Figure 1.
Diagrams showing the various measurements of both the NPC and IF carried out in the present study. (a) Sagittal view of the NPC, Line 1 – Diameter of the NPC at the level of Stenson’s foramen, Line 2 – Diameter at mid-point of NPC, Line 3 – Diameter at the level of IF, Line 4 – Length of NPC, Line 5 – Thickness of maxillary bone at the alveolar crest, Line 6 – Thickness of maxillary bone at mid-point, Line 7 – Thickness of maxillary bone at nasal spine. (b) Sagittal view of the NPC, Angle 1 – Angulation of maxillary bone from the horizontal plane, Angle 2 – Angulation of NPC from the horizontal plane. (c) Coronal view of the NPC, Line A – Diameter of NPC at Stenson’s foramen, Line B – Diameter at mid-point of NPC, Line C – Diameter at the level of IF. 1d: Axial view at the level of IF, Line I – Mediolateral diameter of IF, Line II – Anteroposterior diameter of IF.
Figure 1.
Diagrams showing the various measurements of both the NPC and IF carried out in the present study. (a) Sagittal view of the NPC, Line 1 – Diameter of the NPC at the level of Stenson’s foramen, Line 2 – Diameter at mid-point of NPC, Line 3 – Diameter at the level of IF, Line 4 – Length of NPC, Line 5 – Thickness of maxillary bone at the alveolar crest, Line 6 – Thickness of maxillary bone at mid-point, Line 7 – Thickness of maxillary bone at nasal spine. (b) Sagittal view of the NPC, Angle 1 – Angulation of maxillary bone from the horizontal plane, Angle 2 – Angulation of NPC from the horizontal plane. (c) Coronal view of the NPC, Line A – Diameter of NPC at Stenson’s foramen, Line B – Diameter at mid-point of NPC, Line C – Diameter at the level of IF. 1d: Axial view at the level of IF, Line I – Mediolateral diameter of IF, Line II – Anteroposterior diameter of IF.
Figure 2.
Axial CBCT sections showing the number of Stenson’s foramina. (a) Single foramen (b) 2 foramina (c) 3 foramina.
Figure 3.
Representative sagittal CBCT sections of the NPC showing the various shapes encountered in the study with, a clustered column bar chart showing the shape prevalence of the NPC in a sagittal view for both male and female Kenyans. A combined percentage value for both genders is also depicted. (a) Cylindrical (b) Hourglass (c) Conical (d) Banana (e) Funnel (f) Tree branch.
Figure 3.
Representative sagittal CBCT sections of the NPC showing the various shapes encountered in the study with, a clustered column bar chart showing the shape prevalence of the NPC in a sagittal view for both male and female Kenyans. A combined percentage value for both genders is also depicted. (a) Cylindrical (b) Hourglass (c) Conical (d) Banana (e) Funnel (f) Tree branch.
