Abstract
This review critically examines the integration of Virtual Reality (VR) and Augmented Reality (AR) in medical training across Low- and Middle-Income Countries (LMICs), offering a novel perspective by combining quantitative analysis with qualitative insights from medical students in Egypt and Ghana. Through a systematic review process, 17 peer-reviewed studies published between 2010 and 2023 were analysed. Altogether, these studies involved a total of 887 participants. The analysis reveals a growing interest in VR and AR applications for medical training in LMICs with a peak in published articles in 2023, indicating an expanding research landscape. A unique contribution of this review is the integration of feedback from 35 medical students assessed through questionnaires, which demonstrates the perceived effectiveness of immersive technologies over traditional 2D illustrations in understanding complex medical concepts. Key findings highlight that VR and AR technologies in medical training within LMICs predominantly focus on surgical skills. The majority of studies focus on enhancing surgical training, particularly general surgery. This emphasis reflects the technology’s strong alignment with the needs of LMICs, where surgical skills training is often a priority. Despite the promising applications and expanding interest in VR and AR, significant challenges such as accessibility and device limitations remain, demonstrating the need for ongoing research and integration with traditional methods to fully leverage these technologies for effective medical education. Therefore, this review provides a comprehensive analysis of existing VR and AR applications, their evaluation methodologies, and student perspectives to address educational challenges and enhance healthcare outcomes in LMICs.
1. Introduction
Today, the world of medicine is facing many challenges, ranging from the shortages of health workers in Low- and Middle-Income Countries (LMICs) to the urgent need for specialised training [1]. To solve these problems, new tools like Virtual Reality (VR) and Augmented Reality (AR) are emerging as pivotal tools, particularly since VR can be used for anything DICE (Dangerous, Impossible, Counterproductive or Expensive) [2].
Historically, medical education has been a blend of theoretical knowledge and practical exposure. Cadavers, for instance, have been the cornerstone of anatomy teaching for centuries. However, not only are they expensive and ethically challenging but their availability is also limited [3,4]. Therefore, traditional medical teaching methods, although time-tested, present financial, ethical, and logistical challenges that, in today’s fast-paced and ever-evolving medical landscape, often prove limiting. However, with VR and AR, medical students can practise in a computer-generated environment, which means they can try things many times without any real-world risks [5].
The essence of medical training is rooted in practice [6]. It is about making decisions in real time, handling stress, and repeatedly engaging in complex procedures until they become second nature. In comparison to traditional clinical education, deliberate practice in simulation-based medical education has been proven to offer more significant benefits [7,8]. This repetitive and immersive practice is where VR, with its highly realistic simulations, demonstrates significant potential. Learners have the opportunity to engage in realistic scenarios without the fear of adverse effects on actual patients [9].
Moreover, medicine is an inherently collaborative discipline [10]. Whether it is nurses and doctors working in teams during operations or different departments discussing complicated cases, no medical professional works in isolation. VR can help train the team members to maintain good collaboration and communication skills in emergency situations [11,12]. For example, a student in Egypt may be able to practise a procedure with a student in India while both are being guided by an experienced professor from the UK—all of them brought together in a virtual environment. This demonstrates the transformative potential of VR technology in enhancing teamwork and collaboration without the constraints and costs of traditional travel or logistics [13,14]. In fact, removing such geographic boundaries promises new co-learning opportunities as well as the integration of diverse cultural insights and clinical experiences for learners.
Another benefit of VR is that it can offer the same training experience to everyone, everywhere. With VR, every scenario can be controlled, replicated, and assessed uniformly, ensuring that learners receive standardised and consistent quality education [15,16]. Furthermore, integrating Artificial Intelligence (AI) into these virtual platforms can provide in-depth performance analytics, tailor scenarios to individual learner needs, and make virtual patient [17,18] interactions more realistic. Combining the concepts of standardised medical education and virtual patients is called virtual standardised patients (VSPs), which can make learning more personal and realistic without losing consistency and credibility [19]. This dynamic synergy of VR and AI can make learning more personal and realistic.
In an effort to achieve the Sustainable Development Goals (SDGs) by 2030, particularly goal 3C, which stresses the enhancement of the health workforce in income-limited countries, digital technologies such as VR can help achieve this [20]. With their versatility, they can mirror varied training needs, ensuring that health professionals are equipped with a comprehensive skill set, from diagnostic skills to crucial communication abilities.
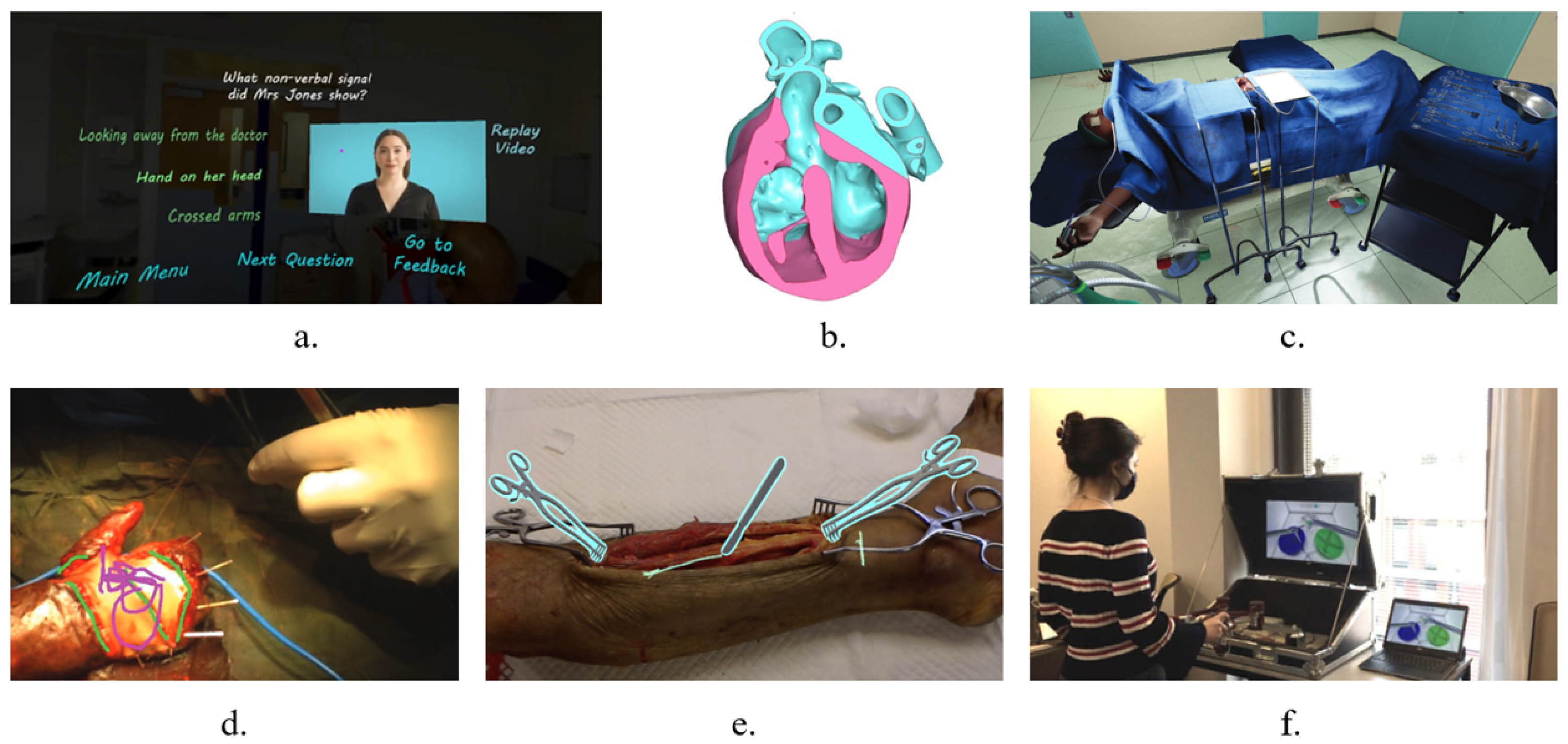
Some studies in LMICs have tried integrating extended reality (XR) technology into medical training, including the following fields: anatomy, surgery and human interpersonal behaviour (as shown in Figure 1). These applications seem to help increase the technical or non-technical skills of medical practitioners while further developing the medical career in LMICs. However, there are few medical applications of VR in LMICs. Also, the current research is still in the initial stage and lacks a systematic and critical literature review to elucidate the medical needs of LMICs.
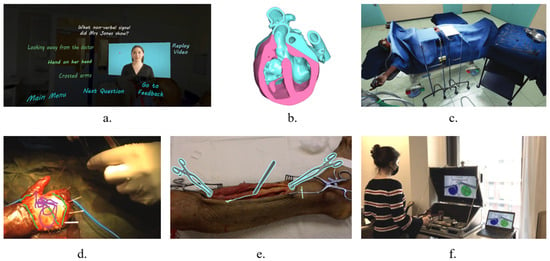
Figure 1.
Snapshots of current VR and AR applications in LMICs. (a) Human interpersonal behaviour: Non-technical skills training by reflection questions (reproduced with permission [21]. Copyright 2023, Elsevier). (b) Anatomy: Tetralogy of Fallot Colour VR model of the heart (reproduced with permission [22]. Copyright 2023, Springer). (c) Surgery: View of virtual operating theatre (reproduced with permission [23]. Copyright 2019, ecancer Global Foundation). (d) Telementoring: Remote annotate images in surgeon’s visual field (reproduced with permission [24]. Copyright 2018, Wolters Kluwer Health). (e) Augmented Reality 3D annotations (reproduced with permission [25]. Copyright 2020, Elsevier). (f) VR system for laparoscopic surgery training (reproduced with permission [26]. Copyright 2021, Springer).
This paper, therefore, seeks to comprehensively review the literature on the use of VR and AR in medical education and training in Low- and Middle-Income Countries, and to explore the real needs of LMICs through questionnaires. By examining their merits, understanding their limitations, and projecting their potential, we aim to provide a holistic overview of their role in shaping the future of medical education in these regions. To achieve these goals, several research questions should be addressed, as follows:
- RQ1
- What medical disciplines in training do immersive technology currently apply to?
- RQ2
- Is it necessary to use VR and AR in LMICs for medical education?
- RQ3
- What evaluation methods are used to measure the effectiveness of VR and AR for medical training in LMICs?
- RQ4
- Which medical disciplines in LMICs require immersive technology the most?
- RQ5
- What is the transformative potential of VR and AR to improve medical education?
2. Methodology
In this section, we demonstrate the research methodology used to explore the potential of Virtual Reality (VR) and Augmented Reality (AR) for medical training in Low- and Middle-Income Countries (LMICs). We use two complementary approaches: (A) A comprehensive systematic review and analysis of existing research to understand how VR and AR is used for medical training in LMIC settings. This will help answer RQ1–RQ4. (B) A focused survey is used, targeting medical students in Egypt and Ghana, which will gather data on their experiences and perspectives regarding VR and AR applications for medical training.
2.1. Literature Review
The literature review was based on the theory of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [27] and this study adhered to the guidelines outlined in the PRISMA-Checklist (see Supplementary Materials). The risks of bias were reduced by following a rigorous and transparent review protocol. The review protocol was not registered. It included four parts: (1) search strategy and selection criteria, (2) inclusion and exclusion criteria, (3) manual screening, and (4) review results.
2.1.1. Search Strategy and Selection Criteria
The reviews identified in this study were searched through the following main databases: IEEE Xplore Digital Library, University Digital Library, PubMed, ScienceDirect, and Scopus. The publications were only included from 1 January 2010, to 31 December 2023, as the increased use of VR and AR began in the early 2010s [28]. To ensure coverage of all relevant literature for this study, keywords used for search were classified into the four concepts of immersive technology, medical discipline, training methods, and resource-limited (shown in Table 1). The keywords were used alone or in combination. To accurately find the relevant literature about the application of VR and AR in medical training, an advanced search was used in this step.

Table 1.
Search terms used in the systematic review.
2.1.2. Inclusion and Exclusion Criteria
The theory of population, intervention, comparison, and outcome (PICO) [29] was changed [30] slightly to manage the inclusion criteria and exclusion criteria of this study as shown in Table 2. In addition, literature reviews, non-English literature, and literature not available in full text online were excluded.

Table 2.
PICO framework of the systematic review.
