1. Introduction
The adoption of artificial intelligence (AI) and advanced digital workflows is transforming full-arch implant dentistry, especially for edentulous patients who require precise implant placement and prosthetic fit to restore both function and facial aesthetics. This is particularly significant for geriatric individuals with atrophic arches, for whom facial symmetry, soft tissue support, and smile harmony are critical to overall satisfaction and quality of life. Traditional full-arch rehabilitation methods are often time-consuming and technique-sensitive, frequently involving multiple appointments for impressions, trial fittings, and framework adjustments. By contrast, digital intraoral scanning and AI-guided planning have been shown to streamline workflows while improving accuracy and predictability—factors essential for achieving passive fit and aesthetic predictability [
1].
Recent studies confirm that AI can enhance scanning trueness, optimise prosthetic alignment with facial reference points, and reduce operator errors, thereby directly influencing symmetry and smile design [
1]. For example, the integration of facial scans and algorithmic midline and occlusal plane verification supports more predictable aesthetic outcomes, even in complex edentulous cases. This paradigm shift not only enhances technical precision but also aligns treatment outcomes with each patient’s unique facial characteristics, fostering greater confidence in rehabilitated smiles.
The combination of AI and digital workflows therefore represents a significant leap forward in prosthodontics, enabling tailored solutions that balance functional reliability with individualised aesthetics. As these technologies continue to evolve, dental practitioners must remain adaptable and committed to integrating AI-driven solutions into everyday practice to elevate patient care, especially for vulnerable populations such as elderly edentulous patients.
This narrative review synthesises the current evidence on AI-supported intraoral scanning and prosthetic workflows for full-arch implant rehabilitation. A structured literature search (PubMed and Google Scholar) was conducted for studies published from 2018 to 2025, using terms including “AI in prosthodontics”, “intraoral scanning accuracy”, “edentulous arch digital workflow”, and “smile design”. The inclusion criteria focused on peer-reviewed clinical or in vitro studies reporting on scanning accuracy, aesthetic parameters, patient-reported outcomes, or relevant technological innovations. Single-case reports, opinion papers, and non-peer-reviewed sources were excluded.
This paper highlights innovations such as the Medit SmartX All-on-X scanning workflow and the Scan Ladder system, examining their documented impact on accuracy, passivity, and facial harmony. By exploring these developments, this review aims to provide clinicians with a clearer understanding of how AI technologies can help achieve consistently superior functional and aesthetic outcomes in edentulous full-arch prosthodontics.
2. Challenges in Edentulous Full-Arch Implant Scanning
Rehabilitating a fully edentulous arch with implants demands an extremely high accuracy to ensure the passive fit of the prosthesis across all implants. Conventional intraoral scanners face inherent challenges in this scenario: the absence of teeth or distinct landmarks in an edentulous jaw makes it difficult for software to stitch scan segments without distortion. Errors tend to accumulate over long spans, leading to cross-arch discrepancies such as angular distortions and linear misalignment between implant positions.
These inaccuracies can translate into a lack of passive fit of the final prosthesis, in which the implant framework does not seat stress-free on all implants, increasing the risk of screw loosening, marginal bone stress, or prosthetic fracture. Even minor distortions, measured in tens of microns, can lead to vertical discrepancies of 50–100 µm across an arch, significantly impacting occlusal contacts and framework passivity [
2].
Indeed, in vitro comparisons have shown that conventional intraoral scans of a full edentulous arch remain the least accurate among impression techniques: for example, Iturrate et al. [
3] and Abuduwaili et al. [
4] (both in vitro studies) reported intraoral scanning with a mean RMS error of ~92 µm—more than double that of conventional impressions (~40 µm) and far higher than photogrammetry-based impressions (~11–13 µm). Intraoral scans also exhibited notable cross-arch angular deviations of approximately 0.5°, compared to around 0.1° for photogrammetric methods, which can translate to misfits of up to 100 µm in distal implant positions.