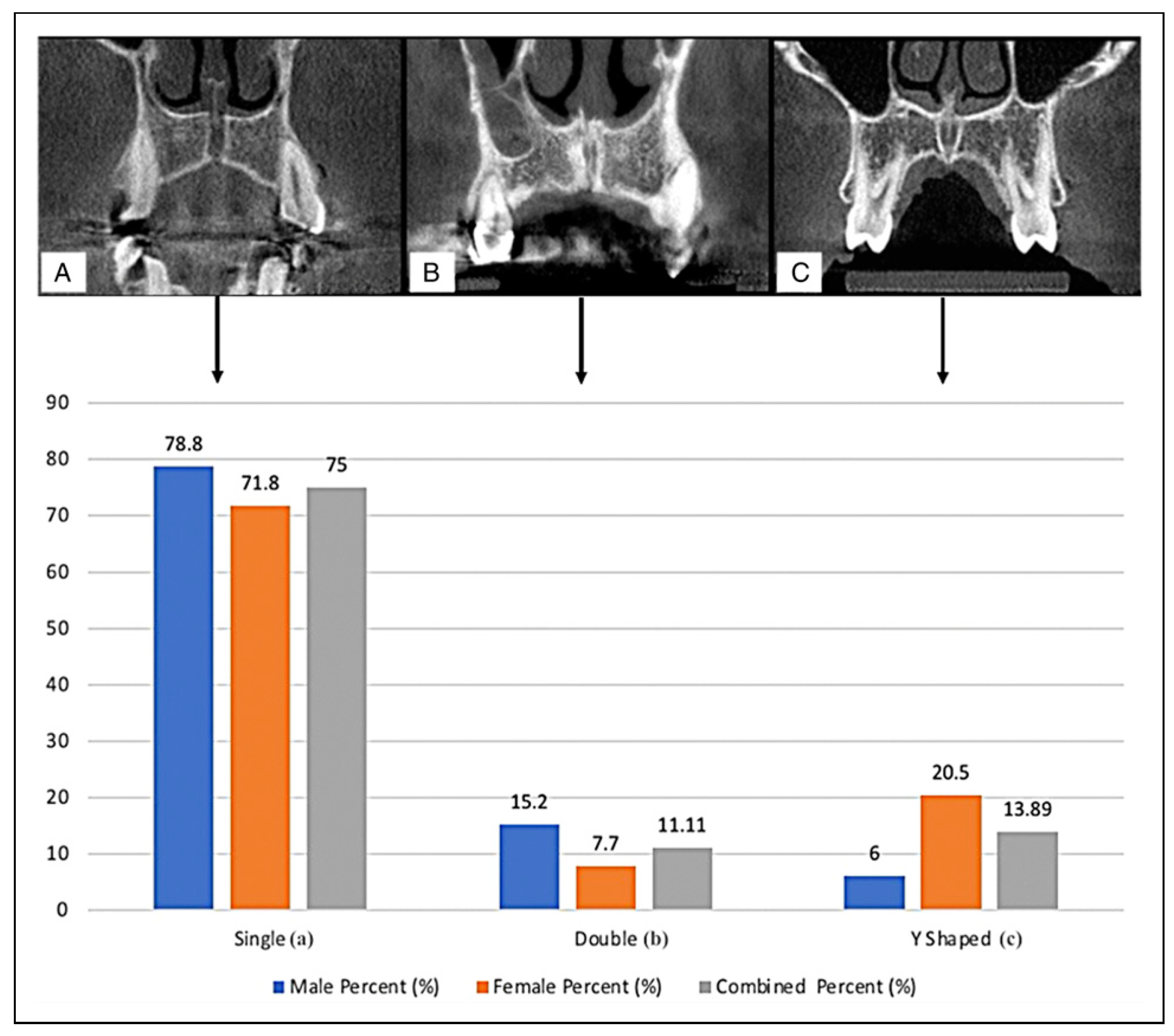
Figure 4.
Representative coronal CBCT sections of the NPC showing the various shapes encountered in the study with a clustered column bar chart showing the shape prevalence of the NPC in a coronal view for both male and female Kenyans. A combined percentage value for both genders is also depicted. (a) Single (b) Double (c) Y-shaped.
Figure 4.
Representative coronal CBCT sections of the NPC showing the various shapes encountered in the study with a clustered column bar chart showing the shape prevalence of the NPC in a coronal view for both male and female Kenyans. A combined percentage value for both genders is also depicted. (a) Single (b) Double (c) Y-shaped.
Figure 5.
Representative axial CBCT sections of the IF showing the various shapes encountered in the study, with a clustered column bar chart showing the shape prevalence of the IF for both male and female Kenyans. A combined percentage value for both genders is also depicted. (a) Round (b) Oval (c) Teardrop (d) Heart (e) Diamond (f) Triangle.
Figure 5.
