Health Concerns of Various Nanoparticles: A Review of Their in Vitro and in Vivo Toxicity
Abstract
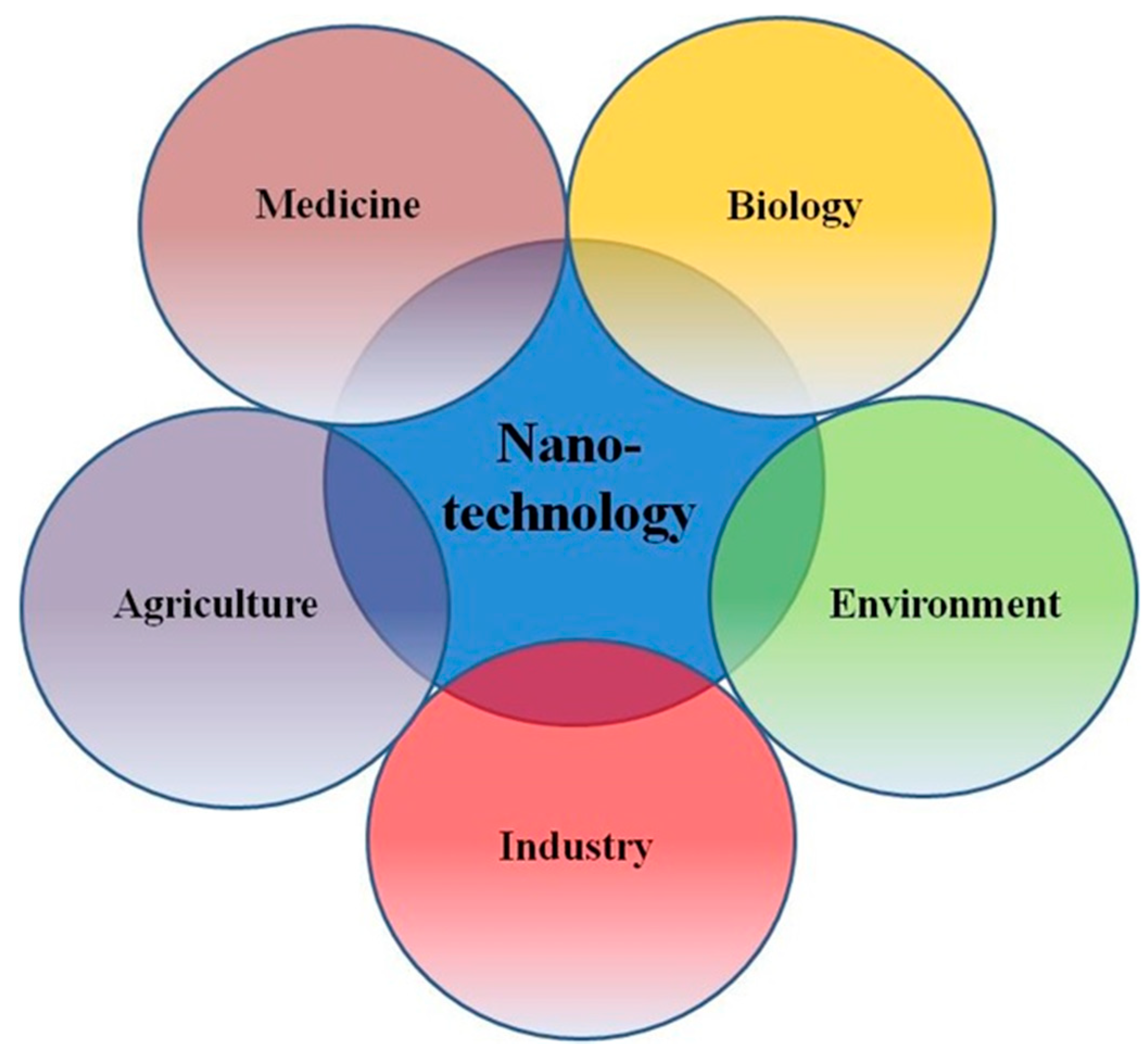
:1. Introduction
2. Medical Applications of Nanoparticles
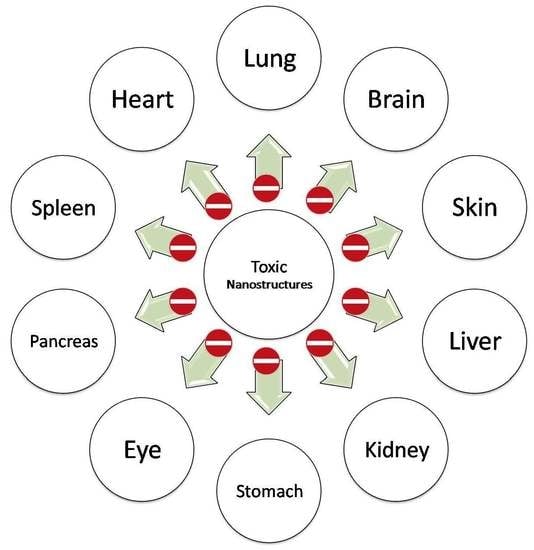
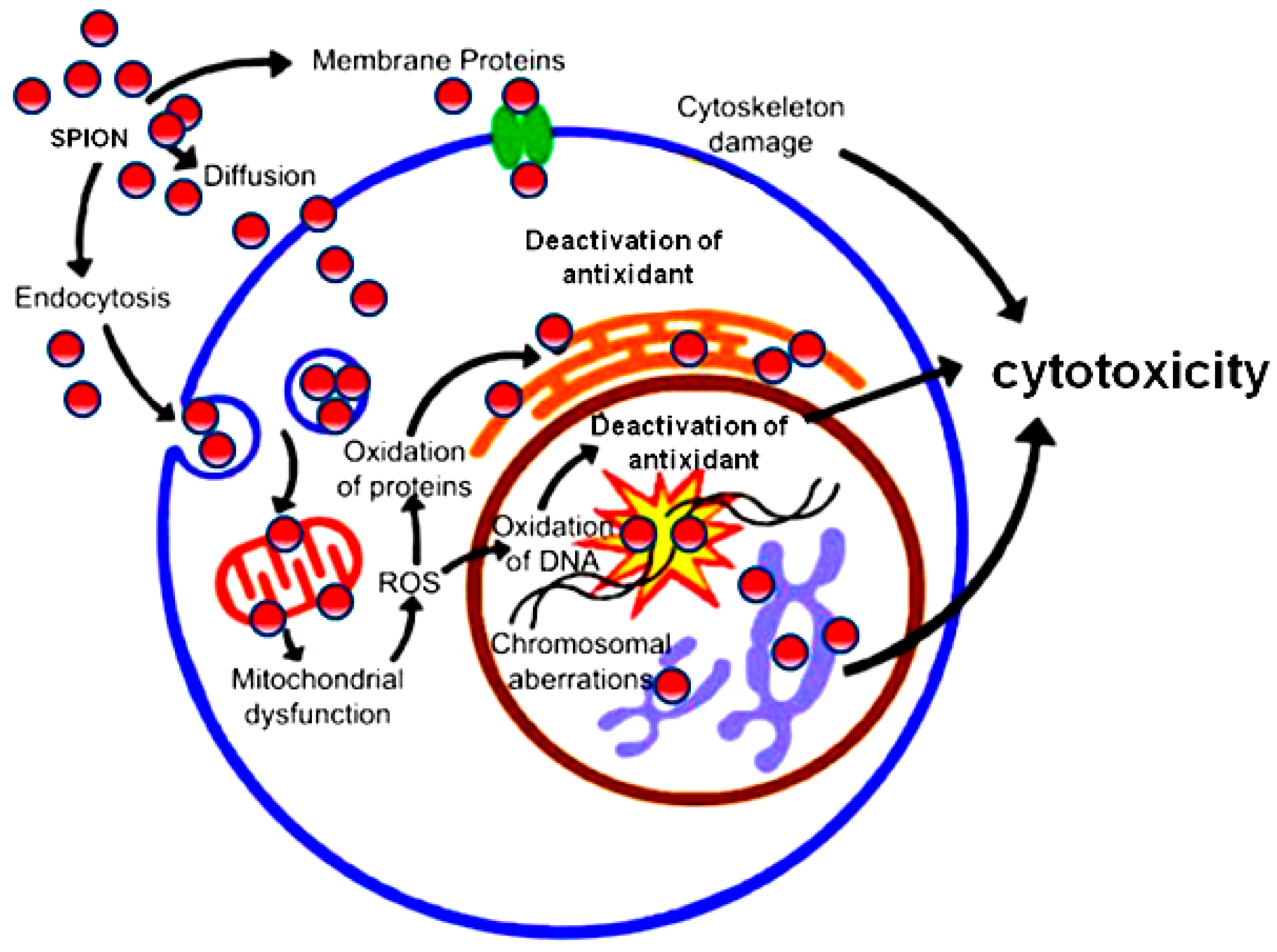
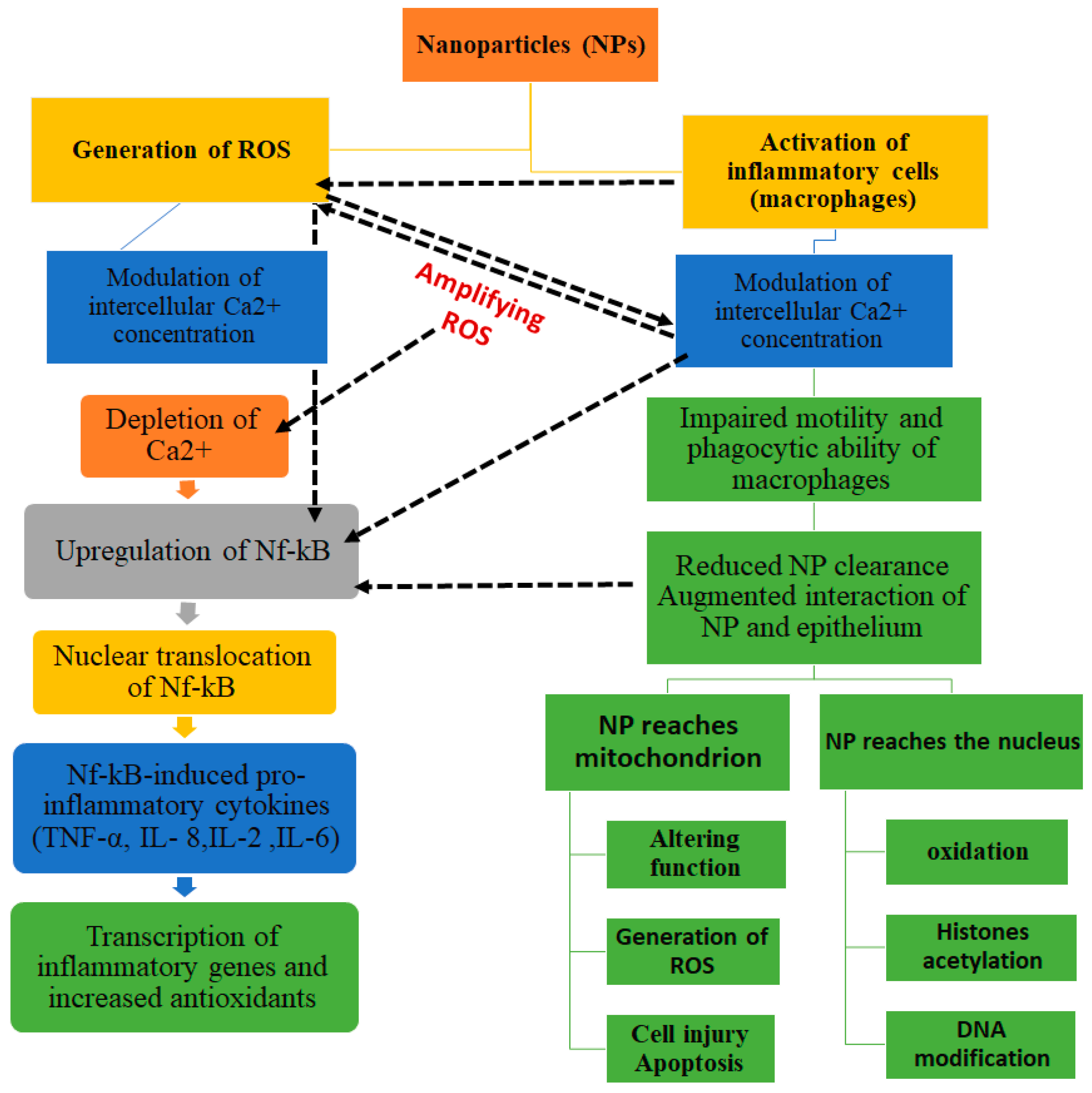
3. Mechanisms of Nanoparticle Toxicity: NP-Cell Interactions
- NPs may cause oxidation via increase of reactive oxygen species (ROS)
- NPs may damage cell membranes by perforating them
- NPs damage components of the cytoskeleton, disturbing intracellular transport and cell division
- NPs disturb transcription and damage DNA, thus accelerating mutagenesis
- NPs damage mitochondria and disturb their metabolism, which leads to cell energy imbalance
- NPs interfere with the formation of lysosomes, thereby hampering autophagy and degradation of macromolecules and triggering the apoptosis
- NPs cause structural changes in membrane proteins and disturb the transport of substances into and out of cells, including intercellular transport
- NPs activate the synthesis of inflammatory mediators by disturbing the normal mechanisms of cell metabolism, as well as tissue and organ metabolism (Figure 3).
