Abstract
Foreign body intestinal perforation is a critical and potentially life-threatening condition that presents significant diagnostic challenges, especially in rural populations who are often distant from healthcare facilities and lack access to necessary resources. In these settings, the surgical approach is further complicated by prolonged diagnostic times and delayed access to appropriate care. This article presents a series of cases involving patients with foreign body intestinal perforation of both vegetable and animal origin. Among these cases, one patient died due to delayed voluntary treatment, and another presented without leukocytosis, further complicating the diagnosis. Socioeconomic barriers made follow-up challenging in most cases, negatively impacting patient outcomes. This study details patient characteristics, surgical approaches, and outcomes. Community education, improved infrastructure, and greater awareness among healthcare providers are essential to improving outcomes, particularly in rural areas where healthcare delivery is more challenging and intensified efforts are required to enhance patient care and quality of life.
1. Introduction
The gastrointestinal system functions as a closed system, with primary roles of nutrient breakdown, absorption, and waste elimination. Intestinal perforation occurs when the integrity of this closed system is compromised, allowing gastrointestinal contents to leak into adjacent structures. Common causes of intestinal perforation include inflammation, ischemia, trauma, obstruction, foreign bodies, and surgical interventions. The presentation of pain can vary depending on the mechanism of perforation, ranging from progressive to sudden onset. Physical examination findings also depend on the mechanism, location, and progression of the perforation. Early-stage, progressive lower perforations may manifest as generalized abdominal pain, often accompanied by nausea, vomiting, anorexia, and reduced bowel movements. In more severe cases, patients may exhibit rebound tenderness and signs of peritoneal irritation, which can rapidly progress to shock and hemodynamic instability due to peritonitis [1,2]. Mortality rates for patients in this advanced stage can reach as high as 60% [3]. Treatment primarily involves stabilizing the patient for surgery, which may be laparoscopic or open, depending on the surgeon’s assessment, in combination with broad-spectrum antibiotics. Computed tomography (CT) is the preferred imaging modality, if available, to localize and assess the perforation, aiding in surgical planning [4]. When CT is unavailable, X-rays and ultrasound can be used to detect free gas, which is indicative of intestinal perforation [5].
Small intestine perforation has an incidence ranging from 1 in 300,000 to 350,000 cases, accounting for approximately 0.4% of all acute abdomen cases. In developed countries, malignancy and closed-loop obstruction are the primary causes, whereas in developing countries, infectious etiologies are the leading cause of perforation [6]. A case series reports that foreign body ingestion is responsible for 23% of non-traumatic small intestine perforations, indicating that nearly one in four patients with this condition have a foreign body etiology [7]. The morphology of the foreign object also plays a significant role in the perforation process. Long, elongated, and pointed objects are most associated with small traumatic perforations. Items such as fish bones, toothpicks, and chicken bones, which have these characteristics, are reported to cause up to 83% of perforations in ileal loops [8]. Given the associated pathophysiology, complications, and high mortality rates, it is crucial to promptly identify, diagnose, stabilize, and treat these patients to minimize morbidity and mortality.
Research data are more frequently collected from urban areas, contrasting sharply with rural regions. The larger populations and technological advancements in data collection and storage make urban datasets more accessible and robust. However, rural patients face limited and complicated access to healthcare, coupled with technological barriers, making it challenging to gather and report data to the scientific community. This lack of rural data may lead to inaccuracies in epidemiological estimates. Additionally, regional feeding patterns and customs influence individual risks for intestinal perforation due to foreign body ingestion [8]. Expanding data collection from rural populations would enable a greater focus on preventive and health-promoting services, ultimately improving the quality of life for these patients [9,10]. The objective of this study is to report and characterize patients presenting with foreign body intestinal perforation in the rural jungle region of Caquetá, Colombia. Sociodemographic factors, clinical signs and symptoms, surgical approaches, antibiotic coverage, and patient outcomes are detailed. One case involved a patient who voluntarily withdrew from the healthcare facility, resulting in delayed treatment and eventual mortality. Another patient did not present with leukocytosis in blood tests, complicating the diagnostic process.