2.1.3. Manual Screening
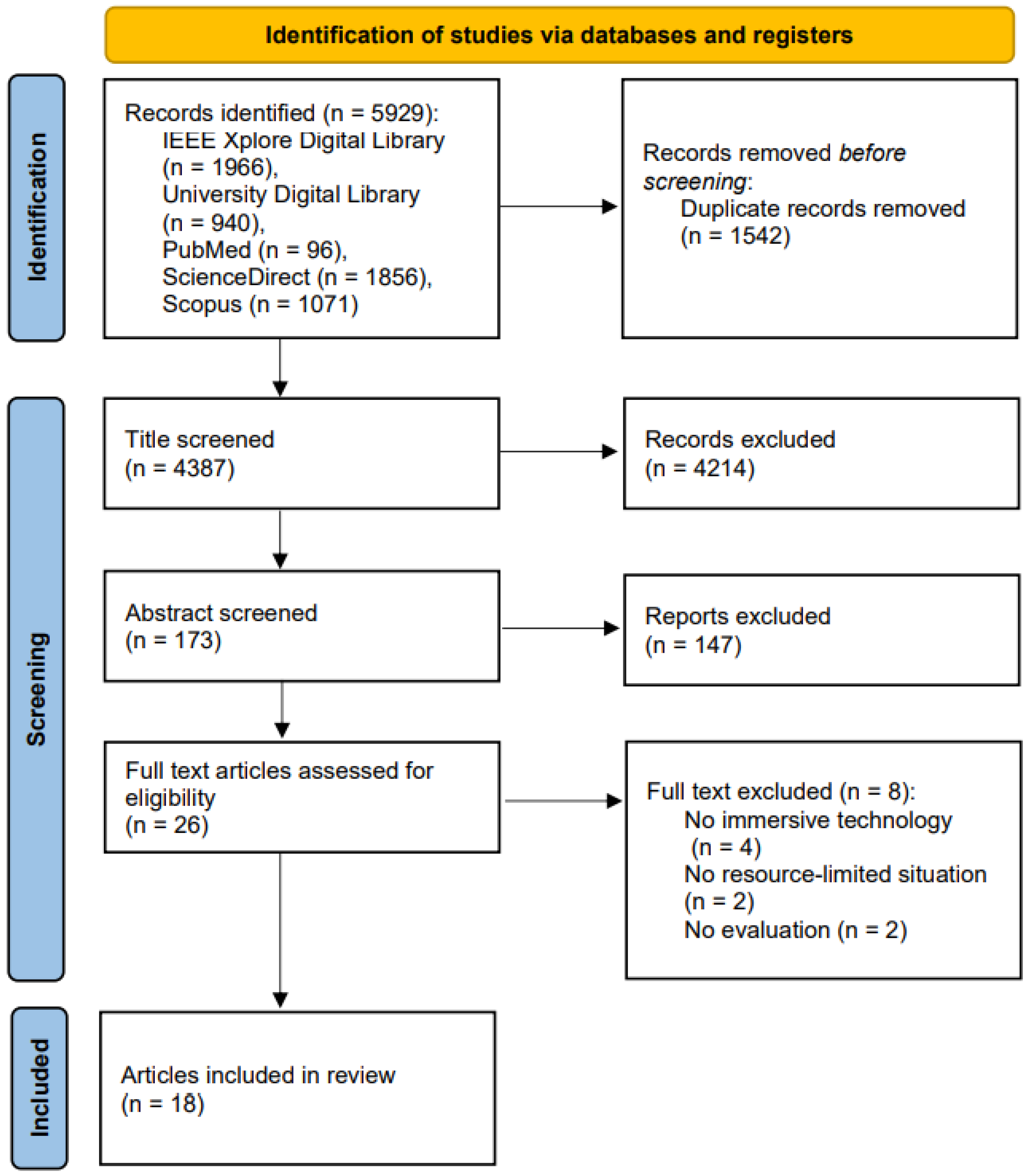
The criteria for inclusion and exclusion served as a reference for manual screening. The articles found in the databases were further screened according to the title and abstract. The full-text articles were assessed in the next step to exclude irrelevant articles and the same articles from different databases. In addition, some literature might be identified in the articles’ reference lists. The overall screening process was produced as a PRISMA flowchart shown in Figure 2.
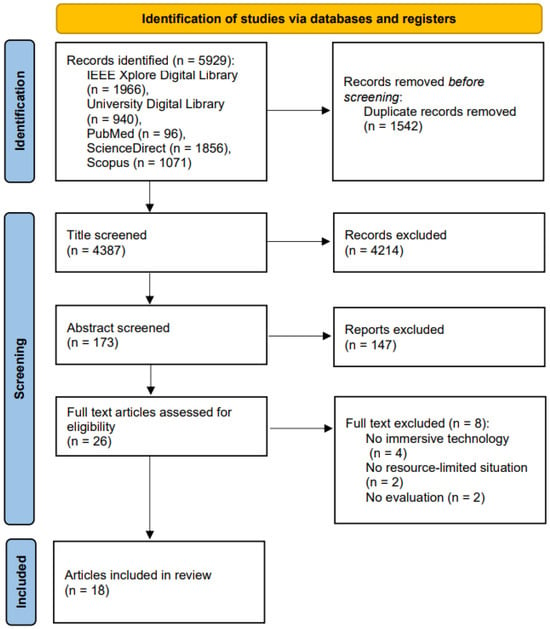
Figure 2.
PRISMA flowchart [27] for systematic reviews.
2.2. Questionnaire Survey
To answer RQ4, we conducted a questionnaire survey to hear from more authentic voices from LMICs. The survey focused on the expectations for the use of immersive technology tools, such as VR and AR. It was given to two student groups: Egyptian medical students from New Giza University and Ghanaian medical students from Kwame Nkrumah University of Science and Technology since these students would be the future main medical force in LMICs. Their views would have a significant impact on 3D virtualisation in local medical education.
To develop the questionnaire for this review, we referred to the existing literature and research methods. The study by Marvin Mergen and colleagues [31] on integrating Virtual Reality into medical curricula provides a comprehensive survey structure that includes demographic data, prior VR experience, and expectations regarding the inclusion of VR in medical training. This framework helped us design questions that assess the target group’s attitudes and needs regarding immersive technology. The questionnaire was divided into three sections: (1) Background information: This section included the respondents’ year of study, specialty, and learning experience. (2) Core questions: This section involved specific views and expectations on the use of VR and AR technologies in different medical disciplines. For example, questions were asked about the perceived benefits of using VR in anatomy or surgical training. (3) Concluding questions: This section covered overall opinions and future expectations for the use of these technologies, such as the willingness to adopt VR and AR in daily medical practice and the anticipated challenges.
A total of 26 Egyptian medical students and 9 Ghanaian medical students participated in this survey, all of whom had been studying for 2–5 years, which ensured that they had a certain degree of medical learning experience rather than just being beginners.
3. Results and Analysis
This section includes the presentation and analysis of the results of the identified literature and the questionnaire survey. The research questions serve as a framework for this section.
3.1. Literature Review
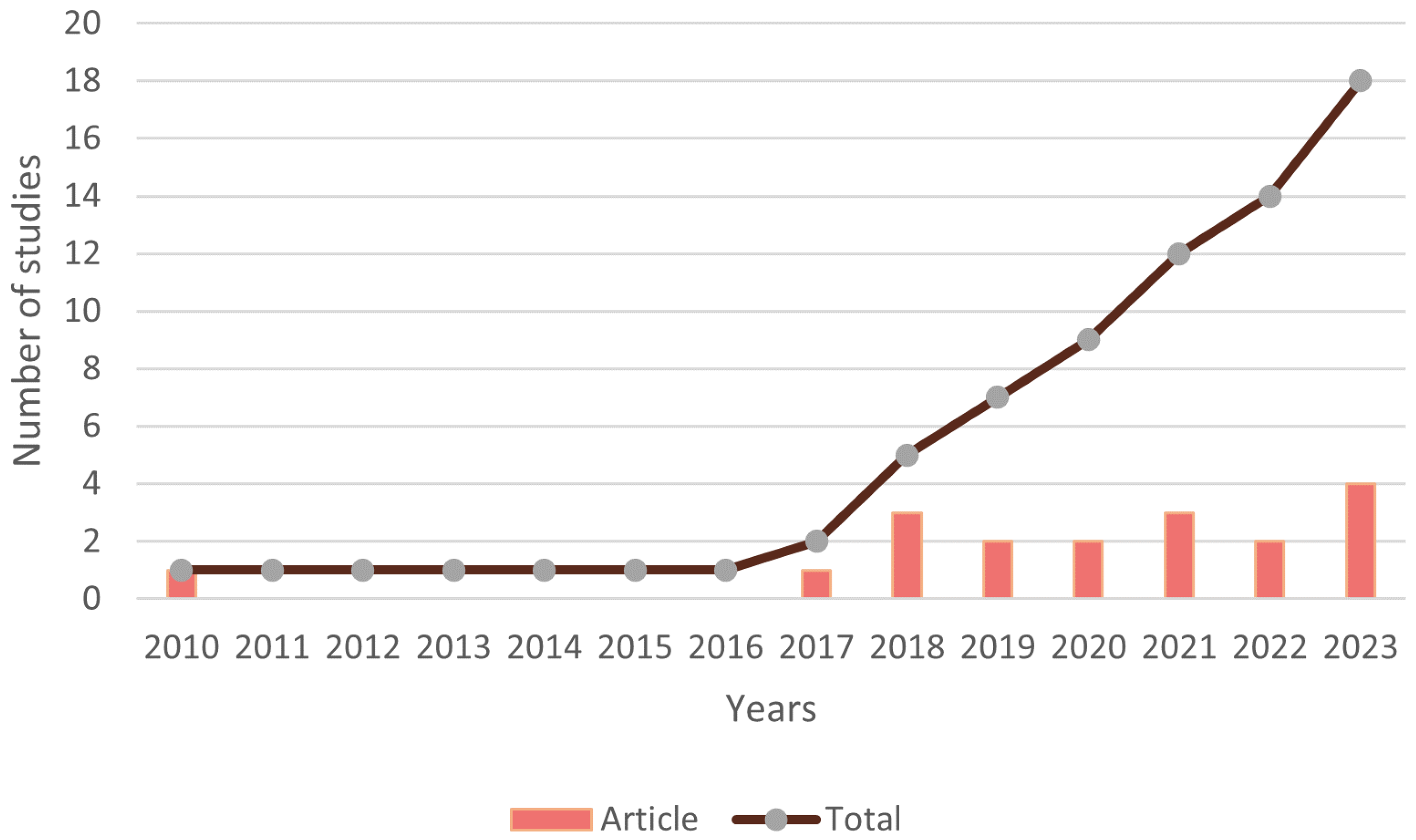
Following adherence to our inclusion and exclusion criteria, a total of 18 articles were shortlisted after screening (as shown in Figure 2). In fact, there has been a significant increase in the number of publications in this domain since 2017 as evidenced by Figure 3. This trend coincides with the major consumer releases of affordable VR/AR devices in 2016, such as the Oculus Rift, Microsoft HoloLens, and HTC Vive, along with the increasing accessibility of mobile technology [32,33]. Of course, this progress has been fuelled by the continuous increase in GPU computational power over the years. GPU computational power in Gigaflops (GFlops) has been steadily rising since 2010, driven by advancements in nanofabrication process technology, which progressed from 40 nm to 16 nm in 2016 [34]. This trend continues with the current 3 nm process technology [35], promising to produce life-like VR experiences. As the cost of immersive technology decreases, it becomes more accessible to institutions and individuals in LMICs. This lowered barrier to entry enables medical training programs in these regions to consider VR and AR as viable options.
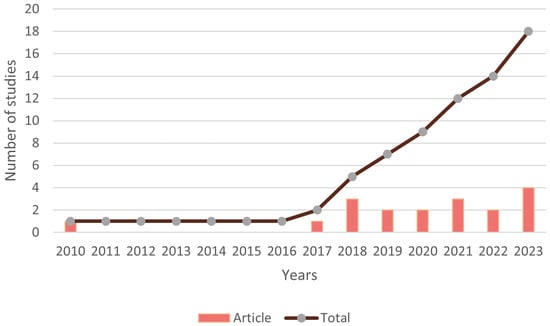
Figure 3.
Number of research studies on applications of VR and AR for medical training in resource-limited situations.
According to our shortlisted articles, most of the studies related to the application of VR and AR for medical training in LMICs took place after 2016 and only one study was conducted in 2010 by Debes et al. [36]. This 2010 study was excluded from consideration since the equipment used was different from the portable headset technology commonly associated with VR and AR. Therefore, the characteristics of the remaining 17 research studies are presented in Table 3.

Table 3.
Shortlisted articles included in our systematic review.
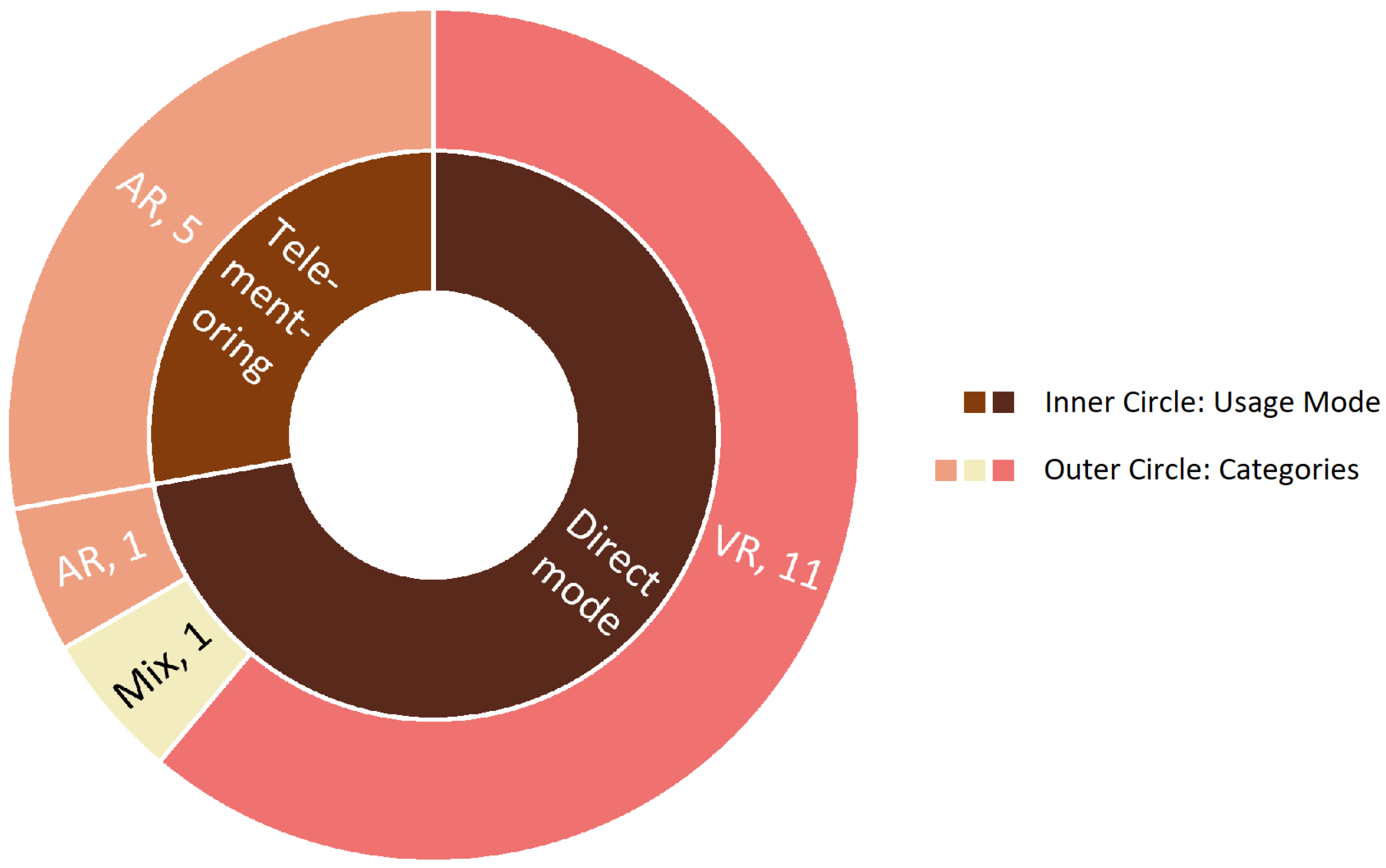
The distribution of the immersive technology employed by the investigations in these papers is displayed in Figure 4. More than half of the studies (11 studies) applied VR to medical training in resource-limited situations, while 7 studies employed AR in medical training, and only 1 study took both VR and AR into consideration. The usage mode of the immersive technology can be classified into two groups: direct mode and telementoring. Direct mode means the participants could gain knowledge or train their skills directly. Telementoring means that when the participants are conducting their training, assistants or professors could use the telecommunication device to provide guidance. It could be noticed that VR tended to utilise direct mode, while AR preferred telementoring. This could be as a result of AR technology’s ability to overlay data or visuals in real time, which makes it simpler for specialists to lead participants. As for which mode is more productive and profitable in LMICs, it has not yet been researched in the present era.