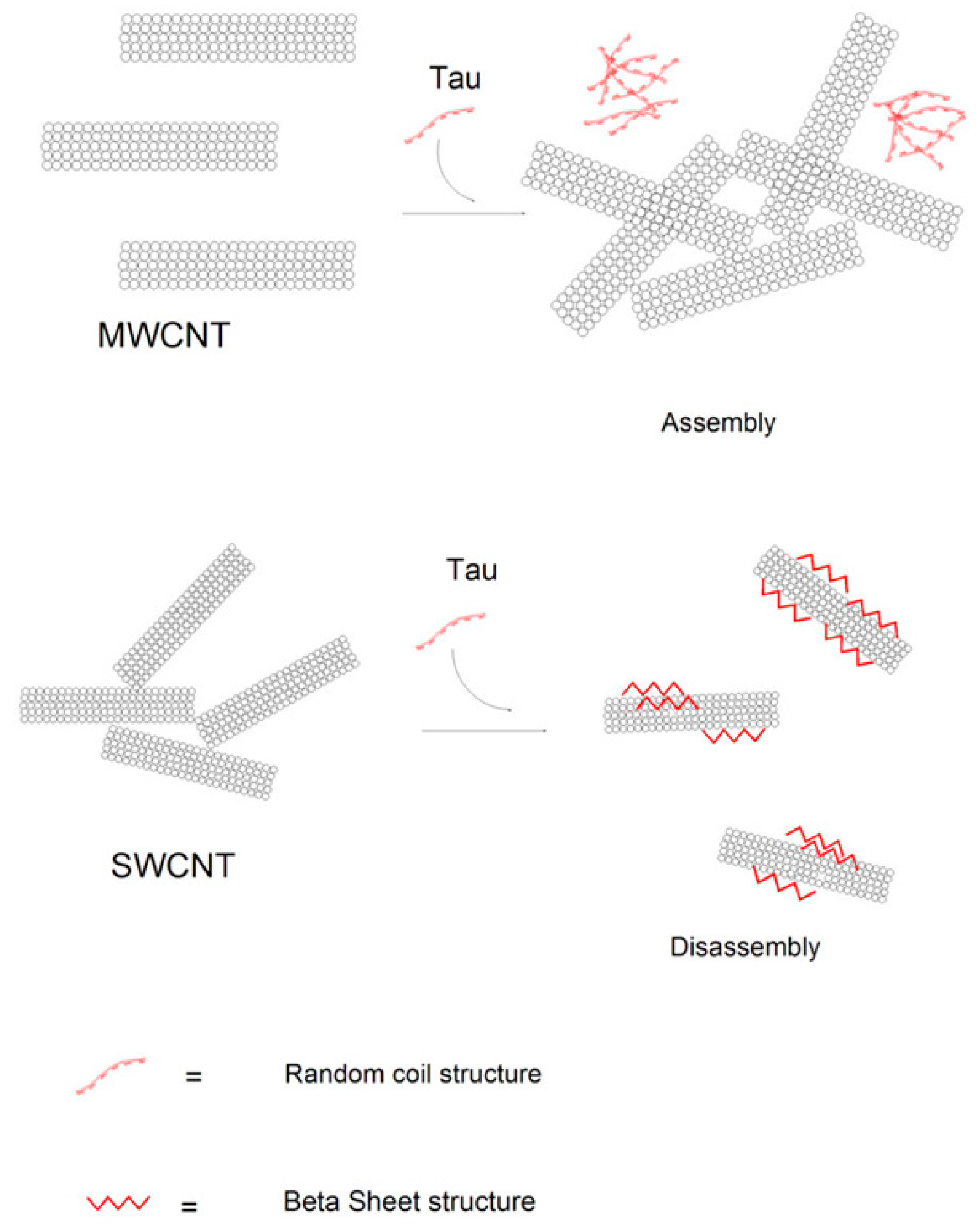
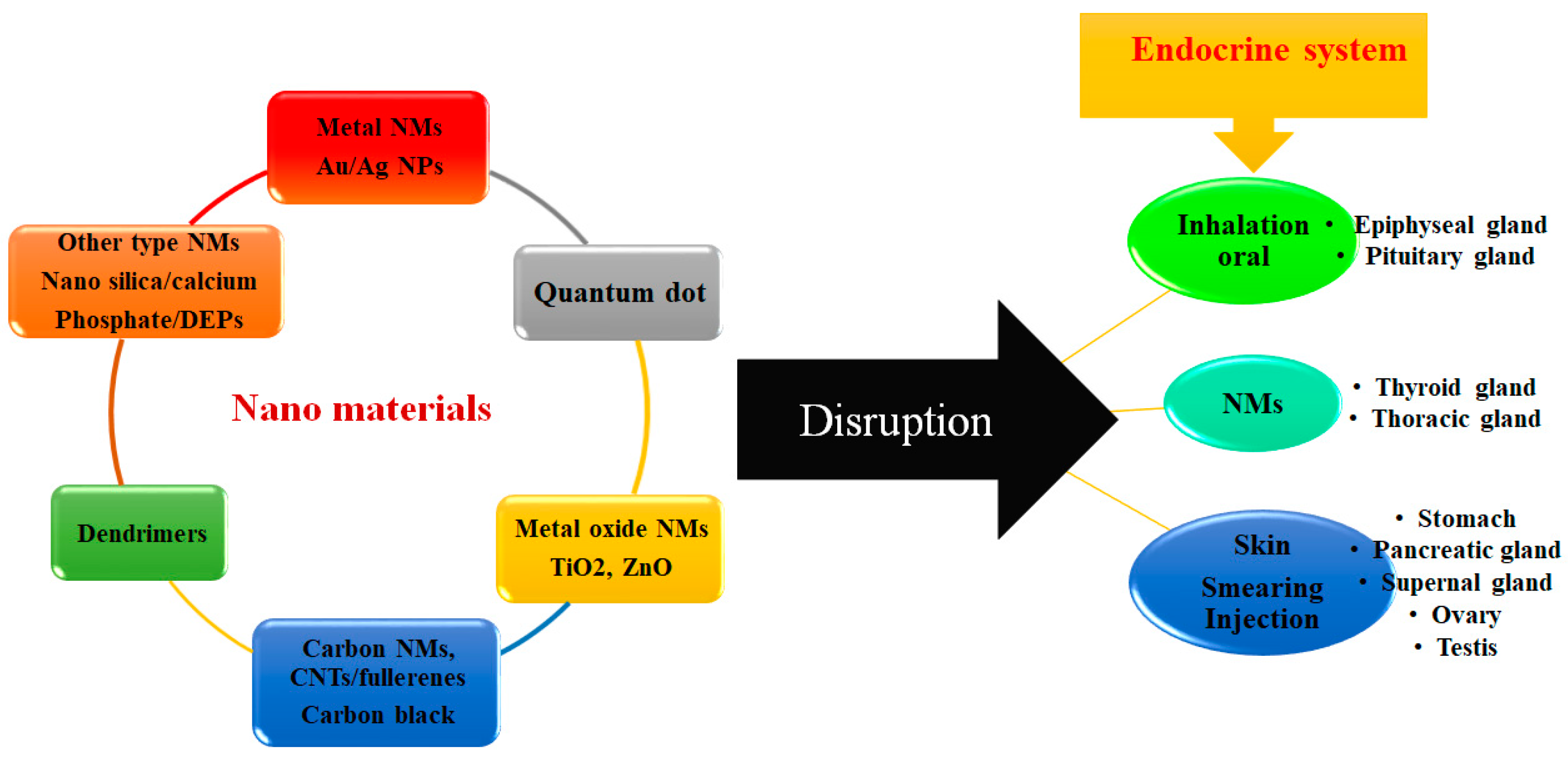
3.1. The Effect of NP on the Protein Conformational Changes
3.2. The Effect of Protein Corona on the Toxicity of NPs
3.3. The Effect of Protein Corona on Non-specific Cellular Uptake
3.4. The Effect of Protein Corona on Bio-distribution of NPs
3.5. The Effect of Surface Charge of NPs on Their Toxicity
4. The Effects of Physicochemical Properties of NPs on Cytotoxicity
4.1. The Effect of NPs Size on Cytotoxicity
4.2. The effect of NPs Structure and Shape on Cytotoxicity
4.3. The Effect of NPs Surface on Cytotoxicity
4.4. The Effect of NPs Concentration on Cytotoxicity
5. In Vivo Study of Nanoparticle Toxicity
6. Study of Toxicity in Cell Cultures
7. Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
Abbreviations
| AD | Albumin Derivatized |
| BBB | Blood–Brain-Barrier |
| BMECs | Brain Microvascular Endothelial Cells |
| CNS | Central Nervous System |
| CSF | Cerebrospinal Fluid |
| DD | Dextran Derivatized |
| Ag NP | Silver Nanoparticle |
| DA | Dopamine |
| Au NP | Gold Nanoparticles |
| MRI | Magnetic Resonance Imaging |
| CNTs | Carbon nano tubes |
| MWCNTs | Multi-Walled Carbon Nanotubes |
| NPs | Nanoparticles |
| QDs | Quantum Dots |
| SWCNTs | Single-Walled Carbon Nanotubes |
| SPIONs | Superparamagnetic Iron Oxide Nanoparticles |
| USPIONs | Ultra-Small Superparamagnetic Iron Oxide Nanoparticles |
References
- Cheng, R.; Feng, F.; Meng, F.; Deng, C.; Feijen, J.; Zhong, Z. Glutathione-responsive nano-vehicles as a promising platform for targeted intracellular drug and gene delivery. J. Control. Release 2011, 152, 2–12. [Google Scholar] [CrossRef] [PubMed]
- Sajid, M.; Ilyas, M.; Basheer, C.; Tariq, M.; Daud, M.; Baig, N.; Shehzad, F. Impact of nanoparticles on human and environment: Review of toxicity factors, exposures, control strategies, and future prospects. Environ. Sci. Pollut. Res. 2015, 22, 4122–4143. [Google Scholar] [CrossRef] [PubMed]
- Dwivedi, A.D.; Dubey, S.P.; Sillanpää, M.; Kwon, Y.-N.; Lee, C.; Varma, R.S. Fate of engineered nanoparticles: Implications in the environment. Coord. Chem. Rev. 2015, 287, 64–78. [Google Scholar] [CrossRef]
- Ajdari, M.; Ghahnavieh, M.Z. Histopathology effects of nickel nanoparticles on lungs, liver, and spleen tissues in male mice. Int. Nano Lett. 2014, 4, 113. [Google Scholar] [CrossRef]
- Negahdary, M.; Ajdary, M. The toxicity of gold, silver, and zinc oxide nanoparticles on LDH enzyme in male mice. Annu. Res. Rev. Biol. 2014, 4, 1346–1352. [Google Scholar] [CrossRef]
- Hornos Carneiro, M.F.; Barbosa, F., Jr. Gold nanoparticles: A critical review of therapeutic applications and toxicological aspects. J. Toxic. Environ. Health 2016, 19, 129–148. [Google Scholar] [CrossRef] [PubMed]
- Moulton, M.C.; Braydich-Stolle, L.K.; Nadagouda, M.N.; Kunzelman, S.; Hussain, S.M.; Varma, R.S. Synthesis, characterization and biocompatibility of “green” synthesized silver nanoparticles using tea polyphenols. Nanoscale 2010, 2, 763–770. [Google Scholar] [CrossRef] [PubMed]
- Warheit, D.B.; Laurence, B.R.; Reed, K.L.; Roach, D.H.; Reynolds, G.A.; Webb, T.R. Comparative pulmonary toxicity assessment of single-wall carbon nanotubes in rats. Toxicol. Sci. 2004, 77, 117–125. [Google Scholar] [CrossRef] [PubMed]
- Hussain, S.; Hess, K.; Gearhart, J.; Geiss, K.; Schlager, J. In vitro toxicity of nanoparticles in BRL 3A rat liver cells. Toxicol. In Vitro 2005, 19, 975–983. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.J.; Kim, B.M.; Lee, Y.J.; Chung, H.W. Titanium dioxide nanoparticles trigger p53-mediated damage response in peripheral blood lymphocytes. Environ. Mol. Mutagen. 2008, 49, 399–405. [Google Scholar] [CrossRef] [PubMed]
- Xia, T.; Kovochich, M.; Brant, J.; Hotze, M.; Sempf, J.; Oberley, T.; Sioutas, C.; Yeh, J.I.; Wiesner, M.R.; Nel, A.E. Comparison of the abilities of ambient and manufactured nanoparticles to induce cellular toxicity according to an oxidative stress paradigm. Nano Lett. 2006, 6, 1794–1807. [Google Scholar] [CrossRef] [PubMed]
- Muller, J.; Huaux, F.; Moreau, N.; Misson, P.; Heilier, J.-F.; Delos, M.; Arras, M.; Fonseca, A.; Nagy, J.B.; Lison, D. Respiratory toxicity of multi-wall carbon nanotubes. Toxic. Appl. Pharmacol. 2005, 207, 221–231. [Google Scholar] [CrossRef] [PubMed]
- Mutlu, G.k.M.; Budinger, G.S.; Green, A.A.; Urich, D.; Soberanes, S.; Chiarella, S.E.; Alheid, G.F.; McCrimmon, D.R.; Szleifer, I.; Hersam, M.C. Biocompatible nanoscale dispersion of single-walled carbon nanotubes minimizes in vivo pulmonary toxicity. Nano Lett. 2010, 10, 1664–1670. [Google Scholar] [CrossRef] [PubMed]
- Fard, J.K.; Jafari, S.; Eghbal, M.A. A review of molecular mechanisms involved in toxicity of nanoparticles. Adv. Pharm. Bull. 2015, 5, 447–454. [Google Scholar] [CrossRef] [PubMed]
- Gualtierotti, R.; Guarnaccia, L.; Beretta, M.; Navone, S.E.; Campanella, R.; Riboni, L.; Rampini, P.; Marfia, G. Modulation of neuroinflammation in the central nervous system: Role of chemokines and sphingolipids. Adv. Ther. 2017, 34, 396–420. [Google Scholar] [CrossRef] [PubMed]
- Ma, L.; Zou, X.; Chen, W. A new X-ray activated nanoparticle photosensitizer for cancer treatment. J. Biomed. Nanotechnol. 2014, 10, 1501–1508. [Google Scholar] [CrossRef] [PubMed]
- Guan, X.; Avci-Adali, M.; Alarçin, E.; Cheng, H.; Kashaf, S.S.; Li, Y.; Chawla, A.; Jang, H.L.; Khademhosseini, A. Development of hydrogels for regenerative engineering. Biotechnol. J. 2017, 12, 1600394. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dorniani, D.; Hussein, M.Z.B.; Kura, A.U.; Fakurazi, S.; Shaari, A.H.; Ahmad, Z. Preparation of Fe3O4 magnetic nanoparticles coated with gallic acid for drug delivery. Int. J. Nanomed. 2012, 7, 5745–5756. [Google Scholar] [CrossRef] [PubMed]
- Benita, S. Microencapsulation: Methods and Industrial Applications; Taylor & Francis: Boca Raton, FL, USA, 2006. [Google Scholar]
- Mishra, A.K. Nanomedicine for Drug Delivery and Therapeutics; Wiley: New York, NY, USA, 2013. [Google Scholar]
- Sharma, V.K.; Filip, J.; Zboril, R.; Varma, R.S. Natural inorganic nanoparticles–formation, fate, and toxicity in the environment. Chem. Soc. Rev. 2015, 44, 8410–8423. [Google Scholar] [CrossRef] [PubMed]
- You, Y.; He, L.; Ma, B.; Chen, T. High-drug-loading mesoporous silica nanorods with reduced toxicity for precise cancer therapy against nasopharyngeal carcinoma. Adv. Funct. Mater. 2017, 27, 1703313. [Google Scholar] [CrossRef]
- Coradeghini, R.; Gioria, S.; García, C.P.; Nativo, P.; Franchini, F.; Gilliland, D.; Ponti, J.; Rossi, F. Size-dependent toxicity and cell interaction mechanisms of gold nanoparticles on mouse fibroblasts. Toxicol. Lett. 2013, 217, 205–216. [Google Scholar] [CrossRef] [PubMed]
- Asharani, P.; Hande, M.P.; Valiyaveettil, S. Anti-proliferative activity of silver nanoparticles. BMC Cell Biol. 2009, 10, 65. [Google Scholar] [CrossRef] [PubMed]
- Nair, S.; Sasidharan, A.; Rani, V.D.; Menon, D.; Nair, S.; Manzoor, K.; Raina, S. Role of size scale of ZnO nanoparticles and microparticles on toxicity toward bacteria and osteoblast cancer cells. J. Mater. Sci. Mater. Med. 2009, 20, 235–241. [Google Scholar] [CrossRef] [PubMed]
- Premanathan, M.; Karthikeyan, K.; Jeyasubramanian, K.; Manivannan, G. Selective toxicity of ZnO nanoparticles toward gram-positive bacteria and cancer cells by apoptosis through lipid peroxidation. Nanomed. Nanotechnol. Biol. Med. 2011, 7, 184–192. [Google Scholar] [CrossRef] [PubMed]
- Zou, J.; Li, M.; Zhang, Y.; Zheng, G.; Chen, D.; Chen, S.; Zheng, H. Transport augmentation through the blood-inner ear barriers of guinea pigs treated with 3-nitropropionic acid and patients with acute hearing loss, visualized with 3.0 T MRI. Otol. Neurotol. 2011, 32, 204–212. [Google Scholar] [CrossRef] [PubMed]
