Advancing Medical Education Using Virtual and Augmented Reality in Low- and Middle-Income Countries: A Systematic and Critical Review
Abstract
:1. Introduction
- RQ1
- What medical disciplines in training do immersive technology currently apply to?
- RQ2
- Is it necessary to use VR and AR in LMICs for medical education?
- RQ3
- What evaluation methods are used to measure the effectiveness of VR and AR for medical training in LMICs?
- RQ4
- Which medical disciplines in LMICs require immersive technology the most?
- RQ5
- What is the transformative potential of VR and AR to improve medical education?
2. Methodology
2.1. Literature Review
2.1.1. Search Strategy and Selection Criteria
2.1.2. Inclusion and Exclusion Criteria
2.1.3. Manual Screening
2.2. Questionnaire Survey
3. Results and Analysis
3.1. Literature Review
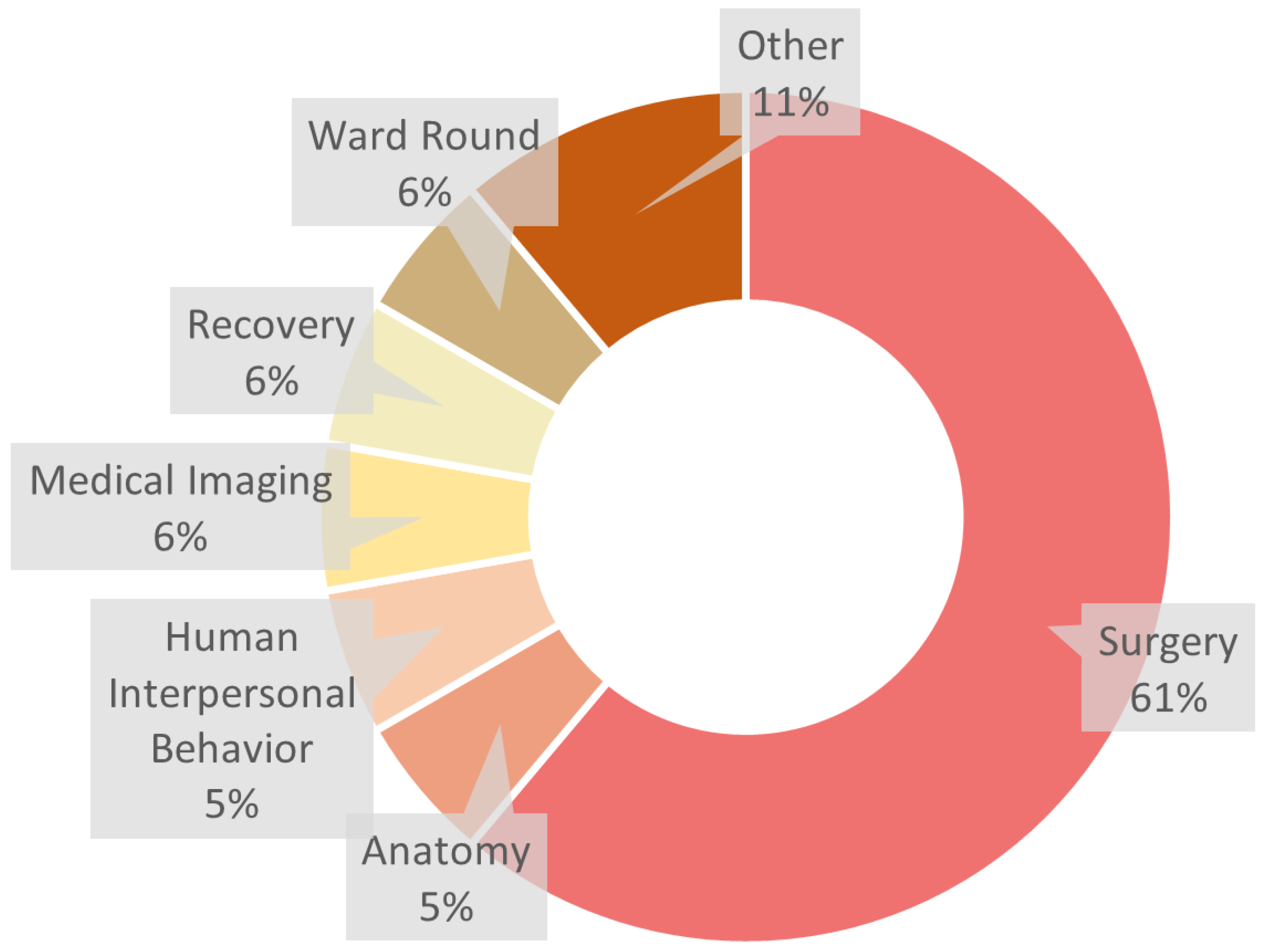
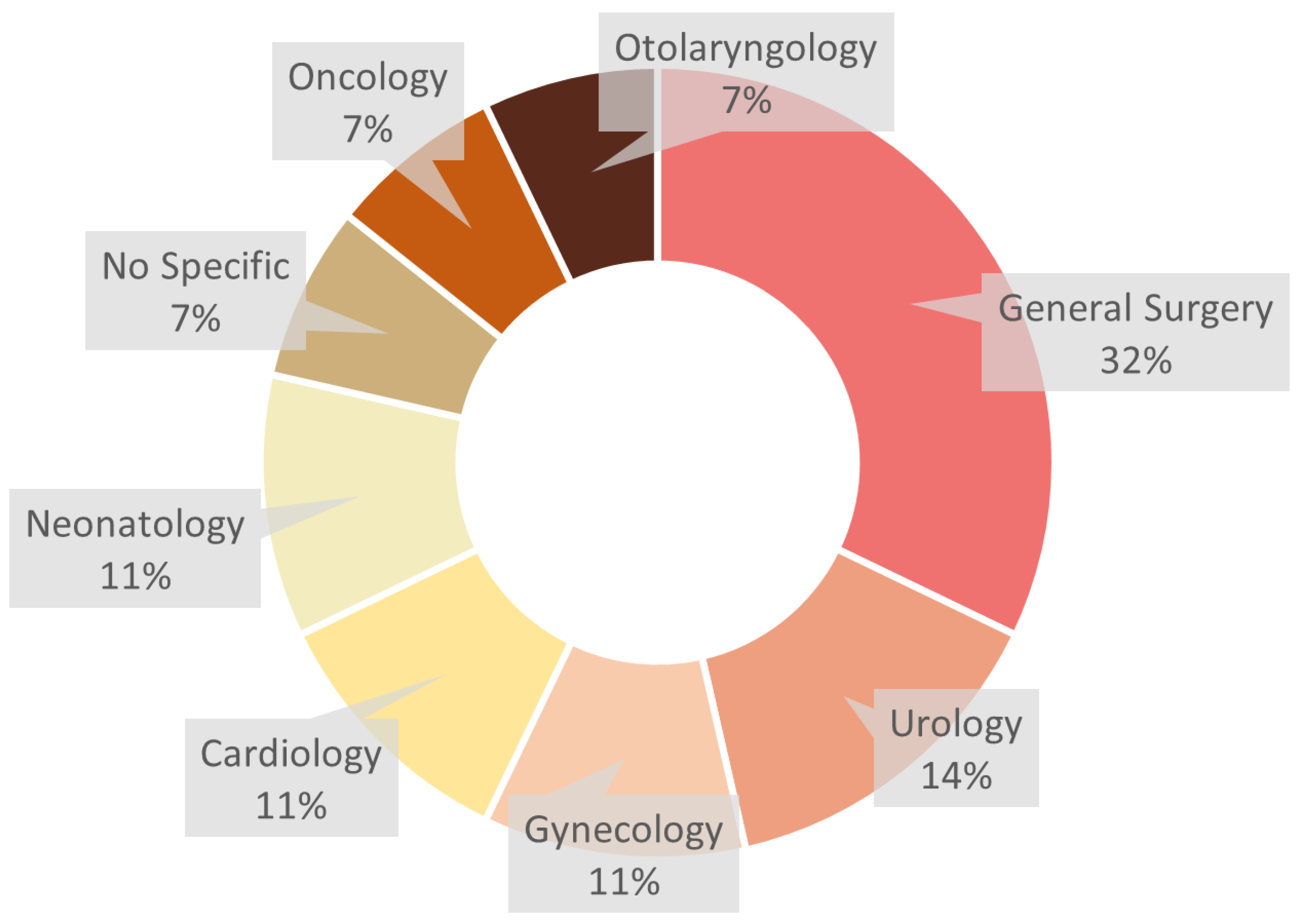
3.1.1. Medical Disciplines with VR and AR
3.1.2. The Necessity of VR and AR
3.1.3. Evaluation Methods for VR and AR in Medical Training
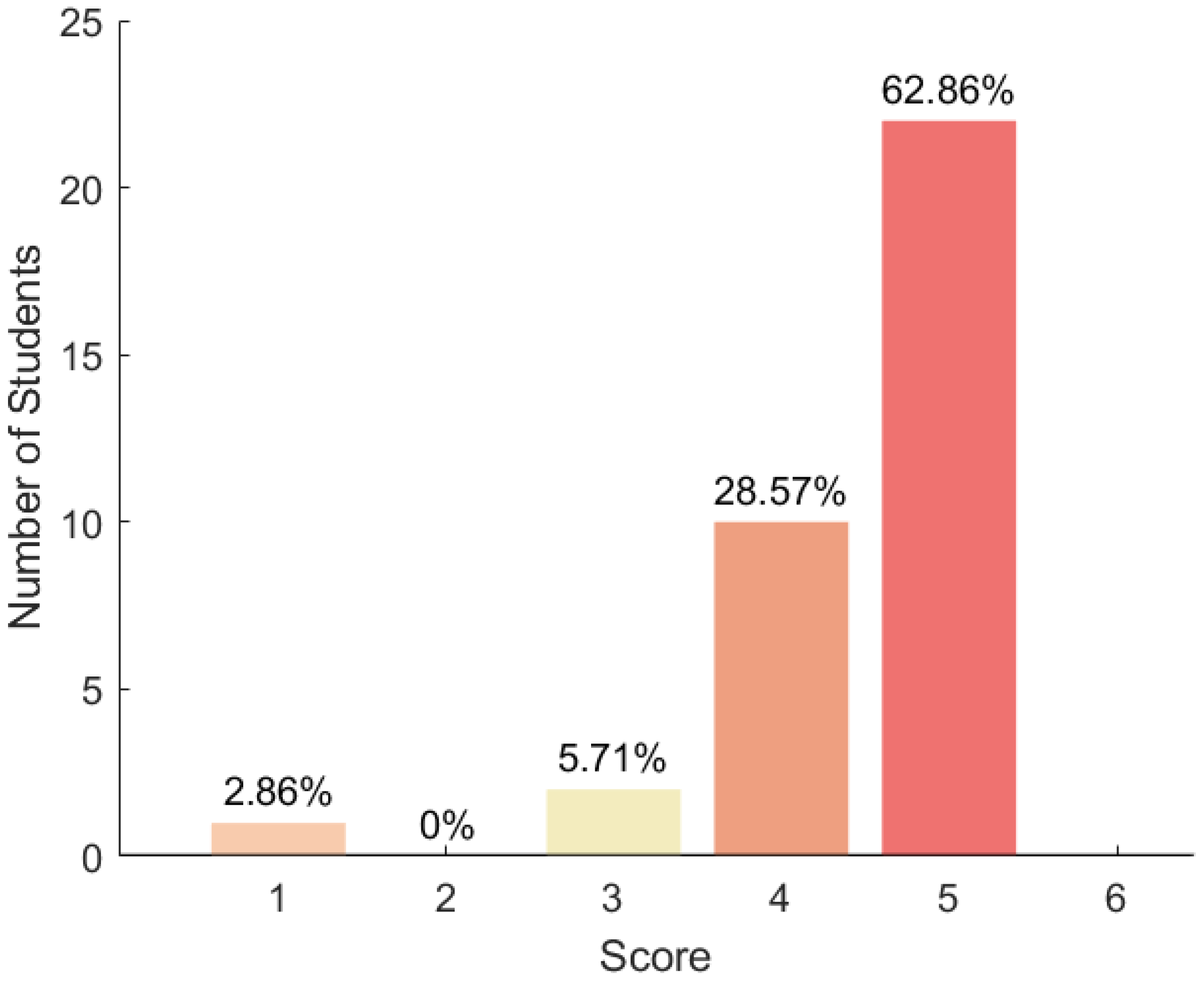
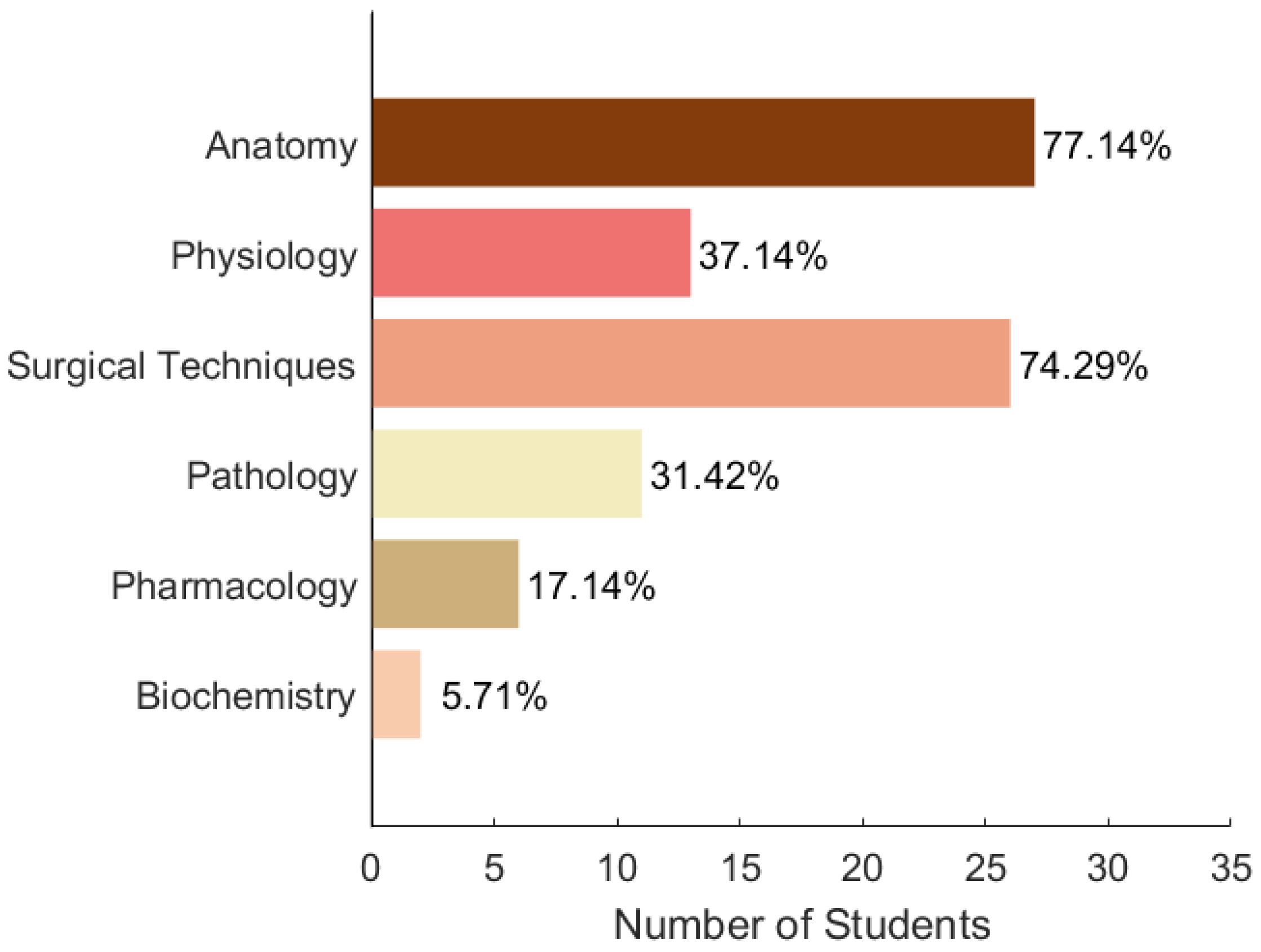
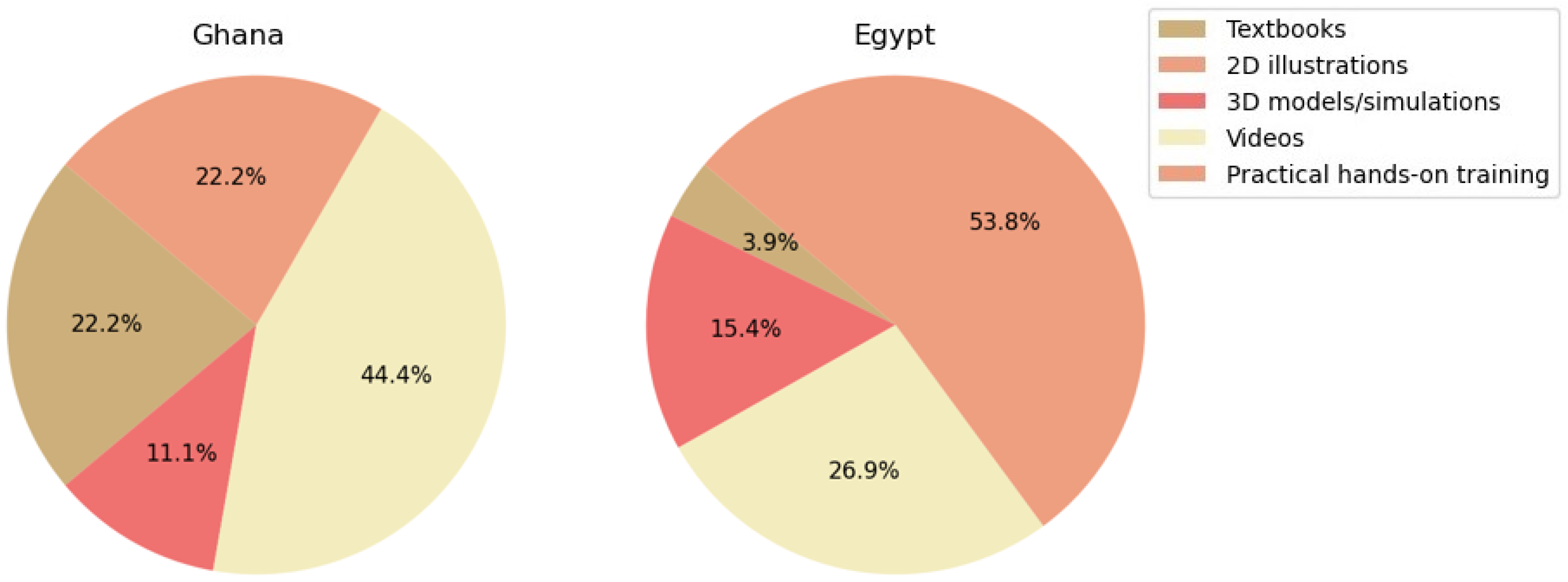
3.2. Questionnaire Survey
4. Discussion
4.1. Main Applications and Uses
4.1.1. Anatomy
4.1.2. Surgery
4.1.3. Human Interpersonal Behaviour
4.2. Benefits
4.3. Problems and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Reddy, B.; Thomas, S.; Karachiwala, B.; Sadhu, R.; Iyer, A.; Sen, G.; Mehrtash, H.; Tunçalp, Ö. A scoping review of the impact of organisational factors on providers and related interventions in LMICs: Implications for respectful maternity care. PLoS Glob. Public Health 2022, 21, e0001134. [Google Scholar] [CrossRef] [PubMed]
- Bailenson, J. Experience on Demand: What Virtual Reality Is, How It Works, and What It Can Do; W.W. Norton & Company: New York, NY, USA; London UK, 2018. [Google Scholar]
- McLachlan, J.C.; Bligh, J.; Bradley, P.; Searle, J. Teaching Anatomy without Cadavers. Med. Educ. 2004, 38, 418–424. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.; Botelho, F.; Pinkham, L.; Guadagno, E.; Poenaru, D. Technology-enhanced trauma training in low-resource settings: A scoping review and feasibility analysis of educational technologies. J. Pediatr. Surg. 2023, 58, 955–963. [Google Scholar] [CrossRef] [PubMed]
- Magi, C.E.; Bambi, S.; Iovino, P.; El Aoufy, K.; Amato, C.; Balestri, C.; Rasero, L.; Longobucco, Y. Virtual reality and augmented reality training in disaster medicine courses for students in nursing: A scoping review of adoptable tools. Behav. Sci. 2023, 13, 616. [Google Scholar] [CrossRef] [PubMed]
- Richardson, D.; Kinnear, B.; Hauer, K.; Turner, T.; Warm, E.; Hall, A.; Ross, S.; Thoma, B.; Van Melle, E. Growth mindset in competency-based medical education. Med. Teach. 2021, 43, 1–7. [Google Scholar] [CrossRef]
- McGaghie, W.C.; Issenberg, S.B.; Cohen, E.R.; Barsuk, J.H.; Wayne, D.B. Does Simulation-Based Medical Education With Deliberate Practice Yield Better Results Than Traditional Clinical Education? A Meta-Analytic Comparative Review of the Evidence. Acad. Med. 2011, 86, 706–711. [Google Scholar] [CrossRef]
- Higgins, M.; Madan, C.R.; Patel, R. Deliberate practice in simulation-based surgical skills training: A scoping review. J. Surg. Educ. 2021, 78, 1328–1339. [Google Scholar] [CrossRef]