2. Materials and Methods
A retrospective, multicentric case series was conducted, involving patients who presented with intestinal perforation due to vegetable foreign bodies. Data from five patients were collected retrospectively between 2016 and 2024 from Corpomédica and Hospital de María Inmaculada in Florencia, Caquetá, Colombia, where gastrointestinal perforations and corrective surgeries were performed.
The following variables were evaluated during the study period: gender, age, preoperative vital signs, preoperative laboratory results, surgical procedures, antibiotic regimen, need for ICU care, length of hospital stay, complications, and mortality. Postoperative follow-ups were conducted when possible.
The surgical approach was tailored to each case based on intraoperative findings. Postoperative management included a 3–5 day course of antibiotics, after which patients were discharged. Ethical approval was waived due to the retrospective nature of the study, which relied on clinical record data. All patients provided signed consent for the use of their data. This study falls under the category of “research with no risk” as outlined by Resolution 8430 of 1993 in Colombian legislation. According to Article 11 of this regulation, such research involves the retrospective review of clinical records without intervention or modification of the participants’ biological, physiological, psychological, or social variables and does not involve sensitive aspects of behavior.
3. Results
The various procedures offer distinct perspectives on foreign bodies encountered during surgery. The pathological findings for each case are illustrated with corresponding figures.
Pathological Findings
In Case 1, a perforated sigmoid colon is observed, with its contents revealing a foreign body surrounded by Chinese ink (Figure 1).
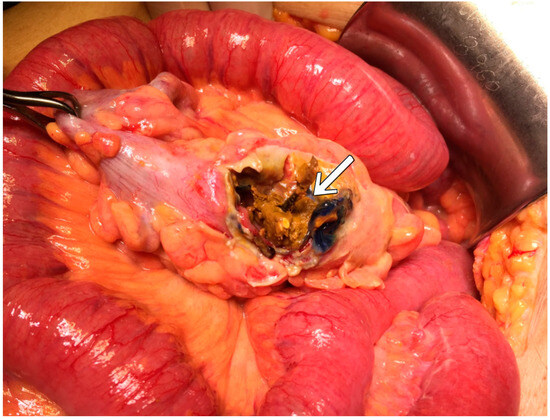
Figure 1.
Foreign body, unidentified as either vegetable or animal.
In Case 2, edematous, shiny, and congested loops of the small intestine are observed, with perforations caused by a foreign body and the presence of fibrinoid membranes (Figure 2).
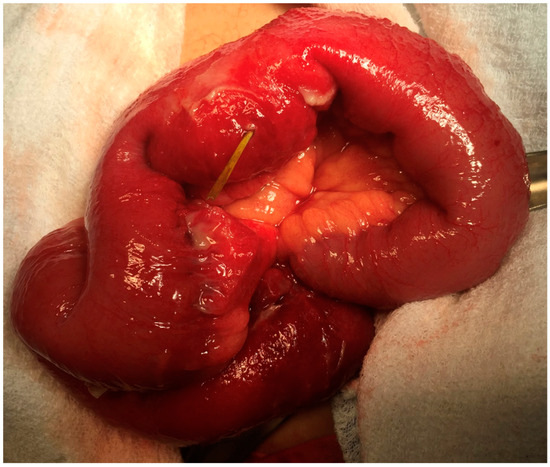
Figure 2.
Mild acute periappendicitis.
In the third case, a foreign body approximately 5 cm in length perforated the intestinal loop (Figure 3).