Representative axial CBCT sections of the IF showing the various shapes encountered in the study, with a clustered column bar chart showing the shape prevalence of the IF for both male and female Kenyans. A combined percentage value for both genders is also depicted. (a) Round (b) Oval (c) Teardrop (d) Heart (e) Diamond (f) Triangle.
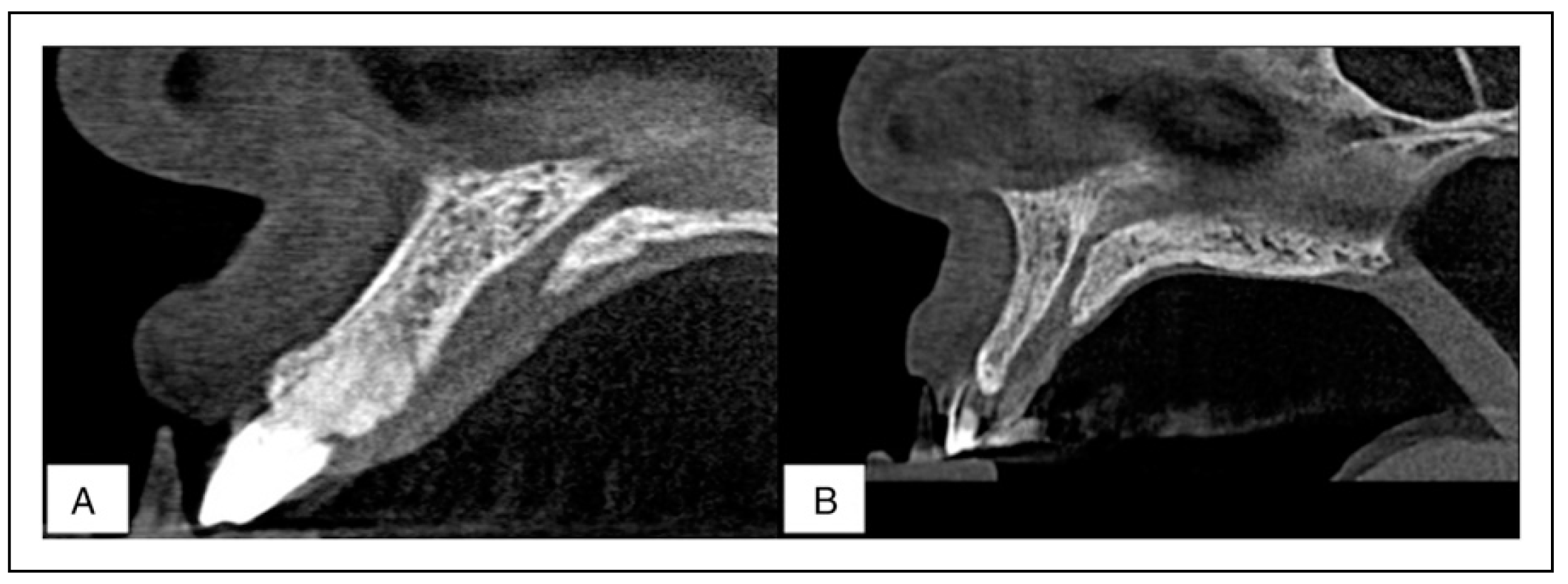
Figure 6.
Sagittal CBCT sections of the maxillary bone both the flat (a) and concave (b) shapes encountered in the present study.