- Brunzini, A.; Papetti, A.; Messi, D.; Germani, M. A comprehensive method to design and assess mixed reality simulations. Virtual Real. 2022, 26, 1257–1275. [Google Scholar] [CrossRef]
- Dinh, J.; Traylor, A.; Kilcullen, M.; Perez, J.; Schweissing, E.; Venkatesh, A.; Salas, E. Cross-Disciplinary Care: A Systematic Review on Teamwork Processes in Health Care. Small Group Res. 2019, 51, 104649641987200. [Google Scholar] [CrossRef]
- Khanal, P.; Vankipuram, A.; Ashby, A.; Vankipuram, M.; Gupta, A.; Drumm-Gurnee, D.; Josey, K.; Tinker, L.; Smith, M. Collaborative Virtual Reality Based Advanced Cardiac Life Support Training Simulator Using Virtual Reality Principles. J. Biomed. Inform. 2014, 51, 49–59. [Google Scholar] [CrossRef]
- Liaw, S.Y.; Ooi, S.W.; Rusli, K.D.B.; Lau, T.C.; Tam, W.W.S.; Chua, W.L. Nurse-Physician Communication Team Training in Virtual Reality Versus Live Simulations: Randomized Controlled Trial on Team Communication and Teamwork Attitudes. J. Med. Internet Res. 2020, 22, e17279. [Google Scholar] [CrossRef] [PubMed]
- Prasolova-Førland, E.; McCallum, S.; Estrada, J.G. Collaborative learning in VR for cross-disciplinary distributed student teams. In Proceedings of the 2021 IEEE Conference on virtual reality and 3D user interfaces abstracts and workshops (VRW), Virtual, 27 March–3 April 2021; pp. 320–325. [Google Scholar]
- Wang, X.; Song, G.; Ghannam, R. Enhancing Teamwork and Collaboration: A Systematic Review of Algorithm-Supported Pedagogical Methods. Educ. Sci. 2024, 14, 675. [Google Scholar] [CrossRef]
- Von Jan, U.; Noll, C.; Behrends, M.; Albrecht, U.V. mARble—Augmented Reality in Medical Education. Biomed. Eng./Biomed. Tech. 2012, 57, 67–70. [Google Scholar] [CrossRef]
- Barteit, S.; Lanfermann, L.; Bärnighausen, T.; Neuhann, F.; Beiersmann, C. Augmented, mixed, and virtual reality-based head-mounted devices for medical education: Systematic review. JMIR Serious Games 2021, 9, e29080. [Google Scholar] [CrossRef] [PubMed]
- Berman, N.B.; Durning, S.J.; Fischer, M.R.; Huwendiek, S.; Triola, M.M. The Role for Virtual Patients in the Future of Medical Education. Acad. Med. 2016, 91, 1217–1222. [Google Scholar] [CrossRef]
- Antel, R.; Abbasgholizadeh-Rahimi, S.; Guadagno, E.; Harley, J.M.; Poenaru, D. The use of artificial intelligence and virtual reality in doctor-patient risk communication: A scoping review. Patient Educ. Couns. 2022, 105, 3038–3050. [Google Scholar] [CrossRef]
- Talbot, T.B.; Sagae, K.; John, B.; Rizzo, A.A. Sorting Out the Virtual Patient: How to Exploit Artificial Intelligence, Game Technology and Sound Educational Practices to Create Engaging Role-Playing Simulations. Int. J. Gaming Comput.-Mediat. Simul. 2012, 4, 1–19. [Google Scholar] [CrossRef]
- Tzachor, A.; Sabri, S.; Richards, C.; Rajabifard, A.; Acuto, M. Potential and limitations of digital twins to achieve the Sustainable Development Goals. Nat. Sustain. 2022, 5, 1–8. [Google Scholar] [CrossRef]
- Pears, M.; Rochester, M.; Wadhwa, K.; Payne, S.R.; Konstantinidis, S.; Hanchanale, V.; Elmamoun, M.H.; Biyani, C.S.; Doherty, R. A Pilot Study Evaluating a Virtual Reality-Based Nontechnical Skills Training Application for Urology Trainees: Usability, Acceptability, and Impact. J. Surg. Educ. 2023, 80, 1836–1842. [Google Scholar] [CrossRef]