To address these challenges, recent advancements in scanning techniques, such as the use of auxiliary devices, have demonstrated an improved accuracy for digital impressions of edentulous arches [
5]. For instance, splinted scan bodies and auxiliary geometry parts help reduce both linear and angular deviations, stabilising the scan path and improving stitching precision [
6,
7]. These improvements are clinically significant: better scan trueness directly reduces the likelihood of framework rocking, occlusal discrepancies, and the need for time-consuming adjustments or remakes [
8,
9].
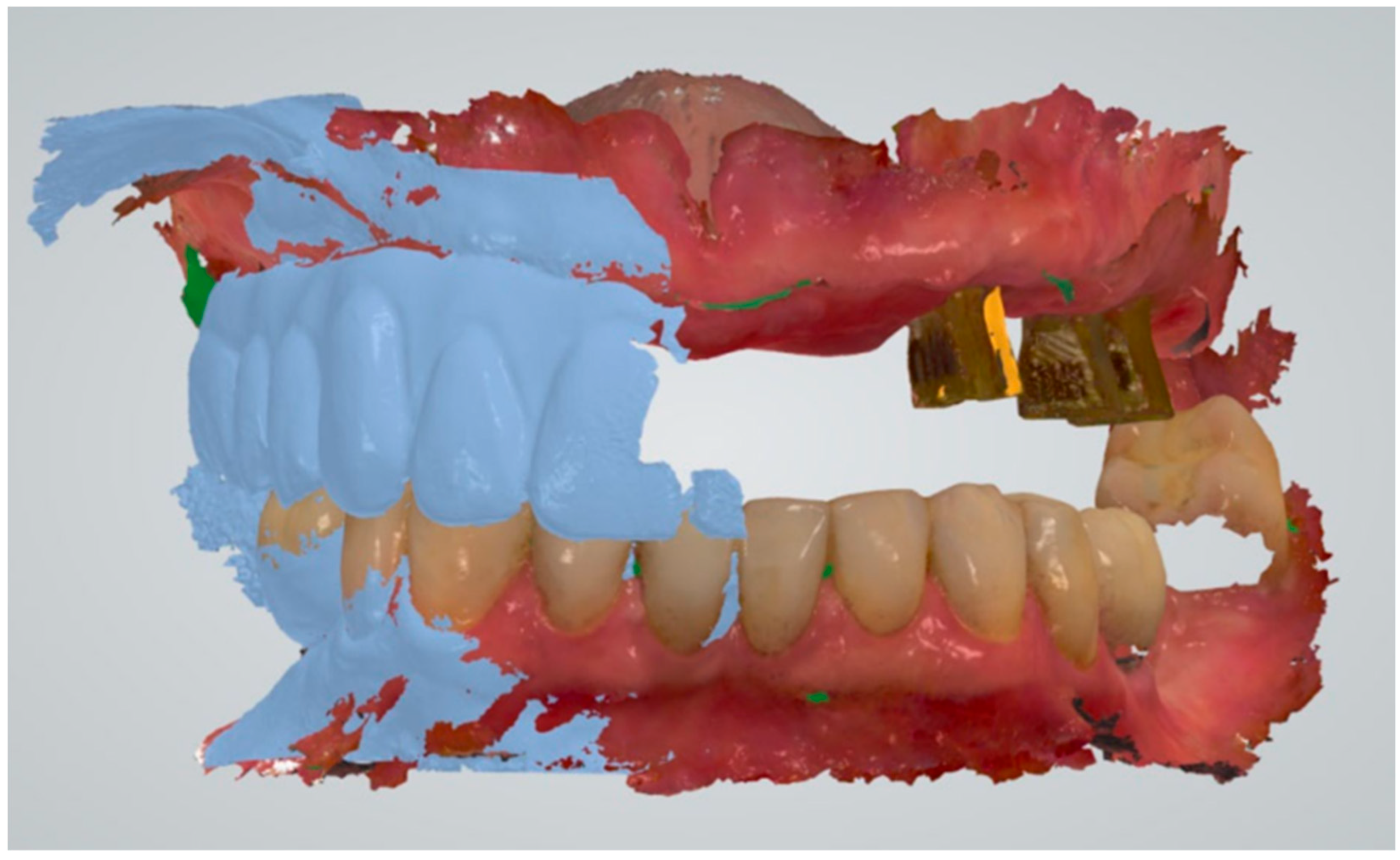
Such errors in recording implant positions can have substantial clinical consequences. (
Figure 1) A misfit of the implant framework may manifest as rocking, uneven torque on prosthetic screws, or occlusal discrepancies, each requiring extensive chairside corrections [
10]. If left undetected, a non-passive prosthesis can impose continuous biomechanical stress on implants and surrounding bone, contributing to marginal bone loss or implant failure. Analog workflows have long employed verification jigs and sectioned frameworks to confirm passive fit; similarly, robust verification protocols remain critical in digital workflows to ensure that digital impressions translate accurately into physical prostheses [
11,
12].
In summary, the edentulous full-arch case remains a “stress test” for any digital impression system, pushing the limits of achievable trueness and precision. The challenges are amplified in geriatric patients with atrophic ridges, minimal bony landmarks, and resilient soft tissue, which further complicate scanning and prosthesis support. For these patients, who often have reduced tolerance for multiple lengthy appointments, first-time accuracy is not just desirable but essential.
3. Aesthetic Considerations in Edentulous Implant Dentistry
Achieving optimal aesthetic outcomes in edentulous implant dentistry requires careful consideration of gingival morphology, tooth shape, and the preservation of soft tissue integrity—all of which are crucial for enhancing patient satisfaction and quality of life [
13]. The interplay between soft tissue aesthetics and precise implant placement is especially important, as it directly influences the final appearance of the prosthesis and overall patient-reported outcomes.
Digital workflows must therefore address the challenge of reproducing natural gingival contours and maintaining the health of peri-implant tissues, particularly in geriatric patients who may have significant ridge resorption. Advanced scanning technologies are essential for capturing and replicating the complex anatomy of the edentulous ridge, ensuring that the final prosthesis achieves both functional stability and a natural appearance [
14].
Combining accurate digital impressions with AI-driven prosthetic design can significantly enhance aesthetic predictability by optimising midline verification, occlusal plane alignment, and tooth proportions relative to the patient’s facial references [
15]. Recent studies, such as Liu et al. [
16] and Chau et al. [
17], have demonstrated that AI-designed crowns and prostheses can match or even surpass traditional designs in terms of occlusal contact accuracy and aesthetic integration, while also improving consistency and efficiency [
18,
19]. Leveraging these AI capabilities allows for individualised tooth setups and soft tissue profiles that better align with the patient’s facial features.
For geriatric patients in particular, this focus on natural-looking results and soft tissue support is vital for restoring confidence and enhancing their oral health-related quality of life (OHRQoL). Measures such as the OHIP-EDENT index have been shown to improve significantly when soft tissue contours and smile line transitions are planned with digital smile design and AI-supported workflows [
18].
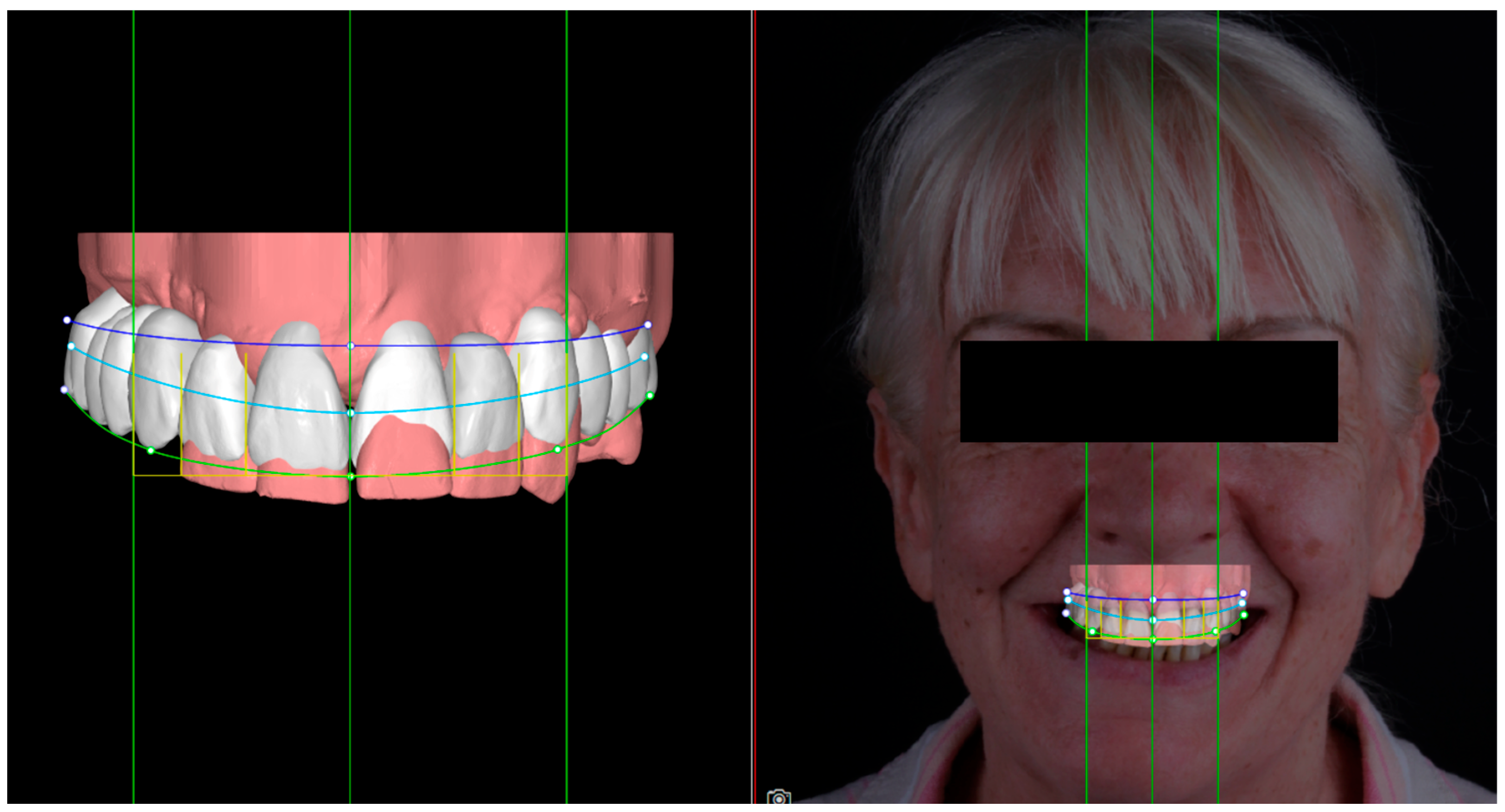
This integrated approach not only streamlines the design process but also contributes to a more predictable and satisfying treatment experience for patients. (
Figure 2 By reducing the need for extensive chairside adjustments and enabling the visualisation of aesthetic outcomes in advance, AI-driven workflows improve treatment acceptance and satisfaction, particularly for elderly patients with limited tolerance for repeat visits [
19,
20].