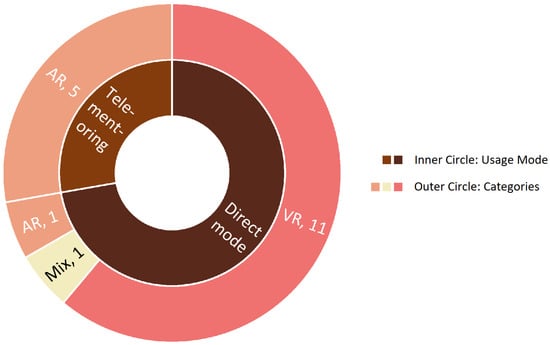
Figure 4.
Research divided by category and usage mode of immersive technology.
3.1.1. Medical Disciplines with VR and AR
(RQ1. What medical disciplines in training do immersive technology currently apply to?)
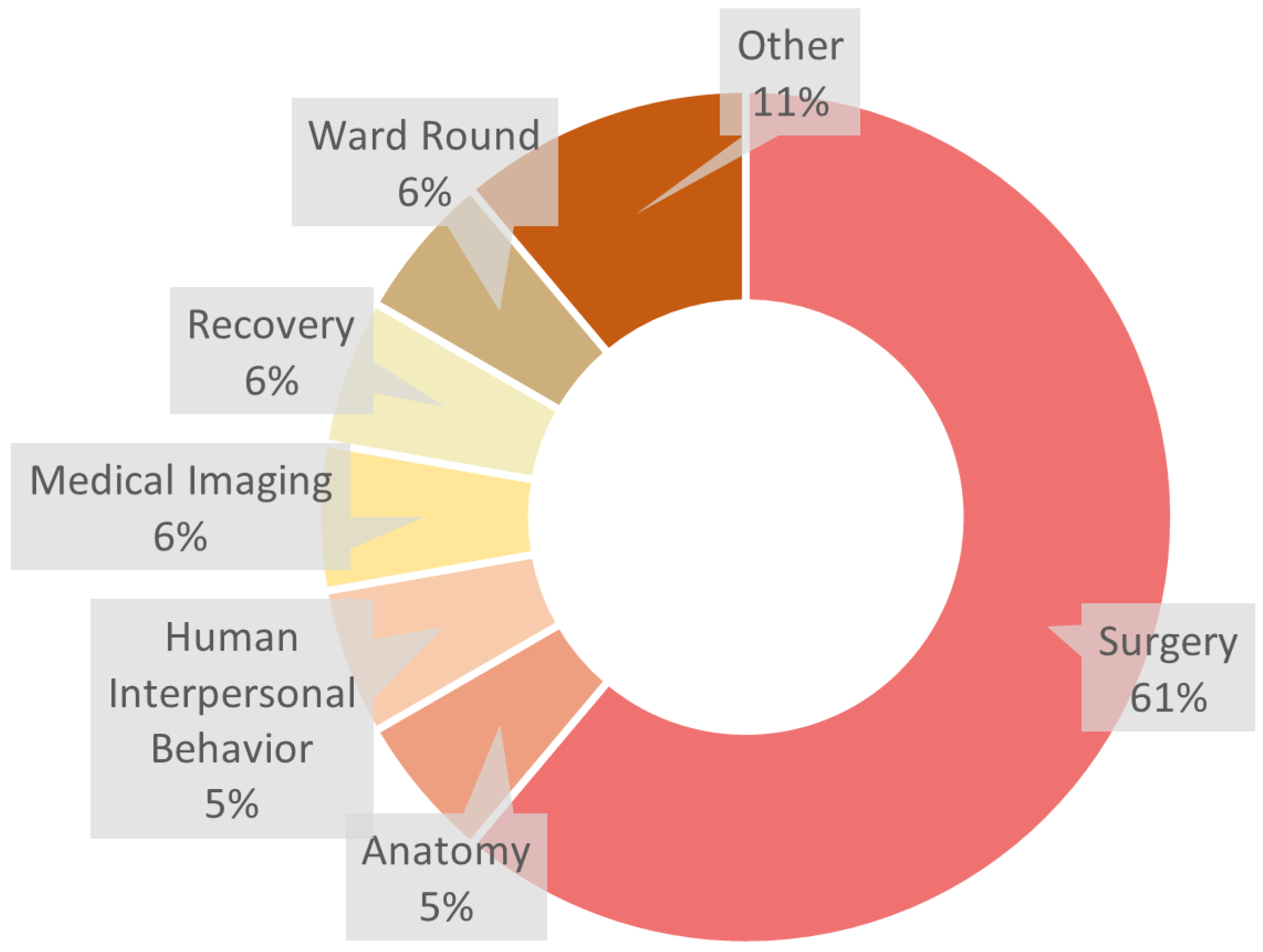
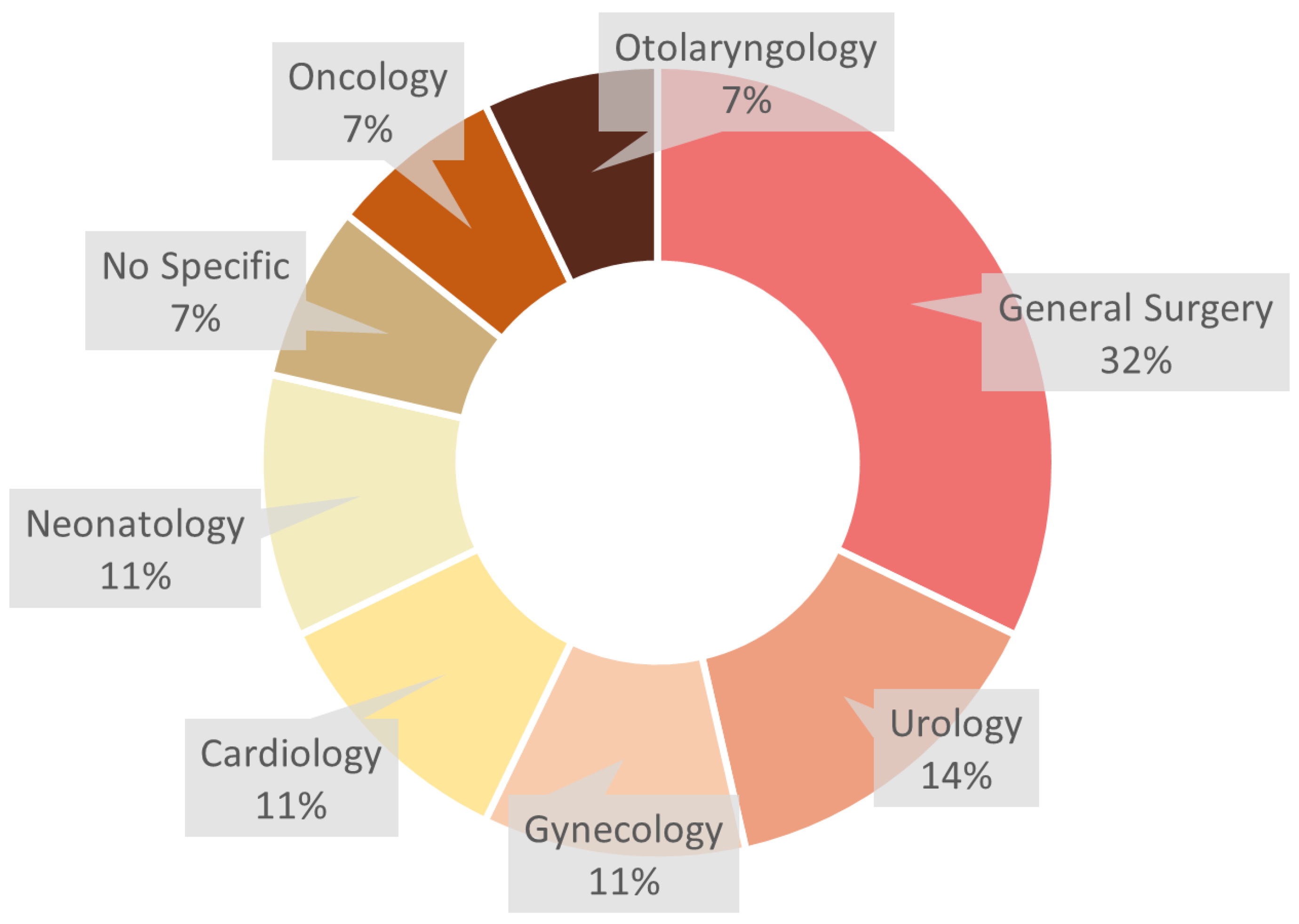
When it comes to the application field of VR and AR, most of the studies (10 studies) focused on the training of surgical skills, while other applications, such as anatomy and human interpersonal behaviour, only appeared once (Figure 5). Figure 6 presents the different medical disciplines in which VR and AR exist. The two most frequently occurring disciplines in this study are general surgery and urology, while the occurrence of other disciplines (gynaecology, cardiology, neonatology, oncology, and otolaryngology) is much lower, demonstrating the importance of these two disciplines in the medical education of LMICs. It should be noted that the medical discipline is classified manually, as some surgery does not exclusively belong to a certain discipline. Laparoscopic surgery and minimally invasive surgery could be used for various disciplines. At present, laparoscopic surgery has a wide range of indications and can be used for many gynaecological, urological, and general surgical diseases [26,36]. Further, minimally invasive surgery is a common concept and is suitable for numerous diseases [23]. Even laparoscopic surgery could be viewed as a kind of minimally invasive surgery, as the size of the small incision tends to be 0.5–1 cm.
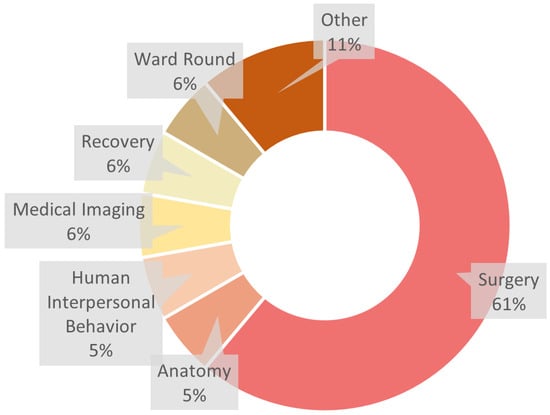
Figure 5.
Medical application of VR and AR. Image shows that “surgery” is the most common application.
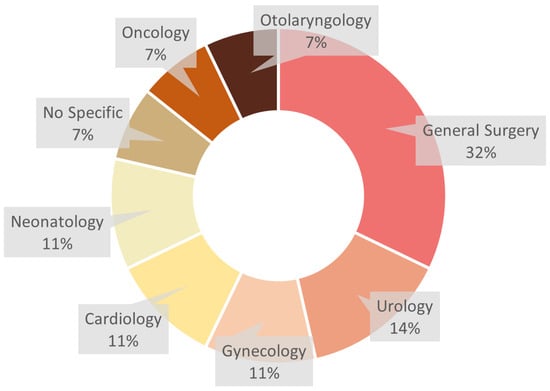
Figure 6.
Medical disciplines that have used VR or AR, with surgery (32%) being the most popular, followed by cardiology (12%), neonatology (12%) and urology (12%).