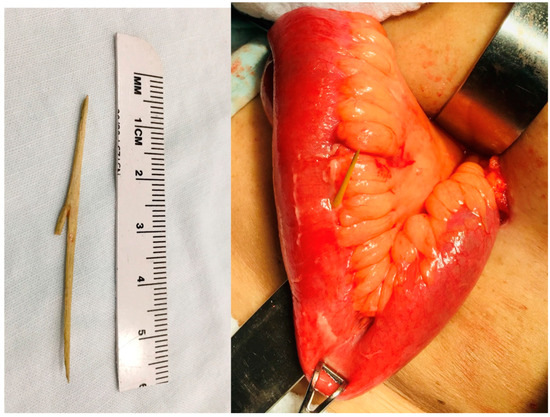
Figure 3.
An appendix with an embedded fish bone featuring bifurcation.
In Case 4, edematous intestinal loops with fibrinopurulent membranes on the mesenteric border were observed, along with a foreign body in the same region. Additionally, hematomas, ulcers, and necrosis were noted in the perforations of the small intestine (Figure 4).
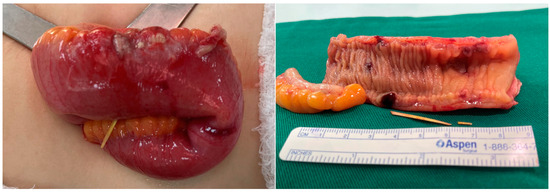
Figure 4.
Transmural necrosis and secondary perforation caused by a foreign animal body.
In Case 5, a perforated transfixing Meckel’s diverticulum was observed, accompanied by edematous, distended loops and peritonitis. The diverticulum contained small bone fragments, along with a congested cecal appendix (Figure 5).
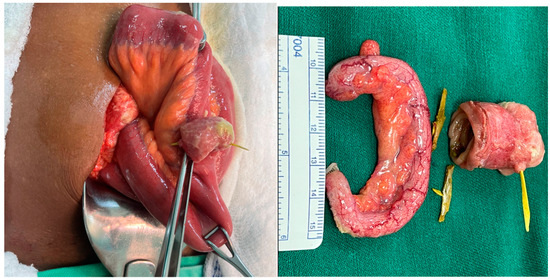
Figure 5.
Meckel’s diverticulum with perforation by vegetable foreign body.
The characterization of the population involved in these cases (Table 1) shows that most patients were female and middle-aged. The duration of symptoms varied, ranging from 3 h (Case 3) to 20 days (Case 1). None of the patients presented with fever, although all exhibited signs of peritoneal irritation. Most did not experience nausea, and their heart rates were generally near tachycardia, with normal blood pressure readings. The average neutrophil percentage was 81.64%, and the average hospital stay after surgery was 3.6 days. Survival was successful in most cases, with the only mortality occurring in a patient who did not undergo surgery upon admission (Case 1). Postoperative antibiotic regimens included clindamycin, gentamicin, cefazolin, metronidazole, ampicillin–sulbactam, ceftriaxone, and meropenem. Pathology reports identified the foreign body in each case, with most patients not requiring close follow-up. However, during postoperative appointments, all cases except Case 1 had favorable outcomes.

Table 1.
Case population characterization.
4. Discussion
Over an eight-year period in this rural area, five cases of foreign body intestinal perforation were diagnosed and surgically treated. The rural landscape, characterized by adjacent rivers, makes the consumption of animals such as fish, chicken, and hen more common in the area. Additionally, the use of toothpicks and chewable straws, typical of rural life, is prevalent. The cohort consisted of three female and two male patients, most of whom were over 50 years old, and all were treated at two institutions by the same lead general surgeon. All patients exhibited clinical signs of acute abdomen, and one presented with hypotension at the time of evaluation. Laboratory tests revealed leukocytosis in three patients and neutrophilia in four. In three cases, the foreign body was removed from the terminal ileum. The average hospital stay was 3.6 days, with only one mortality occurring seven days after presentation. This patient had initially refused surgery despite a confirmed diagnosis of acute abdomen at another institution, later requiring ICU admission due to metabolic acidosis, pleural effusion, and the need for vasopressors to manage blood pressure. Due to the severity of the case, referral to a higher-level care facility was necessary. Pathology reports identified foreign bodies of both animal origin (bones) and vegetable origin (toothpick, straw). Follow-up was challenging due to the socioeconomic difficulties of the rural population, and only one patient consented to follow-up via telephone. A particularly unusual case involved a perforation within a Meckel’s diverticulum, where multiple animal bones were found. Interestingly, one case did not present with leukocytosis or neutrophilia, which is uncommon in such scenarios [2].
