Abstract
Recent decades have seen a rapid advancement in nonsurgical facial rejuvenation techniques due to technological advances and growing patient preference for minimally invasive aesthetic procedures. Laser resurfacing and chemical peels are two popular modalities that address aging skin, improve skin texture, and reduce signs of photodamage. In this work, we examine the historical evolution of these modalities, review current trends, and analyze their comparative efficacy in the context of facial rejuvenation. We discuss each modalities’ mechanisms, clinical indications, efficacy, and safety profiles. We additionally explore the impact of emerging technologies, such as fractional lasers, picosecond lasers, and novel chemical peel formulations, on patient outcomes, recovery times, and novel indications. Furthermore, we consider how recent advances have enabled safer and more effective treatment across diverse skin types, focusing primarily on higher Fitzpatrick skin. Additionally, a scoping review including adjunctive and non-surgical modalities is discussed and synthesized to highlight current evidence, clinical guidelines, and technological advances. This review aims to guide clinicians in optimizing procedure choice and patient outcomes in nonsurgical facial rejuvenation.
1. Introduction
1.1. Background: The Rise of Nonsurgical Facial Rejuvenation
Over the past decade, the landscape of facial rejuvenation has undergone a paradigm shift, driven by increasing patient demand for interventions offering minimal downtime, reduced procedural risk, and natural-looking outcomes [1]. In 2023, there were over 25 million minimally invasive procedures recorded in the United States, with a 7% increase from 2022. Skin resurfacing, comprising chemical peels, lasers, dermabrasion, and microdermabrasion, represents one of the top five most popular cosmetic minimally invasive procedures, with over 3.5 million procedures in 2023 and a 5% increase from 2022 [2]. The rise in popularity stems from a combination of societal trends valuing convenience and subtlety, coupled with an aversion to the extended recovery and potential complications associated with invasive surgical procedures such as facelifts. The demand for less invasive solutions has been bolstered by the continued development of treatment modalities, making nonsurgical methods increasingly accessible, effective, and reliable [3].
1.2. Significance of Laser Resurfacing and Chemical Peels
Among nonsurgical rejuvenation options, laser resurfacing and chemical peels stand as core modalities for addressing the quintessential signs of facial aging and photodamage. They serve as foundational and reliable treatments for improving skin texture, reducing dyschromia (hyperpigmentation), smoothing fine lines and rhytides (wrinkles), and managing acne-related concerns. While both of these treatments have been used in practice for many years, they have evolved over time, with modifications to chemical peel formulas, innovations in laser technologies, and changes to pre- and post-treatment protocols. All these refinements have served to enhance the efficacy, safety profiles, and application of the treatments to reach a broader audience with a wider range of skin types over the years.
1.3. Rationale for the Review
The dynamic field of rejuvenation is characterized by technological advancements and changes in aesthetic trends. Innovations, such as fractional and picosecond laser platforms, novel peel formulations, and optimized delivery methods, have continually emerged. This continued evolution, as well as the relative lack of literature on the subject compared to surgical treatments, creates a need for an updated investigation that discusses and compares the relative efficacy, safety, characteristics, and specific indications for lasers and peels. Furthermore, there is rightfully a growing prioritization for safe and effective application across diverse skin types, particularly darker Fitzpatrick skin types IV–VI, where we see increased risks for post-inflammatory hyperpigmentation (PIH) and scarring. This review addresses how safe and efficacious laser resurfacing and chemical peels are for nonsurgical facial rejuvenation, and asks whether there have been significant advancements with regard to treatment of diverse skin types in the past decade. This paper will first provide an overview on the history, efficacy, and safety of rejuvenation modalities, before providing a scoping review of the literature from 2015–2025.
1.4. Review Aims and Objectives
This scoping review aims to (1) map the historical evolution and current landscape of both laser resurfacing and chemical peel technologies; (2) compare their fundamental mechanisms of action, primary indications, clinical efficacy, and safety profiles based on depth/intensity; (3) evaluate advances enabling enhanced safety and efficacy in higher Fitzpatrick skin types (IV–VI); and (4) identify key clinical considerations for evidence-based patient selection and procedure choice.
In addition to the comparison, we will evaluate adjunctive non-surgical advances by (5) synthesizing evidence on recent technological advances and their impact on treatment outcomes, recovery times, and expanded indications; and (6) discuss the key points and highlight the gaps in current evidence, and suggest future research directions.
2. Materials and Methods
We conducted a scoping review aimed at identifying the population of patients seeking nonsurgical facial rejuvenation and advances in techniques, technologies, efficacy, safety, and trends in laser resurfacing and chemical peels in order to better understand recent technological advances and comparative effectiveness in laser resurfacing and chemical peels. The scoping review was reported according to the Preferred Reporting of Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR).
We used the following databases: PubMed/MEDLINE and SCOPUS. Key terms were “laser resurfacing,” “chemical peel,” “facial rejuvenation,” “nonsurgical,” “ablative laser,” “non-ablative laser,” “fractional laser,” “picosecond laser,” “phenol peel,” “TCA peel,” “glycolic acid,” “salicylic acid,” “Jessner’s peel,” “skin of color,” “Fitzpatrick,” “efficacy,” “safety,” “complications,” “recovery,” “patient satisfaction.” Our search included “((((“laser resurfacing” OR “chemical peel” OR “nonsurgical” OR “ablative laser” OR “non-ablative laser” OR “fractional laser” OR “picosecond laser” OR “phenol peel” OR “TCA peel” OR “glycolic acid” OR “salicylic acid” OR “Jessner’s peel”)) AND ((“facial rejuvenation” OR “nonsurgical”))) AND ((Fitzpatrick OR “skin of color”))) AND ((“efficacy” OR “safety” OR “complication” OR “recovery” OR “patient satisfaction”))” and “(facial rejuvenation OR rejuvenation) AND ((phenol peel) OR (TCA peel) OR (glycolic acid) OR (salicylic acid) OR (Jessner’s peel)) AND (efficacy OR safety OR complication OR recovery OR (patient satisfaction))”. We filtered based on English language, human subjects, and publications within the last 10 years (2015–2025).
