.3 mmHg. Good methodology, and trusted results | 2014 [22] |
| 4 | Meta-analysis | 25 eligible studies, 1476 subjects | Both green and black tea intake,≥ 12 weeks | USA | Long-term (≥12 weeks) ingestion of tea could result in a significant Reduction in SBP and DBP Good methodology, a large population analysis and trusted results | 2014 [23] |
| 5 | Meta-analysis | 10 trials (834 participants) hypertensive individuals | Tea regular consumption | UK | Significant reductions in SBP (2.36 mmHg) and DBP (1.77 mmHg). Good methodology and trusted results. | 2015 [24] |
| 6 | Meta-analysis | 971 overweight and obese adult participants (47% women) | Green tea or green tea extract | China | Significant reduction in both SBP (1.42 mmHg) and DBP (1.25 mmHg). Good methodology and trusted results. | 2015 [27] |
| 7 | Multivariable analysis | 472 men and 637 women | Tea (green, black and mixed teas) consumption | China | The consumption of green tea is inversely associated with five-year BP change in Chinese adults, an effect was diminished by smoking. Long term study and trusted results. | 2014 [28] |
| 8 | Meta-analysis | 711 men and 796 women | 120 mL/day (half a cup)green or oolong tea, a year | China | Significantly reduces the risk of developing hypertension. A large special population, and trusted results. | 2004 [29] |
| 9 | Meta-analysis | 9,856 men and 10,233 women (35–49 years of age) | Black tea regular consumption | Norway | SBP was inversely related to tea consumption with differences of 2.1 mmHg in men and 3.5 mmHg in women. Good methodology, a large population analysis and trusted results. | 1992 [31] |
| 10 | Randomized controlled trial | 95 men and women aged 35 to 75 who were regular tea drinkers | 3 cups/d of regular black tea consumption, ≥ 6 months | Australia | Reductions in SBP and DBP of between 2 and 3 mmHg. A small population trial, and a reasonable result. | 2012 [32] |
| 11 | Double-blind parallel multicenter trial | 240 Japanese women and men with visceral fat-type obesity | 583 mg of catechins or 96 mg of catechins per day, green tea | Japan | Catechin group decreased initial SBP that is 130 mmHg or higher. A small population trial, and a reasonable result. | 2007 [38] |
| 12 | Randomized controlled trial | Overweight or obese male subjects, aged 40–65 years | 400 mg capsules of EGCG (n = 46) or the placebo lactose (n = 42), twice a day for eight weeks. | UK | EGCG treatment did reduce DBP (mean change: placebo -0·058 mmHg; EGCG -2·68 mmHg). A small population trial, and a reasonable result. | 2009 [39] |
| 13 | Randomized clinical trial | Obese pre-hypertensive women | 500 mg of GTE or a matching placebo consumption, four weeks | Brazil | Short-term daily intake of GTE may decrease BP in obese pre-hypertensive women. A small population, short term trial, and a reasonable result. | 2016 [40] |
| 14 | Double-blind | 56 obese, hypertensive subjects | Daily supplement 379 mg of GTE or a matching placebo, 3 months | Poland | Both SBP and DBP had significantly decreased compared with the placebo group. A small population trial, and a reasonable result. | 2012 [41] |
| 15 | Randomized, double-blind | 19 patients | Black tea (129 mg flavonoids) or a placebo twice a day for eight days. | Italy | Black tea consumption decreases SBP and DBP by 3.2 mmHg and 2.6 mmHg, respectively, and prevented BP increase after a fat consumption. A small population trial may results in bias result. | 2015 [42] |
| 16 | Randomized clinical trial | 100 stage1 hypertensive patients with diabetes | Drink green tea infusion three times a day 2 hours after each meal, four weeks | Iran | Stage1 hypertensive type 2 diabetic individuals who drink green tea daily show significantly lower SBP and DBP. A small population trial, and a reasonable result. | 2013 [44] |
| 17 | Cross-sectional study | 60 volunteers, fasting blood glucose levels of ≥6.1 mmol/L or non-fasting blood glucose levels of ≥7.8 mmol/L | 544 mg polyphenols (456 mg catechins) daily consumption, 3 months | Japan | Supplementation of GTE powder led to a significant reduction in DBP, but no significant changes in SBP. A small population trial, and a reasonable result. | 2008 [45] |
| 18 | Cross-sectional study | 218 women over 70 years old | 250 mL/day (one cup) | Australia | Regular tea consumption may have a favorable effect on BP in older women. A small population trial, and a reasonable result. | 2003 [32] |
| 19 | Cross-sectional study | 4579 adults aged 60 years or older | tea consumption questionnaire | China | Higher tea consumption frequency was associated with lower systolic BP. A large population trial, and a reasonable result. | 2017 [35] |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, D.; Wang, R.; Huang, J.; Cai, Q.; Yang, C.S.; Wan, X.; Xie, Z. Effects and Mechanisms of Tea Regulating Blood Pressure: Evidences and Promises. Nutrients 2019, 11, 1115. https://doi.org/10.3390/nu11051115
Li D, Wang R, Huang J, Cai Q, Yang CS, Wan X, Xie Z. Effects and Mechanisms of Tea Regulating Blood Pressure: Evidences and Promises. Nutrients. 2019; 11(5):1115. https://doi.org/10.3390/nu11051115
Chicago/Turabian StyleLi, Daxiang, Ruru Wang, Jinbao Huang, Qingshuang Cai, Chung S. Yang, Xiaochun Wan, and Zhongwen Xie. 2019. "Effects and Mechanisms of Tea Regulating Blood Pressure: Evidences and Promises" Nutrients 11, no. 5: 1115. https://doi.org/10.3390/nu11051115
APA StyleLi, D., Wang, R., Huang, J., Cai, Q., Yang, C. S., Wan, X., & Xie, Z. (2019). Effects and Mechanisms of Tea Regulating Blood Pressure: Evidences and Promises. Nutrients, 11(5), 1115. https://doi.org/10.3390/nu11051115