Before 2019, the primary focus of studies was on using VR and AR for surgical training, aiming to enhance the proficiency of medical students and professionals in performing various surgical procedures. Additionally, a few studies began to explore the use of VR in teaching medical imaging [37], aiming to improve the imaging interpretation skills. Between 2019 and 2021, the application fields of VR and AR expanded beyond surgical training to include neonatology [43] and cardiology [41]. These disciplines started recognising the potential benefits of immersive technologies for training purposes. Furthermore, a few studies began exploring the use of VR for patient education [41] and nurse training [24,43], indicating an expanding scope, aiming to improve the knowledge and skills of patients and nursing staff through immersive experiences. From 2021 to 2023, the use of VR and AR in medical training saw a significant increase across multiple disciplines, particularly in oncology [47] and otolaryngology [46]. These technologies were leveraged to provide comprehensive training solutions spanning various medical specialties. More studies also focused on the comprehensive application of VR and AR, covering a wide range of training scenarios from anatomy to surgical skills, aiming to offer a complete training experience that enhances both theoretical knowledge and practical skills. This trend reflects the growing recognition of the value of immersive technologies in enhancing medical education and training outcomes.
3.1.2. The Necessity of VR and AR
(RQ2. Is it necessary to use VR and AR in LMICs for medical education?)
Table 3 demonstrates that most of the studies agree on the effectiveness of VR and AR in medical education in resource-limited situations. The only exception [41] that provided a negative answer had a complex situation. It claimed that VR technology increased programme adherence, but on the other hand, it reduced patients’ motivation and absorption.
Before 2019, studies such as Wang et al. [37] highlighted the potential of VR and AR technologies to enhance the continuity of treatment, decrease the frequency of medical visits, and improve access to primary and professional health services. During this period, there was an emerging recognition of the feasibility and acceptability of immersive technologies in medical training, particularly in resource-limited settings. Between 2019 and 2021, more comprehensive studies were conducted. Studies like Bala et al. [42] demonstrated the effectiveness of remote access mixed reality tools in delivering medical training. These technologies were found to be attractive, as they could provide 3D perspectives in almost any direction, making them highly effective for the technical skill development in surgery [39,40]. From 2021 to 2023, the research further solidified the necessity of VR and AR in medical education within LMICs. Studies such as Pears et al. [21] showed that immersive technologies are not only feasible and acceptable but also highly effective for patient communication. These studies highlighted that VR and AR could help with both technical and non-technical skills, increasing the overall confidence and competence of medical interns.
3.1.3. Evaluation Methods for VR and AR in Medical Training
(RQ3. What evaluation methods are used to measure the effectiveness of VR and AR for medical training in LMICs?)
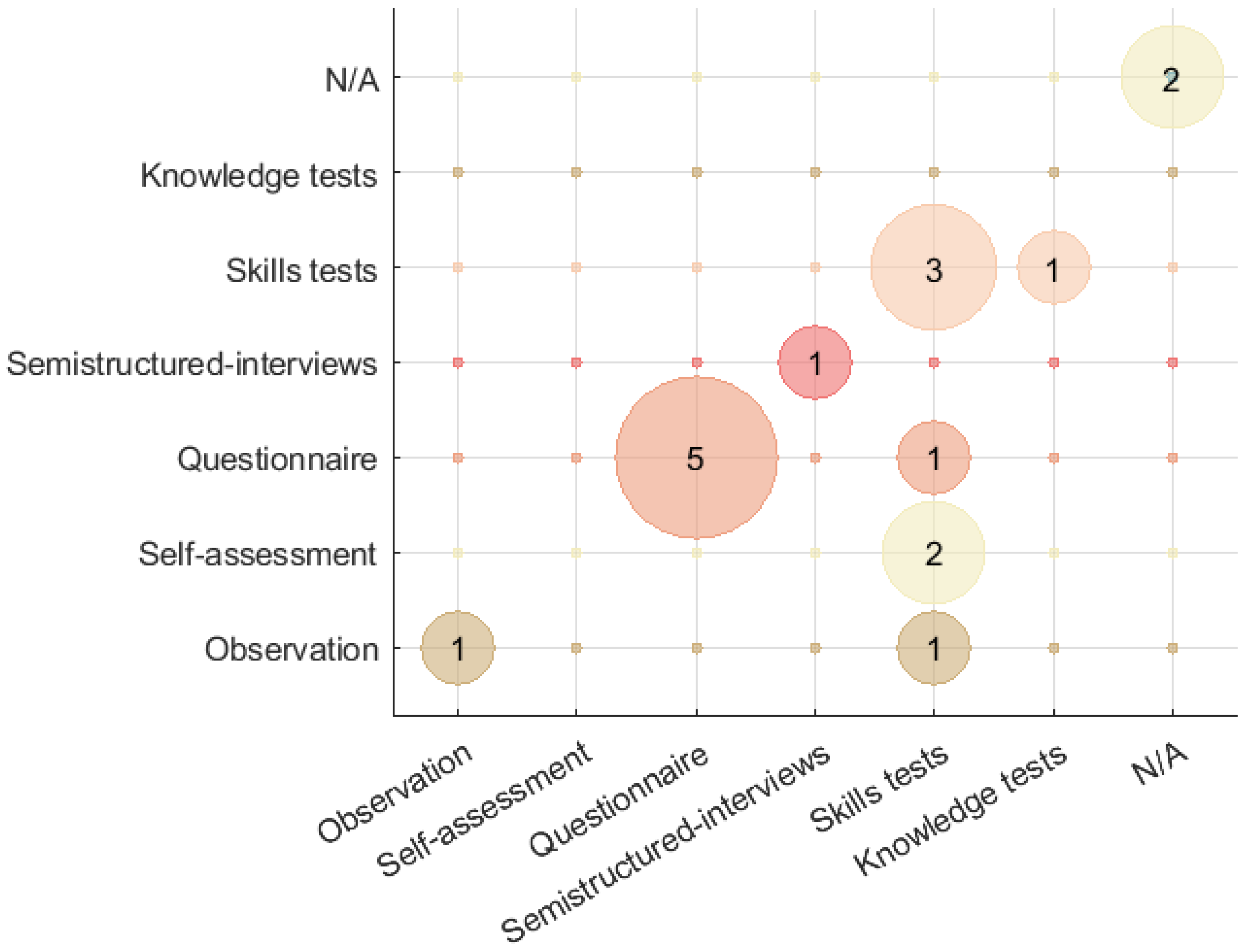
Most of the screened articles have no more than two evaluation methods for VR and AR in medical training (11 articles with one method, 5 articles with two methods), while 2 articles lack clarity in their evaluation methods [38,47]. The overall evaluation methods in the screened articles are shown in Figure 7. In terms of evaluation methods, the research since 2017 has not changed much. Questionnaires and skill tests have always been the mainstream. It should be noted that the bubble chart has the same horizontal and vertical axes, and the coordinate value of one bubble represents the two evaluation methods used in the specific article. Furthermore, if one bubble’s horizontal coordinate equals its vertical coordinate, it means there is only one evaluation method in that article. The size of the bubble shows the number of articles that use the same types of evaluation methods.
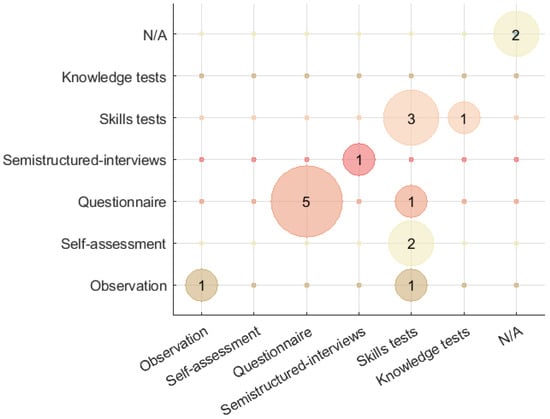
Figure 7.
Evaluation methods for VR or AR in medical training.
A total of six evaluation methods are identified in this study: observation, self-assessment, questionnaire, semistructured interview, skills test, and knowledge test. Among the evaluation methods, only the semistructured interview is a qualitative method based on grounded theory [44]. This research strategy can openly collect the views and attitudes of participants towards the application of VR and AR in medical education while effectively summarising and extracting the results. Bing et al. [44] identified five main topics related to VR in medical education from the interview, goals, non-technical skills and technical skills development, skill transfer, barriers, and recommendations, that could indicate the research direction or framework for subsequent research. Others belong to quantitative methods. Using these quantitative methods to assess the efficacy of VR and AR in medical education could provide a clearer picture of performance variations pre- and post test. However, it should be noticed that, except for the skills test and knowledge test, there is a certain degree of subjectivity in other evaluation methods. In total, 7 out of 17 articles utilised the skill test to prove the objectivity of their results. Questionnaires are the second most commonly used research method, which might be a result of the method’s ability to gather user experiences in a more transparent manner and to gather and analyse data faster. In addition, all of the studies conducted their experiments with the strategy of a ‘control group’. Through the control group experiments, they could make a comparison between the effects before and after using this method.
3.2. Questionnaire Survey
Requirements of LMICs: (RQ4. Which medical disciplines in LMICs require immersive technology the most?)
When asked about the familiarity of VR and AR, 62.8% of all students believe that they have used or seen 3D visualisations driven by immersive technology (like 3D models or interactive simulations) in some classes. On the other hand, 22.8% of students are still inexperienced with this mode.
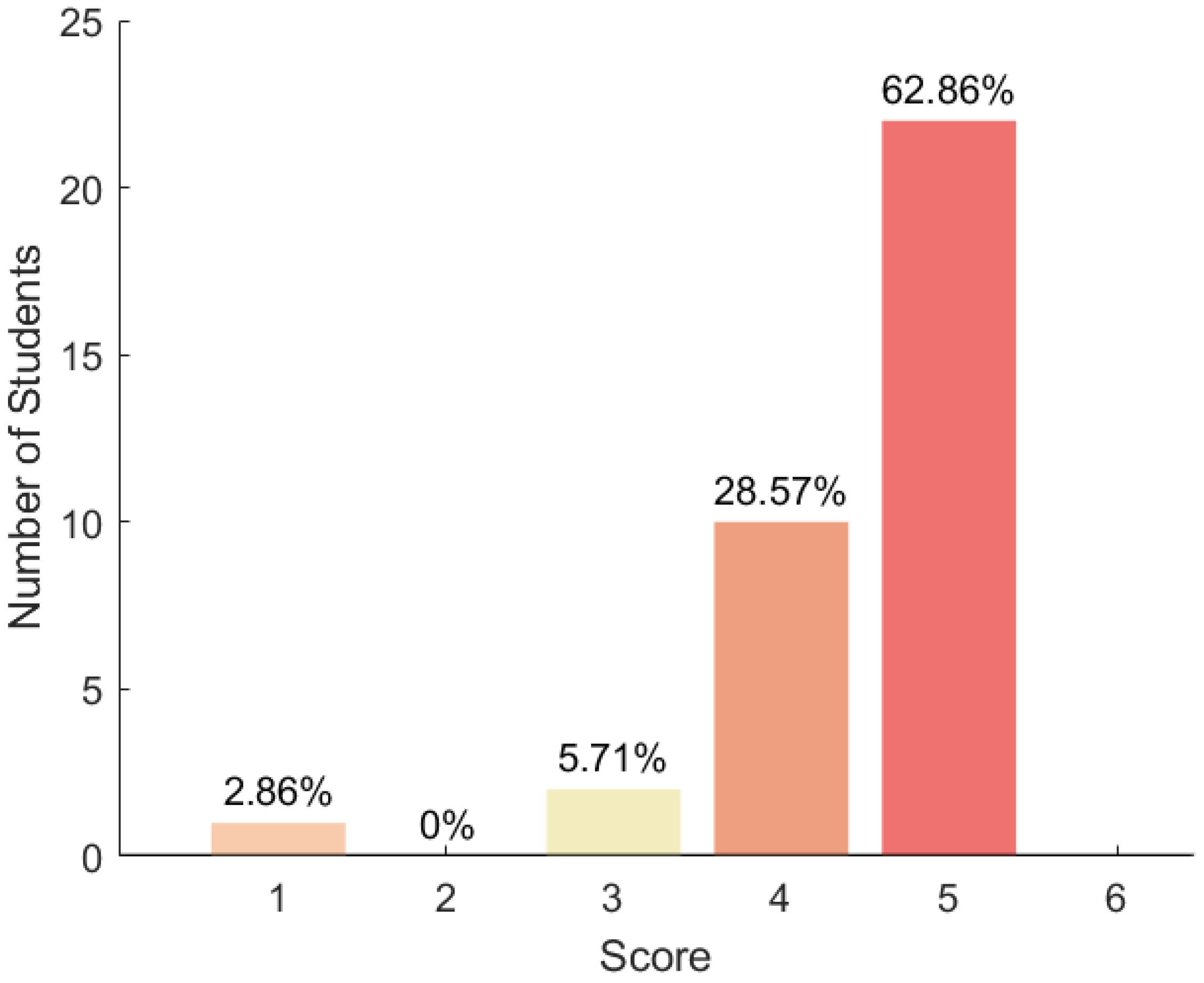
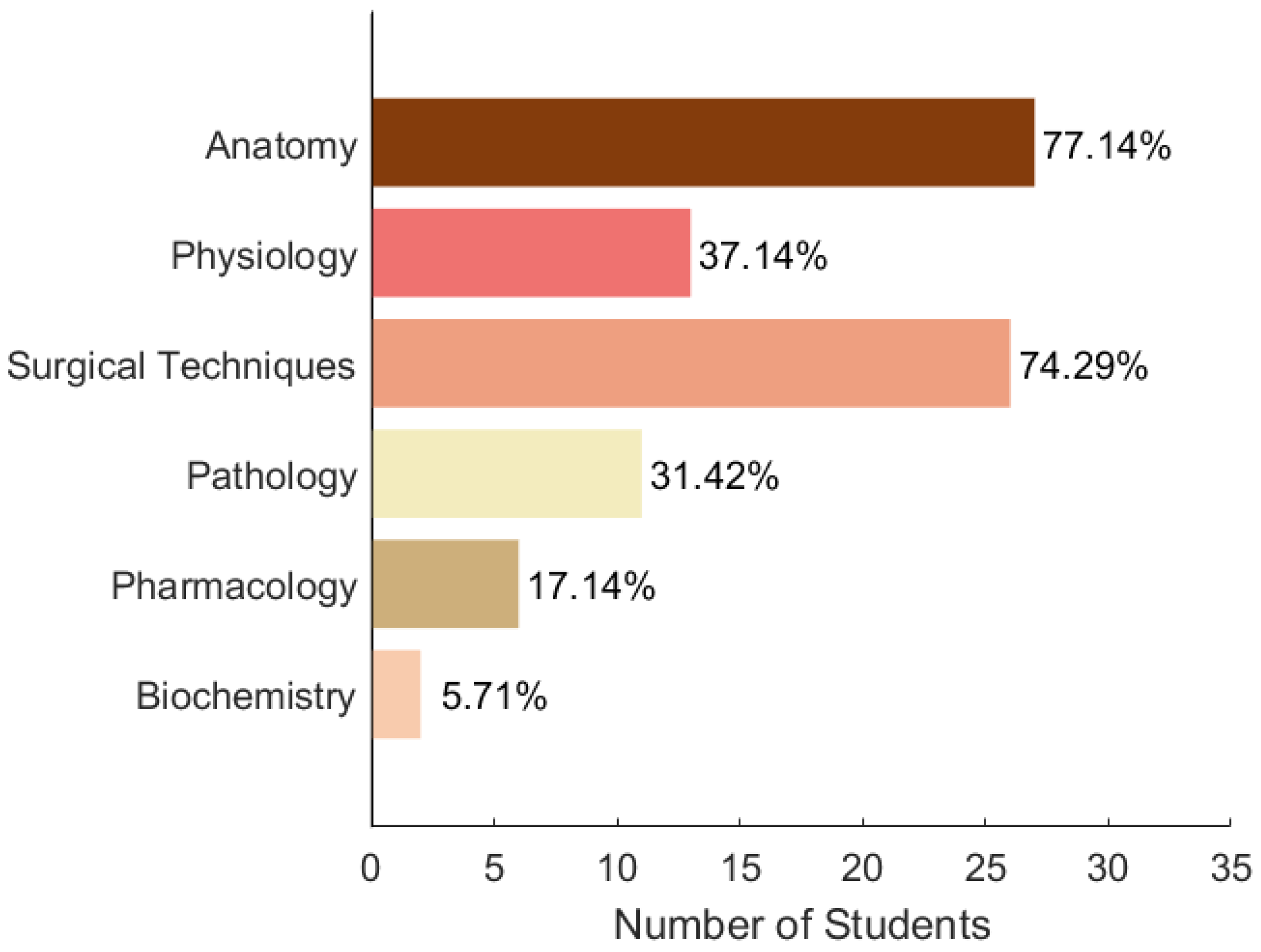
Figure 8 demonstrates the medical students’ attitudes towards the effectiveness of VR and AR in helping students understand difficult concepts compared to traditional 2D illustrations on a scale from 1 to 5. The majority of the participants believe that immersive technology can be helpful. These medical students also share the topics that they believe were the hardest to visualise and understand using only textbooks or 2D illustrations during their studies, which can be seen in Figure 9. More than 70% of students from both countries believe that anatomy and surgical techniques were the most difficult in that respect.