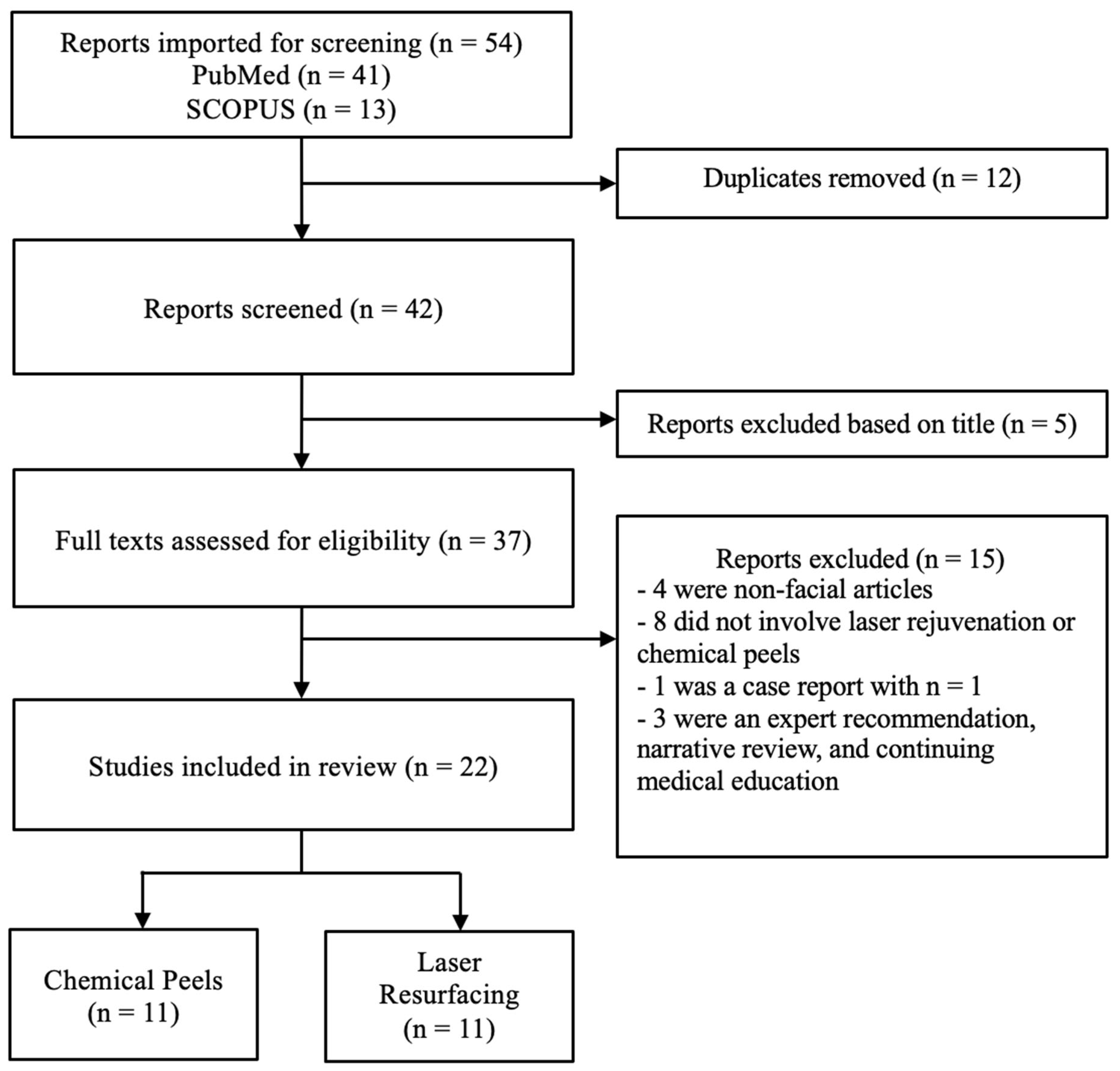
We included primary research (randomized control trials, prospective/retrospective cohorts, large case series), systematic reviews, meta-analyses, and major clinical guidelines. We focused on facial rejuvenation and included all Fitzpatrick skin types. Our exclusion criteria is as follows. We excluded animal studies, non-facial studies, single small case reports (<5 patients), non-English, and non-peer-reviewed opinion pieces. Duplicates were removed (n = 12), reports were removed when title deemed irrelevant (n = 5), and reports excluded for being non-facial (n = 4), for not involving laser rejuvenation or chemical peels (n = 8), being a case report with n = 1 (n = 1), for being expert recommendation, narrative review, and continuing medical education (n = 3).
We independently screened titles and abstracts for eligibility, followed by full-text review. Data were extracted on study design, population characteristics, interventions, outcomes (efficacy, safety, recovery, and patient satisfaction), and Fitzpatrick skin type representation. Discrepancies were resolved by consensus. Findings were synthesized narratively, given heterogeneity in study designs and outcomes.
3. Historical Evolution and Current Trends
3.1. Chemical Peels
Chemical exfoliation can be traced back ancient origins, with early records documenting the use of sour milk (lactic acid) in Egypt and fermented grapes (tartaric acid) in Rome [4]. Modern peel development accelerated in the 19th and 20th centuries. Key milestones include the introduction of phenol peels in the late 19th century, the standardized Baker-Gordon phenol formula in the 1960s, the rise of trichloroacetic acid (TCA) as a versatile agent, and the popularization of alpha-hydroxy acids (AHAs—glycolic, lactic) and beta-hydroxy acid (BHA—salicylic) for superficial rejuvenation starting in the 1980s and 90s [5]. Current trends emphasize the rise of combination peels, in which different agents are layered or combined in pre-mixed solutions to enhance results and reduce side effects, including combination Jessner’s solution followed by TCA peels and salicylic and mandelic acid mixtures [6]. The combination peels have been shown to enhance results and reduce side effects with faster recovery. There has also been an increasing emphasis on pre-treatment and post-treatment care, with the integration of topical retinoids and depigmenting agents to optimize efficacy and maintain peel outcomes.
3.2. Laser Resurfacing
Laser skin resurfacing emerged primarily in the 1980s–90s with early ablative CO2 and erbium-doped yttrium aluminum garnet (Er:YAG) lasers [3]. These offered significant reduction in rhytides for patients, but were limited by prolonged recovery, significant erythema, and risks of scarring and dyspigmentation, particularly among patients with darker complexions. This led to a shift towards non-ablative lasers (i.e., neodymium-doped yttrium aluminum garnet (Nd:YAG; 1320 nm, 1540 nm)) in the early 2000s, which targeted the dermis for remodeling and collagen production paired with epidermal sparing, thereby enabling reduced downtime but potentially resulting in less dramatic results compared to the ablative counterparts [3]. The introduction of fractional photothermolysis in 2003 revolutionized the field with its mechanism of targeting deep tissue by delivering microscopic columns of thermal injury [7]. The microscopic treatment zones (MTZs) are surrounded by healthy tissue, enabling significant efficacy improvements over non-ablative devices while drastically reducing downtime and risks compared to fully ablative lasers. This concept was subsequently applied to both non-ablative and ablative lasers to develop fractional options. More recently, picosecond technology, initially developed for tattoo removal, has expanded into resurfacing applications using diffractive lens arrays or specific wavelengths to create laser-induced optical breakdown for pigment and texture improvement [8]. Current trends involve refinement of fractional devices to optimize the technology in ablative and non-ablative lasers, explore hybrid approaches to combine wavelengths or modalities with one device, or combining treatments by using lasers with radiofrequency, or lasers with peels [9].
3.3. Overall Market and Practice Trends
The technological developments in peels and lasers align strongly with patient preferences for procedures with minimal social downtime, lower risk profiles, and more natural results. Economic factors, including the relatively affordability of superficial treatments also contribute demand. Studies have shown that the majority of patients who eventually pursue surgical facial rejuvenation (i.e., rhytidectomy) overall do not regret the costs associated with noninvasive methods prior to their surgeries [10]. Technological adoption rates remain high, with practitioners integrating new laser platforms and peel formulations into their practices to meet patient expectations and remain competitive [11].
4. Modalities: Mechanisms, Indications, Efficacy, and Safety
4.1. Chemical Peels: Mechanism
Mechanism of Action: Chemical peels induce controlled chemical injury through keratolysis and protein denaturation/coagulation within the epidermis and dermis. Peels induce exfoliation followed by epidermal and dermal regeneration from the surrounding epithelium and skin adnexa [12]. The depth of injury, classified as superficial (epidermis), medium (papillary/upper reticular dermis), or deep (mid-reticular dermis), determines the biological response (i.e., coagulation, inflammation, collagen production, elastin remodeling) and clinical effects.
4.2. Common Agents and Formulations
- ▪
- Superficial: Glycolic Acid (AHA), Salicylic Acid (BHA), Jessner’s Solution (resorcinol, salicylic acid, lactic acid in ethanol), Retonic Acid, Pyruvic Acid (AHA), Lactic Acid (AHA), Mandelic Acid (AHA), TCA (10–35%).
- ▪
- Medium: TCA (various concentrations 20–50% and application techniques—single vs. multiple coats), Modified Jessner’s + TCA (combination).
- ▪
- Deep: Phenol formulations (Baker-Gordon, Hetter, Stone—varying croton oil concentrations).
4.3. Clinical Indications
- ▪
- Superficial: Mild dyschromia, texture irregularities, actinic keratosis prophylaxis, acne vulgaris, complexion irregularities in sun-damaged skin, epidermal and mixed melasma [12,13].
- ▪
- Medium: Moderate dyschromia, fine lines, superficial rhytides, superficial atrophic acne scars, actinic keratoses.