There are no epidemiological studies that specifically address factors related to intestinal perforation, as most reports focus on individual cases rather than a series of cases. For instance, “Meckel’s diverticulum perforation: a case report” [11] exemplifies this trend. The rarity of simultaneous cases of intestinal perforation, especially those involving foreign bodies of animal origin, such as buffalo bones [12], makes it difficult to characterize the condition at a population level, including identifying risk factors, relevant clinical histories, and predispositions. In our series, we observed a correlation between patients with anodontia and foreign body ingestion. Patients with anodontia often undergo prosthetic treatment [13], which may reduce oral sensitivity during chewing [14]. Intestinal perforation can potentially occur during or after dental treatments [15]. While many scientific articles focus on individual case reports, this study provides a series of cases, offering a novel perspective on these types of patients. The inclusion of multiple cases allows for a more comprehensive understanding of commonalities and differences, offering insights that individual case reports cannot provide.
The mortality rate for gastrointestinal foreign body ingestion can reach up to 10%, primarily due to delayed diagnosis or misdiagnosis [16]. In our series, the patient’s mortality resulted from delayed intervention, as they initially refused surgery at another institution, bringing our mortality rate to 20% based on raw numbers. However, given the small sample size, this single fatality aligns with one of the leading causes of death in these cases: delayed diagnosis or intervention. Meckel’s diverticulum has an incidence of approximately 2% in the global population, with up to 6.5% of those affected developing complications, the most common being intestinal obstruction [17]. As of 2021, only eight cases of Meckel’s diverticulum perforation due to foreign animal bodies have been reported, making this the rarest complication associated with the condition. In our case, the patient had accumulated multiple foreign animal bodies within the diverticulum, significantly increasing the risk of perforation, which eventually occurred. Bowel perforation compromises the integrity of the intestinal wall, releasing damage-associated molecular patterns (DAMPs) that activate a non-specific immune response, leading to an increase in leukocytes and neutrophils [18]. However, there are rare reports, such as those by Yamaguchi, M., et al., of bowel perforation without an elevated white blood cell count [19]. These unexpected findings were noted in our cases as well.
This study reports on five cases, which constitutes a small sample size. To draw statistically significant conclusions, a larger population would be necessary. However, due to the rural nature of the Colombian patients, the data presented are still valuable. One of the primary challenges of conducting research in this rural context is the limited access to healthcare. Rural patients face barriers such as inadequate infrastructure, a shortage of physicians, and limited resources, all of which contribute to delays in diagnosis and ultimately worsen patient outcomes [20,21]. As a result, many cases of intestinal perforation are likely underreported, underdiagnosed, and undertreated, reflecting the broader difficulties of rural healthcare. Additionally, follow-up presents a significant challenge. The low socioeconomic status of these patients is often associated with poorer health outcomes [22]. Most of the patients were farmers or informal workers who lived far from healthcare centers and needed to be discharged quickly to provide for their families, making it difficult to adhere to standard guidelines for hospital stays and antibiotic coverage. These circumstances highlight the importance of patient education [23]. Patients need to be informed about the risks of bowel perforation due to foreign bodies, such as the use of toothpicks, vegetable straws, and the consumption of fish or chicken bones. Increasing health awareness and encouraging regular medical consultations can improve medical outcomes and enable earlier diagnoses in rural populations.