Implementing AI solutions in aesthetic rehabilitation therefore holds strong promise for achieving patient-centred, high-quality results in complex edentulous cases. As AI technologies continue to evolve, their role in optimising prosthetic aesthetics—and in improving patients’ daily confidence and social interactions—will become increasingly significant, especially for the growing geriatric population [
20,
21].
4. Facial Symmetry, Smile Aesthetics, and the Impact of Incorrect Scan Alignment
Achieving facial symmetry is a fundamental goal in aesthetic dentistry, as it directly influences patient satisfaction and the perceived success of treatment outcomes. Incorporating advanced digital workflows can help mitigate the risks associated with incorrect scan alignment in prosthodontic procedures, which might otherwise cause discrepancies in prosthesis fit that adversely affect both facial symmetry and smile harmony [
21]. Even a small misalignment in the digital scan can translate into an incisal plane cant or off-centre midline when the prosthesis is seated intraorally, highlighting the need for precise protocols and verification steps [
22].
Clinical protocols such as Digital Smile Design (DSD) (
Figure 3) and 3D facial scans have been shown to improve midline verification and occlusal plane control by aligning intraoral scans with extraoral reference points, including the interpupillary line and mid-sagittal plane. Hassan et al. [
23] demonstrated that integrating facial scans into CAD workflows helps maintain symmetry by reducing discrepancies during the design-to-delivery process.
Furthermore, the implementation of AI-driven technologies can support the real-time monitoring of scan alignment, automatically flagging angular or linear deviations that exceed clinical tolerance thresholds. This enhances treatment precision and reduces the likelihood of unexpected asymmetries in the final prosthesis. By minimising errors through continuous AI validation, clinicians can achieve results that more closely align with patient expectations for facial balance and smile aesthetics—an outcome that is particularly valuable for geriatric patients with reduced soft tissue support [
24].
The integration of AI in these verification steps not only elevates precision but also fosters a deeper understanding of how digital workflows interact with facial aesthetics [
25]. By implementing such protocols, clinicians can deliver restorations that are harmonised with the patient’s unique facial features, ensuring higher satisfaction and quality of life.
5. AI-Driven Intraoral Scanning Innovations
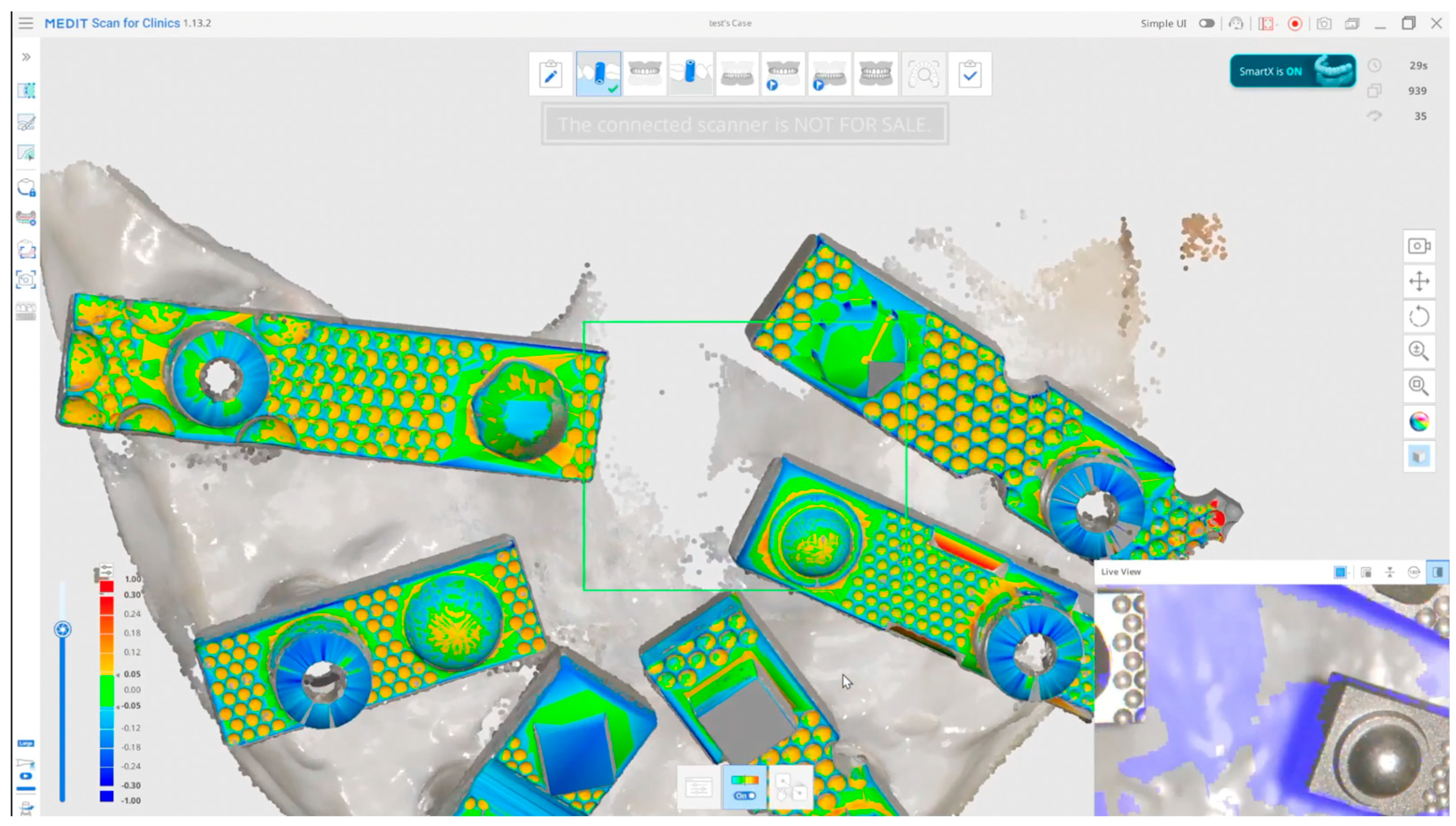