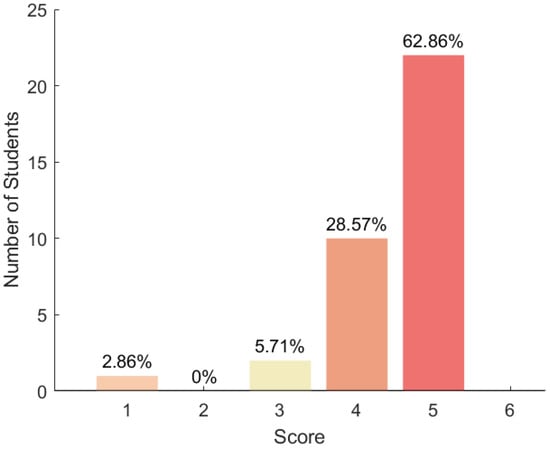
Figure 8.
Perceived benefits of VR and AR, on a scale of 1 to 5, in comparison to traditional 2D illustrations.
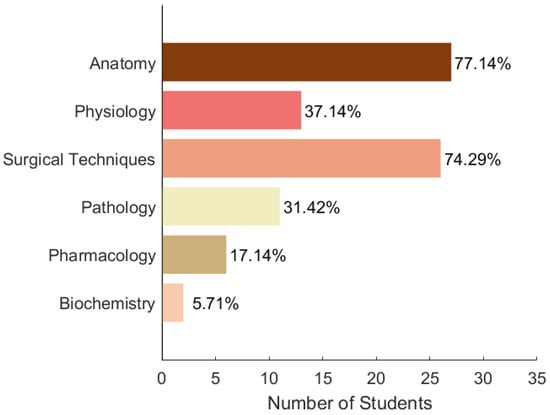
Figure 9.
Topics that are challenging to visualise and understand using only textbooks or 2D illustrations. According to student responses, anatomy and surgery were most challenging.
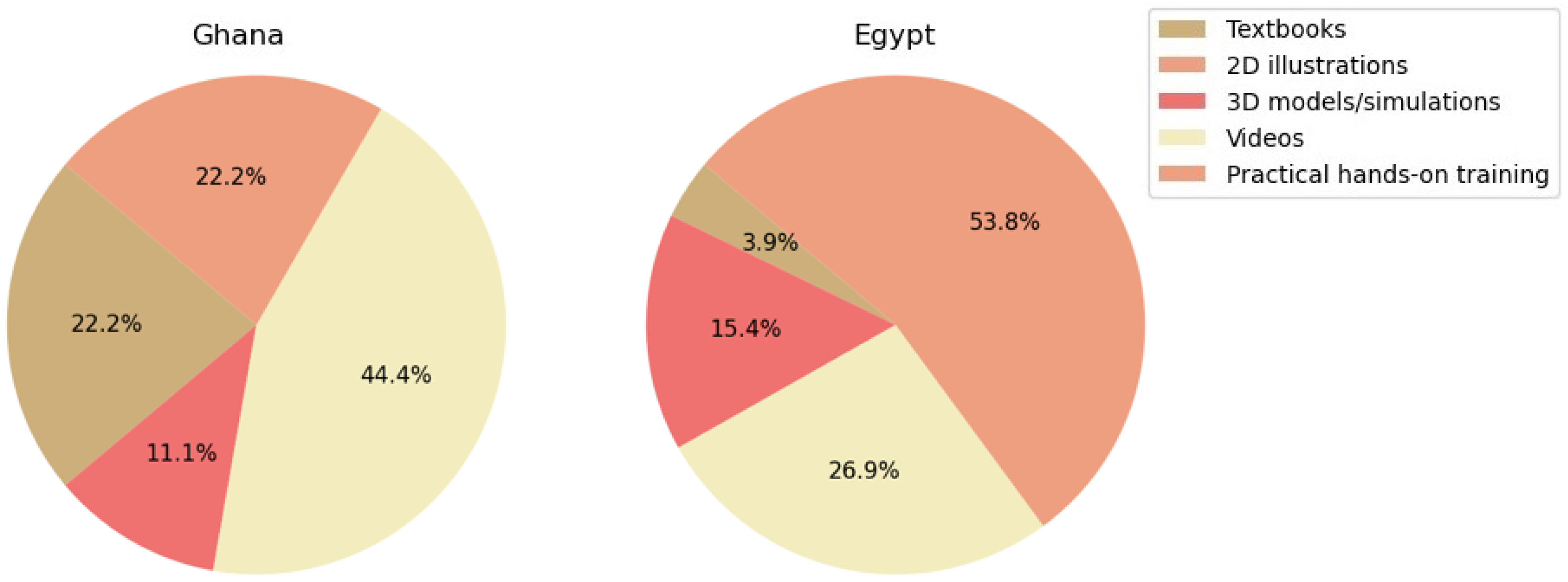
When asked about their preferred approach to studying, the results differed between Egyptian and Ghanaian students. As shown in Figure 10, the majority of students from Egypt believe that the best method to retain information is through practical, hands-on training. On the other hand, in Ghana, their preferences are more diverse, with a majority of 44.4% expressing that videos are the best method to learn new information. Their inexperience with VR technology and reservations about utilising it for medical education could be the cause of this phenomenon.
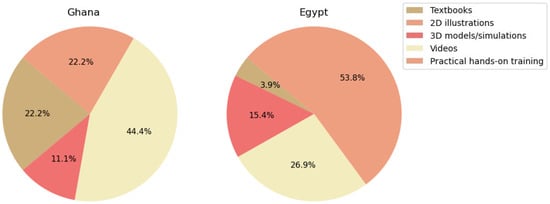
Figure 10.
Preferred learning modality according to two different LMIC countries (Egypt and Ghana).
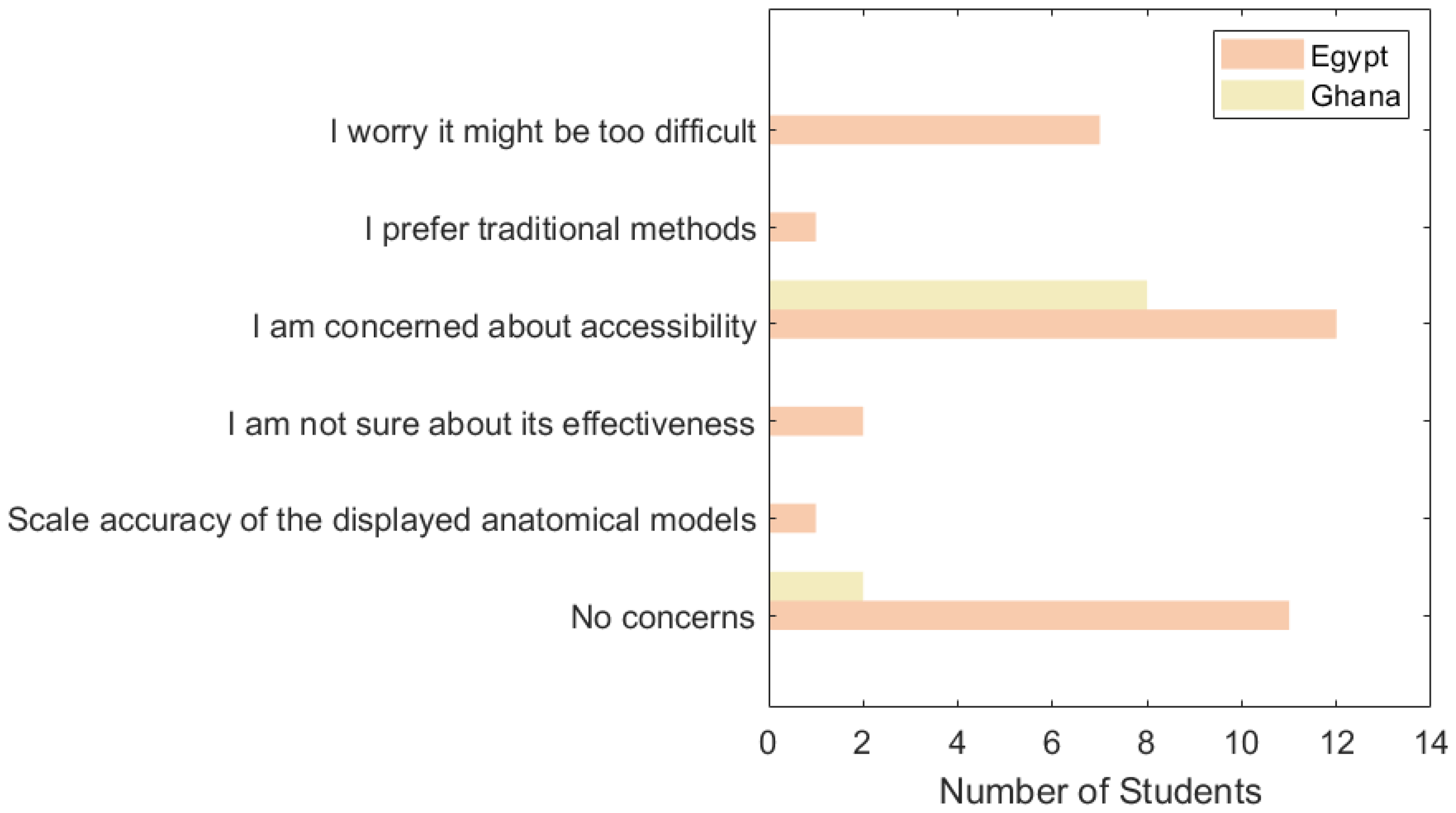
Figure 11 shows the students’ concerns about using VR and AR for medical training. Accessibility is the most significant problem in both countries, with difficulty being the second most significant problem in Egypt. Upon further analysis, almost half of the Egyptian students who expressed their concern regarding the difficulty were students who were not familiar with VR technology and 3D visualisations.
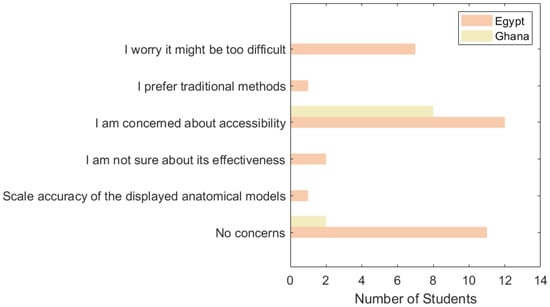
Figure 11.
Barriers and concerns about using VR and AR in medical education.