- ▪
- Deep: Coarse rhytides, deeper acne scars, significant photodamage, dermal melasma (caution).
4.4. Efficacy
Superficial peels offer modest, temporary improvements requiring regular maintenance. They are commonly effective for mild to moderate acne with glycolic acid (GA) 30% and salicylic acid (SA) 30% being similarly effective in a split-face randomized controlled trial (RCT) [13]. They have shown reductions in acne scarring, MASs, post-acne pigmentation (How [14]). GA peels are effective and safe for melanoma reduction (Dorghum [15], Sarkar [16]). Jessner’s and SA peels have improved acne vulgaris (How [14]) and photo damage (Liu [17], Heyman [18]). Medium-depth peels, especially TCA-based, provide significant, reproducible improvement in moderate photodamage, dyschromia, and fine lines, with results lasting 1–2+ years. A study comparing Jessner’s solution (JS) with 20% TCA compared to TCA alone in those with higher Fitzpatrick skin types found that the combination peel was more effective in treating melasma, however with higher immediate discomfort [19] (Sarkar [20]). Deep peels such as phenol peels offer dramatic, long-lasting results on the order of years for severe damage but also carry the highest risk profile (Maymone [21]).
4.5. Safety Profile and Complications
Expected reactions include transient erythema, desquamation, and edema. Key complications center on post-inflammatory hyperpigmentation (PIH), particularly in darker skin types, which is the most common adverse event (Maymone [21], Dorgham [15], How [14]). Hypopigmentation (especially with phenol), hyperpigmentation, scarring, and infection (viral, bacterial, fungal) make up some of the more significant risks, which increase with peel depth [22]. Phenol carries risks of systemic toxicity (cardiac arrhythmia, hepatotoxicity) requiring careful perioperative management [13]. Although, a study had described a punctuated-pattern 88% phenol technique applied to single rhytids, thereby reducing phenol exposure [23]. The primary risk factors for all chemical peel complications include Fitzpatrick skin type IV–VI, inadequate pre-peel priming, history of keloids or poor wound healing, recent sun exposure, and improper peel technique/concentration [24].
4.6. Laser Types and Technologies
Laser types include ablative, nonablative, fractional, and picosecond. Ablative laser resurfacing involves selective thermal destruction to the level of the dermis, while non-ablative lasers target the dermis and spare the epidermis. Fractional photothermolysis employs the targeting of MTZs by delivering columns of localized thermal injury without affecting surrounding tissues to limit damage. There are both ablative fractional (AF) and nonablative fractional (NAF) lasers in clinical practice. Picosecond lasers deliver short pulses of non-thermal to induce Laser-Induced Optical Breakdown (LIOB), which leads to a photomechanical effect to promote collagen remodeling and pigment fragmentation [25]. This is often used in tattoo removal, but has also been employed in skin resurfacing, acne scar treatment, and treatment of melasma and other hyperpigmentation [26]. Laser resurfacing principles and types are summarized in Table 1, with laser indications and target patient profiles outlined in Table 2. Adverse effects for RF micro needling were erythema and scabbing (Cheles [27]), picosecond lasers had moderate pain (Wang [28], Khetarpal [25]). Fractional ablative and dual-wavelength lasers caused erythema and edema (Belletti [29], Munavelli [30]).

Table 1.
Laser resurfacing technologies.

Table 2.
Clinical indications by laser type.
5. Comparative Analysis: Laser Resurfacing
Ablative lasers comprise Er:YAG and CO2; nonablative lasers comprise erbium-doped glass (Er:Glass), Nd:YAG, and alexandrite. Both nonablative and ablative lasers can be titrated based on rate of pulsations, for example, picosecond versus quasi. Nonablative lasers target the mid reticular dermis while preserving the epidermis and dermal-epidermal junction [31]. Ablative lasers result in epidermal ablation. The result is that ablative lasers have been thought of as being more effective while having more adverse effects and longer time to heal. Nonablative lasers by comparison have less downtime but require more treatment sessions with a more subtle effect per treatment. A systematic review and meta-analysis of 10 RCTs (n = 365; facial subjects) comparing efficacy and safety of ablative and non-ablative lasers showed statistically insignificant outcomes (p = 0.55) and similar likelihood of side effects [32]. Studies using I-GAIS/P-GAIS and other validated scores (Lemperle Wrinkle Scale) showed improvement (Cheles [27], Wang [16], Tao [33], Khetarpal [25], Belletti [29]).
6. Comparative Analysis: Chemical Peels
Superficial- and medium-depth chemical peels have proliferated in aesthetic medicine as lasers have largely replaced deep peels due to high complication risk, particularly with phenol formulations [34]. Chemical peels allow for controlled keratocoagulation and protein denaturation, followed by a targeted wound healing cascade. Superficial peels penetrate the epidermis only, medium-depth peels go down to the entire epidermis and papillary dermis, and deep peels most often exert effect down to the mid-reticular dermis. However, peel depth depends on the type of chemical used, chemical concentration, timing and number of applications, as well as the patient’s Fitzpatrick skin type. For example, a higher concentration will affect a greater depth of keratocoagulation in less time. When comparing peel depth, healing time, necessary patient downtime, and risks are directly proportional to the depth. However, deeper peels will result in the greatest improvement in cosmetic outcome [34]. Using TCA peels as an example, a concentration less than 30% penetrates only the epidermis (i.e., superficial) to treat low-depth melasma and mild dyschromia, whereas TCA use greater than 35% to 50% as a medium-depth peel can be used to target deeper pathologies including moderate dyschromia and actinic keratoses. However, currently medium-depth peels are not recommended for Fitzpatrick skin types greater than IV given increased risk of scarring and PIH [13] (Maymone [21], How [14]). Comparative analysis between laser resurfacing and chemical peels is displayed in Table 3. Key safety comparisons based on multiple parameters are shown in Table 4.

Table 3.
Comparative analysis of laser resurfacing and chemical peels.

Table 4.
Key safety comparisons.
7. Advancements for Diverse Skin Types (Fitzpatrick IV–VI)
7.1. Historical Challenges
Traditional ablative lasers and deep chemical peels carried an unacceptably high risk of PIH, dyspigmentation, and scarring in Fitzpatrick skin types IV–VI, severely limiting treatment options for these populations.
7.2. Laser Advances for Skin of Color
Significant progress has been made through safer parameters for fractional lasers. Utilizing lower densities and energies and employing longer wavelengths like a nonablative and ablative fractional laser at 1550 nm with ER:YAG can penetrate deeper with less epidermal melanin absorption, which dramatically reduces complication rates. The role of picosecond lasers for pigment-specific concerns and texture improvement offers an alternative with a lower PIH risk profile compared to Q-switched lasers and some fractional devices [26]. Utilizing test spots and conservative protocols such as fewer passes and lower intensity are critical for risk reduction when considering laser skin rejuvenation for patients with higher Fitzpatrick skin types [24].
7.3. Chemical Peel Advances for Skin of Color
Treatment strategies emphasize a focus on superficial and medium-depth peels using modified protocols (lower concentrations, shorter application times, fewer passes, avoiding aggressive neutralization for AHAs). Rigorous pre-peel priming with melanin-inhibiting agents (hydroquinone, retinoids) for 4–6 weeks is essential. Although medium-depth peels are not recommended in those with Fitzpatrick skin type greater than IV, PIH risk can be reduced with one month of hydroquinone pretreatment or peeling during the winter months. It is also recommended for tretinoin cessation one week prior to treatment to further decrease this risk [13]. Specific peel formulations demonstrate favorable profiles, including salicylic acid (anti-inflammatory, comedolytic), Mandelic acid (larger molecule, slower penetration), and lower percentages of TCA (e.g., 15–30%) often combined with Jessner’s or used in a Chemical Reconstruction of Skin Scars, or “CROSS,” technique for scars, preceded by priming.