Recent advances are harnessing AI and novel reference devices to overcome the challenges of accurate full-arch implant scanning. Medit SmartX is a dedicated All-on-X AI scanning workflow introduced in 2025, designed to improve full-arch implant impression accuracy and efficiency without requiring special hardware. It operates on existing Medit intraoral scanners (i700, i700 Wireless, i600, and i900 models) and provides an optimised, step-by-step protocol for edentulous implant cases [
26]. One key feature is real-time automatic library alignment: the SmartX software uses AI-powered geometric recognition algorithms—rather than machine learning—to identify implant scan bodies as they are scanned and instantly align them to their corresponding CAD library files in the correct 3D position. This geometric matching approach reduces cumulative stitching errors by offloading alignment to known reference geometries (the scan bodies and Scan Ladder;
Figure 4) and ensures each implant’s position is registered with high fidelity.
The workflow also emphasises an optimised scan strategy and data capture technique. For example, it guides the user to scan in a specific sequence—beginning with a preliminary scan of the edentulous arch, then scanning the attached scan bodies, followed by the opposing arch and occlusion—to minimise distortion. Medit reports that this protocol, coupled with real-time geometric recognition, yields exceptionally precise and detailed full-arch scans, even in feature-poor edentulous scenarios [
26]. Early clinical adopters have found that SmartX streamlines the All-on-4/6 workflow by enabling the immediate digital verification of implant pick-up and often reduces the need for traditional verification jigs. This integrated AI matching not only speeds up the scanning process (by automatically locating and aligning scan bodies) but also helps to avoid the stitching errors that have historically plagued full-arch intraoral scans.
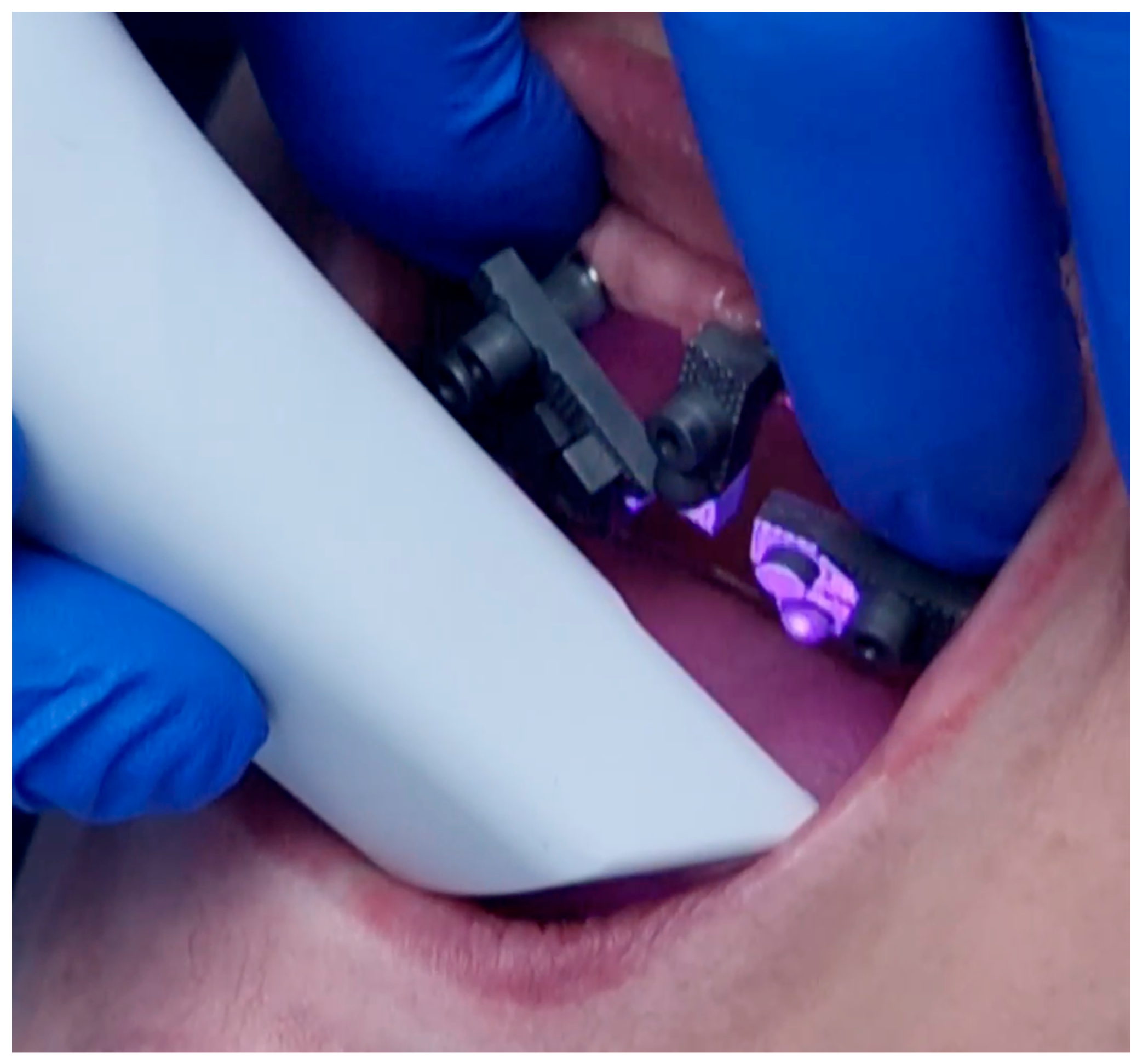
Complementing software innovations like SmartX, physical scanning aids have also emerged to boost edentulous scan accuracy. The Scan Ladder system is one such innovation: a patented set of scanning auxiliaries that provide additional 3D reference geometry during the intraoral scanning of implants. The device can be used in two variants: an indirect Scan Ladder (attached onto conventional scan bodies) and a direct titanium Scan Ladder (a reusable ladder-like frame that directly connects to multi-unit abutments) [
27]. In essence, the Scan Ladder introduces a rigid scaffold with recognisable, individual geometry to each scan body, which the scanner can easily track. As the surface is structured and unique for each segment, the scanner’s algorithm can merge each 3D scan frame accurately, avoiding poor alignment on a featureless edentulous surface (
Figure 5). This reduces the reliance on indistinct gum topography for stitching. The ladder’s distinct pattern acts like an expanded scan body, enabling the software to “lock in” the relative positions of implants across the arch.
