Abstract
Gastric leak represents one of the most common, serious and challenging complications in bariatric procedures, and it is caused by both ischemic and mechanical failure. The management of these leaks remains controversial. In this clinical case, we describe the occurrence of a gastric leak after a gastric sleeve, which was successfully treated by gastric bypass using a laparoscopic technique.
1. Introduction
Currently, multiple organizations recognize obesity as a pathology that is not only a predisposing and aggravating factor of other conditions, such as type 2 diabetes mellitus, arterial hypertension, cardiovascular diseases and various oncological pathologies, but has also become one of the main public health problems of the 21st century [1]. Obesity is defined by a body mass index (BMI) greater than 30 kg/m2. Although prevention and measures such as the modification of eating habits, increased physical activity and biopsychosocial change are essential as initial treatments, in most cases, these measures fail due to inadequate implementation or low patient adherence, resulting in disease progression [2].
Bariatric surgery is presented as the most effective option when conservative treatment fails to resolve or significantly hinders the improvement of comorbidities associated with obesity [3]. Some procedures have proven to be effective and safe, ensuring significant, long-lasting and effective weight loss. These procedures include vertical sleeve gastrectomy, Roux-en-Y gastric bypass, adjustable gastric banding and the duodenal switch procedure [4,5]. Despite the multiple benefits offered by these procedures, there is still limited access and insufficient dissemination of these resources as a resolution measure for patients with obesity. Nevertheless, bariatric surgery is one of the areas of general surgery that is experiencing remarkable growth year after year.
In spite of the safety that a surgical procedure can offer and its high success rate, none of them is free of associated complications in early and late stages. One of the most significant complications in bariatric procedures is gastric leakage (GL), which can be caused by staple line dehiscence or perforation. Although the incidence of this complication varies between 0.4% and 3%, it is important to note that it can increase overall morbidity and mortality by up to 61% and 15%, respectively [6]. The following is the case of a 28-year-old woman with a BMI of 40 kg/m2 who underwent surgery and had a 5-day postoperative readmission for a gastric sleeve. The complication was subsequently successfully resolved with a Roux-en-Y procedure.
2. Detailed Case Description
We present a case of a 28-year-old female patient with no relevant clinical or surgical history who was diagnosed with grade III obesity (BMI 40). A vertical gastrectomy was scheduled as a weight loss treatment. On the day of surgery, the patient measured 172 cm in height and weighed 117 kg. During the procedure, reloading failure occurred on the second shot of the stapling device, causing a 2 cm defect in the distal third of the stapling line near the gastric antrum. This defect was successfully repaired by manual suturing in two planes with PDS 2 thread. A watertightness test with methylene blue was performed, confirming the integrity of the suture. The surgical procedure continued and was completed without additional incidents. Considering the event that occurred, a postoperative study was performed with water-soluble contrast medium, which showed no evidence of leakage (Figure 1). The patient was discharged in good general condition on the third postoperative day.
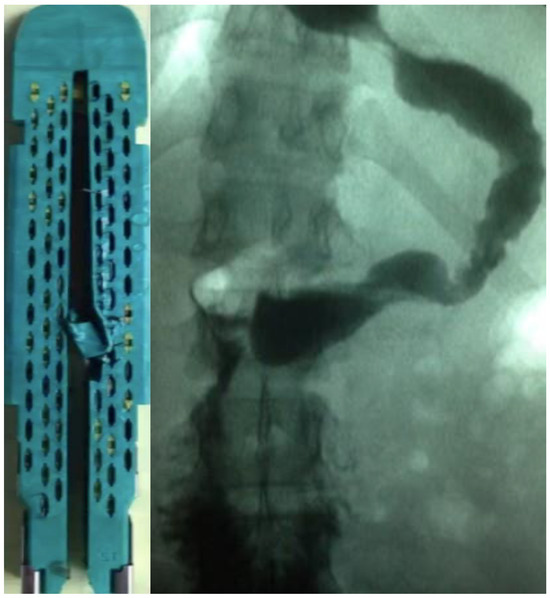
Figure 1.
Echelon Endopath Reload Green stapler (60 Mm, 2.0 Mm staple height) with defective reload, and water-soluble contrast medium study of vertical gastrectomy with no evidence of postoperative leakage.