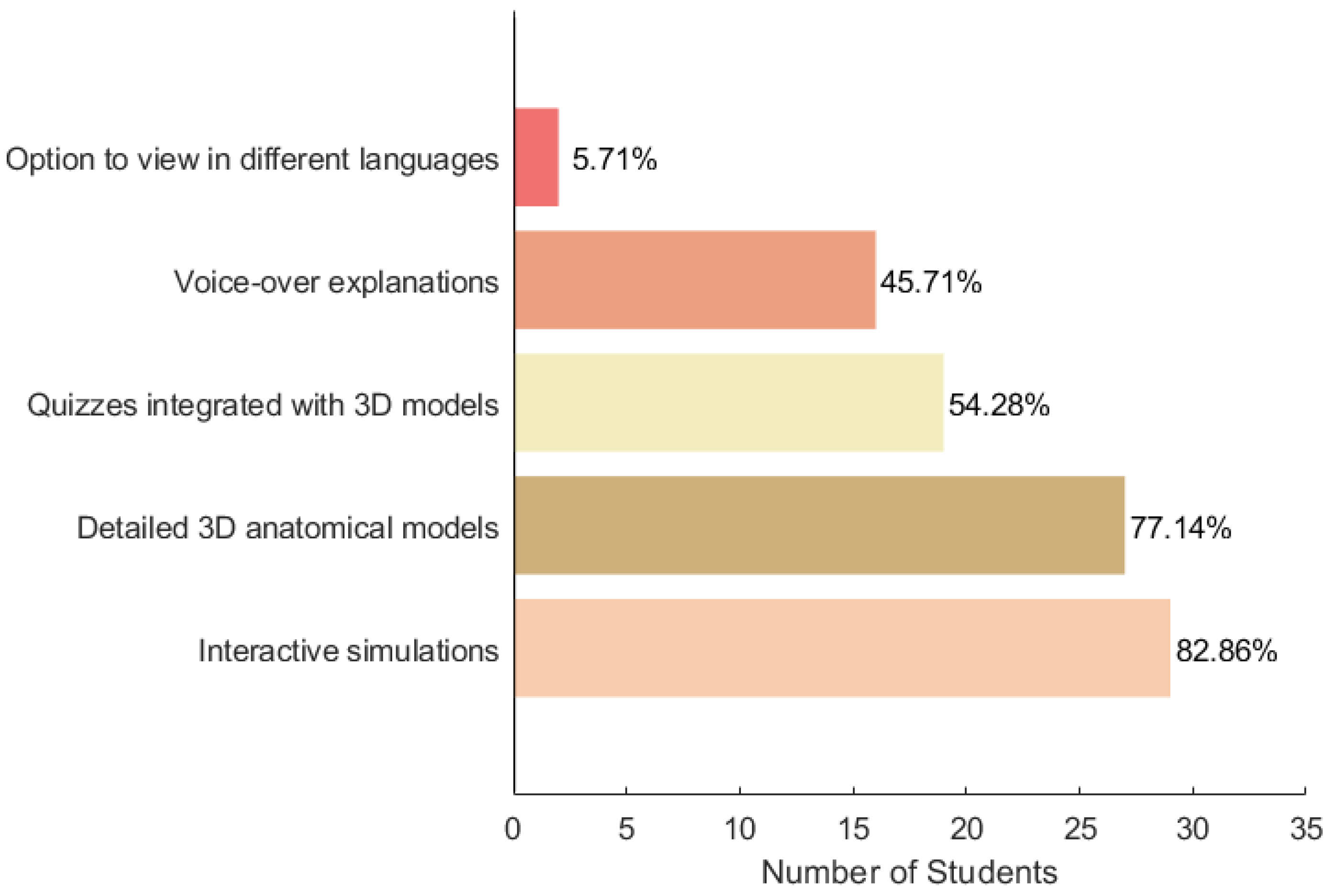
Finally, the students were asked, in the case that a 3D visualisation tool is introduced to help in understanding medical and surgical topics, which features they would find most beneficial. Their response can be seen in Figure 12, where most students agreed that interactive simulations and detailed 3D anatomical models would be favourable in their educational journey. After closer examination, a noteworthy observation emerged, whereby a majority of students exhibiting familiarity with VR technology endorsed the recommendation of interactive simulations. On the other hand, students who lacked exposure to VR technology were more inclined to suggest detailed 3D anatomical models.
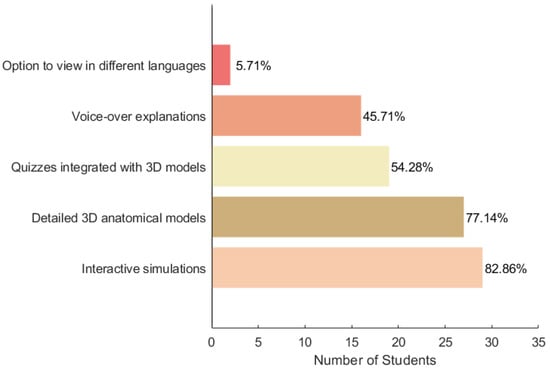
Figure 12.
Suggestions on immersive technology applications in medical education.
4. Discussion
4.1. Main Applications and Uses
Other than anatomy and surgery mentioned by the students, there is another important application, and that is human interpersonal behaviour. Also, from the results of the literature review part, it could be concluded that the main applications of VR and AR for medical training are surgery, anatomy, and human interpersonal behaviour as shown in Figure 5. Here is some detailed information about these three applications.
4.1.1. Anatomy
Traditional learning methods: Traditionally, students have had limited access to cadavers for hands-on learning [48]. To supplement their anatomical knowledge, they have frequently relied on 2D resources such as lecture slides, textbooks, and flashcards. Some early computer education software also used 2D resources for explanation and practice. Although such 2D workspaces were relatively more effective than traditional methods, working in a 3D environment may prove to be counterintuitive [49]. This often leaves a gap in understanding the intricate details and spatial relationships of body structures.
Innovations with AR/VR: With the advent of Head-Mounted Displays (HMDs) and immersive technologies, students can now delve deep into human anatomy through virtual exploration. This technology aids in grasping “threshold concepts” [50], foundational ideas in anatomy. A significant indicator of a student’s aptitude for learning anatomy is their spatial abilities. Three-dimensional structures can help with this [51,52]. The 360° views provided by HMDs unveil detailed structures, thereby enhancing comprehension. In addition, learning with HMDs has proven to be more stimulating and interactive than traditional methods [53], particularly with 3D brain structures [54]. As the integration of these technologies into medical education continues to evolve, they are setting new standards for how anatomy knowledge is delivered, making them an indispensable tool in the training of future healthcare professionals [55].
4.1.2. Surgery
Traditional training shortfalls: “See one, Do one, Teach one” was the traditional theory often used for medical training, especially for surgery [56]. It was mainly based on observation, followed by practice on actual patients [57]. This method presented risks and depended heavily on available patient cases.
AR/VR in surgical training: Virtual Reality has revolutionised this training by providing a controlled, risk-free environment. Continuous practice in these simulated settings has shown substantial improvements in surgical skill acquisition [58]. For instance, some previous studies indicate marked reductions in procedural errors [58] and improvements in instrument handling [59]. Moreover, specific surgeries like hysterectomy [39], laparoscopy [60], and total hip arthroscopy [61,62] can be practised repeatedly, ensuring mastery. In fields like ophthalmology [63,64], virtual training environments extend practical hours, offering more opportunities for skill acquisition without the need for actual patients.
4.1.3. Human Interpersonal Behaviour
Importance in medical training: Apart from technical know-how, a significant part of medical training is understanding human behaviour. Interacting with patients, understanding their concerns, and communicating effectively is as crucial as medical expertise [65].
Role of AR/VR: AR and VR training scenarios simulate interactions with virtual environments [66], allowing medical professionals to prepare for a wide range of situations. These scenarios offer a safe space to practise interpersonal skills, from breaking bad news to understanding non-verbal cues. The emphasis is on decision-making, critical thinking, and effective communication [67,68,69]. Furthermore, in high-pressure environments, like medical emergencies, clinicians can train to manage stress and ensure clear communication. These non-technical skills (NTS) are pivotal for patient care and also have a significant impact on medical outcomes [70].
4.2. Benefits
(RQ5. What is the transformative potential of VR and AR to improve medical education?)
The immersive nature of AR/VR platforms exposes students to an environment that mimics the real world, enhancing their cognitive abilities [16]. In the literature, studies have shown that with repeated practice in Virtual Reality, medical residents not only hone their surgical techniques [71] but can also achieve expert proficiency levels on many key performance metrics. For instance, our review indicated significant reductions in procedural errors, improved instrument handling, and efficiency in completing surgeries.
Traditional anatomy classes have always faced the challenge of cadaver availability. Students often resort to 2D resources like textbooks and slides to supplement their learning. This is where Head-Mounted Displays (HMDs) can revolutionise the learning experience. These devices empower students to be more proactive, allowing them to explore, understand, and grasp complex medical concepts at their own pace. It is a proven fact that active learning fosters better retention and understanding [72]. Additionally, our review spotlighted how HMDs have been extensively utilised in surgery and anatomy with impressive outcomes, like reduced surgical errors and enhanced knowledge retention [16]. In fields such as ophthalmology, where practising on actual human eyes is limited, virtual scenarios can significantly extend training hours [64].
High-stress environments, particularly during medical emergencies, demand impeccable skill and calm composure from healthcare professionals. Preparing for such high-pressure scenarios is crucial. XR training modules can replicate these intense conditions, offering clinicians a safe space to prepare for real-life challenges [73].
Furthermore, it is worth emphasising the importance of ‘threshold concepts’ in medical education. These are foundational ideas, without which students cannot progress. With immersive technologies, these concepts become more accessible [74]. Traditional 2D materials, like textbooks, often fail to provide the spatial understanding required for grasping intricate organ structures, a gap that HMDs effectively bridge.
The modern medical curriculum is voluminous, demanding students to assimilate vast amounts of information. The motivation derived from interactive and immersive 3D models can significantly elevate engagement levels, making the learning process more efficient and enjoyable [75]. Think about it: when a student can virtually dissect and explore a 3D model of the human brain, it is bound to be more captivating than simply flipping through textbook diagrams.
In conclusion, AR and VR technologies in medical education are not just about flashy visuals. They are about maximising learning opportunities, ensuring consistency in training, and preparing our future healthcare professionals for the real-world challenges they will inevitably face. Whether it is the scarcity of cadavers or the need for safe training environments, AR/VR offers practical solutions that are both effective and cost-efficient. The era of traditional, rote-based learning is giving way to a more interactive, immersive, and impactful pedagogical approach.
4.3. Problems and Limitations
As the medical students point out in the questionnaire, the most significant barrier to revolutionising medical education in LMICs by using VR and AR is the accessibility of 3D visualisation devices. However, as investment increases in this area, it will no longer be a problem in the near future [76]. Although many medical departments in LMICs now use immersive equipment for training, there are still many medical projects that still use traditional methods for training and need to be explored using VR and AR. While VR and AR can provide immersive 3D perspectives and enhance medical skills as noted by Bing et al. [39], technical issues such as hardware malfunctions, software glitches, internet issues [21], and the need for regular updates can impede their effectiveness. These technologies require robust digital infrastructure, which is not always available in LMICs.
Other problems can be attributed to certain technical deficiencies symptoms [77]. Bala and colleagues reported that it was difficult to interact when there were multiple participants because the background noise might occur simultaneously [42]. Some users have shown physical discomforts, including nausea, dizziness, and temporary vision impairment. These symptoms often occur after just 20 min of use. Specifically, the lag time and the human eye’s challenge in fixating on “artificially distant” 3D objects are identified [78].
(1) Motion sickness: While motion sickness can be mitigated by limiting head movements or leveraging higher-resolution HMDs [79], it still remains a concern for many users. Interestingly, Augmented Reality (AR) has demonstrated potential for reducing the effects of motion sickness.
(2) Lack of model detail and haptic feedback: Accurate representation and the sensation of touch are crucial in medical training. However, current XR systems sometimes fall short in these areas [80,81].
(3) Familiarisation workload: The learning curve associated with getting acquainted with XR devices can place additional strain on users [82].
(4) User experience limitations: The limited Field Of View (FOV) or the inherent weight of the devices can occasionally hamper the user experience [83,84].
(5) Device constraints: Given that a single HMD typically supports just one user, it becomes time intensive to conduct group-based experiments or training sessions [85]. Furthermore, shared devices can raise hygiene concerns, especially during health crises like the COVID-19 pandemic.
5. Conclusions
This paper aims to explore the current applications and the real requirements of VR and AR technology as medical training methods in LMICs through a literature review and a questionnaire survey. The review collects a total of 17 articles published from 2010 to 2023, analysing their focused application fields, medical disciplines, evaluation methods, benefits, and limitations. Also, the questionnaire exposes the relatively objective views of medical students in Egypt and Ghana on VR and AR in medical training.
This paper shows that the number of studies on XR technology for medical training within LMICs is relatively small. Thankfully, though, research in related fields has been steadily increasing in recent years. Most of the studies focus on surgery, but they are not fixed within specific disciplines. Maybe universal surgical skills, such as laparoscopy, are more suitable for LMICs. It should also be noted that most studies have not mentioned the economic aspects of immersive technology devices or systems. Also, NTS (non-technical skills) is another aspect overlooked by most of the existing research. In other areas where circumstances allow, employing immersive technology for the training of NTS has become a prevalent approach [86,87].