Crucially, the Scan Ladder scan bodys (
Figure 5) can be repositioned mid-scan without losing alignment, thanks to a common matching cylinder geometry in each segment. This helps capture long spans without distortion, essentially providing an intraoral photogrammetry-like workflow using a standard scanner. Other recent techniques, such as the reverse scan body protocol (e.g., Straumann’s RevEX system), also aim to improve full-arch digital impressions by capturing implant positions in a stable extraoral setup [
28]. While these approaches do not use AI in the machine learning sense, they leverage smart geometric matching and workflow design to achieve accuracy once limited to expensive photogrammetry rigs. They highlight a clear trend: using practical innovations to push intraoral scanners closer to traditional benchmark accuracy.
6. Accuracy and Clinical Outcomes with AI-Integrated Workflows
The introduction of AI-integrated scanning workflows and scanning aids has yielded significant improvements in full-arch accuracy. In a recent in vivo pilot study, Nulty [
29] evaluated edentulous implant scans in 10 patients using two high-end intraoral scanners (Primescan and Medit i900), both with and without the Scan Ladder device, compared against a reference standard. The results were striking: using the Scan Ladder significantly enhanced the overall trueness and precision of both scanners, to the point that there were no statistically significant differences (
p > 0.05) between the ladder-aided scans and those captured with a dedicated intraoral photogrammetry system. The effect size for the trueness improvement was reported to be large (Cohen’s d ≈ 0.7–0.8).
In other words, the conventional scanners alone showed notable deviation from the true implant positions, but once the Scan Ladder was applied, their accuracy matched that of the photogrammetric method (long regarded as the gold standard for full-arch implant capture). These results suggest that the Scan Ladder effectively compensates for the known weaknesses of intraoral scanning in edentulous cases, enabling standard IOS devices to achieve photogrammetry-level accuracy within tens of microns. Such improvements are not just theoretical; better trueness and precision translate directly into clinical gains by reducing prosthetic misfits. Achieving a passive fit reduces complications such as screw loosening and helps preserve the planned occlusion and smile aesthetics by minimising the need for framework or tooth adjustments.
It is important to note that inter-operator variability can significantly affect these outcomes. Studies have shown that a short learning curve—often five to ten full-arch cases—is necessary for clinicians to achieve consistent sub-20 µm misfits using advanced scanning workflows and aids [
29]. Training in scan path strategy and real-time deviation checks is therefore essential to maximise the potential of AI-integrated workflows in routine practice.
These findings highlight why integrating advanced scanning technologies and AI-driven solutions is critical for enhancing patient care and long-term treatment success. When comparing these digital advancements (
Figure 6) to traditional methods, the evidence suggests that well-implemented digital workflows can deliver comparable clinical success. For example, a 2025 systematic review by Vieira et al. [
30] found that survival rates and complication rates for full-arch fixed prostheses were statistically similar between intraoral scanning and conventional impressions, with marginal bone loss comparable in both groups. Additionally, intraoral scanning significantly reduced chair time compared to analogue impressions, with patients reporting greater comfort. Although digital cases sometimes require additional rescans or adjustments, the overall treatment efficiency and patient experience generally favour digital workflows—especially when aided by the latest AI and scanning devices.
It is worth noting that many of the studies in that review predated these recent AI enhancements; thus, further improvements can reasonably be expected with state-of-the-art workflows like Medit SmartX. Cheng et al. [
31] showed that conventional intraoral scans without dedicated aids displayed significant cross-arch discrepancies that were not fully corrected even when scan bodies were splinted in software, whereas photogrammetry remained far superior for meeting clinical passivity thresholds.
Now, however, with real-time AI matching and physical aids like the Scan Ladder, this accuracy gap is closing. For example, Abuduwaili et al. (2025) [
4] reported that standard IOS (Trios) performed least accurately in their model test, but photogrammetry systems (PIC and iCam) produced the best results. The goal of innovations such as SmartX and the Scan Ladder is to empower intraoral scanners to overcome these limitations, delivering the efficiency of digital workflows without sacrificing accuracy. This appears to be increasingly feasible, as shown in recent pilot studies. The integration of AI-driven technologies in intraoral scanning not only enhances accuracy but also boosts workflow efficiency, leading to better patient experiences and outcomes in full-arch implant rehabilitation.
From a clinical perspective, these accuracy gains translate into fewer prosthetic complications and a more comfortable process for the patient (
Figure 7). When implant positions are captured precisely, the final prosthesis seats fully on day one—reducing or eliminating the need for manual grinding, inter-proximal adjustments, or sectioning and soldering the framework. Occlusion is more likely to be delivered as planned if the digital bite is based on an accurate scan, minimising intraoral compensations. This efficiency is especially important for elderly patients, who may have limited ability to travel or sit through multiple lengthy adjustment appointments.
7. Influence on Aesthetic Outcomes in Geriatric Patients
Beyond mechanical fit, the precision afforded by AI-integrated scanning can profoundly influence aesthetic outcomes. Full-arch implant rehabilitations not only restore teeth but also recreate soft tissue contours and facial support—effectively serving as the foundation for the lower third of a patient’s face. Even slight inaccuracies in the digital model can lead to the subtle misalignment of the prosthetic teeth, which might result in an asymmetrical smile or a canted occlusal plane [
32]. For example, a distorted scan in which one side of the arch is slightly “tilted” can produce a prosthesis with an incisal plane sloping relative to the patient’s interpupillary line. High trueness helps ensure that the planned midline and occlusal plane in the software translate accurately to the mouth, preserving facial symmetry and smile harmony [
33].