- Lundqvist, M.; Stigler, J.; Elia, G.; Lynch, I.; Cedervall, T.; Dawson, K.A. Nanoparticle size and surface properties determine the protein corona with possible implications for biological impacts. Proc. Natl. Acad. Sci. USA 2008, 105, 14265–14270. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jordan, A.; Scholz, R.; Maier-Hauff, K.; van Landeghem, F.K.; Waldoefner, N.; Teichgraeber, U.; Pinkernelle, J.; Bruhn, H.; Neumann, F.; Thiesen, B. The effect of thermotherapy using magnetic nanoparticles on rat malignant glioma. J. Neuro-Oncology 2006, 78, 7–14. [Google Scholar] [CrossRef] [PubMed]
- Wang, F.; Gao, F.; Lan, M.; Yuan, H.; Huang, Y.; Liu, J. Oxidative stress contributes to silica nanoparticle-induced cytotoxicity in human embryonic kidney cells. Toxicol. In Vitro 2009, 23, 808–815. [Google Scholar] [CrossRef] [PubMed]
- Shang, L.; Nienhaus, K.; Nienhaus, G.U. Engineered nanoparticles interacting with cells: Size matters. J. Nanobiotechnol. 2014, 12, 5. [Google Scholar] [CrossRef] [PubMed]
- Zhang, K. Integration of er stress, oxidative stress and the inflammatory response in health and disease. Int. J. Clin. Exp. Med. 2010, 3, 33–40. [Google Scholar] [PubMed]
- Ceccon, A.; Tugarinov, V.; Bax, A.; Clore, G.M. Global dynamics and exchange kinetics of a protein on the surface of nanoparticles revealed by relaxation-based solution NMR spectroscopy. J. Am. Chem. Soc. 2016, 138, 5789–5792. [Google Scholar] [PubMed]
- Pham, N.; Radajewski, D.; Round, A.; Brennich, M.; Pernot, P.; Biscans, B.; Bonneté, F.; Teychené, S. Coupling high throughput microfluidics and small-angle X-ray scattering to study protein crystallization from solution. Anal. Chem. 2017, 89, 2282–2287. [Google Scholar] [CrossRef] [PubMed]
- Pishkar, L.; Taheri, S.; Makarem, S.; Alizadeh Zeinabad, H.; Rahimi, A.; Saboury, A.A.; Falahati, M. Studies on the interaction between nanodiamond and human hemoglobin by surface tension measurement and spectroscopy methods. J. Biomol. Struct. Dyn. 2017, 35, 603–615. [Google Scholar] [CrossRef] [PubMed]
- Huang, R.; Lau, B.L. Biomolecule–nanoparticle interactions: Elucidation of the thermodynamics by isothermal titration calorimetry. Biochim. Biophys. Acta Gen. Subj. 2016, 1860, 945–956. [Google Scholar] [CrossRef] [PubMed]
- Manyanga, F.; Sithole, A.; Rivera, R.; Karamehmedovic, N.; Martin, N. Use of differential scanning calorimetry (DSC) to study the thermodynamics of DNA-based interactions and nucleic acid-based therapeutics. J. Anal. Pharm. Res. 2016, 2, 00013. [Google Scholar]
- Esfandfar, P.; Falahati, M.; Saboury, A. Spectroscopic studies of interaction between cuo nanoparticles and bovine serum albumin. J. Biomol. Struct. Dyn. 2016, 34, 1962–1968. [Google Scholar] [CrossRef] [PubMed]
- Jafari Azad, V.; Kasravi, S.; Alizadeh Zeinabad, H.; Memar Bashi Aval, M.; Saboury, A.A.; Rahimi, A.; Falahati, M. Probing the conformational changes and peroxidase-like activity of cytochrome c upon interaction with iron nanoparticles. J. Biomol. Struct. Dyn. 2017, 35, 2565–2577. [Google Scholar] [CrossRef] [PubMed]
- Zeinabad, H.A.; Zarrabian, A.; Saboury, A.A.; Alizadeh, A.M.; Falahati, M. Interaction of single and multi wall carbon nanotubes with the biological systems: Tau protein and PC12 cells as targets. Sci. Rep. 2016, 6, 26508. [Google Scholar] [PubMed]
- Zeinabad, H.A.; Kachooei, E.; Saboury, A.A.; Kostova, I.; Attar, F.; Vaezzadeh, M.; Falahati, M. Thermodynamic and conformational changes of protein toward interaction with nanoparticles: A spectroscopic overview. RSC Adv. 2016, 6, 105903–105919. [Google Scholar] [CrossRef]
- Hajsalimi, G.; Taheri, S.; Shahi, F.; Attar, F.; Ahmadi, H.; Falahati, M. Interaction of iron nanoparticles with nervous system: An in vitro study. J. Biomol. Struct. Dyn. 2018, 36, 928–937. [Google Scholar] [CrossRef] [PubMed]
- Vroman, L.; Adams, A.; Fischer, G.; Munoz, P. Interaction of high molecular weight kininogen, factor XII, and fibrinogen in plasma at interfaces. Blood 1980, 55, 156–159. [Google Scholar] [PubMed]
- Walkey, C.D.; Chan, W.C. Understanding and controlling the interaction of nanomaterials with proteins in a physiological environment. Chem. Soc. Rev. 2012, 41, 2780–2799. [Google Scholar] [CrossRef] [PubMed]
- Lundqvist, M.; Stigler, J.; Cedervall, T.; Berggård, T.; Flanagan, M.B.; Lynch, I.; Elia, G.; Dawson, K. The evolution of the protein corona around nanoparticles: A test study. ACS Nano 2011, 5, 7503–7509. [Google Scholar] [CrossRef] [PubMed]
- Ge, C.; Du, J.; Zhao, L.; Wang, L.; Liu, Y.; Li, D.; Yang, Y.; Zhou, R.; Zhao, Y.; Chai, Z. Binding of blood proteins to carbon nanotubes reduces cytotoxicity. Proc. Natl. Acad. Sci. USA 2011, 108, 16968–16973. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hu, W.; Peng, C.; Lv, M.; Li, X.; Zhang, Y.; Chen, N.; Fan, C.; Huang, Q. Protein corona-mediated mitigation of cytotoxicity of graphene oxide. ACS Nano 2011, 5, 3693–3700. [Google Scholar] [CrossRef] [PubMed]
- Peng, Q.; Zhang, S.; Yang, Q.; Zhang, T.; Wei, X.-Q.; Jiang, L.; Zhang, C.-L.; Chen, Q.-M.; Zhang, Z.-R.; Lin, Y.-F. Preformed albumin corona, a protective coating for nanoparticles based drug delivery system. Biomaterials 2013, 34, 8521–8530. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Li, J.; Pan, J.; Jiang, X.; Ji, Y.; Li, Y.; Qu, Y.; Zhao, Y.; Wu, X.; Chen, C. Revealing the binding structure of the protein corona on gold nanorods using synchrotron radiation-based techniques: Understanding the reduced damage in cell membranes. J. Am. Chem. Soc. 2013, 135, 17359–17368. [Google Scholar] [CrossRef] [PubMed]
- Corbo, C.; Molinaro, R.; Parodi, A.; Furman, N.E.T.; Salvatore, F.; Tasciotti, E. The impact of nanoparticle protein corona on cytotoxicity, immunotoxicity and target drug delivery. Nanomedicine 2016, 11, 81–100. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Treuel, L.; Brandholt, S.; Maffre, P.; Wiegele, S.; Shang, L.; Nienhaus, G.U. Impact of protein modification on the protein corona on nanoparticles and nanoparticle–cell interactions. ACS Nano 2014, 8, 503–513. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.J.; Browning, L.M.; Nallathamby, P.D.; Xu, X.-H.N. Study of charge-dependent transport and toxicity of peptide-functionalized silver nanoparticles using zebrafish embryos and single nanoparticle plasmonic spectroscopy. Chem. Res. Toxicol. 2013, 26, 904–917. [Google Scholar] [CrossRef] [PubMed]
- Piao, M.J.; Kang, K.A.; Lee, I.K.; Kim, H.S.; Kim, S.; Choi, J.Y.; Choi, J.; Hyun, J.W. Silver nanoparticles induce oxidative cell damage in human liver cells through inhibition of reduced glutathione and induction of mitochondria-involved apoptosis. Toxicol. Lett. 2011, 201, 92–100. [Google Scholar] [CrossRef] [PubMed]
- Carlson, C.; Hussain, S.M.; Schrand, A.M.; Braydich-Stolle, L.K.; Hess, K.L.; Jones, R.L.; Schlager, J.J. Unique cellular interaction of silver nanoparticles: Size-dependent generation of reactive oxygen species. J. Phys. Chem. B 2008, 112, 13608–13619. [Google Scholar] [CrossRef] [PubMed]
- Sharma, V.K. Aggregation and toxicity of titanium dioxide nanoparticles in aquatic environment—A review. J. Environ. Sci. Health Part A 2009, 44, 1485–1495. [Google Scholar] [CrossRef] [PubMed]
- Nel, A.; Xia, T.; Mädler, L.; Li, N. Toxic potential of materials at the nanolevel. Science 2006, 311, 622–627. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Wu, Y.; Wang, C.; Li, H.C.; Wang, T.; Liao, C.Y.; Cui, L.; Zhou, Q.F.; Yan, B.; Jiang, G.B. Impact of silver nanoparticles on human cells: Effect of particle size. Nanotoxicology 2010, 4, 319–330. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chithrani, B.D.; Chan, W.C. Elucidating the mechanism of cellular uptake and removal of protein-coated gold nanoparticles of different sizes and shapes. Nano Lett. 2007, 7, 1542–1550. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.H.; Kim, M.; Park, H.S.; Shin, U.S.; Gong, M.S.; Kim, H.W. Size-dependent cellular toxicity of silver nanoparticles. J. Biomed. Mater. Res. Part A 2012, 100, 1033–1043. [Google Scholar] [CrossRef] [PubMed]