On the fifth day after the initial medical discharge and the eighth postoperative day, the patient returned to the emergency room for symptoms of acute pain in the left shoulder, fever and draining material. Immediately, a computed tomography (CT) scan was performed, which revealed an extensive leak in the distal portion of the suture line right at the site of the initial defect. In addition, it was accompanied by extensive subphrenic collections. In view of this situation, it was decided to perform an urgent exploratory laparoscopy in which diffuse peritonitis and multiple adhesions were detected (Figure 2). The collections were drained, and the adhesions were released until the point of leakage was located. Subsequently, the proximal portion of the gastric sleeve was sectioned by a mechanical suture, followed by a second lavage to resect the affected segment of the stomach.
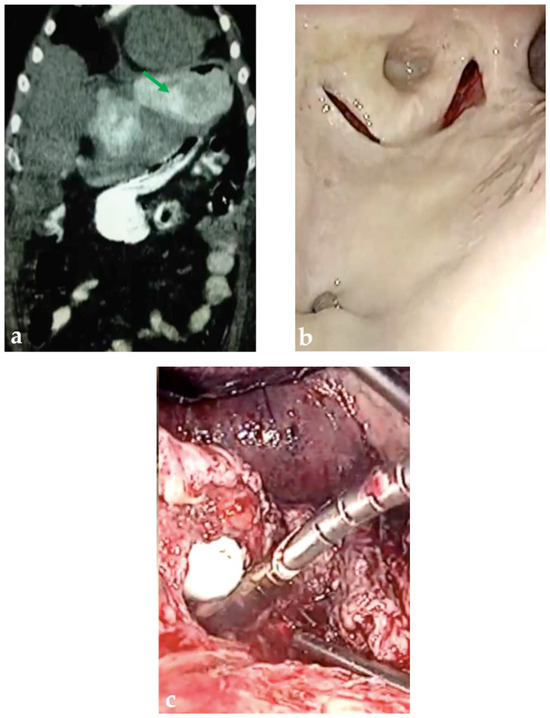
Figure 2.
Admission CT scan and laparoscopic findings. (a) Collection images in subphrenic space by means of CT (green arrow). (b) Intrabdominal collection. (c) Gastric perforation in distal third of suture line.
Finally, an end-to-end gastrojejunal anastomosis was performed with a mechanical suture, followed by a jejunojejunal anastomosis also with a mechanical suture. With these procedures, the initial procedure was converted to a Roux-en-Y bypass (Appendix A). A drain was placed, and the intervention was completed in 240 min with estimated bleeding of 100 cc. The procedure was successfully completed, and the patient tolerated it without complications. On the fifth day of the second intervention, the patient began to accept and tolerate the oral route. She was discharged on the tenth postoperative day, and a reevaluation was performed fifteen days later in the outpatient clinic, where an adequate evolution and weight loss within the expected percentage was evidenced without additional complications.
3. Discussion
In 1998, the World Health Organization (OMS) classified obesity as an epidemic disease and a significant public health problem. Currently, it is recognized as one of the pathologies with the greatest impact on the morbidity and mortality of the affected population [7,8]. Despite governmental and health system efforts to implement preventive and conservative measures, most of them fail to meet the established objectives. Factors such as low adherence to treatments, a lack of motivation, personal perception of the disease or denial of it [2] and the pathophysiological course of obesity itself contribute to this. This course includes complex and persistent hormonal, metabolic and neurochemical adaptations that hinder weight loss and promote weight regain [9].
In patients with obesity with difficulty losing weight and/or significant health problems related to excess weight, metabolic and bariatric procedures have proven to be effective in the treatment of this disease [1,5,10]. These procedures not only help protect against the development and progression of comorbid conditions associated with morbid obesity, but also substantially improve patients’ quality of life [11]. Among the alternative bariatric procedures is the gastric sleeve, which is a restrictive procedure that involves stapling the end of the greater curvature of the stomach. This method stands out for its numerous advantages, such as a low complication rate, reduced operative times and the absence of anastomosis and malabsorption problems. In addition, it offers the possibility of conversion to other bariatric procedures if necessary [12].