Despite the enormous potential of VR and AR, it is crucial to recognise the importance of blending these technologies with existing pedagogical methods. While VR and AR can replicate clinical scenarios, advanced communication skills and in situ simulations still require traditional approaches [88]. Certain skills, such as effective patient communication, cannot be fully imparted through immersive technologies. Only the integration of VR and AR can enable educators to focus more on other skills. What VR and AR offer, actually, is the freedom to reallocate resources, both in terms of space and faculty, to areas they are best suited for.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/virtualworlds3030021/s1, PRISMA-Checklist.
Author Contributions
Conceptualisation, X.L. and R.G.; methodology, X.L. and G.S.; formal analysis, X.L.; investigation, D.E.; writing—original draft preparation, X.L.; writing—review and editing, G.S.; visualisation, X.L., D.E. and G.S.; supervision, R.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was approved by the Ethics Committee of College of Science and Engineering, University of Glasgow (Application Number: 300230176).
Informed Consent Statement
Informed consent was obtained from all particpants involved in the study.
Data Availability Statement
No new data were created or analysed in this study.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Reddy, B.; Thomas, S.; Karachiwala, B.; Sadhu, R.; Iyer, A.; Sen, G.; Mehrtash, H.; Tunçalp, Ö. A scoping review of the impact of organisational factors on providers and related interventions in LMICs: Implications for respectful maternity care. PLoS Glob. Public Health 2022, 21, e0001134. [Google Scholar] [CrossRef] [PubMed]
- Bailenson, J. Experience on Demand: What Virtual Reality Is, How It Works, and What It Can Do; W.W. Norton & Company: New York, NY, USA; London UK, 2018. [Google Scholar]
- McLachlan, J.C.; Bligh, J.; Bradley, P.; Searle, J. Teaching Anatomy without Cadavers. Med. Educ. 2004, 38, 418–424. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.; Botelho, F.; Pinkham, L.; Guadagno, E.; Poenaru, D. Technology-enhanced trauma training in low-resource settings: A scoping review and feasibility analysis of educational technologies. J. Pediatr. Surg. 2023, 58, 955–963. [Google Scholar] [CrossRef] [PubMed]
- Magi, C.E.; Bambi, S.; Iovino, P.; El Aoufy, K.; Amato, C.; Balestri, C.; Rasero, L.; Longobucco, Y. Virtual reality and augmented reality training in disaster medicine courses for students in nursing: A scoping review of adoptable tools. Behav. Sci. 2023, 13, 616. [Google Scholar] [CrossRef] [PubMed]
- Richardson, D.; Kinnear, B.; Hauer, K.; Turner, T.; Warm, E.; Hall, A.; Ross, S.; Thoma, B.; Van Melle, E. Growth mindset in competency-based medical education. Med. Teach. 2021, 43, 1–7. [Google Scholar] [CrossRef]
- McGaghie, W.C.; Issenberg, S.B.; Cohen, E.R.; Barsuk, J.H.; Wayne, D.B. Does Simulation-Based Medical Education With Deliberate Practice Yield Better Results Than Traditional Clinical Education? A Meta-Analytic Comparative Review of the Evidence. Acad. Med. 2011, 86, 706–711. [Google Scholar] [CrossRef]
- Higgins, M.; Madan, C.R.; Patel, R. Deliberate practice in simulation-based surgical skills training: A scoping review. J. Surg. Educ. 2021, 78, 1328–1339. [Google Scholar] [CrossRef]
- Brunzini, A.; Papetti, A.; Messi, D.; Germani, M. A comprehensive method to design and assess mixed reality simulations. Virtual Real. 2022, 26, 1257–1275. [Google Scholar] [CrossRef]
- Dinh, J.; Traylor, A.; Kilcullen, M.; Perez, J.; Schweissing, E.; Venkatesh, A.; Salas, E. Cross-Disciplinary Care: A Systematic Review on Teamwork Processes in Health Care. Small Group Res. 2019, 51, 104649641987200. [Google Scholar] [CrossRef]
- Khanal, P.; Vankipuram, A.; Ashby, A.; Vankipuram, M.; Gupta, A.; Drumm-Gurnee, D.; Josey, K.; Tinker, L.; Smith, M. Collaborative Virtual Reality Based Advanced Cardiac Life Support Training Simulator Using Virtual Reality Principles. J. Biomed. Inform. 2014, 51, 49–59. [Google Scholar] [CrossRef]
- Liaw, S.Y.; Ooi, S.W.; Rusli, K.D.B.; Lau, T.C.; Tam, W.W.S.; Chua, W.L. Nurse-Physician Communication Team Training in Virtual Reality Versus Live Simulations: Randomized Controlled Trial on Team Communication and Teamwork Attitudes. J. Med. Internet Res. 2020, 22, e17279. [Google Scholar] [CrossRef] [PubMed]
- Prasolova-Førland, E.; McCallum, S.; Estrada, J.G. Collaborative learning in VR for cross-disciplinary distributed student teams. In Proceedings of the 2021 IEEE Conference on virtual reality and 3D user interfaces abstracts and workshops (VRW), Virtual, 27 March–3 April 2021; pp. 320–325. [Google Scholar]
- Wang, X.; Song, G.; Ghannam, R. Enhancing Teamwork and Collaboration: A Systematic Review of Algorithm-Supported Pedagogical Methods. Educ. Sci. 2024, 14, 675. [Google Scholar] [CrossRef]
- Von Jan, U.; Noll, C.; Behrends, M.; Albrecht, U.V. mARble—Augmented Reality in Medical Education. Biomed. Eng./Biomed. Tech. 2012, 57, 67–70. [Google Scholar] [CrossRef]
- Barteit, S.; Lanfermann, L.; Bärnighausen, T.; Neuhann, F.; Beiersmann, C. Augmented, mixed, and virtual reality-based head-mounted devices for medical education: Systematic review. JMIR Serious Games 2021, 9, e29080. [Google Scholar] [CrossRef] [PubMed]
- Berman, N.B.; Durning, S.J.; Fischer, M.R.; Huwendiek, S.; Triola, M.M. The Role for Virtual Patients in the Future of Medical Education. Acad. Med. 2016, 91, 1217–1222. [Google Scholar] [CrossRef]
- Antel, R.; Abbasgholizadeh-Rahimi, S.; Guadagno, E.; Harley, J.M.; Poenaru, D. The use of artificial intelligence and virtual reality in doctor-patient risk communication: A scoping review. Patient Educ. Couns. 2022, 105, 3038–3050. [Google Scholar] [CrossRef]
- Talbot, T.B.; Sagae, K.; John, B.; Rizzo, A.A. Sorting Out the Virtual Patient: How to Exploit Artificial Intelligence, Game Technology and Sound Educational Practices to Create Engaging Role-Playing Simulations. Int. J. Gaming Comput.-Mediat. Simul. 2012, 4, 1–19. [Google Scholar] [CrossRef]
- Tzachor, A.; Sabri, S.; Richards, C.; Rajabifard, A.; Acuto, M. Potential and limitations of digital twins to achieve the Sustainable Development Goals. Nat. Sustain. 2022, 5, 1–8. [Google Scholar] [CrossRef]
- Pears, M.; Rochester, M.; Wadhwa, K.; Payne, S.R.; Konstantinidis, S.; Hanchanale, V.; Elmamoun, M.H.; Biyani, C.S.; Doherty, R. A Pilot Study Evaluating a Virtual Reality-Based Nontechnical Skills Training Application for Urology Trainees: Usability, Acceptability, and Impact. J. Surg. Educ. 2023, 80, 1836–1842. [Google Scholar] [CrossRef]
- Awori, J.; Friedman, S.D.; Howard, C.; Kronmal, R.; Buddhe, S. Comparative Effectiveness of Virtual Reality (VR) vs 3D Printed Models of Congenital Heart Disease in Resident and Nurse Practitioner Educational Experience. 3D Print. Med. 2023, 9, 2. [Google Scholar] [CrossRef]
- Parham, G.; Bing, E.G.; Cuevas, A.; Fisher, B.; Skinner, J.; Mwanahamuntu, M.; Sullivan, R. Creating a Low-Cost Virtual Reality Surgical Simulation to Increase Surgical Oncology Capacity and Capability. Ecancermedicalscience 2019, 13, 910. [Google Scholar] [CrossRef] [PubMed]
- McCullough, M.C.; Kulber, L.; Sammons, P.; Santos, P.; Kulber, D.A. Google Glass for Remote Surgical Tele-proctoring in Low- and Middle-income Countries: A Feasibility Study from Mozambique. Plast. Reconstr. Surg.-Glob. Open 2018, 6, e1999. [Google Scholar] [CrossRef] [PubMed]
- Rojas-Muñoz, E.; Cabrera, M.E.; Lin, C.; Andersen, D.; Popescu, V.; Anderson, K.; Zarzaur, B.L.; Mullis, B.; Wachs, J.P. The System for Telementoring with Augmented Reality (STAR): A Head-Mounted Display to Improve Surgical Coaching and Confidence in Remote Areas. Surgery 2020, 167, 724–731. [Google Scholar] [CrossRef] [PubMed]
- Hardon, S.F.; Kooijmans, A.; Horeman, R.; Van Der Elst, M.; Bloemendaal, A.L.A.; Horeman, T. Validation of the Portable Virtual Reality Training System for Robotic Surgery (PoLaRS): A Randomized Controlled Trial. Surg. Endosc. 2022, 36, 5282–5292. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Anastasiou, E.; Balafoutis, A.T.; Fountas, S. Applications of Extended Reality (XR) in Agriculture, Livestock Farming, and Aquaculture: A Review. Smart Agric. Technol. 2023, 3, 100105. [Google Scholar] [CrossRef]
- Eriksen, M.B.; Frandsen, T.F. The Impact of Patient, Intervention, Comparison, Outcome (PICO) as a Search Strategy Tool on Literature Search Quality: A Systematic Review. J. Med. Libr. Assoc. 2018, 106, 420–431. [Google Scholar] [CrossRef]
- Schiavenato, M.; Chu, F. PICO: What it is and what it is not. Nurse Educ. Pract. 2021, 56, 103194. [Google Scholar] [CrossRef]
- Mergen, M.; Meyerheim, M.; Graf, N. Towards Integrating Virtual Reality into Medical Curricula: A Single Center Student Survey. Educ. Sci. 2023, 13, 477. [Google Scholar] [CrossRef]
- Microsoft. Announcing Microsoft HoloLens Development Edition Open for Pre-Order, Shipping. 2016. Available online: https://blogs.windows.com/devices/2016/02/29/announcing-microsoft-hololens-development-edition-open-for-pre-order-shipping-march-30/ (accessed on 2 September 2024).
- The Guardian. Facebook Confirms Oculus Rift Virtual Reality Headset Will Ship in 2016. 2015. Available online: https://www.theguardian.com/technology/2015/may/06/facebook-oculus-rift-virtual-reality-2016 (accessed on 20 July 2024).
- Cuervo, E.; Chintalapudi, K.; Kotaru, M. Creating the perfect illusion: What will it take to create life-like virtual reality headsets? In Proceedings of the 19th International Workshop on Mobile Computing Systems & Applications, Tempe, AZ, USA, 12–13 February 2018; pp. 7–12. [Google Scholar]
- Taiwan Semiconductor Manufacturing Company (TSMC). 7 nm Technology. 2024. Available online: https://www.tsmc.com/english/dedicatedFoundry/technology/logic/l_7nm (accessed on 20 July 2024).