- Favi, P.M.; Gao, M.; Johana Sepúlveda Arango, L.; Ospina, S.P.; Morales, M.; Pavon, J.J.; Webster, T.J. Shape and surface effects on the cytotoxicity of nanoparticles: Gold nanospheres versus gold nanostars. J. Biomed. Mater. Res. Part A 2015, 103, 3449–3462. [Google Scholar] [CrossRef] [PubMed]
- Verma, A.; Stellacci, F. Effect of surface properties on nanoparticle–cell interactions. Small 2010, 6, 12–21. [Google Scholar] [CrossRef] [PubMed]
- Champion, J.A.; Mitragotri, S. Role of target geometry in phagocytosis. Proc. Natl. Acad. Sci. USA 2006, 103, 4930–4934. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, X.; Gao, H.; Uo, M.; Sato, Y.; Akasaka, T.; Abe, S.; Feng, Q.; Cui, F.; Watari, F. Maturation of osteoblast-like SaoS2 induced by carbon nanotubes. Biomed. Mater. 2008, 4, 015005. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Ali, S.F.; Dervishi, E.; Xu, Y.; Li, Z.; Casciano, D.; Biris, A.S. Cytotoxicity effects of graphene and single-wall carbon nanotubes in neural phaeochromocytoma-derived PC12 cells. ACS Nano 2010, 4, 3181–3186. [Google Scholar] [CrossRef] [PubMed]
- Gurr, J.-R.; Wang, A.S.; Chen, C.-H.; Jan, K.-Y. Ultrafine titanium dioxide particles in the absence of photoactivation can induce oxidative damage to human bronchial epithelial cells. Toxicology 2005, 213, 66–73. [Google Scholar] [CrossRef] [PubMed]
- Georgieva, J.V.; Kalicharan, D.; Couraud, P.-O.; Romero, I.A.; Weksler, B.; Hoekstra, D.; Zuhorn, I.S. Surface characteristics of nanoparticles determine their intracellular fate in and processing by human blood–brain barrier endothelial cells in vitro. Mol. Ther. 2011, 19, 318–325. [Google Scholar] [CrossRef] [PubMed]
- Shahbazi, M.A.; Hamidi, M.; Makila, E.M.; Zhang, H.; Almeida, P.V.; Kaasalainen, M.; Salonen, J.J.; Hirvonen, J.T.; Santos, H.A. The mechanisms of surface chemistry effects of mesoporous silicon nanoparticles on immunotoxicity and biocompatibility. Biomaterials 2013, 34, 7776–7789. [Google Scholar] [CrossRef] [PubMed]
- Calatayud, M.P.; Sanz, B.; Raffa, V.; Riggio, C.; Ibarra, M.R.; Goya, G.F. The effect of surface charge of functionalized Fe3O4 nanoparticles on protein adsorption and cell uptake. Biomaterials 2014, 35, 6389–6399. [Google Scholar] [CrossRef] [PubMed]
- Santos, H.A.; Riikonen, J.; Salonen, J.; Mäkilä, E.; Heikkilä, T.; Laaksonen, T.; Peltonen, L.; Lehto, V.-P.; Hirvonen, J. In vitro cytotoxicity of porous silicon microparticles: Effect of the particle concentration, surface chemistry and size. Acta Biomater. 2010, 6, 2721–2731. [Google Scholar] [CrossRef] [PubMed]
- Kiss, B.; Bíró, T.; Czifra, G.; Tóth, B.I.; Kertész, Z.; Szikszai, Z.; Kiss, Á.Z.; Juhász, I.; Zouboulis, C.C.; Hunyadi, J. Investigation of micronized titanium dioxide penetration in human skin xenografts and its effect on cellular functions of human skin-derived cells. Exp. Dermatol. 2008, 17, 659–667. [Google Scholar] [CrossRef] [PubMed]
- Korani, M.; Rezayat, S.M.; Bidgoli, S.A. Sub-chronic dermal toxicity of silver nanoparticles in guinea pig: Special emphasis to heart, bone and kidney toxicities. Iran. J. Pharm. Res. 2013, 12, 511–519. [Google Scholar] [PubMed]
- Narayanan, D.; Geena, M.; Lakshmi, H.; Koyakutty, M.; Nair, S.; Menon, D. Poly-(ethylene glycol) modified gelatin nanoparticles for sustained delivery of the anti-inflammatory drug ibuprofen-sodium: An in vitro and in vivo analysis. Nanomed. Nanotechnol. Biol. Med. 2013, 9, 818–828. [Google Scholar] [CrossRef] [PubMed]
- Ema, M.; Matsuda, A.; Kobayashi, N.; Naya, M.; Nakanishi, J. Evaluation of dermal and eye irritation and skin sensitization due to carbon nanotubes. Regul. Toxicol. Pharm. 2011, 61, 276–281. [Google Scholar] [CrossRef] [PubMed]
- Kato, S.; Itoh, K.; Yaoi, T.; Tozawa, T.; Yoshikawa, Y.; Yasui, H.; Kanamura, N.; Hoshino, A.; Manabe, N.; Yamamoto, K. Organ distribution of quantum dots after intraperitoneal administration, with special reference to area-specific distribution in the brain. Nanotechnology 2010, 21, 335103. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.; Hu, Y.; Tang, M.; Kong, L.; Ying, J.; Wu, T.; Xue, Y.; Pu, Y. Liver toxicity of cadmium telluride quantum dots (CdTe QDs) due to oxidative stress in vitro and in vivo. Int. J. Mol. Sci. 2015, 16, 23279–23299. [Google Scholar] [CrossRef] [PubMed]
- Trickler, W.J.; Lantz, S.M.; Murdock, R.C.; Schrand, A.M.; Robinson, B.L.; Newport, G.D.; Schlager, J.J.; Oldenburg, S.J.; Paule, M.G.; Slikker, W., Jr. Silver nanoparticle induced blood-brain barrier inflammation and increased permeability in primary rat brain microvessel endothelial cells. Toxicol. Sci. 2010, 118, 160–170. [Google Scholar] [CrossRef] [PubMed]
- Truong, L.; Saili, K.S.; Miller, J.M.; Hutchison, J.E.; Tanguay, R.L. Persistent adult zebrafish behavioral deficits results from acute embryonic exposure to gold nanoparticles. Comp. Biochem. Physiol. C Toxicol. Pharmacol. 2012, 155, 269–274. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sharma, H.S. Hyperthermia induced brain oedema: Current status and future perspectives. Indian J. Med. Res. 2006, 123, 629–652. [Google Scholar]
- Hardman, R. A toxicologic review of quantum dots: Toxicity depends on physicochemical and environmental factors. Environ. Health Perspect. 2006, 114, 165–172. [Google Scholar] [CrossRef] [PubMed]
- Muldoon, L.L.; Sàndor, M.; Pinkston, K.E.; Neuwelt, E.A. Imaging, distribution, and toxicity of superparamagnetic iron oxide magnetic resonance nanoparticles in the rat brain and intracerebral tumor. Neurosurgery 2005, 57, 785–796. [Google Scholar] [CrossRef] [PubMed]
- Pongrac, I.M.; Pavičić, I.; Milić, M.; Ahmed, L.B.; Babič, M.; Horák, D.; Vrček, I.V.; Gajović, S. Oxidative stress response in neural stem cells exposed to different superparamagnetic iron oxide nanoparticles. Int. J. Nanomed. 2016, 11, 1701–1715. [Google Scholar]
- Jeng, H.A.; Swanson, J. Toxicity of metal oxide nanoparticles in mammalian cells. J. Environ. Sci. Health Part A 2006, 41, 2699–2711. [Google Scholar] [CrossRef] [PubMed]
- Dal Bosco, L.; Weber, G.E.; Parfitt, G.M.; Paese, K.; Gonçalves, C.O.; Serodre, T.M.; Furtado, C.A.; Santos, A.P.; Monserrat, J.M.; Barros, D.M. Pegylated carbon nanotubes impair retrieval of contextual fear memory and alter oxidative stress parameters in the rat hippocampus. Biomed. Res. Int. 2015, 2015, 104135. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Sun, P.; Bao, Y.; Liu, J.; An, L. Cytotoxicity of single-walled carbon nanotubes on PC12 cells. Toxicol. In Vitro 2011, 25, 242–250. [Google Scholar] [CrossRef] [PubMed]
- Mahto, S.K.; Yoon, T.H.; Rhee, S.W. Cytotoxic effects of surface-modified quantum dots on neuron-like pc12 cells cultured inside microfluidic devices. Biochip J. 2010, 4, 82–88. [Google Scholar] [CrossRef]
- Sung, J.H.; Ji, J.H.; Yoon, J.U.; Kim, D.S.; Song, M.Y.; Jeong, J.; Han, B.S.; Han, J.H.; Chung, Y.H.; Kim, J. Lung function changes in sprague-dawley rats after prolonged inhalation exposure to silver nanoparticles. Inhal. Toxicol. 2008, 20, 567–574. [Google Scholar] [CrossRef] [PubMed]
- Lanone, S.; Rogerieux, F.; Geys, J.; Dupont, A.; Maillot-Marechal, E.; Boczkowski, J.; Lacroix, G.; Hoet, P. Comparative toxicity of 24 manufactured nanoparticles in human alveolar epithelial and macrophage cell lines. Part. Fibre Toxicol. 2009, 6, 14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ahamed, M.; Siddiqui, M.A.; Akhtar, M.J.; Ahmad, I.; Pant, A.B.; Alhadlaq, H.A. Genotoxic potential of copper oxide nanoparticles in human lung epithelial cells. Biochem. Biophys. Res. Commun. 2010, 396, 578–583. [Google Scholar] [CrossRef] [PubMed]