- Awori, J.; Friedman, S.D.; Howard, C.; Kronmal, R.; Buddhe, S. Comparative Effectiveness of Virtual Reality (VR) vs 3D Printed Models of Congenital Heart Disease in Resident and Nurse Practitioner Educational Experience. 3D Print. Med. 2023, 9, 2. [Google Scholar] [CrossRef]
- Parham, G.; Bing, E.G.; Cuevas, A.; Fisher, B.; Skinner, J.; Mwanahamuntu, M.; Sullivan, R. Creating a Low-Cost Virtual Reality Surgical Simulation to Increase Surgical Oncology Capacity and Capability. Ecancermedicalscience 2019, 13, 910. [Google Scholar] [CrossRef] [PubMed]
- McCullough, M.C.; Kulber, L.; Sammons, P.; Santos, P.; Kulber, D.A. Google Glass for Remote Surgical Tele-proctoring in Low- and Middle-income Countries: A Feasibility Study from Mozambique. Plast. Reconstr. Surg.-Glob. Open 2018, 6, e1999. [Google Scholar] [CrossRef] [PubMed]
- Rojas-Muñoz, E.; Cabrera, M.E.; Lin, C.; Andersen, D.; Popescu, V.; Anderson, K.; Zarzaur, B.L.; Mullis, B.; Wachs, J.P. The System for Telementoring with Augmented Reality (STAR): A Head-Mounted Display to Improve Surgical Coaching and Confidence in Remote Areas. Surgery 2020, 167, 724–731. [Google Scholar] [CrossRef] [PubMed]
- Hardon, S.F.; Kooijmans, A.; Horeman, R.; Van Der Elst, M.; Bloemendaal, A.L.A.; Horeman, T. Validation of the Portable Virtual Reality Training System for Robotic Surgery (PoLaRS): A Randomized Controlled Trial. Surg. Endosc. 2022, 36, 5282–5292. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Anastasiou, E.; Balafoutis, A.T.; Fountas, S. Applications of Extended Reality (XR) in Agriculture, Livestock Farming, and Aquaculture: A Review. Smart Agric. Technol. 2023, 3, 100105. [Google Scholar] [CrossRef]
- Eriksen, M.B.; Frandsen, T.F. The Impact of Patient, Intervention, Comparison, Outcome (PICO) as a Search Strategy Tool on Literature Search Quality: A Systematic Review. J. Med. Libr. Assoc. 2018, 106, 420–431. [Google Scholar] [CrossRef]
- Schiavenato, M.; Chu, F. PICO: What it is and what it is not. Nurse Educ. Pract. 2021, 56, 103194. [Google Scholar] [CrossRef]
- Mergen, M.; Meyerheim, M.; Graf, N. Towards Integrating Virtual Reality into Medical Curricula: A Single Center Student Survey. Educ. Sci. 2023, 13, 477. [Google Scholar] [CrossRef]
- Microsoft. Announcing Microsoft HoloLens Development Edition Open for Pre-Order, Shipping. 2016. Available online: https://blogs.windows.com/devices/2016/02/29/announcing-microsoft-hololens-development-edition-open-for-pre-order-shipping-march-30/ (accessed on 2 September 2024).
- The Guardian. Facebook Confirms Oculus Rift Virtual Reality Headset Will Ship in 2016. 2015. Available online: https://www.theguardian.com/technology/2015/may/06/facebook-oculus-rift-virtual-reality-2016 (accessed on 20 July 2024).
- Cuervo, E.; Chintalapudi, K.; Kotaru, M. Creating the perfect illusion: What will it take to create life-like virtual reality headsets? In Proceedings of the 19th International Workshop on Mobile Computing Systems & Applications, Tempe, AZ, USA, 12–13 February 2018; pp. 7–12. [Google Scholar]
- Taiwan Semiconductor Manufacturing Company (TSMC). 7 nm Technology. 2024. Available online: https://www.tsmc.com/english/dedicatedFoundry/technology/logic/l_7nm (accessed on 20 July 2024).
- Debes, A.J.; Aggarwal, R.; Balasundaram, I.; Jacobsen, M.B. A Tale of Two Trainers: Virtual Reality versus a Video Trainer for Acquisition of Basic Laparoscopic Skills. Am. J. Surg. 2010, 199, 840–845. [Google Scholar] [CrossRef]