5. Conclusions
In conclusion, this descriptive study highlights the complexities of diagnosing and managing intestinal perforation caused by foreign body ingestion in rural populations. The limited access to healthcare and delayed presentations observed in these cases underline the challenges faced in such settings. Although the study cannot conclusively attribute delays solely to geographical or socioeconomic factors, the findings suggest that timely recognition and intervention are critical for improving patient outcomes. Moving forward, focused strategies such as enhancing healthcare provider training and community education on the risks of foreign body ingestion may help address these challenges. Further analytical studies are needed to explore the specific social determinants impacting access to care in rural settings.
Author Contributions
Conceptualization, F.E.-C. and S.A.S.-G.; methodology, V.V.-M.; results, F.E.-C. and V.V.-M.; discussion, F.E.-C., S.A.S.-G. and V.V.-M.; formal analysis, S.A.S.-G.; investigation, F.E.-C., S.A.S.-G. and V.V.-M.; resources, F.E.-C.; data curation, F.E.-C.; writing—original draft preparation, F.E.-C., S.A.S.-G. and V.V.-M.; writing—review and editing, V.V.-M.; visualization, V.V.-M.; supervision, F.E.-C. and S.A.S.-G.; project administration, F.E.-C. and S.A.S.-G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The ethical approval is waived due to the nature of the study, which is a retrospective analysis using information from clinical records. The patients provided signed consent for their data to be used in this manner. This type of study falls under the category of “investigation with no risk” as defined by the Resolution 8430 from 1993 in Colombian legislation. According to Article 11 of this regulation, such research involves the retrospective review of clinical records without any intervention or modification of the participants’ biological, physiological, psychological, or social variables, and does not involve sensitive aspects of their behavior.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
The data presented in this study are available on request from the corresponding author due to identity protection measurements.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Hafner, J.; Tuma, F.; Hoilat, G.J.; Marar, O. Intestinal Perforation; StatPearls: Treasure Island, FL, USA, 2024. [Google Scholar]
- Jones, M.W.; Kashyap, S.; Zabbo, C.P. Bowel Perforation; StatPearls: Treasure Island, FL, USA, 2024. [Google Scholar]
- Yoo, R.N.; Kye, B.H.; Kim, G.; Kim, H.J.; Cho, H.M. Mortality risk factor analysis in colonic perforation: Would retroperitoneal contamination increase mortality in colonic perforation? Ann. Surg. Treat. Res. 2017, 93, 203–208. [Google Scholar] [CrossRef] [PubMed]
- Pouli, S.; Kozana, A.; Papakitsou, I.; Daskalogiannaki, M.; Raissaki, M. Gastrointestinal perforation: Clinical and MDCT clues for identification of aetiology. Insights Imaging 2020, 11, 31. [Google Scholar] [CrossRef] [PubMed]
- Singh, J.P.; Steward, M.J.; Booth, T.C.; Mukhtar, H.; Murray, D. Evolution of imaging for abdominal perforation. Ann. R. Coll. Surg. Engl. 2010, 92, 182–188. [Google Scholar] [CrossRef] [PubMed]
- Hines, J.; Rosenblat, J.; Duncan, D.R.; Friedman, B.; Katz, D.S. Perforation of the mesenteric small bowel: Etiologies and CT findings. Emerg. Radiol. 2013, 20, 155–161. [Google Scholar] [CrossRef] [PubMed]