- Debes, A.J.; Aggarwal, R.; Balasundaram, I.; Jacobsen, M.B. A Tale of Two Trainers: Virtual Reality versus a Video Trainer for Acquisition of Basic Laparoscopic Skills. Am. J. Surg. 2010, 199, 840–845. [Google Scholar] [CrossRef]
- Wang, S.; Parsons, M.; Stone-McLean, J.; Rogers, P.; Boyd, S.; Hoover, K.; Meruvia-Pastor, O.; Gong, M.; Smith, A. Augmented Reality as a Telemedicine Platform for Remote Procedural Training. Sensors 2017, 17, 2294. [Google Scholar] [CrossRef] [PubMed]
- Greenfield, M.J.; Luck, J.; Billingsley, M.L.; Heyes, R.; Smith, O.J.; Mosahebi, A.; Khoussa, A.; Abu-Sittah, G.; Hachach-Haram, N. Demonstration of the Effectiveness of Augmented Reality Telesurgery in Complex Hand Reconstruction in Gaza. Plast. Reconstr. Surg.-Glob. Open 2018, 6, e1708. [Google Scholar] [CrossRef] [PubMed]
- Bing, E.G.; Parham, G.P.; Cuevas, A.; Fisher, B.; Skinner, J.; Mwanahamuntu, M.; Sullivan, R. Using low-cost virtual reality simulation to build surgical capacity for cervical cancer treatment. J. Glob. Oncol. 2019, 5, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Alvarez-Lopez, F.; Maina, M.F.; Arango, F.; Saigí-Rubió, F. Use of a Low-Cost Portable 3D Virtual Reality Simulator for Psychomotor Skill Training in Minimally Invasive Surgery: Task Metrics and Score Validity. JMIR Serious Games 2020, 8, e19723. [Google Scholar] [CrossRef] [PubMed]
- Da Cruz, M.M.A.; Ricci-Vitor, A.L.; Borges, G.L.B.; Da Silva, P.F.; Turri-Silva, N.; Takahashi, C.; Grace, S.L.; Vanderlei, L.C.M. A Randomized, Controlled, Crossover Trial of Virtual Reality in Maintenance Cardiovascular Rehabilitation in a Low-Resource Setting: Impact on Adherence, Motivation, and Engagement. Phys. Ther. 2021, 101, pzab071. [Google Scholar] [CrossRef]
- Bala, L.; Kinross, J.; Martin, G.; Koizia, L.J.; Kooner, A.S.; Shimshon, G.J.; Hurkxkens, T.J.; Pratt, P.J.; Sam, A.H. A Remote Access Mixed Reality Teaching Ward Round. Clin. Teach. 2021, 18, 386–390. [Google Scholar] [CrossRef]
- Umoren, R.; Bucher, S.; Hippe, D.S.; Ezenwa, B.N.; Fajolu, I.B.; Okwako, F.M.; Feltner, J.; Nafula, M.; Musale, A.; Olawuyi, O.A.; et al. eHBB: A Randomised Controlled Trial of Virtual Reality or Video for Neonatal Resuscitation Refresher Training in Healthcare Workers in Resource-Scarce Settings. BMJ Open 2021, 11, e048506. [Google Scholar] [CrossRef]
- Bing, E.G.; Brown, M.L.; Cuevas, A.; Sullivan, R.; Parham, G.P. User experience with low-cost virtual reality cancer surgery simulation in an African setting. JCO Glob. Oncol. 2021, 7, 435–442. [Google Scholar] [CrossRef]
- Ezenwa, B.N.; Umoren, R.; Fajolu, I.B.; Hippe, D.S.; Bucher, S.; Purkayastha, S.; Okwako, F.; Esamai, F.; Feltner, J.B.; Olawuyi, O.; et al. Using Mobile Virtual Reality Simulation to Prepare for In-Person Helping Babies Breathe Training: Secondary Analysis of a Randomized Controlled Trial (the eHBB/mHBS Trial). JMIR Med. Educ. 2022, 8, e37297. [Google Scholar] [CrossRef]
- Tapiala, J.; Iso-Mustajärvi, M.; Timonen, T.; Vrzáková, H.; Dietz, A. Impact of Virtual Reality Training on Mastoidectomy Performance: A Prospective Randomised Study. Eur. Arch. Oto-Rhino 2024, 281, 701–710. [Google Scholar] [CrossRef]
- Samantaray, A.; Kaur, T.; Singhal, S.; Gandhi, T.K. Remote Assistance in Cervical Cancer Screening Using Microsoft Hololens 2: An Augmented-Reality Based Approach. In Proceedings of the 2023 International Conference on Recent Advances in Electrical, Electronics & Digital Healthcare Technologies (REEDCON), New Delhi, India, 1–3 May 2023; pp. 123–126. [Google Scholar] [CrossRef]
- Singh, K.; Gaur, U.; Hall, K.; Mascoll, K.; Cohall, D.; Majumder, M.A. Teaching anatomy and dissection in an era of social distancing and remote learning. Adv. Hum. Biol. 2020, 10, 90. [Google Scholar] [CrossRef]
- Thomas, R.G.; John, N.W.; Delieu, J. Augmented Reality for Anatomical Education. J. Vis. Commun. Med. 2010, 33, 6–15. [Google Scholar] [CrossRef] [PubMed]
- Carroll, M.A.; McKenzie, A.; Tracy-Bee, M. Movement System Theory and Anatomical Competence: Threshold Concepts for Physical Therapist Anatomy Education. Anat. Sci. Educ. 2022, 15, 420–430. [Google Scholar] [CrossRef] [PubMed]
- Garg, A.X.; Norman, G.R.; Norman, G.; Sperotable, L. How Medical Students Learn Spatial Anatomy. Lancet 2001, 357, 363–364. [Google Scholar] [CrossRef] [PubMed]
- Kong, X.; Nie, L.; Zhang, H.; Wang, Z.; Ye, Q.; Tang, L.; Li, J.; Huang, W. Do Three-dimensional Visualization and Three-dimensional Printing Improve Hepatic Segment Anatomy Teaching? A Randomized Controlled Study. J. Surg. Educ. 2016, 73, 264–269. [Google Scholar] [CrossRef]
- Zhao, J.; Xu, X.; Jiang, H.; Ding, Y. The effectiveness of virtual reality-based technology on anatomy teaching: A meta-analysis of randomized controlled studies. BMC Med. Educ. 2020, 20, 127. [Google Scholar] [CrossRef]
- Stepan, K.; Zeiger, J.; Hanchuk, S.; Del Signore, A.; Shrivastava, R.; Govindaraj, S.; Iloreta, A. Immersive Virtual Reality as a Teaching Tool for Neuroanatomy: Immersive VR as a Neuroanatomy Teaching Tool. Int. Forum Allergy Rhinol. 2017, 7, 1006–1013. [Google Scholar] [CrossRef]
- Tene, T.; Vique López, D.F.; Valverde Aguirre, P.E.; Orna Puente, L.M.; Vacacela Gomez, C. Virtual reality and augmented reality in medical education: An umbrella review. Front. Digit. Health 2024, 6, 1365345. [Google Scholar] [CrossRef]
- Vozenilek, J. See One, Do One, Teach One: Advanced Technology in Medical Education. Acad. Emerg. Med. 2004, 11, 1149–1154. [Google Scholar] [CrossRef]
- Polavarapu, H.V.; Kulaylat, A.N.; Sun, S.; Hamed, O.H. 100 Years of Surgical Education: The Past, Present, and Future. Bull. Am. Coll. Surg. 2013, 98, 22–27. [Google Scholar]
- Higgins, M.; Madan, C.; Patel, R. Development and decay of procedural skills in surgery: A systematic review of the effectiveness of simulated-based medical education interventions. Surg. 2020, 19, e67–e77. [Google Scholar] [CrossRef] [PubMed]
- Berthold, D.P.; Muench, L.N.; Rupp, M.C.; Siebenlist, S.; Cote, M.P.; Mazzocca, A.D.; Quindlen, K. Head-Mounted Display Virtual Reality Is Effective in Orthopaedic Training: A Systematic Review. Arthrosc. Sport. Med. Rehabil. 2022, 4, e1843–e1849. [Google Scholar] [CrossRef] [PubMed]
- Taba, J.V.; Cortez, V.S.; Moraes, W.A.; Iuamoto, L.R.; Hsing, W.T.; Suzuki, M.O.; do Nascimento, F.S.; Pipek, L.Z.; de Mattos, V.C.; D’Albuquerque, E.C.; et al. The development of laparoscopic skills using virtual reality simulations: A systematic review. PLoS ONE 2021, 16, e0252609. [Google Scholar] [CrossRef] [PubMed]
- Logishetty, K.; Rudran, B.; Cobb, J.P. Virtual Reality Training Improves Trainee Performance in Total Hip Arthroplasty: A Randomized Controlled Trial. Bone Jt. J. 2019, 101-B, 1585–1592. [Google Scholar] [CrossRef]
- Verhey, J.; Haglin, J.; Verhey, E.; Hartigan, D. Virtual, augmented, and mixed reality applications in Orthopedic surgery. Int. J. Med. Robot. Comput. Assist. Surg. 2019, 16, e2067. [Google Scholar] [CrossRef] [PubMed]
- Leitritz, M.A.; Ziemssen, F.; Suesskind, D.; Partsch, M.; Voykov, B.; Bartz-Schmidt, K.U.; Szurman, G.B. Critical evaluation of the usability of augmented reality ophthalmoscopy for the training of inexperienced examiners. Retina 2014, 34, 785–791. [Google Scholar] [CrossRef]
- Muñoz, E.G.; Fabregat, R.; Bacca-Acosta, J.; Duque-Méndez, N.; Avila-Garzon, C. Augmented reality, virtual reality, and game technologies in ophthalmology training. Information 2022, 13, 222. [Google Scholar] [CrossRef]
- Yedidia, M.J. Effect of Communications Training on Medical Student Performance. JAMA 2003, 290, 1157. [Google Scholar] [CrossRef]
- Tan, Y.; Xu, W.; Li, S.; Chen, K. Augmented and Virtual Reality (AR/VR) for Education and Training in the AEC Industry: A Systematic Review of Research and Applications. Buildings 2022, 12, 1529. [Google Scholar] [CrossRef]
- Triola, M.; Feldman, H.; Kalet, A.L.; Zabar, S.; Kachur, E.K.; Gillespie, C.; Anderson, M.; Griesser, C.; Lipkin, M. A Randomized Trial of Teaching Clinical Skills Using Virtual and Live Standardized Patients. J. Gen. Intern. Med. 2006, 21, 424–429. [Google Scholar] [CrossRef]
- Real, F.J.; DeBlasio, D.; Beck, A.F.; Ollberding, N.J.; Davis, D.; Cruse, B.; Samaan, Z.; McLinden, D.; Klein, M.D. A Virtual Reality Curriculum for Pediatric Residents Decreases Rates of Influenza Vaccine Refusal. Acad. Pediatr. 2017, 17, 431–435. [Google Scholar] [CrossRef] [PubMed]
- Stefan, H.; Mortimer, M.; Horan, B. Evaluating the effectiveness of virtual reality for safety-relevant training: A systematic review. Virtual Real. 2023, 27, 2839–2869. [Google Scholar] [CrossRef]
- Prineas, S.; Mosier, K.; Mirko, C.; Guicciardi, S. Non-technical skills in healthcare. In Textbook of Patient Safety and Clinical Risk Management; Springer: Cham, Switzerland, 2021; pp. 413–434. [Google Scholar]
- McCloy, R.F.; Stone, R. Science, Medicine, and the Future. Virtual Reality in Surgery. BMJ 2001, 323, 912–915. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.; Egbue, O.; Palkie, B.; Madden, J. Active learning: Engaging students to maximize learning in an online course. Electron. J. E-Learn. 2017, 15, 107–115. [Google Scholar]
- Mathew, P.S.; Pillai, A.S. Role of immersive (XR) technologies in improving healthcare competencies: A review. Virtual and Augmented Reality in Education, Art, and Museums; IGI: Hershey, PA, USA, 2020; pp. 23–46. [Google Scholar]
- Herur-Raman, A.; Almeida, N.D.; Greenleaf, W.; Williams, D.; Karshenas, A.; Sherman, J.H. Next-Generation Simulation—Integrating Extended Reality Technology Into Medical Education. Front. Virtual Real. 2021, 2, 693399. [Google Scholar] [CrossRef]
- Moro, C.; Štromberga, Z.; Raikos, A.; Stirling, A. The Effectiveness of Virtual and Augmented Reality in Health Sciences and Medical Anatomy. Anat. Sci. Educ. 2017, 10, 549–559. [Google Scholar] [CrossRef]
- Curran, V.R.; Xu, X.; Aydin, M.Y.; Meruvia-Pastor, O. Use of extended reality in medical education: An integrative review. Med. Sci. Educ. 2023, 33, 275–286. [Google Scholar] [CrossRef]
- Saredakis, D.; Szpak, A.; Birckhead, B.; Keage, H.A.; Rizzo, A.; Loetscher, T. Factors associated with virtual reality sickness in head-mounted displays: A systematic review and meta-analysis. Front. Hum. Neurosci. 2020, 14, 96. [Google Scholar] [CrossRef]
- Sandrone, S. Medical education in the metaverse. Nat. Med. 2022, 28, 2456–2457. [Google Scholar] [CrossRef]
- Takata, R.; Kanehira, M.; Kato, Y.; Matsuura, T.; Kato, R.; Maekawa, S.; Obara, W. Improvement of three-dimensional motion sickness using a virtual reality simulator for robot-assisted surgery in undergraduate medical students: A prospective observational study. BMC Med. Educ. 2021, 21, 498. [Google Scholar] [CrossRef]
- Wersényi, G. Perception Accuracy of a Multi-Channel Tactile Feedback System for Assistive Technology. Sensors 2022, 22, 8962. [Google Scholar] [CrossRef] [PubMed]
- Sacchetti, S.; McGlone, F.; Cazzato, V.; Mirams, L. The off-line effect of affective touch on multisensory integration and tactile perceptual accuracy during the somatic signal detection task. PLoS ONE 2021, 16, e0261060. [Google Scholar] [CrossRef] [PubMed]
- Syahry, A.; Basuki, D.K.; Sukaridhoto, S.; Budiarti, R.P.N.; Hanifati, K.; Muntahir, I. Implementation of Augmented Reality in Medical Education. In Proceedings of the 2022 International Electronics Symposium (IES), Surabaya, Indonesia, 9–11 August 2022; pp. 684–690. [Google Scholar]
- El-Araby, N.; Kocemba, J.; Dufeau, D. Limitations of Visualization Technology and Virtual Instruction in Medical Education. FASEB J. 2021, 35. [Google Scholar] [CrossRef]
- Celebi, K.C.; Bailey, S.K.; Burns, M.W.; Bansal, K. Is virtual reality streaming ready for remote medical education? measuring latency of stereoscopic VR for telementoring. In Proceedings of the Human Factors and Ergonomics Society Annual Meeting, Baltimore, MD, USA, 3–8 October 2021; Volume 65, pp. 757–761. [Google Scholar]
- Xu, X.; Mangina, E.; Campbell, A.G. HMD-based virtual and augmented reality in medical education: A systematic review. Front. Virtual Real. 2021, 2, 692103. [Google Scholar] [CrossRef]
- Bracq, M.S.; Michinov, E.; Jannin, P. Virtual reality simulation in nontechnical skills training for healthcare professionals: A systematic review. Simul. Healthc. 2019, 14, 188–194. [Google Scholar] [CrossRef]
- Birkheim, S.L.; Calogiuri, G.; Martinsen, R. Advancing immersive virtual reality-based simulation practices: Developing an evidence-based and theory-driven pedagogical framework for VR-based simulations of non-technical skills among healthcare professionals. Interact. Learn. Environ. 2023, 1–13. [Google Scholar] [CrossRef]
- da Cruz Torquato, M.; Menezes, J.M.; Belchior, G.; Mazzotti, F.P.; Bittar, J.S.; Dos Santos, G.G.R.; Ruiz, T.M.; de Oliveira Pereira, W.; Paes, A.T. Virtual reality as a complementary learning tool in anatomy education for medical students. Med. Sci. Educ. 2023, 33, 507–516. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).