- Wang, S.; Parsons, M.; Stone-McLean, J.; Rogers, P.; Boyd, S.; Hoover, K.; Meruvia-Pastor, O.; Gong, M.; Smith, A. Augmented Reality as a Telemedicine Platform for Remote Procedural Training. Sensors 2017, 17, 2294. [Google Scholar] [CrossRef] [PubMed]
- Greenfield, M.J.; Luck, J.; Billingsley, M.L.; Heyes, R.; Smith, O.J.; Mosahebi, A.; Khoussa, A.; Abu-Sittah, G.; Hachach-Haram, N. Demonstration of the Effectiveness of Augmented Reality Telesurgery in Complex Hand Reconstruction in Gaza. Plast. Reconstr. Surg.-Glob. Open 2018, 6, e1708. [Google Scholar] [CrossRef] [PubMed]
- Bing, E.G.; Parham, G.P.; Cuevas, A.; Fisher, B.; Skinner, J.; Mwanahamuntu, M.; Sullivan, R. Using low-cost virtual reality simulation to build surgical capacity for cervical cancer treatment. J. Glob. Oncol. 2019, 5, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Alvarez-Lopez, F.; Maina, M.F.; Arango, F.; Saigí-Rubió, F. Use of a Low-Cost Portable 3D Virtual Reality Simulator for Psychomotor Skill Training in Minimally Invasive Surgery: Task Metrics and Score Validity. JMIR Serious Games 2020, 8, e19723. [Google Scholar] [CrossRef] [PubMed]
- Da Cruz, M.M.A.; Ricci-Vitor, A.L.; Borges, G.L.B.; Da Silva, P.F.; Turri-Silva, N.; Takahashi, C.; Grace, S.L.; Vanderlei, L.C.M. A Randomized, Controlled, Crossover Trial of Virtual Reality in Maintenance Cardiovascular Rehabilitation in a Low-Resource Setting: Impact on Adherence, Motivation, and Engagement. Phys. Ther. 2021, 101, pzab071. [Google Scholar] [CrossRef]
- Bala, L.; Kinross, J.; Martin, G.; Koizia, L.J.; Kooner, A.S.; Shimshon, G.J.; Hurkxkens, T.J.; Pratt, P.J.; Sam, A.H. A Remote Access Mixed Reality Teaching Ward Round. Clin. Teach. 2021, 18, 386–390. [Google Scholar] [CrossRef]
- Umoren, R.; Bucher, S.; Hippe, D.S.; Ezenwa, B.N.; Fajolu, I.B.; Okwako, F.M.; Feltner, J.; Nafula, M.; Musale, A.; Olawuyi, O.A.; et al. eHBB: A Randomised Controlled Trial of Virtual Reality or Video for Neonatal Resuscitation Refresher Training in Healthcare Workers in Resource-Scarce Settings. BMJ Open 2021, 11, e048506. [Google Scholar] [CrossRef]
- Bing, E.G.; Brown, M.L.; Cuevas, A.; Sullivan, R.; Parham, G.P. User experience with low-cost virtual reality cancer surgery simulation in an African setting. JCO Glob. Oncol. 2021, 7, 435–442. [Google Scholar] [CrossRef]
- Ezenwa, B.N.; Umoren, R.; Fajolu, I.B.; Hippe, D.S.; Bucher, S.; Purkayastha, S.; Okwako, F.; Esamai, F.; Feltner, J.B.; Olawuyi, O.; et al. Using Mobile Virtual Reality Simulation to Prepare for In-Person Helping Babies Breathe Training: Secondary Analysis of a Randomized Controlled Trial (the eHBB/mHBS Trial). JMIR Med. Educ. 2022, 8, e37297. [Google Scholar] [CrossRef]
- Tapiala, J.; Iso-Mustajärvi, M.; Timonen, T.; Vrzáková, H.; Dietz, A. Impact of Virtual Reality Training on Mastoidectomy Performance: A Prospective Randomised Study. Eur. Arch. Oto-Rhino 2024, 281, 701–710. [Google Scholar] [CrossRef]
- Samantaray, A.; Kaur, T.; Singhal, S.; Gandhi, T.K. Remote Assistance in Cervical Cancer Screening Using Microsoft Hololens 2: An Augmented-Reality Based Approach. In Proceedings of the 2023 International Conference on Recent Advances in Electrical, Electronics & Digital Healthcare Technologies (REEDCON), New Delhi, India, 1–3 May 2023; pp. 123–126. [Google Scholar] [CrossRef]