- Brunner, T.J.; Wick, P.; Manser, P.; Spohn, P.; Grass, R.N.; Limbach, L.K.; Bruinink, A.; Stark, W.J. In vitro cytotoxicity of oxide nanoparticles: Comparison to asbestos, silica, and the effect of particle solubility. Environ. Sci. Technol. 2006, 40, 4374–4381. [Google Scholar] [CrossRef] [PubMed]
- Könczöl, M.; Ebeling, S.; Goldenberg, E.; Treude, F.; Gminski, R.; Gieré, R.; Grobéty, B.; Rothen-Rutishauser, B.; Merfort, I.; Mersch-Sundermann, V. Cytotoxicity and genotoxicity of size-fractionated iron oxide (magnetite) in A549 human lung epithelial cells: Role of ROS, JNK, and NF-κB. Chem. Res. Toxicol. 2011, 24, 1460–1475. [Google Scholar] [CrossRef] [PubMed]
- Guan, R.; Kang, T.; Lu, F.; Zhang, Z.; Shen, H.; Liu, M. Cytotoxicity, oxidative stress, and genotoxicity in human hepatocyte and embryonic kidney cells exposed to zno nanoparticles. Nanoscale Res. Lett. 2012, 7, 602. [Google Scholar] [CrossRef] [PubMed]
- Davoren, M.; Herzog, E.; Casey, A.; Cottineau, B.; Chambers, G.; Byrne, H.J.; Lyng, F.M. In vitro toxicity evaluation of single walled carbon nanotubes on human A549 lung cells. Toxicol. In Vitro 2007, 21, 438–448. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, G.G.; Wang, C.-T.; Tang, H.-T.; Huang, Y.-S.; Yang, J. Zno nanoparticle-modified infrared internal reflection elements for selective detection of volatile organic compounds. Anal. Chem. 2006, 78, 2397–2404. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.J.; Kim, Y.J.; Lee, J.W.; Lee, Y.; Lim, Y.-B.; Chung, H.W. Cyto-/genotoxic effect of CdSe/ZnS quantum dots in human lung adenocarcinoma cells for potential photodynamic UV therapy applications. J. Nanosci. Nanotechnol. 2012, 12, 2160–2168. [Google Scholar] [CrossRef] [PubMed]
- Taju, G.; Majeed, S.A.; Nambi, K.; Hameed, A.S. In vitro assay for the toxicity of silver nanoparticles using heart and gill cell lines of catla catla and gill cell line of labeo rohita. Comp. Biochem. Physiol. C: Toxicol. Pharmacol. 2014, 161, 41–52. [Google Scholar] [CrossRef] [PubMed]
- Baratli, Y.; Charles, A.-L.; Wolff, V.; Tahar, L.B.; Smiri, L.; Bouitbir, J.; Zoll, J.; Piquard, F.; Tebourbi, O.; Sakly, M. Impact of iron oxide nanoparticles on brain, heart, lung, liver and kidneys mitochondrial respiratory chain complexes activities and coupling. Toxic. In Vitro 2013, 27, 2142–2148. [Google Scholar] [CrossRef] [PubMed]
- Hosseinpour, M.; Azimirad, V.; Alimohammadi, M.; Shahabi, P.; Sadighi, M.; Nejad, G.G. The cardiac effects of carbon nanotubes in rat. BioImpacts BI 2016, 6, 79–84. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harvey, J.; Dong, L.; Kim, K.; Hayden, J.; Wang, J. Uptake of single-walled carbon nanotubes conjugated with DNA by microvascular endothelial cells. J. Nanotechnol. 2011, 2012, 196189. [Google Scholar] [CrossRef]
- Nguyen, K.C.; Rippstein, P.; Tayabali, A.F.; Willmore, W.G. Mitochondrial toxicity of cadmium telluride quantum dot nanoparticles in mammalian hepatocytes. Toxicol. Sci. 2015, 146, 31–42. [Google Scholar] [CrossRef] [PubMed]
- Trop, M.; Novak, M.; Rodl, S.; Hellbom, B.; Kroell, W.; Goessler, W. Silver-coated dressing acticoat caused raised liver enzymes and argyria-like symptoms in burn patient. J. Trauma Acute Care Surg. 2006, 60, 648–652. [Google Scholar] [CrossRef] [PubMed]
- Mavon, A.; Miquel, C.; Lejeune, O.; Payre, B.; Moretto, P. In vitro percutaneous absorption and in vivo stratum corneum distribution of an organic and a mineral sunscreen. Skin Sharm. Physiol. 2007, 20, 10–20. [Google Scholar] [CrossRef] [PubMed]
- Alili, L.; Chapiro, S.; Marten, G.U.; Schmidt, A.M.; Zanger, K.; Brenneisen, P. Effect of Fe3O4 nanoparticles on skin tumor cells and dermal fibroblasts. BioMed Res. Int. 2015, 2015, 530957. [Google Scholar]
- Zhang, L.W.; Zeng, L.; Barron, A.R.; Monteiro-Riviere, N.A. Biological interactions of functionalized single-wall carbon nanotubes in human epidermal keratinocytes. Int. J. Toxicol. 2007, 26, 103–113. [Google Scholar] [CrossRef] [PubMed]
- Patlolla, A.; Knighten, B.; Tchounwou, P. Multi-walled carbon nanotubes induce cytotoxicity, genotoxicity and apoptosis in normal human dermal fibroblast cells. Ethn. Dis. 2010, 20, 65–72. [Google Scholar]
- Ryman-Rasmussen, J.P.; Riviere, J.E.; Monteiro-Riviere, N.A. Penetration of intact skin by quantum dots with diverse physicochemical properties. Toxicol. Sci. 2006, 91, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Samberg, M.E.; Oldenburg, S.J.; Monteiro-Riviere, N.A. Evaluation of silver nanoparticle toxicity in skin in vivo and keratinocytes in vitro. Environ. Health Perspect. 2010, 118, 407–413. [Google Scholar] [CrossRef] [PubMed]
- Arora, S.; Jain, J.; Rajwade, J.; Paknikar, K. Interactions of silver nanoparticles with primary mouse fibroblasts and liver cells. Toxicol. Appl. Pharm. 2009, 236, 310–318. [Google Scholar] [CrossRef] [PubMed]
- Derfus, A.M.; Chan, W.C.; Bhatia, S.N. Probing the cytotoxicity of semiconductor quantum dots. Nano Lett. 2004, 4, 11–18. [Google Scholar] [CrossRef] [PubMed]
- Murali, M.; Suganthi, P.; Athif, P.; Bukhari, A.S.; Mohamed, H.S.; Basu, H.; Singhal, R. Histological alterations in the hepatic tissues of Al2O3 nanoparticles exposed freshwater fish oreochromis mossambicus. J. Trace Elem. Med. Biol. 2017, 44, 125–131. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Ma, L.; Liu, J.; Zhao, J.; Yan, J.; Hong, F. Toxicity of nano-anatase TiO2 to mice: Liver injury, oxidative stress. Toxic. Environ. Chem. 2010, 92, 175–186. [Google Scholar] [CrossRef]
- Buford, M.C.; Hamilton, R.F.; Holian, A. A comparison of dispersing media for various engineered carbon nanoparticles. Part. Fibre Toxicol. 2007, 4, 6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kermanizadeh, A.; Gaiser, B.K.; Hutchison, G.R.; Stone, V. An in vitro liver model-assessing oxidative stress and genotoxicity following exposure of hepatocytes to a panel of engineered nanomaterials. Part. Fibre Toxicol. 2012, 9, 28. [Google Scholar] [CrossRef] [PubMed]
- Lin, P.; Chen, J.-W.; Chang, L.W.; Wu, J.-P.; Redding, L.; Chang, H.; Yeh, T.-K.; Yang, C.S.; Tsai, M.-H.; Wang, H.-J. Computational and ultrastructural toxicology of a nanoparticle, quantum dot 705, in mice. Environ. Sci. Technol. 2008, 42, 6264–6270. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.-D.; Wu, D.; Shen, X.; Liu, P.-X.; Fan, F.-Y.; Fan, S.-J. In vivo renal clearance, biodistribution, toxicity of gold nanoclusters. Biomaterials 2012, 33, 4628–4638. [Google Scholar] [CrossRef] [PubMed]
- Khlebtsov, N.; Dykman, L. Biodistribution and toxicity of engineered gold nanoparticles: A review of in vitro and in vivo studies. Chem. Soc. Rev. 2011, 40, 1647–1671. [Google Scholar] [CrossRef] [PubMed]
- Yan, G.; Huang, Y.; Bu, Q.; Lv, L.; Deng, P.; Zhou, J.; Wang, Y.; Yang, Y.; Liu, Q.; Cen, X. Zinc oxide nanoparticles cause nephrotoxicity and kidney metabolism alterations in rats. J. Environ. Sci. Health Part A 2012, 47, 577–588. [Google Scholar] [CrossRef] [PubMed]
- Privalova, L.I.; Katsnelson, B.A.; Loginova, N.V.; Gurvich, V.B.; Shur, V.Y.; Valamina, I.E.; Makeyev, O.H.; Sutunkova, M.P.; Minigalieva, I.A.; Kireyeva, E.P. Subchronic toxicity of copper oxide nanoparticles and its attenuation with the help of a combination of bioprotectors. Int. J. Mol. Sci. 2014, 15, 12379–12406. [Google Scholar] [CrossRef] [PubMed]
- Lewinski, N.; Colvin, V.; Drezek, R. Cytotoxicity of nanoparticles. Small 2008, 4, 26–49. [Google Scholar] [CrossRef] [PubMed]
- Demir, E.; Burgucu, D.; Turna, F.; Aksakal, S.; Kaya, B. Determination of TiO2, ZrO2, and Al2O3 nanoparticles on genotoxic responses in human peripheral blood lymphocytes and cultured embyronic kidney cells. J. Toxic. Environ. Health Part A 2013, 76, 990–1002. [Google Scholar] [CrossRef] [PubMed]