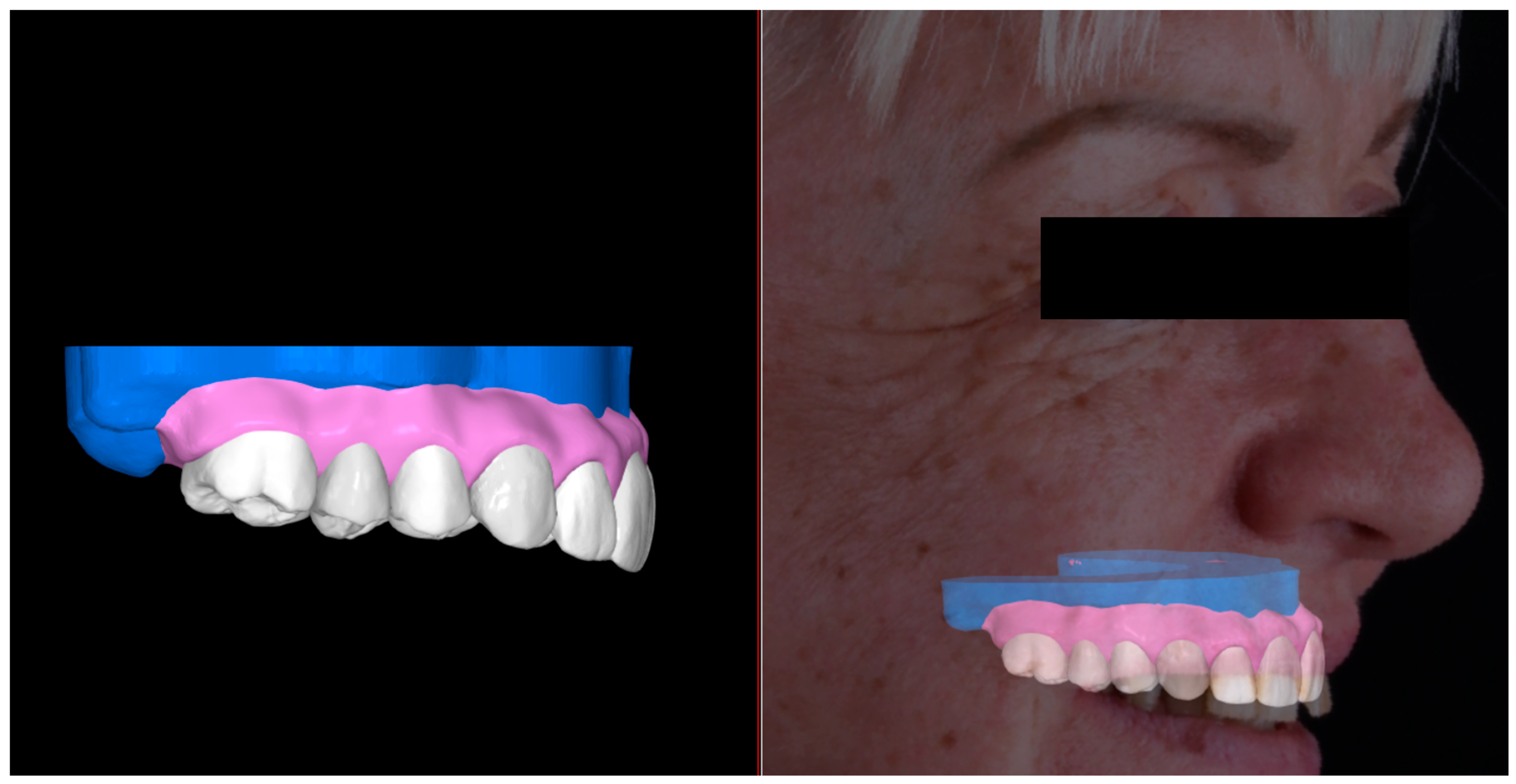
In an aesthetically driven protocol, the clinician typically captures extra-oral photographs or a 3D facial scan to record the facial mid-sagittal plane, lip line, and smile arc [
34]. These references guide the digital design: ideally, the virtual tooth setup is aligned so the occlusal plane is parallel to the interpupillary line and the dental midline coincides with the facial midline (
Figure 8). If the arch scan is inaccurate, achieving this alignment digitally is pointless—the prosthesis may look correct in CAD but seat incorrectly intraorally. By improving full-arch scan trueness, SmartX and the Scan Ladder help ensure that what is designed with respect to the patient’s facial references is what is delivered, preserving symmetry and a properly oriented smile line [
35]. This is particularly vital for geriatric patients, whose facial features and soft tissue contours strongly influence their confidence and overall quality of life.
Older patients often present with advanced ridge resorption and reduced lip support. Full-arch prostheses for these patients frequently require a flange or gingival portion (an FP-3 prosthesis) to restore facial fullness. One critical aesthetic parameter is the transition line—the junction between the prosthetic pink resin/ceramic and the natural gingiva. For patients with a high smile line, an exposed transition line is an aesthetic flaw [
18]. Digital planning allows this line to be positioned optimally (usually just under the lip line) by simulating the smile. AI tools now assist with this too: for example, some dental CAD software such as Exocad uses facial scans or photographs to automatically propose tooth positions that match the patient’s facial proportions—a form of AI-powered digital smile design. In the full-arch context, AI-driven design software can arrange prosthetic teeth to maximise facial harmony, accounting for symmetry, tooth display, and even the patient’s lip dynamics captured on video [
35]. With Medit SmartX now integrated with Imagoworks’ AI prosthetic design platform, scan data can feed directly into an algorithm that produces a full-arch design in minutes, giving clinicians and patients rapid visual feedback.
Once implant positions and jaw relationships are accurately recorded, AI-supported CAD can suggest a tooth setup that the clinician or technician can then fine-tune. This rapid turnaround is particularly valuable in geriatric cases: a printed try-in prosthesis or “digital wax-up” can be fabricated on the same day as scanning, allowing the patient to preview the aesthetics (such as tooth shape, smile line, and lip support) much earlier in the process [
36]. Quick AI-driven iterations make it possible to adjust tooth positioning or gingival contours before final milling or printing. Early studies indicate that such workflows improve patient satisfaction and perceived quality of care, as patients see a near-final result sooner and can provide input to achieve an outcome that meets their expectations [
37]. This alignment with patient-reported satisfaction measures, including OHRQoL tools like the OHIP-EDENT index, demonstrates that improved aesthetic predictability does translate into tangible quality-of-life gains for elderly patients.