- Singh, K.; Gaur, U.; Hall, K.; Mascoll, K.; Cohall, D.; Majumder, M.A. Teaching anatomy and dissection in an era of social distancing and remote learning. Adv. Hum. Biol. 2020, 10, 90. [Google Scholar] [CrossRef]
- Thomas, R.G.; John, N.W.; Delieu, J. Augmented Reality for Anatomical Education. J. Vis. Commun. Med. 2010, 33, 6–15. [Google Scholar] [CrossRef] [PubMed]
- Carroll, M.A.; McKenzie, A.; Tracy-Bee, M. Movement System Theory and Anatomical Competence: Threshold Concepts for Physical Therapist Anatomy Education. Anat. Sci. Educ. 2022, 15, 420–430. [Google Scholar] [CrossRef] [PubMed]
- Garg, A.X.; Norman, G.R.; Norman, G.; Sperotable, L. How Medical Students Learn Spatial Anatomy. Lancet 2001, 357, 363–364. [Google Scholar] [CrossRef] [PubMed]
- Kong, X.; Nie, L.; Zhang, H.; Wang, Z.; Ye, Q.; Tang, L.; Li, J.; Huang, W. Do Three-dimensional Visualization and Three-dimensional Printing Improve Hepatic Segment Anatomy Teaching? A Randomized Controlled Study. J. Surg. Educ. 2016, 73, 264–269. [Google Scholar] [CrossRef]
- Zhao, J.; Xu, X.; Jiang, H.; Ding, Y. The effectiveness of virtual reality-based technology on anatomy teaching: A meta-analysis of randomized controlled studies. BMC Med. Educ. 2020, 20, 127. [Google Scholar] [CrossRef]
- Stepan, K.; Zeiger, J.; Hanchuk, S.; Del Signore, A.; Shrivastava, R.; Govindaraj, S.; Iloreta, A. Immersive Virtual Reality as a Teaching Tool for Neuroanatomy: Immersive VR as a Neuroanatomy Teaching Tool. Int. Forum Allergy Rhinol. 2017, 7, 1006–1013. [Google Scholar] [CrossRef]
- Tene, T.; Vique López, D.F.; Valverde Aguirre, P.E.; Orna Puente, L.M.; Vacacela Gomez, C. Virtual reality and augmented reality in medical education: An umbrella review. Front. Digit. Health 2024, 6, 1365345. [Google Scholar] [CrossRef]
- Vozenilek, J. See One, Do One, Teach One: Advanced Technology in Medical Education. Acad. Emerg. Med. 2004, 11, 1149–1154. [Google Scholar] [CrossRef]
- Polavarapu, H.V.; Kulaylat, A.N.; Sun, S.; Hamed, O.H. 100 Years of Surgical Education: The Past, Present, and Future. Bull. Am. Coll. Surg. 2013, 98, 22–27. [Google Scholar]
- Higgins, M.; Madan, C.; Patel, R. Development and decay of procedural skills in surgery: A systematic review of the effectiveness of simulated-based medical education interventions. Surg. 2020, 19, e67–e77. [Google Scholar] [CrossRef] [PubMed]
- Berthold, D.P.; Muench, L.N.; Rupp, M.C.; Siebenlist, S.; Cote, M.P.; Mazzocca, A.D.; Quindlen, K. Head-Mounted Display Virtual Reality Is Effective in Orthopaedic Training: A Systematic Review. Arthrosc. Sport. Med. Rehabil. 2022, 4, e1843–e1849. [Google Scholar] [CrossRef] [PubMed]
- Taba, J.V.; Cortez, V.S.; Moraes, W.A.; Iuamoto, L.R.; Hsing, W.T.; Suzuki, M.O.; do Nascimento, F.S.; Pipek, L.Z.; de Mattos, V.C.; D’Albuquerque, E.C.; et al. The development of laparoscopic skills using virtual reality simulations: A systematic review. PLoS ONE 2021, 16, e0252609. [Google Scholar] [CrossRef] [PubMed]
- Logishetty, K.; Rudran, B.; Cobb, J.P. Virtual Reality Training Improves Trainee Performance in Total Hip Arthroplasty: A Randomized Controlled Trial. Bone Jt. J. 2019, 101-B, 1585–1592. [Google Scholar] [CrossRef]
- Verhey, J.; Haglin, J.; Verhey, E.; Hartigan, D. Virtual, augmented, and mixed reality applications in Orthopedic surgery. Int. J. Med. Robot. Comput. Assist. Surg. 2019, 16, e2067. [Google Scholar] [CrossRef] [PubMed]