7.4. Comparative Safety and Efficacy in Fitzpatrick IV–VI
Evidence indicates that both modalities, when appropriately selected and modified, can be safe and effective. Superficial peels and low-density NAF/picosecond resurfacing are first-line for mild-moderate concerns, with excellent safety. Medium-depth peels (carefully applied) and fractional ablative Er:YAG (conservative settings) offer greater efficacy for moderate-severe concerns but require meticulous patient selection, priming, and post-care to mitigate PIH risk. Picosecond lasers excel for pigment-focused rejuvenation. The choice depends heavily on the primary indication, desired depth of effect, and practitioner expertise.
8. Clinical Application and Decision-Making
8.1. Patient Assessment and Selection
A comprehensive consultation is essential, focusing on the patient’s specific concerns (rhytides, pigment, texture, scars) and expectations. The evaluation should include skin type, level of photodamage, and specific indications. A thorough medical history must identify contraindications like a history of keloids, herpes zoster, herpes simplex virus (requiring prophylaxis), recent isotretinoin use (wait 6–12 months), immunosuppression, and relevant medications.
8.2. Matching Modality/Technology to Patient and Indication
Selection requires an algorithmic approach integrating Fitzpatrick skin type, severity of the primary concern(s), and the patient’s desired downtime. Generally, higher Fitzpatrick types and lower downtime tolerance favor superficial peels, NAF lasers, or picosecond resurfacing. These methods have shown acceptable safety and efficacy in darker skin types (Wang [28], Tao [33]). More severe photodamage or scarring in lighter skin types may warrant fractional ablative lasers or medium/deep peels. Combination therapies have had an increasing role, involving sequential peels and lasers that may involve a superficial peel followed weeks later by fractional laser, or combining lasers with other energy-based devices such as radiofrequency for tightening to have synergistic outcomes [35]. RF microneedling and picosecond lasers had high satisfaction (Cheles [27], Wang [28], Tao [33]).
8.3. Pre-Treatment Considerations
Skin priming for 4–6 weeks pre-peel is especially important for peels and lasers in higher Fitzpatrick types or when treating pigment. This typically includes nightly retinoids to enhance penetration and normalize keratinization, hydroquinone to suppress melanin, and rigorous broad-spectrum sun protection. Antiviral prophylaxis against herpes simplex virus reactivation is standard for all ablative procedures and medium/deep peels, and often used for fractional ablative; antibiotic prophylaxis may be considered for deep peels or extensive ablative resurfacing [24].
8.4. Post-Treatment Care and Management
Standard protocols after both chemical peels and laser treatment involve gentle cleansing, frequent moisturization, and strict sun avoidance/protection. Managing expected reactions (erythema, edema, peeling) involves soothing emollients and cool compresses. Mitigating complications, especially PIH, relies heavily on prompt recognition, proactive sun protection, and early intervention with topical hydroquinone, retinoids, kojic acid, azelaic acid, or corticosteroids as indicated [36]. Herpes simplex virus often presents on day 2 or 3 after re-epithelialization, so it is recommended to prescribe 7 days of antiviral medication postprocedure from chemical peels. Any pustule formation should warrant culture and initiation of fungal and/or bacterial empiric therapy [13].
8.5. Setting Realistic Expectations
Clear communication regarding outcomes and strategies to mitigate complications is essential for maximizing patient satisfaction. Important points to discuss as part of informed consent include expected degree of improvement, need for multiple sessions if indicated, expected recovery timeline, and potential complications. Managing expectations is as vital as technical skill in achieving successful nonsurgical rejuvenation.
9. Results
The PubMed search resulted in 41 results. The SCOPUS search resulted in 13 results. 12 were excluded as duplicates; 1 was excluded as a Case Report with n = 1; 3 were excluded as an expert recommendation, narrative review, or continuing medical education. In total, 22 articles discussing laser resurfacing (n = 11) and chemical peels (n = 11) were included in the analysis. A diagram of the scoping literature search with reasons for exclusion according to PRISMA criteria is displayed in Figure 1.
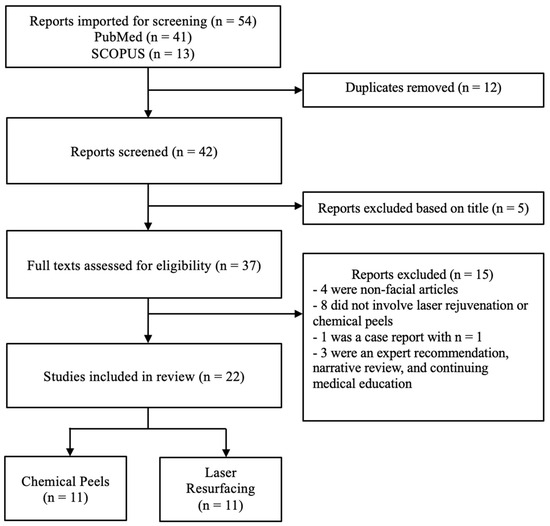
Figure 1.
PRISMA flow diagram.
The primary studies’ (excluding meta-analysis and systematic reviews) sample sizes ranged from 7 to 40 with subjects spanning 30 to 75 years of age. When gender was disclosed, females were predominant. Most studies included patients with Fitzpatrick skin types I–IV with some inclusion of V and VI.
9.1. Treatment Modalities
The studies used a wide variety of treatment modalities, including the following:
- Radiofrequency microneedling (Cheles, Tao, Munavalli) [27];
- Picosecond lasers (Wang, Khetarpal, Dierickx, Tao) [37];
- Intense Pulsed Light (IPL) (Sales) [38];
- CO2/1540 nm fractional lasers (Belletti) [29];
- Plasma exeresis (Ferreira) [39];
- Calcium hydroxylapatite fillers (Wollina) [40];
- Combination therapies (Dayan, Munavalli, Tao) [41];
- Chemical peels in isolation and in combination, including TCA, SA, GA, JS, and phenol (Abdel Meguid, Ali, Artzi, de Vries, Dorgham, How, Kligman, Liu, Maymone, Murtaza, Sarkar) [14,15,16,17,18,20,21,42,43,44,45].
Studies were filtered to focus on the face. Several studies had a more specialized focus: on the midface and lower face (Wollina) [40], submental region (Wang) [28], upper eyelids (Ferreira) [39], and periorbital region (Cheles) [27].
9.2. Efficacy Outcomes
i. Efficacy measures
Of the measures used to assess treatment efficacy, the Investigator-assessed and Patient-assessed Global Aesthetic Improvement Score (I-GAIS/P-GAIS) was the most commonly employed (Cheles, Wang, Tao, Khetarpal, Dierickx, Wollina) [27]. Other tools included the Lemperle Classification of Facial Wrinkles (LFW; Cheles) [27], Q-Blefaro questionnaire (Ferreira) [39], Fitzpatrick Wrinkle Assessment Scale/Wrinkle & Elastosis Scale (FWCS; Dayan, Munavalli, Dierickx, Belletti) [29], Skin Quality Assessment (Dayan) [41], State Self-Esteem Scale (Dayan), the 6-point Acne Scar Improvement Score (Dierickx) [37], the Melasma Area and Severity Index (MASI) (Sarkar, Maymone, Murtaza, Dorgham) [15,16,20,21], Michaelsson Acne Score (MAS) (How) [14], and the Goodman and Baron Scarring Global Quantification Grading System (Ali) [43]. Other evaluative methods included general patient satisfaction questionnaires and photograph evaluation by blinded dermatologists (Belletti, Dierickx) [29]. Results from the scoping review search are shown in Table 5.

Table 5.
Summary of PRISMA review.
ii. Improvement measures following laser and radio-frequency treatment
Most studies demonstrated statistically significant improvements in targeted areas of intervention.