By improving initial accuracy and leveraging AI in prosthetic design, the risk of aesthetic compromises from mid-process corrections is reduced. For example, if a misfit is discovered late, a prosthesis may need to be sectioned or remade, which can harm the final aesthetics (e.g., unintended spacing or thickened flanges). Avoiding this via accurate scanning helps ensure the smile design is realised as planned (
Figure 9).
Moreover, many geriatric patients have diminished adaptability to changes in their prosthesis; a precisely fitting implant denture that maintains the vertical dimension and lip support of the temporary prosthesis (to which they have adapted) helps preserve their facial appearance and comfort [
37]. Overall, the synergy of high-fidelity scanning and AI-guided prosthetic planning (
Figure 9) yields an end result in which facial symmetry, gingival aesthetics, and smile dynamics are optimised. Contemporary prosthodontics increasingly emphasises this macro-aesthetic perspective—considering the patient’s entire face and smile, not just the teeth in isolation. Tools like virtual articulators, smile simulation software, and facial scanners are now routine in full-arch cases; AI integration supercharges these capabilities, making it feasible to achieve a harmonious result consistently, even in complex geriatric cases. One notable example is the rehabilitation of a severely atrophic edentulous mandible in just three fully digital appointments—demonstrating that digital planning can address extreme cases while preserving both function and facial aesthetics. In summary, AI-enhanced precision underpins the technical requirements for aesthetics (accurate midline, occlusal plane, and lip support), while AI design automation offers new avenues to customise and preview the smile for the patient, ultimately improving aesthetic satisfaction and quality of life in this population [
38].
8. Comparison with Traditional Workflows
Traditional full-arch implant workflows rely on analogue impressions (often using custom trays, border moulding, and verification jigs) and a series of trial fittings (wax try-ins for tooth setup and often a metal framework try-in) to finalise the fit and aesthetics. These methods have proven to be successful and remain the reference standard for many clinicians. However, they come with notable drawbacks: impression techniques can be uncomfortable for patients (e.g., gagging or pressure from trays), and the process from when the impression is taken to delivery may stretch over numerous visits. Errors can also arise at various stages, including impression material distortion, plaster cast inaccuracies, or the mishandling of verification jigs during transport [
39,
40].
Digital workflows aim to eliminate some of these steps: a single intraoral scan replaces the physical impression and stone cast, and virtual try-ins can reduce the number of physical appointments. Historically, the main question has been whether digital impressions could match the accuracy of well-executed conventional impressions [
41]. Early studies indicated that standard intraoral scanning might fall short without additional aids. As a result, photogrammetry systems were often recommended to complement or replace IOS for full-arch implant cases to achieve an accuracy comparable to that of the traditional gold standard. However, with the addition of AI-driven solutions such as SmartX’s algorithmic alignment and physical references like the Scan Ladder, this gap is closing. For example, while adding a splint bar to connect implant scan bodies did not measurably improve scanner accuracy in earlier tests [
42], the structured approach of SmartX (guided scan sequence with real-time matching) and the robust reference geometry of the Scan Ladder have demonstrated significant gains. This convergence of digital and analogue methods signals a transformative shift in prosthodontics—enhancing both efficiency and patient satisfaction through improved accuracy and streamlined workflows.
From a practical standpoint, these new digital workflows simplify procedures and reduce steps that historically required multiple appointments. The Medit SmartX protocol consolidates scanning and verification: clinicians can immediately inspect the merged scan with all implants positioned, something not possible with a traditional impression until the cast is poured and indexed. Moreover, digital workflows enable remote collaboration: laboratories and specialists can receive scan data instantly via cloud platforms like Medit Link, which speeds up the design and fabrication phase. Traditional workflows often require physical models to be shipped or lab technicians to visit the clinic for shade and aesthetic checks—tasks that can now be handled via shared digital images or live video calls with the 3D model onscreen [
43]. Geriatric patients stand to gain significantly from these efficiencies: fewer appointments and a faster turnaround help reduce the overall treatment burden.
A recent systematic review noted that clinical chair time is significantly shorter with intraoral scanning than with conventional impressions, and patients overwhelmingly prefer avoiding the discomfort of impression materials. That said, analogue methods still play an important role as a backup or fail-safe. Many clinicians use a hybrid approach: for example, they may fabricate a prosthesis based on digital scans but verify fit with an analogue impression or printed jig if any doubt arises. As AI and digital tools continue to mature, confidence in purely digital workflows is steadily increasing, with fewer remakes and fewer manual adjustments required [
44].
Cost and training remain key considerations in this comparison. Traditional analogue methods involve relatively low material costs (trays, impression material, and stone casts), while digital workflows require an upfront capital investment in scanners, software licenses, and ongoing maintenance. However, as technology becomes more widely adopted and competition grows, the cost barrier is falling. Many clinics report that savings in clinical time, reduced remakes, and improved fit offset the initial investment over time. Well-trained teams often find digital full-arch cases more predictable and less prone to last-minute corrections than analogue workflows.
Nonetheless, potential risks must be acknowledged to ensure a balanced view. Digital workflows still carry possible sources of error, such as the misinterpretation of scan data by AI, scanner drift in long-span cases, or software glitches that go unnoticed until prosthesis delivery. If verification protocols are skipped, undetected misfits can occur. It is therefore essential that clinicians maintain robust quality control checks—just as in traditional workflows—and stay up to date with training as AI tools evolve. Furthermore, ethical considerations such as data privacy, patient consent for AI use, and equitable access to advanced technology are especially important when treating vulnerable or geriatric patients [
45,
46].
Ultimately, as digital and analogue methods continue to converge, the goal remains clear: to harness the best of both worlds to deliver more efficient, precise, and patient-centred care.
9. Recent Advances and Future Directions
The landscape of full-arch implant dentistry is undergoing a rapid transformation, driven by the integration of artificial intelligence and digital technologies. AI algorithms for edentulous scanning have advanced considerably, now offering improved pattern recognition, distortion correction, and artefact filtering. For example, machine learning is increasingly used to detect areas of scan distortion and automatically correct them based on known geometric relationships. Intraoral scanners can now flag potential inaccuracies during capture and propose a “best-fit” alignment in real time. Similarly, AI-driven artefact removal algorithms can distinguish soft tissues—such as cheeks, tongue, and reflections from saliva—and exclude them during data acquisition, significantly enhancing scan clarity for large edentulous spans.
Another important development is the integration of CBCT and intraoral scan data through AI-assisted matching. This fusion allows clinicians to merge bone-level imaging with soft-tissue detail, enabling the planning of prostheses with bone reduction guides or immediate-load frameworks more accurately. AI streamlines this process by automatically aligning datasets through common landmarks, saving time and improving consistency in digital planning [
47].