- Leitritz, M.A.; Ziemssen, F.; Suesskind, D.; Partsch, M.; Voykov, B.; Bartz-Schmidt, K.U.; Szurman, G.B. Critical evaluation of the usability of augmented reality ophthalmoscopy for the training of inexperienced examiners. Retina 2014, 34, 785–791. [Google Scholar] [CrossRef]
- Muñoz, E.G.; Fabregat, R.; Bacca-Acosta, J.; Duque-Méndez, N.; Avila-Garzon, C. Augmented reality, virtual reality, and game technologies in ophthalmology training. Information 2022, 13, 222. [Google Scholar] [CrossRef]
- Yedidia, M.J. Effect of Communications Training on Medical Student Performance. JAMA 2003, 290, 1157. [Google Scholar] [CrossRef]
- Tan, Y.; Xu, W.; Li, S.; Chen, K. Augmented and Virtual Reality (AR/VR) for Education and Training in the AEC Industry: A Systematic Review of Research and Applications. Buildings 2022, 12, 1529. [Google Scholar] [CrossRef]
- Triola, M.; Feldman, H.; Kalet, A.L.; Zabar, S.; Kachur, E.K.; Gillespie, C.; Anderson, M.; Griesser, C.; Lipkin, M. A Randomized Trial of Teaching Clinical Skills Using Virtual and Live Standardized Patients. J. Gen. Intern. Med. 2006, 21, 424–429. [Google Scholar] [CrossRef]
- Real, F.J.; DeBlasio, D.; Beck, A.F.; Ollberding, N.J.; Davis, D.; Cruse, B.; Samaan, Z.; McLinden, D.; Klein, M.D. A Virtual Reality Curriculum for Pediatric Residents Decreases Rates of Influenza Vaccine Refusal. Acad. Pediatr. 2017, 17, 431–435. [Google Scholar] [CrossRef] [PubMed]
- Stefan, H.; Mortimer, M.; Horan, B. Evaluating the effectiveness of virtual reality for safety-relevant training: A systematic review. Virtual Real. 2023, 27, 2839–2869. [Google Scholar] [CrossRef]
- Prineas, S.; Mosier, K.; Mirko, C.; Guicciardi, S. Non-technical skills in healthcare. In Textbook of Patient Safety and Clinical Risk Management; Springer: Cham, Switzerland, 2021; pp. 413–434. [Google Scholar]
- McCloy, R.F.; Stone, R. Science, Medicine, and the Future. Virtual Reality in Surgery. BMJ 2001, 323, 912–915. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.; Egbue, O.; Palkie, B.; Madden, J. Active learning: Engaging students to maximize learning in an online course. Electron. J. E-Learn. 2017, 15, 107–115. [Google Scholar]
- Mathew, P.S.; Pillai, A.S. Role of immersive (XR) technologies in improving healthcare competencies: A review. Virtual and Augmented Reality in Education, Art, and Museums; IGI: Hershey, PA, USA, 2020; pp. 23–46. [Google Scholar]
- Herur-Raman, A.; Almeida, N.D.; Greenleaf, W.; Williams, D.; Karshenas, A.; Sherman, J.H. Next-Generation Simulation—Integrating Extended Reality Technology Into Medical Education. Front. Virtual Real. 2021, 2, 693399. [Google Scholar] [CrossRef]
- Moro, C.; Štromberga, Z.; Raikos, A.; Stirling, A. The Effectiveness of Virtual and Augmented Reality in Health Sciences and Medical Anatomy. Anat. Sci. Educ. 2017, 10, 549–559. [Google Scholar] [CrossRef]
- Curran, V.R.; Xu, X.; Aydin, M.Y.; Meruvia-Pastor, O. Use of extended reality in medical education: An integrative review. Med. Sci. Educ. 2023, 33, 275–286. [Google Scholar] [CrossRef]
- Saredakis, D.; Szpak, A.; Birckhead, B.; Keage, H.A.; Rizzo, A.; Loetscher, T. Factors associated with virtual reality sickness in head-mounted displays: A systematic review and meta-analysis. Front. Hum. Neurosci. 2020, 14, 96. [Google Scholar] [CrossRef]