- Shang, S.; Yang, S.-Y.; Liu, Z.-M.; Yang, X. Oxidative damage in the kidney and brain of mice induced by different nano-materials. Front. Biol. 2015, 10, 91–96. [Google Scholar] [CrossRef]
- Reddy, A.R.N.; Krishna, D.; Himabindu, V.; Reddy, Y.N. Single walled carbon nanotubes induce cytotoxicity and oxidative stress in hek293 cells. Toxicol. Environ. Chem. 2014, 96, 931–940. [Google Scholar] [CrossRef]
- Mao, W.-P.; Ye, J.-L.; Guan, Z.-B.; Zhao, J.-M.; Zhang, C.; Zhang, N.-N.; Jiang, P.; Tian, T. Cadmium induces apoptosis in human embryonic kidney (HEK) 293 cells by caspase-dependent and-independent pathways acting on mitochondria. Toxicol. In Vitro 2007, 21, 343–354. [Google Scholar] [CrossRef] [PubMed]
- Sardari, R.R.R.; Zarchi, S.R.; Talebi, A.; Nasri, S.; Imani, S.; Khoradmehr, A.; Sheshde, S.A.R. Toxicological effects of silver nanoparticles in rats. Afr. J. Microbiol. Res. 2012, 6, 5587–5593. [Google Scholar]
- Krug, L.T.; Moser, J.M.; Dickerson, S.M.; Speck, S.H. Inhibition of NF-κB activation in vivo impairs establishment of gammaherpesvirus latency. PLoS Pathog. 2007, 3, e11. [Google Scholar] [CrossRef] [PubMed]
- Ates, M.; Demir, V.; Arslan, Z.; Kaya, H.; Yılmaz, S.; Camas, M. Chronic exposure of tilapia (oreochromis niloticus) to iron oxide nanoparticles: Effects of particle morphology on accumulation, elimination, hematology and immune responses. Aquat. Toxicol. 2016, 177, 22–32. [Google Scholar] [CrossRef] [PubMed]
- Clichici, S.; Biris, A.R.; Catoi, C.; Filip, A.; Tabaran, F. Short-term splenic impact of single-strand DNA functionalized multi-walled carbon nanotubes intraperitoneally injected in rats. J. Appl. Toxicol. JAT 2014, 34, 332–344. [Google Scholar] [CrossRef] [PubMed]
- Gagné, F.; Auclair, J.; Turcotte, P.; Fournier, M.; Gagnon, C.; Sauvé, S.; Blaise, C. Ecotoxicity of cdte quantum dots to freshwater mussels: Impacts on immune system, oxidative stress and genotoxicity. Aquat. Toxicol. 2008, 86, 333–340. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.; Hsieh, H.; Hsieh, Y.; Chiang, C.; Sun, Y.; Wang, C. The in vivo biodistribution and fate of cdse quantum dots in the murine model: A laser ablation inductively coupled plasma mass spectrometry study. Anal. Bioanal. Chem. 2012, 404, 3025–3036. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.-D.; Liu, J.; Yu, X.-F.; He, M.; Pei, X.-F.; Tang, Z.-Y.; Wang, Q.-Q.; Pang, D.-W.; Li, Y. The biocompatibility of quantum dot probes used for the targeted imaging of hepatocellular carcinoma metastasis. Biomaterials 2008, 29, 4170–4176. [Google Scholar] [CrossRef] [PubMed]
- Loeschner, K.; Hadrup, N.; Qvortrup, K.; Larsen, A.; Gao, X.; Vogel, U.; Mortensen, A.; Lam, H.R.; Larsen, E.H. Distribution of silver in rats following 28 days of repeated oral exposure to silver nanoparticles or silver acetate. Part. Fibre Toxicol. 2011, 8, 18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Singh, M.; Harris-Birtill, D.C.; Markar, S.R.; Hanna, G.B.; Elson, D.S. Application of gold nanoparticles for gastrointestinal cancer theranostics: A systematic review. Nanomed. Nanotechnol. Biol. Med. 2015, 11, 2083–2098. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.M.; Kunets, V.P.; Xie, Y.Z.; Schmidbauer, M.; Dorogan, V.G.; Mazur, Y.I.; Salamo, G.J. Multilayer self-organization of ingaas quantum wires on GaAs surfaces. Phys. Lett. A 2010, 375, 170–173. [Google Scholar] [CrossRef]
- Takenaka, S.; Karg, E.; Roth, C.; Schulz, H.; Ziesenis, A.; Heinzmann, U.; Schramel, P.; Heyder, J. Pulmonary and systemic distribution of inhaled ultrafine silver particles in rats. Environ. Health Perspect. 2001, 109, 547–551. [Google Scholar] [CrossRef] [PubMed]
- Pasupuleti, S.; Alapati, S.; Ganapathy, S.; Anumolu, G.; Pully, N.R.; Prakhya, B.M. Toxicity of zinc oxide nanoparticles through oral route. Toxicol. Ind. Health 2012, 28, 675–686. [Google Scholar] [CrossRef] [PubMed]
- Upadhyayula, V.K.; Deng, S.; Mitchell, M.C.; Smith, G.B. Application of carbon nanotube technology for removal of contaminants in drinking water: A review. Sci. Total Environ. 2009, 408, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Poland, C.A.; Duffin, R.; Kinloch, I.; Maynard, A.; Wallace, W.A.; Seaton, A.; Stone, V.; Brown, S.; MacNee, W.; Donaldson, K. Carbon nanotubes introduced into the abdominal cavity of mice show asbestos-like pathogenicity in a pilot study. Nature Nanotechnol. 2008, 3, 423–428. [Google Scholar] [CrossRef] [PubMed]
- Simkó, M.; Nentwich, M.; Gazsó, A.; Fiedeler, U. How Nanoparticles Enter the Human Body and Their Effects There; Nanotrust Dossier No. 003en; Institute of Technology Assessment of the Austrian Academy of Sciences: Vienna, Austria, 2010. [Google Scholar]
- Savolainen, K.; Alenius, H.; Norppa, H.; Pylkkänen, L.; Tuomi, T.; Kasper, G. Risk assessment of engineered nanomaterials and nanotechnologies—A review. Toxicology 2010, 269, 92–104. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Nagesha, D.K.; Selvarasah, S.; Dokmeci, M.R.; Carrier, R.L. Toxicity of cdse nanoparticles in Caco-2 cell cultures. J. Nanobiotechnol. 2008, 6, 11. [Google Scholar] [CrossRef] [PubMed]
- Stensberg, M.C.; Wei, Q.; McLamore, E.S.; Porterfield, D.M.; Wei, A.; Sepúlveda, M.S. Toxicological studies on silver nanoparticles: Challenges and opportunities in assessment, monitoring and imaging. Nanomedicine 2011, 6, 879–898. [Google Scholar] [CrossRef] [PubMed]
- He, Y.; Du, Z.; Ma, S.; Liu, Y.; Li, D.; Huang, H.; Jiang, S.; Cheng, S.; Wu, W.; Zhang, K. Effects of green-synthesized silver nanoparticles on lung cancer cells in vitro and grown as xenograft tumors in vivo. Int. J. Nanomed. 2016, 11, 1879–1887. [Google Scholar] [CrossRef] [PubMed]
- Selim, M.E.; Abd-Elhakim, Y.M.; Al-Ayadhi, L.Y. Pancreatic response to gold nanoparticles includes decrease of oxidative stress and inflammation in autistic diabetic model. Cell. Phys. Biochem. 2015, 35, 586–600. [Google Scholar] [CrossRef] [PubMed]
- Pašukonienė, V.; Mlynska, A.; Steponkienė, S.; Poderys, V.; Matulionytė, M.; Karabanovas, V.; Statkutė, U.; Purvinienė, R.; Kraśko, J.A.; Jagminas, A. Accumulation and biological effects of cobalt ferrite nanoparticles in human pancreatic and ovarian cancer cells. Medicina 2014, 50, 237–244. [Google Scholar] [CrossRef] [PubMed]
- Park, H.-S.; Kim, S.-J.; Lee, T.-J.; Kim, G.-Y.; Meang, E.; Hong, J.-S.; Kim, S.-H.; Koh, S.-B.; Hong, S.-G.; Sun, Y.-S. A 90-day study of sub-chronic oral toxicity of 20 nm positively charged zinc oxide nanoparticles in Sprague Dawley rats. Int. J. Nanomed. 2014, 9, 93–107. [Google Scholar]
- Nakayama, M.; Sasaki, R.; Ogino, C.; Tanaka, T.; Morita, K.; Umetsu, M.; Ohara, S.; Tan, Z.; Nishimura, Y.; Akasaka, H. Titanium peroxide nanoparticles enhanced cytotoxic effects of X-ray irradiation against pancreatic cancer model through reactive oxygen species generation in vitro and in vivo. Radiat. Oncol. 2016, 11, 91. [Google Scholar] [CrossRef] [PubMed]
- Mocan, T.; Matea, C.T.; Cojocaru, I.; Ilie, I.; Tabaran, F.A.; Zaharie, F.; Iancu, C.; Bartos, D.; Mocan, L. Photothermal treatment of human pancreatic cancer using pegylated multi-walled carbon nanotubes induces apoptosis by triggering mitochondrial membrane depolarization mechanism. J. Cancer 2014, 5, 679–688. [Google Scholar] [CrossRef] [PubMed]
- Chang, S.-Q.; Dai, Y.-D.; Kang, B.; Han, W.; Mao, L.; Chen, D. Uv-enhanced cytotoxicity of thiol-capped cdte quantum dots in human pancreatic carcinoma cells. Toxicol. Lett. 2009, 188, 104–111. [Google Scholar] [CrossRef] [PubMed]
- Zou, J.; Feng, H.; Mannerström, M.; Heinonen, T.; Pyykkö, I. Toxicity of silver nanoparticle in rat ear and BALB/c 3T3 cell line. J. Nanobiotechnol. 2014, 12, 52. [Google Scholar] [CrossRef] [PubMed]