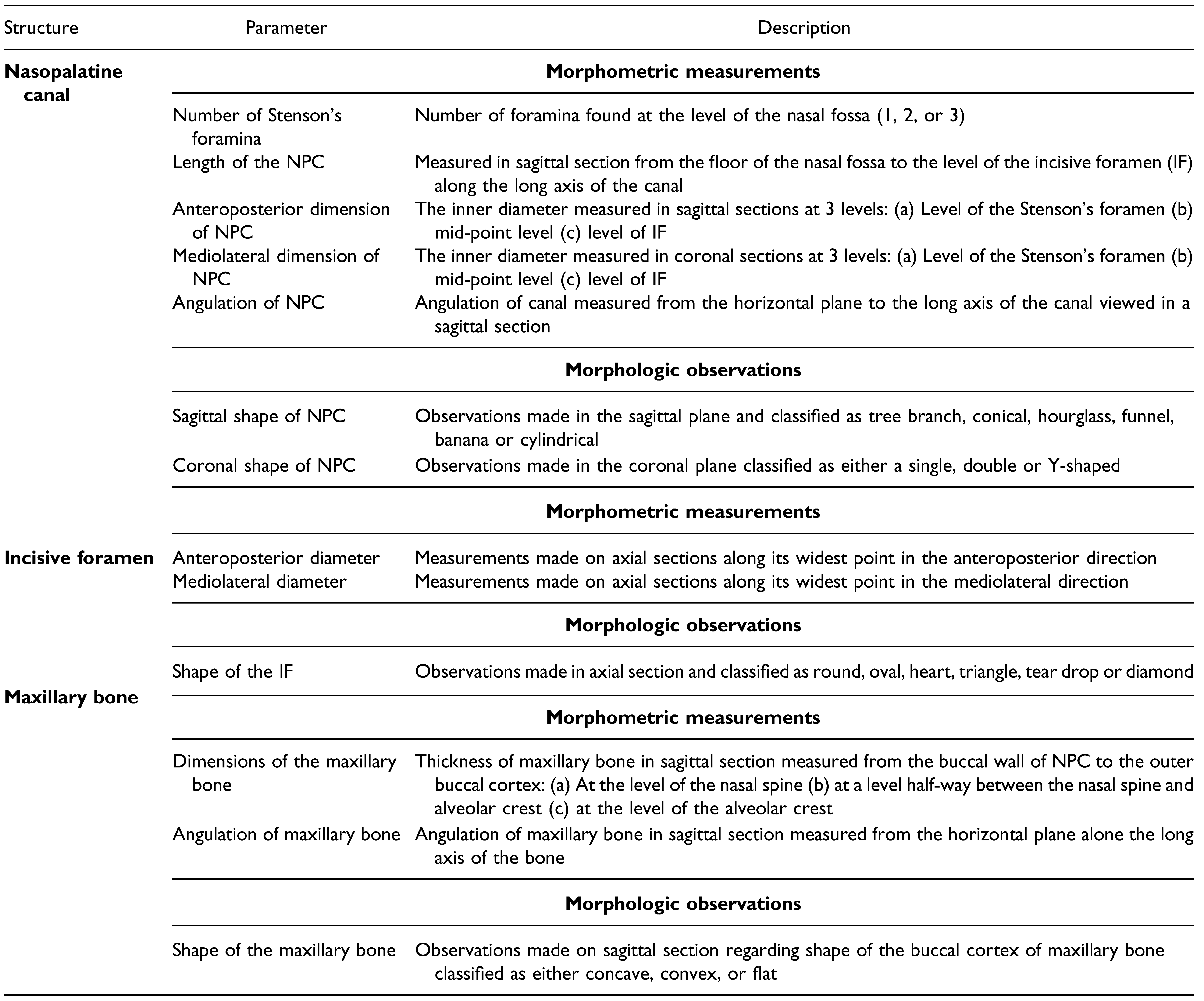
Table 1.
Description of Morphometric Measurements and Morphological Observations Performed in the Present Study.