Radiofrequency Microneedling: RF needling, comparing the Gen100 and Gen36L tips, resulted in an average of 49% reduction in wrinkle severity on the LFW scale (p < 0.05) with an average improvement on I-GAIS and P-GAIS and 83% reported patient satisfaction (Cheles et al.) [27]. In treatment with radiofrequency (RF) microneedling and picosecond laser with fractionated lens array, 100% of subjects showed improvement (I-GAIS) with 88.9% patient satisfaction at 3 months (Tao) [33].
Picosecond lasers: Wang et al. found 81.8% improvement (I-GAIS) at 90 days and maintained improvement at 180 days with 755 nm picosecond laser with diffractive lens array (DLA) (Wang) [28]. Khetarpal demonstrated 93% patient satisfaction 1 month post picosecond laser with 77% of photos correctly identifying baseline versus post-treatment by blinded investigators [25]. Dierickx compared standard and high pulse count with picosecond laser treatment on acne and rhytides and did not find statistically significant improvement [37].
Fractional/Non-ablative lasers: Munavalli used a split-face design comparing same-day sequential Q-switched Nd:YAG laser and 1565 nm non-ablative fractional laser (SST) facial rejuvenation with fractional non-ablative laser (NAFL) with both SST and NAFL leading to improvement in wrinkle/elastosis scores at 6-month follow up, and SST showing more improvement in skin texture and tone [30]. This was confirmed with histological analysis. Belletti demonstrated efficacy of a dual CO2 and 1540 nm wavelength laser in decreasing rhytides, with statistically significant reduction in FWCS score (p < 0.01) and with all subjects reporting subjective improvement [29].
IPL: The systematic review by Sales et al. showed consistent improvement of wrinkles, pigmentation, erythema, texture, and general photoaging with IPL across studies [38].
Other energy-based devices: Ferreira et al. found high initial satisfaction at day 7 following plasma exeresis, with a willingness to undergo repeat procedures declining over time (p = 0.038) [39]. Higher satisfaction at day 30 was associated with Fitzpatrick skin types III and IV (p = 0.043) (Ferreira).
Injectables/Combination Treatment: Calcium hydroxyapatite injections resulted in moderate improvements at 12 months that sustained at 3–5 year follow up (I-/P-GAIS; Wollina and Goldman) [40]. Dayan et al. compared hyaluronic acid filler and neurotoxin followed by either a basic skin care regimen or Nu-Derm (Obagi) skin care system and found a statistically significant difference in aesthetic appearance between groups (GAIS) without a statistical difference in patient satisfaction or self-esteem [41].
iii. Improvement measures following chemical peel treatment
Studies focusing on the efficacy of chemical peels showed similar improvements in the targeted region. Most focused on low- to medium-depth facial skin pathologies, notably acne vulgaris, melasma, and photodamaged skin.
Melasma: A systematic review of 1075 total subjects compared various chemical peels to treat melasma and found GA peels to be the safest and most effective in reducing MASI scores [16]. For specifically patients with epidermal melasma and Fitzpatrick skin types III–V, combining TCA 20% peel with 5% topical magnesium ascorbyl phosphate had a significantly greater reduction in MASI scores compared to TCA peel alone (81.1% vs. 66.2%, p = 0.040) [20]. Another systematic review and meta-analysis on melasma treatment by Dorgham et al. found that GA peels were superior to TCA peels in MASI score reduction (p = 0.007) but that TCA and JS peels still reduced MASI to a greater extent than topical agents like hydroquinone (p < 0.001 and p = 0.004, respectively) [15]. For more persistent melasma, Maymone et al. added croton oil (CO) as a supplement to phenol peels and found a greater reduction in MASI for the <1% CO formulation yet a consistently greater risk of PIH compared to the >1% CO group (44% vs. 30% risk, respectively); however, both groups still significantly reduced MASI compared to baseline [21].
Acne Vulgaris: The chemical peels JS and SA 30% were studied to treat acne vulgaris in skin of color and found significant reductions in the number of lesions, MAS, and postacne pigmentation (p < 0.001) without any notable differences between groups [14]. A similar study found no significant differences in acne vulgaris improvement between TCA 25% or SA 30%, although comedomal improvement favored TCA use (80 vs. 70%), and inflammatory improvement favored SA (85 vs. 80%) [42]. A systematic review compared the strength of evidence among treatment modalities for acne vulgaris based on the statistical significance between and within groups based on the change in clinical signs of inflammatory lesions. They found the strongest evidence for GA (10–40%) peels and moderate evidence for amino fruit acid (20–60%), IPL laser (400–700 nm and 870–1200 nm), and the diode laser (1450 nm). Conflicting evidence was found for PDL (585–595 nm) [44].
Atrophic Acne Scars: Ali et al. found that the addition of Dermapen microneedling to JS chemical peel treatment resulted in the greatest improvement according to the Goodman and Baron scarring global quantification grading system (p = 0.016) [43].
Other indications- disseminated facial verruca plana; photodamaged skin: Other recent advances for disseminated facial verruca plana found that receiving GA 35% peels for 3 sessions at 2-week intervals resulted in >70% lesion reduction in half of patients, a 25% greater reduction than using adapalene gel [17]. To address photodamaged skin, adding either 0.25% tretinoin or retinoic acid to SA peels improved pore size, dryness, roughness, and overall appearance compared to baseline, addressing the mild side effects with SA peels [45].
9.3. Safety and Tolerability
Safety and tolerability profiles for the studies were generally favorable, with no serious immediate or long-term adverse effects. General side effects included erythema, edema, and patient discomfort, which were similar among treatment modalities. Studies used subjective reports and scales such as the Visual Analog Scale (VAS) for treatment discomfort.
RF microneedling: Cheles reported pinpoint epidermal scabs, edema, erythema, and itching, with an average discomfort of 4.1 on VAS [27]. Tao reported a mean pain score of 5.2/10 from RF microneedling compared to 3.1/10 from 755 nm laser [33]. Ali et al. reported erythema and pain during sessions, but no significant difference was found between those who had JS peel alone, RF microneedling, or a combination of both [43].
Lasers: Wang found a mean pain score of 3.8/8 with nodule formation, dyspigmentation, edema, and blistering [28]. Wollina reported bruising and nodule formation [40]. For Khetarpal, a mean pain score of 4.2/10 was reported with general erythema and swelling [25]. For Munavalli, SST and NAFL had equal safety with lower pain in SST [30]. Dierickx reported mild and transient erythema and edema and mild PIH [37]. Belletti reported erythema, edema, and discomfort [29].
Chemical peels: Maymone et al. reported a greater PIH risk for those who had a lower concentration of croton oil added to phenol peels [21]. How et al. had only one instance of PIH in a patient who had a JS peel [14]. Liu et al. found mild erythema and desquamation in the GA 35% peel group [17]. Dorgham et al. reported a higher risk of erythema in the TCA peel group compared to GA (RR = −0.18, p = 0.002). However, no significant differences were found in adverse events between GA and topical agents or PIH between GA and TCA peels [15]. Finally, Heyman et al. found that in patients who received GA 50% plus a novel protective agent called Dermashield to lower the pH, there was a significant reduction in erythema, pain, itching, and recovery time with comparable efficacy [18].
Other energy-based devices: Ferreira reported edema, hematoma, itching, hyperemia, and pigment changes, of which edema and itching were the most common [39].
Systematic reviews: De Vries et al. reported mild side effects among all studies, most notably erythema, tolerable pain, and edema [44].
10. Discussion
Generally, single- and double-modality treatments, including RF microneedling, picosecond lasering, sequential Q-switched Nd:YAG lasering, 1565 nm non-ablative fractional lasering, and dual CO2 and 1540 nm wavelength lasering, were effective in reducing the appearance of facial rhytides and/or acne scarring. Multiple chemical peels, either in isolation or in combination with microneedling and topical agents, remain effective in treating a variety of pathologies, notably acne vulgaris, limited and recurrent melasma, skin discoloration, and photodamaged skin. In recent advances for chemical peels, combined treatment, such as peel therapy with a mineral or topical agent as maintenance, seems to be evolving to not only improve success but minimize the existing side effects with classic chemical peels. The treatment modalities served as both useful adjuncts and primary treatments, with high reports of patient satisfaction, investigator-determined improvement, and reductions in pathology-specific symptom scores. Plasma execresis is a possible exception. Only one study confirmed these results with histologic evaluation. However, studies would benefit from the use of a standardized pain scale, as well as from objective measures of rhytide reduction and improvement in other facial skin pathologies.