The concept of a “digital twin” is also emerging—an advanced virtual replica of the patient that includes hard and soft tissues, facial features, and even functional movements. Tools such as Modjaw (
Figure 10) allow for dynamic occlusal tracking and 4D jaw motion capture, which, when combined with AI interpretation, enable highly individualised prosthetic planning. This technology is particularly advantageous in geriatric patients, for whom age-related changes such as a reduced vertical dimension or facial volume loss can be visualised and addressed through targeted design modifications. AI can even simulate proposed changes, such as increased occlusal vertical dimension, to assess their aesthetic and functional impact before proceeding with treatment [
48,
49].
Hardware innovation is keeping pace. Scanners like the Medit i900 employ third-generation optical engines with enhanced data density and noise reduction, improving the quality of edentulous surface capture. Increased depth of field and wider scanning windows allow for easier capture of entire arches, reducing stitching errors and eliminating the need for physical splinting or additional landmarks. Some systems now support multi-scan merging—scanning the arch in separate left, right, and anterior segments and then using AI to best-fit these datasets into a unified, highly accurate model [
50,
51]. By leveraging AI to weigh the confidence of each region’s scan data, this technique effectively averages out minor distortions and delivers a better overall precision [
52].
In prosthetic design, AI tools like Imagoworks AOX are rapidly reshaping workflows. After receiving a scan, these systems can automatically detect implant positions and generate full-arch prosthesis designs within minutes, using databases of aesthetic smile libraries. The clinician or technician then acts more as a verifier or aesthetic editor, refining the design rather than creating it from scratch. This “Less for More” model—fewer manual steps, more consistent output—is especially valuable as demand for full-arch solutions grows with ageing populations. These tools are also learning continuously from diverse clinical cases, including those with geriatric-specific traits such as supra-eruption, flabby ridges, or enlarged tongue space, allowing them to propose increasingly nuanced and suitable restorations for complex presentations [
2,
53].
Looking forward, real-time AI feedback during intraoral scanning could soon become the norm. Future systems may alert the operator—during scanning—that a particular area may result in an unacceptable misfit, suggesting immediate rescanning to avoid downstream complications. This predictive capability, based on machine learning from thousands of clinical cases, could further reduce remakes and improve passivity from the outset. Additionally, adaptive AI could recommend optimal scan paths based on the individual patient’s anatomy (e.g., advising a mid-arch start point in cases of advanced atrophy) or tailor scan parameters dynamically to reduce glare or artefacts in patients with dry mouths, mobile tissues, or high frenal attachments.
Finally, AI could detect and flag intraoral challenges such as flabby ridges, shallow vestibules, or shiny surfaces, and either compensate digitally or prompt the clinician to take special measures (e.g., apply a tissue conditioner digitally or modify scan settings). These patient-specific adjustments are particularly valuable for elderly individuals, many of whom present with anatomical and functional limitations that compromise traditional scanning methods [
54,
55].
As these tools become more embedded in clinical practice, ethical considerations must also be addressed. The use of facial scans, intraoral data, and patient-specific algorithms raises concerns about data privacy, consent, and the responsible application of AI outputs. Patients—particularly older adults—must understand how their data are being used and give their informed consent for AI-assisted planning. Moreover, the digital divide must not be ignored: some patients may lack access to clinics using advanced technology or may struggle to understand AI-based planning unless clearly communicated by clinicians. Developers and practitioners must also ensure that AI models are trained on demographically diverse datasets to reduce potential biases that could affect outcomes for older patients or those with atypical anatomical features [
47,
48].
In summary, the future of AI in edentulous full-arch prosthodontics is not only about speed and precision—it is about equitable, personalised, and ethically grounded care. These tools have the potential to empower clinicians and improve outcomes dramatically, particularly for geriatric patients whose needs are often the most complex and whose quality of life can be most transformed by thoughtful, accurate rehabilitation.
10. Conclusions
The integration of AI into full-arch implant dentistry marks a new era of precision, efficiency, and truly patient-centred care—especially for edentulous patients with complex functional and aesthetic needs. Technologies such as Medit SmartX and the Scan Ladder system exemplify how smart algorithms and innovative hardware can overcome traditional barriers in intraoral scanning, achieving accuracy levels once limited to laboratory workflows or costly photogrammetry systems. These advancements translate into concrete clinical benefits: more passive-fitting prostheses, reduced alignment errors, and more predictable restorative outcomes with less need for remakes.
For geriatric patients with atrophic arches and diminished tolerance for lengthy, invasive procedures, AI-enhanced digital workflows offer the dual advantage of faster treatment times and highly customised results. By capturing implant positions and oral anatomy with digital precision—and then leveraging AI for real-time validation and prosthetic design—clinicians can ensure that facial symmetry, smile lines, and occlusal harmony are not only planned virtually but reliably delivered at insertion.
Emerging data show that AI-driven workflows can match or even exceed the reliability of conventional methods, with comparable implant survival and complication rates, while improving patient comfort and reducing chair time. Equally important, these tools empower clinicians to deliver outcomes that align with patients’ individual aesthetic expectations and functional needs—an outcome especially valued by elderly patients seeking to regain confidence and increase their quality of life.
Nonetheless, it remains essential to approach these innovations with a critical eye. Not all AI or digital solutions are plug-and-play; a clear learning curve, rigorous verification protocols, and ongoing operator training are needed to maintain high standards. Long-term clinical studies will be vital to confirm the durability of AI-planned rehabilitations across diverse patient groups. Additionally, ethical considerations such as data privacy, informed consent, and equitable access must guide the adoption of these technologies, ensuring that AI truly enhances care for all, not just those with access to premium systems.
Despite these important caveats, the trajectory is clear: AI and digital dentistry are steadily closing the gap between the ideal treatment plan and the final delivered result. For the aesthetics-focused practitioner, this means greater confidence that the carefully crafted smile design on-screen will manifest as intended in the patient’s mouth. For the patient—especially geriatric patients who entrust us to restore not just their teeth but their facial balance and confidence—the fusion of AI and digital workflows is fulfilling that promise more consistently than ever before.
In conclusion, AI integration in full-arch implant workflows—through systems like Medit SmartX and the Scan Ladder—represents not just a technical upgrade but a transformative, human-centred step forward. By marrying precision engineering with the artistry of smile rehabilitation, these innovations are helping clinicians deliver beautiful, functional, and predictable outcomes that improve patients’ daily lives—a goal at the heart of contemporary aesthetic medicine and dentistry.