Although bariatric procedures have a high success rate, like any surgical intervention, they carry risks of complications. These can be divided into early complications, which occur within the first 30 days after the procedure, and late complications, which occur after this period [13]. In the case presented, an early complication was observed: GL. This is one of the most feared complications, which can originate from the dehiscence or perforation of the staple line, which is mainly associated with the stapler misfiring [14]. The incidence of GL varies between 0.4% and 3%, increasing morbidity by up to 61% and overall mortality by up to 15% [6,14]. In addition, this situation is associated with an increase in the length of hospital stay and in the use of health resources.
GL is classified according to the time of its appearance after the primary intervention. Acute leakage is defined as occurring within the first 7 days after surgery, being the most common among all possible leaks. In addition, the most frequent site for these leaks is located near the proximal third of the suture line at the gastroesophageal junction [15]. This area is particularly vulnerable due to the mechanical stress and delicate anatomical nature. In addition, ischemic causes, such as impaired healing mechanisms associated with local risk factors such as deficient blood supply, infection or poor tissue oxygenation, explain why leakage occurs on average on the fifth postoperative day, when the wound healing process is still in the inflammatory and fibrotic phase [16]. Leaks attributed to mechanical failures usually appear on the second or third postoperative day. These are associated with problems such as poor visualization of the stapling line, poor tissue dissection, inadvertent injury or failure of the stapling material, as evidenced in the clinical case mentioned above.
Among the most frequent clinical manifestations of postoperative GL are tachycardia (MHR > 120) and fever; in addition, other clinical symptoms such as tachypnea, abdominal pain, left shoulder pain and leukocytosis have been documented. During the readmission of the patient in question, some of these symptoms were observed. As for the diagnosis, the most commonly used methods to confirm the leak include radiography with water-soluble contrast medium and double-contrast computed tomography. These tests allow for the visualization and localization of the point of contrast medium extravasation as well as the presence of collections and free air in the abdominal cavity. In unstable and severe patients, extension studies should not delay treatment.
The four fundamental principles for treating a patient with a gastric leak are effective drainage, closure of the fistula, decompression of the stomach and ensuring adequate nutrition. To achieve this goal, multiple techniques and approaches have been described in the treatment of gastric leaks, including conservative, endoscopic and surgical strategies. Conservative treatment is based on the early initiation of antibiotics to cover intra-abdominal infections, fluid therapy, proton pump inhibitors, the addition or no addition of total parenteral nutrition and even the use of percutaneous drainage. This measure is reserved for stable patients without signs of severity and usually has high success rates and low readmission rates. However, there are no clear guidelines on its indications and limitations [17,18]. Another alternative to treat leaks is endoscopic treatment, which includes the use of self-expanding metallic and plastic stents, clipping techniques, tissue sealants, suture systems, endoscopic vacuum therapy (EVAC), endoscopic septostomy and internal drainage methods [19], where clip apposition and internal drainage are the most commonly used methods. Although it has established itself as a minimally invasive and effective option compared to surgery, especially in patients without an obvious perforation [20], it still has certain limitations related to its availability and operating costs. In addition, its efficacy has been observed mainly in the reduction in anastomosis-related complications compared to those associated with the stapling technique. In terms of leaks, its advantage is clearer in the treatment of non-acute leaks. [21].
This surgical approach is recommended after the unsuccessful attempt of conservative treatment, which is defined as a leak that persists beyond 12 weeks despite medical management [22], or in a frankly unstable patient, where the delay translates into increased morbidity and mortality [23]. In our case, the patient required immediate surgical intervention, and given the intraoperative findings, it was not possible to identify a suitable area to apply a new stapling line, including the defect, due to the unfavorable tissue conditions caused by the ongoing peritonitis. Therefore, it was decided to transform the high-pressure procedure, such as vertical gastrectomy (gastric sleeve), which reaches mean intragastric pressures of up to 43 ± 8 mmHg, into a low-pressure procedure, such as laparoscopic gastric bypass (Roux-en-Y bypass). Although this is a controversial decision, it allowed us to work on healthy, non-inflamed tissue away from the area of the initial defect (Appendix A). This technique allows for the early and successful closure of the leak and the control of sepsis and reduces the need for total or proximal gastrectomy in complicated cases [12,18,22]. It is essential to point out that in a reoperation, the surgical risk is higher than in the initial surgery due to factors such as tissue stiffness, the presence of edema, adhesions and a greater predisposition to hemorrhage. Therefore, these procedures should be performed in specialized units by surgeons with extensive experience.