- Kong, S.D.; Lee, J.; Ramachandran, S.; Eliceiri, B.P.; Shubayev, V.I.; Lal, R.; Jin, S. Magnetic targeting of nanoparticles across the intact blood–brain barrier. J. Control. Release 2012, 164, 49–57. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thompson, J.; Hipwell, E.; Loo, H.V.; Bannigan, J. Effects of cadmium on cell death and cell proliferation in chick embryos. Reprod. Toxic. 2005, 20, 539–548. [Google Scholar] [CrossRef] [PubMed]
- Gerber, A.; Bundschuh, M.; Klingelhofer, D.; Groneberg, D.A. Gold nanoparticles: Recent aspects for human toxicology. J. Occup. Med. Toxicol. 2013, 8, 32. [Google Scholar] [CrossRef] [PubMed]
- Park, J.-H.; Jeong, H.; Hong, J.; Chang, M.; Kim, M.; Chuck, R.S.; Lee, J.K.; Park, C.-Y. The effect of silica nanoparticles on human corneal epithelial cells. Sci. Rep. 2016, 6, 37762. [Google Scholar] [CrossRef] [PubMed]
- Olson, J.L.; Velez-Montoya, R.; Mandava, N.; Stoldt, C.R. Intravitreal silicon-based quantum dots as neuroprotective factors in a model of retinal photoreceptor degenerationsilicon quantum dots as neuroprotective factors. Investig. Ophthalmol. Vis. Sci. 2012, 53, 5713–5721. [Google Scholar] [CrossRef] [PubMed]
| Target | NP | Concentration, (Size), (Time), Route of Administration | Major Outcomes | Cell | In Vitro Effect |
|---|---|---|---|---|---|
| Brain | AuNP | 0.8–50 μg/mL, (3, 5, 7, 10, 30 and 60 nm), (24 h) | Only the smallest NP tested (3 nm) induced mild signs of cellular toxicity [76]. | rBMEC (primary rat brain microvessel endothelial cells) | Non-toxic even at highest concentrations in 24 h [76]. |
| 50 μg/mL (6–120 h) | - | Zebrafish cembryos | Time- and dose-dependent correlating increases in permeability and cytotoxicity of cells [77]. | ||
| AgNP | 6.25–50 μg/mL, (25, 40 or 80 nm in size), (24 h) | Time- and dose-dependent increase in pro-inflammatory cytokine release and related rises in permeability and cytotoxicity of cells [76]. | rBMEC (primary rat brain microvessel endothelial cells) | Time- and dose-dependent increase in pro-inflammatory cytokine release and correlating increases in permeability and cytotoxicity of cells [78]. | |
| Cu | 30–50 mg/Kg | increasing toxicity on neuromuscular system and increase NPs penetration of the blood-brain barrier [78]. | - | - | |
| Al | 30–50 mg/Kg | increasing toxicity on neuromuscular system and increase NPs penetration of the blood-brain barrier [78]. | - | - | |
| CdSe | 1, 10, 20 nm, (24 h) | - | Primary rat hippocampal neuron cells in culture | Decrease of cells viability [79]. | |
| Superparamagnetic iron-oxide nanoparticles (SPION) | 208 or 1042 μg/mL of: Ferumoxtran-10; Ferumoxytol (20–50 nm); Ferumoxide (60–185 nm) (3 months) | Increasing uptake NPs into the CNS parenchyma [80]. | Murine neural stem cells (NSCs) | Depleted intracellular glutathione levels, altered activities of SOD and GPx, hyperpolarization of the mitochondrial membrane, dissipated cell-membrane potential and increased DNA damage [81]. | |
| TiO2 | 30–45 nm, (2–72 h) | leakage of lactate dehydrogenase (LDH) [82] | Neuro-2A | permeability of NPs in plasma membrane, increasing apoptosis [82]. | |
| ZnO | |||||
| Fe2O3 | |||||
| Al2O3 | |||||
| CrO3 | |||||
| CNT | PEG-SWCNTs at concentrations of 0.5, 2.1 and 1 mg/mL | Accumulation in the hippocampus which induces oxidative stress [83]. | PC12 cells | Decreased mitochondrial membrane potential (MMP), induced ROS and increased the level of lipid peroxide and decreased the activities of superoxide dismutase (SOD), glutathione peroxidase (GSH-Px), catalase (CAT) and glutathione (GSH) [84]. | |
| QD | 0.68 mg containing 50 nmol Cd (13.5 nm in size), (6 h) Intraperitoneal | Moderately high quantities of Cd ions was observed in brain tissue but no signs of inflammation or parenchymal damage were detected [74]. | Neuron like PC12 cells | Cell death, axonal degeneration [85]. | |
| Lung | AgNP | 515 g/m3, (6 h/day, 5 days/week for 13 weeks), inhalation | Dose- and time-dependent increase in blood Ag nanoparticle concentration was observed along with correlating increases in alveolar inflammation and small granulomatous lesions [86]. | - | - |
| Cu | 0.1–3300 µg/mL, (3 and 24 h) | - | Human pulmonary cell line (lung adenocarcinoma epithelial cell line (A549)) | Mitochondria-dependent cellular apoptosis associated with ROS [87]. | |
| Zn | |||||
| CO | |||||
| Sb | |||||
| Ag | |||||
| Ni | |||||
| Fe | |||||
| CuO | 0–40 μg/cm2 | - | Human lung epithelial cells (A549) | Mitochondria-dependent cellular apoptosis associated with DNA damage [88]. | |
| SPION | 200–1000 μg/mL, (24 h) | Increased cytokines, inflammation, TNF-α [89]. | Human lung epithelial cells (A549) | Activation of JNK, stimulation of tumor necrosis factor-alpha (TNFα), reduction of NF-kB, increased ROS [90]. | |
| SWCNT | 10–100 μg/mL (24 h, 48 h and 72 h) | Dose- and time-dependent decline in cell viability: up to 50% decrease at maximum dosage after 72 h. Oxidative stress was exhibited as a mechanism of cytotoxicity [91]. | Human lung epithelial cells (A549) | low acute toxicity was confirmed with the in vivo model by dispersion of SWCNTs in serum [92]. | |
| QD | 12.5 µg, (7 days) | Increased levels of LDH and albumin [93]. | Human lung adenocarcinoma cells | Mitochondria-dependent cellular apoptosis associated with decrease of cells viability [94]. | |
| Heart | AgNPs | 100, 1000 and 10,000 ppm, (period of 13 weeks) | increasing cardiocyte deformity, congestion and inflammation [71]. | Catla heart cell line (SICH) | Increased lipid peroxidation (LPO) level and decreased level of GSH, SOD and CAT [95]. |
| Iron oxide NPs | 100, 200, 300 and 500 μg/mL, (period of 2 weeks) | Showed that baseline maximal oxidative capacities were proteins in the heart [96]. | Cardiac microvascular endothelial cells | Induced a concentration- and time-dependent cytotoxicity with decrease of cells viability | |
| CNT | 1–0.3 mg/Kg body weight | Blocks potassium channels. The suppressed and inhibited IK and potassium channels lead to increased heart rate [97]. | Microvascular Endothelial Cells | Dose- and time-dependent increasing DNA damage [98]. | |
| QD | - | - | Human hepatocellular carcinoma, HepG2 cells | Mitochondria-dependent cellular apoptosis associated with ROS [99]. | |
| Dermal | AgNP | 50 and 100 μg/mL, (24 h) | Mitochondria-dependent cellular apoptosis related to ROS at a concentration of ≥ 50 μg/mL [100]. | A431 (human skin carcinoma) | No evidence for Cellular damage up to a concentration of 6.25 g/mL. Morphological changes at concentrations between 6.25 and 50 g/mL with concomitant rise in GSH, SOD and lipid peroxidation. DNA fragmentation suggests cell death by apoptosis [101]. |
| TiO2 | 15 μg/cm2, (24 h) | Cytotoxicity was detected to be apoptosis [101]. | HaCaT (keratinocyte cell line), human dermal fibroblasts, human immortalized sebaceous gland cell line (SZ95) | Cytotoxicity was observed to be affecting cellular functions such as cell proliferation, differentiation and mobility resulting in apoptosis [70]. | |
| Fe3O4 | 65 nm | - | Skin tumor cells | Increases ROS, deceasing cancer cells [102]. | |
| CNT | 10 μg/mL, (72 h) | NPs increased relatively IL8 and ROS factors in animal [103]. | Human Dermal Fibroblast Cells | Mitochondria-dependent cellular apoptosis associated with decrease cell viability [104]. | |
| QD | 4.6 nm core/shell diameter QD for 8 h and 24 h | Increased IL-1b, IL-6, and IL-8 [105]. | Human epidermal keratinocytes (HEKs) | Increased IL-1β, IL-6, IL-8, and TNF-α factors [106]. | |
| Liver | AgNPs | 10, 50, 100, 150, 200, 400 ppm for 24 h | - | Primary mouse fibroblasts, primary hepatocytes | Production of mediators of oxidative-stress. increase GSH [107]. |
| CdSe | 62.5–1000 µg/mL, (1–8 h) | - | Primary rat hepatocytes | Evidence for cellular damage up to a concentration of 62.5 µg/mL with concomitant rise in GSH, SOD and lipid peroxidation [108]. | |