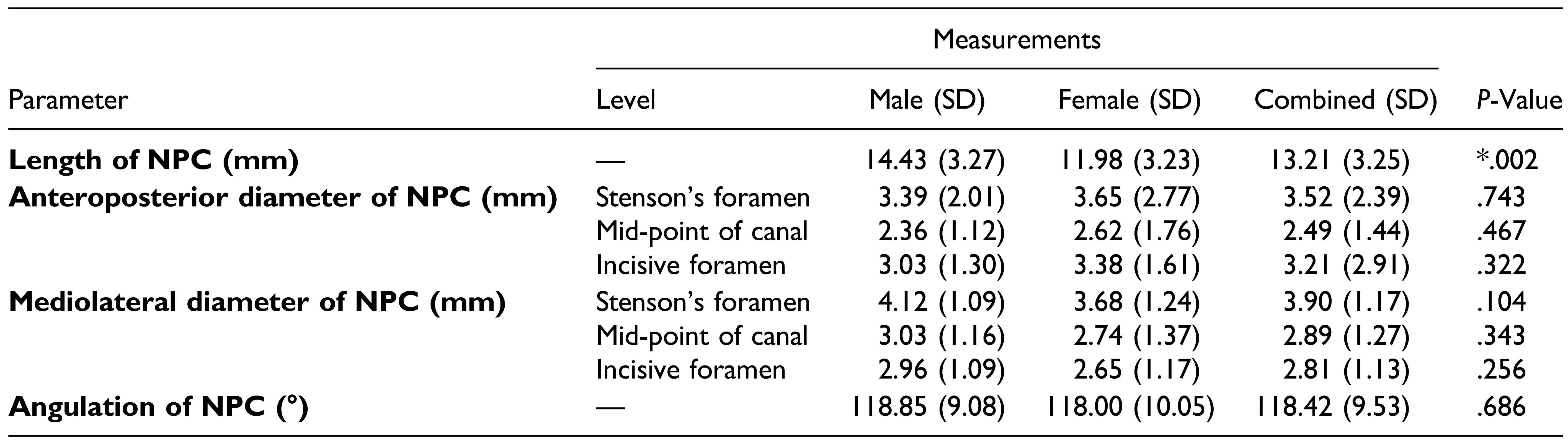
Table 2.
Morphometric Measurements of the NPC with Standard Deviations (SD) and P-Values for both Males and Females (*Independent t-test, P <.05).
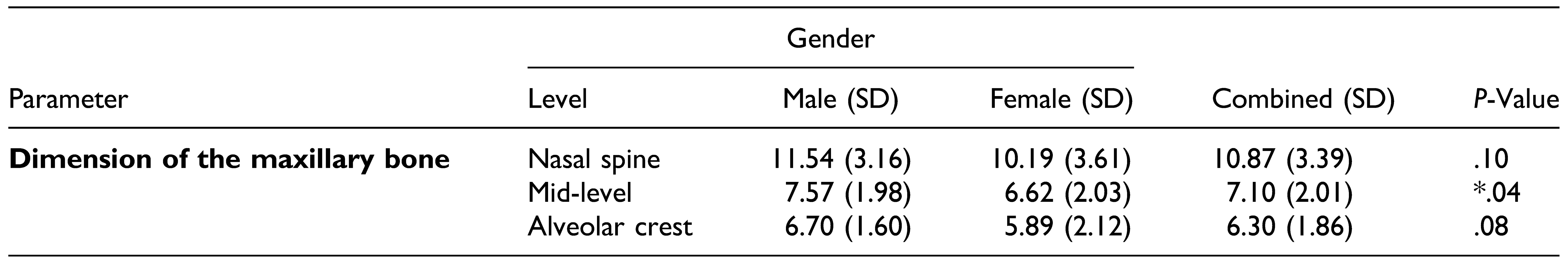
Table 3.
Dimensions of the Maxillary Bone at 3 Different Levels for Both Male and Female Kenyans (*Independent t-test, P <.05).