Indeed, synergistic modalities proved to be effective. An emerging area within nonfacial rejuvenation is the use of combined laser approaches, such as sequential fractionated CO2 followed by 1540/1570 nm wavelengths. This technique has demonstrated promising results in facial rejuvenation with a favorable safety profile, particularly in darker skin phototypes. Recent evidence supports its efficacy and safety, with preclinical and clinical data highlighting synergistic effects in improving texture, rhytides, and pigmentation while minimizing post-inflammatory hyperpigmentation risk. Adding 1540/1570 nm after fractional CO2 broadens the thermal coagulation zone without increasing ablation depth, resulting in enhanced collagen remodeling while maintaining safety profiles similar to CO2 monotherapy [46].
As expected, side effects were predictable, mild, and transient, and did not require further intervention. Adverse effects were not reported. This review demonstrates the wide variety of treatment options for certain skin conditions, improving facial contour, and minimizing age-related skin changes; however, the decision for which modality is highly individual-driven. Certain patient characteristics may contraindicate chemical peels, such as active inflammation (e.g., pustular acne), recent isotretinoin use, pregnancy or lactation, or a predisposition to post-inflammatory hyperpigmentation (e.g., Fitzpatrick IV–VI or a history of PIH). In these cases, laser-based approaches, such as low-energy nonablative or sequential fractional CO2 and 1540/1570 nm protocols, may offer safer, more effective alternatives with reduced pigmentary risk. Thorough discussions of risks, benefits, and adequate clinical judgment remain necessary to provide the optimal treatment modality.
The focus on Fitzpatrick skin type I–IV in the studies confirmed our hypothesis that subjects with Fitzpatrick skin type V–VI would be underrepresented. Quiñonez’ article, which was excluded from our analysis as a Continuing Medical Education review, outlines assessment and preprocedure planning for skin of color, noting limitations in the contemporary literature on nonsurgical cosmetic procedures for people of color, defined as Fitzpatrick skin type IV–VI. Some studies on chemical peels had included Fitzpatrick skin types greater than IV, particularly in the realm of melasma; however, the literature overall remains limited, especially in the treatment of deeper skin pathologies. Several points are of interest: first, that the Fitzpatrick skin type, referring to the skin’s reaction to phototherapy, is directly transferable to skin’s response to cosmetic procedures. The Roberts Skin Type Classification System, which addresses hyperpigmentation and scarring capability, would be more useful in predicting the post-treatment side-effect of PIH. This would, in turn, lead to increased use of mitigating preprocedure cosmeceutical agents such as hydroquinone (a melanogenesis inhibitor) and topical retinoids. Asian skin also has a higher propensity for PIH, meaning that “a greater number of lower density NAFL treatments administered over a longer time period” confers the most benefit while protecting against PIH and rebound melasma. Higher-powered studies inclusive of all skins of color are needed in the field. The use of combined laser treatments with fractional CO2 followed 1540/1570 nm lasers has been shown to have improved safety profiles. Further studies should assess patient outcomes with this laser technique to assess feasibility for greater inclusivity of higher Fitzpatrick skin types.
Given the current lack of literature and, notably, safety concerns for individuals with phototypes IV–VI, future research should more explicitly address strategies to improve the inclusion of underrepresented populations. This could include targeted recruitment efforts in dermatology and aesthetic clinics serving diverse communities, partnerships with community health organizations, and the stratification of study outcomes by phototype or alternative classification systems such as the Roberts Skin Type Classification. Such approaches would not only strengthen the generalizability of findings, but also help guide evidence-based, safer practices for patients with skin of color.
Although the present study provides a widespread review of the use of varying modalities within chemical peels and lasers for rejuvenation, it is not without limitations. The heterogeneity of study designs, treatment protocols, and outcome measures across the included literature limited our ability to perform direct comparisons or generate standardized recommendations. Second, cost-effectiveness was not assessed in our review, restricting insight into the economic considerations of these modalities. Furthermore, our selected articles mainly focused on a single intervention (peel or laser, and an exploration of multimodal strategies, combining the modalities of laser, peel, and radiofrequency, is warranted. Although laser treatments may have a superior side effect profile for those with higher Fitzpatrick skin types, it may not be economically feasible compared to the chemical peel alternative. Additionally, our findings are constrained by the short follow up periods and underrepresentation of higher Fitzpatrick phototypes (IV–VI) within the included studies, which limit the generalizability and long-term applicability of our conclusions.
A possible limitation of our study is that the efficacy measures relied on subjective or semi-quantitative scales, such as the Global Aesthetic Improvement Scale, which is vulnerable to observer bias. There was limited use of objective biometric skin measurements. While split-face pilot studies used a control, most studies did not. Lastly, a majority of studies were underpowered, with n ranging from 7 to 148 in single studies (excluding one study where n = 1075).
11. Conclusions
The current review highlights significant advancements in nonsurgical facial rejuvenation using lasers and chemical peels, alongside emerging adjunctive modalities. These technologies have improved efficacy, safety, and applicability across a broader range of skin types, including higher Fitzpatrick phototypes, although data remain limited for these populations. Underrepresentation of Fitzpatrick phototypes IV–VI has far-reaching clinical implications. A paucity of studies examining these phototypes means that there is a less developed understanding of the risks and strategies for preventing PIH and hypertrophic scarring/keloids. This could lead to over-cautious providers who undertreat certain populations. More equitable access to care could be established by developing evidence-based standardized treatment protocols for lasers and peels. Study methods might include deliberate inclusion of all Fitzpatrick phototypes, ensuring proper recruitment. Other methods would include encouraging regular follow up, monitoring, and reporting of post-treatment complications. This would ideally lead to algorithms customized to a greater diversity of phototypes beyond Fitzpatrick I–III.
Furthermore, variability in study design, outcome measures, and cost-effectiveness reporting underscores the need for standardized protocols and higher-quality research. Future studies should focus on inclusive patient recruitment, long-term outcomes, and comparative cost analyses to better inform clinical decision-making and optimize patient-centered care in facial rejuvenation.
Author Contributions
Conceptualization, methodology, M.X.M.; formal analysis, S.G.; writing—original draft preparation, M.X.M. and S.G.; additional analysis, editing, J.N.T.; writing—review and editing, M.I.D.; supervision, M.I.D. and S.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| AF | Ablative fractional |
| AFCO2 | Ablative fractional CO2 |
| AFEr | Ablative fractional erbion |
| BHAs | Beta-hydroxy acids |
| CO | Croton Oil |
| DLA | Diffractive Lens Array |
| Er:Glass | Erbium-doped glass |
| Er:YAG | Erbium-doped yttrium aluminum garnet |
| FCWS | Fitzpatrick Wrinkle Assessment Scale/Wrinkle & Elastosis Scale |
| GA | Glycolic Acid |
| IPL | Intense Pulsed Light |
| JS | Jessner’s Solution |
| LCW | Lemperle Classification of Wrinkles |
| LFW | Lemperle Classification of Facial Wrinkles |
| LIOB | Laser-Induced Optical Breakdown |
| MAS | Michaelsson Acne Score |
| MASI | Melasma Area and Severity Index |
| MTZs | Microscopic transition zones |
| NAF | Non-ablative fractional |
| NAFL | Non-ablative laser |
| Nd:YAG | Neodynium-doped yttrium aluminum garnet |
| PDL | Pulsed Dye Laser |
| PIH | Non-ablative fractional laser |
| RCT | Randomized Controlled Trial |
| RF | Radio Frequency |
| SA | Salicylic Acid |
| SST | Same-day sequential Q-switched Nd:YAG laser and 1565 nm non-ablative fractional laser |
| TCA | Trichloroacetic acid |
| TST | Thermal Relaxation Time |
| VAS | Visual Analog Scale |
References
- Hari-Raj, A.; Spataro, E.A. Evidence-Based Medicine for Nonsurgical Facial Rejuvenation. Facial Plast. Surg. 2023, 39, 230–236. [Google Scholar] [CrossRef]
- 2023 Plastic Surgery Statistics: Minimally Invasive Procedures. American Society of Plastic Surgeons. 2023. Available online: https://www.plasticsurgery.org/news/plastic-surgery-statistics?sub=2023+Plastic+Surgery+Statistics (accessed on 10 June 2025).