| ZnO NPs | 100, 300 and 600 mg/Kg, (7 days) | - | Human hepatocyte (L02) | Mitochondria-dependent cellular apoptosis associated with ROS, reduction of SOD, depletion of GSH, and oxidative DNA damage [91]. | |
| Al2O3 | 235,245 ppm | Blood cell and melanoma macrophage accumulation, hepatocyte necrosis, vaculation and portal vein alteration [109]. | - | - | |
| TiO2 | 5, 10, 50, 100 or 150 mg/Kg, (daily for 14 days) | NPs increased relatively IL-8 and ROS factors in animal [110]. | Rat liver derived cell line (BRL 3A) | Mitochondria-dependent cellular apoptosis associated with ROS, reduction of SOD, depletion of GSH, and oxidative DNA damage [9]. | |
| CNT | ~25 μg/cm2 | NPs increased relatively apoptosis factor in animal [111]. | Human hepatoblastoma C3A cell line | Mitochondria-dependent cellular apoptosis associated with ROS, IL8, reduction of SOD, depletion of GSH, and oxidative DNA damage [112]. | |
| QDs | 1000 µg/mL, (24 h) | NPs increased relatively ROS in liver [113]. | Primary rat hepatocytes | Cytotoxicity was thought to be due to the release of free cadmium ions [108]. | |
| Kidney | AuNPs | 5, 10,100 ppm, (via IP injection for 7 successive days) | Increase levels of CREA, UREA, total bilirubin ALP in rats’ blood serum were examined to show a degree of kidney functionality [114]. | Embryonic kidney cells (HEK293). | Toxicity was dose dependent. In a dose of 44 mg/mL for 4 h, toxicity was observed on DNA/transferrin [115]. |
| ZnO NPs | 100, 300 and 1000 mg/Kg in 2 weeks | Significant increase in serum creatinine and blood urea nitrogen, decrease in hemoglobin, haematocrit and mean corpuscular hemoglobin concentration [116]. | Human embryonic kidney (HEK293) cells | Lead to cellular morphological modifications, mitochondrial dysfunction, and cause reduction of SOD, depletion of GSH, and oxidative DNA damage [91]. | |
| CuO NPs | A dose of 10 mg/Kg three times a week up to 19 injections | Toxicity showed with DNA fragmentation [117]. | Embryonic kidney cells (HEK293) | Increased ROS, decreased cell viability [118] | |
| TiO2 | 1, 10, 100 µg/mL | Embryonic kidney cells | - | DNA damage and genomic toxicity [119]. | |
| CNT | 4 mg/Kg, (7 days) | Increase level of IL-8, LDH and lipid peroxidation in serum [120]. | Embryonic kidney cells (HEK293) | Decreased cell viability, increase cell membrane damage, LDH release, reduced glutathione (GSH), interleukin-8 (IL-8), lipid peroxidation [121] | |
| QD | 1.5 µmol/Kg, (1, 7, 14, and 28 days) | - | Embryonic kidney cells (HEK293) | Time-dependent decrease of mitochondrial transmembrane potential, up regulate Bcl-2 expression, alleviated apoptosis [122]. | |
| Spleen | AgNPs | 30, 300 and 1000 mg/Kg doses of AgNPs (60 nm), 28 days of oral administration | Ag induces the permeability of cell membrane to potassium and sodium and interrupts the activity of Na-K-ATPase and mitochondria. Inhibition of NF-kB activity, a decrease in expression bcl-2, increase in caspase-3 expression [123,124]. | - | - |
| Fe2O3 | 0.1, 0.5 and 1.0 mg/L (9.2 × 10−4, 4.6 × 10−3 and 9.2 × 10−3 mM) aqueous suspensions for 60 days | Accumulated in the spleen organ and induce acute toxicity [125]. | - | - | |
| CNT | 1.5 mL; 2 mg multi-walled (MW) CNT per body weight (bw), (1, 6, 24, 48 and 144 h) | After i.p. administration, MWCNT translocate progressively in the spleen, with a peak of concentration after 48 h, and determine lymphoid hyperplasia and an increase in the number of cells which undergo apoptosis, in parallel with the enhancement of the mitosis in the white pulp and with transient alterations of oxidative stress and inflammation [126]. | - | - | |
| QD | 6000 g for 10 min, | Distribution in different body organs and aggregation in spleen [127,128,129] | - | - | |
| Stomach | AgNPs | 28-day repeated oral dose of AgNPs of 60 nm, 2.6 mg Ag/Kg b.w./day | Aggregation in stomach tissues [130]. | - | - |
| Au NPs | - | - | Gastrointestinal cancer cells | Removing tumor cells from healthy cells [131]. | |
| CdSe | 0.84 × 105 µm | - | Human colon carcinoma cell line | Removing tumor cells from healthy cells [132]. | |
| TiO2 NPs | 1012 particles/person per day in 2 weeks | Aggregation in stomach tissues [133]. | - | - | |
| ZnO NPs | 5, 50, 300, 1000 and 2000 mg/Kg b.w | Aggregation in stomach tissues [134]. | - | - | |
| CNT | <5 µm, 10–20 µm, (7 days) | Inflammation [135,136,137,138] | - | - | |
| QD | 2 to 200 nmol/mL, (24 h) | NPs increased relativel ROS factors in animal [139] | - | - | |
| Pancreas | Ag NPs | AgNPs (100 μg/mL), (24 h) | NPs increased relatively ROS factors in animal [140]. | Pancreas cancer BxPC-3 Cells | Inhibition of NF-kB activity, a decrease in bcl-2, and an increase in caspase-3 and survivin expression [141]. |
| AuNPs | 50 nm, 2.5 mg/Kg, Male Wistar diabetic with autism spectrum disorder pups, i.p. 7 day | NPs increased relatively ROS factors in animal [142] | - | - | |
| cobalt ferrite NPs | - | - | human pancreatic cancer cells | Accumulation in cells increasing apoptosis [143]. | |
| ZnO NPs | 0, 500, 1000, and 2000 mg/Kg/day for 14 days. | Decreased body weight, feed consumption, alterations in blood factors (HB, HCT, MCV, MCH, MCHC, and LYM) and increase in blood cells (WBCs and NEUs), and histopathological alterations in the pancreas [144]. | - | - | |
| TiO2 | 42 days | - | Pancreatic cancer cells (PANC-1) | Tumor growth inhibition and induce cell toxicity [145]. | |
| CNT | 5, 10 and 50 μg/mL | - | Pancreatic cancer cells (PANC-1) | Hyperthermia; necrosis of malignant cells [146] | |
| QD | 0.2 mL, (7 h) | NPs increased relatively ROS factors in animal organ [147]. | - | - | |
| Ear | AgNPs | 4000 μg/mL AgNPs induced | Hearing loss with partial recovery within 7 days and increasing ROS in animal organ [148]. | BALB/c 3T3 cell line | Impairment of the mitochondrial function [148]. |
| SPION | 150 μL of 15 mg/mL, (1–4 h, 4 and 7 days) | Uptake into the CNS parenchyma [149]. | - | - | |
| CNT | 150 μL of 15 mg/mL, (1, 2, 4 h, 4 and 7 days | Accumulation in CNS parenchyma. No pathological alterations were observed [150]. | - | - | |
| QD | 1 mg/mL or 4.5 mg/mL), (24 h) | Limb abnormalities, body wall defects, neural tube defects [150]. | - | - | |
| Eye | AuNPs | 2, 20 and 200 nm, 72 h | NPs increased relatively ROS factors in animal [151]. | Human corneal cells | Increasing apoptosis and aberrant expression factor pigmentation, development (pax6a, pax6b, otx2, and rx1) and pigmentation (sox10) [151]. |
| Iron oxide | 2, 20 and 200 nm, (72 h) | NPs increased relatively ROS factors in animal [151]. | - | - | |
| Silica NPs | 50, 100 and 150 nm, (48 h) | NPs increased relatively ROS in cell [152]. | - | - | |
| CNT | Up to 750 nm every week for 9 weeks | Eye-irritation, retinal degeneration [74]. | - | - | |
| QD | 17 weeks of age, in the range of 2.7–3.6 Kg in body weight | Eye-irritation, retinal degeneration [153]. | - | - |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ajdary, M.; Moosavi, M.A.; Rahmati, M.; Falahati, M.; Mahboubi, M.; Mandegary, A.; Jangjoo, S.; Mohammadinejad, R.; Varma, R.S. Health Concerns of Various Nanoparticles: A Review of Their in Vitro and in Vivo Toxicity. Nanomaterials 2018, 8, 634. https://doi.org/10.3390/nano8090634
Ajdary M, Moosavi MA, Rahmati M, Falahati M, Mahboubi M, Mandegary A, Jangjoo S, Mohammadinejad R, Varma RS. Health Concerns of Various Nanoparticles: A Review of Their in Vitro and in Vivo Toxicity. Nanomaterials. 2018; 8(9):634. https://doi.org/10.3390/nano8090634
Chicago/Turabian StyleAjdary, Marziyeh, Mohammad Amin Moosavi, Marveh Rahmati, Mojtaba Falahati, Mohammad Mahboubi, Ali Mandegary, Saranaz Jangjoo, Reza Mohammadinejad, and Rajender S. Varma. 2018. "Health Concerns of Various Nanoparticles: A Review of Their in Vitro and in Vivo Toxicity" Nanomaterials 8, no. 9: 634. https://doi.org/10.3390/nano8090634