- Sandrone, S. Medical education in the metaverse. Nat. Med. 2022, 28, 2456–2457. [Google Scholar] [CrossRef]
- Takata, R.; Kanehira, M.; Kato, Y.; Matsuura, T.; Kato, R.; Maekawa, S.; Obara, W. Improvement of three-dimensional motion sickness using a virtual reality simulator for robot-assisted surgery in undergraduate medical students: A prospective observational study. BMC Med. Educ. 2021, 21, 498. [Google Scholar] [CrossRef]
- Wersényi, G. Perception Accuracy of a Multi-Channel Tactile Feedback System for Assistive Technology. Sensors 2022, 22, 8962. [Google Scholar] [CrossRef] [PubMed]
- Sacchetti, S.; McGlone, F.; Cazzato, V.; Mirams, L. The off-line effect of affective touch on multisensory integration and tactile perceptual accuracy during the somatic signal detection task. PLoS ONE 2021, 16, e0261060. [Google Scholar] [CrossRef] [PubMed]
- Syahry, A.; Basuki, D.K.; Sukaridhoto, S.; Budiarti, R.P.N.; Hanifati, K.; Muntahir, I. Implementation of Augmented Reality in Medical Education. In Proceedings of the 2022 International Electronics Symposium (IES), Surabaya, Indonesia, 9–11 August 2022; pp. 684–690. [Google Scholar]
- El-Araby, N.; Kocemba, J.; Dufeau, D. Limitations of Visualization Technology and Virtual Instruction in Medical Education. FASEB J. 2021, 35. [Google Scholar] [CrossRef]
- Celebi, K.C.; Bailey, S.K.; Burns, M.W.; Bansal, K. Is virtual reality streaming ready for remote medical education? measuring latency of stereoscopic VR for telementoring. In Proceedings of the Human Factors and Ergonomics Society Annual Meeting, Baltimore, MD, USA, 3–8 October 2021; Volume 65, pp. 757–761. [Google Scholar]
- Xu, X.; Mangina, E.; Campbell, A.G. HMD-based virtual and augmented reality in medical education: A systematic review. Front. Virtual Real. 2021, 2, 692103. [Google Scholar] [CrossRef]
- Bracq, M.S.; Michinov, E.; Jannin, P. Virtual reality simulation in nontechnical skills training for healthcare professionals: A systematic review. Simul. Healthc. 2019, 14, 188–194. [Google Scholar] [CrossRef]
- Birkheim, S.L.; Calogiuri, G.; Martinsen, R. Advancing immersive virtual reality-based simulation practices: Developing an evidence-based and theory-driven pedagogical framework for VR-based simulations of non-technical skills among healthcare professionals. Interact. Learn. Environ. 2023, 1–13. [Google Scholar] [CrossRef]
- da Cruz Torquato, M.; Menezes, J.M.; Belchior, G.; Mazzotti, F.P.; Bittar, J.S.; Dos Santos, G.G.R.; Ruiz, T.M.; de Oliveira Pereira, W.; Paes, A.T. Virtual reality as a complementary learning tool in anatomy education for medical students. Med. Sci. Educ. 2023, 33, 507–516. [Google Scholar] [CrossRef]







| Concepts | Immersive Technology | Medical Discipline | Training Methods | Resource-Limited |
|---|---|---|---|---|
| Keywords | AR, VR, MR, XR | Anatomy, Surgery, Physiology, Pathology, Pharmacology, Biochemistry | Training, Education, Simulation, Telementoring | LMICs, Low-and-middle-income areas, Rural-and-remote, Resource-limited |
| Framework | Description | Inclusion | Exclusion |
|---|---|---|---|
| Population | Medical staff in resource-limited areas | Medical interns, medical students, surgeons, nurses | No resource- limited situations |
| Intervention | Medical training using immersive technology devices | AR, VR, MR, XR | Non-immersive technology |