- Haykal, D.; Cartier, H.; Goldberg, D.; Gold, M. Advancements in laser technologies for skin rejuvenation: A comprehensive review of efficacy and safety. J. Cosmet. Dermatol. 2024, 23, 3078–3089. [Google Scholar] [CrossRef] [PubMed]
- Feng, X.; Shang, J.; Gu, Z.; Luo, X.; Chen, Y.; Liu, Y. Lactic Acid Chemical Peeling in Skin Disorders. Clin. Cosmet. Investig. Dermatol. 2024, 17, 901–909. [Google Scholar] [CrossRef] [PubMed]
- Weissler, J.M.; Carney, M.J.; Carreras Tartak, J.A.; Bensimon, R.H.; Percec, I. The Evolution of Chemical Peeling and Modern-Day Applications. Plast. Reconstr. Surg. 2017, 140, 920–929. [Google Scholar] [CrossRef]
- Herbig, K.; Trussler, A.P.; Khosla, R.K.; Rohrich, R.J. Combination Jessner’s solution and trichloroacetic acid chemical peel: Technique and outcomes. Plast. Reconstr. Surg. 2009, 124, 955–964. [Google Scholar] [CrossRef] [PubMed]
- Manstein, D.; Herron, G.S.; Sink, R.K.; Tanner, H.; Anderson, R.R. Fractional photothermolysis: A new concept for cutaneous remodeling using microscopic patterns of thermal injury. Lasers Surg. Med. 2004, 34, 426–438. [Google Scholar] [CrossRef]
- Halpin, J.; Amechi, M. Considerations for Laser Therapy, Microneedling, and Chemical Peels When Treating Patients with Skin of Color. Plast Aesthet Nurs. 2023, 43, E2. [Google Scholar] [CrossRef]
- Anayb Baleg, S.M.; Bidin, N.; Suan, L.P.; Sidi Ahmad, M.F.; Krishnan, G.; Johari, A.R.; Hamid, A. Combination of Er:YAG laser and CO2 laser treatment on skin tissue. Photochem. Photobiol. 2015, 91, 134–138. [Google Scholar] [CrossRef]
- Jacono, A.A.; Malone, M.H.; Lavin, T.J. Nonsurgical Facial Rejuvenation Procedures in Patients Under 50 Prior to Undergoing Facelift: Habits, Costs, and Results. Aesthet. Surg. J. 2017, 37, 448–453. [Google Scholar] [CrossRef]
- Liu, Y.; Mao, R.; Xiao, M.; Zhu, W.; Liu, Y.; Xiao, H. Facial Rejuvenation: A Global Trend of Dermatological Procedures in the Last Decade. Plast. Reconstr. Surg. Glob. Open 2024, 12, e5801. [Google Scholar] [CrossRef]
- Amici, J.; Cogrel, O.; Jourdan, M.; Raimbault, C.; Canchy, L.; Kerob, D.; Madfes, D.C.; Tian, Y.; Araviiskaia, E. Expert recommendations on supportive skin care for non-surgical and surgical procedures. J. Eur. Acad. Dermatol. Venereol. 2023, 37 (Suppl. S3), 16–33. [Google Scholar] [CrossRef]
- Lee, K.C.; Wambier, C.G.; Soon, S.L.; Sterling, J.B.; Landau, M.; Rullan, P.; Brody, H.J. Basic chemical peeling: Superficial and medium-depth peels. J. Am. Acad. Dermatol. 2019, 81, 313–324. [Google Scholar] [CrossRef]
- How, K.N.; Lim, P.Y.; Kammal, W.S.L.W.A.; Shamsudin, N. Efficacy and safety of Jessner’s solution peel in comparison with salicylic acid 30% peel in the management of patients with acne vulgaris and postacne hyperpigmentation with skin of color: A randomized, double-blinded, split-face, controlled trial. Int. J. Dermatol. 2020, 59, 804–812. [Google Scholar] [CrossRef] [PubMed]
- Dorgham, N.A.; Hegazy, R.A.; Sharobim, A.K.; Dorgham, D.A. Efficacy and tolerability of chemical peeling as a single agent for melasma in dark-skinned patients: A systematic review and meta-analysis of comparative trials. J. Cosmet. Dermatol. 2020, 19, 2812–2819. [Google Scholar] [CrossRef] [PubMed]
- Sarkar, R.; Lakhani, R.M. Chemical Peels for Melasma: A Systematic Review. Dermatol. Surg. 2024, 50, 656–661. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Ai, J.; Zhu, Z.; Huang, L.; Yi, Z.; Wu, L.; Xu, Y.; Zhu, D.; Li, H.; Yan, Y.; et al. Chemical peeling with 35% glycolic acid for the treatment of disseminated facial verruca plana: A randomized, split-face, evaluator-blinded trial. Dermatol. Ther. 2022, 35, e15594. [Google Scholar] [CrossRef]
- Artzi, O.; Heyman, L.; Carasso, R.; Mehrabi, J. The Efficacy and Safety of a Novel Protective Complex Combined With 50% Glycolic Acid Peel: A Double-Blinded, Split Face, Controlled Study. J. Drugs Dermatol. 2021, 20, 1336–1339. [Google Scholar] [CrossRef]
- Abdel-Meguid, A.M.; Taha, E.A.; Ismail, S.A. Combined Jessner Solution and Trichloroacetic Acid Versus Trichloroacetic Acid Alone in the Treatment of Melasma in Dark-Skinned Patients. Dermatol. Surg. 2017, 43, 651–656. [Google Scholar] [CrossRef]
- Murtaza, F.; Bangash, A.R.; Khushdil, A.; Noor, S.M. Efficacy of Trichloro-Acetic Acid Peel Alone Versus Combined Topical Magnesium Ascorbyl Phosphate for Epidermal Melasma. J. Coll. Physicians Surg. Pak. 2016, 26, 557–561. [Google Scholar]
- Maymone, M.B.; Mirza, F.N.; Steiner, D.; Ribeiro, F.; Landau, M.; Marçon, C.; Celidonio, T.C.; Soon, S.L.; Wambier, C.G. Comparative long-term efficacy of phenol-croton oil chemical peels for persistent melasma at varied Croton tiglium oil concentrations. J. Am. Acad. Dermatol. 2024, 91, 336–338. [Google Scholar] [CrossRef]
- Murray, T.N.; Lohray, R.; Schultz, K.P.; Boutros, S.; Friedman, P.M. Complications of Chemical Peels, Lasers, and Energy-Based Device Procedures Performed by Core Cosmetic Physicians: A Retrospective Analysis. Lasers Surg. Med. 2024, 56, 619–624. [Google Scholar] [CrossRef]
- de Mendonça, M.C.C.M.; Segheto, N.N.; Aarestrup, F.M.; Aarestrup, B.J.D. Punctuated 88% Phenol Peeling for the Treatment of Facial Photoaging: A Clinical and Histopathological Study. Dermatol. Surg. 2018, 44, 241–247. [Google Scholar] [CrossRef]
- Levy, T.; Lerman, I.; Waibel, J.; Gauglitz, G.G.; Clementoni, M.T.; Friedmann, D.P.; Duplechain, K.; Peng, P.; Lim, D.; Al-Niaimi, F.; et al. Expert Consensus on Clinical Recommendations for Fractional Ablative CO2 Laser, in Facial Skin Rejuvenation Treatment. Lasers Surg. Med. 2025, 57, 15–26. [Google Scholar] [CrossRef]