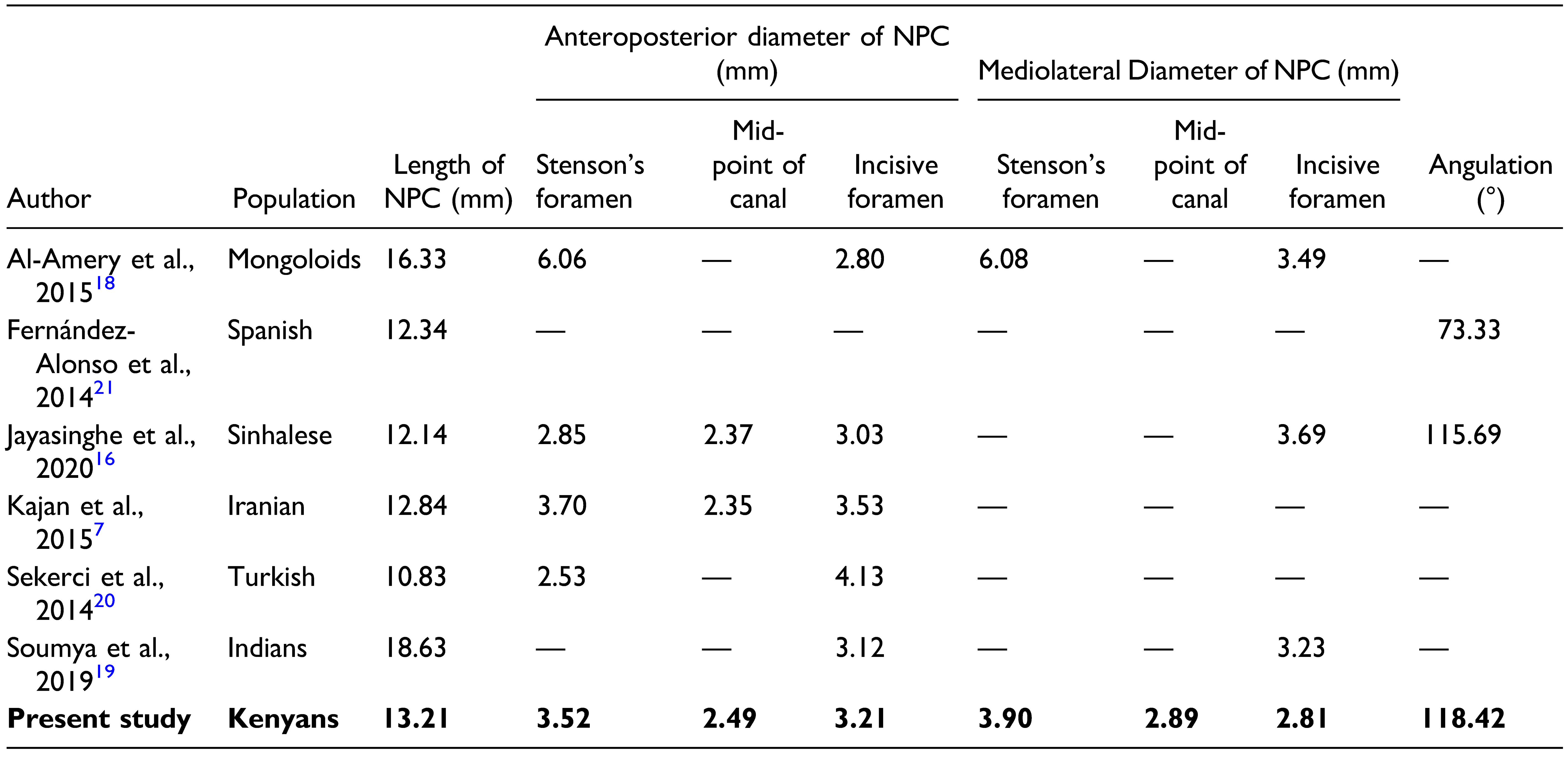
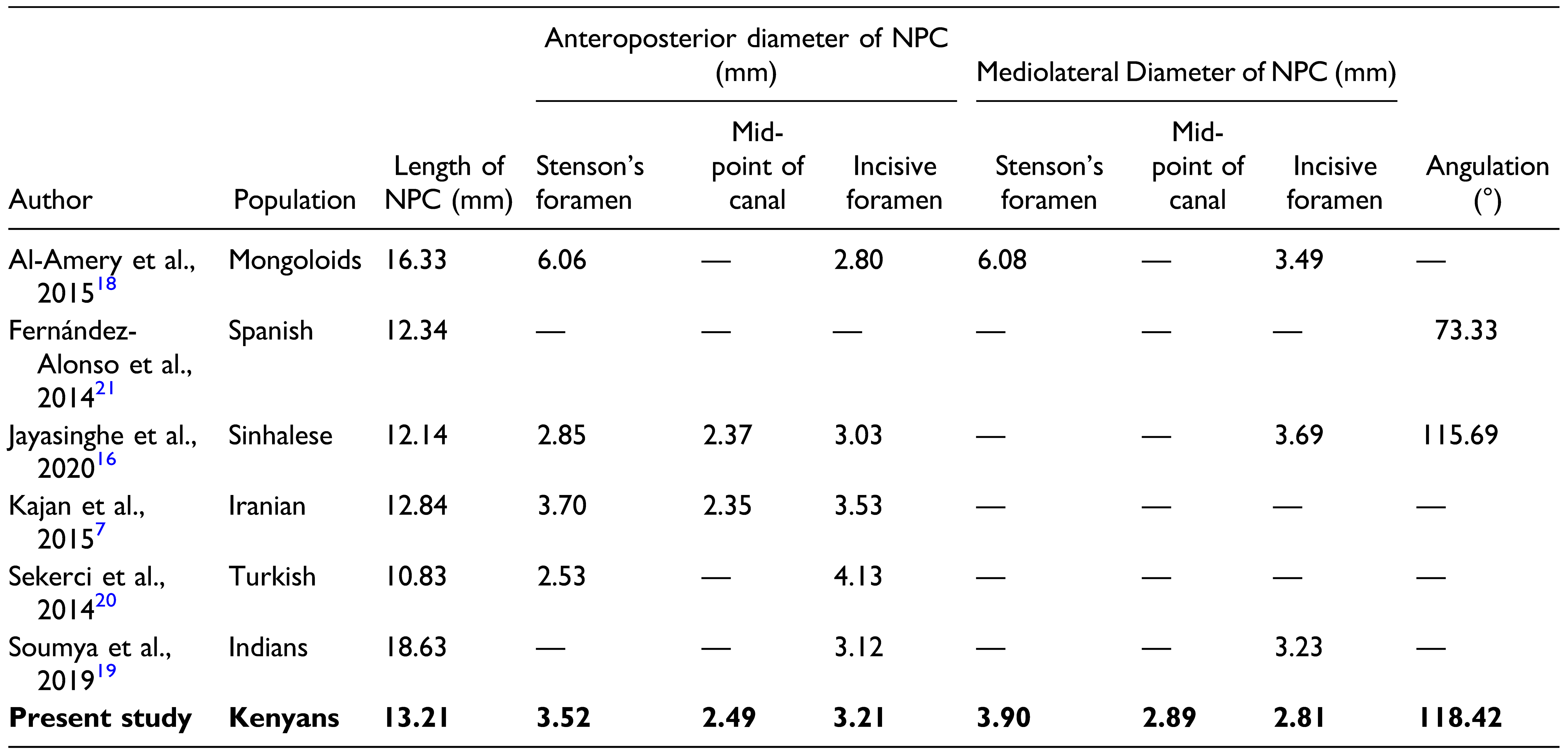
Table 4.
The NPC Dimensions of the Kenyan in Comparison with the Different Populations.
Table 5.
The Shape of the NPC (in the Sagittal View) of the Kenyan Compared with Other Populations.