| Comparison | The comparison of the effectiveness | Only the evaluation of the immersive technology devices, comparisons | No evaluation of the immersive technology devices |
| Outcome | Negative or positive attitudes | New XR system, evaluation | No outcome |
| No. | Year | Location | XR | Device | Application | Discipline | Sample Size | Effect-Iveness | Evaluation Type | Reference |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2017 | Canada * | AR | HoloLens | Medical imaging | Non-specific | 24 | + | Questionnaire | [37] |
| 2 | 2018 | Zambia | VR | Oculus Rift | Surgery | General surgery | 10 | + | Skills tests, Observation | [23] |
| 3 | 2018 | Gaza | AR | N/A | Surgery | General surgery | N/A | + | N/A | [38] |
| 4 | 2018 | Mozam-bique | AR | Google Glass | Surgery | General surgery | 12 | + | Questionnaire | [24] |
| 5 | 2019 | US * | AR | STAR (Hololens) | Surgery | General surgery | 20 | + | Skills tests, self-assessment | [25] |
| 6 | 2019 | Zambia | VR | Oculus Rift | Surgery | General surgery | 10 | + | Skills tests | [39] |
| 7 | 2020 | Colombia | VR | SIMISGEST-VR | Surgery | Minimally invasive surgery *** | 148 | + | Skills tests | [40] |
| 8 | 2020 | Brazil | VR | N/A | Recovery | Cardiology | 61 | - | Observation | [41] |
| 9 | 2021 | UK * | AR | HoloLens 2 | Ward round | Non-specific | 11 | + | Questionnaire | [42] |
| 10 | 2021 | Nigeria, Kenya | VR | N/A | Other | Neonatology | 274 | + | Skills tests, Knowledge tests | [43] |
| 11 | 2021 | Zambia | VR | Oculus Rift | Surgery | General surgery | 11 | + | Semistructured interviews | [44] |
| 12 | 2022 | Nigeria, Kenya | VR | N/A | Other | Neonatology | 179 | + | Skills tests | [45] |
| 13 | 2022 | The Netherlands * | VR | PoLaRS | Surgery | Laparoscopy ** | 38 | + | Questionnaire, skills tests | [26] |
| 14 | 2023 | UK * | VR | N/A | Human interpersonal behaviour | Urology | 32 | + | Questionnaire | [21] |
| 15 | 2023 | USA * | AR, VR | Zspace | Anatomy | Cardiology | 27 | + | Questionnaire | [22] |
| 16 | 2023 | Finland * | VR | HTC Vive Pro | Surgery | Otolaryngology | 30 | + | Skills tests, self-assessment | [46] |
| 17 | 2023 | India | AR | Microsoft Hololens 2 | Surgery | Oncology | N/A | + | N/A | [47] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, X.; Elnagar, D.; Song, G.; Ghannam, R. Advancing Medical Education Using Virtual and Augmented Reality in Low- and Middle-Income Countries: A Systematic and Critical Review. Virtual Worlds 2024, 3, 384-403. https://doi.org/10.3390/virtualworlds3030021
Li X, Elnagar D, Song G, Ghannam R. Advancing Medical Education Using Virtual and Augmented Reality in Low- and Middle-Income Countries: A Systematic and Critical Review. Virtual Worlds. 2024; 3(3):384-403. https://doi.org/10.3390/virtualworlds3030021
Chicago/Turabian StyleLi, Xi, Dalia Elnagar, Ge Song, and Rami Ghannam. 2024. "Advancing Medical Education Using Virtual and Augmented Reality in Low- and Middle-Income Countries: A Systematic and Critical Review" Virtual Worlds 3, no. 3: 384-403. https://doi.org/10.3390/virtualworlds3030021
APA StyleLi, X., Elnagar, D., Song, G., & Ghannam, R. (2024). Advancing Medical Education Using Virtual and Augmented Reality in Low- and Middle-Income Countries: A Systematic and Critical Review. Virtual Worlds, 3(3), 384-403. https://doi.org/10.3390/virtualworlds3030021