- Kimchi, N.A.; Broide, E.; Shapiro, M.; Scapa, E. Non-traumatic perforation of the small intestine. Report of 13 cases and review of the literature. Hepatogastroenterology 2002, 49, 1017–1022. [Google Scholar] [PubMed]
- Nicolodi, G.C.; Trippia, C.R.; Caboclo, M.F.; de Castro, F.G.; Miller, W.P.; de Lima, R.R.; Tazima, L.; Geraldo, J. Intestinal perforation by an ingested foreign body. Radiol. Bras. 2016, 49, 295–299. [Google Scholar] [CrossRef] [PubMed]
- Bain, L.E.; Adeagbo, O.A. There is an urgent need for a global rural health research agenda. Pan Afr. Med. J. 2022, 43, 147. [Google Scholar] [CrossRef] [PubMed]
- Pearson, T.A.; Lewis, C. Rural epidemiology: Insights from a rural population laboratory. Am. J. Epidemiol. 1998, 148, 949–957. [Google Scholar] [CrossRef] [PubMed]
- Natsuki, S.; Iseki, Y.; Nagahara, H.; Fukuoka, T.; Shibutani, M.; Ohira, M. Liver abscess caused by fish bone perforation of Meckel’s diverticulum: A case report. BMC Surg. 2020, 20, 121. [Google Scholar] [CrossRef] [PubMed]
- Yadav, A.K.; Malla, G.; Deo, K.B.; Giri, S.; Bhattarai, B.M.; Adhikary, S. Jejunal perforation due to ingested buffalo bone mimicking acute appendicitis. BMC Res. Notes 2016, 9, 321. [Google Scholar] [CrossRef] [PubMed]
- Kostrica, R. Prosthetic treatment of partial anodontia in the upper jaw and total anodontia in the mandible. Ceskoslovenska Stomatol. 1966, 66, 303–306. [Google Scholar]
- Atria, P.; Sampaio, C.; Rosas, D.; Córdova, C.; Fernández, E.; Jorquera, G. Risk factors associated with tooth sensitivity in fixed dental prosthesis treatment: A literature review. Odontoestomatología 2019, 21, 62–69. [Google Scholar] [CrossRef]
- Ramaraj, P.N.; Ajeya Ranganathan, H.K.; Nithin, V.M.; Lakshmi, G.V. Accidental intraoperative ingestion of a paralleling pin during implant placement. J. Indian Soc. Periodontol. 2020, 24, 383–386. [Google Scholar] [PubMed]
- Jaan, A.; Mulita, F. Gastrointestinal Foreign Body; StatPearls: Treasure Island, FL, USA, 2024. [Google Scholar]
- Chang, Y.C.; Lai, J.N.; Chiu, L.T.; Wu, M.C.; Wie, J.C. Epidemiology of Meckel’s diverticulum: A nationwide population-based study in Taiwan: Characteristics of the cases from surgery between 1996 and 2013. Medicine 2021, 100, e28338. [Google Scholar] [CrossRef] [PubMed]
- Roh, J.S.; Sohn, D.H. Damage-Associated Molecular Patterns in Inflammatory Diseases. Immune Netw. 2018, 18, e27. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, M.; Yoshizawa, Y.; Kigawa, G.; Machida, H.; Nemoto, H.; Nakano, H.; Uemichi, O.; Sanada, Y.; Kumada, K.; Sasaki, J.; et al. Nine cases of non-traumatic bowel perforation with leukopenia. Showa Med. Soc. J. 2000, 60, 692–698. [Google Scholar]
- Nielsen, M.; D’Agostino, D.; Gregory, P. Addressing Rural Health Challenges Head On. Mo. Med. 2017, 114, 363–366. [Google Scholar] [PubMed]
- Tudor Car, L.; Papachristou, N.; Bull, A.; Majeed, A.; Gallagher, J.; El-Khatib, M.; Aylin, P.; Rudan, I.; Atun, R.; Car, J.; et al. Clinician-identified problems and solutions for delayed diagnosis in primary care: A PRIORITIZE study. BMC Fam. Pract. 2016, 17, 131. [Google Scholar]
- Oshio, T. Exploring the health-relevant poverty line: A study using the data of 663,000 individuals in Japan. Int. J. Equity Health 2019, 18, 205. [Google Scholar] [CrossRef] [PubMed]
- Ohta, R.; Ryu, Y.; Kitayuguchi, J.; Sano, C.; Könings, K.D. Educational Intervention to Improve Citizen’s Healthcare Participation Perception in Rural Japanese Communities: A Pilot Study. Int. J. Environ. Res. Public Health 2021, 18, 1782. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).