4. Conclusions
Bariatric surgery has proven to be effective in the treatment of obesity. However, GL represents a serious and feared complication associated with these procedures. Controversy exists regarding the optimal management of this complication, with the endoscopic approach being preferable initially when possible. However, in cases where conservative treatment fails or there are severe complications such as generalized peritonitis, the laparoscopic surgical option emerges as the best alternative to achieve a successful resolution. The favorable evolution of the clinical case post-surgery underlines the crucial importance of a timely and adequate intervention in patients with severe complications after bariatric surgeries.
Author Contributions
Conceptualization, M.J.V., H.T.V., I.M.M. and A.H.L.; methodology, M.J.V., H.T.V., I.M.M. and A.H.L.; formal analysis and investigation, M.J.V., H.T.V., I.M.M. and A.H.L.; writing—original draft preparation, M.J.V., H.T.V., I.M.M. and A.H.L.; writing—review and editing, M.J.V., H.T.V., I.M.M. and A.H.L.; visualization, M.J.V., H.T.V., I.M.M. and A.H.L.; supervision, A.H.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived for this study due to the retrospective nature of this study and the minimal risk to participants.
Informed Consent Statement
Informed consent was obtained from the patient and healthcare proxy/decision maker for the publication of the case report and accompanying images.
Data Availability Statement
The data presented in this study are available upon request from the corresponding author. The data are not publicly available due to patient privacy and confidentiality.
Conflicts of Interest
The authors declare no conflicts of interest.
Appendix A
https://www.youtube.com/watch?v=8iEdiydpp1k (accessed on 4 October 2024).
References
- Díaz-González, B.V.; Bautista-Castaño, I.; Hernández García, E.; Cornejo Torre, J.; Hernández Hernández, J.R.; Serra-Majem, L. Bariatric Surgery: An Opportunity to Improve Quality of Life and Healthy Habits. Nutrients 2024, 16, 1466. [Google Scholar] [CrossRef] [PubMed]
- Trujillo-Garrido, N.; Santi-Cano, M.J. Motivation and Limiting Factors for Adherence to Weight Loss Interventions among Patients with Obesity in Primary Care. Nutrients 2022, 14, 2928. [Google Scholar] [CrossRef] [PubMed]
- Palermo, M.; Nedelcu, M. Complications in Bariatric Surgery. J. Laparoendosc. Adv. Surg. Technol. 2021, 31, 139–140. [Google Scholar] [CrossRef] [PubMed]
- Arterburn, D.E.; Telem, D.A.; Kushner, R.F.; Courcoulas, A.P. Benefits and Risks of Bariatric Surgery in Adults. JAMA 2020, 324, 879. [Google Scholar] [CrossRef] [PubMed]
- Rogers, A.M. Current State of Bariatric Surgery: Procedures, Data, and Patient Management. Technol. Vasc. Interv. Radiol. 2020, 23, 100654. [Google Scholar] [CrossRef]
- Lim, R.; Beekley, A.; Johnson, D.C.; Davis, K.A. Early and late complications of bariatric operation. Trauma Surg. Acute Care Open 2018, 3, e000219. [Google Scholar] [CrossRef]
- Pêgo-Fernandes, P.M.; Bibas, B.J.; Deboni, M. Obesity: The greatest epidemic of the 21st century? Sao Paulo Med. J. 2011, 129, 283–284. [Google Scholar] [CrossRef]
- Arrieta, F.; Pedro-Botet, J. Reconocer la obesidad como enfermedad: Todo un reto. Rev. Clin. Esp. 2021, 221, 544–546. [Google Scholar] [CrossRef]
- Blüher, M. Obesity: Global epidemiology and pathogenesis. Nat. Rev. Endocrinol. 2019, 15, 288–298. [Google Scholar] [CrossRef]