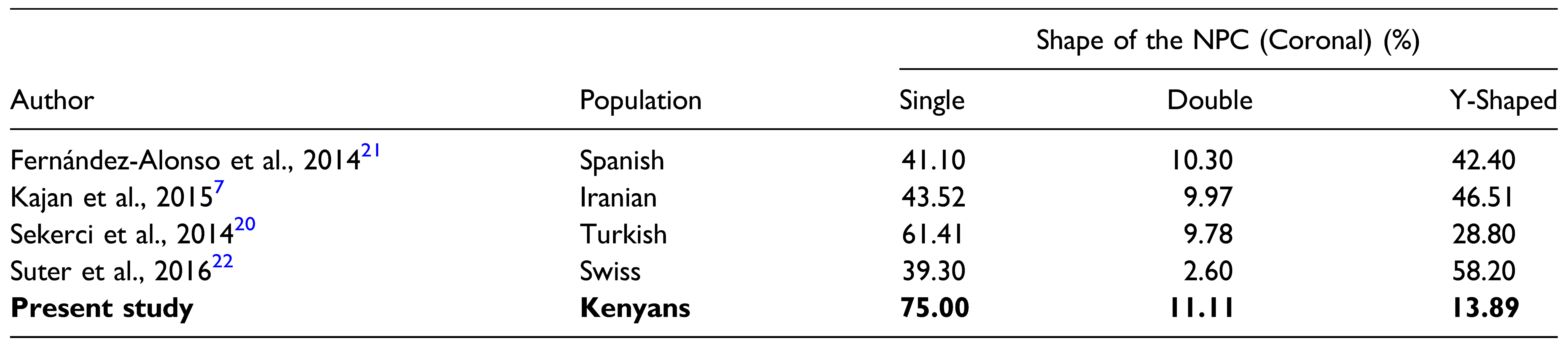
Table 6.
The Shape of the NPC (in the Coronal View) of the Kenyan Compared with Other Populations.
Table 7.
The Shape of the IF of the Kenyan Compared with Other Populations.
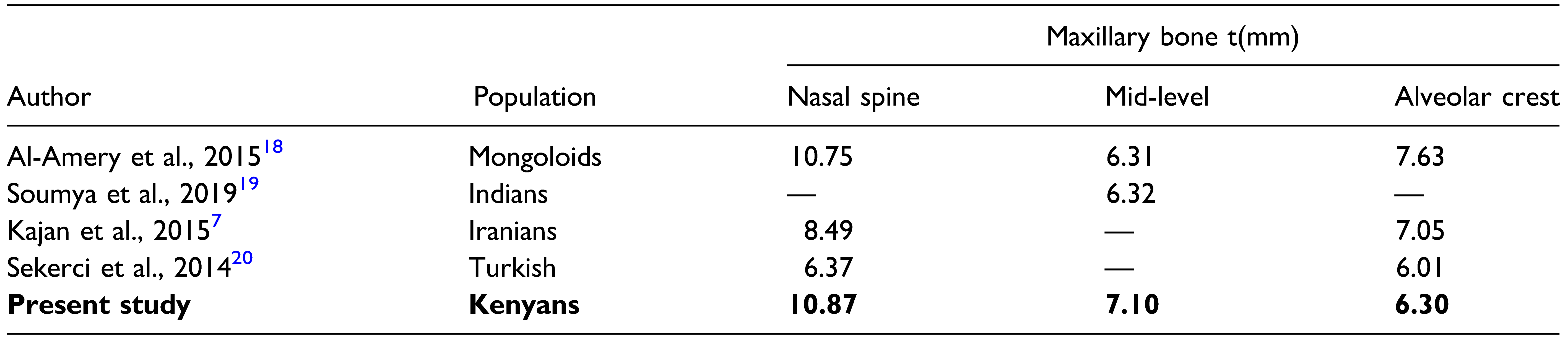
Table 8.
The maxillary Bone Thicknesses of Kenyan Compared with Different Populations.