- Khetarpal, S.; Desai, S.; Kruter, L.; Prather, H.; Petrell, K.; Depina, J.; Arndt, K.; Dover, J.S. Picosecond laser with specialized optic for facial rejuvenation using a compressed treatment interval. Lasers Surg. Med. 2016, 48, 723–726. [Google Scholar] [CrossRef] [PubMed]
- Wu, D.C.; Goldman, M.P.; Wat, H.; Chan, H.H.L. A Systematic Review of Picosecond Laser in Dermatology: Evidence and Recommendations. Lasers Surg. Med. 2021, 53, 9–49. [Google Scholar] [CrossRef] [PubMed]
- Cheles, D.; Vinshtok, Y.; Gershonowitz, A. Microneedling With RF-Assisted Skin Penetration Improves the Hard-to-Treat Periorbital Wrinkles: Nonrandomized Clinical Trial. J. Cosmet. Dermatol. 2024, 23, 3999–4006. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.V.; Christman, M.P.; Feng, H.; Pomerantz, H.; Lederhandler, M.; Geronemus, R.G. Paired facial treatment with 755 nm picosecond laser with diffractive lens array and 1060nm laser lipolysis of the submentum: An open-label prospective trial. J. Cosmet. Dermatol. 2021, 20, 3492–3497. [Google Scholar] [CrossRef]
- Belletti, S.; Madeddu, F.; Brando, A.; Provenzano, E.; Nisticò, S.P.; Fusco, I.; Bennardo, L. Laser Impacts on Skin Rejuvenation: The Use of a Synergistic Emission of CO2 and 1540 nm Wavelengths. Medicina 2023, 59, 1857. [Google Scholar] [CrossRef]
- Munavalli, G. A Split-Face Assessment of the Synergistic Potential of Sequential Q-Switched Nd:YAG Laser and 1565 nm Fractional Nonablative Laser Treatment for Facial Rejuvenation in Fitzpatrick Skin Type II-V Patients. J. Drugs Dermatol. 2016, 15, 1335–1342. [Google Scholar]
- Wat, H.; Wu, D.C.; Chan, H.H. Fractional resurfacing in the Asian patient: Current state of the art. Lasers Surg. Med. 2017, 49, 45–59. [Google Scholar] [CrossRef]
- Seirafianpour, F.; Pour Mohammad, A.; Moradi, Y.; Dehghanbanadaki, H.; Panahi, P.; Goodarzi, A.; Mozafarpoor, S. Systematic review and meta-analysis of randomized clinical trials comparing efficacy, safety, and satisfaction between ablative and non-ablative lasers in facial and hand rejuvenation/resurfacing. Lasers Med. Sci. 2022, 37, 2111–2122. [Google Scholar] [CrossRef] [PubMed]
- Tao, J.; Hashemi, D.A.; Bajaj, S.; Wang, J.V.; Geronemus, R.G. Paired Treatment Using Radiofrequency Microneedling and 755-nm Picosecond Laser with Fractionated Lens Array for Facial Rejuvenation. Dermatol. Surg. 2024, 50, 1163–1166. [Google Scholar] [CrossRef] [PubMed]
- Soleymani, T.; Lanoue, J.; Rahman, Z. A Practical Approach to Chemical Peels: A Review of Fundamentals and Step-by-step Algorithmic Protocol for Treatment. J. Clin. Aesthet. Dermatol. 2018, 11, 21–28. [Google Scholar] [PubMed]
- Nofal, E.; Nofal, A.; Gharib, K.; Nasr, M.; Abdelshafy, A.; Elsaid, E. Combination chemical peels are more effective than single chemical peel in treatment of mild-to-moderate acne vulgaris: A split face comparative clinical trial. J. Cosmet. Dermatol. 2018, 17, 802–810. [Google Scholar] [CrossRef]
- Bae, Y.C.; Rettig, S.; Weiss, E.; Bernstein, L.; Geronemus, R. Treatment of Post-Inflammatory Hyperpigmentation in Patients With Darker Skin Types Using a Low Energy 1927 nm Non-Ablative Fractional Laser: A Retrospective Photographic Review Analysis. Lasers Surg. Med. 2020, 52, 7–12. [Google Scholar] [CrossRef]
- Dierickx, C. Using normal and high pulse coverage with picosecond laser treatment of wrinkles and acne scarring: Long term clinical observations. Lasers Surg. Med. 2018, 50, 51–55. [Google Scholar] [CrossRef]
- Sales, A.F.S.; Pandolfo, I.L.; de Almeida Cruz, M.; Parisi, J.R.; Garcia, L.A.; Martignago, C.C.S.; Renno, A.C.M.; Vassão, P.G. Intense Pulsed Light on skin rejuvenation: A systematic review. Arch. Dermatol. Res. 2022, 314, 823–838. [Google Scholar] [CrossRef]
- Ferreira, F.C.; Sathler, C.S.C.O.; Hida, I.Y.; Leite, S.C.; Kusabara, A.A.; de Castro, A.C.V.; Ribeiro, M.Z.M.L.; Nahas, T.R. Upper eyelid blepharoplasty using plasma exeresis: Evaluation of outcomes, satisfaction, and symptoms after procedure. J. Cosmet. Dermatol. 2021, 20, 2758–2764. [Google Scholar] [CrossRef]
- Wollina, U.; Goldman, A. Long lasting facial rejuvenation by repeated placement of calcium hydroxylapatite in elderly women. Dermatol. Ther. 2020, 33, e14183. [Google Scholar] [CrossRef]
- Dayan, S.H.; Ho, T.T.; Bacos, J.T.; Gandhi, N.D.; Kalbag, A.; Gutierrez-Borst, S. A Randomized Study to Assess the Efficacy of Skin Rejuvenation Therapy in Combination with Neurotoxin and Full Facial Filler Treatments. J. Drugs Dermatol. 2018, 17, 48–54. [Google Scholar]
- Meguid, A.M.A.; Attallah, D.A.E.A.; Omar, H. Trichloroacetic Acid Versus Salicylic Acid in the Treatment of Acne Vulgaris in Dark-Skinned Patients. Dermatol. Surg. 2015, 41, 1398–1404. [Google Scholar] [CrossRef]
- Ali, B.; ElMahdy, N.; Elfar, N.N. Microneedling (Dermapen) and Jessner’s solution peeling in treatment of atrophic acne scars: A comparative randomized clinical study. J. Cosmet. Laser Ther. 2019, 21, 357–363. [Google Scholar] [CrossRef]
- de Vries, F.; Meulendijks, A.; Driessen, R.; van Dooren, A.; Tjin, E.; van de Kerkhof, P. The efficacy and safety of non-pharmacological therapies for the treatment of acne vulgaris: A systematic review and best-evidence synthesis. J. Eur. Acad. Dermatol. Venereol. 2018, 32, 1195–1203. [Google Scholar] [CrossRef]
- Kligman, D.E.; Draelos, Z.D. Combination Superficial Peels with Salicylic Acid and Post-Peel Retinoids. J. Drugs Dermatol. 2016, 15, 442–450. [Google Scholar]
- Clementi, A.; Cannarozzo, G.; Guarino, L.; Zappia, E.; Cassalia, F.; Alma, A.; Sannino, M.; Longo, C.; Nistico, S.P. Sequential Fractional CO2 and 1540/1570 nm Lasers: A Narrative Review of Preclinical and Clinical Evidence. J. Clin. Med. 2025, 14, 3867. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).