- Soroceanu, R.P.; Timofte, D.V.; Danila, R.; Timofeiov, S.; Livadariu, R.; Miler, A.A.; Ciuntu, B.M.; Drugus, D.; Checherita, L.E.; Drochioi, I.C.; et al. The Impact of Bariatric Surgery on Quality of Life in Patients with Obesity. J. Clin. Med. 2023, 12, 4225. [Google Scholar] [CrossRef]
- Raza, M.M.; Njdeaka-Kevin, T.; Polo, J.; Azimuddin, K. Long-Term Outcomes of Bariatric Surgery: A Systematic Review. Cureus 2023, 15, e39638. [Google Scholar] [CrossRef] [PubMed]
- Praveenraj, P.; Gomes, R.M.; Kumar, S.; Senthilnathan, P.; Parthasarathi, R.; Rajapandian, S.; Palanivelu, C. Management of gastric leaks after laparoscopic sleeve gastrectomy for morbid obesity: A tertiary care experience and design of a management algorithm. J. Minim. Access Surg. 2016, 12, 342. [Google Scholar] [CrossRef] [PubMed]
- Hamdan, K.; Somers, S.; Chand, M. Management of late postoperative complications of bariatric surgery. Br. J. Surg. 2011, 98, 1345–1355. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, S.K.; Roy, S.; Chekan, E.; Fegelman, E.J. A Narrative of Intraoperative Staple Line Leaks and Bleeds During Bariatric Surgery. Obes. Surg. 2016, 26, 1601–1606. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Zeng, N.; Liu, Y.; Sun, X.; Yang, W.; Liu, Y.; Mao, Z.; Yao, Q.; Zhao, X.; Liang, H.; et al. Management and outcomes of gastric leak after sleeve gastrectomy: Results from the 2010–2020 national registry. Chin. Med. J. 2023, 136, 1967–1976. [Google Scholar] [CrossRef] [PubMed]
- Soto, F.C. Sleeve Gastrectomy Leaks: The Way, we Treat it. Adv. Obes. Weight. Manag. Control 2015, 2, 119–121. [Google Scholar] [CrossRef]
- Verras, G.I.; Mulita, F.; Lampropoulos, C.; Kehagias, D.; Curwen, O.; Antzoulas, A.; Panagiotopoulos, I.; Leivaditis, V.; Kehagias, I. Risk Factors and Management Approaches for Staple Line Leaks Following Sleeve Gastrectomy: A Single-Center Retrospective Study of 402 Patients. J. Pers. Med. 2023, 13, 1422. [Google Scholar] [CrossRef]
- Kermansaravi, M.; Kassir, R.; Valizadeh, R.; Parmar, C.; Jazi, A.H.; Shahmiri, S.S.; Benois, M. Management of leaks following one-anastomosis gastric bypass: An updated systematic review and meta-analysis of 44 318 patients. Int. J. Surg. 2023, 109, 1497–1508. [Google Scholar] [CrossRef]
- Rogalski, P.; Swidnicka-Siergiejko, A.; Wasielica-Berger, J.; Zienkiewicz, D.; Wieckowska, B.; Wroblewski, E.; Baniukiewicz, A.; Rogalska-Plonska, M.; Siergiejko, G.; Dabrowski, A.; et al. Endoscopic management of leaks and fistulas after bariatric surgery: A systematic review and meta-analysis. Surg. Endosc. 2021, 35, 1067–1087. [Google Scholar] [CrossRef]
- Masood, M.; Low, D.E.; Deal, S.B.; Kozarek, R.A. Endoscopic Management of Post-Sleeve Gastrectomy Complications. J. Clin. Med. 2024, 13, 2011. [Google Scholar] [CrossRef]
- Younis, F.; Shnell, M.; Gluck, N.; Abu-Abeid, S.; Eldar, S.; Fishman, S. Endoscopic treatment of early leaks and strictures after laparoscopic one anastomosis gastric bypass. BMC Surg. 2020, 20, 33. [Google Scholar] [CrossRef] [PubMed]
- Oshiro, T.; Wakamatsu, K.; Nabekura, T.; Moriyama, Y.; Kitahara, N.; Kadoya, K.; Sato, A.; Kitahara, T.; Urita, T.; Sato, Y.; et al. Treatments for Staple Line Leakage after Laparoscopic Sleeve Gastrectomy. J. Clin. Med. 2023, 12, 3495. [Google Scholar] [CrossRef] [PubMed]
- Kassir, R.; Debs, T.; Blanc, P.; Gugenheim, J.; Amor, I.B.; Boutet, C.; Tiffet, O. Complications of bariatric surgery: Presentation and emergency management. Int. J. Surg. 2016, 27, 77–81. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).